
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Complications
- Switching from Conventional Fibrates to Pemafibrate Has Beneficial Effects on the Renal Function of Diabetic Subjects with Chronic Kidney Disease
- Rimi Izumihara, Hiroshi Nomoto, Kenichi Kito, Yuki Yamauchi, Kazuno Omori, Yui Shibayama, Shingo Yanagiya, Aika Miya, Hiraku Kameda, Kyu Yong Cho, So Nagai, Ichiro Sakuma, Akinobu Nakamura, Tatsuya Atsumi, on Behalf of the PARM-TD Study Group
- Received October 15, 2023 Accepted November 22, 2023 Published online February 29, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0370 [Epub ahead of print]
- 707 View
- 129 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Fibrates have renal toxicity limiting their use in subjects with chronic kidney disease (CKD). However, pemafibrate has fewer toxic effects on renal function. In the present analysis, we evaluated the effects of pemafibrate on the renal function of diabetic subjects with or without CKD in a real-world clinical setting.
Methods
We performed a sub-analysis of data collected during a multi-center, prospective, observational study of the effects of pemafibrate on lipid metabolism in subjects with type 2 diabetes mellitus complicated by hypertriglyceridemia (the PARM-T2D study). The participants were allocated to add pemafibrate to their existing regimen (ADD-ON), switch from their existing fibrate to pemafibrate (SWITCH), or continue conventional therapy (CTRL). The changes in estimated glomerular filtration rate (eGFR) over 52 weeks were compared among these groups as well as among subgroups created according to CKD status.
Results
Data for 520 participants (ADD-ON, n=166; SWITCH, n=96; CTRL, n=258) were analyzed. Of them, 56.7% had CKD. The eGFR increased only in the SWITCH group, and this trend was also present in the CKD subgroup (P<0.001). On the other hand, eGFR was not affected by switching in participants with severe renal dysfunction (G3b or G4) and/or macroalbuminuria. Multivariate analysis showed that being older and a switch from fenofibrate were associated with elevation in eGFR (both P<0.05).
Conclusion
A switch to pemafibrate may be associated with an elevation in eGFR, but to a lesser extent in patients with poor renal function.
- Others
- Risk Prediction and Management of Chronic Kidney Disease in People Living with Type 2 Diabetes Mellitus
- Ying-Guat Ooi, Tharsini Sarvanandan, Nicholas Ken Yoong Hee, Quan-Hziung Lim, Sharmila S. Paramasivam, Jeyakantha Ratnasingam, Shireene R. Vethakkan, Soo-Kun Lim, Lee-Ling Lim
- Diabetes Metab J. 2024;48(2):196-207. Published online January 26, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0244
- 1,862 View
- 352 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
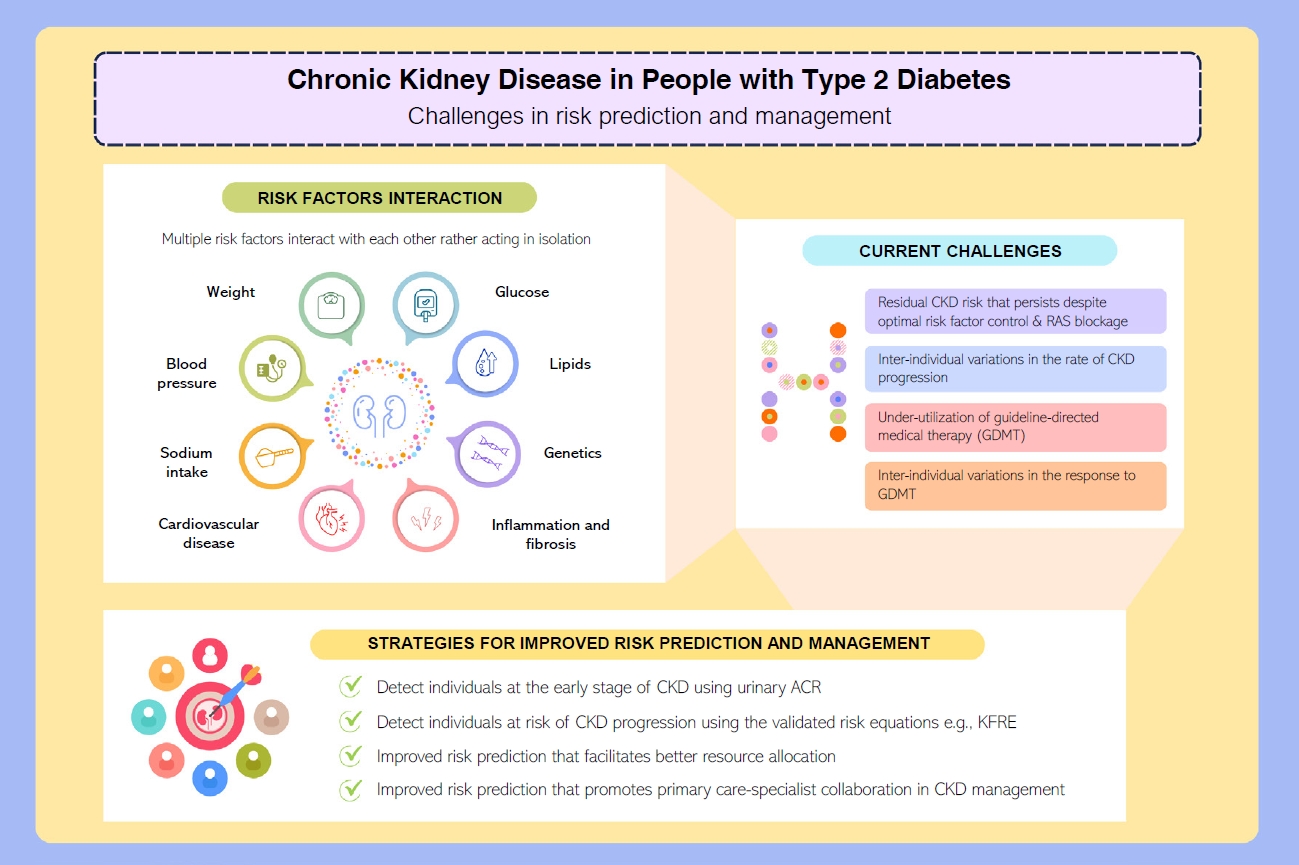
ePub - People with type 2 diabetes mellitus have increased risk of chronic kidney disease and atherosclerotic cardiovascular disease. Improved care delivery and implementation of guideline-directed medical therapy have contributed to the declining incidence of atherosclerotic cardiovascular disease in high-income countries. By contrast, the global incidence of chronic kidney disease and associated mortality is either plateaued or increased, leading to escalating direct and indirect medical costs. Given limited resources, better risk stratification approaches to identify people at risk of rapid progression to end-stage kidney disease can reduce therapeutic inertia, facilitate timely interventions and identify the need for early nephrologist referral. Among people with chronic kidney disease G3a and beyond, the kidney failure risk equations (KFRE) have been externally validated and outperformed other risk prediction models. The KFRE can also guide the timing of preparation for kidney replacement therapy with improved healthcare resources planning and may prevent multiple complications and premature mortality among people with chronic kidney disease with and without type 2 diabetes mellitus. The present review summarizes the evidence of KFRE to date and call for future research to validate and evaluate its impact on cardiovascular and mortality outcomes, as well as healthcare resource utilization in multiethnic populations and different healthcare settings.
- Cardiovascular Risk/Epidemiology
- Glycemic Control and Adverse Clinical Outcomes in Patients with Chronic Kidney Disease and Type 2 Diabetes Mellitus: Results from KNOW-CKD
- Ga Young Heo, Hee Byung Koh, Hyung Woo Kim, Jung Tak Park, Tae-Hyun Yoo, Shin-Wook Kang, Jayoun Kim, Soo Wan Kim, Yeong Hoon Kim, Su Ah Sung, Kook-Hwan Oh, Seung Hyeok Han
- Diabetes Metab J. 2023;47(4):535-546. Published online April 25, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0112
- 2,661 View
- 162 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
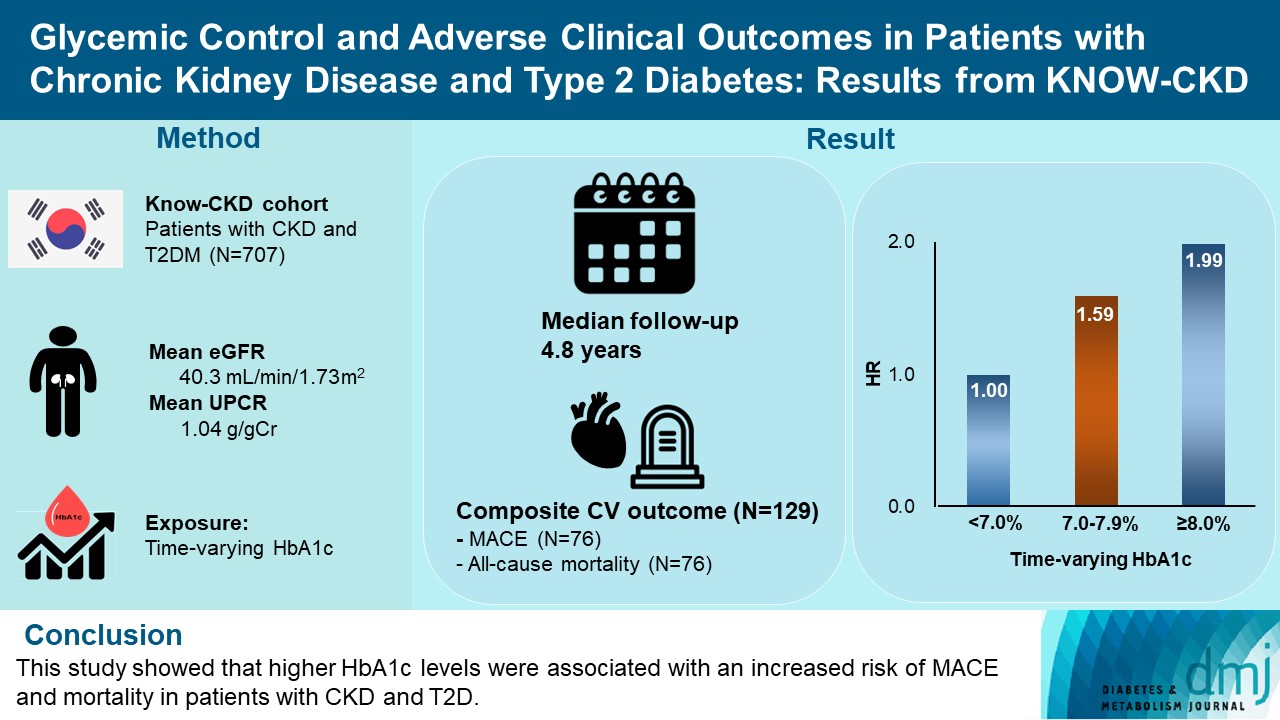
The optimal level of glycosylated hemoglobin (HbA1c) to prevent adverse clinical outcomes is unknown in patients with chronic kidney disease (CKD) and type 2 diabetes mellitus (T2DM).
Methods
We analyzed 707 patients with CKD G1-G5 without kidney replacement therapy and T2DM from the KoreaN Cohort Study for Outcome in Patients With Chronic Kidney Disease (KNOW-CKD), a nationwide prospective cohort study. The main predictor was time-varying HbA1c level at each visit. The primary outcome was a composite of development of major adverse cardiovascular events (MACEs) or all-cause mortality. Secondary outcomes included the individual endpoint of MACEs, all-cause mortality, and CKD progression. CKD progression was defined as a ≥50% decline in the estimated glomerular filtration rate from baseline or the onset of end-stage kidney disease.
Results
During a median follow-up of 4.8 years, the primary outcome occurred in 129 (18.2%) patients. In time-varying Cox model, the adjusted hazard ratios (aHRs) for the primary outcome were 1.59 (95% confidence interval [CI], 1.01 to 2.49) and 1.99 (95% CI, 1.24 to 3.19) for HbA1c levels of 7.0%–7.9% and ≥8.0%, respectively, compared with <7.0%. Additional analysis of baseline HbA1c levels yielded a similar graded association. In secondary outcome analyses, the aHRs for the corresponding HbA1c categories were 2.17 (95% CI, 1.20 to 3.95) and 2.26 (95% CI, 1.17 to 4.37) for MACE, and 1.36 (95% CI, 0.68 to 2.72) and 2.08 (95% CI, 1.06 to 4.05) for all-cause mortality. However, the risk of CKD progression did not differ between the three groups.
