
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Previous issues
- Page Path
- HOME > Browse > Previous issues
Sulwon Lecture 2022
- Others
- Opening the Precision Diabetes Care through Digital Healthcare
- Joonyub Lee, Jin Yu, Kun-Ho Yoon
- Diabetes Metab J. 2023;47(3):307-314. Published online March 29, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0386

- 5,229 View
- 247 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The national healthcare systems of every country in the world cannot sustain the rise in healthcare expenditure caused by chronic diseases and their complications. To sustain the national healthcare system, a novel system should be developed to improve the quality of care and minimize healthcare costs. For 20 years, our team developed patient-communicating digital healthcare platforms and proved their efficacy. National scale randomized control trials are underway to systematically measure the efficacy and economic benefits of this digital health care system. Precision medicine aims to maximize effectiveness of disease management by considering individual variability. Digital health technologies enable precision medicine at a reasonable cost that was not available before. The government launched the “National Integrated Bio-big Data Project” which will collect diverse health data from the participants. Individuals will share their health information to physicians or researchers at their will by gateway named “My-Healthway.’ Taken together, now we stand in front of the evolution of medical care, so-called “Precision medicine.” led by various kinds of technologies and a huge amount of health information exchange. We should lead these new trends as pioneers, not as followers, to establish and implement the best care for our patients that can help them to withstand their devastating diseases.
Reviews
- Basic Research
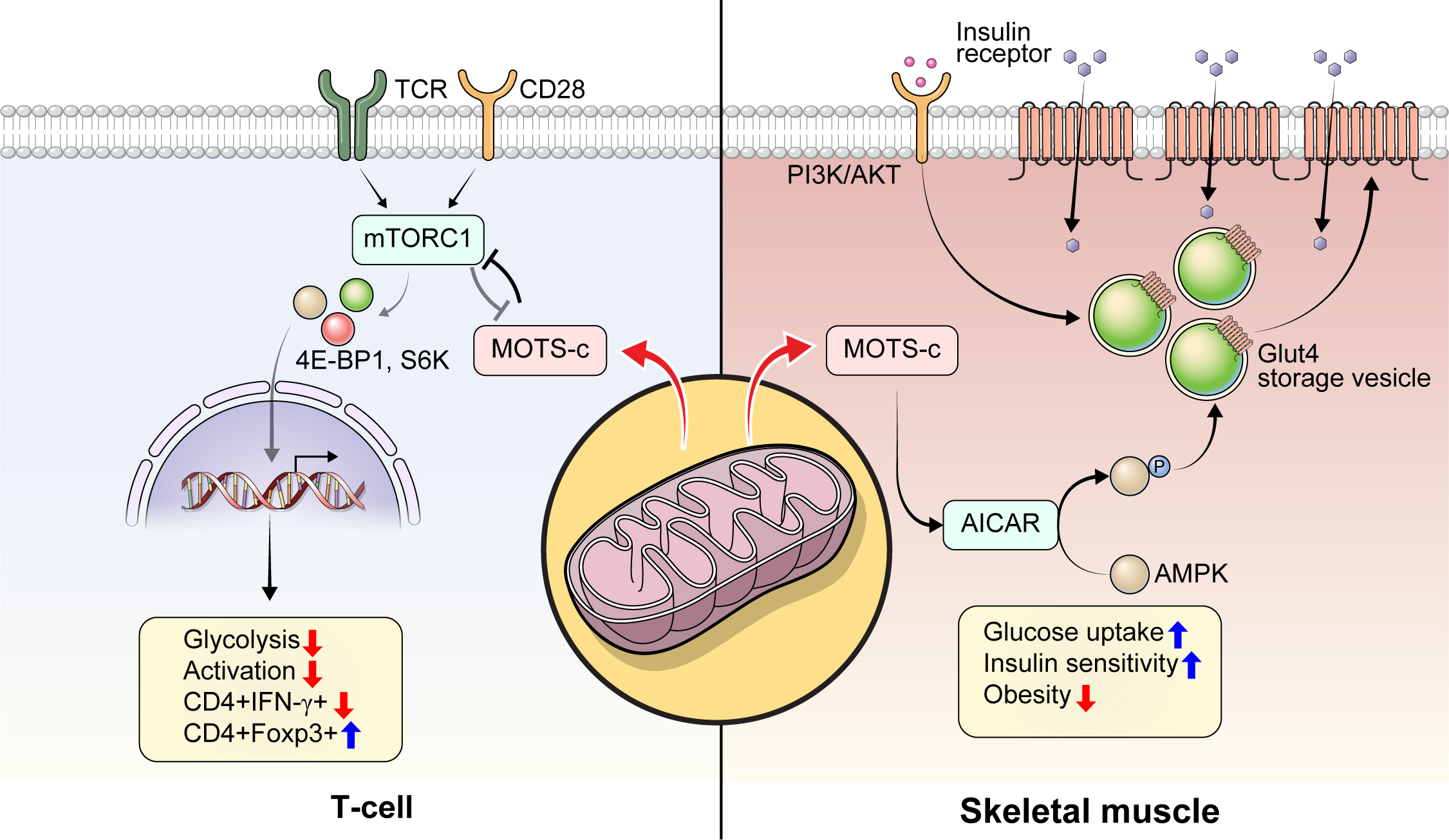
- Mitochondrial-Encoded Peptide MOTS-c, Diabetes, and Aging-Related Diseases
- Byung Soo Kong, Changhan Lee, Young Min Cho
- Diabetes Metab J. 2023;47(3):315-324. Published online February 24, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0333
- 5,709 View
- 284 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Mitochondria are complex metabolic organelles with manifold pathophysiological implications in diabetes. Currently published mitochondrial-encoded peptides, which are expressed from the mitochondrial open reading frame of the 12S ribosomal RNA type-c (MOTS-c), 16S rRNA (humanin and short humanin like peptide 1-6 [SHLP1-6]), or small human mitochondrial open reading frame over serine tRNA (SHMOOSE) are associated with regulation of cellular metabolism and insulin action in age-related diseases, such as type 2 diabetes mellitus. This review focuses mainly on recent advances in MOTS-c research with regards to diabetes, including both type 1 and type 2. The emerging understanding of MOTS-c in diabetes may provide insight into the development of new therapies for diabetes and other age or senescence-related diseases.
