
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Metabolic Risk/Epidemiology
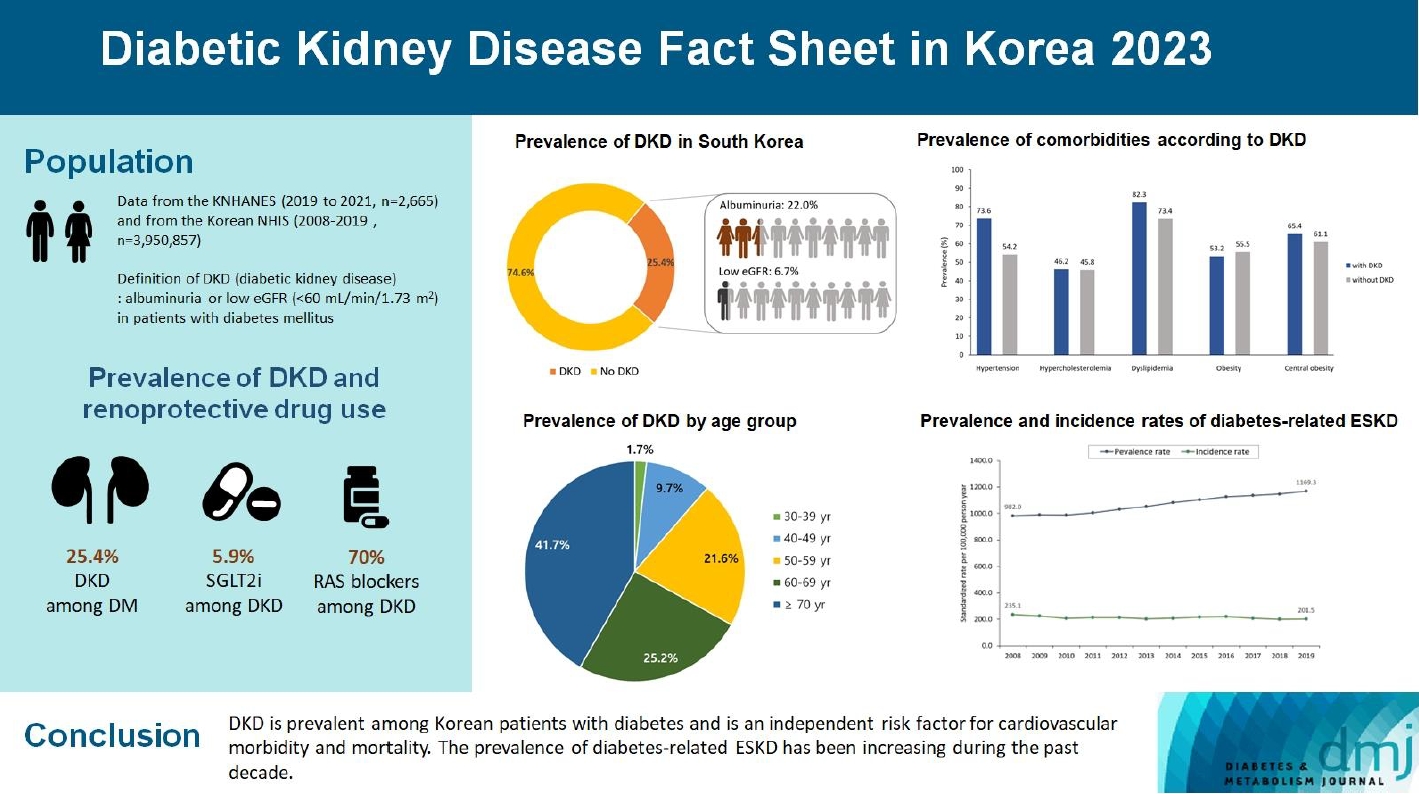
- 2023 Diabetic Kidney Disease Fact Sheet in Korea
- Nam Hoon Kim, Mi-Hae Seo, Jin Hyung Jung, Kyung Do Han, Mi Kyung Kim, Nan Hee Kim, on Behalf of Diabetic Kidney Disease Research Group of the Korean Diabetes Association
- Received July 30, 2023 Accepted January 26, 2024 Published online March 19, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0310 [Epub ahead of print]
- 727 View
- 53 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To investigate the prevalence, incidence, comorbidities, and management status of diabetic kidney disease (DKD) and diabetes-related end-stage kidney disease (ESKD) in South Korea.
Methods
We used the Korea National Health and Nutrition Examination Survey data (2019 to 2021, n=2,665) for the evaluation of prevalence, comorbidities, control rate of glycemia and comorbidities in DKD, and the Korean Health Insurance Service-customized database (2008 to 2019, n=3,950,857) for the evaluation of trends in the incidence and prevalence rate of diabetes-related ESKD, renin-angiotensin system (RAS) blockers and sodium glucose cotransporter 2 (SGLT2) inhibitors use for DKD, and the risk of atherosclerotic cardiovascular disease (ASCVD) and mortality according to DKD stages. DKD was defined as albuminuria or low estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2 in patients with diabetes mellitus.
Results
The prevalence of DKD was 25.4% (albuminuria, 22.0%; low eGFR, 6.73%) in patients with diabetes mellitus aged ≥30 years. Patients with DKD had a higher rate of comorbidities, including hypertension, dyslipidemia, and central obesity; however, their control rates were lower than those without DKD. Prescription rate of SGLT2 inhibitors with reduced eGFR increased steadily, reaching 5.94% in 2019. Approximately 70% of DKD patients were treated with RAS blockers. The prevalence rate of diabetesrelated ESKD has been steadily increasing, with a higher rate in older adults. ASCVD and mortality were significantly associated with an in increase in DKD stage.
Conclusion
DKD is prevalent among Korean patients with diabetes and is an independent risk factor for cardiovascular morbidity and mortality, which requiring intensive management of diabetes and comorbidities. The prevalence of diabetes-related ESKD has been increasing, especially in the older adults, during past decade. -
Citations
Citations to this article as recorded by- Endothelial NOX5 Obliterates the Reno-Protective Effect of Nox4 Deletion by Promoting Renal Fibrosis via Activation of EMT and ROS-Sensitive Pathways in Diabetes
Karin A. M. Jandeleit-Dahm, Haritha R. Kankanamalage, Aozhi Dai, Jaroslawna Meister, Sara Lopez-Trevino, Mark E. Cooper, Rhian M. Touyz, Christopher R. J. Kennedy, Jay C. Jha
Antioxidants.2024; 13(4): 396. CrossRef
- Endothelial NOX5 Obliterates the Reno-Protective Effect of Nox4 Deletion by Promoting Renal Fibrosis via Activation of EMT and ROS-Sensitive Pathways in Diabetes
- Guideline/Fact Sheet
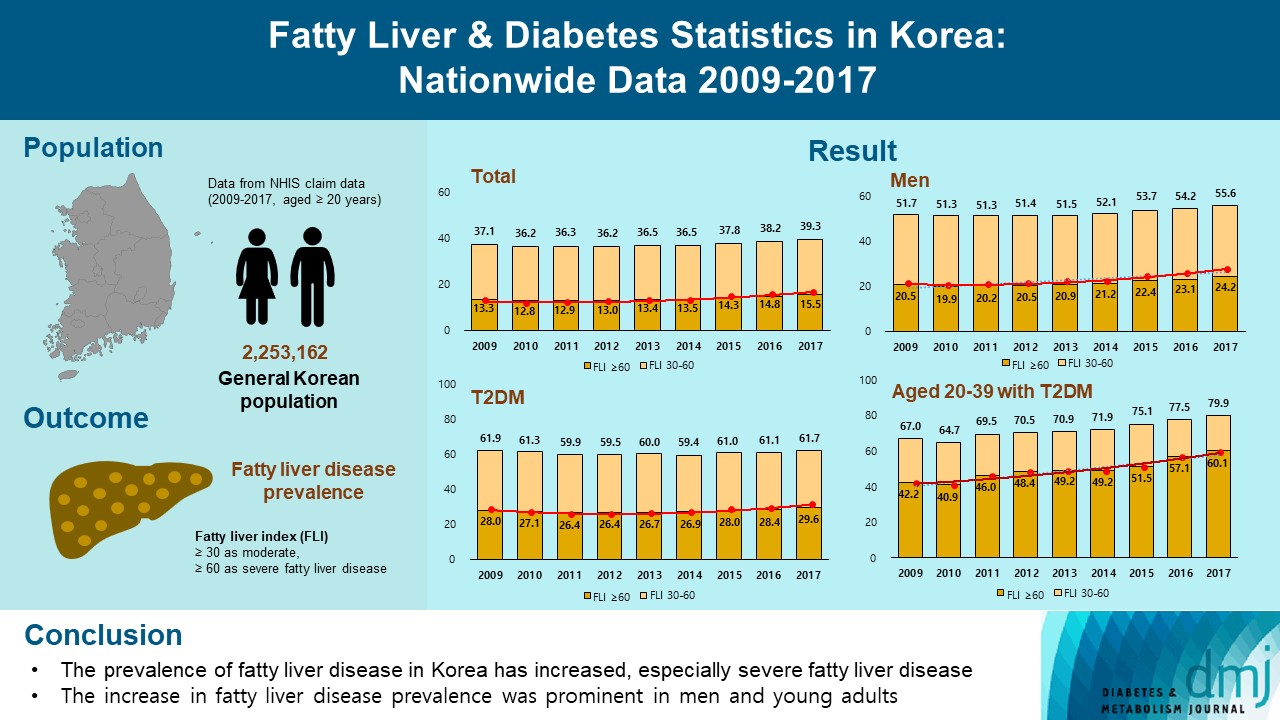
- Fatty Liver & Diabetes Statistics in Korea: Nationwide Data 2009 to 2017
- Eugene Han, Kyung-Do Han, Yong-ho Lee, Kyung-Soo Kim, Sangmo Hong, Jung Hwan Park, Cheol-Young Park, on Behalf of Fatty Liver Research Group of the Korean Diabetes Association
- Diabetes Metab J. 2023;47(3):347-355. Published online March 29, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0444
- 3,547 View
- 206 Download
- 5 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study investigated the changes of fatty liver disease prevalence in general Korean population.
Methods
This study analyzed data from the Korean National Health Insurance Service from 2009 to 2017 that included individuals aged 20 years or older who had undergone a medical health examination. Fatty liver disease was assessed using the fatty liver index (FLI). The disease severity was defined by FLI cutoff, ≥30 as moderate, and ≥60 as severe fatty liver disease.
Results
The prevalence of Korean adults aged 20 years or over with fatty liver disease (FLI ≥60) increased from 13.3% in 2009 to 15.5% in 2017 (P for trend <0.001). The increase in fatty liver disease prevalence was prominent in men (from 20.5% to 24.2%) and the young age (20 to 39 years) group (from 12.8% to 16.4%) (P for interaction <0.001). The prevalence of fatty liver disease was the highest in type 2 diabetes mellitus (T2DM, 29.6%) population compared to that of prediabetes or normoglycemia (10.0% and 21.8%) in 2017. The prevalence of fatty liver disease had statistically increased in individuals with T2DM and prediabetes (P for trend <0.001). Its prevalence increased more steeply in the young-aged population with T2DM, from 42.2% in 2009 to 60.1% in 2017. When applying a lower FLI cutoff (≥30) similar results were observed.
Conclusion
The prevalence of fatty liver disease in the Korean population has increased. Individuals who are young, male, and have T2DM are vulnerable to fatty liver disease. -
Citations
Citations to this article as recorded by- Longitudinal changes in fatty liver index are associated with risk of hepatocellular carcinoma: A nationwide cohort study in Korea
Min Gu Kang, Chang Hun Lee, Chen Shen, Jong Seung Kim, Ji Hyun Park
Journal of Hepatology.2024; 80(5): e216. CrossRef - Repeated detection of non‐alcoholic fatty liver disease increases the incidence risk of type 2 diabetes in young adults
Jin Hwa Kim, Young Sang Lyu, Mee Kyoung Kim, Sang Yong Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024; 26(1): 180. CrossRef - Mortality in metabolic dysfunction-associated steatotic liver disease: A nationwide population-based cohort study
Eugene Han, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Sang Hoon Ahn, Yong-ho Lee, Seung Up Kim
Metabolism.2024; 152: 155789. CrossRef - Association of non-alcoholic fatty liver disease with cardiovascular disease and all cause death in patients with type 2 diabetes mellitus: nationwide population based study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
BMJ.2024; : e076388. CrossRef - Hepatic Fibrosis and Cancer: The Silent Threats of Metabolic Syndrome
Scott L. Friedman
Diabetes & Metabolism Journal.2024; 48(2): 161. CrossRef - Reply to G. Wang et al
Joo-Hyun Park, Jung Yong Hong, Kyungdo Han
Journal of Clinical Oncology.2023; 41(32): 5070. CrossRef - The Role of the Fatty Liver Index (FLI) in the Management of Non-Alcoholic Fatty Liver Disease: A Systematic Review
Teodora Biciusca, Sorina Ionelia Stan, Mara Amalia Balteanu, Ramona Cioboata, Alice Elena Ghenea, Suzana Danoiu, Ana-Maria Bumbea, Viorel Biciusca
Diagnostics.2023; 13(21): 3316. CrossRef - Lean or Non-obese Nonalcoholic Fatty Liver Disease Patients: Are They Really Lean?
Eugene Han, Yong-ho Lee
Clinical and Molecular Hepatology.2023; 29(4): 980. CrossRef - Approach to Fatty Liver Disease in Patients with Type 2 Diabetes
Ji Cheol Bae
The Journal of Korean Diabetes.2023; 24(3): 107. CrossRef
- Longitudinal changes in fatty liver index are associated with risk of hepatocellular carcinoma: A nationwide cohort study in Korea
- Metabolic Risk/Epidemiology
- Rising Incidence of Diabetes in Young Adults in South Korea: A National Cohort Study
- Hyun Ho Choi, Giwoong Choi, Hojun Yoon, Kyoung Hwa Ha, Dae Jung Kim
- Diabetes Metab J. 2022;46(5):803-807. Published online January 11, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0236
- 65,535 View
- 390 Download
- 5 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - We investigated the incidence of diagnosed diabetes in South Korean adults (aged ≥20 years) by analyzing data for the National Health Insurance Service–National Sample Cohort. From 2006 to 2015, the overall incidence rate of diagnosed diabetes decreased by approximately 0.1% per year until 2015. Although, this trend was observed in individuals aged 40 years or over, the rate increased slightly in the 20–29 and 30–39 years age groups, from 0.5 to 0.7 and 2.0 to 2.6 per 1,000 individuals, respectively. The proportion of obese young adults with diabetes increased remarkably, from 51.4% in 2006 to 72.4% in 2015. Thus, young adults need early identification and weight-control strategies to prevent diabetes.
