
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Complications
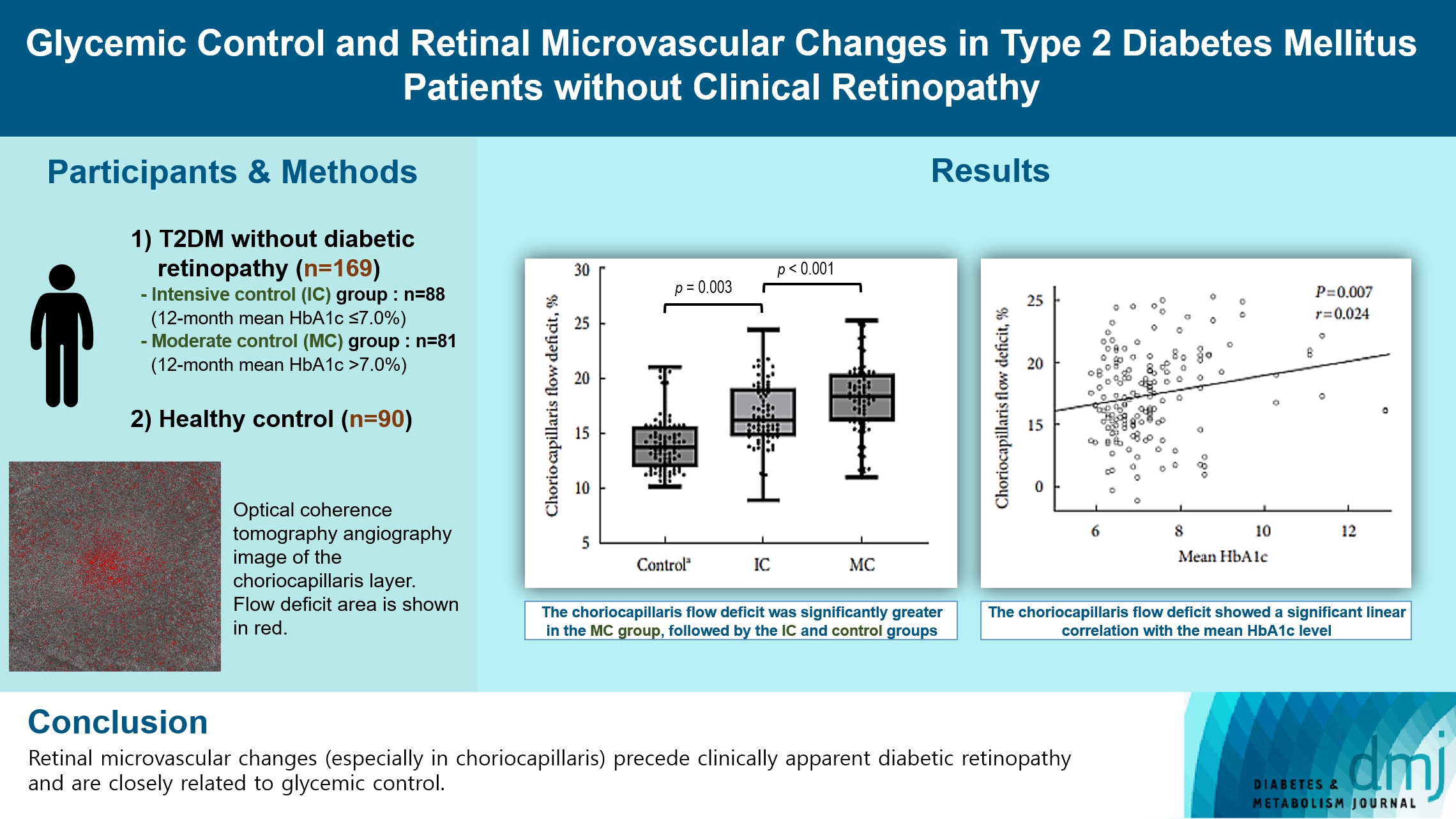
- Glycemic Control and Retinal Microvascular Changes in Type 2 Diabetes Mellitus Patients without Clinical Retinopathy
- Kangmin Lee, Ga Hye Lee, Seung Eun Lee, Jee Myung Yang, Kunho Bae
- Received May 15, 2023 Accepted December 15, 2023 Published online March 13, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0149 [Epub ahead of print]
- 625 View
- 33 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To investigate the association of glycemic control and retinal microvascular changes in patients with type 2 diabetes mellitus (T2DM) without diabetic retinopathy (DR).
Methods
This retrospective, observational, cohort study included patients with T2DM without DR. The patients were categorized into intensive control (IC; mean glycosylated hemoglobin [HbA1c] ≤7.0%) and moderate control (MC; mean HbA1c >7.0%) groups. Optical coherence tomography (OCT) and swept-source OCT angiography (OCTA) image parameters were compared between three groups, including healthy controls.
Results
In total, 259 eyes of 259 participants (88 IC, 81 MC, and 90 controls) were included. The foveal avascular zone area was significantly larger in the MC group than IC and control groups (all P<0.05). The IC group had lower vessel density in the superficial retinal layer and deep retinal layer than the controls (all P<0.05). The choriocapillaris (CC) flow deficit (FD) was significantly greater in the MC group than in the IC and control groups (18.2%, 16.7%, and 14.2%, respectively; all P<0.01). In multivariate regression analysis, CC-FD was associated with the mean HbA1c level (P=0.008). There were no significant differences in OCT parameters among the groups.
Conclusion
OCTA revealed that early CC impairment is associated with HbA1c levels; the CC changes precede clinically apparent DR. The OCTA parameters differed among the groups according to the degree of glycemic control. Our results suggest that microvascular changes precede DR and are closely related to glycemic control.
- Drug/Regimen
- Efficacy and Safety of IDegAsp in a Real-World Korean Population with Type 2 Diabetes Mellitus
- Shinae Kang, Yu-Bae Ahn, Tae Keun Oh, Won-Young Lee, Sung Wan Chun, Boram Bae, Amine Dahaoui, Jin Sook Jeong, Sungeun Jung, Hak Chul Jang
- Received August 24, 2023 Accepted November 22, 2023 Published online February 27, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0297 [Epub ahead of print]

- 649 View
- 42 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study investigated the real-world efficacy and safety of insulin degludec/insulin aspart (IDegAsp) in Korean adults with type 2 diabetes mellitus (T2DM), whose insulin treatment was switched to IDegAsp.
Methods
This was a multicenter, retrospective, observational study comprising two 26-week treatment periods, before and after switching to IDegAsp, respectively. Korean adults with uncontrolled T2DM treated with basal or premix insulin (±oral antidiabetic drugs) were enrolled. The primary objective was to compare the degree of glycosylated hemoglobin (HbA1c) change in each 26-week observation period. The analyses included changes in HbA1c, fasting plasma glucose (FPG), body weight, proportion of participants achieving HbA1c <7.0%, hypoglycemic events, and total daily insulin dose (ClinicalTrials.gov, number NCT04656106).
Results
In total, 196 adults (mean age, 65.95 years; mean T2DM duration, 18.99 years) were analyzed. The change in both HbA1c and FPG were significantly different between the pre-switching and the post-switching period (0.28% vs. –0.51%, P<0.001; 5.21 mg/dL vs. –23.10 mg/dL, P=0.005), respectively. After switching, the rate of achieving HbA1c <7.0% was significantly improved (5.10% at baseline vs. 11.22% with IDegAsp, P=0.012). No significant differences (before vs. after switching) were observed in body weight change, and total daily insulin dose. The rates of overall and severe hypoglycemia were similar in the two periods.
Conclusion
In real-world clinical practice in Korea, the change of insulin regimen to IDegAsp was associated with an improvement in glycemic control without increase of hypoglycemia, supporting the use of IDegAsp for patients with T2DM uncontrolled with basal or premix insulin.
- Metabolic Risk/Epidemiology
- Glycemic Control Is Associated with Histological Findings of Nonalcoholic Fatty Liver Disease
- Teruki Miyake, Shinya Furukawa, Bunzo Matsuura, Osamu Yoshida, Masumi Miyazaki, Akihito Shiomi, Ayumi Kanamoto, Hironobu Nakaguchi, Yoshiko Nakamura, Yusuke Imai, Mitsuhito Koizumi, Takao Watanabe, Yasunori Yamamoto, Yohei Koizumi, Yoshio Tokumoto, Masashi Hirooka, Teru Kumagi, Eiji Takesita, Yoshio Ikeda, Masanori Abe, Yoichi Hiasa
- Received June 24, 2023 Accepted September 21, 2023 Published online February 2, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0200 [Epub ahead of print]

- 926 View
- 40 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Poor lifestyle habits may worsen nonalcoholic fatty liver disease (NAFLD), with progression to nonalcoholic steatohepatitis (NASH) and cirrhosis. This study investigated the association between glycemic control status and hepatic histological findings to elucidate the effect of glycemic control on NAFLD.
Methods
This observational study included 331 patients diagnosed with NAFLD by liver biopsy. Effects of the glycemic control status on histological findings of NAFLD were evaluated by comparing the following four glycemic status groups defined by the glycosylated hemoglobin (HbA1c) level at the time of NAFLD diagnosis: ≤5.4%, 5.5%–6.4%, 6.5%–7.4%, and ≥7.5%.
Results
Compared with the lowest HbA1c group (≤5.4%), the higher HbA1c groups (5.5%–6.4%, 6.5%–7.4%, and ≥7.5%) were associated with advanced liver fibrosis and high NAFLD activity score (NAS). On multivariate analysis, an HbA1c level of 6.5%– 7.4% group was significantly associated with advanced fibrosis compared with the lowest HbA1c group after adjusting for age, sex, hemoglobin, alanine aminotransferase, and creatinine levels. When further controlling for body mass index and uric acid, total cholesterol, and triglyceride levels, the higher HbA1c groups were significantly associated with advanced fibrosis compared with the lowest HbA1c group. On the other hand, compared with the lowest HbA1c group, the higher HbA1c groups were also associated with a high NAS in both multivariate analyses.
Conclusion
Glycemic control is associated with NAFLD exacerbation, with even a mild deterioration in glycemic control, especially a HbA1c level of 6.5%–7.4%, contributing to NAFLD progression.