-
Citations
Citations to this article as recorded by- Mitochondrial-derived peptides: Antidiabetic functions and evolutionary perspectives
Satadeepa Kal, Sumana Mahata, Suborno Jati, Sushil K. Mahata
Peptides.2024; 172: 171147. CrossRef - Mitochondrial Stress and Mitokines: Therapeutic Perspectives for the Treatment of Metabolic Diseases
Benyuan Zhang, Joon Young Chang, Min Hee Lee, Sang-Hyeon Ju, Hyon-Seung Yi, Minho Shong
Diabetes & Metabolism Journal.2024; 48(1): 1. CrossRef - Mitochondrial bioenergetics, metabolism, and beyond in pancreatic β-cells and diabetes
Alejandra María Rivera Nieves, Brian Michael Wauford, Accalia Fu
Frontiers in Molecular Biosciences.2024;[Epub] CrossRef
- Mitochondrial-derived peptides: Antidiabetic functions and evolutionary perspectives
- Drug/Regimen
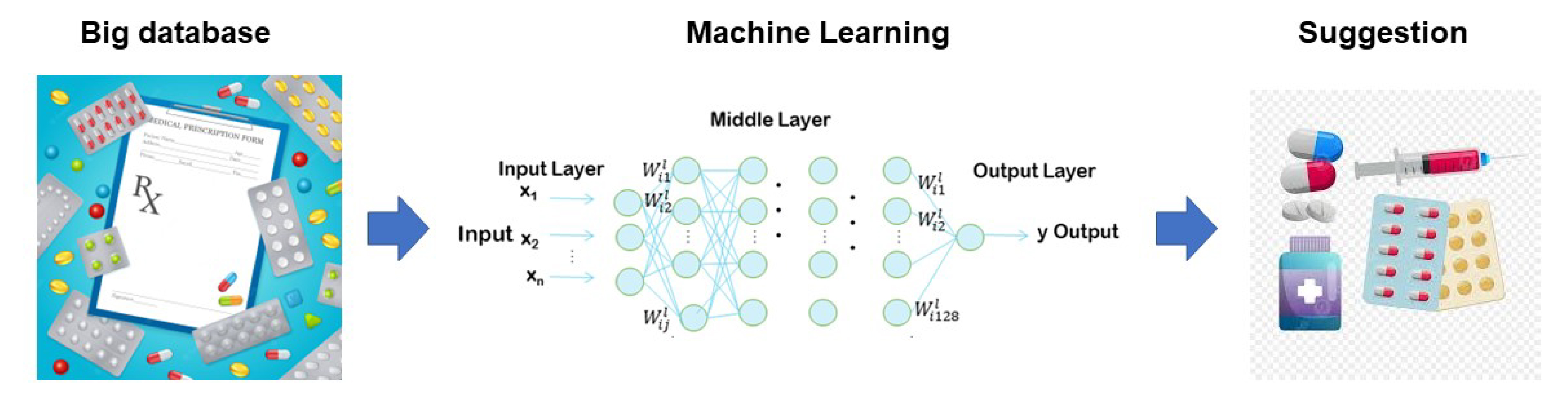
- Machine Learning Approach to Drug Treatment Strategy for Diabetes Care
- Kazuya Fujihara, Hirohito Sone
- Diabetes Metab J. 2023;47(3):325-332. Published online January 12, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0349
- 65,535 View
- 247 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Globally, the number of people with diabetes mellitus has quadrupled in the past three decades, and approximately one in 11 adults worldwide have diabetes mellitus. Since both microvascular and macrovascular diseases in patients with diabetes predispose them to a lower quality of life as well as higher rates of mortality, managing blood glucose levels is of clinical relevance in diabetes care. Many classes of antihyperglycemic drugs are currently approved to treat hyperglycemia in patients with type 2 diabetes mellitus, with several new drugs having been developed during the last decade. Diabetes-related complications have been reduced substantially worldwide. Prioritization of therapeutic agents varies according to national guidelines. However, since the characteristics of participants in clinical trials differ from patients in actual clinical practice, it is difficult to apply the results of such trials to clinical practice. Machine learning approaches became highly topical issues in medicine along with rapid technological innovations in the fields of information and communication in the 1990s. However, adopting these technologies to support decision-making regarding drug treatment strategies for diabetes care has been slow. This review summarizes data from recent studies on the choice of drugs for type 2 diabetes mellitus focusing on machine learning approaches.
-
Citations
Citations to this article as recorded by- Exploring antioxidant activities and inhibitory effects against α‐amylase and α‐glucosidase of Elaeocarpus braceanus fruits: insights into mechanisms by molecular docking and molecular dynamics
Hong Li, Yuanyue Zhang, Zhijia Liu, Chaofan Guo, Maurizio Battino, Shengbao Cai, Junjie Yi
International Journal of Food Science & Technology.2024; 59(1): 343. CrossRef - 3D Convolutional Neural Networks for Predicting Protein Structure for Improved Drug Recommendation
Pokkuluri Kiran Sree, SSSN Usha Devi N
EAI Endorsed Transactions on Pervasive Health and Technology.2024;[Epub] CrossRef
- Exploring antioxidant activities and inhibitory effects against α‐amylase and α‐glucosidase of Elaeocarpus braceanus fruits: insights into mechanisms by molecular docking and molecular dynamics
- Metabolic Risk/Epidemiology
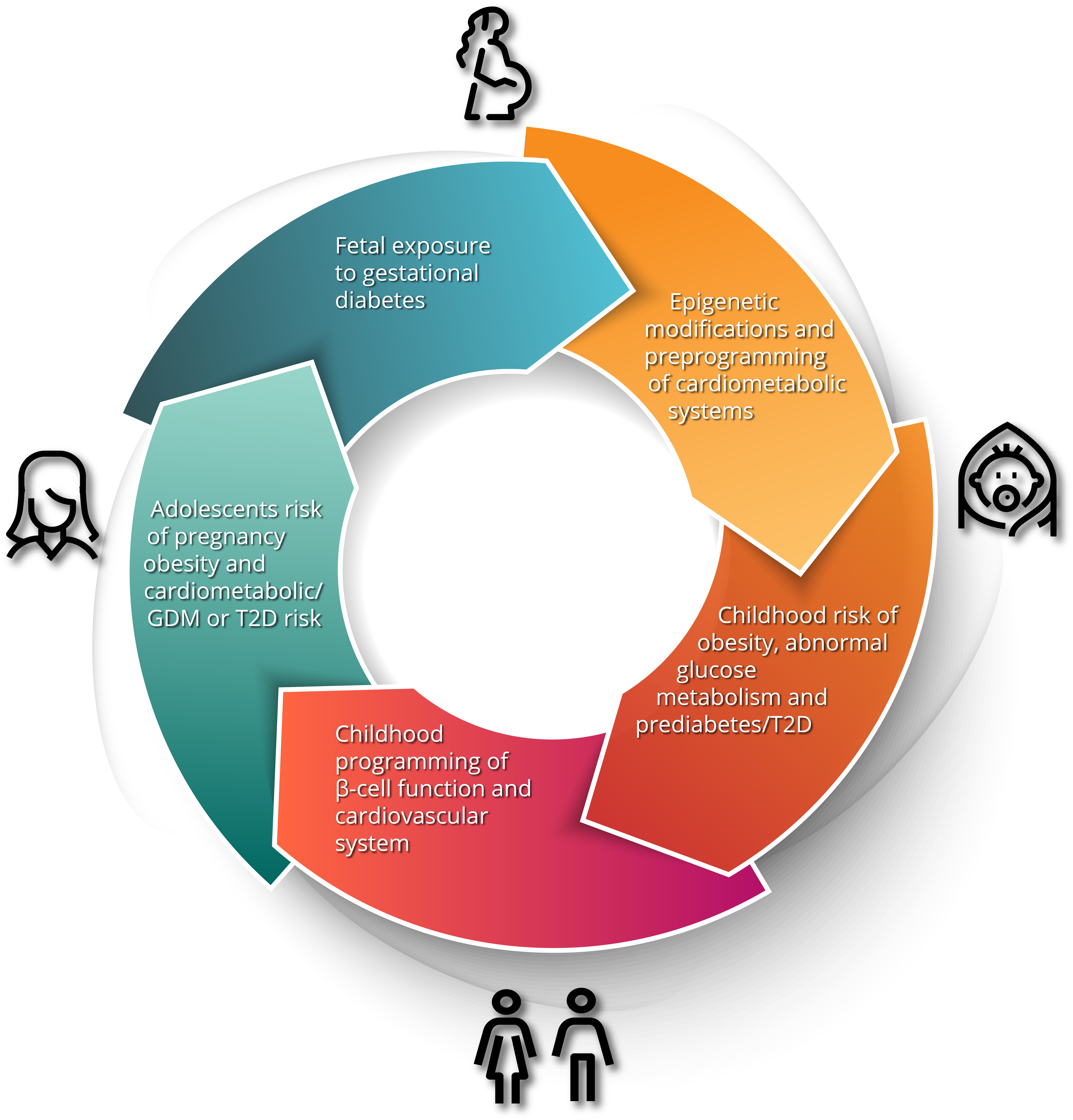
- Gestational Diabetes Mellitus and Its Implications across the Life Span
- Brandy Wicklow, Ravi Retnakaran
- Diabetes Metab J. 2023;47(3):333-344. Published online February 8, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0348
- 5,205 View
- 410 Download
- 6 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Gestational diabetes mellitus (GDM) has historically been perceived as a medical complication of pregnancy that also serves as a harbinger of maternal risk of developing type 2 diabetes mellitus (T2DM) in the future. In recent decades, a growing body of evidence has detailed additional lifelong implications that extend beyond T2DM, including an elevated risk of ultimately developing cardiovascular disease. Furthermore, the risk factors that mediate this lifetime cardiovascular risk are evident not only after delivery but are present even before the pregnancy in which GDM is first diagnosed. The concept thus emerging from these data is that the diagnosis of GDM enables the identification of women who are already on an enhanced track of cardiometabolic risk that starts early in life. Studies of the offspring of pregnancies complicated by diabetes now suggest that the earliest underpinnings of this cardiometabolic risk profile may be determined in utero and may first manifest clinically in childhood. Accordingly, from this perspective, GDM is now seen as a chronic metabolic disorder that holds implications across the life span of both mother and child.