-
Citations
Citations to this article as recorded by- Cumulative exposure to hypertriglyceridemia and risk of type 2 diabetes in young adults
Min-Kyung Lee, Kyungdo Han, Bongsung Kim, Jong-Dai Kim, Moon Jung Kim, Byungpyo Kim, Jung Heo, Jiyeon Ahn, Seo-Young Sohn, Jae-Hyuk Lee
Diabetes Research and Clinical Practice.2024; 208: 111109. CrossRef - Diabetes screening in South Korea: a new estimate of the number needed to screen to detect diabetes
Kyoung Hwa Ha, Kyung Ae Lee, Kyung-Do Han, Min Kyong Moon, Dae Jung Kim
The Korean Journal of Internal Medicine.2023; 38(1): 93. CrossRef - Revisiting the Diabetes Crisis in Korea: Call for Urgent Action
Jun Sung Moon
The Journal of Korean Diabetes.2023; 24(1): 1. CrossRef - Position Statement on the Appropriateness and Significance of Adding the Glycated Hemoglobin Test to the National Health Examination
Ji Hye Kim, Dae Jung Kim, Jaehyun Kim, Sangjoon Park, Kyunghoon Lee, Jun Goo Kang, Eu Jeong Ku, Su Kyoung Kwon, Won Jun Kim, Young Sang Lyu, Jang Won Son, Young Sil Eom, Kyung Ae Lee, Jeongrim Lee, Jung Min Lee, Jung Hwa Lee, Jung Hwa Jung, Hochan Cho, Da
The Journal of Korean Diabetes.2023; 24(4): 178. CrossRef - Diabetes Fact Sheet in Korea 2021
Jae Hyun Bae, Kyung-Do Han, Seung-Hyun Ko, Ye Seul Yang, Jong Han Choi, Kyung Mook Choi, Hyuk-Sang Kwon, Kyu Chang Won
Diabetes & Metabolism Journal.2022; 46(3): 417. CrossRef - 젊은 2형 당뇨병 환자의 관리
재현 배
Public Health Weekly Report.2022; 15(35): 2474. CrossRef - Screening for Prediabetes and Diabetes in Korean Nonpregnant Adults: A Position Statement of the Korean Diabetes Association, 2022
Kyung Ae Lee, Dae Jung Kim, Kyungdo Han, Suk Chon, Min Kyong Moon
Diabetes & Metabolism Journal.2022; 46(6): 819. CrossRef
- Cumulative exposure to hypertriglyceridemia and risk of type 2 diabetes in young adults
- Cardiovascular Risk/Epidemiology
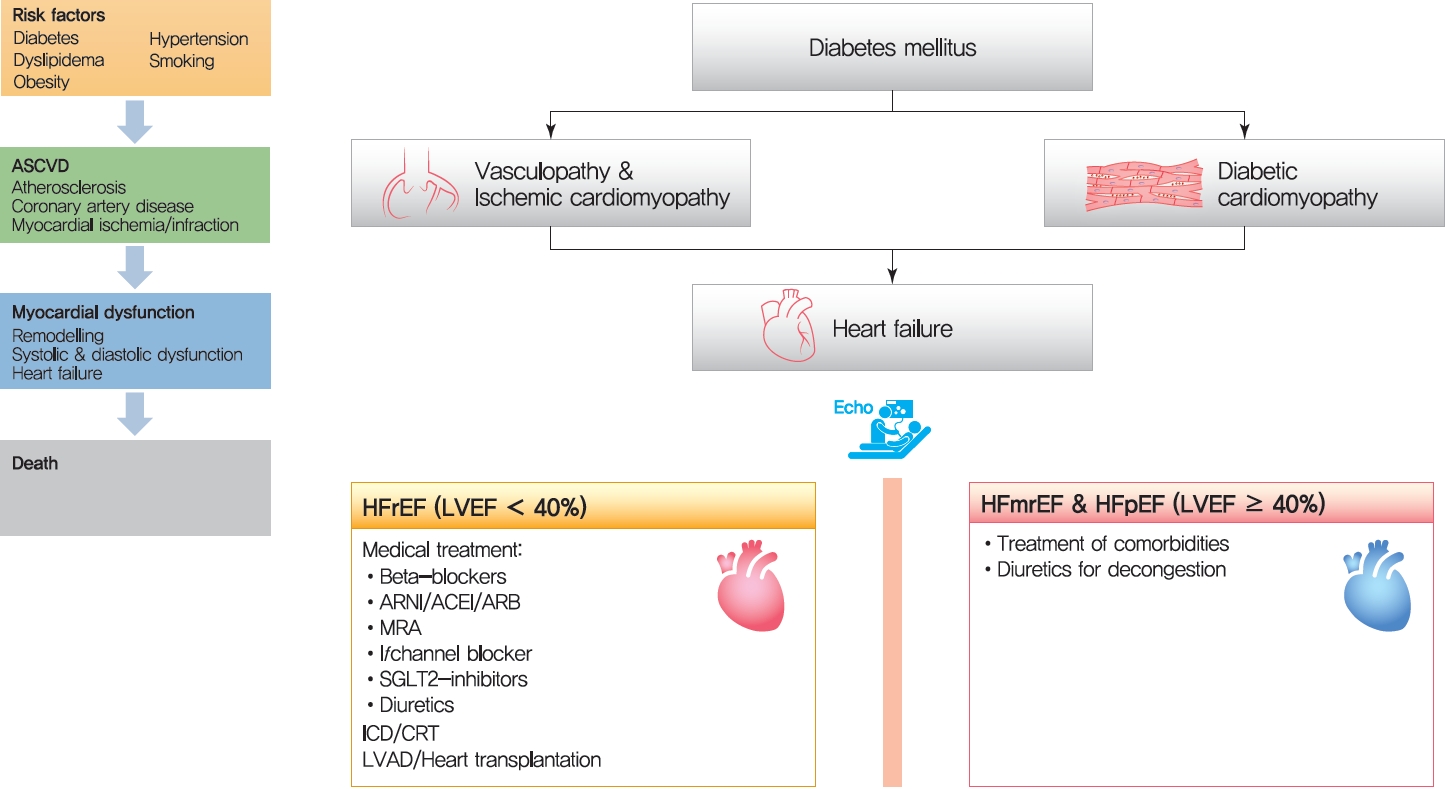
- Epidemiology, Pathophysiology, Diagnosis and Treatment of Heart Failure in Diabetes
- Jin Joo Park
- Diabetes Metab J. 2021;45(2):146-157. Published online March 25, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0282
- Correction in: Diabetes Metab J 2021;45(5):796
- 13,762 View
- 1,206 Download
- 51 Web of Science
- 54 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 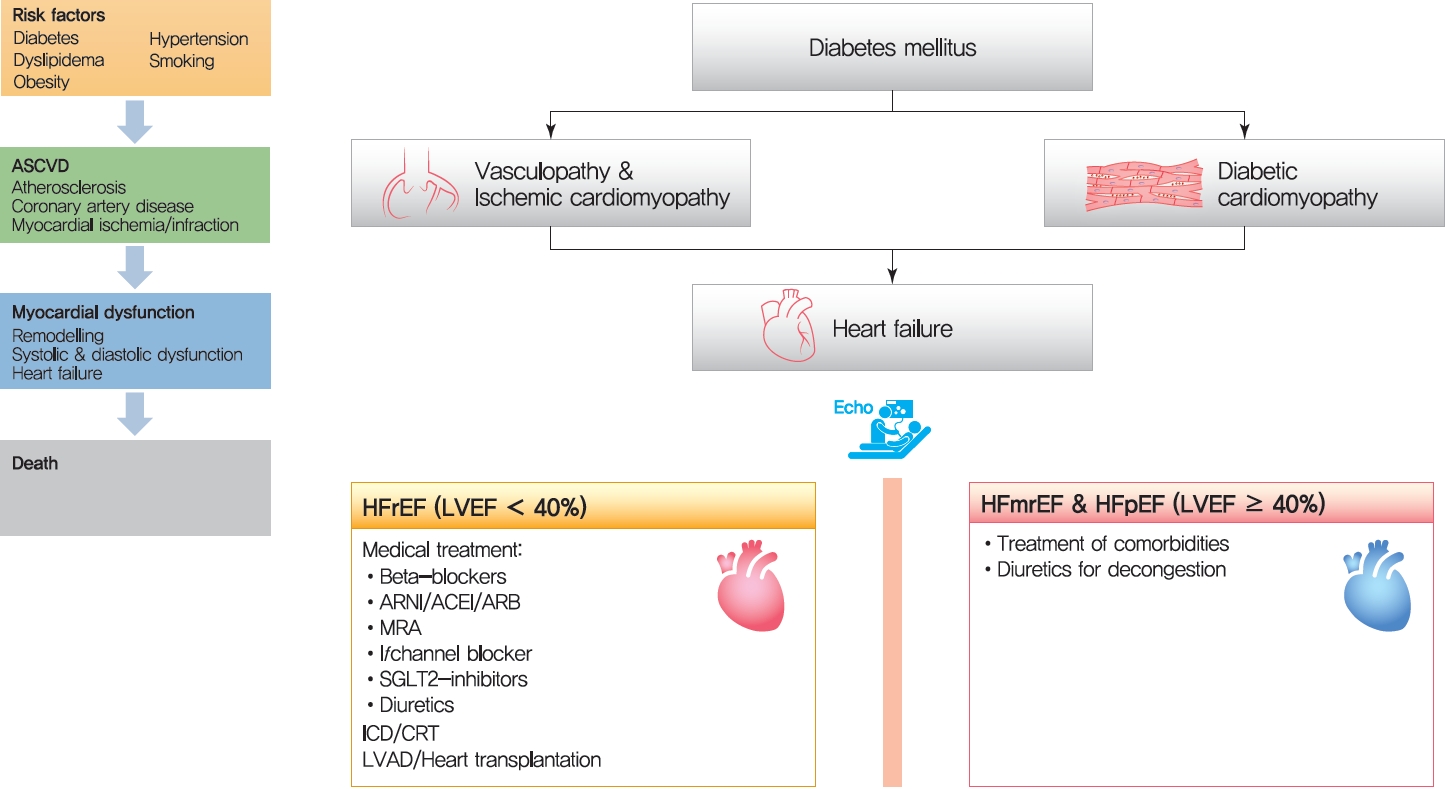
- The cardiovascular disease continuum begins with risk factors such as diabetes mellitus (DM), progresses to vasculopathy and myocardial dysfunction, and finally ends with cardiovascular death. Diabetes is associated with a 2- to 4-fold increased risk for heart failure (HF). Moreover, HF patients with DM have a worse prognosis than those without DM. Diabetes can cause myocardial ischemia via micro- and macrovasculopathy and can directly exert deleterious effects on the myocardium. Hyperglycemia, hyperinsulinemia, and insulin resistance can cause alterations in vascular homeostasis. Then, reduced nitric oxide and increased reactive oxygen species levels favor inflammation leading to atherothrombotic progression and myocardial dysfunction. The classification, diagnosis, and treatment of HF for a patient with and without DM remain the same. Until now, drugs targeting neurohumoral and metabolic pathways improved mortality and morbidity in HF with reduced ejection fraction (HFrEF). Therefore, all HFrEF patients should receive guideline-directed medical therapy. By contrast, drugs modulating neurohumoral activity did not improve survival in HF with preserved ejection fraction (HFpEF) patients. Trials investigating whether sodium-glucose cotransporter-2 inhibitors are effective in HFpEF are on-going. This review will summarize the epidemiology, pathophysiology, and treatment of HF in diabetes.
-
Citations
Citations to this article as recorded by- Efficacy of Platelet-Rich Plasma in the Treatment of Diabetic Foot Ulcers: A Systematic Review and Meta-Analysis
Yundong Peng, JiePing Wang, Xinyao Liu, Yanqing Zhou, Shaohui Jia, Jinrong Xu, Cheng Zheng
Annals of Vascular Surgery.2024; 98: 365. CrossRef - Diabetic Cardiomyopathy: 2023 Update by the International Multidisciplinary Board of Experts
Ashot Avagimyan, Federica Fogacci, Nana Pogosova, Lev Kakrurskiy, Eugenia Kogan, Olga Urazova, Zhanna Kobalava, Liudmila Mikhaleva, Rositsa Vandysheva, Gioeva Zarina, Artem Trofimenko, Grizelda Navasardyan, Lusine Mkrtchyan, Mattia Galli, Zinaida Jndoyan,
Current Problems in Cardiology.2024; 49(1): 102052. CrossRef - Emerging Biomarkers in the Laboratory and in Practice: A Novel Approach to Diagnosing Heart Failure in Diabetes
Rachel E. Aaron, Tiffany Tian, G. Alexander Fleming, David B. Sacks, James L. Januzzi, Rodica Pop-Busui, Ibrahim A. Hashim, Alan H. B. Wu, Ambarish Pandey, David C. Klonoff
Journal of Diabetes Science and Technology.2024;[Epub] CrossRef - Research Progress on the Relationship between HbA1c and Diabetes Complicated with Chronic Heart Failure
·依沙 迪达尔
Advances in Clinical Medicine.2024; 14(01): 1117. CrossRef - Association Between Use of Sodium-Glucose Cotransporter-2 Inhibitors or Angiotensin Receptor-Neprilysin Inhibitor and the Risk of Atherosclerotic Cardiovascular Disease With Coexisting Diabetes and Heart Failure
Ya-Wen Lin, Chun-Hsiang Lin, Cheng-Li Lin, Che-Huei Lin, Ming-Hung Lin
Journal of Cardiovascular Pharmacology and Therapeutics.2024;[Epub] CrossRef - The Role of Epicardial Adipose Tissue in Acute Coronary Syndromes, Post-Infarct Remodeling and Cardiac Regeneration
Kamil Krauz, Marcel Kempiński, Paweł Jańczak, Karol Momot, Maciej Zarębiński, Izabela Poprawa, Małgorzata Wojciechowska
International Journal of Molecular Sciences.2024; 25(7): 3583. CrossRef - Molecular mechanisms of metabolic dysregulation in diabetic cardiomyopathy
Yue Zeng, Yilang Li, Wenyue Jiang, Ning Hou
Frontiers in Cardiovascular Medicine.2024;[Epub] CrossRef - Association between nonalcoholic fatty liver disease and left ventricular diastolic dysfunction: A 7-year retrospective cohort study of 3,496 adults using serial echocardiography
Gyuri Kim, Tae Yang Yu, Jae Hwan Jee, Ji Cheol Bae, Mira Kang, Jae Hyeon Kim
Diabetes & Metabolism.2024; : 101534. CrossRef - SGLT2 Inhibitors in the Cardiovascular Disease
Jin Joo Park
The Journal of Korean Diabetes.2024; 25(1): 26. CrossRef - Metabolic Alteration Bridging the Prediabetic State and Colorectal Cancer
Antonino Colloca, Isabella Donisi, Camilla Anastasio, Maria Luisa Balestrieri, Nunzia D’Onofrio
Cells.2024; 13(8): 663. CrossRef - Inflammation in diabetes complications: molecular mechanisms and therapeutic interventions
Lu Zhao, Haoran Hu, Lin Zhang, Zheting Liu, Yunchao Huang, Qian Liu, Liang Jin, Meifei Zhu, Ling Zhang
MedComm.2024;[Epub] CrossRef - Methods to predict heart failure in diabetes patients
Alexander E. Berezin, Tetiana A Berezina, Uta C. Hoppe, Michael Lichtenauer, Alexander A. Berezin
Expert Review of Endocrinology & Metabolism.2024; : 1. CrossRef - Association between Dapagliflozin, Cardiac Biomarkers and Cardiac Remodeling in Patients with Diabetes Mellitus and Heart Failure
Andrew Xanthopoulos, Nikolaos Katsiadas, Spyridon Skoularigkis, Dimitrios E. Magouliotis, Niki Skopeliti, Sotirios Patsilinakos, Alexandros Briasoulis, Filippos Triposkiadis, John Skoularigis
Life.2023; 13(8): 1778. CrossRef - Empagliflozin for Patients with Heart Failure and Type 2 Diabetes Mellitus: Clinical Evidence in Comparison with Other Sodium-Glucose Co-transporter-2 Inhibitors and Potential Mechanism
Bo Liang, Rui Li, Peng Zhang, Ning Gu
Journal of Cardiovascular Translational Research.2023; 16(2): 327. CrossRef - Causes and Determinants of Heart Failure Readmissions Post Transcutaneous Aortic Valve Replacement: A Systematic Review and Meta-Analysis
Farah Yasmin, Muhammad Aamir, Abdul Moeed, Kinza Iqbal, Aymen Iqbal, Muhammad Sohaib Asghar, Waqas Ullah, Indranee Rajapreyar, Yevgeniy Brailovsky
Current Problems in Cardiology.2023; 48(1): 101428. CrossRef - Discussion of a study on the role of EMS in prognosis of elderly patients with AHF
Qingzhuo Yang, Hui Wu, Di Liu, Yunzhao Li, Gang Zhou, Dong Zhang, Yanfang Liu, Yi Li
International Journal of Cardiology.2023; 377: 91. CrossRef - The management correlation between metabolic index, cardiovascular health, and diabetes combined with cardiovascular disease
Yi Zhang, Chao Liu, Yijing Xu, Yanlei Wang, Fang Dai, Honglin Hu, Tian Jiang, Yunxia Lu, Qiu Zhang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Evaluation and Management of Patients With Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
International Journal of Heart Failure.2023; 5(1): 1. CrossRef - Evaluation and Management of Patients with Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 10. CrossRef - Lower Circulating Cell-Free Mitochondrial DNA Is Associated with Heart Failure in Type 2 Diabetes Mellitus Patients
Tetiana A. Berezina, Mykola P. Kopytsya, Olga V. Petyunina, Alexander A. Berezin, Zeljko Obradovic, Lukas Schmidbauer, Michael Lichtenauer, Alexander E. Berezin
Cardiogenetics.2023; 13(1): 15. CrossRef - Novel model predicts diastolic cardiac dysfunction in type 2 diabetes
Mingyu Hao, Xiaohong Huang, Xueting Liu, Xiaokang Fang, Haiyan Li, Lingbo Lv, Liming Zhou, Tiecheng Guo, Dewen Yan
Annals of Medicine.2023; 55(1): 766. CrossRef - Cholinergic drugs reduce metabolic inflammation and diabetic myocardial injury by regulating the gut bacterial component lipopolysaccharide‐induced ERK/Egr‐1 pathway
Qing Wu, Ming Zhao, Dongling Li, Xi He, Weijin Zang
The FASEB Journal.2023;[Epub] CrossRef - Ferroptosis: roles and molecular mechanisms in diabetic cardiomyopathy
Yangting Zhao, Binjing Pan, Xiaoyu Lv, Chongyang Chen, Kai Li, Yawen Wang, Jingfang Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Cardiorenal syndrome and diabetes: an evil pairing
Ana Belén Méndez Fernández, Ander Vergara Arana, Aleix Olivella San Emeterio, Maria Antonieta Azancot Rivero, Toni Soriano Colome, Maria Jose Soler Romeo
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Therapeutic Potential of Hibiscus sabdariffa Linn. in Attenuating Cardiovascular Risk Factors
Syaifuzah Sapian, Asma Ali Ibrahim Mze, Fatin Farhana Jubaidi, Nor Anizah Mohd Nor, Izatus Shima Taib, Zariyantey Abd Hamid, Satirah Zainalabidin, Nur Najmi Mohamad Anuar, Haliza Katas, Jalifah Latip, Juriyati Jalil, Nur Faizah Abu Bakar, Siti Balkis Budi
Pharmaceuticals.2023; 16(6): 807. CrossRef - Exploring the prospect of intrinsic wave propagation in evaluating myocardial stiffness among patients with type 2 diabetes
Qiao Cheng, Xiao Huang, Xinying Fan, Jie Sun, Jun Zhang, Qiaoying Tang, Youbin Deng, Xiaojun Bi
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - The multidimensional prognostic index (MPI) predicts long-term mortality in old type 2 diabetes mellitus patients: a 13-year follow-up study
F. Salis, E. Cossu, A. Mandas
Journal of Endocrinological Investigation.2023; 47(1): 191. CrossRef - PRDM16 exerts critical role in myocardial metabolism and energetics in type 2 diabetes induced cardiomyopathy
Tongtong Hu, Qingqing Wu, Qi Yao, Jiabin Yu, Kebing Jiang, Ying Wan, Qizhu Tang
Metabolism.2023; 146: 155658. CrossRef - Empagliflozin Reduces Interleukin-6 Levels in Patients with Heart Failure
Michael Gotzmann, Pauline Henk, Ulrik Stervbo, Arturo Blázquez-Navarro, Andreas Mügge, Nina Babel, Timm H. Westhoff
Journal of Clinical Medicine.2023; 12(13): 4458. CrossRef - Features of the course and complications of acute myocardial infarction in type 2 diabetes mellitus
M. N. Zatsepina, F. O. Ushanova, T. L. Bogacheva
FOCUS. Endocrinology.2023; 4(2): 42. CrossRef - Admission triglyceride-glucose index is predictor of long-term mortality and appropriate implantable cardiac defibrillator therapy in patients with heart failure
Kazım S Özcan, Mert İ Hayıroğlu, Tufan Çınar
Biomarkers in Medicine.2023; 17(10): 487. CrossRef - Emerging Roles of Phospholipase C Beta Isozymes as Potential Biomarkers in Cardiac Disorders
Antonietta Fazio, Camilla Evangelisti, Alessandra Cappellini, Sara Mongiorgi, Foteini-Dionysia Koufi, Irene Neri, Maria Vittoria Marvi, Michele Russo, Alessandra Ghigo, Lucia Manzoli, Roberta Fiume, Stefano Ratti
International Journal of Molecular Sciences.2023; 24(17): 13096. CrossRef - Research progress of dihydromyricetin in the treatment of diabetes mellitus
Ziyuan Wang, Zhuoran Cao, Zhiying Yue, Zhengfeng Yang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Assessment of subclinical left ventricular myocardial systolic dysfunction in type 2 diabetes mellitus patients with or without hypertension by global and segmental myocardial work
Guang-An Li, Jun Huang, Xiao Sheng, Li Fan
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Managing heart failure in diabetics with dual acting sotagliflozin—A review
Kushal Seni, Pooja A Chawla
Health Sciences Review.2023; 9: 100130. CrossRef - Association between triglyceride glucose-body mass index and heart failure in subjects with diabetes mellitus or prediabetes mellitus: a cross-sectional study
Shuping Yang, Xiangxiang Shi, Wanlu Liu, Zhaokai Wang, Ruoshui Li, Xianzhi Xu, Chaofan Wang, Lei Li, Ruili Wang, Tongda Xu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Influence of Sociodemographic Variables and Healthy Habits on the Values of Insulin Resistance Indicators in 386,924 Spanish Workers
Miguel Mestre Font, Carla Busquets-Cortés, José Ignacio Ramírez-Manent, Pilar Tomás-Gil, Hernán Paublini, Ángel Arturo López-González
Nutrients.2023; 15(24): 5122. CrossRef - The effect of dapagliflozin on ventricular arrhythmias, cardiac arrest, or sudden death in people with heart failure: a tick in another box for sodium-glucose cotransporter 2 inhibitors
Theocharis Koufakis, George Giannakoulas, Pantelis Zebekakis, Kalliopi Kotsa
Expert Opinion on Pharmacotherapy.2022; 23(3): 321. CrossRef - The peculiar role of vitamin D in the pathophysiology of cardiovascular and neurodegenerative diseases
Milijana Janjusevic, Giulia Gagno, Alessandra Lucia Fluca, Laura Padoan, Antonio Paolo Beltrami, Gianfranco Sinagra, Rita Moretti, Aneta Aleksova
Life Sciences.2022; 289: 120193. CrossRef - Mechanisms of cardiac dysfunction in diabetic cardiomyopathy: molecular abnormalities and phenotypical variants
Francesca Romana Prandi, Isabella Evangelista, Domenico Sergi, Alberto Palazzuoli, Francesco Romeo
Heart Failure Reviews.2022; 28(3): 597. CrossRef - Modern Approaches to Treatment of Chronic Heart Failure in Patients with Type 2 Diabetes Mellitus
Yu. G. Gorb, S. A. Serik, O. V. Tkachenko, V. V. Ryabukha
Ukraïnsʹkij žurnal medicini, bìologìï ta sportu.2022; 7(1): 14. CrossRef - Metabonomic Characteristics of Myocardial Diastolic Dysfunction in Type 2 Diabetic Cardiomyopathy Patients
Mingyu Hao, Jianxin Deng, Xiaohong Huang, Haiyan Li, Huiting Ou, Xiangsheng Cai, Jiajie She, Xueting Liu, Ling Chen, Shujuan Chen, Wenlan Liu, Dewen Yan
Frontiers in Physiology.2022;[Epub] CrossRef - Serum Levels of Irisin Predict Cumulative Clinical Outcomes in Heart Failure Patients With Type 2 Diabetes Mellitus
Alexander A. Berezin, Michael Lichtenauer, Elke Boxhammer, Ivan M. Fushtey, Alexander E. Berezin
Frontiers in Physiology.2022;[Epub] CrossRef - Heart Failure: An Underappreciated Complication of Diabetes. A Consensus Report of the American Diabetes Association
Rodica Pop-Busui, James L. Januzzi, Dennis Bruemmer, Sonia Butalia, Jennifer B. Green, William B. Horton, Colette Knight, Moshe Levi, Neda Rasouli, Caroline R. Richardson
Diabetes Care.2022; 45(7): 1670. CrossRef - Von Willebrand factor (vWF) in patients with heart failure with preserved ejection fraction (HFpEF): A retrospective observational study
Mayila Abudoukelimu, Bayinsilema Ba, Yan Kai Guo, Jie Xu
Medicine.2022; 101(31): e29854. CrossRef - Why Does the Intravenous Iron Supplementation Not Work in Heart Failure Patients on Hemodialysis?