Conclusion
This study showed that higher HbA1c levels were associated with an increased risk of MACE and mortality in patients with CKD and T2DM. -
Citations
Citations to this article as recorded by- The Beneficial Effect of Glycemic Control against Adverse Outcomes in Patients with Type 2 Diabetes Mellitus and Chronic Kidney Disease
Dong-Hwa Lee
Diabetes & Metabolism Journal.2023; 47(4): 484. CrossRef - Prevalence and predictors of chronic kidney disease among type 2 diabetic patients worldwide, systematic review and meta-analysis
Eneyew Talie Fenta, Habitu Birhan Eshetu, Natnael Kebede, Eyob Ketema Bogale, Amare Zewdie, Tadele Derbew Kassie, Tadele Fentabil Anagaw, Elyas Melaku Mazengia, Sintayehu Shiferaw Gelaw
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Efficacy and safety of teneligliptin in patients with type 2 diabetes mellitus: a Bayesian network meta-analysis
Miao Zhu, Ruifang Guan, Guo Ma
Frontiers in Endocrinology.2023;[Epub] CrossRef
- The Beneficial Effect of Glycemic Control against Adverse Outcomes in Patients with Type 2 Diabetes Mellitus and Chronic Kidney Disease
- Metabolic Risk/Epidemiology
- Novel Asian-Specific Visceral Adiposity Indices Are Associated with Chronic Kidney Disease in Korean Adults
- Jonghwa Jin, Hyein Woo, Youngeun Jang, Won-Ki Lee, Jung-Guk Kim, In-Kyu Lee, Keun-Gyu Park, Yeon-Kyung Choi
- Diabetes Metab J. 2023;47(3):426-436. Published online March 6, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0099
- 2,480 View
- 128 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
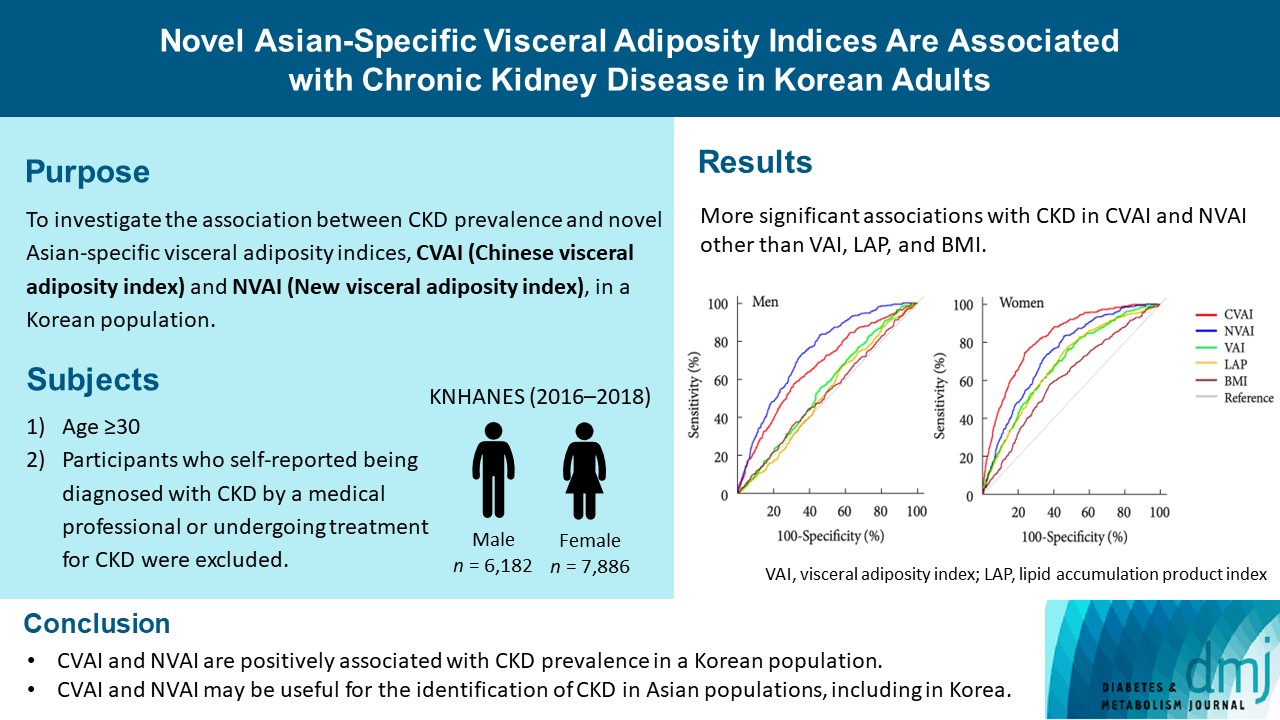
The Chinese visceral adiposity index (CVAI) and new visceral adiposity index (NVAI) are novel indices of visceral adiposity used to predict metabolic and cardiovascular diseases in Asian populations. However, the relationships of CVAI and NVAI with chronic kidney disease (CKD) have not been investigated. We aimed to characterize the relationships of CVAI and NVAI with the prevalence of CKD in Korean adults.
Methods
A total of 14,068 participants in the 7th Korea National Health and Nutrition Examination Survey (6,182 men and 7,886 women) were included. Receiver operating characteristic (ROC) analyses were employed to compare the associations between indices of adiposity and CKD, and a logistic regression model was used to characterize the relationships of CVAI and NVAI with CKD prevalence.
Results
The areas under the ROC curves for CVAI and NVAI were significantly larger than for the other indices, including the visceral adiposity index and lipid accumulation product, in both men and women (all P<0.001). In addition, high CVAI or NVAI was significantly associated with a high CKD prevalence in both men (odds ratio [OR], 2.14; 95% confidence interval [CI], 1.31 to 3.48 in CVAI and OR, 6.47; 95% CI, 2.91 to 14.38 in NVAI, P<0.05) and women (OR, 4.87; 95% CI, 1.85 to 12.79 in CVAI and OR, 3.03; 95% CI, 1.35 to 6.82 in NVAI, P<0.05); this association remained significant after adjustment for multiple confounding factors in men and women.
Conclusion
CVAI and NVAI are positively associated with CKD prevalence in a Korean population. CVAI and NVAI may be useful for the identification of CKD in Asian populations, including in Korea. -
Citations
Citations to this article as recorded by- Association between Chinese visceral adiposity index and risk of stroke incidence in middle-aged and elderly Chinese population: evidence from a large national cohort study
Zenglei Zhang, Lin Zhao, Yiting Lu, Xu Meng, Xianliang Zhou
Journal of Translational Medicine.2023;[Epub] CrossRef
- Association between Chinese visceral adiposity index and risk of stroke incidence in middle-aged and elderly Chinese population: evidence from a large national cohort study
- Pathophysiology
- Renoprotective Mechanism of Sodium-Glucose Cotransporter 2 Inhibitors: Focusing on Renal Hemodynamics
- Nam Hoon Kim, Nan Hee Kim
- Diabetes Metab J. 2022;46(4):543-551. Published online July 27, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0209
- 6,382 View
- 675 Download
- 11 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
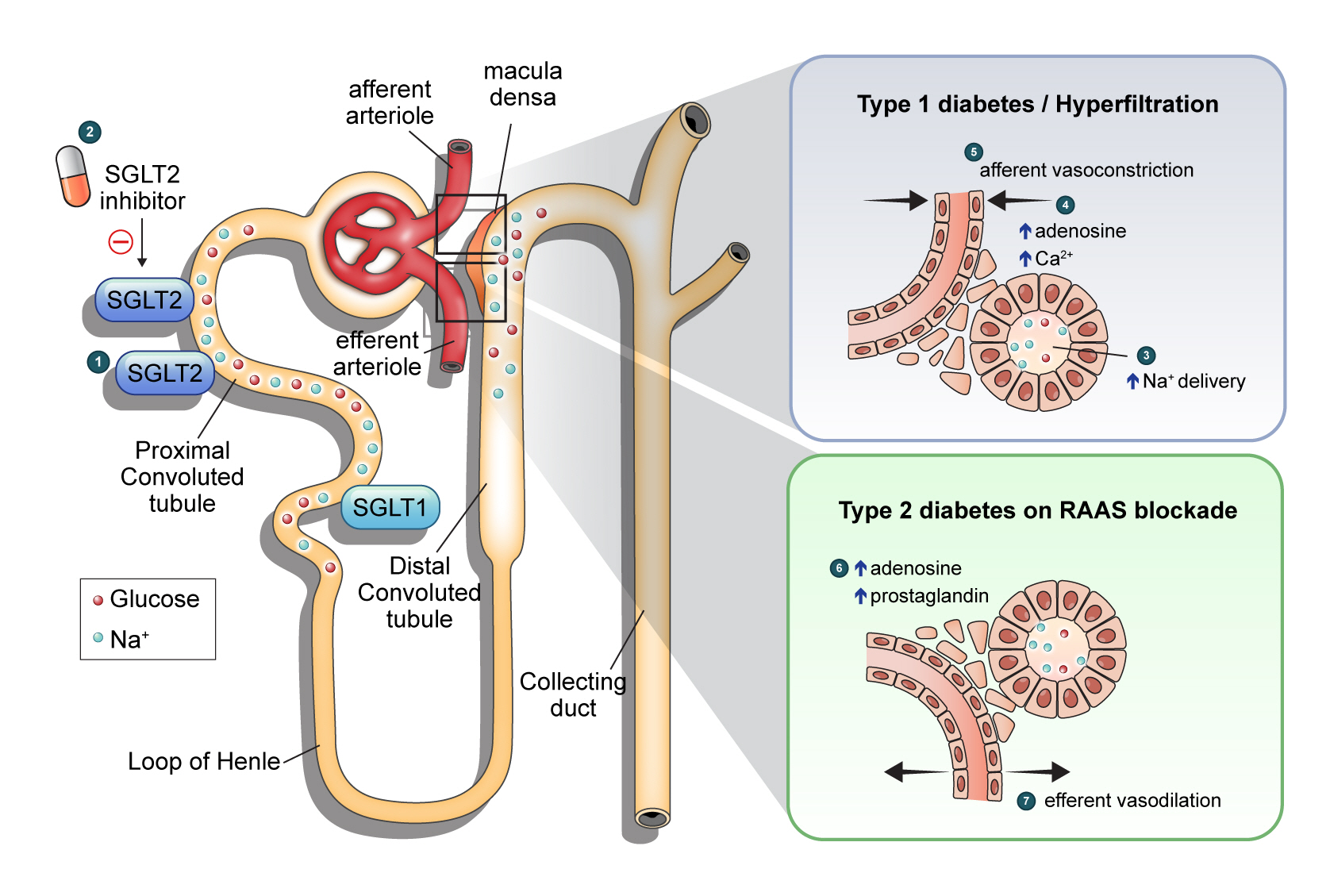
ePub - Diabetic kidney disease (DKD) is a prevalent renal complication of diabetes mellitus that ultimately develops into end-stage kidney disease (ESKD) when not managed appropriately. Substantial risk of ESKD remains even with intensive management of hyperglycemia and risk factors of DKD and timely use of renin-angiotensin-aldosterone inhibitors. Sodium-glucose cotransporter 2 (SGLT2) inhibitors reduce hyperglycemia primarily by inhibiting glucose and sodium reabsorption in the renal proximal tubule. Currently, their effects expand to prevent or delay cardiovascular and renal adverse events, even in those without diabetes. In dedicated renal outcome trials, SGLT2 inhibitors significantly reduced the risk of composite renal adverse events, including the development of ESKD or renal replacement therapy, which led to the positioning of SGLT2 inhibitors as the mainstay of chronic kidney disease management. Multiple mechanisms of action of SGLT2 inhibitors, including hemodynamic, metabolic, and anti-inflammatory effects, have been proposed. Restoration of tubuloglomerular feedback is a plausible explanation for the alteration in renal hemodynamics induced by SGLT2 inhibition and for the associated renal benefit. This review discusses the clinical rationale and mechanism related to the protection SGLT2 inhibitors exert on the kidney, focusing on renal hemodynamic effects.
-
Citations
Citations to this article as recorded by- Using intravoxel incoherent motion imaging to evaluate uric acid-induced renal injury and efficacy after treatment
Zhong-Yuan Cheng, Shang-Ao Gong, Ping-Kang Chen, Zong-Chao Yu, Chen Qiu, Ji-Xin Lin, Jia-Bin Mo, Long Qian, You-Zhen Feng, Xiang-Ran Cai
British Journal of Radiology.2024; 97(1153): 274. CrossRef - Rethinking eGFR Comparisons in SGLT2 Inhibitor Research
Yuzuru Ohshiro
Journal of the American College of Cardiology.2024; 83(9): e87. CrossRef - SGLT2 Inhibitors and Diabetes: Where Does It Come from and Where Does It Go?
Ji Yoon Kim, Sin Gon Kim
The Journal of Korean Diabetes.2024; 25(1): 9. CrossRef - Cardiorenal outcomes and mortality after sodium‐glucose cotransporter‐2 inhibitor initiation in type 2 diabetes patients with percutaneous coronary intervention history
Jin Hwa Kim, Young Sang Lyu, BongSeong Kim, Mee Kyung Kim, Sang Yong Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Baseline eGFR, albuminuria and renal outcomes in patients with SGLT2 inhibitor treatment: an updated meta-analysis
Yunke Ma, Chu Lin, Xiaoling Cai, Suiyuan Hu, Xingyun Zhu, Fang Lv, Wenjia Yang, Linong Ji
Acta Diabetologica.2023; 60(3): 435. CrossRef - Effects of sodium-glucose cotransporter 2 inhibitors on renal risk factors in patients with abnormal glucose metabolism: a meta-analysis of randomized controlled trials
Mengnan Li, Jian Zhang, Guimei Yang, Jiaxin Zhang, Minmin Han, Yi Zhang, Yunfeng Liu
European Journal of Clinical Pharmacology.2023; 79(6): 859. CrossRef - Age at Mortality in Patients with Type 2 Diabetes Who Underwent Kidney Transplantation: An Analysis of Data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
Sun Ok Song, Eugene Han, Kang Ju Son, Bong-Soo Cha, Byung-Wan Lee
Journal of Clinical Medicine.2023; 12(9): 3160. CrossRef - Exposure–Response Analysis of the Sodium–Glucose Cotransporter-2 Inhibitors Dapagliflozin and Empagliflozin on Kidney Hemodynamics in Patients with Type 2 Diabetes
Sjoukje van der Hoek, Jeroen V. Koomen, Erik J. M. van Bommel, Charlotte M. Mosterd, Rosalie A. Scholtes, Anne C. Hesp, Jasper Stevens, Daniel H. van Raalte, Hiddo J. L. Heerspink
Journal of Personalized Medicine.2023; 13(5): 747. CrossRef - Osteopontin as a Biomarker in Chronic Kidney Disease
Satyesh K. Sinha, Michael Mellody, Maria Beatriz Carpio, Robert Damoiseaux, Susanne B. Nicholas
Biomedicines.2023; 11(5): 1356. CrossRef - Increased expression of sodium-glucose cotransporter 2 and O-GlcNAcylation in hepatocytes drives non-alcoholic steatohepatitis
Hye Jin Chun, Eun Ran Kim, Minyoung Lee, Da Hyun Choi, Soo Hyun Kim, Eugene Shin, Jin-Hong Kim, Jin Won Cho, Dai Hoon Han, Bong-Soo Cha, Yong-ho Lee
Metabolism.2023; 145: 155612. CrossRef - Synthesis and biological profile of benzoxazolone derivatives
Parteek Prasher, Tanisqa Mall, Mousmee Sharma
Archiv der Pharmazie.2023;[Epub] CrossRef - SGLT2 inhibitors prevent LPS-induced M1 macrophage polarization and alleviate inflammatory bowel disease by downregulating NHE1 expression
Ye Jin Kim, Jonghwa Jin, Dong-Ho Kim, Daehoon Kim, You Mie Lee, Jun-Kyu Byun, Yeon-Kyung Choi, Keun-Gyu Park
Inflammation Research.2023; 72(10-11): 1981. CrossRef
- Using intravoxel incoherent motion imaging to evaluate uric acid-induced renal injury and efficacy after treatment
- Complications
- Advanced Liver Fibrosis Is Associated with Chronic Kidney Disease in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
- Da Hea Seo, Young Ju Suh, Yongin Cho, Seong Hee Ahn, Seongha Seo, Seongbin Hong, Yong-ho Lee, Young Ju Choi, Eunjig Lee, So Hun Kim
- Diabetes Metab J. 2022;46(4):630-639. Published online January 26, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0130
- 5,532 View
- 274 Download
- 14 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Nonalcoholic fatty liver disease (NAFLD) is associated with chronic kidney disease (CKD). However, the causal relationship between NAFLD and CKD is uncertain, particularly in patients with type 2 diabetes mellitus (T2DM). We aimed to investigate the association between the presence and severity of NAFLD and incident CKD in patients with T2DM.