-
Citations
Citations to this article as recorded by- ATP5me alleviates high glucose-induced myocardial cell injury
Qingsha Hou, Fang Yan, Xiuling Li, Huanling Liu, Xiang Yang, Xudong Dong
International Immunopharmacology.2024; 129: 111626. CrossRef - Prevalence and Predictors of Gestational Diabetes Mellitus and Overt Diabetes in Pregnancy: A Secondary Analysis of Nationwide Data from India
Saurav Basu, Vansh Maheshwari, Rutul Gokalani, Chandrakant Lahariya
Preventive Medicine: Research & Reviews.2024; 1(1): 52. CrossRef - Serum betaine and dimethylglycine in mid-pregnancy and the risk of gestational diabetes mellitus: a case-control study
Ziqing Zhou, Yao Yao, Yanan Sun, Xin Wang, Shang Huang, Jianli Hou, Lijun Wang, Fengxiang Wei
Endocrine.2024;[Epub] CrossRef - Quality assessment of videos on social media platforms related to gestational diabetes mellitus in China: A cross-section study
Qin-Yu Cai, Jing Tang, Si-Zhe Meng, Yi Sun, Xia Lan, Tai-Hang Liu
Heliyon.2024; 10(7): e29020. CrossRef - Inflammation and decreased cardiovagal modulation are linked to stress and depression at 36th week of pregnancy in gestational diabetes mellitus
Manoharan Renugasundari, Gopal Krushna Pal, Latha Chaturvedula, Nivedita Nanda, K. T. Harichandrakumar, Thiyagarajan Durgadevi
Scientific Reports.2023;[Epub] CrossRef - Women with gestational diabetes mellitus, controlled for plasma glucose level, exhibit maternal and fetal dyslipidaemia that may warrant treatment
Barbara J. Meyer, Colin Cortie, Marloes Dekker-Nitert, Helen L. Barrett, Dilys J. Freeman
Diabetes Research and Clinical Practice.2023; 204: 110929. CrossRef - Pregnancy diet to prevent gestational diabetes: study design and dietary assessments
Sylvia H. Ley
The American Journal of Clinical Nutrition.2023; 118(5): 847. CrossRef
- ATP5me alleviates high glucose-induced myocardial cell injury
Editorial
- Navigating the Seas of Glycemic Control: The Role of Continuous Glucose Monitoring in Type 1 Diabetes Mellitus
- Jun Sung Moon
- Diabetes Metab J. 2023;47(3):345-346. Published online May 26, 2023
- DOI: https://doi.org/10.4093/dmj.2023.0125
- 1,210 View
- 91 Download
Original Articles
- Guideline/Fact Sheet
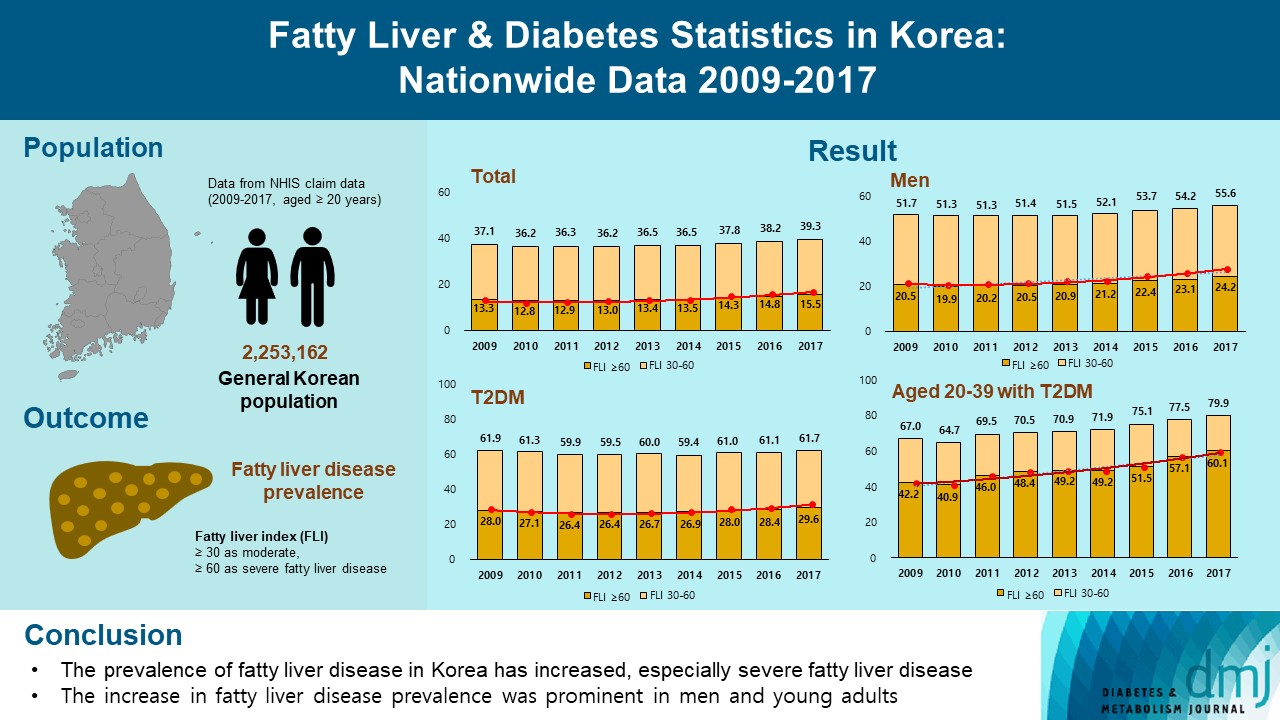
- Fatty Liver & Diabetes Statistics in Korea: Nationwide Data 2009 to 2017
- Eugene Han, Kyung-Do Han, Yong-ho Lee, Kyung-Soo Kim, Sangmo Hong, Jung Hwan Park, Cheol-Young Park, on Behalf of Fatty Liver Research Group of the Korean Diabetes Association
- Diabetes Metab J. 2023;47(3):347-355. Published online March 29, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0444
- 3,537 View
- 206 Download
- 5 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study investigated the changes of fatty liver disease prevalence in general Korean population.
Methods
This study analyzed data from the Korean National Health Insurance Service from 2009 to 2017 that included individuals aged 20 years or older who had undergone a medical health examination. Fatty liver disease was assessed using the fatty liver index (FLI). The disease severity was defined by FLI cutoff, ≥30 as moderate, and ≥60 as severe fatty liver disease.
Results
The prevalence of Korean adults aged 20 years or over with fatty liver disease (FLI ≥60) increased from 13.3% in 2009 to 15.5% in 2017 (P for trend <0.001). The increase in fatty liver disease prevalence was prominent in men (from 20.5% to 24.2%) and the young age (20 to 39 years) group (from 12.8% to 16.4%) (P for interaction <0.001). The prevalence of fatty liver disease was the highest in type 2 diabetes mellitus (T2DM, 29.6%) population compared to that of prediabetes or normoglycemia (10.0% and 21.8%) in 2017. The prevalence of fatty liver disease had statistically increased in individuals with T2DM and prediabetes (P for trend <0.001). Its prevalence increased more steeply in the young-aged population with T2DM, from 42.2% in 2009 to 60.1% in 2017. When applying a lower FLI cutoff (≥30) similar results were observed.
Conclusion
The prevalence of fatty liver disease in the Korean population has increased. Individuals who are young, male, and have T2DM are vulnerable to fatty liver disease. -
Citations
Citations to this article as recorded by- Longitudinal changes in fatty liver index are associated with risk of hepatocellular carcinoma: A nationwide cohort study in Korea
Min Gu Kang, Chang Hun Lee, Chen Shen, Jong Seung Kim, Ji Hyun Park
Journal of Hepatology.2024; 80(5): e216. CrossRef - Repeated detection of non‐alcoholic fatty liver disease increases the incidence risk of type 2 diabetes in young adults
Jin Hwa Kim, Young Sang Lyu, Mee Kyoung Kim, Sang Yong Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024; 26(1): 180. CrossRef - Mortality in metabolic dysfunction-associated steatotic liver disease: A nationwide population-based cohort study
Eugene Han, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Sang Hoon Ahn, Yong-ho Lee, Seung Up Kim
Metabolism.2024; 152: 155789. CrossRef - Association of non-alcoholic fatty liver disease with cardiovascular disease and all cause death in patients with type 2 diabetes mellitus: nationwide population based study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
BMJ.2024; : e076388. CrossRef - Hepatic Fibrosis and Cancer: The Silent Threats of Metabolic Syndrome
Scott L. Friedman
Diabetes & Metabolism Journal.2024; 48(2): 161. CrossRef - Reply to G. Wang et al
Joo-Hyun Park, Jung Yong Hong, Kyungdo Han
Journal of Clinical Oncology.2023; 41(32): 5070. CrossRef - The Role of the Fatty Liver Index (FLI) in the Management of Non-Alcoholic Fatty Liver Disease: A Systematic Review
Teodora Biciusca, Sorina Ionelia Stan, Mara Amalia Balteanu, Ramona Cioboata, Alice Elena Ghenea, Suzana Danoiu, Ana-Maria Bumbea, Viorel Biciusca
Diagnostics.2023; 13(21): 3316. CrossRef - Lean or Non-obese Nonalcoholic Fatty Liver Disease Patients: Are They Really Lean?