Jin Joo Park
CardioMetabolic Syndrome Journal.2022; 2(2): 176. CrossRef - Severe hypoglycemia and risk of hospitalization for heart failure in adults with diabetes treated with oral medications with or without insulin: A population-based study
You-Bin Lee, Yoon-Jong Bae, Hoseob Kim, Jiyun Park, So Yoon Kwon, So Hee Park, Gyuri Kim, Kyu Yeon Hur, Jae Hyeon Kim, Sang-Man Jin
Diabetes Research and Clinical Practice.2022; 192: 110083. CrossRef - Blood Pressure Target in Type 2 Diabetes Mellitus
Hyun-Jin Kim, Kwang-il Kim
Diabetes & Metabolism Journal.2022; 46(5): 667. CrossRef - Application Value of Systemic Inflammatory Indexes in the Clinical Evaluation of Patients with Heart Failure with Preserved Ejection Fraction (HFpEF)
Ruxin Wang, Juan Wu, Haowen Ye, Xiaofang Zhang, Lihong Wang
Medicina.2022; 58(10): 1473. CrossRef - HFpEF and Atrial Fibrillation: The Enigmatic Interplay of Dysmetabolism, Biomarkers, and Vascular Endothelial Dysfunction
Jure Bosanac, Lara Straus, Marko Novaković, Daniel Košuta, Mojca Božič Mijovski, Jerneja Tasič, Borut Jug, Azizah Ugusman
Disease Markers.2022; 2022: 1. CrossRef - The importance of caveolin as a target in the prevention and treatment of diabetic cardiomyopathy
Weiyi Xia, Xia Li, Qingping Wu, Aimin Xu, Liangqing Zhang, Zhengyuan Xia
Frontiers in Immunology.2022;[Epub] CrossRef - Microvascular Burden and Incident Heart Failure Among Middle-Aged and Older Adults With Type 1 or Type 2 Diabetes
Fu-Rong Li, Daniel Nyarko Hukportie, Jing Yang, Huan-Huan Yang, Guo-Chong Chen, Xian-Bo Wu
Diabetes Care.2022; 45(12): 2999. CrossRef - C-reactive protein and statins in heart failure with reduced and preserved ejection fraction
Jin Joo Park, Minjae Yoon, Hyoung-Won Cho, Hyun-Jai Cho, Kye Hun Kim, Dong Heon Yang, Byung-Su Yoo, Seok-Min Kang, Sang Hong Baek, Eun-Seok Jeon, Jae-Joong Kim, Myeong-Chan Cho, Shung Chull Chae, Byung-Hee Oh, Dong-Ju Choi
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Pharmacological treatment of type 2 diabetes in elderly patients with heart failure: randomized trials and beyond
Angela Sciacqua, Elena Succurro, Giuseppe Armentaro, Sofia Miceli, Daniele Pastori, Giuseppe Rengo, Giorgio Sesti
Heart Failure Reviews.2021; 28(3): 667. CrossRef
- Efficacy of Platelet-Rich Plasma in the Treatment of Diabetic Foot Ulcers: A Systematic Review and Meta-Analysis
- Complications
- Trends in Cardiovascular Complications and Mortality among Patients with Diabetes in South Korea
- Jung Hwan Park, Kyoung Hwa Ha, Bo Yeon Kim, Jae Hyuk Lee, Dae Jung Kim
- Diabetes Metab J. 2021;45(1):120-124. Published online December 9, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0175
- Correction in: Diabetes Metab J 2021;45(2):283
- 11,792 View
- 352 Download
- 32 Web of Science
- 37 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 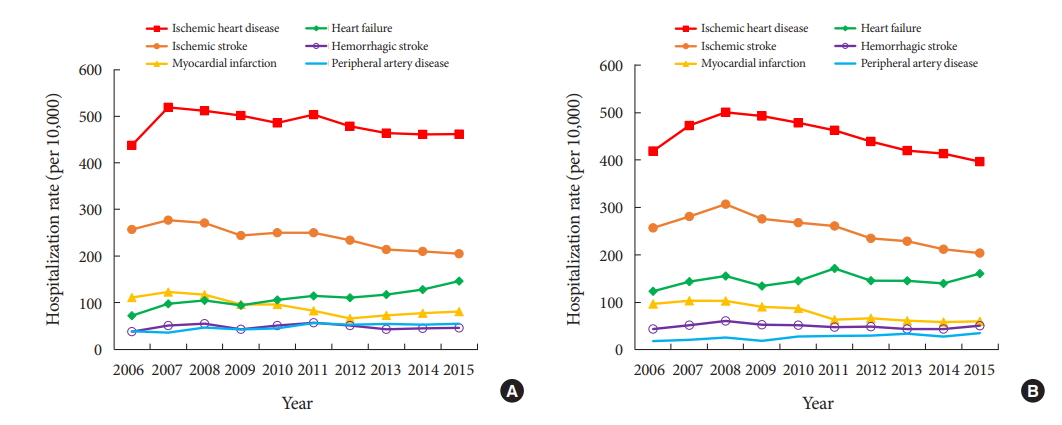
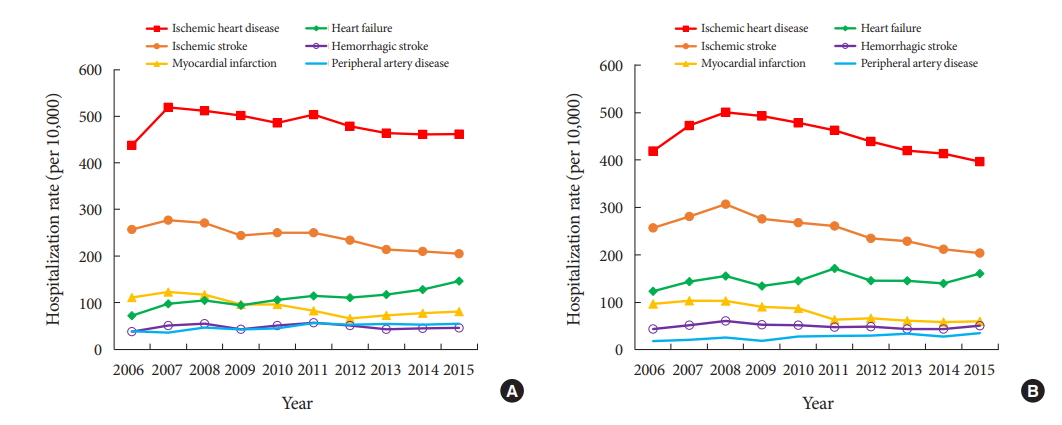
- We investigated the cardiovascular complications and mortality rates of patients with diabetes in South Korea. The rates of hospitalization due to cardiovascular complications and mortality were analyzed using the Korean National Health Insurance Service-National Sample Cohort. From 2006 to 2015, the rates of hospitalization due to major cardiovascular complications decreased, while those due to heart failure (from 72 to 146 and 124 to 161 per 10,000 men and women, respectively) and peripheral artery disease (from 39 to 55 and 19 to 35 per 10,000 men and women, respectively) increased. In the period 2007 to 2015, the mortality rates for cancer, cerebrovascular disease, diabetes, heart disease, and hypertensive disease all decreased. However, the mortality rate for pneumonia increased. We observed a continuous reduction in cardiovascular complications and mortality in adults with diabetes. However, with the increase in some diabetes complications, more efforts are needed to prevent diabetes complications.
-
Citations
Citations to this article as recorded by- Risk factor control and cardiovascular events in patients with type 2 diabetes mellitus
Do Kyeong Song, Young Sun Hong, Yeon-Ah Sung, Hyejin Lee, Hidetaka Hamasaki
PLOS ONE.2024; 19(2): e0299035. CrossRef - Remnant cholesterol is an independent risk factor for the incidence of chronic kidney disease in newly-diagnosed type 2 diabetes: A nationwide population-based study
Soo Yeon Jang, Minwoong Kang, Eyun Song, Ahreum Jang, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
Diabetes Research and Clinical Practice.2024; 210: 111639. CrossRef - Global trends in the incidence of hospital admissions for diabetes-related foot disease and amputations: a review of national rates in the 21st century
Peter A. Lazzarini, Susanna M. Cramb, Jonathan Golledge, Jedidiah I. Morton, Dianna J. Magliano, Jaap J. Van Netten
Diabetologia.2023; 66(2): 267. CrossRef - Inequalities in cancer mortality trends in people with type 2 diabetes: 20 year population-based study in England
Suping Ling, Francesco Zaccardi, Eyad Issa, Melanie J. Davies, Kamlesh Khunti, Karen Brown
Diabetologia.2023; 66(4): 657. CrossRef - Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - Evaluation and Management of Patients With Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
International Journal of Heart Failure.2023; 5(1): 1. CrossRef - Empagliflozin is associated with lower risk of cardiovascular events and all‐cause mortality in routine care in East Asia: Results from the EMPRISE study
Dae Jung Kim, Wayne H‐H Sheu, Wook‐Jin Chung, Daisuke Yabe, Kyoung Hwa Ha, Masaomi Nangaku, Elise Chia‐Hui Tan, Koichi Node, Atsutaka Yasui, Weiyu Lei, Sunwoo Lee, Laura Saarelainen, Anouk Deruaz‐Luyet, Moe H Kyaw, Yutaka Seino
Journal of Diabetes Investigation.2023; 14(3): 417. CrossRef - Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Evaluation and Management of Patients with Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 10. CrossRef - The effect of metabolic dysfunction-associated fatty liver disease and diabetic kidney disease on the risk of hospitalization of heart failure in type 2 diabetes: a retrospective cohort study
Seung Eun Lee, Juhwan Yoo, Bong-Seong Kim, Han Seok Choi, Kyungdo Han, Kyoung-Ah Kim
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Comparison of Operational Definition of Type 2 Diabetes Mellitus Based on Data from Korean National Health Insurance Service and Korea National Health and Nutrition Examination Survey
Jong Ha Baek, Yong-Moon Park, Kyung Do Han, Min Kyong Moon, Jong Han Choi, Seung-Hyun Ko
Diabetes & Metabolism Journal.2023; 47(2): 201. CrossRef - Chronic disease management program applied to type 2 diabetes patients and prevention of diabetic complications: a retrospective cohort study using nationwide data
Min Kyung Hyun, Jang Won Lee, Seung-Hyun Ko
BMC Public Health.2023;[Epub] CrossRef - The Present and Future of Artificial Intelligence-Based Medical Image in Diabetes Mellitus: Focus on Analytical Methods and Limitations of Clinical Use
Ji-Won Chun, Hun-Sung Kim
Journal of Korean Medical Science.2023;[Epub] CrossRef - The Role of Echocardiography in Evaluating Cardiovascular Diseases in Patients with Diabetes Mellitus
Sun Hwa Lee, Jae-Hyeong Park
Diabetes & Metabolism Journal.2023; 47(4): 470. CrossRef - Long-term Effectiveness of the National Diabetes Quality Assessment Program in South Korea
Ji Hye Huh, Serim Kwon, Gui Ok Kim, Bo Yeon Kim, Kyoung Hwa Ha, Dae Jung Kim
Diabetes Care.2023; 46(9): 1700. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk Factors
Ye Seul Yang
The Journal of Korean Diabetes.2023; 24(3): 135. CrossRef - Interpreting global trends in type 2 diabetes complications and mortality
Mohammed K. Ali, Jonathan Pearson-Stuttard, Elizabeth Selvin, Edward W. Gregg
Diabetologia.2022; 65(1): 3. CrossRef - Cardiovascular disease in patients with type 2 diabetes
Ja Young Jeon, Dae Jung Kim
Journal of Diabetes Investigation.2022; 13(4): 614. CrossRef - Effects of physical activity on cardiovascular outcomes and mortality in Korean patients with diabetes: a nationwide population-based cohort study
Inha Jung, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Prevention and Pharmacotherapy.2022; 4(1): 42. CrossRef - Editorial: Management of Diabetes and its Complications: A Focus on Endothelial Dysfunction
Shanhu Qiu, Jianhua Ma, Tongzhi Wu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Smoking, Metabolic Syndrome, and Cardiovascular Disease
Seo Young Kang
Korean Journal of Family Practice.2022; 12(2): 59. CrossRef - Cardiovascular disease in type 2 diabetes mellitus: progress toward personalized management
Cheng-Xu Ma, Xiao-Ni Ma, Cong-Hui Guan, Ying-Dong Li, Dídac Mauricio, Song-Bo Fu
Cardiovascular Diabetology.2022;[Epub] CrossRef - Adherence to healthy lifestyle behaviors as a preventable risk factor for severe hypoglycemia in people with type 2 diabetes: A longitudinal nationwide cohort study
Jae‐Seung Yun, Kyungdo Han, Yong‐Moon Park, Eugene Han, Yong‐ho Lee, Seung‐Hyun Ko
Journal of Diabetes Investigation.2022; 13(9): 1533. CrossRef - Current Status of Low-Density Lipoprotein Cholesterol Target Achievement in Patients with Type 2 Diabetes Mellitus in Korea Compared with Recent Guidelines
Soo Jin Yun, In-Kyung Jeong, Jin-Hye Cha, Juneyoung Lee, Ho Chan Cho, Sung Hee Choi, SungWan Chun, Hyun Jeong Jeon, Ho-Cheol Kang, Sang Soo Kim, Seung-Hyun Ko, Gwanpyo Koh, Su Kyoung Kwon, Jae Hyuk Lee, Min Kyong Moon, Junghyun Noh, Cheol-Young Park, Sung
Diabetes & Metabolism Journal.2022; 46(3): 464. CrossRef - Diabetes Fact Sheet in Korea 2021
Jae Hyun Bae, Kyung-Do Han, Seung-Hyun Ko, Ye Seul Yang, Jong Han Choi, Kyung Mook Choi, Hyuk-Sang Kwon, Kyu Chang Won
Diabetes & Metabolism Journal.2022; 46(3): 417. CrossRef - Advanced Glycation End Products and Their Effect on Vascular Complications in Type 2 Diabetes Mellitus
Jeongmin Lee, Jae-Seung Yun, Seung-Hyun Ko
Nutrients.2022; 14(15): 3086. CrossRef - Renoprotective Mechanism of Sodium-Glucose Cotransporter 2 Inhibitors: Focusing on Renal Hemodynamics
Nam Hoon Kim, Nan Hee Kim
Diabetes & Metabolism Journal.2022; 46(4): 543. CrossRef - Association between carotid atherosclerosis and presence of intracranial atherosclerosis using three-dimensional high-resolution vessel wall magnetic resonance imaging in asymptomatic patients with type 2 diabetes
Ji Eun Jun, You-Cheol Hwang, Kyu Jeong Ahn, Ho Yeon Chung, Geon-Ho Jahng, Soonchan Park, In-Kyung Jeong, Chang-Woo Ryu
Diabetes Research and Clinical Practice.2022; 191: 110067. CrossRef - Blood Pressure Target in Type 2 Diabetes Mellitus
Hyun-Jin Kim, Kwang-il Kim
Diabetes & Metabolism Journal.2022; 46(5): 667. CrossRef - Fenofibrate add-on to statin treatment is associated with low all-cause death and cardiovascular disease in the general population with high triglyceride levels
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Metabolism.2022; 137: 155327. CrossRef - Trends in diabetes-related complications in Singapore, 2013–2020: A registry-based study
Joshua Kuan Tan, Nur Nasyitah Mohamed Salim, Gek Hsiang Lim, Sing Yi Chia, Julian Thumboo, Yong Mong Bee, Ferdinando Carlo Sasso
PLOS ONE.2022; 17(10): e0275920. CrossRef - Association between the Diabetes Drug Cost and Cardiovascular Events and Death in Korea: A National Health Insurance Service Database Analysis
Seung Min Chung, Ji-In Lee, Eugene Han, Hyun-Ae Seo, Eonju Jeon, Hye Soon Kim, Ji Sung Yoon
Endocrinology and Metabolism.2022; 37(5): 759. CrossRef - Impact of hypoglycemia at the time of hospitalization for heart failure from emergency department on major adverse cardiovascular events in patients with and without type 2 diabetes
Seon-Ah Cha, Jae-Seung Yun, Gee-Hee Kim, Yu-Bae Ahn
Cardiovascular Diabetology.2022;[Epub] CrossRef - Heart Failure and Diabetes Mellitus: Dangerous Liaisons
Hae-Young Lee
International Journal of Heart Failure.2022; 4(4): 163. CrossRef - Diabetes and Stroke
Junghyun Noh
The Journal of Korean Diabetes.2021; 22(1): 26. CrossRef - Current trends in epidemiology of cardiovascular disease and cardiovascular risk management in type 2 diabetes
Jae-Seung Yun, Seung-Hyun Ko
Metabolism.2021; 123: 154838. CrossRef
- Risk factor control and cardiovascular events in patients with type 2 diabetes mellitus
- Type 1 Diabetes
- Incidence and Prevalence of Type 1 Diabetes Mellitus among Korean Children and Adolescents between 2007 and 2017: An Epidemiologic Study Based on a National Database
- Hyun Wook Chae, Gi Hyeon Seo, Kyungchul Song, Han Saem Choi, Junghwan Suh, Ahreum Kwon, Sangmi Ha, Ho-Seong Kim
- Diabetes Metab J. 2020;44(6):866-874. Published online November 4, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0212
- 7,738 View
- 319 Download
- 25 Web of Science
- 29 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
The incidence of type 1 diabetes mellitus (T1DM) among children is high in Europe and the USA and relatively low in Asia, including Korea. The present study aimed to investigate the incidence and prevalence of childhood-onset T1DM in Korea and examine trends in incidence.