Methods
In this longitudinal cohort study of patients with T2DM, 3,188 patients with preserved renal function were followed up for the occurrence of incident CKD. NAFLD was defined as the presence of hepatic steatosis on ultrasonography, without any other causes of chronic liver disease. Advanced liver fibrosis of NAFLD was defined as a fibrosis-4 index ≥2.67. CKD was defined as an estimated glomerular filtration rate <60 mL/min/1.73 m2.
Results
At baseline, 1,729 (54.2%) patients had NAFLD, of whom 94 (5.4%) had advanced liver fibrosis. During the follow-up of 8.3±3.6 years, 472 (14.8%) patients developed incident CKD: 220 (15.1%) in the non-NAFLD group, 231 (14.1%) in the NAFLD without advanced fibrosis group and 28 (31.1%) in the NAFLD with advanced fibrosis group. There was no increased risk of incident CKD in the NAFLD group compared to the non-NAFLD group (P=0.435). However, among patients with NAFLD, advanced liver fibrosis was associated with an increased risk of CKD (adjusted hazard ratio, 1.75; 95% confidence interval, 1.15 to 2.66; P=0.009).
Conclusion
Advanced liver fibrosis in patients with NAFLD is independently associated with an increased risk of incident CKD in patients with T2DM. -
Citations
Citations to this article as recorded by- Esteatosis hepática metabólica y nefropatía diabética: una llamada a la acción
Salvador Benlloch, Francesc Moncho, Jose Luis Górriz
Nefrología.2024; 44(2): 129. CrossRef - Longitudinal Outcomes Associated With Metabolic Dysfunction-Associated Steatotic Liver Disease: A Meta-analysis of 129 Studies
Kai En Chan, Elden Yen Hng Ong, Charlotte Hui Chung, Christen En Ya Ong, Benjamin Koh, Darren Jun Hao Tan, Wen Hui Lim, Jie Ning Yong, Jieling Xiao, Zhen Yu Wong, Nicholas Syn, Apichat Kaewdech, Margaret Teng, Jiong-Wei Wang, Nicholas Chew, Dan Yock Young
Clinical Gastroenterology and Hepatology.2024; 22(3): 488. CrossRef - Association of NAFLD/NASH, and MAFLD/MASLD with chronic kidney disease: an updated narrative review
Amedeo Lonardo
Metabolism and Target Organ Damage.2024;[Epub] CrossRef - Targeting metabolic-associated fatty liver disease in diabetic kidney disease: A call to action
Salvador Benlloch, Francesc Moncho, Jose Luis Górriz
Nefrología (English Edition).2024;[Epub] CrossRef - MAFLD and NAFLD in the prediction of incident chronic kidney disease
So Yoon Kwon, Jiyun Park, So Hee Park, You-Bin Lee, Gyuri Kim, Kyu Yeon Hur, Janghyun Koh, Jae Hwan Jee, Jae Hyeon Kim, Mira Kang, Sang-Man Jin
Scientific Reports.2023;[Epub] CrossRef - Associations of non-invasive indices of liver steatosis and fibrosis with progressive kidney impairment in adults with type 2 diabetes
Mei Chung Moh, Sharon Li Ting Pek, Kenny Ching Pan Sze, Serena Low, Tavintharan Subramaniam, Keven Ang, Wern Ee Tang, Simon Biing Ming Lee, Chee Fang Sum, Su Chi Lim
Acta Diabetologica.2023; 60(6): 827. CrossRef - Pancreatic beta-cell specific BAG3 knockout results in chronic hyperinsulinemia inducing insulin resistance
Verena Damiani, Alessia Lamolinara, Ilaria Cicalini, Maria Concetta Cufaro, Francesco Del Pizzo, Federica Di Marco, Piero Del Boccio, Beatrice Dufrusine, Michael Hahne, Rossano Lattanzio, Damiana Pieragostino, Manuela Iezzi, Massimo Federici, Maria Cateri
Molecular Metabolism.2023; 74: 101752. CrossRef - Utility of non-invasive liver fibrosis markers to predict the incidence of chronic kidney disease (CKD): A systematic review, meta-analysis, and meta-regression
Rudi Supriyadi, Theo Audi Yanto, Timotius Ivan Hariyanto, Ketut Suastika
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(8): 102814. CrossRef - Significance of Diabetic Kidney Disease Biomarkers in Predicting Metabolic-Associated Fatty Liver Disease
Jaehyun Bae, Byung-Wan Lee
Biomedicines.2023; 11(7): 1928. CrossRef - Hepatic Fibrosis Evaluated in Patients with Type 2 Diabetes with and without Chronic Kidney Disease
Therese Adrian, Mads Hornum, Filip Krag Knop, Karl Bang Christensen, Thomas Almdal, Peter Rossing, Lisa Í Lídaa, Niels Søndergaard Heinrich, Vincent Oltman Boer, Anouk Marsman, Esben Thade Petersen, Hartwig Roman Siebner, Bo Feldt-Rasmussen
Nephron.2023; 147(11): 673. CrossRef - Clinical Interest of Serum Alpha-2 Macroglobulin, Apolipoprotein A1, and Haptoglobin in Patients with Non-Alcoholic Fatty Liver Disease, with and without Type 2 Diabetes, before or during COVID-19
Olivier Deckmyn, Thierry Poynard, Pierre Bedossa, Valérie Paradis, Valentina Peta, Raluca Pais, Vlad Ratziu, Dominique Thabut, Angelique Brzustowski, Jean-François Gautier, Patrice Cacoub, Dominique Valla
Biomedicines.2022; 10(3): 699. CrossRef - Fibrosis Risk in Nonalcoholic Fatty Liver Disease Is Related to Chronic Kidney Disease in Older Type 2 Diabetes Patients
Yifan Sun, Liang Hong, Zhe Huang, Lihong Wang, Yanqin Xiong, Shuhang Zong, Rui Zhang, Jun Liu, Shufei Zang
The Journal of Clinical Endocrinology & Metabolism.2022; 107(9): e3661. CrossRef - Beyond Liver Disease: Non-Alcoholic Fatty Liver Disease and Advanced Liver Fibrosis in Kidney Disease
Eugene Han
Diabetes & Metabolism Journal.2022; 46(4): 564. CrossRef - A higher FIB‐4 index is associated with an increased incidence of renal failure in the general population
Eva Maria Schleicher, Simon Johannes Gairing, Peter Robert Galle, Julia Weinmann‐Menke, Jörn M. Schattenberg, Karel Kostev, Christian Labenz
Hepatology Communications.2022; 6(12): 3505. CrossRef - Advanced Liver Fibrosis Is Associated with Chronic Kidney Disease in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2022;46:630-9)
Ji Hye Huh
Diabetes & Metabolism Journal.2022; 46(6): 953. CrossRef - Advanced Liver Fibrosis Is Associated with Chronic Kidney Disease in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2022;46:630-9)
Da Hea Seo, So Hun Kim
Diabetes & Metabolism Journal.2022; 46(6): 956. CrossRef
- Esteatosis hepática metabólica y nefropatía diabética: una llamada a la acción
- Cardiovascular Risk/Epidemiology
- Performance of Diabetes and Kidney Disease Screening Scores in Contemporary United States and Korean Populations
- Liela Meng, Keun-Sang Kwon, Dae Jung Kim, Yong-ho Lee, Jeehyoung Kim, Abhijit V. Kshirsagar, Heejung Bang
- Diabetes Metab J. 2022;46(2):273-285. Published online September 9, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0054
- 65,535 View
- 239 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Risk assessment tools have been actively studied, and they summarize key predictors with relative weights/importance for a disease. Currently, standardized screening scores for type 2 diabetes mellitus (DM) and chronic kidney disease (CKD)—two key global health problems—are available in United States and Korea. We aimed to compare and evaluate screening scores for DM (or combined with prediabetes) and CKD, and assess the risk in contemporary United States and Korean populations.
Methods
Four (2×2) models were evaluated in the United States-National Health and Nutrition Examination Survey (NHANES 2015–2018) and Korea-NHANES (2016–2018)—8,928 and 16,209 adults. Weighted statistics were used to describe population characteristics. We used logistic regression for predictors in the models to assess associations with study outcomes (undiagnosed DM and CKD) and diagnostic measures for temporal and cross-validation.
Results
Korean adult population (mean age 47.5 years) appeared to be healthier than United States counterpart, in terms of DM and CKD risks and associated factors, with exceptions of undiagnosed DM, prediabetes and prehypertension. Models performed well in own country and external populations regarding predictor-outcome association and discrimination. Risk tests (high vs. low) showed area under the curve >0.75, sensitivity >84%, specificity >45%, positive predictive value >8%, and negative predictive value >99%. Discrimination was better for DM, compared to the combined outcome of DM and prediabetes, and excellent for CKD due to age.
Conclusion
Four easy-to-use screening scores for DM and CKD are well-validated in contemporary United States and Korean populations. Prevention of DM and CKD may serve as first-step in public health, with these self-assessment tools as basic tools to help health education and disparity. -
Citations
Citations to this article as recorded by- A meta‐analysis of diabetes risk prediction models applied to prediabetes screening
Yujin Liu, Sunrui Yu, Wenming Feng, Hangfeng Mo, Yuting Hua, Mei Zhang, Zhichao Zhu, Xiaoping Zhang, Zhen Wu, Lanzhen Zheng, Xiaoqiu Wu, Jiantong Shen, Wei Qiu, Jianlin Lou
Diabetes, Obesity and Metabolism.2024; 26(5): 1593. CrossRef - Performance Analysis and Assessment of Type 2 Diabetes Screening Scores in Patients with Non-Alcoholic Fatty Liver Disease
Norma Latif Fitriyani, Muhammad Syafrudin, Siti Maghfirotul Ulyah, Ganjar Alfian, Syifa Latif Qolbiyani, Chuan-Kai Yang, Jongtae Rhee, Muhammad Anshari
Mathematics.2023; 11(10): 2266. CrossRef - A Comprehensive Analysis of Chinese, Japanese, Korean, US-PIMA Indian, and Trinidadian Screening Scores for Diabetes Risk Assessment and Prediction
Norma Latif Fitriyani, Muhammad Syafrudin, Siti Maghfirotul Ulyah, Ganjar Alfian, Syifa Latif Qolbiyani, Muhammad Anshari
Mathematics.2022; 10(21): 4027. CrossRef
- A meta‐analysis of diabetes risk prediction models applied to prediabetes screening
- Complications
- High Incidence of Chronic Kidney Disease among Iranian Diabetic Adults: Using CKD-EPI and MDRD Equations for Estimated Glomerular Filtration Rate
- Seyyed Saeed Moazzeni, Reyhane Hizomi Arani, Mitra Hasheminia, Maryam Tohidi, Fereidoun Azizi, Farzad Hadaegh
- Diabetes Metab J. 2021;45(5):684-697. Published online March 16, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0109
- 5,828 View
- 157 Download
- 13 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To investigate the population based incidence rate of chronic kidney disease (CKD) and its potential risk factors among Iranian diabetic adults during over 14 years of follow-up.
Methods
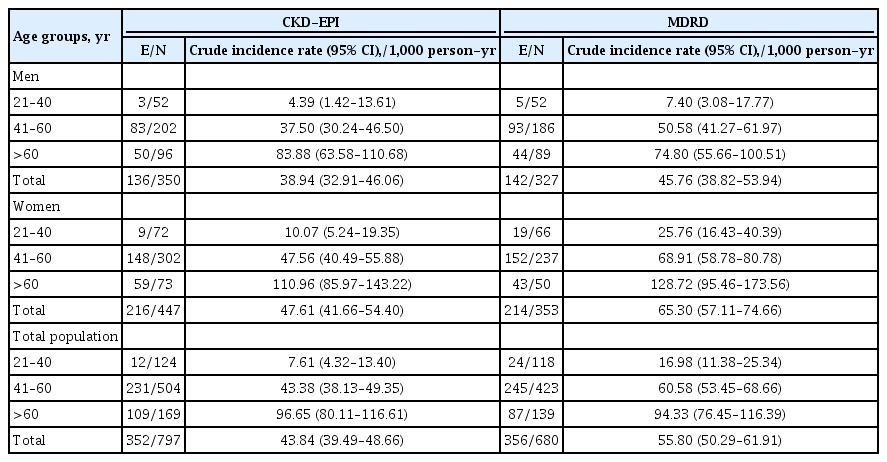
Two different equations (Chronic Kidney Disease Epidemiology Collaboration [CKD-EPI] and Modification of Diet in Renal Disease [MDRD]) were applied for the calculating the estimated glomerular filtration rate (eGFR). Among a total of 1,374 diabetic Tehranian adults, 797 and 680 individuals were eligible for CKD-EPI and MDRD analyses, respectively. CKD was defined as eGFR lower than 60 mL/min/1.73 m2. Multivariable Cox proportional hazard models were used to estimate the hazard ratios (HRs) and 95% confidence intervals (CI) for all potential risk factors.
Results
The incidence rates (95% CI) of CKD per 1,000 person-years were 43.84 (39.49 to 48.66) and 55.80 (50.29 to 61.91) based on CKD-EPI and MDRD equations, respectively. Being older, a history of cardiovascular disease, and having lower levels of eGFR were significant risk factors in both equations. Moreover, in CKD-EPI, using glucose-lowering medications and hypertension, and in MDRD, female sex and fasting plasma glucose ≥10 mmol/L were also independent risk factors. Regarding the discrimination index, CKD-EPI equation showed a higher range of C-index for the predicted probability of incident CKD in the full-adjusted model, compared to MDRD equation (0.75 [0.72 to 0.77] vs. 0.69 [0.66 to 0.72]).