Eugene Han, Yong-ho Lee
Clinical and Molecular Hepatology.2023; 29(4): 980. CrossRef - Approach to Fatty Liver Disease in Patients with Type 2 Diabetes
Ji Cheol Bae
The Journal of Korean Diabetes.2023; 24(3): 107. CrossRef
- Longitudinal changes in fatty liver index are associated with risk of hepatocellular carcinoma: A nationwide cohort study in Korea
- COVID-19
- Safety of COVID-19 Vaccines among Patients with Type 2 Diabetes Mellitus: Real-World Data Analysis
- Hye Jun Kim, Sang Jun Lee, Soonok Sa, Jung Ho Bae, Gyuseon Song, Chae Won Lee, Ju Hee Kim, Sung Ryul Shim, Myunghee Hong, Hyun Wook Han
- Diabetes Metab J. 2023;47(3):356-365. Published online March 6, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0129

- 3,970 View
- 239 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Little is known about the adverse events (AEs) associated with coronavirus disease 2019 (COVID-19) vaccination in patients with type 2 diabetes mellitus (T2DM).
Methods
This study used vaccine AE reporting system data to investigate severe AEs among vaccinated patients with T2DM. A natural language processing algorithm was applied to identify people with and without diabetes. After 1:3 matching, we collected data for 6,829 patients with T2DM and 20,487 healthy controls. Multiple logistic regression analysis was used to calculate the odds ratio for severe AEs.
Results
After COVID-19 vaccination, patients with T2DM were more likely to experience eight severe AEs than controls: cerebral venous sinus thrombosis, encephalitis myelitis encephalomyelitis, Bell’s palsy, lymphadenopathy, ischemic stroke, deep vein thrombosis (DVT), thrombocytopenia (TP), and pulmonary embolism (PE). Moreover, patients with T2DM vaccinated with BNT162b2 and mRNA-1273 were more vulnerable to DVT and TP than those vaccinated with JNJ-78436735. Among patients with T2DM administered mRNA vaccines, mRNA-1273 was safer than BNT162b2 in terms of the risk of DVT and PE.
Conclusion
Careful monitoring of severe AEs in patients with T2DM may be necessary, especially for those related to thrombotic events and neurological dysfunctions after COVID-19 vaccination. -
Citations
Citations to this article as recorded by- Herbal-based therapeutics for diabetic patients with SARS-Cov-2 infection
Yousef Rasmi, Ighli di Bari, Shah Faisal, Munima Haque, Pornanong Aramwit, Aline da Silva, Elmira Roshani Asl
Molecular Biology Reports.2024;[Epub] CrossRef - Tuberculosis vaccines update: Is an RNA-based vaccine feasible for tuberculosis?
Sasha E. Larsen, Susan L. Baldwin, Rhea N. Coler
International Journal of Infectious Diseases.2023; 130: S47. CrossRef - Neurological Disorders following COVID-19 Vaccination
Ying Yang, Lisu Huang
Vaccines.2023; 11(6): 1114. CrossRef - Safety of COVID-19 Vaccines among Patients with Type 2 Diabetes Mellitus: Real-World Data Analysis (Diabetes Metab J 2023;47:356-65)
Hye Jun Kim, Sung Ryul Shim, Myunghee Hong, Hyun Wook Han
Diabetes & Metabolism Journal.2023; 47(5): 717. CrossRef - Safety of COVID-19 Vaccines among Patients with Type 2 Diabetes Mellitus: Real-World Data Analysis (Diabetes Metab J 2023;47:356-65)
Jung Hun Ohn
Diabetes & Metabolism Journal.2023; 47(5): 715. CrossRef
- Herbal-based therapeutics for diabetic patients with SARS-Cov-2 infection
- Basic Research
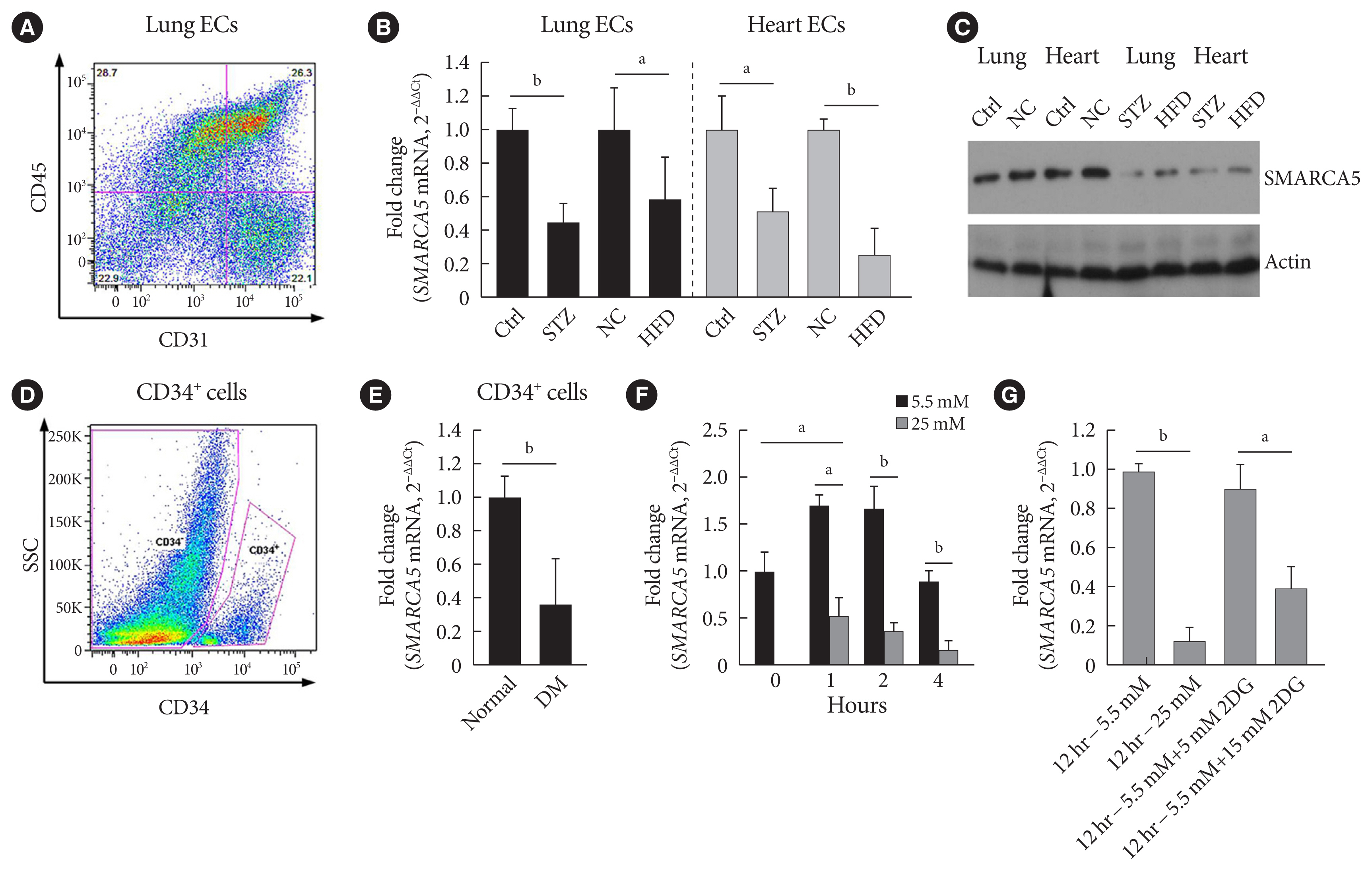
- Hyperglycemia-Suppressed SMARCA5 Disrupts Transcriptional Homeostasis to Facilitate Endothelial Dysfunction in Diabetes
- Ju Wang, Hui Zhou, Jinhua Shao, Shu Zhang, Jing Jin
- Diabetes Metab J. 2023;47(3):366-381. Published online March 6, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0179
- 1,674 View
- 98 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Dysfunction of vascular endothelial cells (ECs) plays a central role in the pathogenesis of cardiovascular complications in diabetes. SWI/SNF-related matrix-associated actin-dependent regulator of chromatin subfamily A member 5 (SMARCA5) is a key regulator of chromatin structure and DNA repair, but its role in ECs remains surprisingly unexplored. The current study was designed to elucidate the regulated expression and function of SMARCA5 in diabetic ECs.