Methods
This study was conducted using the national registry data provided by the Health Insurance Review and Assessment Service in Korea from 2007 to 2017. We included children aged 0 to 14 years who were newly registered with a T1DM diagnosis each year (code E10).
Results
A total of 29,013 children were registered. The overall incidence of T1DM was 4.45 per 100,000 persons (girls, 4.93; boys, 4.01). The overall incidence of childhood-onset T1DM in Korea increased from 3.70 in 2008 to 4.77 in 2016 (P=0.002). The incidence of T1DM increased from 3.07 in 2008 to 4.89 in 2016 (P<0.001) among boys. Although the incidence of the disease increased significantly among boys aged 5–9 and 10–14 years, it remained constant among girls (4.39 in 2008, 4.64 in 2016). The overall prevalence of childhood-onset T1DM in Korea increased from 32.85 in 2007 to 41.03 per 100,000 persons in 2017 (girls, 35.54 to 43.88; boys, 32.85 to 41.03).
Conclusion
We calculated relatively accurate incidence and prevalence of childhood-onset T1DM from a nation-based registry. The incidence increased by 3% to 4% every year from 2007 to 2017. The increasing trend is noteworthy compared with previous reports. -
Citations
Citations to this article as recorded by- Risk of non-thyroidal autoimmune diseases in patients with Graves’ disease: a nationwide retrospective cohort study
Seo Young Sohn, Jiyeon Ahn, Min Kyung Lee, Jae Hyuk Lee, Ji-Won Kwon, Ji-Min Kweon, Ju-Yeun Lee
Rheumatology.2024;[Epub] CrossRef - Effectiveness of Non-pharmacological Interventions for Adolescents With Type 1 Diabetes in the Last Five Years: A Systematic Review and Meta-analysis
DaeEun Lee, Haejung Lee, YoonYoung Shin, Gaeun Park
Asian Nursing Research.2024; 18(1): 51. CrossRef - Development and Testing of the School Healthcare Partnership Scale for Parents
Ju-Yeon Uhm, Suhee Kim
Western Journal of Nursing Research.2024; 46(3): 219. CrossRef - Trends in incidence rates of childhood type 1 diabetes mellitus: A retrospective study in Isfahan province, Iran
Mahin Hashemipour, Mohammadreza Maracy, Shaghayegh Haghjooy Javanmard, Farzane Zamaneh, Neda Mostofizadeh, Silva Hovsepian
Journal of Diabetes Investigation.2023; 14(3): 376. CrossRef - Incidence of Childhood Type 1 Diabetes in Beijing During 2011–2020 and Predicted Incidence for 2025–2035: A Multicenter, Hospitalization-Based Study
Yuchuan Li, Kun Qian, Di Wu, Xinli Wang, Hong Cui, Geheng Yuan, Jinfang Yuan, Lijun Yang, Liya Wei, Bingyan Cao, Chang Su, Xuejun Liang, Min Liu, Wenjing Li, Miao Qin, Jiajia Chen, Xi Meng, Rui Wang, Shan Su, Xiaobo Chen, Hui Chen, Chunxiu Gong
Diabetes Therapy.2023; 14(3): 519. CrossRef - Utilization of nutrition labels and related factors among patients with diabetes in Korea
So-Jung Lee, Mi Ah Han, Jong Park, So Yeon Ryu
Nutrition Research and Practice.2023; 17(2): 297. CrossRef - Long-term trends of pediatric type 1 diabetes incidence in Japan before and after the COVID-19 pandemic
Fumika Matsuda, Tomoyo Itonaga, Miwako Maeda, Kenji Ihara
Scientific Reports.2023;[Epub] CrossRef - The burdens faced by parents of preschoolers with type 1 diabetes mellitus: an integrative review
Sunyeob Choi, Hyewon Shin
Child Health Nursing Research.2023; 29(3): 166. CrossRef - Hypoglycemic Effect of an Herbal Decoction (Modified Gangsimtang) in a Patient with Severe Type 2 Diabetes Mellitus Refusing Oral Anti-Diabetic Medication: A Case Report
Sungjun Joo, Hyonjun Chun, Jisu Lee, Seungmin Seo, Jungmin Lee, Jungtae Leem
Medicina.2023; 59(11): 1919. CrossRef - Improving self-management and diabetes indicators in adolescents with type 1 diabetes through self-care education
Narges Asghari, Bahman Dashtebozorgi, Shahnaz Rostami, Saeed Ghanbari, Kourosh Riahi-Ghahfarokhi
Journal of Family Medicine and Primary Care.2023; 12(10): 2322. CrossRef - Механізм дії та особливості застосування холекальциферолу в дітей та підлітків на етапах розвитку цукрового діабету 1-го типу
V.V. Popova, N.V. Het´man, Ya.I. Labanets, H.V. Kulikovs´ka, O.V. Furmanova, K.P. Zak
Endokrynologia.2023; 28(1): 36. CrossRef - Comparison of Initial Presentation of Pediatric Diabetes Before and During the Coronavirus Disease 2019 Pandemic Era
Yoonha Lee, Minseung Kim, Kyeongeun Oh, Eungu Kang, Young-Jun Rhie, Jieun Lee, Yong Hee Hong, Young-Lim Shin, Jae Hyun Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef - Recent information on test utilization and intraindividual change in anti-glutamic acid decarboxylase antibody in Korea: a retrospective study
Rihwa Choi, Wonseo Park, Gayoung Chun, Jiwon Lee, Sang Gon Lee, Eun Hee Lee
BMJ Open Diabetes Research & Care.2022; 10(3): e002739. CrossRef - Comparison of the clinical characteristics and outcomes of pediatric patients with and without diabetic ketoacidosis at the time of type 1 diabetes diagnosis
Young-Jun Seo, Chang Dae Kum, Jung Gi Rho, Young Suk Shim, Hae Sang Lee, Jin Soon Hwang
Annals of Pediatric Endocrinology & Metabolism.2022; 27(2): 126. CrossRef - Prevalence trends of type 1 and type 2 diabetes in children and adolescents in North Rhine-Westphalia, the most populous federal state in Germany, 2002-2020
C. Baechle, A. Stahl-Pehe, N. Prinz, T. Meissner, C. Kamrath, R.W. Holl, J. Rosenbauer
Diabetes Research and Clinical Practice.2022; 190: 109995. CrossRef - Diabetic ketoacidosis in children with new-onset type 1 diabetes mellitus: demographics, risk factors and outcome: an 11 year review in Hong Kong
Sarah Wing-yiu Poon, Joanna Yuet-ling Tung, Wilfred Hing-sang Wong, Pik-to Cheung, Antony Chun-cheung Fu, Gloria Shir-wey Pang, Sharon Wing-yan To, Lap-ming Wong, Wai-yu Wong, Suk-yan Chan, Ho-chung Yau, Wing-shan See, Betty Wai-man But, Shirley Man-yee W
Journal of Pediatric Endocrinology and Metabolism.2022; 35(9): 1132. CrossRef - School Nurse–Parent Partnership in School Health Care for Children with Type 1 Diabetes: A Hybrid Method Concept Analysis
Ju-Yeon Uhm, Mi-Young Choi
Asian Nursing Research.2022; 16(5): 282. CrossRef - Increased Incidence of Pediatric Diabetic Ketoacidosis After COVID-19: A Two-Center Retrospective Study in Korea
Min Jeong Han, Jun Ho Heo
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 783. CrossRef - Age at Diagnosis and the Risk of Diabetic Nephropathy in Young Patients with Type 1 Diabetes Mellitus (Diabetes Metab J 2021;45:46-54)
Ye Seul Yang, Tae Seo Sohn
Diabetes & Metabolism Journal.2021; 45(2): 277. CrossRef - Relationships between emissions of toxic airborne molecules and type 1 diabetes incidence in children: An ecologic study
Agostino Di Ciaula, Piero Portincasa
World Journal of Diabetes.2021; 12(5): 673. CrossRef - Diagnosis and management of pediatric type 1 diabetes mellitus
Jieun Lee
Journal of the Korean Medical Association.2021; 64(6): 425. CrossRef - Diabetes in Adolescence, Appropriate Transition to Adult Clinic
Jieun Lee, Jae Hyun Kim
The Journal of Korean Diabetes.2021; 22(2): 77. CrossRef - Trajectories in glycated hemoglobin and body mass index in children and adolescents with diabetes using the common data model
Yun Jeong Lee, Sooyoung Yoo, Soyoung Yi, Seok Kim, Chunggak Lee, Jihoon Cho, Soyeon Ahn, Sunkyu Choi, Hee Hwang, Young Ah Lee, Choong Ho Shin, Hyung-Jin Yoon, Kwangsoo Kim, Eunhye Song, Jin Ho Choi, Han Wook Yoo, Young-Hak Kim, Ji Seon Oh, Eun-Ae Kang, Ga
Scientific Reports.2021;[Epub] CrossRef - What Affects Quality of Life for People with Type 1 Diabetes?: A Cross-Sectional Observational Study
Mi-Kyoung Cho, Mi-Young Kim
International Journal of Environmental Research and Public Health.2021; 18(14): 7623. CrossRef - The Relationship between Diabetes Family Conflict and Parental Conflict on Problem Recognition in Illness Self-Management among Individuals with Type 1 Diabetes Mellitus
Mi-Kyoung Cho, Mi Young Kim
International Journal of Environmental Research and Public Health.2021; 18(17): 8914. CrossRef - Relationship between Diabetes Family Conflicts or Problem Recognition in Illness Self-Management and Quality of Life of Adolescents with T1DM and Their Parents
Mi-Kyoung Cho, Mi Young Kim
International Journal of Environmental Research and Public Health.2021; 18(20): 10710. CrossRef - Current Advances of Artificial Pancreas Systems: A Comprehensive Review of the Clinical Evidence
Sun Joon Moon, Inha Jung, Cheol-Young Park
Diabetes & Metabolism Journal.2021; 45(6): 813. CrossRef - History of insulin treatment of pediatric patients with diabetes in Korea
Jae Hyun Kim, Choong Ho Shin, Sei Won Yang
Annals of Pediatric Endocrinology & Metabolism.2021; 26(4): 237. CrossRef - A Position Statement of the Utilization and Support Status of Continuous Glucose Monitoring in Korea
Won Jun Kim, Jae Hyun Kim, Hye Jin Yoo, Jang Won Son, Ah Reum Khang, Su Kyoung Kwon, Ji Hye Kim, Tae Ho Kim, Ohk Hyun Ryu, Kyeong Hye Park, Sun Ok Song, Kang-Woo Lee, Woo Je Lee, Jung Hwa Jung, Ho-Chan Cho, Min Jeong Gu, Jeongrim Lee, Dal Lae Ju, Yeon Hee
The Journal of Korean Diabetes.2021; 22(4): 225. CrossRef
- Risk of non-thyroidal autoimmune diseases in patients with Graves’ disease: a nationwide retrospective cohort study
- Metabolic Risk/Epidemiology
- The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea
- Hoon Sung Choi, Sung Woo Lee, Jin Taek Kim, Hong Kyu Lee
- Diabetes Metab J. 2020;44(5):699-710. Published online April 16, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0109
- 6,135 View
- 104 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background We sought to explore whether reduced pulmonary function is an independent risk factor for incident diabetes in Koreans.
Methods We conducted a prospective cohort study of pulmonary function as a risk factor for incident diabetes using 10-year follow-up data from 3,864 middle-aged adults from the Ansung cohort study in Korea. The incidence of diabetes was assessed using both oral glucose tolerance tests and glycosylated hemoglobin levels.