Conclusion
We found an incidence rate of more than 4%/year for CKD development among our Iranian diabetic population. Compared to MDRD, it can be suggested that CKD-EPI equation can be a better choice to use for prediction models of incident CKD among the Iranian diabetic populations. -
Citations
Citations to this article as recorded by- The Effect of the Holy Quran Recitation on Inflammatory Markers in Hemodialysis Patients in Iran: A Randomized Clinical Trial
Maedeh Teimourzadeh, Hassan Babamohamadi, Maliheh Yarmohamadi, Raheb Ghorbani, Harold G. Koenig
Journal of Religion and Health.2024;[Epub] CrossRef - Prevalence of anemia and its associated factors among patients with type 2 diabetes mellitus in a referral diabetic clinic in the north of Iran
Reyhane Hizomi Arani, Farima Fakhri, Mohammad Naeimi Tabiee, Fatemeh Talebi, Zahra Talebi, Negin Rashidi, Maryam Zahedi
BMC Endocrine Disorders.2023;[Epub] CrossRef - The association between fasting plasma glucose variability and incident eGFR decline: evidence from two cohort studies
Niloofar Deravi, Yasaman Sharifi, Fatemeh Koohi, Seyed Saeed Tamehri Zadeh, Soroush Masrouri, Fereidoun Azizi, Farzad Hadaegh
BMC Public Health.2023;[Epub] CrossRef - Low LncRNA LUCAT1 Expression Assists in the Diagnosis of Chronic Heart Failure and Predicts Poor Prognosis
Jian Wang, Xujin Wu, Li Wang, Chengyong Zhao
International Heart Journal.2023; 64(3): 409. CrossRef - Comparison of eGFR formulas (CKD-EPI and MDRD) in patients with multiple myeloma
Osman ERİNÇ, Soner YEŞİLYURT, Meliha NALCACİ
Cukurova Medical Journal.2023; 48(2): 336. CrossRef - Comparison and evaluation of the 2009 and 2021 chronic kidney disease-epidemiological collaboration equations among Jordanian patients with type 2 diabetes mellitus
Randa I. Farah, Abdulrahman Alhajahjeh, Oraib Al-farahid, Hana Abuzaid, Dana Hiasat, Rama Rayyan, Laith Bdier, Izzat AlAwwa, Kamel Ajlouni
Acta Diabetologica.2023; 61(2): 169. CrossRef - Effect of teaching health-promoting behaviors on the care burden of family caregivers of hemodialysis patients: a four-group clinical trial
Mehrdad Hayati, Razieh Bagherzadeh, Mehdi Mahmudpour, Fatemeh Heidari, Hakimeh Vahedparast
BMC Nursing.2023;[Epub] CrossRef - Impact of social and clinical factors on the diagnostic delay of chronic kidney disease: an evaluation study
Mousa Ghelichi-Ghojogh, Mohammad fararouei, Mozhgan Seif, Bahram Shahryari, Maryam Pakfetrat
International Urology and Nephrology.2022; 54(7): 1603. CrossRef - Chronic kidney disease and its health-related factors: a case-control study
Mousa Ghelichi-Ghojogh, Mohammad Fararouei, Mozhgan Seif, Maryam Pakfetrat
BMC Nephrology.2022;[Epub] CrossRef - Incidence and risk factors of severe non‐proliferative/proliferative diabetic retinopathy: More than a decade follow up in the Tehran Lipids and Glucose Study
Mahsa Sardarinia, Samaneh Asgari, Reyhane Hizomi Arani, Fatemeh Eskandari, Fereidoun Azizi, Davood Khalili, Farzad Hadaegh
Journal of Diabetes Investigation.2022; 13(2): 317. CrossRef - Pathophysiologic Mechanisms and Potential Biomarkers in Diabetic Kidney Disease
Chan-Young Jung, Tae-Hyun Yoo
Diabetes & Metabolism Journal.2022; 46(2): 181. CrossRef - Prevalence of chronic kidney diseases and its determinants among Iranian adults: results of the first phase of Shahedieh cohort study
Ali Dehghani, Sadegh Alishavandi, Nader Nourimajalan, Hossein Fallahzadeh, Vahid Rahmanian
BMC Nephrology.2022;[Epub] CrossRef - Construct a classification decision tree model to select the optimal equation for estimating glomerular filtration rate and estimate it more accurately
Zhenliang Fan, Qiaorui Yang, Zhuohan Xu, Ke Sun, Mengfan Yang, Riping Yin, Dongxue Zhao, Junfen Fan, Hongzhen Ma, Yiwei Shen, Hong Xia
Scientific Reports.2022;[Epub] CrossRef - Novel biomarkers for diabetic kidney disease
Chan-Young Jung, Tae-Hyun Yoo
Kidney Research and Clinical Practice.2022; 41(Suppl 2): S46. CrossRef - Prevalence and Associated Factors of Kidney Dysfunction in Patients with Hypertension and/or Diabetes Mellitus from a Primary Care Population in Northwest China
Mengyue Lin, Mulalibieke Heizhati, Lin Wang, Lin Gan, Mei Li, Wenbo Yang, Ling Yao, Zhongrong Wang, Zhikang Yang, Reyila Abudoyreyimu, Zihao Wu, Nanfang Li
International Journal of General Medicine.2021; Volume 14: 7567. CrossRef
- The Effect of the Holy Quran Recitation on Inflammatory Markers in Hemodialysis Patients in Iran: A Randomized Clinical Trial
- Guideline/Fact Sheet
- Metformin Treatment for Patients with Diabetes and Chronic Kidney Disease: A Korean Diabetes Association and Korean Society of Nephrology Consensus Statement
- Kyu Yeon Hur, Mee Kyoung Kim, Seung Hyun Ko, Miyeun Han, Dong Won Lee, Hyuk-Sang Kwon
- Diabetes Metab J. 2020;44(1):3-10. Published online February 21, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0004
- 9,462 View
- 332 Download
- 14 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
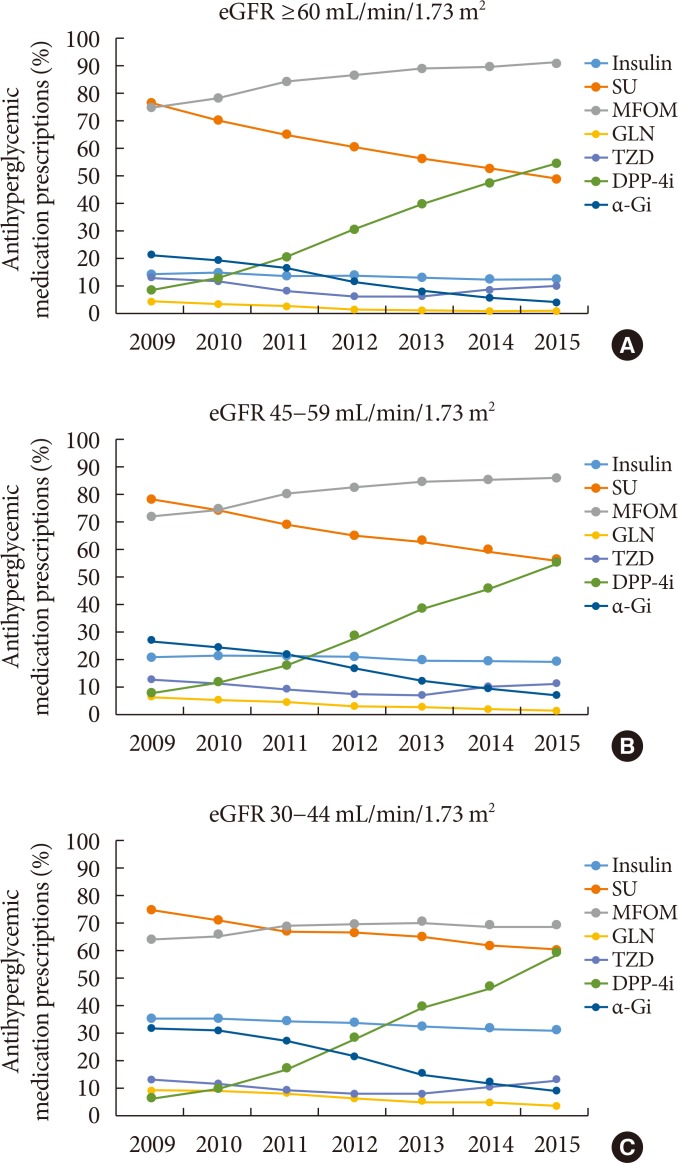
PubReader The safety of metformin use for patients with type 2 diabetes mellitus (T2DM) and advanced kidney disease is controversial, and more recent guidelines have suggested that metformin be used cautiously in this group until more definitive evidence concerning its safety is available. The Korean Diabetes Association and the Korean Society of Nephrology have agreed on consensus statements concerning metformin use for patients with T2DM and renal dysfunction, particularly when these patients undergo imaging studies using iodinated contrast media (ICM). Metformin can be used safely when the estimated glomerular filtration rate (eGFR) is ≥45 mL/min/1.73 m2. If the eGFR is between 30 and 44 mL/min/1.73 m2, metformin treatment should not be started. If metformin is already in use, a daily dose of ≤1,000 mg is recommended. Metformin is contraindicated when the eGFR is <30 mL/min/1.73 m2. Renal function should be evaluated prior to any ICM-related procedures. During procedures involving intravenous administration of ICM, metformin should be discontinued starting the day of the procedures and up to 48 hours post-procedures if the eGFR is <60 mL/min/1.73 m2.
-
Citations
Citations to this article as recorded by- Distribution and elimination kinetics of midazolam and metabolites after post-resuscitation care: a prospective observational study
Wonjoon Jeong, Jung Sunwoo, Yeonho You, Jung Soo Park, Jin Hong Min, Yong Nam In, Hong Joon Ahn, So Young Jeon, Jang Hee Hong, Ji Hye Song, Hyein Kang, My Tuyen Thi Nguyen, Jaehan Kim, Changshin Kang
Scientific Reports.2024;[Epub] CrossRef - Prediction of glycosylated hemoglobin level in patients with cardiovascular diseases and type 2 diabetes mellitus with respect to anti-diabetic medication
Alisher Ikramov, Shakhnoza Mukhtarova, Raisa Trigulova, Dilnoza Alimova, Saodat Abdullaeva
Frontiers in Endocrinology.2024;[Epub] CrossRef - Determinants of vitamin B12 deficiency in patients with type-2 diabetes mellitus — A primary-care retrospective cohort study
Andrew Kien Han Wee, Rehena Sultana
BMC Primary Care.2023;[Epub] CrossRef - Risk factors for post-contrast acute kidney injury in patients sequentially administered iodine- and gadolinium-based contrast media on the same visit to the emergency department: a retrospective study
Changshin Kang, Soo Hyun Han, Jung Soo Park, Dae Eun Choi
Kidney Research and Clinical Practice.2023; 42(3): 358. CrossRef - Guideline for the diagnosis and treatment of diabetes mellitus in patients with transfusion-dependent thalassemia
Mohammad E. Khamseh, Mojtaba Malek, Nahid Hashemi-madani, Fariba Ghassemi, Neda Rahimian, Amir Ziaee, Mohammad Reza Foroughi-Gilvaee, Pooya Faranoush, Negin Sadighnia, Ali Elahinia, Mohammad Reza Rezvany, Mohammad Faranoush
Iranian Journal of Blood and Cancer.2023; 15(4): 293. CrossRef - Continuous use of metformin in patients receiving contrast medium: what is the evidence? A systematic review and meta-analysis
Ting-Wan Kao, Kuo-Hua Lee, Wing P. Chan, Kang-Chih Fan, Che-Wei Liu, Yu-Chen Huang
European Radiology.2022; 32(5): 3045. CrossRef - Glucagon-Like Peptide-1 Receptor Agonists in Type 2 Diabetes Mellitus and Cardiovascular Disease: The Past, Present, and Future
Filipe Ferrari, Rafael S. Scheffel, Vítor M. Martins, Raul D. Santos, Ricardo Stein
American Journal of Cardiovascular Drugs.2022; 22(4): 363. CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef - Treatment Patterns of Type 2 Diabetes Assessed Using a Common Data Model Based on Electronic Health Records of 2000–2019
Kyung Ae Lee, Heung Yong Jin, Yu Ji Kim, Yong-Jin Im, Eun-Young Kim, Tae Sun Park
Journal of Korean Medical Science.2021;[Epub] CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2021;45:698-707)
Eugene Han, Hye Soon Kim
Diabetes & Metabolism Journal.2021; 45(6): 972. CrossRef - KRCP's past and future path
Tae-Hyun Yoo
Kidney Research and Clinical Practice.2020; 39(3): 233. CrossRef - Metformin Use and Risk of All-Cause Mortality and Cardiovascular Events in Patients With Chronic Kidney Disease—A Systematic Review and Meta-Analysis
Yao Hu, Min Lei, Guibao Ke, Xin Huang, Xuan Peng, Lihui Zhong, Ping Fu
Frontiers in Endocrinology.2020;[Epub] CrossRef - Pharmacotherapy for patients with diabetes mellitus
Joon Ho Moon, Soo Lim
Journal of the Korean Medical Association.2020; 63(12): 766. CrossRef
- Distribution and elimination kinetics of midazolam and metabolites after post-resuscitation care: a prospective observational study
- Complications
- Higher Prevalence and Progression Rate of Chronic Kidney Disease in Elderly Patients with Type 2 Diabetes Mellitus
- Kyung-Soo Kim, Seok Won Park, Yong-Wook Cho, Soo-Kyung Kim
- Diabetes Metab J. 2018;42(3):224-232. Published online May 31, 2018
- DOI: https://doi.org/10.4093/dmj.2017.0065
- 5,253 View
- 73 Download
- 31 Web of Science
- 33 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background To evaluate the prevalence of chronic kidney disease (CKD) and progression rate to CKD in elderly patients with type 2 diabetes mellitus (T2DM).