Methods
SMARCA5 expression was evaluated in ECs from diabetic mouse and human circulating CD34+ cells using quantitative reverse transcription polymerase chain reaction and Western blot. Effects of SMARCA5 manipulation on ECs function were evaluated using cell migration, in vitro tube formation and in vivo wound healing assays. Interaction among oxidative stress, SMARCA5 and transcriptional reprogramming was elucidated using luciferase reporter assay, electrophoretic mobility shift assay and chromatin immunoprecipitation.
Results
Endothelial SMARCA5 expression was significantly decreased in diabetic rodents and humans. Hyperglycemia-suppressed SMARCA5 impaired EC migration and tube formation in vitro, and blunted vasculogenesis in vivo. Contrarily, overexpression of SMARCA5 in situ by a SMARCA5 adenovirus-incorporated hydrogel effectively promoted the rate of wound healing in a dorsal skin punch injury model of diabetic mice. Mechanistically, hyperglycemia-elicited oxidative stress suppressed SMARCA5 transactivation in a signal transducer and activator of transcription 3 (STAT3)-dependent manner. Moreover, SMARCA5 maintained transcriptional homeostasis of several pro-angiogenic factors through both direct and indirect chromatin-remodeling mechanisms. In contrast, depletion of SMARCA5 disrupted transcriptional homeostasis to render ECs unresponsive to established angiogenic factors, which ultimately resulted in endothelial dysfunction in diabetes.
Conclusion
Suppression of endothelial SMARCA5 contributes to, at least in part, multiple aspects of endothelial dysfunction, which may thereby exacerbate cardiovascular complications in diabetes.
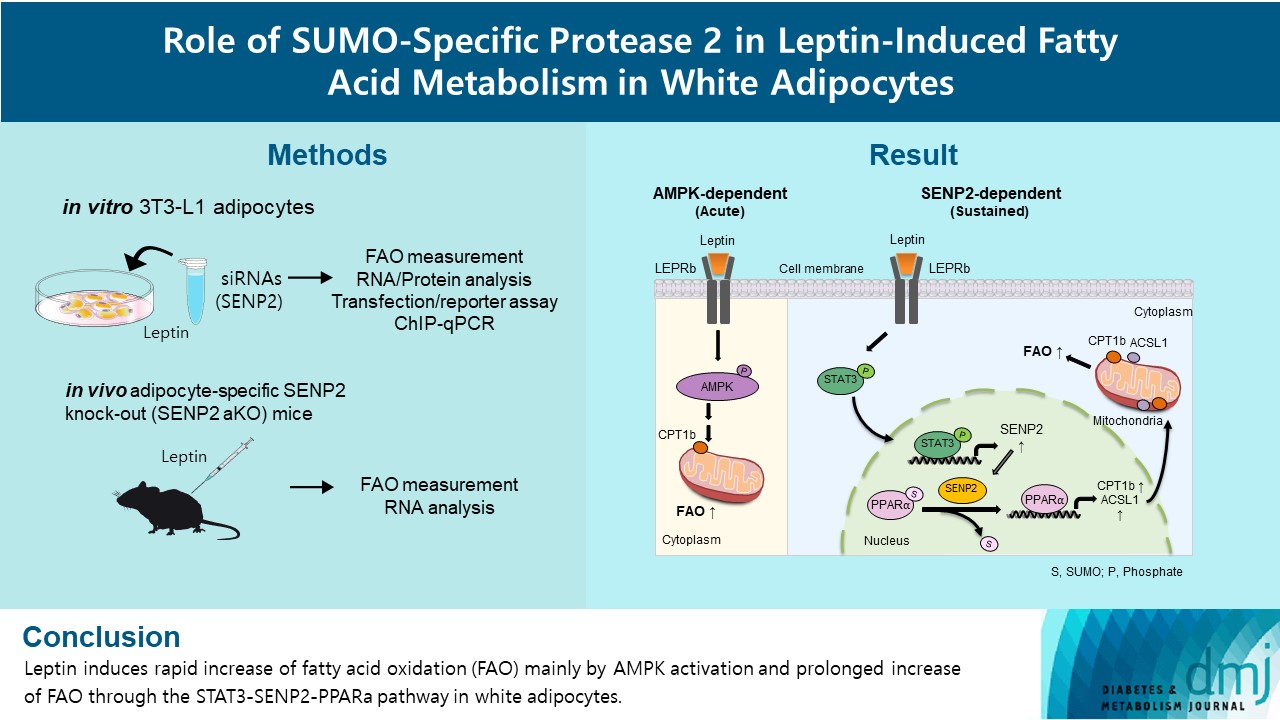
- Basic Research
- Role of SUMO-Specific Protease 2 in Leptin-Induced Fatty Acid Metabolism in White Adipocytes
- Praise Chanmee Kim, Ji Seon Lee, Sung Soo Chung, Kyong Soo Park
- Diabetes Metab J. 2023;47(3):382-393. Published online March 6, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0156
- 3,188 View
- 158 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Leptin is a 16-kDa fat-derived hormone with a primary role in controlling adipose tissue levels. Leptin increases fatty acid oxidation (FAO) acutely through adenosine monophosphate-activated protein kinase (AMPK) and on delay through the SUMO-specific protease 2 (SENP2)–peroxisome proliferator-activated receptor δ/γ (PPARδ/γ) pathway in skeletal muscle. Leptin also directly increases FAO and decreases lipogenesis in adipocytes; however, the mechanism behind these effects remains unknown. Here, we investigated the role of SENP2 in the regulation of fatty acid metabolism by leptin in adipocytes and white adipose tissues.
Methods
The effects of leptin mediated by SENP2 on fatty acid metabolism were tested by siRNA-mediated knockdown in 3T3-L1 adipocytes. The role of SENP2 was confirmed in vivo using adipocyte-specific Senp2 knockout (Senp2-aKO) mice. We revealed the molecular mechanism involved in the leptin-induced transcriptional regulation of carnitine palmitoyl transferase 1b (Cpt1b) and long-chain acyl-coenzyme A synthetase 1 (Acsl1) using transfection/reporter assays and chromatin immunoprecipitation.
Results
SENP2 mediated the increased expression of FAO-associated enzymes, CPT1b and ACSL1, which peaked 24 hours after leptin treatment in adipocytes. In contrast, leptin stimulated FAO through AMPK during the initial several hours after treatment. In white adipose tissues, FAO and mRNA levels of Cpt1b and Acsl1 were increased by 2-fold 24 hours after leptin injection in control mice but not in Senp2-aKO mice. Leptin increased PPARα binding to the Cpt1b and Acsl1 promoters in adipocytes through SENP2.