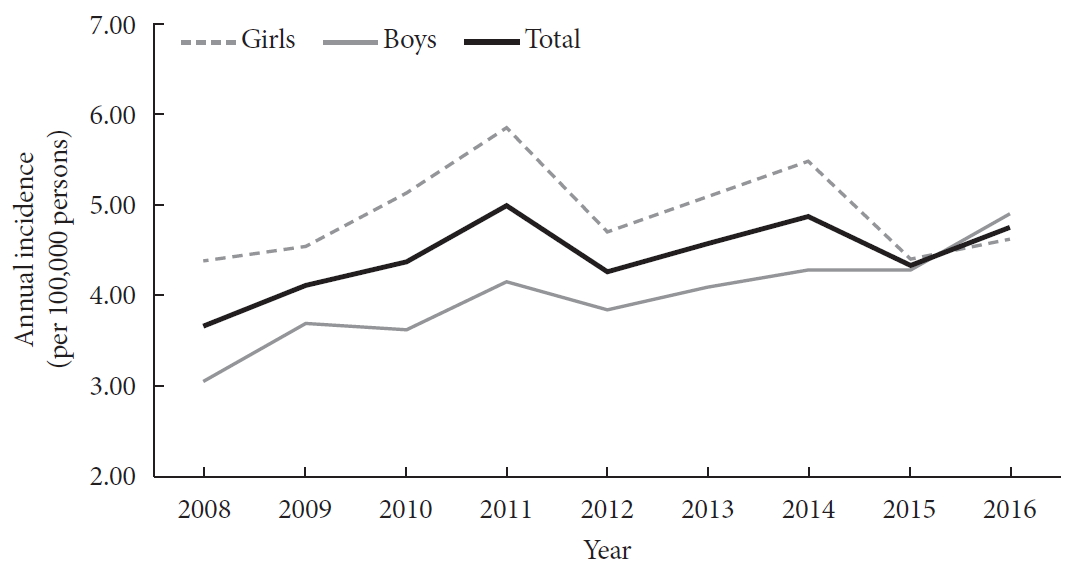
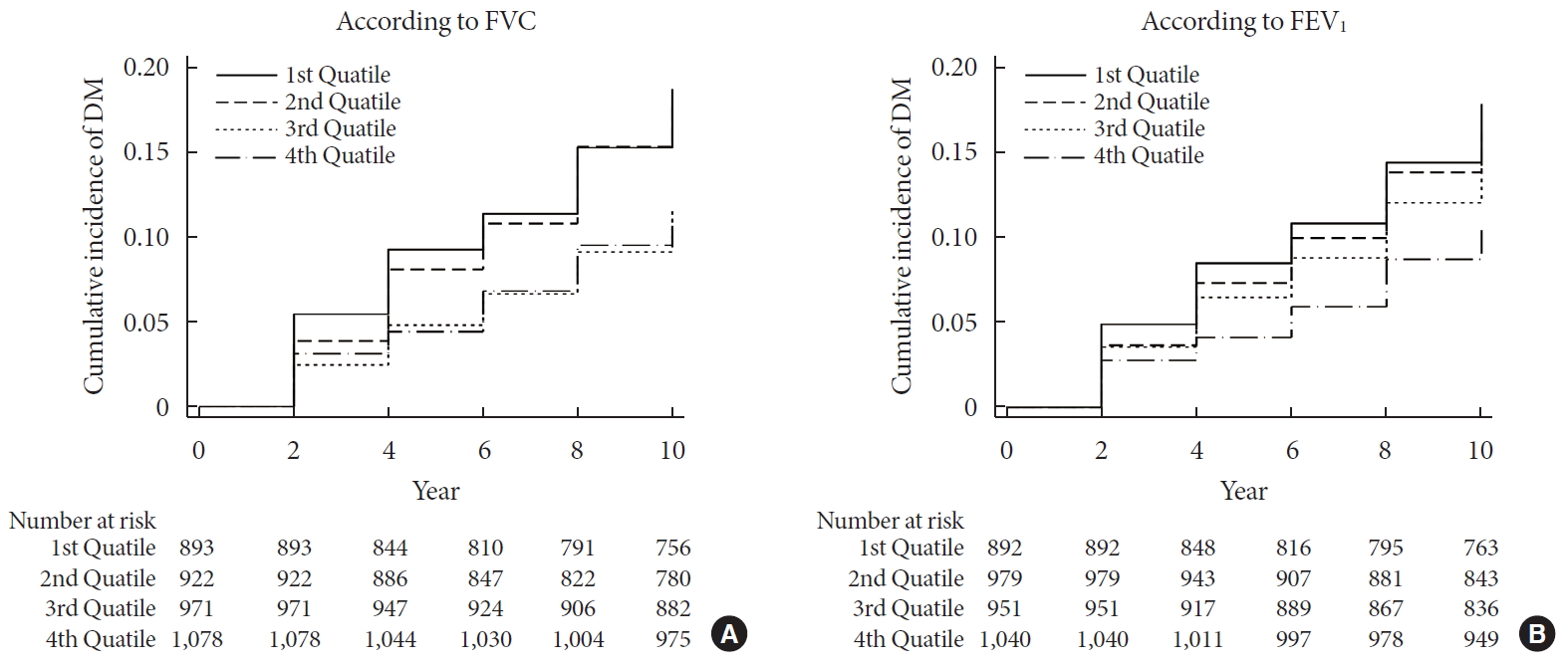
Results During 37,118 person-years of follow-up, 583 participants developed diabetes (incidence rate: 15.7 per 1,000 person-years). The mean follow-up period was 8.0±3.7 years. Forced vital capacity (FVC; % predicted) and forced expiratory volume in 1 second (FEV1; % predicted) were significantly correlated with incident diabetes in a graded manner after adjustment for sex, age, smoking, exercise, and metabolic parameters. The adjusted hazard ratio (HR) and confidence interval (CI) for diabetes were 1.408 (1.106 to 1.792) and 1.469 (1.137 to 1.897) in the first quartiles of FVC and FEV1, respectively, when compared with the highest quartile. Furthermore, the FVC of the lowest first and second quartiles showed a significantly higher 10-year panel homeostasis model assessment of insulin resistance index, with differences of 0.095 (95% CI, 0.010 to 0.018;
P =0.028) and 0.127 (95% CI, 0.044 to 0.210;P =0.003), respectively, when compared to the highest quartiles.Conclusion FVC and FEV1 are independent risk factors for developing diabetes in Koreans. Pulmonary factors are possible risk factors for insulin resistance and diabetes.
-
Citations
Citations to this article as recorded by- Validation of the Framingham Diabetes Risk Model Using Community-Based KoGES Data
Hye Ah Lee, Hyesook Park, Young Sun Hong
Journal of Korean Medical Science.2024;[Epub] CrossRef - Independent and combined associations of multiple-heavy-metal exposure with lung function: a population-based study in US children
Yiting Chen, Anda Zhao, Rong Li, Wenhui Kang, Jinhong Wu, Yong Yin, Shilu Tong, Shenghui Li, Jianyu Chen
Environmental Geochemistry and Health.2023; 45(7): 5213. CrossRef - Role of Pulmonary Function in Predicting New-Onset Cardiometabolic Diseases and Cardiometabolic Multimorbidity
Guochen Li, Yanqiang Lu, Yanan Qiao, Die Hu, Chaofu Ke
Chest.2022; 162(2): 421. CrossRef - Reduced lung function predicts risk of incident type 2 diabetes: insights from a meta-analysis of prospective studies
Yunping Zhou, Fei Meng, Min Wang, Linlin Li, Pengli Yu, Yunxia Jiang
Endocrine Journal.2022; 69(3): 299. CrossRef - Development of Various Diabetes Prediction Models Using Machine Learning Techniques
Juyoung Shin, Jaewon Kim, Chanjung Lee, Joon Young Yoon, Seyeon Kim, Seungjae Song, Hun-Sung Kim
Diabetes & Metabolism Journal.2022; 46(4): 650. CrossRef - Improving Machine Learning Diabetes Prediction Models for the Utmost Clinical Effectiveness
Juyoung Shin, Joonyub Lee, Taehoon Ko, Kanghyuck Lee, Yera Choi, Hun-Sung Kim
Journal of Personalized Medicine.2022; 12(11): 1899. CrossRef - The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea (Diabetes Metab J 2020;44: 699-710)
Hoon Sung Choi, Sung Woo Lee, Jin Taek Kim, Hong Kyu Lee
Diabetes & Metabolism Journal.2020; 44(6): 944. CrossRef - The Association between Pulmonary Functions and Incident Diabetes: Longitudinal Analysis from the Ansung Cohort in Korea (Diabetes Metab J 2020;44: 699-710)
Jin Hwa Kim
Diabetes & Metabolism Journal.2020; 44(6): 940. CrossRef
- Validation of the Framingham Diabetes Risk Model Using Community-Based KoGES Data
- Metabolic Risk/Epidemiology
- Intra-Abdominal Fat and High Density Lipoprotein Cholesterol Are Associated in a Non-Linear Pattern in Japanese-Americans
- Sun Ok Song, You-Cheol Hwang, Steven E. Kahn, Donna L. Leonetti, Wilfred Y. Fujimoto, Edward J. Boyko
- Diabetes Metab J. 2020;44(2):277-285. Published online March 10, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0008
- 4,663 View
- 63 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We describe the association between high density lipoprotein cholesterol (HDL-C) concentration and computed tomography (CT)-measured fat depots.
Methods We examined the cross-sectional associations between HDL-C concentration and intra-abdominal (IAF), abdominal subcutaneous (SCF), and thigh fat (TF) areas in 641 Japanese-American men and women. IAF, SCF, and TF were measured by CT at the level of the umbilicus and mid-thigh. The associations between fat area measurements and HDL-C were examined using multivariate linear regression analysis adjusting for age, sex, diabetes family history, homeostasis model assessment of insulin resistance (HOMA-IR), and body mass index (BMI). Non-linearity was assessed using fractional polynomials.
Results Mean±standard deviation of HDL-C concentration and IAF in men and women were 1.30±0.34 mg/dL, 105±55.3 cm2, and 1.67±0.43 mg/dL, 74.4±46.6 cm2 and differed significantly by gender for both comparisons (
P <0.001). In univariate analysis, HDL-C concentration was significantly associated with CT-measured fat depots. In multivariate analysis, IAF was significantly and non-linearly associated with HDL-C concentration adjusted for age, sex, BMI, HOMA-IR, SCF, and TF (IAF: β=−0.1012, P<0.001; IAF2: β=0.0008,P <0.001). SCF was also negatively and linearly associated with HDL-C (β=−0.4919,P =0.001).Conclusion HDL-C does not linearly decline with increasing IAF in Japanese-Americans. A more complex pattern better fits this association.
-
Citations
Citations to this article as recorded by- Associations of Serum Uric Acid to High-Density Lipoprotein Cholesterol Ratio with Trunk Fat Mass and Visceral Fat Accumulation
Yansu Wang, Yiting Xu, Tingting Hu, Yunfeng Xiao, Yufei Wang, Xiaojing Ma, Haoyong Yu, Yuqian Bao
Diabetes, Metabolic Syndrome and Obesity.2024; Volume 17: 121. CrossRef - Obesity-related parameters in carriers of some BDNF genetic variants may depend on daily dietary macronutrients intake
Urszula Miksza, Edyta Adamska-Patruno, Witold Bauer, Joanna Fiedorczuk, Przemyslaw Czajkowski, Monika Moroz, Krzysztof Drygalski, Andrzej Ustymowicz, Elwira Tomkiewicz, Maria Gorska, Adam Kretowski
Scientific Reports.2023;[Epub] CrossRef - Computed tomography-based investigation of the correlation of abdominal fat areas with metabolic syndrome
Kai-Yuan Cheng, Tsung-Hsien Yen, Jay Wu, Pei-Hsuan Li, Tian-Yu Shih
Journal of Radiological Science.2023; 48(1): 15. CrossRef - Lower High-Density Lipoprotein Cholesterol Concentration Is Independently Associated with Greater Future Accumulation of Intra-Abdominal Fat
Sun Ok Song, You-Cheol Hwang, Han Uk Ryu, Steven E. Kahn, Donna L. Leonetti, Wilfred Y. Fujimoto, Edward J. Boyko
Endocrinology and Metabolism.2021; 36(4): 835. CrossRef
- Associations of Serum Uric Acid to High-Density Lipoprotein Cholesterol Ratio with Trunk Fat Mass and Visceral Fat Accumulation
- Cardiovascular Risk/Epidemiology
- Validation of Risk Prediction Models for Atherosclerotic Cardiovascular Disease in a Prospective Korean Community-Based Cohort
- Jae Hyun Bae, Min Kyong Moon, Sohee Oh, Bo Kyung Koo, Nam Han Cho, Moon-Kyu Lee
- Diabetes Metab J. 2020;44(3):458-469. Published online January 13, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0061
- 6,873 View
- 226 Download
- 14 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background To investigate the performance of the 2013 American College of Cardiology/American Heart Association Pooled Cohort Equations (PCE) in a large, prospective, community-based cohort in Korea and to compare it with that of the Framingham Global Cardiovascular Disease Risk Score (FRS-CVD) and the Korean Risk Prediction Model (KRPM).
Methods In the Korean Genome and Epidemiology Study (KOGES)-Ansan and Ansung study, we evaluated calibration and discrimination of the PCE for non-Hispanic whites (PCE-WH) and for African Americans (PCE-AA) and compared their predictive abilities with the FRS-CVD and the KRPM.
Results The present study included 7,932 individuals (3,778 men and 4,154 women). The PCE-WH and PCE-AA moderately overestimated the risk of atherosclerotic cardiovascular disease (ASCVD) for men (6% and 13%, respectively) but underestimated the risk for women (−49% and −25%, respectively). The FRS-CVD overestimated ASCVD risk for men (91%) but provided a good risk prediction for women (3%). The KRPM underestimated ASCVD risk for men (−31%) and women (−31%). All the risk prediction models showed good discrimination in both men (C-statistic 0.730 to 0.735) and women (C-statistic 0.726 to 0.732). Recalibration of the PCE using data from the KOGES-Ansan and Ansung study substantially improved the predictive accuracy in men.
Conclusion In the KOGES-Ansan and Ansung study, the PCE overestimated ASCVD risk for men and underestimated the risk for women. The PCE-WH and the FRS-CVD provided an accurate prediction of ASCVD in men and women, respectively.
-
Citations
Citations to this article as recorded by- Risk Factors for Infertility in Korean Women
Juyeon Lee, Chang-Woo Choo, Kyoung Yong Moon, Sang Woo Lyu, Hoon Kim, Joong Yeup Lee, Jung Ryeol Lee, Byung Chul Jee, Kyungjoo Hwang, Seok Hyun Kim, Sue K. Park
Journal of Korean Medical Science.2024;[Epub] CrossRef - Evaluating cardiovascular disease risk stratification using multiple-polygenic risk scores and pooled cohort equations: insights from a 17-year longitudinal Korean cohort study
Yi Seul Park, Hye-Mi Jang, Ji Hye Park, Bong-Jo Kim, Hyun-Young Park, Young Jin Kim
Frontiers in Genetics.2024;[Epub] CrossRef - Moderation of Weight Misperception on the Associations Between Obesity Indices and Estimated Cardiovascular Disease Risk
Kayoung Lee
International Journal of Behavioral Medicine.2023; 30(1): 89. CrossRef - Validation of the general Framingham Risk Score (FRS), SCORE2, revised PCE and WHO CVD risk scores in an Asian population
Sazzli Shahlan Kasim, Nurulain Ibrahim, Sorayya Malek, Khairul Shafiq Ibrahim, Muhammad Firdaus Aziz, Cheen Song, Yook Chin Chia, Anis Safura Ramli, Kazuaki Negishi, Nafiza Mat Nasir
The Lancet Regional Health - Western Pacific.2023; 35: 100742. CrossRef - Principles of cardiovascular risk management in perimenopausal women with type 2 diabetes
F. O. Ushanova, T. Yu. Demidova, T. N. Korotkova
FOCUS. Endocrinology.2023; 4(2): 19. CrossRef - Prediction of the 10-year risk of atherosclerotic cardiovascular disease in the Korean population
Sangwoo Park, Yong-Giun Kim, Soe Hee Ann, Young-Rak Cho, Shin-Jae Kim, Seungbong Han, Gyung-Min Park
Epidemiology and Health.2023; 45: e2023052. CrossRef - Triglyceride-Glucose Index Predicts Future Atherosclerotic Cardiovascular Diseases: A 16-Year Follow-up in a Prospective, Community-Dwelling Cohort Study
Joon Ho Moon, Yongkang Kim, Tae Jung Oh, Jae Hoon Moon, Soo Heon Kwak, Kyong Soo Park, Hak Chul Jang, Sung Hee Choi, Nam H. Cho
Endocrinology and Metabolism.2023; 38(4): 406. CrossRef - Validity of the models predicting 10-year risk of cardiovascular diseases in Asia: A systematic review and prediction model meta-analysis
Mahin Nomali, Davood Khalili, Mehdi Yaseri, Mohammad Ali Mansournia, Aryan Ayati, Hossein Navid, Saharnaz Nedjat, Hean Teik Ong
PLOS ONE.2023; 18(11): e0292396. CrossRef - Assessing the Validity of the Criteria for the Extreme Risk Category of Atherosclerotic Cardiovascular Disease: A Nationwide Population-Based Study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Journal of Lipid and Atherosclerosis.2022; 11(1): 73. CrossRef - Mediation of Grip Strength on the Association Between Self-Rated Health and Estimated Cardiovascular Disease Risk
Kayoung Lee
Metabolic Syndrome and Related Disorders.2022; 20(6): 344. CrossRef - Implications of the heterogeneity between guideline recommendations for the use of low dose aspirin in primary prevention of cardiovascular disease
Xiao-Ying Li, Li Li, Sang-Hoon Na, Francesca Santilli, Zhongwei Shi, Michael Blaha
American Journal of Preventive Cardiology.2022; 11: 100363. CrossRef - The Risk of Cardiovascular Disease According to Chewing Status Could Be Modulated by Healthy Diet in Middle-Aged Koreans
Hyejin Chun, Jongchul Oh, Miae Doo
Nutrients.2022; 14(18): 3849. CrossRef - Management of Cardiovascular Risk in Perimenopausal Women with Diabetes
Catherine Kim
Diabetes & Metabolism Journal.2021; 45(4): 492. CrossRef - Comparative performance of the two pooled cohort equations for predicting atherosclerotic cardiovascular disease
Alessandra M. Campos-Staffico, David Cordwin, Venkatesh L. Murthy, Michael P. Dorsch, Jasmine A. Luzum
Atherosclerosis.2021; 334: 23. CrossRef - Usefulness of Relative Handgrip Strength as a Simple Indicator of Cardiovascular Risk in Middle-Aged Koreans
Won Bin Kim, Jun-Bean Park, Yong-Jin Kim
The American Journal of the Medical Sciences.2021; 362(5): 486. CrossRef
- Risk Factors for Infertility in Korean Women
- Metabolic Risk/Epidemiology
- Multiple Biomarkers Improved Prediction for the Risk of Type 2 Diabetes Mellitus in Singapore Chinese Men and Women
- Yeli Wang, Woon-Puay Koh, Xueling Sim, Jian-Min Yuan, An Pan
- Diabetes Metab J. 2020;44(2):295-306. Published online November 22, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0020
- 5,517 View
- 101 Download
- 6 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Multiple biomarkers have performed well in predicting type 2 diabetes mellitus (T2DM) risk in Western populations. However, evidence is scarce among Asian populations.