- Cardiovascular Risk/Epidemiology
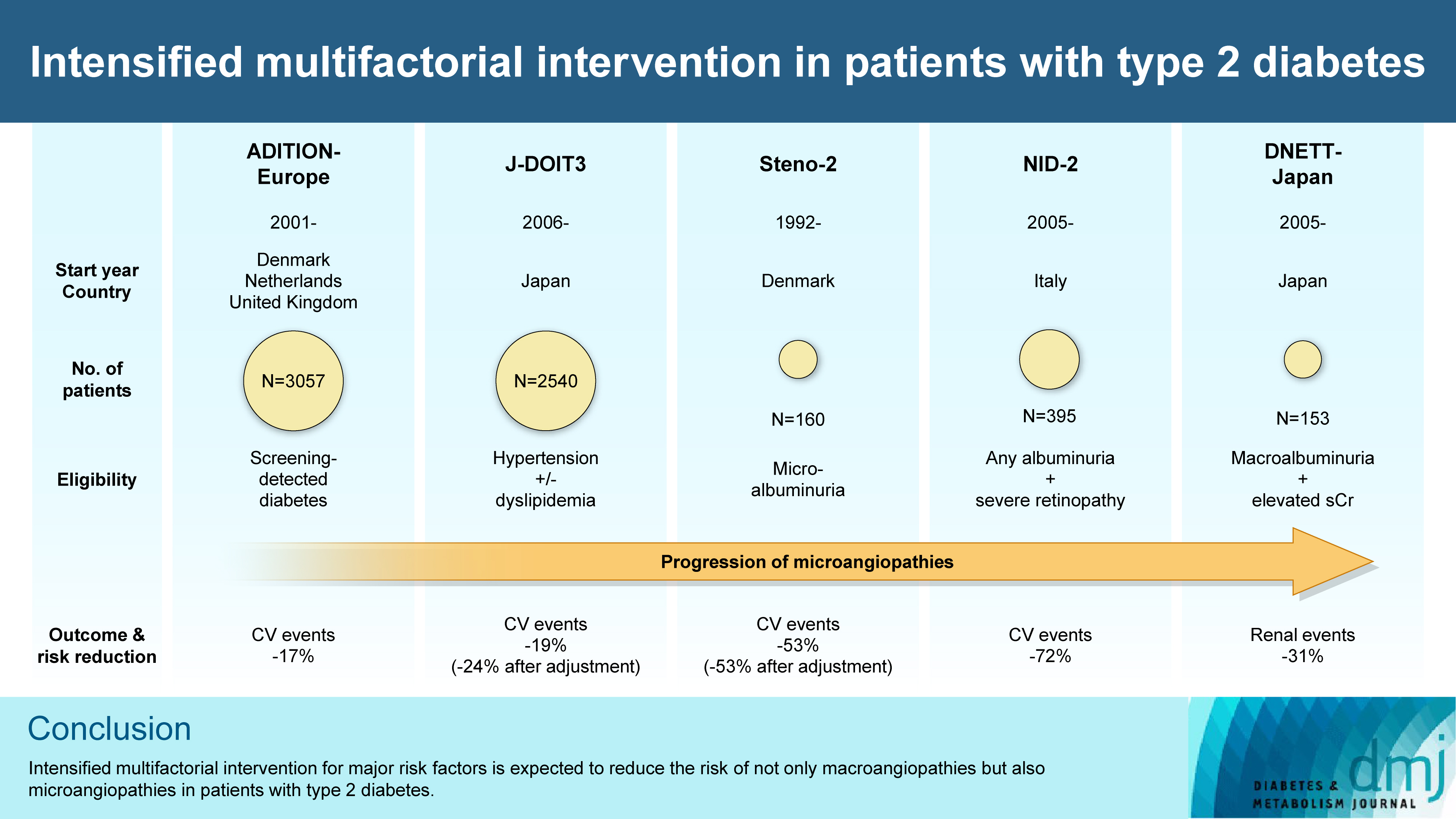
- Intensified Multifactorial Intervention in Patients with Type 2 Diabetes Mellitus
- Takayoshi Sasako, Toshimasa Yamauchi, Kohjiro Ueki
- Diabetes Metab J. 2023;47(2):185-197. Published online January 12, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0325
- 5,089 View
- 358 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - In the management of diabetes mellitus, one of the most important goals is to prevent its micro- and macrovascular complications, and to that end, multifactorial intervention is widely recommended. Intensified multifactorial intervention with pharmacotherapy for associated risk factors, alongside lifestyle modification, was first shown to be efficacious in patients with microalbuminuria (Steno-2 study), then in those with less advanced microvascular complications (the Anglo-Danish-Dutch Study of Intensive Treatment In People with Screen Detected Diabetes in Primary Care [ADDITION]-Europe and the Japan Diabetes Optimal Treatment study for 3 major risk factors of cardiovascular diseases [J-DOIT3]), and in those with advanced microvascular complications (the Nephropathy In Diabetes-Type 2 [NID-2] study and Diabetic Nephropathy Remission and Regression Team Trial in Japan [DNETT-Japan]). Thus far, multifactorial intervention led to a reduction in cardiovascular and renal events, albeit not necessarily significant. It should be noted that not only baseline characteristics but also the control status of the risk factors and event rates during intervention among the patients widely varied from one trial to the next. Further evidence is needed for the efficacy of multifactorial intervention in a longer duration and in younger or elderly patients. Moreover, now that new classes of antidiabetic drugs are available, it should be addressed whether strict and safe glycemic control, alongside control of other risk factors, could lead to further risk reductions in micro- and macrovascular complications, thereby decreasing all-cause mortality in patients with type 2 diabetes mellitus.
-
Citations
Citations to this article as recorded by- Exploring mechanisms underlying diabetes comorbidities and strategies to prevent vascular complications
Takayoshi Sasako
Diabetology International.2024; 15(1): 34. CrossRef - Targeting ERS-mitophagy in hippocampal neurons to explore the improvement of memory by tea polyphenols in aged type 2 diabetic rats
Wenjuan Feng, Chenhui Lv, Le Cheng, Xin Song, Xuemin Li, Haoran Xie, Shuangzhi Chen, Xi Wang, Lushan Xue, Cheng Zhang, Jie Kou, Lili Wang, Haifeng Zhao
Free Radical Biology and Medicine.2024; 213: 293. CrossRef - Risk of Dementia Among Patients With Diabetes in a Multidisciplinary, Primary Care Management Program
Kailu Wang, Shi Zhao, Eric Kam-Pui Lee, Susan Zi-May Yau, Yushan Wu, Chi-Tim Hung, Eng-Kiong Yeoh
JAMA Network Open.2024; 7(2): e2355733. CrossRef - Causes of In-Hospital Death and Pharmaceutical Associations with Age of Death during a 10-Year Period (2011–2020) in Individuals with and without Diabetes at a Japanese Community General Hospital
Minae Hosoki, Taiki Hori, Yousuke Kaneko, Kensuke Mori, Saya Yasui, Seijiro Tsuji, Hiroki Yamagami, Saki Kawata, Tomoyo Hara, Shiho Masuda, Yukari Mitsui, Kiyoe Kurahashi, Takeshi Harada, Shingen Nakamura, Toshiki Otoda, Tomoyuki Yuasa, Akio Kuroda, Itsur
Journal of Clinical Medicine.2024; 13(5): 1283. CrossRef - External validation of a minimal-resource model to predict reduced estimated glomerular filtration rate in people with type 2 diabetes without diagnosis of chronic kidney disease in Mexico: a comparison between country-level and regional performance
Camilla Sammut-Powell, Rose Sisk, Ruben Silva-Tinoco, Gustavo de la Pena, Paloma Almeda-Valdes, Sonia Citlali Juarez Comboni, Susana Goncalves, Rory Cameron
Frontiers in Endocrinology.2024;[Epub] CrossRef - Gut Microbiota Targeted Approach by Natural Products in Diabetes Management: An Overview
Priyanka Sati, Praveen Dhyani, Eshita Sharma, Dharam Chand Attri, Arvind Jantwal, Rajni Devi, Daniela Calina, Javad Sharifi-Rad
Current Nutrition Reports.2024;[Epub] CrossRef - Cardiovascular Risk Reduction in Type 2 Diabetes: Further Insights into the Power of Weight Loss and Exercise
Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(3): 302. CrossRef - Sarcopenia: Loss of mighty armor against frailty and aging
Takayoshi Sasako, Kohjiro Ueki
Journal of Diabetes Investigation.2023; 14(10): 1145. CrossRef
- Exploring mechanisms underlying diabetes comorbidities and strategies to prevent vascular complications
- Guideline/Fact Sheet
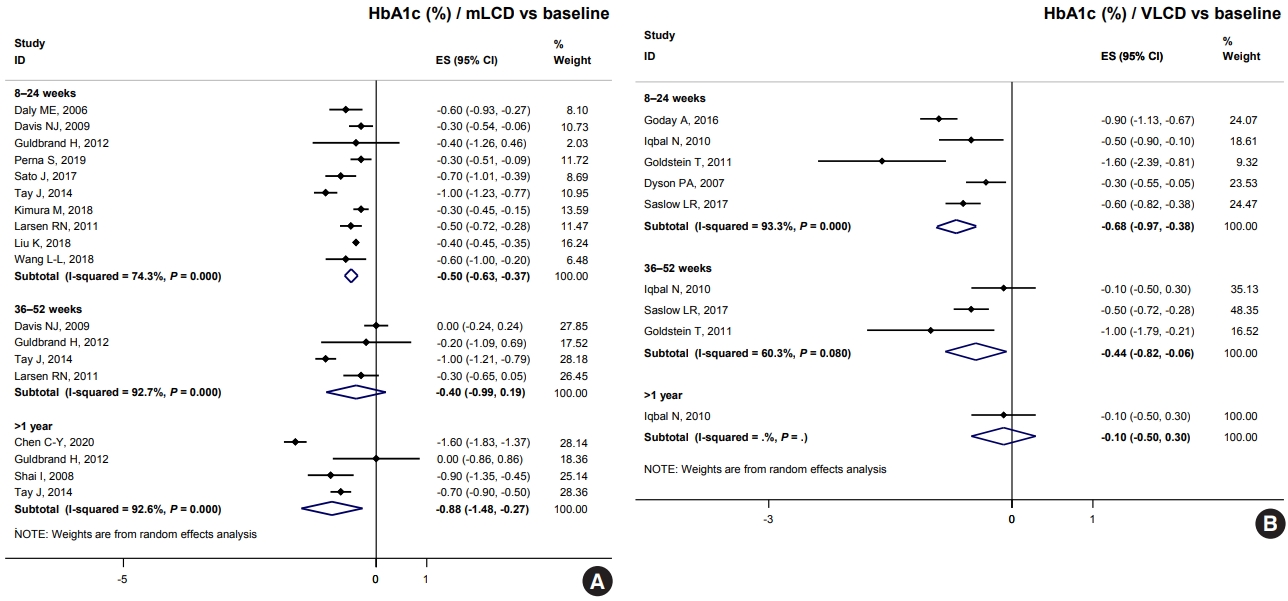
- Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hypertension
- Jong Han Choi, Jee-Hyun Kang, Suk Chon
- Diabetes Metab J. 2022;46(3):377-390. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0051
- 4,954 View
- 249 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The Joint Committee of the Korean Diabetes Association, the Korean Society for the Study of Obesity, and the Korean Society of Hypertension announced a consensus statement on carbohydrate-restricted diets and intermittent fasting, representing an emerging and popular dietary pattern. In this statement, we recommend moderately-low-carbohydrate or low-carbohydrate diets, not a very-low-carbohydrate diet, for patients with type 2 diabetes mellitus. These diets can be considered a dietary regimen to improve glycemic control and reduce body weight in adults with type 2 diabetes mellitus. This review provides the detailed results of a meta-analysis and systematic literature review on the potential harms and benefits of carbohydrate-restricted diets in patients with diabetes. We expect that this review will help experts and patients by fostering an in-depth understanding and appropriate application of carbohydrate-restricted diets in the comprehensive management of diabetes.