Conclusion
These results suggest that the SENP2-PPARα pathway plays an important role in leptin-induced FAO in white adipocytes. -
Citations
Citations to this article as recorded by- Intermittent cold stimulation affects energy metabolism and improves stress resistance in broiler heart
Tingting Li, Haidong Wei, Shijie Zhang, Xiaotao Liu, Lu Xing, Yuanyuan Liu, Rixin Gong, Jianhong Li
Poultry Science.2024; 103(1): 103190. CrossRef
- Intermittent cold stimulation affects energy metabolism and improves stress resistance in broiler heart
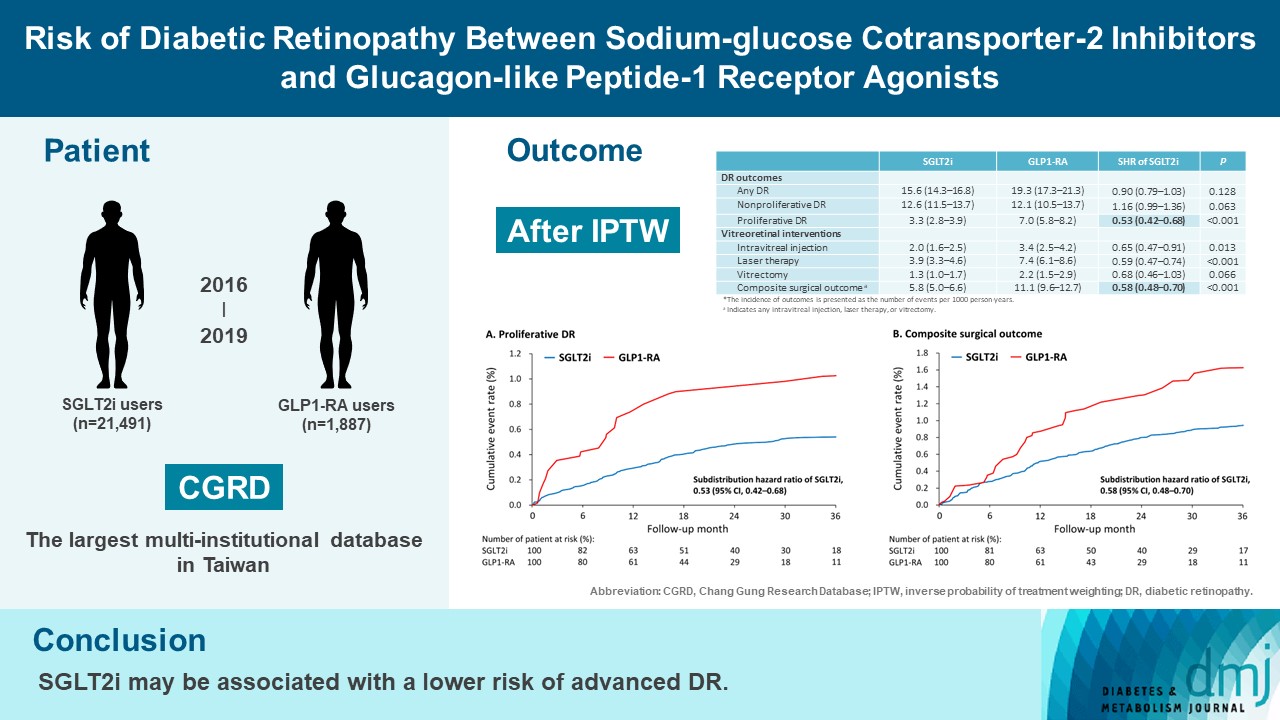
- Drug/Regimen
- Risk of Diabetic Retinopathy between Sodium-Glucose Cotransporter-2 Inhibitors and Glucagon-Like Peptide-1 Receptor Agonists
- Tzu-Yi Lin, Eugene Yu-Chuan Kang, Shih-Chieh Shao, Edward Chia-Cheng Lai, Sunir J. Garg, Kuan-Jen Chen, Je-Ho Kang, Wei-Chi Wu, Chi-Chun Lai, Yih-Shiou Hwang
- Diabetes Metab J. 2023;47(3):394-404. Published online March 6, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0221
- 6,547 View
- 271 Download
- 7 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To compare risk of diabetic retinopathy (DR) between patients taking sodium-glucose cotransporter-2 inhibitors (SGLT2is) and those taking glucagon-like peptide-1 receptor agonists (GLP1-RAs) in routine care.
Methods
This retrospective cohort study emulating a target trial included patient data from the multi-institutional Chang Gung Research Database in Taiwan. Totally, 33,021 patients with type 2 diabetes mellitus using SGLT2is and GLP1-RAs between 2016 and 2019 were identified. 3,249 patients were excluded due to missing demographics, age <40 years, prior use of any study drug, a diagnosis of retinal disorders, a history of receiving vitreoretinal procedure, no baseline glycosylated hemoglobin, or no follow-up data. Baseline characteristics were balanced using inverse probability of treatment weighting with propensity scores. DR diagnoses and vitreoretinal interventions served as the primary outcomes. Occurrence of proliferative DR and DR receiving vitreoretinal interventions were regarded as vision-threatening DR.
Results
There were 21,491 SGLT2i and 1,887 GLP1-RA users included for the analysis. Patients receiving SGLT2is and GLP-1 RAs exhibited comparable rate of any DR (subdistribution hazard ratio [SHR], 0.90; 95% confidence interval [CI], 0.79 to 1.03), whereas the rate of proliferative DR (SHR, 0.53; 95% CI, 0.42 to 0.68) was significantly lower in the SGLT2i group. Also, SGLT2i users showed significantly reduced risk of composite surgical outcome (SHR, 0.58; 95% CI, 0.48 to 0.70).
Conclusion
Compared to those taking GLP1-RAs, patients receiving SGLT2is had a lower risk of proliferative DR and vitreoretinal interventions, although the rate of any DR was comparable between the SGLT2i and GLP1-RA groups. Thus, SGLT2is may be associated with a lower risk of vision-threatening DR but not DR development. -
Citations
Citations to this article as recorded by- Incretin‐based drugs and the risk of diabetic retinopathy among individuals with type 2 diabetes: A systematic review and meta‐analysis of observational studies
Samuel Igweokpala, Naheemot Olaoluwa Sule, Antonios Douros, Oriana H. Y. Yu, Kristian B. Filion
Diabetes, Obesity and Metabolism.2024; 26(2): 721. CrossRef - Association of sodium–glucose cotransporter‐2 inhibitors and the risk of retinal vascular occlusion: A real‐world retrospective cohort study in Taiwan
Tzu‐Yi Lin, Eugene Yu‐Chuan Kang, Shih‐Chieh Shao, Edward Chia‐Cheng Lai, Nan‐Kai Wang, Sunir J. Garg, Kuan‐Jen Chen, Je‐Ho Kang, Wei‐Chi Wu, Chi‐Chun Lai, Yih‐Shiou Hwang
Diabetes/Metabolism Research and Reviews.2024;[Epub] CrossRef - Risk of rotator cuff tear and rotator cuff repair surgery comparison between sodium-glucose cotransporter 2 inhibitors and glucagon like peptide-1 receptor agonists: A real-world study
Yu-Chi Su, Pei-Chun Hsieh, Edward Chia-Cheng Lai, Yu-Ching Lin
Diabetes & Metabolism.2024; 50(2): 101522. CrossRef - Optimising renal risk parameters in type 2 diabetes mellitus: Perspectives from a retinal viewpoint
Sarita Jacob, George I. Varughese
Clinical Medicine.2024; 24(2): 100031. CrossRef - Risk of diabetic retinopathy and diabetic macular oedema with sodium–glucose cotransporter 2 inhibitors and glucagon-like peptide 1 receptor agonists in type 2 diabetes: a real-world data study from a global federated database
Aikaterini Eleftheriadou, David Riley, Sizheng S. Zhao, Philip Austin, Gema Hernández, Gregory Y. H. Lip, Timothy L. Jackson, John P. H. Wilding, Uazman Alam
Diabetologia.2024;[Epub] CrossRef - Impact of GLP-1 Agonists and SGLT-2 Inhibitors on Diabetic Retinopathy Progression: An Aggregated Electronic Health Record Data Study
Karen M. Wai, Kapil Mishra, Euna Koo, Cassie Ann Ludwig, Ravi Parikh, Prithvi Mruthyunjaya, Ehsan Rahimy
American Journal of Ophthalmology.2024;[Epub] CrossRef - Risk of Diabetic Retinopathy between Sodium-Glucose Cotransporter-2 Inhibitors and Glucagon-Like Peptide-1 Receptor Agonists (Diabetes Metab J 2023;47:394-404)
Tzu-Yi Lin, Eugene Yu-Chuan Kang, Shih-Chieh Shao, Edward Chia-Cheng Lai, Yih-Shiou Hwang
Diabetes & Metabolism Journal.2023; 47(4): 573. CrossRef - Risk of Diabetic Retinopathy between Sodium-Glucose Cotransporter-2 Inhibitors and Glucagon-Like Peptide-1 Receptor Agonists (Diabetes Metab J 2023;47:394-404)
Jihee Ko, Sun Joon Moon
Diabetes & Metabolism Journal.2023; 47(4): 571. CrossRef - Sodium-Glucose Cotransporter 2 Inhibitors and Risk of Retinopathy in Patients With Type 2 Diabetes
Fu-Shun Yen, James Cheng-Chung Wei, Teng-Shun Yu, Yu-Tung Hung, Chih-Cheng Hsu, Chii-Min Hwu
JAMA Network Open.2023; 6(12): e2348431. CrossRef
- Incretin‐based drugs and the risk of diabetic retinopathy among individuals with type 2 diabetes: A systematic review and meta‐analysis of observational studies
- Technology/Device
- Glycemia according to the Use of Continuous Glucose Monitoring among Adults with Type 1 Diabetes Mellitus in Korea: A Real-World Study
- You-Bin Lee, Minjee Kim, Jae Hyeon Kim
- Diabetes Metab J. 2023;47(3):405-414. Published online March 6, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0032

- 3,256 View
- 122 Download
- 2 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We explored the association between continuous glucose monitoring (CGM) use and glycemia among adults with type 1 diabetes mellitus (T1DM) and determined the status of CGM metrics among adults with T1DM using CGM in the real-world.