Methods Plasma triglyceride-to-high density lipoprotein (TG-to-HDL) ratio, alanine transaminase (ALT), high-sensitivity C-reactive protein (hs-CRP), ferritin, adiponectin, fetuin-A, and retinol-binding protein 4 were measured in 485 T2DM cases and 485 age-and-sex matched controls nested within the prospective Singapore Chinese Health Study cohort. Participants were free of T2DM at blood collection (1999 to 2004), and T2DM cases were identified at the subsequent follow-up interviews (2006 to 2010). A weighted biomarker score was created based on the strengths of associations between these biomarkers and T2DM risks. The predictive utility of the biomarker score was assessed by the area under receiver operating characteristics curve (AUC).
Results The biomarker score that comprised of four biomarkers (TG-to-HDL ratio, ALT, ferritin, and adiponectin) was positively associated with T2DM risk (
P trend <0.001). Compared to the lowest quartile of the score, the odds ratio was 12.0 (95% confidence interval [CI], 5.43 to 26.6) for those in the highest quartile. Adding the biomarker score to a base model that included smoking, history of hypertension, body mass index, and levels of random glucose and insulin improved AUC significantly from 0.81 (95% CI, 0.78 to 0.83) to 0.83 (95% CI, 0.81 to 0.86;P =0.002). When substituting the random glucose levels with glycosylated hemoglobin in the base model, adding the biomarker score improved AUC from 0.85 (95% CI, 0.83 to 0.88) to 0.86 (95% CI, 0.84 to 0.89;P =0.032).Conclusion A composite score of blood biomarkers improved T2DM risk prediction among Chinese.
-
Citations
Citations to this article as recorded by- The association between retinol-binding protein 4 and risk of type 2 diabetes: A systematic review and meta-analysis
Xiaomeng Tan, Han Zhang, Limin Liu, Zengli Yu, Xinxin Liu, Lingling Cui, Yao Chen, Huanhuan Zhang, Zhan Gao, Zijian Zhao
International Journal of Environmental Health Research.2024; 34(2): 1053. CrossRef - Baseline glycated albumin level and risk of type 2 diabetes mellitus in Healthy individuals: a retrospective longitudinal observation in Korea
Kang-Su Shin, Min-Seung Park, Mi Yeon Lee, Eun Hye Cho, Hee-Yeon Woo, Hyosoon Park, Min-Jung Kwon
Scandinavian Journal of Clinical and Laboratory Investigation.2024; : 1. CrossRef - Remnant Cholesterol Is an Independent Predictor of Type 2 Diabetes: A Nationwide Population-Based Cohort Study
Ji Hye Huh, Eun Roh, Seong Jin Lee, Sung-Hee Ihm, Kyung-Do Han, Jun Goo Kang
Diabetes Care.2023; 46(2): 305. CrossRef - A FRAMEWORK FOR THE ANALYSIS OF COMORBID CONDITIONS USING INTELLIGENT EXTRACTION OF MULTIPLE FLUID BIOMARKERS
PRIYANKA JADHAV, VINOTHINI SELVARAJU, SARITH P SATHIAN, RAMAKRISHNAN SWAMINATHAN
Journal of Mechanics in Medicine and Biology.2023;[Epub] CrossRef - Strikes and Gutters: Biomarkers and anthropometric measures for predicting diagnosed diabetes mellitus in adults in low- and middle-income countries
Sally Sonia Simmons
Heliyon.2023; 9(9): e19494. CrossRef - Association of IL-16 rs11556218 T/G polymorphism with the risk of developing type 2 diabetes mellitus
Dalia Ghareeb Mohammad, Hamdy Omar, Taghrid B. El-Abaseri, Wafaa Omar, Shaymaa Abdelraheem
Journal of Diabetes & Metabolic Disorders.2021; 20(1): 649. CrossRef - Biomarker Score in Risk Prediction: Beyond Scientific Evidence and Statistical Performance
Heejung Bang
Diabetes & Metabolism Journal.2020; 44(2): 245. CrossRef
- The association between retinol-binding protein 4 and risk of type 2 diabetes: A systematic review and meta-analysis
- Metabolic Risk/Epidemiology
- Plasma CD36 and Incident Diabetes: A Case-Cohort Study in Danish Men and Women
- Yeli Wang, Jingwen Zhu, Sarah Aroner, Kim Overvad, Tianxi Cai, Ming Yang, Anne Tjønneland, Aase Handberg, Majken K. Jensen
- Diabetes Metab J. 2020;44(1):134-142. Published online October 18, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0273
- 4,273 View
- 70 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Membrane CD36 is a fatty acid transporter implicated in the pathogenesis of metabolic disease. We aimed to evaluate the association between plasma CD36 levels and diabetes risk and to examine if the association was independent of adiposity among Danish population.
Methods We conducted a case-cohort study nested within the Danish Diet, Cancer and Health study among participants free of cardiovascular disease, diabetes and cancer and with blood samples and anthropometric measurements (height, weight, waist circumference, and body fat percentage) at baseline (1993 to 1997). CD36 levels were measured in 647 incident diabetes cases that occurred before December 2011 and a total of 3,515 case-cohort participants (236 cases overlap).
Results Higher plasma CD36 levels were associated with higher diabetes risk after adjusting for age, sex and other lifestyle factors. The hazard ratio (HR) comparing high versus low tertile of plasma CD36 levels was 1.36 (95% confidence interval [CI], 1.00 to 1.86). However, the association lost its significance after further adjustment for different adiposity indices such as body mass index (HR, 1.23; 95% CI, 0.87 to 1.73), waist circumference (HR, 1.21; 95% CI, 0.88 to 1.68) or body fat percentage (HR, 1.20; 95% CI, 0.86 to 1.66). Moreover, raised plasma CD36 levels were moderately associated with diabetes risk among lean participants, but the association was not present among overweight/obese individuals.
Conclusion Higher plasma CD36 levels were associated with higher diabetes risk, but the association was not independent of adiposity. In this Danish population, the association of CD36 with diabetes risk could be either mediated or confounded by adiposity.
-
Citations
Citations to this article as recorded by- The Multifunctionality of CD36 in Diabetes Mellitus and Its Complications—Update in Pathogenesis, Treatment and Monitoring
Kamila Puchałowicz, Monika Ewa Rać
Cells.2020; 9(8): 1877. CrossRef - The Role of CD36 in Type 2 Diabetes Mellitus: β-Cell Dysfunction and Beyond
Jun Sung Moon, Udayakumar Karunakaran, Elumalai Suma, Seung Min Chung, Kyu Chang Won
Diabetes & Metabolism Journal.2020; 44(2): 222. CrossRef
- The Multifunctionality of CD36 in Diabetes Mellitus and Its Complications—Update in Pathogenesis, Treatment and Monitoring
- Epidemiology
- Plasma Fetuin-A Levels and Risk of Type 2 Diabetes Mellitus in A Chinese Population: A Nested Case-Control Study
- Yeli Wang, Woon-Puay Koh, Majken K. Jensen, Jian-Min Yuan, An Pan
- Diabetes Metab J. 2019;43(4):474-486. Published online March 20, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0171
- 4,572 View
- 71 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Fetuin-A is a hepatokine that involved in the pathogenesis of insulin resistance. Previous epidemiological studies have found a positive association between blood fetuin-A and type 2 diabetes mellitus (T2DM) risk among Caucasians and African Americans. We aimed to investigate the prospective relationship between fetuin-A and T2DM in an Asian population for the first time.
Methods A nested case-control study was established within a prospective cohort of Chinese living in Singapore. At blood collection (1999 to 2004), all participants were free of diagnosed T2DM and aged 50 to 79 years. At subsequent follow-up (2006 to 2010), 558 people reported to have T2DM and were classified as incident cases, and 558 controls were randomly chosen from the participants who did not develop T2DM to match with cases on age, sex, dialect group, and date of blood collection. Plasma fetuin-A levels were measured retrospectively in cases and controls using samples collected at baseline. Conditional logistic regression models were used to compute the odds ratio (OR) and 95% confidence interval (CI). Restricted cubic spline analysis was used to examine a potential non-linear association between fetuin-A levels and T2DM risk.
Results Compared with those in the lowest fetuin-A quintile, participants in the highest quintile had a two-fold increased risk of developing T2DM (OR, 2.06; 95% CI, 1.21 to 3.51). A non-linear association was observed (
P nonlinearity=0.005), where the association between fetuin-A levels and T2DM risk plateaued at plasma concentrations around 830 µg/mL.Conclusion There is a positive association between plasma fetuin-A levels and risk of developing T2DM in this Chinese population.
-
Citations
Citations to this article as recorded by- Type 2 diabetes and gut health - Narrative review
Janeline Lunghar, A. Thahira Banu
International Journal of Noncommunicable Diseases.2024; 9(1): 4. CrossRef - The predicted mechanisms and evidence of probiotics on type 2 diabetes mellitus (T2DM)
Ousman Bajinka, Kodzovi Sylvain Dovi, Lucette Simbilyabo, Ishmail Conteh, Yurong Tan
Archives of Physiology and Biochemistry.2023; : 1. CrossRef - Multiplexed measurements of salivary fetuin-A, insulin, and adiponectin as potential non-invasive biomarkers in childhood obesity
Vaithinathan Selvaraju, Jeganathan R. Babu, Thangiah Geetha
Cytokine.2022; 153: 155843. CrossRef - Recent Developments in Biomarkers for Diagnosis and Screening of Type 2 Diabetes Mellitus
Margarita Ortiz-Martínez, Mirna González-González, Alexandro J. Martagón, Victoria Hlavinka, Richard C. Willson, Marco Rito-Palomares
Current Diabetes Reports.2022; 22(3): 95. CrossRef - Serum Fetuin-A and Risk of Gestational Diabetes Mellitus: An Observational Study and Mendelian Randomization Analysis
Ping Wu, Yi Wang, Yi Ye, Xue Yang, Qi Lu, Jiaying Yuan, Li Zha, Yan Liu, Xingyue Song, Shijiao Yan, Ying Wen, Xiaorong Qi, Chun-Xia Yang, Yixin Wang, Gang Liu, Chuanzhu Lv, Xiong-Fei Pan, An Pan
The Journal of Clinical Endocrinology & Metabolism.2022; 107(9): e3841. CrossRef - Hepatokines as a Molecular Transducer of Exercise
Dae Yun Seo, Se Hwan Park, Jubert Marquez, Hyo-Bum Kwak, Tae Nyun Kim, Jun Hyun Bae, Jin-Ho Koh, Jin Han
Journal of Clinical Medicine.2021; 10(3): 385. CrossRef - Serum Fetuin-B Levels Are Elevated in Women with Metabolic Syndrome and Associated with Increased Oxidative Stress
Shiyao Xue, Hongdong Han, Shunli Rui, Mengliu Yang, Yizhou Huang, Bin Zhan, Shan Geng, Hua Liu, Chen Chen, Gangyi Yang, Ling Li, Colin Murdoch
Oxidative Medicine and Cellular Longevity.2021; 2021: 1. CrossRef - CD44, a Predominant Protein in Methylglyoxal-Induced Secretome of Muscle Cells, is Elevated in Diabetic Plasma
Shakuntala Bai, Arvindkumar H. Chaurasiya, Reema Banarjee, Prachi B. Walke, Faraz Rashid, Ambika G. Unnikrishnan, Mahesh J. Kulkarni
ACS Omega.2020; 5(39): 25016. CrossRef
- Type 2 diabetes and gut health - Narrative review
- Complications
- Nonalcoholic Fatty Liver Disease in Diabetes. Part I: Epidemiology and Diagnosis
- Yong-ho Lee, Yongin Cho, Byung-Wan Lee, Cheol-Young Park, Dae Ho Lee, Bong-Soo Cha, Eun-Jung Rhee
- Diabetes Metab J. 2019;43(1):31-45. Published online December 17, 2018
- DOI: https://doi.org/10.4093/dmj.2019.0011
- Correction in: Diabetes Metab J 2019;43(5):731
- 8,213 View
- 167 Download
- 106 Web of Science
- 101 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Nonalcoholic fatty liver disease (NAFLD) and diabetes are common metabolic disorders whose prevalence rates are expected to rise worldwide, corresponding to aging and increasingly obese populations. Compared to the general population (around 25%), 50% to 70% of people with diabetes have NAFLD, and NAFLD severity (including fibrosis) tends to be worsened by the presence of diabetes. NAFLD is considered an emerging risk factor for type 2 diabetes mellitus and a contributor to the development of chronic diabetes-related complications. This reciprocal relationship demonstrates the importance of confirming suspected NAFLD in patients with diabetes. Due to the invasive nature of liver biopsy to assess NAFLD status, various alternative non-invasive modalities have been developed and validated. Here, we summarized the epidemiology of NAFLD in patients with diabetes and reviewed currently available imaging modalities and biomarker-based prediction models for their ability to detect liver steatosis and/or fibrosis.
-
Citations
Citations to this article as recorded by- Mortality in metabolic dysfunction-associated steatotic liver disease: A nationwide population-based cohort study
Eugene Han, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Sang Hoon Ahn, Yong-ho Lee, Seung Up Kim
Metabolism.2024; 152: 155789. CrossRef - Intact ketogenesis predicted reduced risk of moderate-severe metabolic-associated fatty liver disease assessed by liver transient elastography in newly diagnosed type 2 diabetes
Sejeong Lee, Jaehyun Bae, Seung Up Kim, Minyoung Lee, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Frontiers in Endocrinology.2024;[Epub] CrossRef - ZJU Index as a Predictive Tool for Diabetes Incidence: Insights from a Population-Based Cohort Study
Chenjiao Wu, Yi Hao Loh, Hangkai Huang, Chengfu Xu
Diabetes, Metabolic Syndrome and Obesity.2024; Volume 17: 715. CrossRef - Sigmoidal relationship between liver fat content and nonalcoholic fatty liver disease in Chinese adults
Pingping Yu, Huachao Yang, Hu Li, Ying Mei, Yuanyuan Wu, Hongfeng Cheng, Huiru Su, Yueling Deng, Tao Jiang, Zhongxiang He, Peng Hu
Postgraduate Medical Journal.2024;[Epub] CrossRef - Safety and Efficacy of Efruxifermin in Combination With a GLP-1 Receptor Agonist in Patients With NASH/MASH and Type 2 Diabetes in a Randomized Phase 2 Study
Stephen A. Harrison, Juan P. Frias, K. Jean Lucas, Gary Reiss, Guy Neff, Sureka Bollepalli, Yan Su, Doreen Chan, Erik J. Tillman, Ali Moulton, Brittany de Temple, Arian Zari, Reshma Shringarpure, Timothy Rolph, Andrew Cheng, Kitty Yale
Clinical Gastroenterology and Hepatology.2024;[Epub] CrossRef - Association between nonalcoholic fatty liver disease and left ventricular diastolic dysfunction: A 7-year retrospective cohort study of 3,380 adults using serial echocardiography
Gyuri Kim, Tae Yang Yu, Jae Hwan Jee, Ji Cheol Bae, Mira Kang, Jae Hyeon Kim
Diabetes & Metabolism.2024; 50(3): 101534. CrossRef - Plasma Adiponectin and Its Correlation with Carotid Intima-Media Thickness in Obesity and in Type 2 Diabetes and Nonalcoholic Fatty Liver Disease
Maha Hussein, Aasem Saif, Mona Amin, Osama Khalafallah, Ahmed Hussien, Samar Aboulsoud, Shrook Mousa, S. Razzaque Mohammed
Journal of Nutrition and Metabolism.2023; 2023: 1. CrossRef - Exposure to Bisphenol A, S, and F and its Association with Obesity and Diabetes Mellitus in General Adults of Korea: Korean National Environmental Health Survey (KoNEHS) 2015–2017
Min Kyong Moon, Min Joo Kim, Inae Lee, Sunmi Kim, Sohyeon Choi, Jeongim Park, Yoon Hee Cho, Sooyeon Hong, Jiyoung Yoo, Hyunwoong Park, Gi Jeong Cheon, Young Joo Park, Kyungho Choi
Exposure and Health.2023; 15(1): 53. CrossRef - Liver fat content assessed by conventional B-mode ultrasound and metabolic profile in non-diabetic patients: Implications for clinical practice
Rosanna Villani, Grazia Pia Magnati, Giulia Tuccari, Moris Sangineto, Antonino Davide Romano, Tommaso Cassano, Gaetano Serviddio
Ultrasound.2023; 31(3): 177. CrossRef - Association of cardiovascular health metrics with annual incidence of prediabetes or diabetes: Analysis of a nationwide real‐world database
Akira Okada, Hidehiro Kaneko, Satoshi Matsuoka, Hidetaka Itoh, Yuta Suzuki, Katsuhito Fujiu, Nobuaki Michihata, Taisuke Jo, Norifumi Takeda, Hiroyuki Morita, Satoko Yamaguchi, Koichi Node, Toshimasa Yamauchi, Hideo Yasunaga, Issei Komuro