-
Citations
Citations to this article as recorded by- Efficacy of convenience meal-type foods designed for diabetes in the management of metabolic syndrome based on a 3-week trial
Do Gyeong Lee, In Gyeong Kang, Tae Seok Kim, Yun Ahn, Sang Yun Lee, Hye Jin Ahn, Yoo Kyoung Park
Nutrition.2024; 118: 112287. CrossRef - Long-Term Results of a Digital Diabetes Self-Management and Education Support Program Among Adults With Type 2 Diabetes: A Retrospective Cohort Study
Ashley Berthoumieux, Sarah Linke, Melinda Merry, Alison Megliola, Jessie Juusola, Jenna Napoleone
The Science of Diabetes Self-Management and Care.2024; 50(1): 19. CrossRef - Medical nutrition therapy for diabetes mellitus
Suk Chon
Journal of the Korean Medical Association.2023; 66(7): 421. CrossRef
- Efficacy of convenience meal-type foods designed for diabetes in the management of metabolic syndrome based on a 3-week trial
- Drug/Regimen
- Comparison of Efficacy of Glimepiride, Alogliptin, and Alogliptin-Pioglitazone as the Initial Periods of Therapy in Patients with Poorly Controlled Type 2 Diabetes Mellitus: An Open-Label, Multicenter, Randomized, Controlled Study
- Hae Jin Kim, In Kyung Jeong, Kyu Yeon Hur, Soo-Kyung Kim, Jung Hyun Noh, Sung Wan Chun, Eun Seok Kang, Eun-Jung Rhee, Sung Hee Choi
- Diabetes Metab J. 2022;46(5):689-700. Published online March 17, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0183
- 5,662 View
- 377 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The choice of an optimal oral hypoglycemic agent in the initial treatment periods for type 2 diabetes mellitus (T2DM) patients remains difficult and deliberate. We compared the efficacy and safety of glimepiride (GLIM), alogliptin (ALO), and alogliptin-pioglitazone (ALO-PIO) in poorly controlled T2DM patients with drug-naïve or metformin failure.
Methods
In this three-arm, multicenter, open-label, randomized, controlled trial, poorly controlled T2DM patients were randomized to receive GLIM (n=35), ALO (n=31), or ALO-PIO (n=33) therapy for 24 weeks. The primary endpoint was change in the mean glycosylated hemoglobin (HbA1c) levels at week 24 from baseline. Secondary endpoints were changes in HbA1c level at week 12 from baseline, fasting plasma glucose (FPG) levels, lipid profiles at weeks 12 and 24, and parameters of glycemic variability, assessed by continuous glucose monitoring for 24 weeks.
Results
At weeks 12 and 24, the ALO-PIO group showed significant reduction in HbA1c levels compared to the ALO group (–0.96%±0.17% vs. –0.37%±0.17% at week 12; –1.13%±0.19% vs. –0.18%±0.2% at week 24). The ALO-PIO therapy caused greater reduction in FPG levels and significant increase in high-density lipoprotein cholesterol levels at weeks 12 and 24 than the ALO therapy. Compared to low-dose GLIM therapy, ALO-PIO therapy showed greater improvement in glycemic variability. The adverse events were similar among the three arms.
Conclusion
ALO-PIO combination therapy during the early period exerts better glycemic control than ALO monotherapy and excellency in glycemic variability than low-dose sulfonylurea therapy in uncontrolled, drug-naïve or metformin failed T2DM patients. -
Citations
Citations to this article as recorded by- A Comprehensive Review on Weight Loss Associated with Anti-Diabetic Medications
Fatma Haddad, Ghadeer Dokmak, Maryam Bader, Rafik Karaman
Life.2023; 13(4): 1012. CrossRef - Role of Dipeptidyl Peptidase 4 Inhibitors in Antidiabetic Treatment
Ruili Yin, Yongsong Xu, Xin Wang, Longyan Yang, Dong Zhao
Molecules.2022; 27(10): 3055. CrossRef
- A Comprehensive Review on Weight Loss Associated with Anti-Diabetic Medications
- Metabolic Risk/Epidemiology
- Sex Differences in the Effects of CDKAL1 Variants on Glycemic Control in Diabetic Patients: Findings from the Korean Genome and Epidemiology Study
- Hye Ah Lee, Hyesook Park, Young Sun Hong
- Diabetes Metab J. 2022;46(6):879-889. Published online February 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0265
- 65,535 View
- 178 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Using long-term data from the Korean Genome and Epidemiology Study, we defined poor glycemic control and investigated possible risk factors, including variants related to type 2 diabetes mellitus (T2DM). In addition, we evaluated interaction effects among risk factors for poor glycemic control.
Methods
Among 436 subjects with newly diagnosed diabetes, poor glycemic control was defined based on glycosylated hemoglobin trajectory patterns by group-based trajectory modeling. For the variants related to T2DM, genetic risk scores (GRSs) were calculated and divided into quartiles. Risk factors for poor glycemic control were assessed using a logistic regression model.
Results
Of the subjects, 43% were in the poor-glycemic-control group. Body mass index (BMI) and triglyceride (TG) were associated with poor glycemic control. The risk for poor glycemic control increased by 11.0% per 1 kg/m2 increase in BMI and by 3.0% per 10 mg/dL increase in TG. The risk for GRS with poor glycemic control was sex-dependent (Pinteraction=0.07), and a relationship by GRS quartiles was found in females but not in males. Moreover, the interaction effect was found to be significant on both additive and multiplicative scales. The interaction effect was evident in the variants of cyclin-dependent kinase 5 regulatory subunit-associated protein 1-like (CDKAL1).
Conclusion
Females with risk alleles of variants in CDKAL1 associated with T2DM had a higher risk for poor glycemic control than males. -
Citations
Citations to this article as recorded by- Hepatic Cdkal1 deletion regulates HDL catabolism and promotes reverse cholesterol transport
Dan Bi An, Soo-jin Ann, Seungmin Seok, Yura Kang, Sang-Hak Lee
Atherosclerosis.2023; 375: 21. CrossRef
- Hepatic Cdkal1 deletion regulates HDL catabolism and promotes reverse cholesterol transport
- Drug/Regimen
- Comparison of Prevailing Insulin Regimens at Different Time Periods in Hospitalized Patients: A Real-World Experience from a Tertiary Hospital
- Sun Joon Moon, Hun Jee Choe, Soo Heon Kwak, Hye Seung Jung, Kyong Soo Park, Young Min Cho
- Diabetes Metab J. 2022;46(3):439-450. Published online October 20, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0065

- 65,535 View
- 268 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Prevailing insulin regimens for glycemic control in hospitalized patients have changed over time. We aimed to determine whether the current basal-bolus insulin (BBI) regimen is superior to the previous insulin regimen, mainly comprising split-mixed insulin therapy.
Methods
This was a single tertiary center, retrospective observational study that included non-critically ill patients with type 2 diabetes mellitus who were treated with split-mixed insulin regimens from 2004 to 2007 (period 1) and with BBI from 2008 to 2018 (period 2). Patients from each period were analyzed after propensity score matching. The mean difference in glucose levels and the achievement of fasting and preprandial glycemic targets by day 6 of admission were assessed. The total daily insulin dose, incidence of hypoglycemia, and length of hospital stay were also evaluated.
Results
Among 244 patients from each period, both fasting glucose (estimated mean±standard error, 147.4±3.1 mg/dL vs. 129.4±3.2 mg/dL, P<0.001, day 6) and preprandial glucose (177.7±2.8 mg/dL vs. 152.8±2.8 mg/dL, P<0.001, day 6) were lower in period 2 than in period 1. By day 6 of hospital admission, 42.6% and 67.2% of patients achieved a preprandial glycemic target of <140 mg/dL in periods 1 and 2, respectively (relative risk, 2.00; 95% confidence interval, 1.54 to 2.59), without an increased incidence of hypoglycemia. Length of stay was shorter in period 2 (10.23±0.26 days vs. 8.70±0.26 days, P<0.001).
Conclusion
BBI improved glycemic control in a more efficacious manner than a split-mixed insulin regimen without increasing the risk of hypoglycemia in a hospital setting.
- Type 1 Diabetes
- Real-World Analysis of Therapeutic Outcome in Type 1 Diabetes Mellitus at a Tertiary Care Center
- Antonia Kietaibl, Michaela Riedl, Latife Bozkurt
- Diabetes Metab J. 2022;46(1):149-153. Published online July 6, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0267

- 4,357 View
- 144 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Insulin replacement in type 1 diabetes mellitus (T1DM) needs intensified treatment, which can either be performed by multiple daily injections (MDI) or continuous subcutaneous insulin infusion (CSII). This retrospective analysis of a real-world scenario aimed to evaluate whether glycaemic and cardiovascular risk factors could be controlled with CSII outclass MDI as suggested by recent evidence. Data from patients with either insulin pump (n=68) or injection (n=224) therapy at an Austrian tertiary care centre were analysed between January 2016 and December 2017. There were no significant differences with regard to the latest glycosylated hemoglobin, cardiovascular risk factor control or diabetes-associated late complications. Hypoglycaemia was less frequent (P<0.001), sensor-augmented therapy was more common (P=0.003) and mean body mass index (BMI) was higher (P=0.002) with CSII treatment. This retrospective analysis of real-world data in T1DM did not demonstrate the superiority of insulin pump treatment with regard to glycaemic control or cardiovascular risk factor control.