Methods We investigated the medical records of 190 elderly patients (65 years or older) with T2DM from 2005 to 2011 in 6-month increments. Mean follow-up duration was 64.5 months. CKD was defined as estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2 and/or the presence of albuminuria.
Results The mean age was 70.4 years and mean diabetes duration was 10.6 years. Among all the participants, 113 patients (59.5%) had CKD. The eGFR was significantly decreased between baseline (65.7±15.0 mL/min/1.73 m2) and the end of follow-up (52.7±17.5 mL/min/1.73 m2,
P <0.001). At the end of follow-up, the prevalence of eGFR <60 mL/min/1.73 m2 had increased by 61.6% (at baseline, 44.2%). Furthermore, in patients with eGFR ≥60 mL/min/1.73 m2, the progression rate to more than CKD stage 3 was 39.6% at the end of follow-up; 30.2% of elderly diabetic patients had progressed to albuminuria from normoalbuminuria. Kaplan-Meier analysis showed that the time interval to worsening nephropathy was significantly shorter in elderly patients with diabetes duration ≥10 years than in those with diabetes duration <5 years (P =0.018).Conclusion CKD was commonly observed in older patients with T2DM, and the progression rate to CKD is also high. Consequently, it is important to identify and manage CKD as early as possible in elderly patients with T2DM, especially in those with diabetes duration ≥10 years.
-
Citations
Citations to this article as recorded by- Assessing heatwave effects on disabled persons in South Korea
Yeji Kang, Ingul Baek, Jongchul Park
Scientific Reports.2024;[Epub] CrossRef - Combination of Risks of BMI and Health-Related Lifestyles on Kidney Function in the Prediabetic Japanese Population: A Prospective Cohort Study
Jou-Yin Chen, Shiqi Deng, Yukiko Wagatsuma
International Journal of Environmental Research and Public Health.2023; 20(7): 5338. CrossRef - Hormonal imbalance in patients with chronic renal failure in the pre-dialysis and dialysis periods (part1)
I.P. Katerenchuk, S.T. Rustamyan, V.V. Talash, T.I. Yarmola
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2023; 19(1): 65. CrossRef - The Beneficial Effect of Glycemic Control against Adverse Outcomes in Patients with Type 2 Diabetes Mellitus and Chronic Kidney Disease
Dong-Hwa Lee
Diabetes & Metabolism Journal.2023; 47(4): 484. CrossRef - Association Between Continuous Glucose Monitoring-Derived Glycemia Risk Index and Albuminuria in Type 2 Diabetes
Jee Hee Yoo, Ji Yoon Kim, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2023; 25(10): 726. CrossRef - Global burden and influencing factors of chronic kidney disease due to type 2 diabetes in adults aged 20–59 years, 1990–2019
Dandan Xie, Tianpeng Ma, Haoliang Cui, Jing Li, Aihua Zhang, Zhifeng Sheng, Yiqiang Xie
Scientific Reports.2023;[Epub] CrossRef - Effectiveness of Early Advanced Glycation End Product Accumulation Testing in the Diagnosis of Diabetes: A Health Risk Factor Analysis Using the Body Mass Index as a Moderator
Yi Zhang, Tian Jiang, Chao Liu, Honglin Hu, Fang Dai, Li Xia, Qiu Zhang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Causal association pathways between fetuin-A and kidney function: a mediation analysis
Philip Etabee Bassey, Pawin Numthavaj, Sasivimol Rattanasiri, Piyamitr Sritara, Mark McEvoy, Boonsong Ongphiphadhanakul, Ammarin Thakkinstian
Journal of International Medical Research.2022; 50(4): 030006052210828. CrossRef - Advanced glycation end products and diabetes and other metabolic indicators
Tian Jiang, Yi Zhang, Fang Dai, Chao Liu, Honglin Hu, Qiu Zhang
Diabetology & Metabolic Syndrome.2022;[Epub] CrossRef - Type 2 diabetes management in people aged over seventy-five years: targets and treatment strategies
Theocharis Koufakis, Maria Grammatiki, Kalliopi Kotsa
Maturitas.2021; 143: 118. CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef - Chronic kidney disease progression in aged patients
Murat Tuğcu, Dilek Barutçu Ataş
International Urology and Nephrology.2021; 53(12): 2619. CrossRef - Factors determining the clinical significance of dipeptidyl peptidase-4 inhibitors in the treatment of elderly patients with type 2 diabetes mellitus
I. V. Glinkina, A. V. Balashova, A. S. Shyman, A. V. Oderij, S. A. Khan, G. E. Runova, T. B. Morgunova, V. V. Fadeev
Meditsinskiy sovet = Medical Council.2021; (7): 56. CrossRef - Effect of Oral carnosine supplementation on urinary TGF-β in diabetic nephropathy: a randomized controlled trial
Narongrit Siriwattanasit, Bancha Satirapoj, Ouppatham Supasyndh
BMC Nephrology.2021;[Epub] CrossRef - Estimation of the prevalence of type 2 diabetes in combination with diabetic kidney disease and identification of the associated factors in patients attending primary hospitals in Anhui Province, China
Li Xia, Lanlan Cheng, Tian Jiang, Chao Liu, Shiqi Zhang, Honglin Hu, Fang Dai, Qiu Zhang, Yunxia Lu
Journal of International Medical Research.2021; 49(10): 030006052110512. CrossRef - A STUDY TO EVALUATE THE EFFECT OF ANAEMIA IN TYPE-2 DIABETIC PATIENTS
Radhika Maheshwari, Divya J., J. Sahayaraj, Muthukrishnan R.
GLOBAL JOURNAL FOR RESEARCH ANALYSIS.2021; : 117. CrossRef - Metformin treatment for patients with diabetes and chronic kidney disease: A Korean Diabetes Association and Korean Society of Nephrology consensus statement
Kyu Yeon Hur, Mee Kyoung Kim, Seung Hyun Ko, Miyeun Han, Dong Won Lee, Hyuk-Sang Kwon
Kidney Research and Clinical Practice.2020; 39(1): 32. CrossRef - Metformin Treatment for Patients with Diabetes and Chronic Kidney Disease: A Korean Diabetes Association and Korean Society of Nephrology Consensus Statement
Kyu Yeon Hur, Mee Kyoung Kim, Seung Hyun Ko, Miyeun Han, Dong Won Lee, Hyuk-Sang Kwon
Diabetes & Metabolism Journal.2020; 44(1): 3. CrossRef - The prevalence of diabetic chronic kidney disease in adult Greek subjects with type 2 diabetes mellitus: A series from hospital-based diabetes clinics
Ilias N. Migdalis, Nikolaos Papanas, Athanasios E. Raptis, Ioannis M. Ioannidis, Alexios E. Sotiropoulos, George D. Dimitriadis
Diabetes Research and Clinical Practice.2020; 166: 108243. CrossRef - Proteinuria Is Associated with Carotid Artery Atherosclerosis in Non-Albuminuric Type 2 Diabetes: A Cross-Sectional Study
Jaehyun Bae, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Journal of Clinical Medicine.2020; 9(1): 136. CrossRef - Renal status in elderly patients with type 2 diabetes
Kazunaga Takamatsu
Clinical and Experimental Nephrology.2020; 24(1): 53. CrossRef - The fat mass, estimated glomerular filtration rate, and chronic inflammation in type 2 diabetic patients
Tomáš Šálek, Alena Adamíková, Petr Ponížil
Journal of Clinical Laboratory Analysis.2020;[Epub] CrossRef - Insulin: Trigger and Target of Renal Functions
Ana F. Pina, Diego O. Borges, Maria João Meneses, Patrícia Branco, Rita Birne, Antonio Vilasi, Maria Paula Macedo
Frontiers in Cell and Developmental Biology.2020;[Epub] CrossRef - Rate of kidney function decline and factors predicting progression of kidney disease in type 2 diabetes mellitus patients with reduced kidney function: A nationwide retrospective cohort study
Wisit Kaewput, Charat Thongprayoon, Api Chewcharat, Ram Rangsin, Bancha Satirapoj, Chalermrat Kaewput, Picha Suwannahitatorn, Tarun Bathini, Michael A. Mao, Liam D. Cato, Andrew M. Harrison, Pradeep Vaitla, Wisit Cheungpasitporn
Therapeutic Apheresis and Dialysis.2020; 24(6): 677. CrossRef - Association Between Continuous Glucose Monitoring-Derived Time in Range, Other Core Metrics, and Albuminuria in Type 2 Diabetes
Jee Hee Yoo, Min Sun Choi, Jiyeon Ahn, Sung Woon Park, Yejin Kim, Kyu Yeon Hur, Sang-Man Jin, Gyuri Kim, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2020; 22(10): 768. CrossRef - Comparison of Renal Effects of Ezetimibe–Statin Combination versus Statin Monotherapy: A Propensity-Score-Matched Analysis
Jaehyun Bae, Namki Hong, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Yong-ho Lee
Journal of Clinical Medicine.2020; 9(3): 798. CrossRef - Metformin Use and Risk of All-Cause Mortality and Cardiovascular Events in Patients With Chronic Kidney Disease—A Systematic Review and Meta-Analysis
Yao Hu, Min Lei, Guibao Ke, Xin Huang, Xuan Peng, Lihui Zhong, Ping Fu
Frontiers in Endocrinology.2020;[Epub] CrossRef - Treatment with Cinacalcet in Hemodialysis Patients with Severe Secondary Hyperparathyroidism, Influences Bone Mineral Metabolism and Anemia Parameters
Maria Aktsiali, Theodora Papachrysanthou , Ioannis Griveas, Christos Andriopoulos, Panagiotis Sitaras, Ioannis K. Triantafyllopoulos , George I. Lambrou
Current Drug Therapy.2020; 15(3): 249. CrossRef - Gemigliptin Attenuates Renal Fibrosis Through Down-Regulation of the NLRP3 Inflammasome
Jung Beom Seo, Yeon-Kyung Choi, Hye-In Woo, Yun-A Jung, Sungwoo Lee, Seunghyeong Lee, Mihyang Park, In-Kyu Lee, Gwon-Soo Jung, Keun-Gyu Park
Diabetes & Metabolism Journal.2019; 43(6): 830. CrossRef - Glucometabolic characteristics and higher vascular complication risk in Korean patients with type 2 diabetes with non-albumin proteinuria
Yongin Cho, Yong-ho Lee, Eun Seok Kang, Bong-soo Cha, Byung-wan Lee
Journal of Diabetes and its Complications.2019; 33(8): 585. CrossRef - Assessment of kidney function and associated risk factors among type 2 diabetic patients
Moyad Jamal Shahwan, Nageeb Abdul galil Hassan, Rima Ahd Shaheen
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(4): 2661. CrossRef - Influence of diabetes mellitus on patients with lumbar spinal stenosis: A nationwide population-based study
Chang Kyu Lee, Sun Kyu Choi, Dong Ah Shin, Seong Yi, Yoon Ha, Keung Nyun Kim, Insoo Kim, Gregory W.J. Hawryluk
PLOS ONE.2019; 14(3): e0213858. CrossRef - Predictores de progresión de enfermedad renal en el paciente anciano
Manuel Heras Benito, Mª José Fernández Reyes Luis
Enfermería Nefrológica.2019; 22(1): 19. CrossRef
- Assessing heatwave effects on disabled persons in South Korea
- Obesity and Metabolic Syndrome
- Non-Alcoholic Fatty Liver Disease: The Emerging Burden in Cardiometabolic and Renal Diseases
- Eugene Han, Yong-ho Lee
- Diabetes Metab J. 2017;41(6):430-437. Published online November 17, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.6.430
- 4,937 View
- 86 Download
- 51 Web of Science
- 54 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader As the number of individuals with non-alcoholic fatty liver disease (NAFLD) has increased, the influence of NAFLD on other metabolic diseases has been highlighted. Accumulating epidemiologic evidence indicates that NAFLD not only affects the liver but also increases the risk of extra-hepatic diseases such as type 2 diabetes mellitus, metabolic syndrome, dyslipidemia, hypertension, cardiovascular or cerebrovascular diseases, and chronic kidney disease. Non-alcoholic steatohepatitis, an advanced type of NAFLD, can aggravate these inter-organ relationships and lead to poorer outcomes. NAFLD induces insulin resistance and exacerbates systemic chronic inflammation and oxidative stress, which leads to organ dysfunction in extra-hepatic tissues. Although more research is needed to identify the pathophysiological mechanisms and causal relationship between NAFLD and cardiometabolic and renal diseases, screening for heart, brain, and kidney diseases, risk assessment for diabetes, and a multidisciplinary approach for managing these patients should be highly encouraged.
-
Citations
Citations to this article as recorded by- Inter‐relationships between cardiovascular, renal and metabolic diseases: Underlying evidence and implications for integrated interdisciplinary care and management
Jiten Vora, David Cherney, Mikhail N. Kosiborod, Jonas Spaak, Naresh Kanumilli, Kamlesh Khunti, Carolyn S. P. Lam, Michael Bachmann, Peter Fenici
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Relationship between Uric Acid to High Density Lipoprotein Cholesterol Ratio and Nonalcoholic Fatty Liver Disease in Nonoverweight/Obese Patients with Type 2 Diabetes
Yuliang Cui, Zhenzhen Qu, Wenmei Hu, Haiyan Shi, Faustino R. Perez-Lopez
International Journal of Endocrinology.2023; 2023: 1. CrossRef - Emerging Role of Protein O-GlcNAcylation in Liver Metabolism: Implications for Diabetes and NAFLD
Ziyan Xie, Ting Xie, Jieying Liu, Qian Zhang, Xinhua Xiao
International Journal of Molecular Sciences.2023; 24(3): 2142. CrossRef - Lean or Non-obese Nonalcoholic Fatty Liver Disease Patients: Are They Really Lean?