Methods
For this propensity-matched cross-sectional study, individuals with T1DM who visited the outpatient clinic of the Endocrinology Department of Samsung Medical Center between March 2018 and February 2020 were screened. Among them, 111 CGM users (for ≥9 months) were matched based on propensity score considering age, sex, and diabetes duration in a 1:2 ratio with 203 CGM never-users. The association between CGM use and glycemic measures was explored. In a subpopulation of CGM users who had been using official applications (not “do-it-yourself” software) such that Ambulatory Glucose Profile data for ≥1 month were available (n=87), standardized CGM metrics were summarized.
Results
Linear regression analyses identified CGM use as a determining factor for log-transformed glycosylated hemoglobin. The fully-adjusted odds ratio (OR) and 95% confidence interval (CI) for uncontrolled glycosylated hemoglobin (>8%) were 0.365 (95% CI, 0.190 to 0.703) in CGM users compared to never-users. The fully-adjusted OR for controlled glycosylated hemoglobin (<7%) was 1.861 (95% CI, 1.119 to 3.096) in CGM users compared to never-users. Among individuals who had been using official applications for CGM, time in range (TIR) values within recent 30- and 90-day periods were 62.45%±16.63% and 63.08%±15.32%, respectively.
Conclusion
CGM use was associated with glycemic control status among Korean adults with T1DM in the real-world, although CGM metrics including TIR might require further improvement among CGM users. -
Citations
Citations to this article as recorded by- Real-World Continuous Glucose Monitoring Data from a Population with Type 1 Diabetes in South Korea: Nationwide Single-System Analysis
Ji Yoon Kim, Sang-Man Jin, Sarah Andrade, Boyang Chen, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2024;[Epub] CrossRef - Accuracy and Safety of the 15-Day CareSens Air Continuous Glucose Monitoring System
Kyung-Soo Kim, Seung-Hwan Lee, Won Sang Yoo, Cheol-Young Park
Diabetes Technology & Therapeutics.2024; 26(4): 222. CrossRef - Navigating the Seas of Glycemic Control: The Role of Continuous Glucose Monitoring in Type 1 Diabetes Mellitus
Jun Sung Moon
Diabetes & Metabolism Journal.2023; 47(3): 345. CrossRef - Smart Insulin Pen: Managing Insulin Therapy for People with Diabetes in the Digital Era
Jee Hee Yoo, Jae Hyeon Kim
The Journal of Korean Diabetes.2023; 24(4): 190. CrossRef
- Real-World Continuous Glucose Monitoring Data from a Population with Type 1 Diabetes in South Korea: Nationwide Single-System Analysis
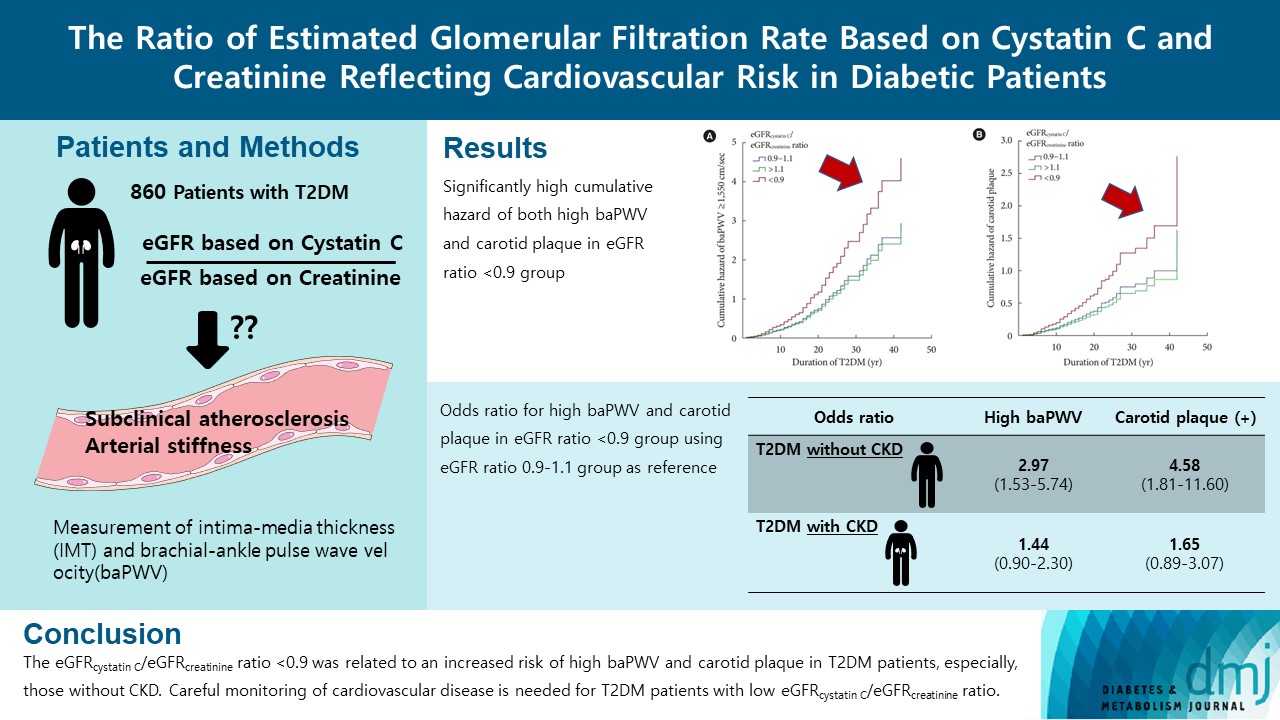
- Cardiovascular Risk/Epidemiology
- The Ratio of Estimated Glomerular Filtration Rate Based on Cystatin C and Creatinine Reflecting Cardiovascular Risk in Diabetic Patients
- Ah Reum Khang, Min Jin Lee, Dongwon Yi, Yang Ho Kang
- Diabetes Metab J. 2023;47(3):415-425. Published online March 6, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0177
- 1,823 View
- 112 Download
- 2 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The ratio of estimated glomerular filtration rate (eGFR) based on cystatin C and creatinine (eGFRcystatin C/eGFRcreatinine ratio) is related to accumulating atherosclerosis-promoting proteins and increased mortality in several cohorts.
Methods
We assessed whether the eGFRcystatin C/eGFRcreatinine ratio is a predictor of arterial stiffness and sub-clinical atherosclerosis in type 2 diabetes mellitus (T2DM) patients, who were followed up during 2008 to 2016. GFR was estimated using an equation based on cystatin C and creatinine.
Results
A total of 860 patients were stratified according to their eGFRcystatin C/eGFRcreatinine ratio (i.e., <0.9, 0.9–1.1 [a reference group], and >1.1). Intima-media thickness was comparable among the groups; however, presence of carotid plaque was frequent in the <0.9 group (<0.9 group, 38.3%; 0.9–1.1 group, 21.6% vs. >1.1 group, 17.2%, P<0.001). Brachial-ankle pulse wave velocity (baPWV) was faster in the <0.9 group (<0.9 group, 1,656.3±333.0 cm/sec; 0.9–1.1 group, 1,550.5±294.8 cm/sec vs. >1.1 group, 1,494.0±252.2 cm/sec, P<0.001). On comparing the <0.9 group with the 0.9–1.1 group, the multivariate-adjusted odds ratios of prevalence of high baPWV and carotid plaque were 2.54 (P=0.007) and 1.95 (P=0.042), respectively. Cox regression analysis demonstrated near or over 3-fold higher risks of the prevalence of high baPWV and carotid plaque in the <0.9 group without chronic kidney disease (CKD).