- Type 1 Diabetes
- Non-Insulin Antidiabetes Treatment in Type 1 Diabetes Mellitus: A Systematic Review and Meta-Analysis
- Xiaoling Cai, Chu Lin, Wenjia Yang, Lin Nie, Linong Ji
- Diabetes Metab J. 2021;45(3):312-325. Published online March 15, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0171

- 6,241 View
- 272 Download
- 5 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- In order to evaluate the efficacy and side effects of the non-insulin antidiabetes medications as an adjunct treatment in type 1 diabetes mellitus (T1DM), we conducted systematic searches in MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials for randomized controlled trials published between the date of inception and March 2020 to produce a systematic review and meta-analysis. Overall, 57 studies were included. Compared with placebo, antidiabetes agents in adjunct to insulin treatment resulted in significant reduction in glycosylated hemoglobin (weighted mean difference [WMD], –0.30%; 95% confidence interval [CI], –0.34 to –0.25%; P<0.01) and body weight (WMD, –2.15 kg; 95% CI, –2.77 to –1.53 kg; P<0.01), and required a significantly lower dosage of insulin (WMD, –5.17 unit/day; 95% CI, –6.77 to –3.57 unit/day; P<0.01). Compared with placebo, antidiabetes agents in adjunct to insulin treatment increased the risk of hypoglycemia (relative risk [RR], 1.04; 95% CI, 1.01 to 1.08; P=0.02) and gastrointestinal side effects (RR, 1.99; 95% CI, 1.61 to 2.46; P<0.01) in patients with T1DM. Compared with placebo, the use of non-insulin antidiabetes agents in addition to insulin could lead to glycemic improvement, weight control and lower insulin dosage, while they might be associated with increased risks of hypoglycemia and gastrointestinal side effects in patients with T1DM.
-
Citations
Citations to this article as recorded by- Dioscin: Therapeutic potential for diabetes and complications
Haoyang Gao, Ze Wang, Danlin Zhu, Linlin Zhao, Weihua Xiao
Biomedicine & Pharmacotherapy.2024; 170: 116051. CrossRef - The Impact of Body Mass Index, Residual Beta Cell Function and Estimated Glucose Disposal Rate on the Development of Double Diabetes and Microvascular Complications in Patients With Type 1 Diabetes Mellitus
Rameez Raja Bhagadurshah, Subbiah Eagappan, Raghavan Kasthuri Santharam, Sridhar Subbiah
Cureus.2023;[Epub] CrossRef - Prescribing patterns of adjunctive therapy for the treatment of type 1 diabetes mellitus among Australian endocrinologists
Patrice Forner, Jennifer Snaith, Jerry R. Greenfield
Internal Medicine Journal.2023;[Epub] CrossRef - Type 1 diabetes glycemic management: Insulin therapy, glucose monitoring, and automation
Bruce A. Perkins, Jennifer L. Sherr, Chantal Mathieu
Science.2021; 373(6554): 522. CrossRef - Current Advances of Artificial Pancreas Systems: A Comprehensive Review of the Clinical Evidence
Sun Joon Moon, Inha Jung, Cheol-Young Park
Diabetes & Metabolism Journal.2021; 45(6): 813. CrossRef
- Dioscin: Therapeutic potential for diabetes and complications
- Clinical Diabetes & Therapeutics
- The Effectiveness of Green Tea or Green Tea Extract on Insulin Resistance and Glycemic Control in Type 2 Diabetes Mellitus: A Meta-Analysis
- Jinyue Yu, Peige Song, Rachel Perry, Chris Penfold, Ashley R. Cooper
- Diabetes Metab J. 2017;41(4):251-262. Published online August 22, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.4.251
- 7,445 View
- 115 Download
- 47 Web of Science
- 51 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Green tea or green tea extract (GT/GTE) has been demonstrated to reduce insulin resistance and improve glycemic control. However, evidence for this health beneficial effect is inconsistent. This systematic review evaluated the effect of GT/GTE on insulin resistance and glycemic control in people with pre-diabetes/type 2 diabetes mellitus (T2DM). Ovid MEDLINE, Embase, AMED, Web of Science, and the Cochrane Library were searched up to April 2017 for randomised controlled trials of participants with pre-diabetes or T2DM, where the intervention was GT/GTE. Meta-analysis was performed to assess the standardised mean difference (SMD) in biomarkers of insulin resistance and glycemic control between GT/GTE and placebo groups. Six studies (
n =382) were pooled into random-effects meta-analysis. Overall, no differences were found between GT/GTE and the placebo for glycosylated hemoglobin (HbA1c: SMD, −0.32; 95% confidence interval [CI], −0.86 to 0.23), homeostatic model assessment for insulin resistance (HOMA-IR: SMD, 0.10; 95% CI, −0.17 to 0.38), fasting insulin (SMD, −0.25; 95% CI, −0.64 to 0.15), and fasting glucose (SMD, −0.10; 95% CI, −0.50 to 0.30). No evidence support the consumption of GT/GTE could reduce the levels of HbA1c, HOMA-IR, fasting insulin, or fasting glucose in people with pre-diabetes/T2DM. However, the studies included were small and of varying quality.-
Citations
Citations to this article as recorded by- Is breakfast consumption detrimental, unnecessary, or an opportunity for health promotion? A review of cardiometabolic outcomes and functional food choices
Heitor O. Santos, Grant M. Tinsley
Diabetes/Metabolism Research and Reviews.2024;[Epub] CrossRef - A comparison of the effects of green tea and cocoa on glycaemic control and insulin sensitivity in patients with type 2 diabetes mellitus: a systematic review and meta-analysis
Hind Mesfer S. Alkhudaydi, Jeremy P.E. Spencer
Nutrition and Healthy Aging.2024; 9(1): 17. CrossRef - Association between green tea intake and digestive system cancer risk in European and East Asian populations: a Mendelian randomization study
Duorui Nie, Xiaoyu He, Hao Zheng, Deyu Deng, Fanghui He, Ruyi Li, Xiaoting Ni, Shunxiang Li, Fei Xu
European Journal of Nutrition.2024;[Epub] CrossRef - From Gut to Glucose: A Comprehensive Review on Functional Foods and
Dietary Interventions for Diabetes Management
Nirali Patel, Susha Dinesh, Sameer Sharma
Current Diabetes Reviews.2024;[Epub] CrossRef - Gut microbiota as a driver of the interindividual variability of cardiometabolic effects from tea polyphenols
Qiqiong Li, Tom Van de Wiele
Critical Reviews in Food Science and Nutrition.2023; 63(11): 1500. CrossRef - Recent insights on tea metabolites, their biosynthesis and chemo-preventing effects: A review
Ramkumar Samynathan, Muthu Thiruvengadam, Shivraj Hariram Nile, Mohammad Ali Shariati, Maksim Rebezov, Raghvendra Kumar Mishra, Baskar Venkidasamy, Sureshkumar Periyasamy, Ill-Min Chung, Mirian Pateiro, José M. Lorenzo
Critical Reviews in Food Science and Nutrition.2023; 63(18): 3130. CrossRef - Tea's anti‐obesity properties, cardiometabolic health‐promoting potentials, bioactive compounds, and adverse effects: A review focusing on white and green teas
Behnaz Abiri, Shirin Amini, Mahdi Hejazi, Farhad Hosseinpanah, Afshin Zarghi, Faeze Abbaspour, Majid Valizadeh
Food Science & Nutrition.2023; 11(10): 5818. CrossRef - An investigation into the potential action of polyphenols against human Islet Amyloid Polypeptide aggregation in type 2 diabetes
Anns Mahboob, Degiri Kalana Lasanga Senevirathne, Pradipta Paul, Faisal Nabi, Rizwan Hasan Khan, Ali Chaari
International Journal of Biological Macromolecules.2023; 225: 318. CrossRef - Association between green tea consumption and metabolic syndrome among Korean adults: results from the Health Examinees study
Hyeonjin Cho, Sunwoo Han, Jiwon Jeong, Hyein Jung, Sangah Shin
Journal of Nutrition and Health.2023; 56(1): 70. CrossRef - Relevance of Indian traditional tisanes in the management of type 2 diabetes mellitus: A review
Devi Datt Joshi, Lokesh Deb, Bharat G. Somkuwar, Virendra Singh Rana
Saudi Pharmaceutical Journal.2023; 31(5): 626. CrossRef - Evaluation the Effect of Chronic Obestatin Therapy on the Serum Glucose, Insulin And Lipid Levels in Type 2 Diabetic Rats
Safa Al-Halbouni, Shadi Homsi, Nabil koshji
The Open Public Health Journal.2023;[Epub] CrossRef - Supplementation with a New Standardized Extract of Green and Black Tea Exerts Antiadipogenic Effects and Prevents Insulin Resistance in Mice with Metabolic Syndrome
Mario De la Fuente-Muñoz, María De la Fuente-Fernández, Marta Román-Carmena, Sara Amor, María C. Iglesias-de la Cruz, Guillermo García-Laínez, Silvia Llopis, Patricia Martorell, David Verdú, Eva Serna, Ángel L. García-Villalón, Sonia I. Guilera, Antonio M
International Journal of Molecular Sciences.2023; 24(10): 8521. CrossRef - The effect of green tea supplementation on the anthropometric outcomes in overweight and obese women: a time and dose-response meta-analysis of randomized controlled trials
Yiyi Zhang, Nie Tang, Wei Xia, Shaikh Sanjid Seraj, Marcos Pereira, Periyannan Velu, Hui Zhou, Hanshu Yang, Guanggang Du
Critical Reviews in Food Science and Nutrition.2023; : 1. CrossRef - Ampelopsis grossedentata improves type 2 diabetes mellitus through modulating the gut microbiota and bile acid metabolism
Yu-li Hu, Mei Li, Lei Ding, Chuan Peng, You Wu, Wei Liu, Dan Zhao, Ling-ling Qin, Xiang-yu Guo, Li-li Wu, Tong-hua Liu
Journal of Functional Foods.2023; 107: 105622. CrossRef - Green Tea and Decaffeinated Light Roasted Green Coffee Extract Combination Improved Cardiac Insulin Resistance through Free Fatty Acids and Adiponectin/FAS Pathways Amelioration in Metabolic Syndrome Rat Model
Mifetika Lukitasari, Mohammad Saifur Rohman, Dwi Adi Nugroho, Mukhamad Nur Kholis, Nila Aisyah Wahyuni, Nashi Widodo
F1000Research.2023; 10: 990. CrossRef - Impact of Polyphenols on Inflammatory and Oxidative Stress Factors in Diabetes Mellitus: Nutritional Antioxidants and Their Application in Improving Antidiabetic Therapy
Michal Krawczyk, Izabela Burzynska-Pedziwiatr, Lucyna A. Wozniak, Malgorzata Bukowiecka-Matusiak
Biomolecules.2023; 13(9): 1402. CrossRef - Research progress on the antidiabetic activities of tea and its bioactive components
Jianjian Gao, Dan Chen, Zhiyuan Lin, Jiakun Peng, Shuai Yu, Chuang Zhou, Huimin Jiang, Ruofan Sun, Zhi Lin, Weidong Dai
Beverage Plant Research.2023;[Epub] CrossRef - Identifying Glucose Metabolism Status in Nondiabetic Japanese Adults Using Machine Learning Model with Simple Questionnaire
Tomoki Uchida, Takeshi Kanamori, Takanori Teramoto, Yuji Nonaka, Hiroki Tanaka, Satoshi Nakamura, Norihito Murayama, Rajesh Kaluri