Eugene Han, Yong-ho Lee
Clinical and Molecular Hepatology.2023; 29(4): 980. CrossRef - Factores de riesgo para fibrosis hepática en pacientes diabéticos con enfermedad renal cronica terminal
Ismael Yepes Barreto, Diana Romero Florez, Jorge Coronado Daza
Revista colombiana de Gastroenterología.2023; 38(3): 278. CrossRef - Circ_0004535/miR-1827/CASP8 network involved in type 2 diabetes mellitus with nonalcoholic fatty liver disease
Min Li, Ai Zeng, Xinle Tang, Hui Xu, Wei Xiong, Yanying Guo
Scientific Reports.2023;[Epub] CrossRef - Non-alcoholic fatty liver disease associated with greater herpes zoster risk than alcoholic fatty liver disease
Cheng-Wei Yu, Chia-Hung Chen, Yung-Chi Cheng, Wen-Che Hsieh, Tzu-Ju Hsu, Fuu-Jen Tsai, Chao-Yu Hsu
European Journal of Medical Research.2023;[Epub] CrossRef - A GLP‐1/GLP‐2 receptor dual agonist to treat NASH: Targeting the gut‐liver axis and microbiome
Eun Ran Kim, Jeong Su Park, Jin Hee Kim, Ji Young Oh, In Jeong Oh, Da Hyun Choi, Yu seol Lee, I. Seul Park, SeungWon Kim, Da Hyun Lee, Jae Hee Cheon, Jin‐Woo Bae, Minyoung Lee, Jin Won Cho, In Bok An, Eun Joo Nam, Sang‐In Yang, Myung‐Shik Lee, Soo Han Bae
Hepatology.2022; 75(6): 1523. CrossRef - Analysis of Severe Hypoglycemia Among Adults With Type 2 Diabetes and Nonalcoholic Fatty Liver Disease
Ji-Yeon Lee, Young-eun Kim, Kyungdo Han, Eugene Han, Byung Wan Lee, Eun Seok Kang, Bong-Soo Cha, Seung-Hyun Ko, Yong-ho Lee
JAMA Network Open.2022; 5(2): e220262. CrossRef - State-of-the-Art Overview of the Pharmacological Treatment of Non-Alcoholic Steatohepatitis
Yongin Cho, Yong-ho Lee
Endocrinology and Metabolism.2022; 37(1): 38. CrossRef - Fatty Liver Index is a valid predictor of non-alcoholic fatty liver disease (NAFLD) in pregnancy
Iresha Sandamali Koralegedara, Janith Niwanthaka Warnasekara, Ashani Rathnayake, Korale Gedara Dayaratne, Suneth Buddhika Agampodi
BMJ Open Gastroenterology.2022; 9(1): e000913. CrossRef - A Prediction Model of the Incidence of Nonalcoholic Fatty Liver Disease With Visceral Fatty Obesity: A General Population-Based Study
Yang Zhou, Xiangping Chai, Tuo Guo, Yuting Pu, Mengping Zeng, Aifang Zhong, Guifang Yang, Jiajia Cai
Frontiers in Public Health.2022;[Epub] CrossRef - Non-alcoholic fatty liver disease and sarcopenia is associated with the risk of albuminuria independent of insulin resistance, and obesity
Eugene Han, Mi Kyung Kim, Seung-Soon Im, Byoung Kuk Jang, Hye Soon Kim
Journal of Diabetes and its Complications.2022; 36(8): 108253. CrossRef - Increased Risk of NAFLD in Adults with Glomerular Hyperfiltration: An 8-Year Cohort Study Based on 147,162 Koreans
Dae-Jeong Koo, Mi Yeon Lee, Inha Jung, Sun Joon Moon, Hyemi Kwon, Eun-Jung Rhee, Cheol-Young Park, Won-Young Lee, Ki Won Oh, Se Eun Park
Journal of Personalized Medicine.2022; 12(7): 1142. CrossRef - Effects of Avocado Oil Supplementation on Insulin Sensitivity, Cognition, and Inflammatory and Oxidative Stress Markers in Different Tissues of Diet-Induced Obese Mice
Schérolin de Oliveira Marques, Alexandre Pastoris Muller, Thais Fernandes Luciano, Natália dos Santos Tramontin, Mateus da Silva Caetano, Bruno Luis da Silva Pieri, Tatiane Lima Amorim, Marcone Augusto Leal de Oliveira, Cláudio Teodoro de Souza
Nutrients.2022; 14(14): 2906. CrossRef - Relationship Between Handgrip Strength and Laboratory Values in Adolescents With Non-Alcoholic Fatty Liver Disease
Si Yeong Lee, Yong Whi Jeong, Hong Koh, Yunkoo Kang
Journal of Clinical Densitometry.2022; 25(4): 490. CrossRef - Association between non-alcoholic fatty liver disease and metabolically healthy deterioration across different body shape phenotypes at baseline and change patterns
Liu Lei, Wang Changfa, Wang Jiangang, Chen Zhiheng, Yuan Ting, Zhu Xiaoling, Deng Yuling, Wang Yaqin
Scientific Reports.2022;[Epub] CrossRef - Muscle fat contents rather than muscle mass determines nonalcoholic steatohepatitis and liver fibrosis in patients with severe obesity
Eugene Han, Mi Kyung Kim, Hye Won Lee, Seungwan Ryu, Hye Soon Kim, Byoung Kuk Jang, Youngsung Suh
Obesity.2022; 30(12): 2440. CrossRef - Prediction of decreased estimated glomerular filtration rate using liver fibrosis markers: a renal biopsy-based study
Akira Mima
Scientific Reports.2022;[Epub] CrossRef - Therapeutic implications of shared mechanisms in non-alcoholic fatty liver disease and chronic kidney disease
Mehmet Kanbay, Mustafa C. Bulbul, Sidar Copur, Baris Afsar, Alan A. Sag, Dimitrie Siriopol, Masanari Kuwabara, Silvia Badarau, Adrian Covic, Alberto Ortiz
Journal of Nephrology.2021; 34(3): 649. CrossRef - Taxifolin ameliorate high-fat-diet feeding plus acute ethanol binge-induced steatohepatitis through inhibiting inflammatory caspase-1-dependent pyroptosis
Zi-Ying Zhan, Mei Wu, Yue Shang, Min Jiang, Jian Liu, Chun-Ying Qiao, Huan Ye, Yong-Ce Lin, Mei-Hua Piao, Rong-Hui Sun, Zhi-Hong Zhang, Jing-Ya Jiao, Yan-Ling Wu, Ji-Xing Nan, Li-Hua Lian
Food & Function.2021; 12(1): 362. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Eugene Han, Mi Kyung Kim, Byoung Kuk Jang, Hye Soon Kim
Diabetes & Metabolism Journal.2021; 45(5): 698. CrossRef - The Leg Fat to Total Fat Ratio Is Associated with Lower Risks of Non-Alcoholic Fatty Liver Disease and Less Severe Hepatic Fibrosis: Results from Nationwide Surveys (KNHANES 2008–2011)
Hyun Min Kim, Yong-ho Lee
Endocrinology and Metabolism.2021; 36(6): 1232. CrossRef - A preliminary report about the detection of ventricular repolarisation in patients with non-alcoholic fatty liver disease
Marwan S. Al-Nimer, Vian A. Esmail, Dler S. Hamid, Mohammad O. Mohammad
Journal of Taibah University Medical Sciences.2020; 15(4): 284. CrossRef - Atorvastatin attenuates obese-induced kidney injury and impaired renal organic anion transporter 3 function through inhibition of oxidative stress and inflammation
Nattavadee Pengrattanachot, Rada Cherngwelling, Krit Jaikumkao, Anchalee Pongchaidecha, Laongdao Thongnak, Myat Theingi Swe, Varanuj Chatsudthipong, Anusorn Lungkaphin
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2020; 1866(6): 165741. CrossRef - Correlation Between Non-Alcoholic Fatty Liver and Chronic Kidney Disease
Hasyim Kasim, St. Rabiul Zatalia, Haerani Rasyid, Syakib Bakri, Muhammad L. Parewangi, Fardah Akil, Arifin Seweng
The Open Urology & Nephrology Journal.2020; 13(1): 1. CrossRef - Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Mellitus: A Position Statement of the Fatty Liver Research Group of the Korean Diabetes Association
Byung-Wan Lee, Yong-ho Lee, Cheol-Young Park, Eun-Jung Rhee, Won-Young Lee, Nan-Hee Kim, Kyung Mook Choi, Keun-Gyu Park, Yeon-Kyung Choi, Bong-Soo Cha, Dae Ho Lee
Diabetes & Metabolism Journal.2020; 44(3): 382. CrossRef - Sarcopenia: an emerging risk factor for non-alcoholic fatty liver disease
Yong-ho Lee, Seung Up Kim
Hepatology International.2020; 14(1): 5. CrossRef - Association between Non-Alcoholic Steatohepatitis and Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Mellitus
Hokyou Lee, Gyuri Kim, Young Ju Choi, Byung Wook Huh, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Eun Jig Lee, Yong-ho Lee, Kap Bum Huh
Diabetes & Metabolism Journal.2020; 44(2): 267. CrossRef - Ipragliflozin Additively Ameliorates Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Controlled with Metformin and Pioglitazone: A 24-Week Randomized Controlled Trial
Eugene Han, Yong-ho Lee, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha
Journal of Clinical Medicine.2020; 9(1): 259. CrossRef - Non-alcoholic steatohepatitis and progression of carotid atherosclerosis in patients with type 2 diabetes: a Korean cohort study
Hyeok-Hee Lee, Yongin Cho, Young Ju Choi, Byung Wook Huh, Byung-Wan Lee, Eun Seok Kang, Seok Won Park, Bong-Soo Cha, Eun Jig Lee, Yong-ho Lee, Kap Bum Huh
Cardiovascular Diabetology.2020;[Epub] CrossRef - Hepatic fibrosis is associated with total proteinuria in Korean patients with type 2 diabetes
Eugene Han, Yongin Cho, Kyung-won Kim, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-wan Lee
Medicine.2020; 99(33): e21038. CrossRef - Association between NAFLD and risk of prevalent chronic kidney disease: why there is a difference between east and west?
Min Zhang, Su Lin, Ming-fang Wang, Jiao-feng Huang, Shi-ying Liu, Su-mei Wu, Hao-yang Zhang, Zi-mu Wu, Wen-Yue Liu, Dong-Chu Zhang, Chuan-ming Hao, Yue-yong Zhu, Ming-Hua Zheng, Xiao-zhong Wang
BMC Gastroenterology.2020;[Epub] CrossRef - Association Between Serum Bilirubin and the Progression of Carotid Atherosclerosis in Type 2 Diabetes
Inkuk Lee, Hyeok-Hee Lee, Yongin Cho, Young Ju Choi, Byung Wook Huh, Byung-Wan Lee, Eun Seok Kang, Seok Won Park, Bong-Soo Cha, Eun Jig Lee, Yong-ho Lee, Kap Bum Huh
Journal of Lipid and Atherosclerosis.2020; 9(1): 195. CrossRef - Letter: Sarcopenia Is Significantly Associated with Presence and Severity of Nonalcoholic Fatty Liver Disease (J Obes Metab Syndr 2019;28:129-38)
Chan-Hee Jung
Journal of Obesity & Metabolic Syndrome.2020; 29(2): 158. CrossRef - Metabolic Syndrome and Abnormal Peri-Organ or Intra-Organ Fat (APIFat) Deposition in Chronic Obstructive Pulmonary Disease: An Overview
Niki Katsiki, Anca Pantea Stoian, Paschalis Steiropoulos, Nikolaos Papanas, Andra-Iulia Suceveanu, Dimitri P. Mikhailidis
Metabolites.2020; 10(11): 465. CrossRef - Heart Failure and Liver Disease
Andrew Xanthopoulos, Randall C. Starling, Takeshi Kitai, Filippos Triposkiadis
JACC: Heart Failure.2019; 7(2): 87. CrossRef - Risk factors for non-alcoholic fatty liver disease-associated hepatic fibrosis in type 2 diabetes patients
Asieh Mansour, Mohammad Reza Mohajeri-Tehrani, Majid Samadi, Hadis Gerami, Mostafa Qorbani, Nick Bellissimo, Hossein Poustchi, Azita Hekmatdoost
Acta Diabetologica.2019; 56(11): 1199. CrossRef - Targeting CYP4A attenuates hepatic steatosis in a novel multicellular organotypic liver model
Jae-Sung Ryu, Minji Lee, Seon Ju Mun, Sin-Hyoung Hong, Ho-Joon Lee, Hyo-Suk Ahn, Kyung-Sook Chung, Gun-Hwa Kim, Myung Jin Son
Journal of Biological Engineering.2019;[Epub] CrossRef - Non-alcoholic steatohepatitis and type 2 diabetes mellitus: the effects of weight loss versus drug treatment
Niki Katsiki, Vasilios G Athyros
Current Medical Research and Opinion.2019; 35(7): 1305. CrossRef - Nonalcoholic Fatty Liver Disease in Diabetes. Part I: Epidemiology and Diagnosis
Yong-ho Lee, Yongin Cho, Byung-Wan Lee, Cheol-Young Park, Dae Ho Lee, Bong-Soo Cha, Eun-Jung Rhee
Diabetes & Metabolism Journal.2019; 43(1): 31. CrossRef - Progress in the Study of the Pathogenesis of Chronic Kidney Disease Associated with Nonalcoholic Fatty Liver Disease
清莲 宋
Advances in Clinical Medicine.2019; 09(09): 1073. CrossRef - Association Between Nonalcoholic Fatty Liver Disease and Future Deterioration of Metabolic Health: A Cohort Study
You‐Cheol Hwang, Hong‐Yup Ahn, Cheol‐Young Park
Obesity.2019; 27(8): 1360. CrossRef - Subfornical organ insulin receptors tonically modulate cardiovascular and metabolic function
Jin Kwon Jeong, Julie A. Horwath, Hayk Simonyan, Katherine A. Blackmore, Scott D. Butler, Colin N. Young
Physiological Genomics.2019; 51(8): 333. CrossRef - Nonalcoholic Fatty Liver Disease and Diabetes: Part II: Treatment
Kyung-Soo Kim, Byung-Wan Lee, Yong Jin Kim, Dae Ho Lee, Bong-Soo Cha, Cheol-Young Park
Diabetes & Metabolism Journal.2019; 43(2): 127. CrossRef - Chicken Protein Hydrolysates Have Anti-Inflammatory Effects on High-Fat Diet Induced Obesity in Mice
Thomas Aloysius, Ana Carvajal, Rasa Slizyte, Jon Skorve, Rolf Berge, Bodil Bjørndal