Journal of Diabetes Investigation.2023; 14(3): 452. CrossRef - Effects of Environmental Cadmium Exposure on the Liver in Korean Adults: Cross-Sectional and Longitudinal Studies
Mi-Na Seo, Sang-Yong Eom, Ji-Ae Lim, Jung-Eum Lee, Byung-Sun Choi, Ho-Jang Kwon, Young-Seoub Hong, Heon Kim, Jung-Duck Park
Archives of Environmental Contamination and Toxicology.2023; 84(2): 237. CrossRef - Newer Glucose-Lowering Therapies in Older Adults with Type 2 Diabetes
Anika Bilal, Richard E. Pratley
Endocrinology and Metabolism Clinics of North America.2023; 52(2): 355. CrossRef - CD24 Gene Expression as a Risk Factor for Non-Alcoholic Fatty Liver Disease
Mona A. Amin, Halla M. Ragab, Nabila Abd El Maksoud, Wafaa Abd Elaziz
Diagnostics.2023; 13(5): 984. CrossRef - Metabolic Dysfunction-Associated Fatty Liver Disease and Mortality: A Population-Based Cohort Study
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes & Metabolism Journal.2023; 47(2): 220. CrossRef - Non-Alcoholic Fatty Liver Disease with Sarcopenia and Carotid Plaque Progression Risk in Patients with Type 2 Diabetes Mellitus
Yongin Cho, Hye-Sun Park, Byung Wook Huh, Yong-ho Lee, Seong Ha Seo, Da Hea Seo, Seong Hee Ahn, Seongbin Hong, So Hun Kim
Diabetes & Metabolism Journal.2023; 47(2): 232. CrossRef - Nonalcoholic fatty liver disease and type 2 diabetes: an observational and Mendelian randomization study
Yuetian Yu, Yuefeng Yu, Yuying Wang, Yi Chen, Ningjian Wang, Bin Wang, Yingli Lu
Frontiers in Endocrinology.2023;[Epub] CrossRef - β-sitosterol attenuates high- fat diet-induced hepatic steatosis in rats by modulating lipid metabolism, inflammation and ER stress pathway
Omayma AR Abo-Zaid, Fatma SM Moawed, Effet Soliman Ismail, Mostafa A. Farrag
BMC Pharmacology and Toxicology.2023;[Epub] CrossRef - Fatty Liver & Diabetes Statistics in Korea: Nationwide Data 2009 to 2017
Eugene Han, Kyung-Do Han, Yong-ho Lee, Kyung-Soo Kim, Sangmo Hong, Jung Hwan Park, Cheol-Young Park
Diabetes & Metabolism Journal.2023; 47(3): 347. CrossRef - Increased expression of sodium-glucose cotransporter 2 and O-GlcNAcylation in hepatocytes drives non-alcoholic steatohepatitis
Hye Jin Chun, Eun Ran Kim, Minyoung Lee, Da Hyun Choi, Soo Hyun Kim, Eugene Shin, Jin-Hong Kim, Jin Won Cho, Dai Hoon Han, Bong-Soo Cha, Yong-ho Lee
Metabolism.2023; 145: 155612. CrossRef - Role of vascular endothelial growth factor B in nonalcoholic fatty liver disease and its potential value
Yu-Qi Li, Lei Xin, Yu-Chi Zhao, Shang-Qi Li, Ya-Nuo Li
World Journal of Hepatology.2023; 15(6): 786. CrossRef - Increased risk of incident diabetes in patients with MAFLD not meeting the criteria for NAFLD
So Hee Park, Jiyun Park, So Yoon Kwon, You-Bin Lee, Gyuri Kim, Kyu Yeon Hur, Janghyun Koh, Jae Hwan Jee, Jae Hyeon Kim, Mira Kang, Sang-Man Jin
Scientific Reports.2023;[Epub] CrossRef - Significance of Diabetic Kidney Disease Biomarkers in Predicting Metabolic-Associated Fatty Liver Disease
Jaehyun Bae, Byung-Wan Lee
Biomedicines.2023; 11(7): 1928. CrossRef - An Evidence-Based Review of Diabetes Care: History, Types, Relationship
to Cancer and Heart Disease, Co-Morbid Factors, and Preventive
Measures
Umesh Chandra Gupta, Subhas Chandra Gupta, Shayle Sugandh Gupta
Current Nutrition & Food Science.2023; 19(4): 399. CrossRef - Associations of serum aminotransferase and the risk of all-cause and cause-specific mortality in Chinese type 2 diabetes: a community-based cohort study
Jian Su, Haoyu Guan, Xikang Fan, Hao Yu, Yu Qin, Jie Yang, Zheng Zhu, Chong Shen, Enchun Pan, Yan Lu, Jin-Yi Zhou, Ming Wu
BMJ Open.2023; 13(7): e068160. CrossRef - Retinoic acid signaling in fatty liver disease
Fathima N. Cassim Bawa, Yanqiao Zhang
Liver Research.2023; 7(3): 189. CrossRef - Pharmaceutical Strategies to Improve Druggability of Potential Drug Candidates in Nonalcoholic Fatty Liver Disease Therapy
Reeju Amatya, Donghee Lee, Kyoung Ah Min, Meong Cheol Shin
Pharmaceutics.2023; 15(7): 1963. CrossRef - Prevalence of Non-Alcoholic Fatty Liver Disease and Its Risk Factors in Korean Population
Sang Gyeong Lee, Songchan Oh, Moon Seong Kim, Jooyeon Kim, Eunjin Jung, Young Jun Kim, Jiyoun Hong
Food Supplements and Biomaterials for Health.2023;[Epub] CrossRef - Low‑dose ionizing radiation attenuates high glucose‑induced hepatic apoptosis and immune factor release via modulation of a miR‑155‑SOCS1 axis
Hongqiong Fan, Shanshan Liu, Benzheng Jiao, Xinyue Liang
Molecular Medicine Reports.2023;[Epub] CrossRef - CT-based measurement of visceral adipose tissue volume as a reliable tool for assessing metabolic risk factors in prediabetes across subtypes
Jihyun Kim, Keunyoung Kim
Scientific Reports.2023;[Epub] CrossRef - The Role of the Fatty Liver Index (FLI) in the Management of Non-Alcoholic Fatty Liver Disease: A Systematic Review
Teodora Biciusca, Sorina Ionelia Stan, Mara Amalia Balteanu, Ramona Cioboata, Alice Elena Ghenea, Suzana Danoiu, Ana-Maria Bumbea, Viorel Biciusca
Diagnostics.2023; 13(21): 3316. CrossRef - Circ_0004535/miR-1827/CASP8 network involved in type 2 diabetes mellitus with nonalcoholic fatty liver disease
Min Li, Ai Zeng, Xinle Tang, Hui Xu, Wei Xiong, Yanying Guo
Scientific Reports.2023;[Epub] CrossRef - Prevalence of High and Moderate Risk of Liver Fibrosis Among Patients With Diabetes at a Noncommunicable Diseases (NCD) Clinic in a Primary Healthcare Center in Northern India
Anubhav Mondal, Aninda Debnath, Ghurumourthy Dhandapani, Abhishek Sharma, Shveta Lukhmana, Geeta Yadav
Cureus.2023;[Epub] CrossRef - Therapeutic outcome of dapagliflozin on various parameters in non-alcoholic fatty liver disease (NAFLD) patients
Mazhar Hussain, Muhammad Zafar Majeed Babar, Saba Tariq, Muhammad Irfan Ahmad, Lubna Akhtar
International Journal of Diabetes in Developing Countries.2022; 42(2): 290. CrossRef - Lead, mercury, and cadmium exposures are associated with obesity but not with diabetes mellitus: Korean National Environmental Health Survey (KoNEHS) 2015–2017
Min Kyong Moon, Inae Lee, Aram Lee, Hyunwoong Park, Min Joo Kim, Sunmi Kim, Yoon Hee Cho, Sooyeon Hong, Jiyoung Yoo, Gi Jeong Cheon, Kyungho Choi, Young Joo Park, Jeongim Park
Environmental Research.2022; 204: 111888. CrossRef - Association of Prenatal Famine Exposure With Inflammatory Markers and Its Impact on Adulthood Liver Function Across Consecutive Generations
Shiwei Yan, Jingqi Ruan, Yu Wang, Jiaxu Xu, Changhao Sun, Yucun Niu
Frontiers in Nutrition.2022;[Epub] CrossRef - Serum Metabolomics in Patients with Coexisting NAFLD and T2DM Using Liquid Chromatography-Mass Spectrometry
Cheng Hu, Xiaoyu Zhuang, Jiaqi Zhang, Tao Wang, Shengnan Du, Jinping Wang, Xuelian Peng, Qin Cao, Mingcai Zhang, Yuanye Jiang
Laboratory Medicine.2022; 53(4): 360. CrossRef - Genistein—Opportunities Related to an Interesting Molecule of Natural Origin
Ewa Garbiec, Judyta Cielecka-Piontek, Magdalena Kowalówka, Magdalena Hołubiec, Przemysław Zalewski
Molecules.2022; 27(3): 815. CrossRef - Renal Tubular Damage Marker, Urinary N-acetyl-β-D-Glucosaminidase, as a Predictive Marker of Hepatic Fibrosis in Type 2 Diabetes Mellitus
Hae Kyung Kim, Minyoung Lee, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Diabetes & Metabolism Journal.2022; 46(1): 104. CrossRef - Long-term effects of the changes in hepatic steatosis status on the risk of incident type 2 diabetes mellitus: A 15-year community-based prospective cohort study
Seung Min Chung, Min Kyu Kang, Jinho Jung, Ji Sung Yoon, Kyu Chang Won, Hyoung Woo Lee, Rohit Loomba, Jung Gil Park, Jun Sung Moon
Diabetes Research and Clinical Practice.2022; 184: 109208. CrossRef - Prevalence and Risk Factors of Advanced Liver Fibrosis in a Population‐Based Study in Germany
Yvonne Huber, Andreas Schulz, Irene Schmidtmann, Manfred Beutel, Norbert Pfeiffer, Thomas Münzel, Peter R. Galle, Philipp S. Wild, Karl J. Lackner, Jörn M. Schattenberg
Hepatology Communications.2022; 6(6): 1457. CrossRef - Non-alcoholic fatty liver disease: Epidemiology, pathophysiology and an update on the therapeutic approaches
RehabF Abdel-Rahman
Asian Pacific Journal of Tropical Biomedicine.2022; 12(3): 99. CrossRef - State-of-the-Art Overview of the Pharmacological Treatment of Non-Alcoholic Steatohepatitis
Yongin Cho, Yong-ho Lee
Endocrinology and Metabolism.2022; 37(1): 38. CrossRef - Obesity is an important determinant of severity in newly defined metabolic dysfunction-associated fatty liver disease
Ji Hye Huh, Kwang Joon Kim, Seung Up Kim, Bong-Soo Cha, Byung-Wan Lee
Hepatobiliary & Pancreatic Diseases International.2022; 21(3): 241. CrossRef - The associations of hepatic steatosis and fibrosis using fatty liver index and BARD score with cardiovascular outcomes and mortality in patients with new-onset type 2 diabetes: a nationwide cohort study
Jiyun Park, Gyuri Kim, Bong-Sung Kim, Kyung-Do Han, So Yoon Kwon, So Hee Park, You-Bin Lee, Sang-Man Jin, Jae Hyeon Kim
Cardiovascular Diabetology.2022;[Epub] CrossRef - Sociodemographic and genetic determinants of nonalcoholic fatty liver disease in type 2 diabetes mellitus patients
Muhammad Adnan, Abdul Wajid, Wasif Noor, Andleeb Batool, Muhammad Aasim, Kamran Abbas, Quratul Ain
Journal of Genetic Engineering and Biotechnology.2022; 20(1): 68. CrossRef - Concordance between indirect fibrosis and steatosis indices and their predictors in subjects with overweight/obesity
Gaggini Melania, Vigna Luisella, Di Piazza Salvina, Gori Francesca, Tirelli Amedea Silvia, Bamonti Fabrizia, Maltinti Maristella, Napolitano Filomena, Chatzianagnostou Kyriazoula, Cristina Vassalle
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity.2022; 27(7): 2617. CrossRef - Stéatopathie métabolique hépatique évaluée par le FibroScan® avec contrôle des paramètres d’atténuation (CAP) chez la personne diabétique de type 2 en Côte d’Ivoire
Jacko Abodo, Dimitri Kouamé, Jocelyne Danho, Moumouni Léilatou, Pierre Koffi-Dago, Adelaïde Hué, Assita Yao, Franck Kouassi, Anselme N’Guessan, Fulgence Bathaix
Médecine des Maladies Métaboliques.2022; 16(6): 550. CrossRef - Non-invasive diagnosis and staging of non-alcoholic fatty liver disease
Stergios Kechagias, Mattias Ekstedt, Christian Simonsson, Patrik Nasr
Hormones.2022; 21(3): 349. CrossRef - Association between organochlorine pesticides and nonalcoholic fatty liver disease in the National Health and Nutrition Examination Survey 2003–2004
Hyunji Sang, Kyu-Na Lee, Chang Hee Jung, Kyungdo Han, Eun Hee Koh
Scientific Reports.2022;[Epub] CrossRef - Increased Risk of NAFLD in Adults with Glomerular Hyperfiltration: An 8-Year Cohort Study Based on 147,162 Koreans
Dae-Jeong Koo, Mi Yeon Lee, Inha Jung, Sun Joon Moon, Hyemi Kwon, Eun-Jung Rhee, Cheol-Young Park, Won-Young Lee, Ki Won Oh, Se Eun Park
Journal of Personalized Medicine.2022; 12(7): 1142. CrossRef - Advanced Liver Fibrosis Is Associated with Chronic Kidney Disease in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Da Hea Seo, Young Ju Suh, Yongin Cho, Seong Hee Ahn, Seongha Seo, Seongbin Hong, Yong-ho Lee, Young Ju Choi, Eunjig Lee, So Hun Kim
Diabetes & Metabolism Journal.2022; 46(4): 630. CrossRef - New Insights into Non-Alcoholic Fatty Liver Disease and Coronary Artery Disease: The Liver-Heart Axis
Georgiana-Diana Cazac, Cristina-Mihaela Lăcătușu, Cătălina Mihai, Elena-Daniela Grigorescu, Alina Onofriescu, Bogdan-Mircea Mihai
Life.2022; 12(8): 1189. CrossRef - Efficacy and mechanism of Jiedu Tongluo Tiaogan Formula in treating type 2 diabetes mellitus combined with non-alcoholic fatty liver disease: Study protocol for a parallel-armed, randomized controlled trial
Jinghan Xu, Chunli Piao, Yue Qu, Tianjiao Liu, Yuting Peng, Qi Li, Xiaohua Zhao, Pei Li, Xuemin Wu, Yawen Fan, Binqin Chen, Jie Yang
Frontiers in Pharmacology.2022;[Epub] CrossRef - Ultrasound-Based Hepatic Elastography in Non-Alcoholic Fatty Liver Disease: Focus on Patients with Type 2 Diabetes
Georgiana-Diana Cazac, Cristina-Mihaela Lăcătușu, Cătălina Mihai, Elena-Daniela Grigorescu, Alina Onofriescu, Bogdan-Mircea Mihai
Biomedicines.2022; 10(10): 2375. CrossRef - Diosgenin Ameliorated Type II Diabetes-Associated Nonalcoholic Fatty Liver Disease through Inhibiting De Novo Lipogenesis and Improving Fatty Acid Oxidation and Mitochondrial Function in Rats
Yujie Zhong, Zhiman Li, Ruyi Jin, Yanpeng Yao, Silan He, Min Lei, Xin Wang, Chao Shi, Li Gao, Xiaoli Peng
Nutrients.2022; 14(23): 4994. CrossRef - The associations between changes in hepatic steatosis and heart failure and mortality: a nationwide cohort study
Jiyun Park, Gyuri Kim, Hasung Kim, Jungkuk Lee, Sang-Man Jin, Jae Hyeon Kim
Cardiovascular Diabetology.2022;[Epub] CrossRef - Recent advances and potentiality of postbiotics in the food industry: Composition, inactivation methods, current applications in metabolic syndrome, and future trends
Yujie Zhong, Tao Wang, Ruilin Luo, Jiayu Liu, Ruyi Jin, Xiaoli Peng
Critical Reviews in Food Science and Nutrition.2022; : 1. CrossRef - Association of nonalcoholic fatty liver disease with coronary artery disease in type 2 diabetes mellitus: A cross-sectional study from a tertiary care medical college hospital
Neelakandan Ramya, Golepu Karthikeya, SethuPrabhu Shankar
Acta Medica International.2022; 9(1): 31. CrossRef - NAFLDin type 2 diabetes mellitus: Still many challenging questions
Simona Cernea, Itamar Raz
Diabetes/Metabolism Research and Reviews.2021;[Epub] CrossRef - The protective effect of shrimp cooked in different methods on high-cholesterol- induced fatty liver in rats
Nora A. AlFaris, Ghedeir M. Alshammari, Jozaa Z. AlTamimi, Lujain A. AlMousa, Nora M. AlKehayez, Dalal H. Aljabryn, Reham I. Alagal, Mohammed A. Yahya
Saudi Journal of Biological Sciences.2021; 28(1): 170. CrossRef - Evolution of liver fibrosis and steatosis markers in patients with type 2 diabetes after metformin treatment for 2 years
Hye Won Lee, Jae Seung Lee, Beom Kyung Kim, Jun Yong Park, Do Young Kim, Sang Hoon Ahn, Seung Up Kim
Journal of Diabetes and its Complications.2021; 35(1): 107747. CrossRef - Prognostic value of non-alcoholic fatty liver disease for predicting cardiovascular events in patients with diabetes mellitus with suspected coronary artery disease: a prospective cohort study
Keishi Ichikawa, Toru Miyoshi, Kazuhiro Osawa, Takashi Miki, Hironobu Toda, Kentaro Ejiri, Masatoki Yoshida, Yusuke Nanba, Masashi Yoshida, Kazufumi Nakamura, Hiroshi Morita, Hiroshi Ito
Cardiovascular Diabetology.2021;[Epub] CrossRef - Implications of Abdominal Adipose Tissue Distribution on Nonalcoholic Fatty Liver Disease and Metabolic Syndrome: A Chinese General Population Study
Chileka Chiyanika, Vincent Wai-Sun Wong, Grace Lai-Hung Wong, Henry Lik-Yuen Chan, Steve C. N. Hui, David K. W. Yeung, Winnie C. W. Chu
Clinical and Translational Gastroenterology.2021; 12(2): e00300. CrossRef - Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease: Diagnosis and Treatment
Sook Jung Lee, Byung-Wan Lee
The Journal of Korean Diabetes.2021; 22(1): 38. CrossRef - Pioglitazone for NAFLD Patients With Prediabetes or Type 2 Diabetes Mellitus: A Meta-Analysis
Jingxuan Lian, Jianfang Fu
Frontiers in Endocrinology.2021;[Epub] CrossRef - Allopurinol ameliorates high fructose diet induced hepatic steatosis in diabetic rats through modulation of lipid metabolism, inflammation, and ER stress pathway
In-Jin Cho, Da-Hee Oh, Jin Yoo, You-Cheol Hwang, Kyu Jeung Ahn, Ho-Yeon Chung, Soung Won Jeong, Ju-Young Moon, Sang-Ho Lee, Sung-Jig Lim, In-Kyung Jeong
Scientific Reports.2021;[Epub] CrossRef - Diabetic Kidney Disease, Cardiovascular Disease and Non-Alcoholic Fatty Liver Disease: A New Triumvirate?