Computational and Mathematical Methods in Medicine.2022; 2022: 1. CrossRef - Potential Bioactive Components and Health Promotional Benefits of Tea (Camellia sinensis)
Saptadip Samanta
Journal of the American Nutrition Association.2022; 41(1): 65. CrossRef - A Mendelian Randomization Study of the Effect of Tea Intake on Type 2 Diabetes
Yanan Zhang, Ruiqing Wang, Xinhua Tang, Yanjun Wang, Ping Guo, Shukang Wang, Jing Liu
Frontiers in Genetics.2022;[Epub] CrossRef - Dietary Supplements for Weight Management: A Narrative Review of Safety and Metabolic Health Benefits
Eunice Mah, Oliver Chen, DeAnn J. Liska, Jeffrey B. Blumberg
Nutrients.2022; 14(9): 1787. CrossRef - Antioxidative, Anti-Inflammatory, Anti-Obesogenic, and Antidiabetic Properties of Tea Polyphenols—The Positive Impact of Regular Tea Consumption as an Element of Prophylaxis and Pharmacotherapy Support in Endometrial Cancer
Piotr Olcha, Anna Winiarska-Mieczan, Małgorzata Kwiecień, Łukasz Nowakowski, Andrzej Miturski, Andrzej Semczuk, Bożena Kiczorowska, Krzysztof Gałczyński
International Journal of Molecular Sciences.2022; 23(12): 6703. CrossRef - Herbal tea, a novel adjuvant therapy for treating type 2 diabetes mellitus: A review
Xiangyuan Zhang, Lili Zhang, Boxun Zhang, Ke Liu, Jun Sun, Qingwei Li, Linhua Zhao
Frontiers in Pharmacology.2022;[Epub] CrossRef - Green tea and cancer and cardiometabolic diseases: a review of the current epidemiological evidence
Sarah Krull Abe, Manami Inoue
European Journal of Clinical Nutrition.2021; 75(6): 865. CrossRef - Green and white teas as health-promoting foods
Daniel Hinojosa-Nogueira, Sergio Pérez-Burillo, Silvia Pastoriza de la Cueva, José Ángel Rufián-Henares
Food & Function.2021; 12(9): 3799. CrossRef - A systematic review and meta-analysis of association between brain-derived neurotrophic factor and type 2 diabetes and glycemic profile
Milad Davarpanah, Nafiseh Shokri-mashhadi, Rahele Ziaei, Parvane Saneei
Scientific Reports.2021;[Epub] CrossRef - Maltodextrin encapsulation improves thermal and pH stability of green tea extract catechins
Aimara V. De La Cruz‐Molina, Jesus F. Ayala Zavala, Ariadna T. Bernal Mercado, Manuel R. Cruz Valenzuela, Gustavo A. González‐Aguilar, Jaime Lizardi‐Mendoza, Francisco Brown‐Bojorquez, Brenda A. Silva‐Espinoza
Journal of Food Processing and Preservation.2021;[Epub] CrossRef - Camellia sinensis in Dentistry: Technological Prospection and Scientific Evidence
Lídia Audrey Rocha Valadas, Rosueti Diógenes de Oliveira Filho, Edilson Martins Rodrigues Neto, Mary Anne Medeiros Bandeira, Marta Maria de França Fonteles, Vanara Florêncio Passos, Ana Cristina de Mello Fiallos, Mara Assef Leitao Lotif, Nara Juliana Cust
Evidence-Based Complementary and Alternative Medicine.2021; 2021: 1. CrossRef - A comprehensive insight into effects of green tea extract in polycystic ovary syndrome: a systematic review
Vahid Maleki, Ehsaneh Taheri, Parisa Varshosaz, Fatemeh Pourteymour Fard Tabrizi, Jalal Moludi, Hamed Jafari-Vayghan, Mahdi Shadnoush, Seyed Hossein Yahyazadeh Jabbari, Mehri Seifoleslami, Mohammad Alizadeh
Reproductive Biology and Endocrinology.2021;[Epub] CrossRef - Green Tea and Decaffeinated Light Roasted Green Coffee Extract Combination Improved Cardiac Insulin Resistance through Free Fatty Acids and Adiponectin/FAS Pathway Amelioration in Metabolic Syndrome Rat Model
Mifetika Lukitasari, Mohammad Saifur Rohman, Dwi Adi Nugroho, Mukhamad Nur Kholis, Nila Aisyah Wahyuni, Nashi Widodo
F1000Research.2021; 10: 990. CrossRef - Mechanisms Underlying the Antidiabetic Activities of Polyphenolic Compounds: A Review
Tina Nie, Garth J. S. Cooper
Frontiers in Pharmacology.2021;[Epub] CrossRef - Green tea and selenium-enriched green tea ameliorates non-alcoholic fatty liver disease through peripheral 5-hydroxytryptamine signals in high-fat diet-fed mice
Lin Zhang, Jia-Ying Xu, Ya-Fang Du, Zhang-Min Wang, Jian-Xiang Li, N. Ou-Yang, Yan Wang, Xue-Bin Yin, Li-Qiang Qin
International Food Research Journal.2021; 28(5): 996. CrossRef - Green Tea Consumption May Be Associated with Cardiovascular Disease Risk and Nonalcoholic Fatty Liver Disease in Type 2 Diabetics: A Cross-Sectional Study in Southeast China
Huan-Huan Yang, Hui Zhou, Wan-Zhan Zhu, Cai-Long Chen, Guo-Chong Chen, Lu-Gang Yu, Li-Qiang Qin
Journal of Medicinal Food.2020; 23(10): 1120. CrossRef - The effect of green coffee extract supplementation on lipid profile: A systematic review of clinical trial and in-vivo studies
Omid Nikpayam, Amir Hossein Faghfouri, Omid Mohammad Tavakoli-Rouzbehani, Seyyed-Mostafa Jalali, Marziyeh Najafi, Golbon Sohrab
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2020; 14(5): 1521. CrossRef - Biological fates of tea polyphenols and their interactions with microbiota in the gastrointestinal tract: implications on health effects
Tingting Chen, Chung S. Yang
Critical Reviews in Food Science and Nutrition.2020; 60(16): 2691. CrossRef - Effects of Timing of Acute and Consecutive Catechin Ingestion on Postprandial Glucose Metabolism in Mice and Humans
Masaki Takahashi, Mamiho Ozaki, Miku Tsubosaka, Hyeon-Ki Kim, Hiroyuki Sasaki, Yuji Matsui, Masanobu Hibi, Noriko Osaki, Masashi Miyashita, Shigenobu Shibata
Nutrients.2020; 12(2): 565. CrossRef - Green tea (Camellia sinensis) for the prevention of cancer
Tommaso Filippini, Marcella Malavolti, Francesca Borrelli, Angelo A Izzo, Susan J Fairweather-Tait, Markus Horneber, Marco Vinceti
Cochrane Database of Systematic Reviews.2020;[Epub] CrossRef - Metabolic Impact of Flavonoids Consumption in Obesity: From Central to Peripheral
Viviana Sandoval, Hèctor Sanz-Lamora, Giselle Arias, Pedro F. Marrero, Diego Haro, Joana Relat
Nutrients.2020; 12(8): 2393. CrossRef - Pathophysiological mechanisms of diabetic cardiomyopathy and the therapeutic potential of epigallocatechin-3-gallate
Amir M. Al Hroob, Mohammad H. Abukhalil, Omnia E. Hussein, Ayman M. Mahmoud
Biomedicine & Pharmacotherapy.2019; 109: 2155. CrossRef - Effects and Mechanisms of Tea for the Prevention and Management of Diabetes Mellitus and Diabetic Complications: An Updated Review
Jin-Ming Meng, Shi-Yu Cao, Xin-Lin Wei, Ren-You Gan, Yuan-Feng Wang, Shu-Xian Cai, Xiao-Yu Xu, Pang-Zhen Zhang, Hua-Bin Li
Antioxidants.2019; 8(6): 170. CrossRef - Improvement in fasting blood sugar, anthropometric measurement and hs-CRP after consumption of epigallocatechin-3-gallate (EGCG) in patients with type 2 diabetes mellitus
Said Hadi, Meysam Alipour, Vahideh Aghamohammadi, Sahar Shahemi, Fatemeh Ghafouri-Taleghani, Niloufar Pourjavidi, Mona Foroughi, Mackaan Chraqipoor
Nutrition & Food Science .2019; 50(2): 348. CrossRef - The Phosphorylation of IRS1S307 and AktS473 Molecules in Insulin‐Resistant C2C12 Cells Induced with Palmitate Is Influenced by Epigallocatechin Gallate from Green Tea
Salar Bakhtiyari, Motahareh Zaherara, Karimeh Haghani, Mehrdad Khatami, Ali Rashidinejad
Lipids.2019; 54(2-3): 141. CrossRef - Effect of annatto-extracted tocotrienols and green tea polyphenols on glucose homeostasis and skeletal muscle metabolism in obese male mice
Eunhee Chung, Salvatore N. Campise, Hayli E. Joiner, Michael D. Tomison, Gurvinder Kaur, Jannette M. Dufour, Lillian Cole, Latha Ramalingam, Naima Moustaid-Moussa, Chwan-Li Shen
The Journal of Nutritional Biochemistry.2019; 67: 36. CrossRef - Studies on the Prevention of Cancer and Cardiometabolic Diseases by Tea: Issues on Mechanisms, Effective Doses, and Toxicities
Chung S. Yang, Jinsong Zhang
Journal of Agricultural and Food Chemistry.2019; 67(19): 5446. CrossRef - Salvianolic acid B plays an anti-obesity role in high fat diet-induced obese mice by regulating the expression of mRNA, circRNA, and lncRNA
Tian An, Jing Zhang, Bohan Lv, Yufei Liu, Jiangpinghao Huang, Juan Lian, Yanxiang Wu, Sihua Gao, Guangjian Jiang
PeerJ.2019; 7: e6506. CrossRef - Popular functional foods and herbs for the management of type-2-diabetes mellitus: A comprehensive review with special reference to clinical trials and its proposed mechanism
Kamesh Venkatakrishnan, Hui-Fang Chiu, Chin-Kun Wang
Journal of Functional Foods.2019; 57: 425. CrossRef - Green Tea Polyphenols Modify the Gut Microbiome in db/db Mice as Co‐Abundance Groups Correlating with the Blood Glucose Lowering Effect
Tingting Chen, Anna B. Liu, Shili Sun, Nadim J. Ajami, Matthew C. Ross, Hong Wang, Le Zhang, Kenneth Reuhl, Koichi Kobayashi, Janet C. Onishi, Liping Zhao, Chung S. Yang
Molecular Nutrition & Food Research.2019;[Epub] CrossRef - Effect of herbal tea on glycemic control in patients with type 2 diabetes
Boxun Zhang, Rensong Yue, Xiaoying Huang, Ying Wang, Yayi Jiang, Jiawei Chin
Medicine.2019; 98(50): e18346. CrossRef - Effects of polysaccharides and polyphenolics fractions of Zijuan tea (Camellia sinensis var. kitamura) on α‐glucosidase activity and blood glucose level and glucose tolerance of hyperglycaemic mice
Dejing Chen, Jingyuan Sun, Weixue Dong, Yixiao Shen, Zhimin Xu
International Journal of Food Science & Technology.2018; 53(10): 2335. CrossRef - Green tea consumption reduces apelin and orexin-A in overweight and obese women with different training modalities
Rahman Soori, Azadeh Safei, Parisa Pournemati, Amine Ghram
Sport Sciences for Health.2018; 14(2): 421. CrossRef - Green tea consumption and risk of type 2 diabetes in Chinese adults: the Shanghai Women’s Health Study and the Shanghai Men’s Health Study
Xiaona Liu, Wanghong Xu, Hui Cai, Yu-Tang Gao, Honglan Li, Bu-Tian Ji, Xiang Shu, Thomas Wang, Robert E Gerszten, Wei Zheng, Yong-Bing Xiang, Xiao-Ou Shu
International Journal of Epidemiology.2018; 47(6): 1887. CrossRef
- Is breakfast consumption detrimental, unnecessary, or an opportunity for health promotion? A review of cardiometabolic outcomes and functional food choices
- Clinical Diabetes & Therapeutics
- Determinants of Long-Term Durable Glycemic Control in New-Onset Type 2 Diabetes Mellitus
- Kyoung Jin Kim, Ju Hee Choi, Kyeong Jin Kim, Jee Hyun An, Hee Young Kim, Sin Gon Kim, Nam Hoon Kim
- Diabetes Metab J. 2017;41(4):284-295. Published online August 3, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.4.284
- 4,371 View
- 80 Download
- 11 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Long-term durable glycemic control is a difficult goal in the management of type 2 diabetes mellitus (T2DM). We evaluated the factors associated with durable glycemic control in a real clinical setting.