Medicines.2018; 6(1): 5. CrossRef - STK25 Regulates Cardiovascular Disease Progression in a Mouse Model of Hypercholesterolemia
Emmelie Cansby, Elin Magnusson, Esther Nuñez-Durán, Manoj Amrutkar, Matteo Pedrelli, Paolo Parini, Jenny Hoffmann, Marcus Ståhlman, Brian W. Howell, Hanns-Ulrich Marschall, Jan Borén, Margit Mahlapuu
Arteriosclerosis, Thrombosis, and Vascular Biology.2018; 38(8): 1723. CrossRef - Organ-Specific Mechanisms of Transendothelial Neutrophil Migration in the Lung, Liver, Kidney, and Aorta
Sanne L. Maas, Oliver Soehnlein, Joana R. Viola
Frontiers in Immunology.2018;[Epub] CrossRef - Visceral adiposity index as a predictor of NAFLD: A prospective study with 4‐year follow‐up
Chaonan Xu, Zhimin Ma, Yunfeng Wang, Xiangtong Liu, Lixin Tao, Deqiang Zheng, Xiuhua Guo, Xinghua Yang
Liver International.2018; 38(12): 2294. CrossRef - Obesity induced alterations in redox homeostasis and oxidative stress are present from an early age
Alfonso M. Lechuga-Sancho, David Gallego-Andujar, Pablo Ruiz-Ocaña, Francisco M. Visiedo, Ana Saez-Benito, Mónica Schwarz, Carmen Segundo, Rosa M. Mateos, Manuel Portero-Otin
PLOS ONE.2018; 13(1): e0191547. CrossRef - Capybara Oil Improves Hepatic Mitochondrial Dysfunction, Steatosis, and Inflammation in a Murine Model of Nonalcoholic Fatty Liver Disease
Polyana C. Marinho, Aline B. Vieira, Priscila G. Pereira, Kíssila Rabelo, Bianca T. Ciambarella, Ana L. R. Nascimento, Erika Cortez, Aníbal S. Moura, Fernanda V. Guimarães, Marco A. Martins, Gonzalo Barquero, Rodrigo N. Ferreira, Jorge J. de Carvalho
Evidence-Based Complementary and Alternative Medicine.2018; 2018: 1. CrossRef - Persistently Increased Resting Energy Expenditure Predicts Short-Term Mortality in Patients with Acute-on-Chronic Liver Failure
Jia Yao, Xiaoshuang Zhou, Hui Wang, Lili Yuan, Yu Chen, Zhongping Duan
Annals of Nutrition and Metabolism.2018; 73(1): 2. CrossRef - The Sodium-Glucose Cotransporter 2 Inhibitor Dapagliflozin Prevents Renal and Liver Disease in Western Diet Induced Obesity Mice
Dong Wang, Yuhuan Luo, Xiaoxin Wang, David Orlicky, Komuraiah Myakala, Pengyuan Yang, Moshe Levi
International Journal of Molecular Sciences.2018; 19(1): 137. CrossRef - Association of sex hormone-binding globulin with nonalcoholic fatty liver disease in Chinese adults
Jing Luo, Qian Chen, Tianran Shen, Xu Wang, Wanjun Fang, Xiaocai Wu, Zenan Yuan, Gengdong Chen, Wenhua Ling, Yuming Chen
Nutrition & Metabolism.2018;[Epub] CrossRef
- Inter‐relationships between cardiovascular, renal and metabolic diseases: Underlying evidence and implications for integrated interdisciplinary care and management
- Diabetic Kidney Disease: From Epidemiology to Clinical Perspectives
- Cheol Whee Park
- Diabetes Metab J. 2014;38(4):252-260. Published online August 20, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.4.252
- 6,526 View
- 58 Download
- 76 Web of Science
- 69 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader With worldwide epidemic of diabetes mellitus, diabetic nephropathy which is one of the major causes of microvascular complication has become a serious concern in Korea as well as the rest of the world. In view of its significance, there is an urgent and paramount need for proper managements that could either deter or slow the progression of diabetic nephropathy. Despite advances in care, ever increasing number of patients suffering from diabetic kidney disease and from end-stage renal disease implies that the current management is not adequate in many aspects. The reasons for these inadequacies compromise lack of early diagnosis, failure to intervene with timely and aggressive manner, and lack of understanding on the kind of interventions required. Another issue equally important for the adequate care of patients with diabetic nephropathy is an understanding of past, present and future epidemiology of diabetic nephropathy which serves, especially in Korea, as a material determining standard diagnosis and treatment and a national health-policy decision.
-
Citations
Citations to this article as recorded by- N6-methyladenosine RNA methylation in diabetic kidney disease
Jiaan Huang, Fan Yang, Yan Liu, Yuehua Wang
Biomedicine & Pharmacotherapy.2024; 171: 116185. CrossRef - Association of advanced chronic kidney disease with diabetic retinopathy severity in older patients with diabetes: a retrospective cross-sectional study
Geun Woo Lee, Chul Ho Lee, Seong Gyu Kim
Journal of Yeungnam Medical Science.2023; 40(2): 146. CrossRef - Age at Mortality in Patients with Type 2 Diabetes Who Underwent Kidney Transplantation: An Analysis of Data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
Sun Ok Song, Eugene Han, Kang Ju Son, Bong-Soo Cha, Byung-Wan Lee
Journal of Clinical Medicine.2023; 12(9): 3160. CrossRef - Single‐cell RNA‐seq with spatial transcriptomics to create an atlas of human diabetic kidney disease
Duo Chen, Mingwei Shao, Yi Song, Gaofei Ren, Feng Guo, Xunjie Fan, Yanyan Wang, Wei Zhang, Guijun Qin
The FASEB Journal.2023;[Epub] CrossRef - Metabolomic profiling of amino acids study reveals a distinct diagnostic model for diabetic kidney disease
Jiao Wang, Chunyu Zhou, Qing Zhang, Zhangsuo Liu
Amino Acids.2023; 55(11): 1563. CrossRef - New insights into the mechanisms of diabetic kidney disease: Role of circadian rhythm and Bmal1
Zhimei Peng, Yanting Liang, Xueying Liu, Jie Shao, Nan Hu, Xinzhou Zhang
Biomedicine & Pharmacotherapy.2023; 166: 115422. CrossRef - Physical exercise as a friend not a foe in acute kidney diseases through immune system modulation
Ana Carolina Costanti-Nascimento, Leonilia Brelaz-Abreu, Elayne Bragança-Jardim, Welbert de Oliveira Pereira, Niels Olsen Saraiva Camara, Mariane Tami Amano
Frontiers in Immunology.2023;[Epub] CrossRef - Sodium-dependent glucose transporter 2 inhibitor alleviates renal lipid deposition and improves renal oxygenation levels in newly diagnosed type 2 diabetes mellitus patients: a randomized controlled trial
Li Zhang, Tongdan Wang, Yan Kong, Haizhen Sun, Yuling Zhang, Junmei Wang, Zhida Wang, Shan Lu, Pei Yu, Saijun Zhou
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Neutrophil lymphocyte ratio: a reliable biomarker for diabetic nephropathy?
Ashutosh Singh, Anshu Kumar Jha, Bipul Chandra Kalita, Dharmendra Kumar Jha, Yash Alok
International Journal of Diabetes in Developing Countries.2022; 42(3): 523. CrossRef - miR-193a as a potential mediator of WT-1/synaptopodin in the renoprotective effect of Losartan on diabetic kidney
Dan Gao, Pei Yu, Sanhui Jing, Chengcheng Yan, Dandan Ding, Yingjin Qiao, Ge Wu
Canadian Journal of Physiology and Pharmacology.2022; 100(1): 26. CrossRef - 3-Hydroxybutyrate Ameliorates the Progression of Diabetic Nephropathy
Jeeyoun Jung, Woo Yeong Park, Yun Jin Kim, Mikyung Kim, Misun Choe, Kyubok Jin, Ji Hae Seo, Eunyoung Ha
Antioxidants.2022; 11(2): 381. CrossRef - Emerging Role of Epitranscriptomics in Diabetes Mellitus and Its Complications
Xinqian Geng, Zheng Li, Ying Yang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Analysis of serum circulating MicroRNAs level in Malaysian patients with gestational diabetes mellitus
Sajad Jamalpour, Shamsul Mohd Zain, Reza Vazifehmand, Zahurin Mohamed, Yuh Fen Pung, Hesam Kamyab, Siti Zawiah Omar
Scientific Reports.2022;[Epub] CrossRef - Combined Single-Cell RNA-Seq and Spatial Transcriptomics Reveal an Atlas of Human Diabetic Kidney Disease
Duo Chen, Mingwei Shao, Yi Song, Gaofei Ren, Feng Guo, Xunjie Fan, Yanyan Wang, Wei Zhang, Guijun Qin
SSRN Electronic Journal .2022;[Epub] CrossRef - How to inhibit transforming growth factor beta safely in diabetic kidney disease
Yuxin Yang, Kexin Shi, Devang M. Patel, Fang Liu, Tieqiao Wu, Zhonglin Chai
Current Opinion in Nephrology & Hypertension.2021; 30(1): 115. CrossRef - Plasma miR-193a-3p can be a potential biomarker for the diagnosis of diabetic nephropathy
Yan Hong, Jidong Wang, Lai Zhang, Wenjuan Sun, Xuefang Xu, Kaiyue Zhang
Annals of Clinical Biochemistry: International Journal of Laboratory Medicine.2021; 58(2): 141. CrossRef - Severe hypoglycemia and the risk of end stage renal disease in type 2 diabetes
Jae-Seung Yun, Yong-Moon Park, Kyungdo Han, Hyung-Wook Kim, Seon-Ah Cha, Yu-Bae Ahn, Seung-Hyun Ko
Scientific Reports.2021;[Epub] CrossRef - Integrin β3 overexpression contributes to podocyte injury through inhibiting RhoA/YAP signaling pathway
Zhuo Li, Zhiwen Lian, Jianchao Ma, Li Zhang, Xingji Lian, Shuangxin Liu, Jianteng Xie, Zhonglin Feng, Ting Lin, Hong Zhang, Xinling Liang
Bioengineered.2021; 12(1): 1138. CrossRef - A Nonlinear Relationship Between Serum 25-Hydroxyvitamin D and Urine Albumin to Creatinine Ratio in Type 2 Diabetes: A Cross-Sectional Study in China
Qian Liang, Haofei Hu, Han Wu, Xuan Chen, Wei Wang, Ying Le, Shufen Yang, Lijing Jia
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 2581. CrossRef - Proteinuria as a significant predictive factor for the progression of carotid artery atherosclerosis in non-albuminuric type 2 diabetes
Young-eun Kim, Minyoung Lee, Yong-ho Lee, Eun Seok Kang, Bong-soo Cha, Byung-Wan Lee
Diabetes Research and Clinical Practice.2021; 181: 109082. CrossRef - USP9X prevents AGEs-induced upregulation of FN and TGF-β1 through activating Nrf2-ARE pathway in rat glomerular mesangial cells
Kaipeng Huang, Xilin Zhao
Experimental Cell Research.2020; 393(2): 112100. CrossRef - D-dimer Levels in Chronic Kidney Illness: A Comprehensive and Systematic Literature Review
Sahar Vahdat, Shahrzad Shahidi
Proceedings of the National Academy of Sciences, India Section B: Biological Sciences.2020; 90(5): 911. CrossRef - Circulating Expression Level of LncRNA Malat1 in Diabetic Kidney Disease Patients and Its Clinical Significance
Lian-ji Zhou, Da-wei Yang, Li-Na Ou, Xing-Rong Guo, Biao-liang Wu
Journal of Diabetes Research.2020; 2020: 1. CrossRef - Impact of chronic kidney disease definition on assessment of its incidence and risk factors in patients with newly diagnosed type 1 and type 2 diabetes in the UK: A cohort study using primary care data from the United Kingdom
Antonio González-Pérez, Maria E. Saéz, David Vizcaya, Marcus Lind, Luis A. García Rodríguez
Primary Care Diabetes.2020; 14(4): 381. CrossRef Resveratrol Inhibits Lipopolysaccharide-Induced Extracellular Matrix Accumulation and Inflammation in Rat Glomerular Mesangial Cells by SphK1/S1P2/NF-κB Pathway
Wenyan Gong, Jie Li, Wenying Chen, Fuzhen Feng, Yanhui Deng
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 4495. CrossRef- Effects of dietary iron restriction on kidney mitochondria function and oxidative stress in streptozotocin-diabetic rats
Donovan J. Peña-Montes, Maribel Huerta-Cervantes, Mónica Ríos-Silva, Xóchitl Trujillo, Christian Cortés-Rojo, Miguel Huerta, Alfredo Saavedra-Molina
Mitochondrion.2020; 54: 41. CrossRef - Significance of glycated LDL in different stages of diabetic nephropathy
Khalid Siddiqui, Teena P. George, Shaik Sarfaraz Nawaz, Maram Yaslam, Ebtehal Almogbel, Khalid Al-Rubeaan
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(1): 548. CrossRef - Prognostic value of visit-to-visit systolic blood pressure variability related to diabetic kidney disease among patients with type 2 diabetes
Zhe-Bin Yu, Jian-Bing Wang, Die Li, Xue-Yu Chen, Hong-Bo Lin, Kun Chen
Journal of Hypertension.2019; 37(7): 1411. CrossRef - Epigenetics and epigenomics in diabetic kidney disease and metabolic memory