Conclusion
We concluded that eGFRcystatin C/eGFRcreatinine ratio <0.9 was related to an increased risk of high baPWV and carotid plaque in T2DM patients, especially, those without CKD. Careful monitoring of cardiovascular disease is needed for T2DM patients with low eGFRcystatin C/eGFRcreatinine ratio. -
Citations
Citations to this article as recorded by- Research Progress of Creatinine, Cystatin C, and Their Ratio in Renal Diseases
广智 杨
Advances in Clinical Medicine.2024; 14(04): 976. CrossRef - Muscle mass, creatinine, cystatin C and selective glomerular hypofiltration syndromes
Linnea Malmgren, Anders Grubb
Clinical Kidney Journal.2023; 16(8): 1206. CrossRef - Investigating kidney function changes in young adults with COVID-19: Serum creatinine level, glomerular filtration rate, and biochemical profile analysis
Nikita Matyushin, Dmitriy Ermakov, Inna Vasileva, Roza Vakolyuk, Anastasiya Spaska
Electronic Journal of General Medicine.2023; 20(6): em547. CrossRef - Intraindividual difference in estimated GFR by creatinine and cystatin C, cognitive trajectories and motoric cognitive risk syndrome
Jinqi Wang, Yueruijing Liu, Rui Jin, Xiaoyu Zhao, Zhiyuan Wu, Ze Han, Zongkai Xu, Xiuhua Guo, Lixin Tao
Nephrology Dialysis Transplantation.2023;[Epub] CrossRef
- Research Progress of Creatinine, Cystatin C, and Their Ratio in Renal Diseases
- Metabolic Risk/Epidemiology
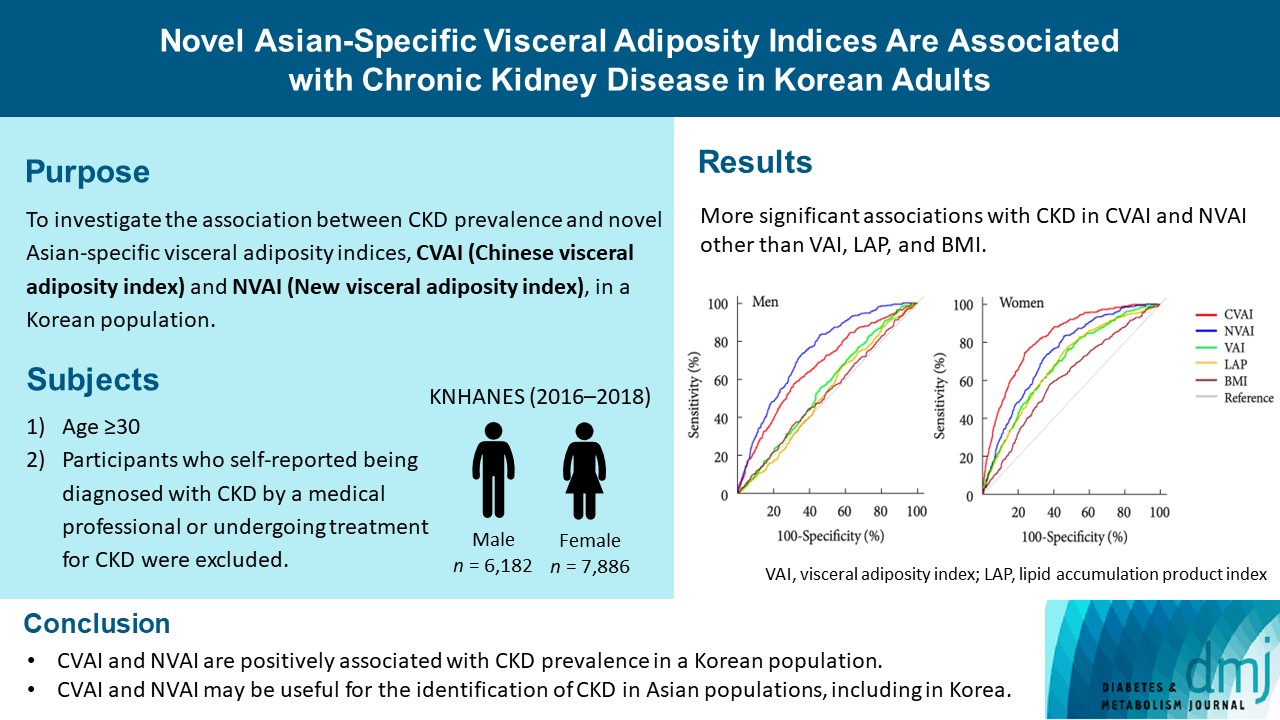
- Novel Asian-Specific Visceral Adiposity Indices Are Associated with Chronic Kidney Disease in Korean Adults
- Jonghwa Jin, Hyein Woo, Youngeun Jang, Won-Ki Lee, Jung-Guk Kim, In-Kyu Lee, Keun-Gyu Park, Yeon-Kyung Choi
- Diabetes Metab J. 2023;47(3):426-436. Published online March 6, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0099
- 2,472 View
- 128 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The Chinese visceral adiposity index (CVAI) and new visceral adiposity index (NVAI) are novel indices of visceral adiposity used to predict metabolic and cardiovascular diseases in Asian populations. However, the relationships of CVAI and NVAI with chronic kidney disease (CKD) have not been investigated. We aimed to characterize the relationships of CVAI and NVAI with the prevalence of CKD in Korean adults.
Methods
A total of 14,068 participants in the 7th Korea National Health and Nutrition Examination Survey (6,182 men and 7,886 women) were included. Receiver operating characteristic (ROC) analyses were employed to compare the associations between indices of adiposity and CKD, and a logistic regression model was used to characterize the relationships of CVAI and NVAI with CKD prevalence.
Results
The areas under the ROC curves for CVAI and NVAI were significantly larger than for the other indices, including the visceral adiposity index and lipid accumulation product, in both men and women (all P<0.001). In addition, high CVAI or NVAI was significantly associated with a high CKD prevalence in both men (odds ratio [OR], 2.14; 95% confidence interval [CI], 1.31 to 3.48 in CVAI and OR, 6.47; 95% CI, 2.91 to 14.38 in NVAI, P<0.05) and women (OR, 4.87; 95% CI, 1.85 to 12.79 in CVAI and OR, 3.03; 95% CI, 1.35 to 6.82 in NVAI, P<0.05); this association remained significant after adjustment for multiple confounding factors in men and women.
Conclusion
CVAI and NVAI are positively associated with CKD prevalence in a Korean population. CVAI and NVAI may be useful for the identification of CKD in Asian populations, including in Korea. -
Citations
Citations to this article as recorded by- Association between Chinese visceral adiposity index and risk of stroke incidence in middle-aged and elderly Chinese population: evidence from a large national cohort study
Zenglei Zhang, Lin Zhao, Yiting Lu, Xu Meng, Xianliang Zhou
Journal of Translational Medicine.2023;[Epub] CrossRef
- Association between Chinese visceral adiposity index and risk of stroke incidence in middle-aged and elderly Chinese population: evidence from a large national cohort study
Letter
- Association of Body Mass Index and Fracture Risk Varied by Affected Bones in Patients with Diabetes: A Nationwide Cohort Study (Diabetes Metab J 2023;47:242-54)
- So Young Park
- Diabetes Metab J. 2023;47(3):437-438. Published online May 26, 2023
- DOI: https://doi.org/10.4093/dmj.2023.0100
- [Original]
- 1,039 View
- 60 Download
Response
- Association of Body Mass Index and Fracture Risk Varied by Affected Bones in Patients with Diabetes: A Nationwide Cohort Study (Diabetes Metab J 2023;47:242-54)
- Se-Won Lee, Kyungdo Han, Hyuk-Sang Kwon
- Diabetes Metab J. 2023;47(3):439-440. Published online May 26, 2023
- DOI: https://doi.org/10.4093/dmj.2023.0104
- [Original]
- 1,207 View
- 57 Download

 KDA
KDA


 First
First Prev
Prev