Methods We retrospectively reviewed the medical records of 194 new-onset, drug-naïve patients with T2DM who were diagnosed between January 2011 and March 2013, and were followed up for >2 years. Glycemic durability was defined as the maintenance of optimal glycemic control (glycosylated hemoglobin [HbA1c] <7.0%) for 2 years without substitution or adding other glucose-lowering agents. Clinical factors and glycemic markers associated with glycemic durability were compared between two groups: a durability group and a non-durability group.
Results Patients in the durability group had a higher baseline body mass index (26.1 kg/m2 vs. 24.9 kg/m2) and lower HbA1c (8.6% vs. 9.7%) than the non-durability group. The initial choice of glucose-lowering agents was similar in both groups, except for insulin and sulfonylureas, which were more frequently prescribed in the non-durability group. In multiple logistic regression analyses, higher levels of education, physical activity, and homeostasis model assessment of β-cell function (HOMA-β) were associated with glycemic durability. Notably, lower HbA1c (<7.0%) at baseline and first follow-up were significantly associated with glycemic durability (adjusted odds ratio [OR], 7.48; 95% confidence interval [CI], 2.51 to 22.3) (adjusted OR, 9.27; 95% CI, 1.62 to 53.1, respectively), after adjusting for confounding variables including the types of glucose-lowering agents.
Conclusion Early achievement of HbA1c level within the glycemic target was a determinant of long-term glycemic durability in new-onset T2DM, as were higher levels of education, physical activity, and HOMA-β.
-
Citations
Citations to this article as recorded by- Initial Combination Therapy in Type 2 Diabetes
Ji Yoon Kim, Nam Hoon Kim
Endocrinology and Metabolism.2024; 39(1): 23. CrossRef - Validation of RSSDI therapeutic wheel with clinical experience of Indian physicians
Dhruvi Hasnani, Vipul Chavda, Dinesh Agrawal, Bijay Patni, Ashwin David, Sachin Gathe, Rajeev Chawla, Jothydev Kesavadev, Sunil Gupta, Shriji Hasnani, Banshi Saboo
International Journal of Diabetes in Developing Countries.2022; 42(3): 451. CrossRef - Greater Glycemic Burden Is Associated with Further Poorer Glycemic Control in Newly-Diagnosed Type 2 Diabetes Mellitus Patients
Wei-Lun Wen, Hui-Chun Huang, Hsiu-Chu Lin, Wan-Ching Lo, Szu-Chia Chen, Mei-Yueh Lee
Nutrients.2022; 14(2): 320. CrossRef - Durability of glucose-lowering effect of dulaglutide in patients with type 2 diabetes mellitus: A real-world data study
Hwi Seung Kim, Yun Kyung Cho, Myung Jin Kim, Chang Hee Jung, Joong-Yeol Park, Woo Je Lee
Frontiers in Endocrinology.2022;[Epub] CrossRef - Durability of glycaemic control in type 2 diabetes: A systematic review and meta‐analysis for its association with body weight changes
Danpei Li, HuaJie Zou, Ping Yin, Wenjun Li, Junyu He, Shuyun Wang, Li Huang, Shiying Shao, Yong Chen, Yan Yang, Xuefeng Yu
Diabetes, Obesity and Metabolism.2021; 23(1): 208. CrossRef - Early combination versus initial metformin monotherapy in the management of newly diagnosed type 2 diabetes: AnEast Asianperspective
Linong Ji, Juliana C. N. Chan, Miao Yu, Kun Ho Yoon, Sin Gon Kim, Sung Hee Choi, Chien‐Ning Huang, Shih Te Tu, Chih‐Yuan Wang, Päivi Maria Paldánius, Wayne H. H. Sheu
Diabetes, Obesity and Metabolism.2021; 23(1): 3. CrossRef - Time to Reach Target Glycosylated Hemoglobin Is Associated with Long-Term Durable Glycemic Control and Risk of Diabetic Complications in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A 6-Year Observational Study
Kyoung Jin Kim, Jimi Choi, Jae Hyun Bae, Kyeong Jin Kim, Hye Jin Yoo, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2021; 45(3): 368. CrossRef - Effectiveness of Resistance Training and Associated Program Characteristics in Patients at Risk for Type 2 Diabetes: a Systematic Review and Meta-analysis
Raza Qadir, Nicholas F. Sculthorpe, Taylor Todd, Elise C. Brown
Sports Medicine - Open.2021;[Epub] CrossRef - Time to Reach Target Glycosylated Hemoglobin Is Associated with Long-Term Durable Glycemic Control and Risk of Diabetic Complications in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A 6-Year Observational Study (Diabetes Metab J 2021;45:368-78)
Ja Young Jeon
Diabetes & Metabolism Journal.2021; 45(4): 613. CrossRef - Association of Habitual Daily Physical Activity With Glucose Tolerance and β-Cell Function in Adults With Impaired Glucose Tolerance or Recently Diagnosed Type 2 Diabetes From the Restoring Insulin Secretion (RISE) Study
Karla A. Temple, Ashley H. Tjaden, Karen M. Atkinson, Elena Barengolts, Tamara S. Hannon, Kieren J. Mather, Kristina M. Utzschneider, Sharon L. Edelstein, David A. Ehrmann, Babak Mokhlesi, Philip S. Zeitler, Jayne Williams, Melanie Cree-Green, Yesenia Gar
Diabetes Care.2019; 42(8): 1521. CrossRef - Factors Associated with Poor Hemoglobin A1c Control in Patients with Type 2 Diabetes
Salam Alqudah, Anan S. Jarab, Eman A. Alefishat, Fadia Mayyas, Maher Khdour, Sharrel Pinto
Current Diabetes Reviews.2019; 15(2): 164. CrossRef
- Initial Combination Therapy in Type 2 Diabetes
- The Role of Glucagon-Like Peptide-1 Receptor Agonists in Type 2 Diabetes: Understanding How Data Can Inform Clinical Practice in Korea
- Seungjoon Oh, Suk Chon, Kyu Jeong Ahn, In-Kyung Jeong, Byung-Joon Kim, Jun Goo Kang
- Diabetes Metab J. 2015;39(3):177-187. Published online June 15, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.3.177
- 4,198 View
- 47 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Glucagon-like peptide-1 receptor agonists (GLP-1RAs) reduce glycosylated hemoglobin (HbA1c, 0.5% to 1.0%), and are associated with moderate weight loss and a relatively low risk of hypoglycemia. There are differences between Asian and non-Asian populations. We reviewed available data on GLP-1RAs, focusing on Korean patients, to better understand their risk/benefit profile and help inform local clinical practice. Control of postprandial hyperglycemia is important in Asians in whom the prevalence of post-challenge hyperglycemia is higher (vs. non-Asians). The weight lowering effects of GLP-1RAs are becoming more salient as the prevalence of overweight and obesity among Korean patients increases. The higher rate of gastrointestinal adverse events amongst Asian patients in clinical trials may be caused by higher drug exposure due to the lower body mass index of the participants (vs. non-Asian studies). Data on the durability of weight loss, clinically important health outcomes, safety and optimal dosing in Korean patients are lacking. Use of GLP-1RAs is appropriate in several patient groups, including patients whose HbA1c is uncontrolled, especially if this is due to postprandial glucose excursions and patients who are overweight or obese due to dietary problems (e.g., appetite control). The potential for gastrointestinal adverse events should be explained to patients at treatment initiation to facilitate the promotion of better compliance.