Mitsuo Kato, Rama Natarajan
Nature Reviews Nephrology.2019; 15(6): 327. CrossRef - Resveratrol inhibits high glucose-induced activation of AP-1 and NF-κB via SphK1/S1P2 pathway to attenuate mesangial cells proliferation and inflammation
Yanhui Deng, Wenyan Gong, Qiang Li, Xian Wu, Liyao Wu, Xiaoxia Zheng, Wenying Chen, Heqing Huang
Journal of Functional Foods.2019; 55: 86. CrossRef - Predictive Factors for Efficacy of AST-120 Treatment in Diabetic Nephropathy: a Prospective Single-Arm, Open-Label, Multi-Center Study
You-Cheol Hwang, Se Won Kim, Kyu Yeon Hur, Bong-Soo Cha, In Joo Kim, Tae Sun Park, Sei Hyun Baik, Kun Ho Yoon, Kwan Woo Lee, In Kyu Lee, Moon-Kyu Lee
Journal of Korean Medical Science.2019;[Epub] CrossRef - Potential Diagnostic Hemorheological Indexes for Chronic Kidney Disease in Patients With Type 2 Diabetes
Hoyoon Lee, Wonwhi Na, Sang Bae Lee, Chul Woo Ahn, Jun Sung Moon, Kyu Chang Won, Sehyun Shin
Frontiers in Physiology.2019;[Epub] CrossRef - Comparing the Effect of Dipeptidyl-Peptidase 4 Inhibitors and Sulfonylureas on Albuminuria in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A Prospective Open-Label Study
Po-Chung Cheng, Shang-Ren Hsu, Jeng-Fu Kuo, Yun-Chung Cheng, Yu-Hsiu Liu, Shih-Te Tu
Journal of Clinical Medicine.2019; 8(10): 1715. CrossRef - Mechanisms of Adiponectin Action: Implication of Adiponectin Receptor Agonism in Diabetic Kidney Disease
Yaeni Kim, Cheol Whee Park
International Journal of Molecular Sciences.2019; 20(7): 1782. CrossRef - Regulatory T cells in acute and chronic kidney diseases
Rahul Sharma, Gilbert R. Kinsey
American Journal of Physiology-Renal Physiology.2018; 314(5): F679. CrossRef - Herba Artemisiae Capillaris Extract Prevents the Development of Streptozotocin-Induced Diabetic Nephropathy of Rat
Jianan Geng, Xiaoyan Yu, Chunyu Liu, Chengbo Sun, Menghuan Guo, Zhen Li, Yingli Jin, Yinggang Zou, Jinghua Yu
Evidence-Based Complementary and Alternative Medicine.2018; 2018: 1. CrossRef - Overview of the burden of illness and the role of once-weekly glucagon-like peptide-1 receptor agonist therapy in type 2 diabetes
Deborah Hinnen
Journal of the American Association of Nurse Practitioners.2018; 30(1): S4. CrossRef - Previous Exercise Training Reduces Markers of Renal Oxidative Stress and Inflammation in Streptozotocin-Induced Diabetic Female Rats
Liliany Souza de Brito Amaral, Cláudia Silva Souza, Rildo Aparecido Volpini, Maria Heloisa Massola Shimizu, Ana Carolina de Bragança, Daniele Canale, Antonio Carlos Seguro, Terezila Machado Coimbra, Amélia Cristina Mendes de Magalhães, Telma de Jesus Soar
Journal of Diabetes Research.2018; 2018: 1. CrossRef - Critical Shear Stress is Associated with Diabetic Kidney Disease in Patients with Type 2 Diabetes
Seung Min Chung, Jung Hyun Oh, Jun Sung Moon, Yu Kyung Kim, Ji Sung Yoon, Kyu Chang Won, Hyoung Woo Lee
Scientific Reports.2018;[Epub] CrossRef - Losartan Alleviates Renal Fibrosis and Inhibits Endothelial-to-Mesenchymal Transition (EMT) Under High-Fat Diet-Induced Hyperglycemia
Yufeng Yao, Yong Li, Xiaofei Zeng, Zheng Ye, Xia Li, Lu Zhang
Frontiers in Pharmacology.2018;[Epub] CrossRef - Association between poor psychosocial conditions and diabetic nephropathy in Japanese type 2 diabetes patients: A cross‐sectional study
Hiroyo Ninomiya, Naoto Katakami, Taka‐aki Matsuoka, Mitsuyoshi Takahara, Hitoshi Nishizawa, Norikazu Maeda, Michio Otsuki, Akihisa Imagawa, Hiroyasu Iso, Tetsuya Ohira, Iichiro Shimomura
Journal of Diabetes Investigation.2018; 9(1): 162. CrossRef - Urinary Microvesicle-Bound Uromodulin: A Potential Molecular Biomarker in Diabetic Kidney Disease
Neng-jun Lou, Yi-hong Ni, Hong-ying Jia, Jing-ti Deng, Lu Jiang, Feng-jie Zheng, Ai-li Sun
Journal of Diabetes Research.2017; 2017: 1. CrossRef - Renoprotective effect of fucoidan from Acaudina molpadioides in streptozotocin/high fat diet-induced type 2 diabetic mice
Shiwei Hu, Jinhui Wang, Jingfeng Wang, Shijie Li, Wei Jiang, Yu Liu
Journal of Functional Foods.2017; 31: 123. CrossRef - Analysis and comparison of the cost-effectiveness of statins according to the baseline low-density lipoprotein cholesterol level in Korea
Y. J. Jeong, H. Kim, S. J. Baik, T. M. Kim, S. J. Yang, S.-H. Lee, J.-H. Cho, H. Lee, H. W. Yim, I. Y. Choi, K.-H. Yoon, H.-S. Kim
Journal of Clinical Pharmacy and Therapeutics.2017; 42(3): 292. CrossRef - Visualization of kidney fibrosis in diabetic nephropathy by long diffusion tensor imaging MRI with spin-echo sequence
Jun-Ya Kaimori, Yoshitaka Isaka, Masaki Hatanaka, Satoko Yamamoto, Naotsugu Ichimaru, Akihiko Fujikawa, Hiroshi Shibata, Akira Fujimori, Sosuke Miyoshi, Takashi Yokawa, Kagayaki Kuroda, Toshiki Moriyama, Hiromi Rakugi, Shiro Takahara
Scientific Reports.2017;[Epub] CrossRef - Rutin suppresses high glucose-induced ACTA2 and p38 protein expression in diabetic nephropathy
Chun-Shan Han, Kai Liu, Ning Zhang, Shi-Wen Li, Hai-Cheng Gao
Experimental and Therapeutic Medicine.2017; 14(1): 181. CrossRef - Emodin self-emulsifying platform ameliorates the expression of FN, ICAM-1 and TGF-β1 in AGEs-induced glomerular mesangial cells by promoting absorption
Jiani Huang, Wenyan Gong, Zhiquan Chen, Junying Huang, Qiuhong Chen, Heqing Huang, Chunshun Zhao
European Journal of Pharmaceutical Sciences.2017; 99: 128. CrossRef - New therapeutic agents in diabetic nephropathy
Yaeni Kim, Cheol Whee Park
The Korean Journal of Internal Medicine.2017; 32(1): 11. CrossRef - Urine clusterin/apolipoprotein J is linked to tubular damage and renal outcomes in patients with type 2 diabetes mellitus
Sang Soo Kim, Sang Heon Song, Jong Ho Kim, Yun Kyung Jeon, Bo Hyun Kim, Min‐Cheol Kang, Sung Wan Chun, Soo Hyun Hong, Michelle Chung, Yong Ki Kim, In Joo Kim, Young‐Bum Kim
Clinical Endocrinology.2017; 87(2): 156. CrossRef - Treatment of diabetic kidney disease: current and future targets
Mi-Kyung Kim
The Korean Journal of Internal Medicine.2017; 32(4): 622. CrossRef - Sphingosine kinase 1 mediates AGEs-induced fibronectin upregulation in diabetic nephropathy
Cheng Chen, Wenyan Gong, Changzheng Li, Fengxiao Xiong, Shaogui Wang, Junying Huang, Yu Wang, Zhiquan Chen, Qiuhong Chen, Peiqing Liu, Tian Lan, Heqing Huang
Oncotarget.2017; 8(45): 78660. CrossRef - Comparison between Atorvastatin and Rosuvastatin in Renal Function Decline among Patients with Diabetes
Eugene Han, Gyuri Kim, Ji-Yeon Lee, Yong-ho Lee, Beom Seok Kim, Byung-Wan Lee, Bong-Soo Cha, Eun Seok Kang
Endocrinology and Metabolism.2017; 32(2): 274. CrossRef - Glycemic Management of Patients Undergoing Dialysis
Mi-Kyung Kim
The Journal of Korean Diabetes.2016; 17(3): 164. CrossRef - Probucol in Albuminuric Type 2 Diabetes Mellitus Patients on Renin–Angiotensin System Blockade
Sang-Man Jin, Kyung Ah Han, Jae Myung Yu, Tae Seo Sohn, Sung Hee Choi, Choon Hee Chung, Ie Byung Park, Eun Jung Rhee, Sei Hyun Baik, Tae Sun Park, In-Kyu Lee, Seung-Hyun Ko, You-Cheol Hwang, Bong Soo Cha, Hyoung Woo Lee, Moon-Suk Nam, Moon-Kyu Lee
Arteriosclerosis, Thrombosis, and Vascular Biology.2016; 36(10): 2108. CrossRef - MicroRNA-27a promotes renal tubulointerstitial fibrosis via suppressing PPARγ pathway in diabetic nephropathy
Xiaoyan Hou, Jianwei Tian, Jian Geng, Xiao Li, Xun Tang, Jun Zhang, Xiaoyan Bai
Oncotarget.2016; 7(30): 47760. CrossRef - Lipoprotein(a) predicts a new onset of chronic kidney disease in people with Type 2 diabetes mellitus
J.‐S. Yun, Y.‐B. Ahn, K.‐H. Song, K.‐D. Yoo, Y.‐M. Park, H.‐W. Kim, S.‐H. Ko
Diabetic Medicine.2016; 33(5): 639. CrossRef - Metabolic biomarkers for chronic kidney disease
Marc Breit, Klaus M. Weinberger
Archives of Biochemistry and Biophysics.2016; 589: 62. CrossRef - Effect of Sodium-Glucose Co-Transporter 2 Inhibitor, Dapagliflozin, on Renal Renin-Angiotensin System in an Animal Model of Type 2 Diabetes
Seok Joon Shin, Sungjin Chung, Soo Jung Kim, Eun-Mi Lee, Young-Hye Yoo, Ji-Won Kim, Yu-Bae Ahn, Eun-Sook Kim, Sung-Dae Moon, Myung-Jun Kim, Seung-Hyun Ko, Kwang-Hyun Baek
PLOS ONE.2016; 11(11): e0165703. CrossRef - Renoprotective Effect of Gemigliptin, a Dipeptidyl Peptidase-4 Inhibitor, in Streptozotocin-Induced Type 1 Diabetic Mice
Gwon-Soo Jung, Jae-Han Jeon, Mi Sun Choe, Sung-Woo Kim, In-Kyu Lee, Mi-Kyung Kim, Keun-Gyu Park
Diabetes & Metabolism Journal.2016; 40(3): 211. CrossRef - Beneficial effects of previous exercise training on renal changes in streptozotocin-induced diabetic female rats
Liliany S de Brito Amaral, Fernanda A Silva, Vicente B Correia, Clara EF Andrade, Bárbara A Dutra, Márcio V Oliveira, Amélia CM de Magalhães, Rildo A Volpini, Antonio C Seguro, Terezila M Coimbra, Telma de J Soares
Experimental Biology and Medicine.2016; 241(4): 437. CrossRef - Adenosine monophosphate–activated protein kinase in diabetic nephropathy
Yaeni Kim, Cheol Whee Park
Kidney Research and Clinical Practice.2016; 35(2): 69. CrossRef - Estimated Glucose Disposal Rate (eGDR) – A Marker for the Assessment of Insulin Resistance in Type 1 Diabetes Mellitus
Mihaela L. Bîcu, Daniel Bîcu, Sigina Gârgavu, Magdalena Sandu, Mihaela I. Vladu, Diana Clenciu, Eugen Moţa, Maria Moţa
Romanian Journal of Diabetes Nutrition and Metabolic Diseases.2016; 23(2): 177. CrossRef - Polydatin attenuates AGEs-induced upregulation of fibronectin and ICAM-1 in rat glomerular mesangial cells and db/db diabetic mice kidneys by inhibiting the activation of the SphK1-S1P signaling pathway
Cheng Chen, Kaipeng Huang, Jie Hao, Junying Huang, Zhiying Yang, Fengxiao Xiong, Peiqing Liu, Heqing Huang
Molecular and Cellular Endocrinology.2016; 427: 45. CrossRef - Glycated albumin and the risk of micro- and macrovascular complications in subjects with Type 1 Diabetes
Hye-jin Yoon, Yong-ho Lee, So Ra Kim, Tyler Hyungtaek Rim, Eun Young Lee, Eun Seok Kang, Bong-Soo Cha, Hyun Chul Lee, Byung-Wan Lee
Cardiovascular Diabetology.2015;[Epub] CrossRef - Tripterygium Glycosides Tablet Ameliorates Renal Tubulointerstitial Fibrosis via the Toll-Like Receptor 4/Nuclear Factor Kappa B Signaling Pathway in High-Fat Diet Fed and Streptozotocin-Induced Diabetic Rats
Ze-jun Ma, Xiao-na Zhang, Li Li, Wei Yang, Shan-shan Wang, Xin Guo, Pei Sun, Li-ming Chen
Journal of Diabetes Research.2015; 2015: 1. CrossRef - The association between abnormal heart rate variability and new onset of chronic kidney disease in patients with type 2 diabetes: A ten-year follow-up study
Jae-Seung Yun, Yu-Bae Ahn, Ki-Ho Song, Ki-Dong Yoo, Hyung-Wook Kim, Yong-Moon Park, Seung-Hyun Ko
Diabetes Research and Clinical Practice.2015; 108(1): 31. CrossRef - Finerenone: third-generation mineralocorticoid receptor antagonist for the treatment of heart failure and diabetic kidney disease
Licette CY Liu, Elise Schutte, Ron T Gansevoort, Peter van der Meer, Adriaan A Voors
Expert Opinion on Investigational Drugs.2015; 24(8): 1123. CrossRef - Effects of pentoxifylline on proteinuria and glucose control in patients with type 2 diabetes: a prospective randomized double-blind multicenter study
Seung Jin Han, Hae Jin Kim, Dae Jung Kim, Seung Soo Sheen, Choon Hee Chung, Chul Woo Ahn, Se Hwa Kim, Yong-Wook Cho, Seok Won Park, Soo-Kyung Kim, Chul Sik Kim, Kyung Wook Kim, Kwan Woo Lee
Diabetology & Metabolic Syndrome.2015;[Epub] CrossRef - Proteomic Profile in Glomeruli of Type-2 Diabetic KKAy Mice using 2-Dimensional Differential Gel Electrophoresis
Lining Wang
Medical Science Monitor.2014; 20: 2705. CrossRef
- N6-methyladenosine RNA methylation in diabetic kidney disease

 KDA
KDA
 First
First Prev
Prev