-
Citations
Citations to this article as recorded by- Tolerability and Effectiveness of Switching to Dulaglutide in Patients With Type 2 Diabetes Inadequately Controlled With Insulin Therapy
Youngsook Kim, Ji Hye Huh, Minyoung Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Frontiers in Endocrinology.2022;[Epub] CrossRef - Antihyperglycemic Agent Therapy for Adult Patients with Type 2 Diabetes Mellitus 2017: A Position Statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
Diabetes & Metabolism Journal.2017; 41(5): 337. CrossRef - Antihyperglycemic agent therapy for adult patients with type 2 diabetes mellitus 2017: a position statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
The Korean Journal of Internal Medicine.2017; 32(6): 947. CrossRef
- Tolerability and Effectiveness of Switching to Dulaglutide in Patients With Type 2 Diabetes Inadequately Controlled With Insulin Therapy
- Subjective Assessment of Diabetes Self-Care Correlates with Perceived Glycemic Control but not with Actual Glycemic Control
- Jung Hun Ohn, Ju Hee Lee, Eun Shil Hong, Bo Kyung Koo, Sang Wan Kim, Ka Hee Yi, Min Kyong Moon
- Diabetes Metab J. 2015;39(1):31-36. Published online February 16, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.1.31
- 3,501 View
- 29 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We investigated whether patients' perceived glycemic control and self-reported diabetes self-care correlated with their actual glycemic control.
Methods A survey was administered among patients with diabetes mellitus at an outpatient clinic with structured self-report questionnaires regarding perceived glycemic control and diabetes self-management. Actual glycemic control was defined as a change in glycated hemoglobin (A1C) or fasting plasma glucose (FPG) since the last clinic visit.
Results Patients who perceived their glycemic control as "improved" actually showed a mild but significant decrease in the mean A1C (-0.1%,
P =0.02), and those who perceived glycemic control as "aggravated" had a significant increase in the mean FPG (10.5 mg/dL or 0.59 mmol/L,P =0.04) compared to the "stationary" group. However, one-half of patients falsely predicted their actual glycemic control status. Subjective assessment of diabetes self-care efforts, such as adherence to a diet regimen or physical activity, correlated positively with perceived glycemic control but showed no association with actual glycemic control.Conclusion Patients should be encouraged to assess and monitor diabetes self-care more objectively to motivate behavioral modifications and improve their actual glycemic control.
-
Citations
Citations to this article as recorded by- Social Networking Services-Based Communicative Care for Patients with Diabetes Mellitus in Korea
Hun-Sung Kim, Yoo Jeong, Sun Baik, So Yang, Tong Kim, Hyunah Kim, Hyunyong Lee, Seung-Hwan Lee, Jae Cho, In-Young Choi, Kun-Ho Yoon
Applied Clinical Informatics.2016; 07(03): 899. CrossRef
- Social Networking Services-Based Communicative Care for Patients with Diabetes Mellitus in Korea
- Current Status of Glycemic Control of Patients with Diabetes in Korea: The Fifth Korea National Health and Nutrition Examination Survey
- Ja Young Jeon, Dae Jung Kim, Seung-Hyun Ko, Hyuk-Sang Kwon, Soo Lim, Sung Hee Choi, Chul Sik Kim, Jee Hyun An, Nan Hee Kim, Jong Chul Won, Jae Hyeon Kim, Bong-Yun Cha, Kee-Ho Song
- Diabetes Metab J. 2014;38(3):197-203. Published online June 17, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.3.197
- 4,538 View
- 56 Download
- 45 Web of Science
- 49 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The Korea National Health and Nutrition Examination Survey (KNHANES) III (2005) reported that 22.9% of individuals with diabetes have a glycated hemoglobin (HbA1c) <6.5% and that 43.5% have an HbA1c <7%. We investigated the levels of glycemic control and the factors associated with glycemic control using data from the KNHANES V (2010 to 2012).
Methods Subjects with diabetes diagnosed by a physician or those taking antidiabetic medications were classified as individuals with known diabetes. Of 1,498 subjects aged ≥30 years with diabetes, we excluded 157 individuals who were missing HbA1c data. A total of 1,341 subjects were included in the final analysis.
Results The prevalence of known diabetes was 7.7% (
n =1,498, estimated to be 2.32 million people). The proportions of well-controlled diabetes meeting a HbA1c goal of <6.5% and <7% were 27% and 45.6%, respectively. HbA1c increased as the duration of diabetes increased. HbA1c in subjects with a duration of diabetes ≤5 years was lower than in subjects with a duration >5 years. HbA1c in the group taking only oral hypoglycemic agents (OHAs) was significantly lower than that in the group administered only insulin or OHA and insulin in combination. In logistic regression analysis, a longer duration of diabetes, insulin use and the absence of chronic renal failure were associated with HbA1c levels >6.5%.Conclusion The level of adequate glycemic control was similar to but slightly improved compared with previous levels. The glycemic control of long-standing diabetes patients is more difficult even though they receive insulin treatment.
-
Citations
Citations to this article as recorded by- Therapeutic Effects of Switching to Anagliptin from Other DPP-4 Inhibitors in T2DM Patients with Inadequate Glycemic Control: A Non-interventional, Single-Arm, Open-Label, Multicenter Observational Study
Sang-Yong Kim, Sungrae Kim
Diabetes Therapy.2023; 14(1): 109. CrossRef - Declined incidence of patients treated for vision-threatening diabetic retinopathy in South Korea: a 12-year nationwide population-based study
Jiwon Kim, Hyojin Seong, Kang Ju Son, Eun Jee Chung
Graefe's Archive for Clinical and Experimental Ophthalmology.2022; 260(1): 101. CrossRef - Glycemic status and general characteristics among individuals with undiagnosed diabetes; findings from second National Diabetes Survey of Pakistan 2016–2017 (NDSP 08)
Abdul Basit, Nazish Waris, Asher Fawwad, Bilal Tahir, Iftikhar Ahmed Siddiqui, Mujeeb Ur Rehman Abro, Khawaja Ishfaq Ahmed, Khurshid Ahmed, Sobia Sabir Ali, Ahmed Bilal, Anam Butt, Bikha Ram Devrajani, Ijaz Hayder, Yasir Humayun, Rabia Irshad, Riasat Ali
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2022; 16(6): 102535. CrossRef - Glycemic control and its determinants among people with type 2 diabetes mellitus in Ernakulam district, Kerala
ShanaShirin Najeeb, TeenaMary Joy, Aswathy Sreedevi, K Vijayakumar
Indian Journal of Public Health.2022; 66(5): 80. CrossRef - C-peptide level as predictor of type 2 diabetes remission and body composition changes in non-diabetic and diabetic patients after Roux-en-Y gastric bypass
Roberto de Cleva, Flavio Kawamoto, Georgia Borges, Priscila Caproni, Alex Jones Flores Cassenote, Marco Aurelio Santo
Clinics.2021; 76: e2906. CrossRef - Inadequate achievement of ABC goals (HbA1c, blood pressure, LDL-C) among patients with type 2 diabetes in an Iranian population, 2012–2017
Mehrdad Larry, Saeid Alizadeh, Sina Naderi, Bahareh Salekani, Mohammad Ali Mansournia, Soghra Rabizadeh, Alireza Esteghamati, Manouchehr Nakhjavani
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2020; 14(4): 619. CrossRef - Site-specific cancer risk in patients with type 2 diabetes: a nationwide population-based cohort study in Korea
Suk Kyeong Kim, Ju-Young Jang, Dong-Lim Kim, Young A Rhyu, Suh Eun Lee, Seung-Hyun Ko, Kyungdo Han, Kee-Ho Song
The Korean Journal of Internal Medicine.2020; 35(3): 641. CrossRef - The development of oral semaglutide, an oral GLP-1 analog, for the treatment of type 2 diabetes
Mads Frederik Rasmussen
Diabetology International.2020; 11(2): 76. CrossRef - An Assessment of Pharmacokinetic Interaction Between Lobeglitazone and Sitagliptin After Multiple Oral Administrations in Healthy Men
Seol Ju Moon, Kyung-Sang Yu, Min-Gul Kim
Clinical Therapeutics.2020; 42(6): 1047. CrossRef - Nationwide Trends in Pancreatitis and Pancreatic Cancer Risk Among Patients With Newly Diagnosed Type 2 Diabetes Receiving Dipeptidyl Peptidase 4 Inhibitors
Minyoung Lee, Jiyu Sun, Minkyung Han, Yongin Cho, Ji-Yeon Lee, Chung Mo Nam, Eun Seok Kang
Diabetes Care.2019; 42(11): 2057. CrossRef - Factors Influencing Glycemic Control among Type 2 Diabetes Mellitus Patients: The Sixth Korea National Health and Nutrition Examination Survey (2013~2015)
Mee Ock Gu
Korean Journal of Adult Nursing.2019; 31(3): 235. CrossRef - Trends in metabolic risk factors among patients with diabetes mellitus according to income levels: the Korea National Health and Nutrition Examination Surveys 1998 ~ 2014
Sukyung Cho, Kyong Park
Journal of Nutrition and Health.2019; 52(2): 206. CrossRef - Current status of treatment of type 2 diabetes mellitus in Ningbo, China
Tianmeng Yang, Rongjiong Zheng, Qingmei Chen, Yushan Mao
Journal of Clinical Laboratory Analysis.2019;[Epub] CrossRef - Trends in the prevalence and management of diabetes in Korea: 2007-2017
Ji-Yeon Shin
Epidemiology and Health.2019; 41: e2019029. CrossRef - Diabetes Fact Sheets in Korea, 2018: An Appraisal of Current Status
Bo-Yeon Kim, Jong Chul Won, Jae Hyuk Lee, Hun-Sung Kim, Jung Hwan Park, Kyoung Hwa Ha, Kyu Chang Won, Dae Jung Kim, Kyong Soo Park
Diabetes & Metabolism Journal.2019; 43(4): 487. CrossRef - A new comprehensive diabetes health literacy scale: Development and psychometric evaluation
Eun-Hyun Lee, Young Whee Lee, Kwan-Woo Lee, Moonsuk Nam, So Hun Kim
International Journal of Nursing Studies.2018; 88: 1. CrossRef - Women are less likely than men to achieve optimal glycemic control after 1 year of treatment: A multi-level analysis of a Korean primary care cohort
Seung-Ah Choe, Joo Yeong Kim, Young Sun Ro, Sung-Il Cho, Antonio Palazón-Bru
PLOS ONE.2018; 13(5): e0196719. CrossRef - Ten-Year Mortality Trends for Adults with and without Diabetes Mellitus in South Korea, 2003 to 2013
Kyeong Jin Kim, Tae Yeon Kwon, Sungwook Yu, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Dong Seop Choi, Sin Gon Kim, Yousung Park, Nam Hoon Kim
Diabetes & Metabolism Journal.2018; 42(5): 394. CrossRef - Comparison of Adherence to Glimepiride/Metformin Sustained Release Once-daily Versus Glimepiride/Metformin Immediate Release BID Fixed-combination Therapy Using the Medication Event Monitoring System in Patients With Type 2 Diabetes
Jong-Dai Kim, Cheol-Young Park, Bong-Yun Cha, Kyu Jeung Ahn, In Joo Kim, Kyong Soo Park, Hyung Woo Lee, Kyung-Wan Min, Jong Chul Won, Min Young Chung, Jae-Taek Kim, Jun Goo Kang, Sung-Woo Park
Clinical Therapeutics.2018; 40(5): 752. CrossRef - Negative Association of Hepatitis B Virus With Hearing Impairment
SKM Azizul Islam, Jin Wook Chung, Young-Sil Lee, HoChan Cho, Seong-Su Moon
American Journal of Audiology.2018; 27(3): 324. CrossRef - The effectiveness, reproducibility, and durability of tailored mobile coaching on diabetes management in policyholders: A randomized, controlled, open-label study
Da Young Lee, Jeongwoon Park, Dooah Choi, Hong-Yup Ahn, Sung-Woo Park, Cheol-Young Park
Scientific Reports.2018;[Epub] CrossRef - Prediction of Type 2 Diabetes Remission after Bariatric or Metabolic Surgery
Ji Yeon Park
Journal of Obesity & Metabolic Syndrome.2018; 27(4): 213. CrossRef - Past and Current Status of Adult Type 2 Diabetes Mellitus Management in Korea: A National Health Insurance Service Database Analysis
Seung-Hyun Ko, Kyungdo Han, Yong-ho Lee, Junghyun Noh, Cheol-Young Park, Dae-Jung Kim, Chang Hee Jung, Ki-Up Lee, Kyung-Soo Ko
Diabetes & Metabolism Journal.2018; 42(2): 93. CrossRef - Prediction of Diabetes Remission after Bariatric or Metabolic Surgery
Ji Yeon Park
Journal of Metabolic and Bariatric Surgery.2018; 7(1): 22. CrossRef - Detrimental Effects of Higher Body Mass Index and Smoking Habits on Menstrual Cycles in Korean Women
An Na Jung, Ju Hwan Park, Jihyun Kim, Seok Hyun Kim, Byung Chul Jee, Byung Heun Cha, Jae Woong Sull, Jin Hyun Jun
Journal of Women's Health.2017; 26(1): 83. CrossRef - Improved trends in cardiovascular complications among subjects with type 2 diabetes in Korea: a nationwide study (2006–2013)
Chang Hee Jung, Jin Ook Chung, Kyungdo Han, Seung-Hyun Ko, Kyung Soo Ko, Joong-Yeol Park
Cardiovascular Diabetology.2017;[Epub] CrossRef - The differences in the incidence of diabetes mellitus and prediabetes according to the type of HMG-CoA reductase inhibitors prescribed in Korean patients
Tong Min Kim, Hyunah Kim, Yoo Jin Jeong, Sun Jung Baik, So Jung Yang, Seung-Hwan Lee, Jae-Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, In Young Choi, Kun-Ho Yoon, Hun-Sung Kim
Pharmacoepidemiology and Drug Safety.2017; 26(10): 1156. CrossRef - Euglycemic Diabetic Ketoacidosis When Reducing Insulin Dosage in Patients Taking Sodium Glucose Cotransporter 2 Inhibitor
Woo Jin Yi, Soo-Kyung Kim, Sun Ung Youn, Namkyu Kang, Myung Won Lee, Seok O Park
The Ewha Medical Journal.2017; 40(1): 55. CrossRef - Effectiveness of Vildagliptin in Clinical Practice: Pooled Analysis of Three Korean Observational Studies (the VICTORY Study)
Sunghwan Suh, Sun Ok Song, Jae Hyeon Kim, Hyungjin Cho, Woo Je Lee, Byung-Wan Lee
Journal of Diabetes Research.2017; 2017: 1. CrossRef - Prevalence and risk factors for reduced pulmonary function in diabetic patients: The Korea National Health and Nutrition Examination Survey
Hee Yeon Kim, Tae Seo Sohn, Hannah Seok, Chang Dong Yeo, Young Soo Kim, Jae Yen Song, Young Bok Lee, Dong-Hee Lee, Jae-Im Lee, Tae-Kyu Lee, Seong Cheol Jeong, Mihee Hong, Hiun Suk Chae
The Korean Journal of Internal Medicine.2017; 32(4): 682. CrossRef - Delay of insulin initiation in patients with type 2 diabetes mellitus inadequately controlled with oral hypoglycemic agents (analysis of patient‐ and physician‐related factors): A prospective observational DIPP‐FACTOR study in Korea
Sin Gon Kim, Nam Hoon Kim, Bon Jeong Ku, Ho Sang Shon, Doo Man Kim, Tae Sun Park, Yong‐Seong Kim, In Joo Kim, Dong Seop Choi
Journal of Diabetes Investigation.2017; 8(3): 346. CrossRef - Effectiveness and safety of exenatide in Korean patients with type 2 diabetes inadequately controlled with oral hypoglycemic agents: an observational study in a real clinical practice
You-Cheol Hwang, Ari Kim, Euna Jo, Yeoree Yang, Jae-Hyoung Cho, Byung-Wan Lee
BMC Endocrine Disorders.2017;[Epub] CrossRef - Current status of managing diabetes mellitus in Korea
Kyoung Hwa Ha, Dae Jung Kim
The Korean Journal of Internal Medicine.2016; 31(5): 845. CrossRef - Trends of antidiabetic drug use in adult type 2 diabetes in Korea in 2002–2013
Seung-Hyun Ko, Dae-Jung Kim, Jong-Heon Park, Cheol-Young Park, Chang Hee Jung, Hyuk-Sang Kwon, Joong-Yeol Park, Kee-Ho Song, Kyungdo Han, Ki-Up Lee, Kyung-Soo Ko
Medicine.2016; 95(27): e4018. CrossRef - A patient-centric approach to optimise insulin therapy in Asia
Su Yen Goh, Ernesto Ang, Shailendra Bajpai, Chaicharn Deerochanawong, Eun-Gyoung Hong, Zanariah Hussein, Shashank Joshi, Nor Azmi Kamaruddin, Sjoberg Kho, Alice Pik-Shan Kong, Chang Yu Pan, Riccardo Perfetti, Apichati Vichayanrat, Aleksandra Vlajnic, Juli
Journal of Diabetes and its Complications.2016; 30(6): 973. CrossRef - Association between blood glucose level derived using the oral glucose tolerance test and glycated hemoglobin level
Hyoung Joo Kim, Young Geon Kim, Jin Soo Park, Young Hwan Ahn, Kyoung Hwa Ha, Dae Jung Kim
The Korean Journal of Internal Medicine.2016; 31(3): 535. CrossRef - Social Networking Services-Based Communicative Care for Patients with Diabetes Mellitus in Korea
Hun-Sung Kim, Yoo Jeong, Sun Baik, So Yang, Tong Kim, Hyunah Kim, Hyunyong Lee, Seung-Hwan Lee, Jae Cho, In-Young Choi, Kun-Ho Yoon
Applied Clinical Informatics.2016; 07(03): 899. CrossRef - Factors Associated with Poor Glycemic Control among Patients with Type 2 Diabetes Mellitus: The Fifth Korea National Health and Nutrition Examination Survey (2010-2012)
Jinhyun Park, Seungji Lim, Eunshil Yim, Youngdae Kim, Woojin Chung
Health Policy and Management.2016; 26(2): 125. CrossRef - Reduction of Sulfonylurea with the Initiation of Basal Insulin in Patients with Inadequately Controlled Type 2 Diabetes Mellitus Undergoing Long-Term Sulfonylurea-Based Treatment
Yeoree Yang, Jeong-Ah Shin, Hae Kyung Yang, Seung-Hwan Lee, Seung-Hyun Ko, Yu-Bae Ahn, Kun-Ho Yoon, Jae-Hyoung Cho
Diabetes & Metabolism Journal.2016; 40(6): 454. CrossRef - Health inequalities in hypertension and diabetes management among the poor in urban areas: a population survey analysis in south Korea
Young-Jee Jeon, Chung Reen Kim, Joo-Sung Park, Kyung-Hyun Choi, Myoung Joo Kang, Seung Guk Park, Young-Jin Park
BMC Public Health.2016;[Epub] CrossRef - Prediction of Diabetes Remission in Morbidly Obese Patients After Roux-en-Y Gastric Bypass
Ji Yeon Park, Yong Jin Kim
Obesity Surgery.2016; 26(4): 749. CrossRef - Inhibition of advanced glycation end product formation by burdock root extract
Darye Lee, Choon Young Kim
Journal of Nutrition and Health.2016; 49(4): 233. CrossRef - Diabetes in Asians
Eun-Jung Rhee
Endocrinology and Metabolism.2015; 30(3): 263. CrossRef - Insulin Initiation in Insulin-Naïve Korean Type 2 Diabetic Patients Inadequately Controlled on Oral Antidiabetic Drugs in Real-World Practice: The Modality of Insulin Treatment Evaluation Study
Sang Soo Kim, In Joo Kim, Yong Ki Kim, Kun Ho Yoon, Ho Young Son, Sung Woo Park, Yeon Ah Sung, Hong Sun Baek
Diabetes & Metabolism Journal.2015; 39(6): 481. CrossRef - Current status of glucose, blood pressure and lipid management in type 2 diabetes clinic attendees in Isfahan, Iran
Mohsen Janghorbani, Bahman Papi, Masoud Amini
Journal of Diabetes Investigation.2015; 6(6): 716. CrossRef - Trends in the Diabetes Epidemic in Korea
Kyoung Hwa Ha, Dae Jung Kim
Endocrinology and Metabolism.2015; 30(2): 142. CrossRef - The Side Effects of Sodium Glucose Cotransporter 2 (SGLT2) Inhibitor
Won Jin Kim, Sang Soo Kim
The Journal of Korean Diabetes.2014; 15(3): 158. CrossRef - It's Still Not Too Late to Make a Change: Current Status of Glycemic Control in Korea
Sang Yong Kim
Diabetes & Metabolism Journal.2014; 38(3): 194. CrossRef - Association between Diabetes Education Status and Clinical Outcomes of Patients with Diabetes Mellitus: Analysis of the Fifth Korea National Health and Nutrition Examination Survey (KNHANES V)
Jun Sung Kwon, Won Jun Kim, Yang Hee Han, Hyun Joong Kim, Sa Young Shin, Kyoo Ho Choi, Jae Hyuck Jun, Myoung Sook Shim, Jin Yeob Kim
The Journal of Korean Diabetes.2014; 15(4): 236. CrossRef
- Therapeutic Effects of Switching to Anagliptin from Other DPP-4 Inhibitors in T2DM Patients with Inadequate Glycemic Control: A Non-interventional, Single-Arm, Open-Label, Multicenter Observational Study

 KDA
KDA
 First
First Prev
Prev