Carolina M. Perdomo, Nuria Garcia-Fernandez, Javier Escalada
Journal of Clinical Medicine.2021; 10(9): 2040. CrossRef - Fenofibrate, a PPARα agonist, reduces hepatic fat accumulation through the upregulation of TFEB-mediated lipophagy
Jin Yoo, In-Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung, You-Cheol Hwang
Metabolism.2021; 120: 154798. CrossRef - Association Between Thyroid Hormone Levels and Advanced Liver Fibrosis in Patients with Type 2 Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease
Jing Du, Sanbao Chai, Xin Zhao, Jianbin Sun, Xiaomei Zhang, Lili Huo
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 2399. CrossRef - Association between toothbrushing and non-alcoholic fatty liver disease
Ji-Youn Kim, Yong-Moon Park, Gyu-Na Lee, Hyun Chul Song, Yu-Bae Ahn, Kyungdo Han, Seung-Hyun Ko, Houkai Li
PLOS ONE.2021; 16(5): e0243686. CrossRef - Non‐alcoholic fatty liver disease and sarcopenia additively increase mortality: a Korean nationwide survey
Joon Ho Moon, Bo Kyung Koo, Won Kim
Journal of Cachexia, Sarcopenia and Muscle.2021; 12(4): 964. CrossRef - Sodium-Glucose Cotransporter-2 Inhibitors Ameliorate Liver Enzyme Abnormalities in Korean Patients With Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Won Euh, Soo Lim, Jin-Wook Kim
Frontiers in Endocrinology.2021;[Epub] CrossRef - Modulation and bioinformatics screening of hepatic mRNA-lncRNAs (HML) network associated with insulin resistance in prediabetic and exercised mice
Fatemeh Kazeminasab, Sayed Mohammad Marandi, Maryam Baharlooie, Mohammad Hossein Nasr-Esfahani, Kamran Ghaedi
Nutrition & Metabolism.2021;[Epub] CrossRef - Liver Fibrosis Indices for the Prediction of Mortality in Korean Subjects: A 16-Year Prospective Cohort Study
Tae Jung Oh, Kyuho Kim, Jae Hoon Moon, Sung Hee Choi, Nam H Cho, Hak Chul Jang
Journal of the Endocrine Society.2021;[Epub] CrossRef - Non-Laboratory-Based Simple Screening Model for Nonalcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Developed Using Multi-Center Cohorts
Jiwon Kim, Minyoung Lee, Soo Yeon Kim, Ji-Hye Kim, Ji Sun Nam, Sung Wan Chun, Se Eun Park, Kwang Joon Kim, Yong-ho Lee, Joo Young Nam, Eun Seok Kang
Endocrinology and Metabolism.2021; 36(4): 823. CrossRef - The association of hepatic steatosis and fibrosis with heart failure and mortality
Jiyun Park, Gyuri Kim, Hasung Kim, Jungkuk Lee, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Cardiovascular Diabetology.2021;[Epub] CrossRef - Magnetic Resonance-Based Assessments Better Capture Pathophysiologic Profiles and Progression in Nonalcoholic Fatty Liver Disease
Seung Joon Choi, Seong Min Kim, Yun Soo Kim, Oh Sang Kwon, Seung Kak Shin, Kyoung Kon Kim, Kiyoung Lee, Ie Byung Park, Cheol Soo Choi, Dong Hae Chung, Jaehun Jung, MunYoung Paek, Dae Ho Lee
Diabetes & Metabolism Journal.2021; 45(5): 739. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Eugene Han, Mi Kyung Kim, Byoung Kuk Jang, Hye Soon Kim
Diabetes & Metabolism Journal.2021; 45(5): 698. CrossRef - The potential pathophysiological role of altered lipid metabolism and electronegative low-density lipoprotein (LDL) in non-alcoholic fatty liver disease and cardiovascular diseases
Hüseyin Vural, Ferah Armutcu, Omer Akyol, Ralf Weiskirchen
Clinica Chimica Acta.2021; 523: 374. CrossRef - Increased Visit-to-Visit Liver Enzyme Variability Is Associated with Incident Diabetes: A Community-Based 12-Year Prospective Cohort Study
Kyuhoon Bang, Ji Eun Jun, In-Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung, You-Cheol Hwang
Diabetes & Metabolism Journal.2021; 45(6): 890. CrossRef - Efficacy and Safety of GLP-1 Receptor Agonists in Patients With Type 2 Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis
Yuan Zhu, Jiao Xu, Dong Zhang, Xingyu Mu, Yi Shi, Shangtao Chen, Zengxiang Wu, Shuangqing Li
Frontiers in Endocrinology.2021;[Epub] CrossRef - Triglyceride Glucose-Waist Circumference Is Superior to the Homeostasis Model Assessment of Insulin Resistance in Identifying Nonalcoholic Fatty Liver Disease in Healthy Subjects
Hwi Seung Kim, Yun Kyung Cho, Eun Hee Kim, Min Jung Lee, Chang Hee Jung, Joong-Yeol Park, Hong-Kyu Kim, Woo Je Lee
Journal of Clinical Medicine.2021; 11(1): 41. CrossRef - The association between nonalcoholic fatty liver disease and esophageal, stomach, or colorectal cancer: National population-based cohort study
Jung-Min Lee, Yong-Moon Park, Jae-Seung Yun, Yu-Bae Ahn, Kang-Moon Lee, Dae Bum Kim, Ji Min Lee, Kyungdo Han, Seung-Hyun Ko, Ming-Lung Yu
PLOS ONE.2020; 15(1): e0226351. CrossRef - Non-alcoholic steatohepatitis and progression of carotid atherosclerosis in patients with type 2 diabetes: a Korean cohort study
Hyeok-Hee Lee, Yongin Cho, Young Ju Choi, Byung Wook Huh, Byung-Wan Lee, Eun Seok Kang, Seok Won Park, Bong-Soo Cha, Eun Jig Lee, Yong-ho Lee, Kap Bum Huh
Cardiovascular Diabetology.2020;[Epub] CrossRef - Visceral-to-Subcutaneous Abdominal Fat Ratio Is Associated with Nonalcoholic Fatty Liver Disease and Liver Fibrosis
Chan-Hee Jung, Eun-Jung Rhee, Hyemi Kwon, Yoosoo Chang, Seungho Ryu, Won-Young Lee
Endocrinology and Metabolism.2020; 35(1): 165. CrossRef - Fatty liver index and development of cardiovascular disease in Koreans without pre-existing myocardial infarction and ischemic stroke: a large population-based study
Jun Hyung Kim, Jin Sil Moon, Seok Joon Byun, Jun Hyeok Lee, Dae Ryong Kang, Ki Chul Sung, Jang Young Kim, Ji Hye Huh
Cardiovascular Diabetology.2020;[Epub] CrossRef - Non-invasive diagnosis of nonalcoholic fatty liver disease: impact of age and other risk factors
Muharrem Bayrak
The Aging Male.2020; 23(5): 1275. CrossRef - Establishment of a Risk Prediction Model for Non-alcoholic Fatty Liver Disease in Type 2 Diabetes
Yali Zhang, Rong Shi, Liang Yu, Liping Ji, Min Li, Fan Hu
Diabetes Therapy.2020; 11(9): 2057. CrossRef - Noninvasive Evaluation of Nonalcoholic Fatty Liver Disease
Dae Ho Lee
Endocrinology and Metabolism.2020; 35(2): 243. CrossRef - Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Mellitus: A Position Statement of the Fatty Liver Research Group of the Korean Diabetes Association
Byung-Wan Lee, Yong-ho Lee, Cheol-Young Park, Eun-Jung Rhee, Won-Young Lee, Nan-Hee Kim, Kyung Mook Choi, Keun-Gyu Park, Yeon-Kyung Choi, Bong-Soo Cha, Dae Ho Lee
Diabetes & Metabolism Journal.2020; 44(3): 382. CrossRef - Sarcopenia is associated with non-alcoholic fatty liver disease in men with type 2 diabetes
D.H. Seo, Y.-h. Lee, S.W. Park, Y.J. Choi, B.W. Huh, E. Lee, K.B. Huh, S.H. Kim, B.-S. Cha
Diabetes & Metabolism.2020; 46(5): 362. CrossRef - Pharmacological Strategies for Insulin Sensitivity in Obesity and Cancer: Thiazolidinediones and Metformin
Luana A. Biondo, Alexandre A. S. Teixeira, Karen C. de O. S. Ferreira, Jose C. R. Neto
Current Pharmaceutical Design.2020; 26(9): 932. CrossRef -
Diabetes and Metabolism Journal in 2020: Good to Great
In-Kyung Jeong
Diabetes & Metabolism Journal.2020; 44(1): 1. CrossRef - Toll-like receptor 9, a possible blocker of non-alcoholic steatohepatitis?
Soung Won Jeong
Clinical and Molecular Hepatology.2020; 26(2): 185. CrossRef - The sex-specific effects of blood lead, mercury, and cadmium levels on hepatic steatosis and fibrosis: Korean nationwide cross-sectional study
Seung Min Chung, Jun Sung Moon, Ji Sung Yoon, Kyu Chang Won, Hyoung Woo Lee
Journal of Trace Elements in Medicine and Biology.2020; 62: 126601. CrossRef - Hepatic fibrosis is associated with total proteinuria in Korean patients with type 2 diabetes
Eugene Han, Yongin Cho, Kyung-won Kim, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-wan Lee
Medicine.2020; 99(33): e21038. CrossRef - Causal relationships between NAFLD, T2D and obesity have implications for disease subphenotyping
Zhipeng Liu, Yang Zhang, Sarah Graham, Xiaokun Wang, Defeng Cai, Menghao Huang, Roger Pique-Regi, Xiaocheng Charlie Dong, Y. Eugene Chen, Cristen Willer, Wanqing Liu
Journal of Hepatology.2020; 73(2): 263. CrossRef - Prevalence of Nonalcoholic Fatty Liver Disease (NAFLD) in Patients With Type 1 Diabetes Mellitus: A Systematic Review and Meta-Analysis
Marieke de Vries, Jan Westerink, Karin H A H Kaasjager, Harold W de Valk
The Journal of Clinical Endocrinology & Metabolism.2020; 105(12): 3842. CrossRef - Beneficial effect of anti-diabetic drugs for nonalcoholic fatty liver disease
Kyung-Soo Kim, Byung-Wan Lee
Clinical and Molecular Hepatology.2020; 26(4): 430. CrossRef - Nonalcoholic Fatty Liver Disease and Diabetes: An Epidemiological Perspective
Eun-Jung Rhee
Endocrinology and Metabolism.2019; 34(3): 226. CrossRef - Role of sodium-glucose co-transporter-2 inhibitors in the management of nonalcoholic fatty liver disease
Anastasia Kontana, Konstantinos Tziomalos
World Journal of Gastroenterology.2019; 25(28): 3664. CrossRef
- Mortality in metabolic dysfunction-associated steatotic liver disease: A nationwide population-based cohort study
- Complications
- Update on the Impact, Diagnosis and Management of Cardiovascular Autonomic Neuropathy in Diabetes: What Is Defined, What Is New, and What Is Unmet
- Vincenza Spallone
- Diabetes Metab J. 2019;43(1):3-30. Published online November 2, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0259
- 16,058 View
- 404 Download
- 153 Web of Science
- 157 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader The burden of diabetic cardiovascular autonomic neuropathy (CAN) is expected to increase due to the diabetes epidemic and its early and widespread appearance. CAN has a definite prognostic role for mortality and cardiovascular morbidity. Putative mechanisms for this are tachycardia, QT interval prolongation, orthostatic hypotension, reverse dipping, and impaired heart rate variability, while emerging mechanisms like inflammation support the pervasiveness of autonomic dysfunction. Efforts to overcome CAN under-diagnosis are on the table: by promoting screening for symptoms and signs; by simplifying cardiovascular reflex tests; and by selecting the candidates for screening. CAN assessment allows for treatment of its manifestations, cardiovascular risk stratification, and tailoring therapeutic targets. Risk factors for CAN are mainly glycaemic control in type 1 diabetes mellitus (T1DM) and, in addition, hypertension, dyslipidaemia, and obesity in type 2 diabetes mellitus (T2DM), while preliminary data regard glycaemic variability, vitamin B12 and D changes, oxidative stress, inflammation, and genetic biomarkers. Glycaemic control prevents CAN in T1DM, whereas multifactorial intervention might be effective in T2DM. Lifestyle intervention improves autonomic function mostly in pre-diabetes. While there is no conclusive evidence for a disease-modifying therapy, treatment of CAN manifestations is available. The modulation of autonomic function by SGLT2i represents a promising research field with possible clinical relevance.
-
Citations
Citations to this article as recorded by- Rectal sensitivity correlated with gastrointestinal‐mediated glucose disposal, but not the incretin effect
Sondre Meling, Erling Tjora, Heike Eichele, Rasmus B. Nedergaard, Filip K. Knop, Niels Ejskjaer, Siri Carlsen, Pål R. Njølstad, Christina Brock, Eirik Søfteland
Endocrinology, Diabetes & Metabolism.2024;[Epub] CrossRef - Glucose metabolism and autonomic function in healthy individuals and patients with type 2 diabetes mellitus at rest and during exercise
Takuto Hamaoka, Urs A. Leuenberger, Rachel C. Drew, Matthew Murray, Cheryl Blaha, Jonathan Carter Luck, Lawrence I. Sinoway, Jian Cui
Experimental Physiology.2024; 109(2): 214. CrossRef - Quantification of lipoproteins by proton nuclear magnetic resonance spectroscopy (1H-NMRS) improves the prediction of cardiac autonomic dysfunction in patients with type 1 diabetes
L. Nattero-Chávez, M. Insenser, N. Amigó, S. Samino, N. Martínez-Micaelo, B. Dorado Avendaño, A. Quintero Tobar, H. F. Escobar-Morreale, M. Luque-Ramírez
Journal of Endocrinological Investigation.2024;[Epub] CrossRef - Predictors of pacemaker requirement in patients with implantable loop recorder and unexplained syncope: A systematic review and meta‐analysis
Moein Zangiabadian, Kiarash Soltani, Yasaman Gholinejad, Reyhane Yahya, Shayan Bastami, Mohammad Ali Akbarzadeh, Mohammad Sharifian Ardestani, Azadeh Aletaha
Clinical Cardiology.2024;[Epub] CrossRef - Impaired Cardiovagal Activity as a Link Between Hyperglycemia and Arterial Stiffness in Adults With Type 2 Diabetes Mellitus Among an Eastern Indian Population: A Cross-sectional Study
Nibedita Priyadarsini, Devineni Likhitha, Madumathy Ramachandran, Kishore Kumar Behera
Canadian Journal of Diabetes.2024; 48(3): 147. CrossRef - No clear evidence of neuropathy among patients with high risk for the development of prediabetes/diabetes—a pilot study
Anna E. Körei, Magdolna Békeffy, Adrienn Menyhárt, Karola Osgyán, Ildikó Istenes, Viktor J. Horváth, Péter Kempler
Frontiers in Endocrinology.2024;[Epub] CrossRef - Effects of Physical Cues on Stem Cell-Derived Extracellular Vesicles toward Neuropathy Applications
Danyale Berry, Justice Ene, Aakash Nathani, Mandip Singh, Yan Li, Changchun Zeng
Biomedicines.2024; 12(3): 489. CrossRef - Oxidative stress, endothelial dysfunction, and N-acetylcysteine in type-2 diabetes mellitus
Xin Li, Junyong Zou, Aiping Lin, Jingshu Chi, Hong Hao, Hong Chen, Zhenguo Liu
Antioxidants & Redox Signaling.2024;[Epub] CrossRef - High dose cholecalciferol supplementation causing morning blood pressure reduction in patients with type 1 diabetes mellitus and cardiovascular autonomic neuropathy
João Felício, Lorena Moraes, Gabriela Lemos, Ícaro Souza, Giovana Vieira, Lilian Silva, Natércia Queiroz, Ana Carolina Souza, Franciane Melo, João Felício Abrahão Neto, Hana Britto, Manuela Lemos, Márcia Santos, Priscila Figueiredo, Ana Regina Motta, Meli
Scientific Reports.2024;[Epub] CrossRef - Transcutaneous vagal nerve stimulation for treating gastrointestinal symptoms in individuals with diabetes: a randomised, double-blind, sham-controlled, multicentre trial
Ditte S. Kornum, Davide Bertoli, Huda Kufaishi, Anne-Marie Wegeberg, Tina Okdahl, Esben B. Mark, Katrine L. Høyer, Jens B. Frøkjær, Birgitte Brock, Klaus Krogh, Christian S. Hansen, Filip K. Knop, Christina Brock, Asbjørn M. Drewes
Diabetologia.2024;[Epub] CrossRef - Independent and interactive associations of heart rate and obesity with type 2 diabetes mellites: A population‐based study
Tianxin Zhu, Qingyu Chen, Hongxing Chen, Lili You, Dan Liu, Xiaoyun Zhang, Feng Li, Hongshi Wu, Juying Tang, Diaozhu Lin, Kan Sun, Li Yan, Meng Ren
Journal of Diabetes.2024;[Epub] CrossRef - Bladder dysfunction in adolescents with type 1 diabetes
Vinni Faber Rasmussen, Mathilde Thrysøe, Páll Karlsson, Mette Madsen, Esben Thyssen Vestergaard, Jens Randel Nyengaard, Astrid Juhl Terkelsen, Konstantinos Kamperis, Kurt Kristensen
Journal of Pediatric Urology.2024;[Epub] CrossRef - Mortality risk factors in newly diagnosed diabetic cardiac autonomic neuropathy
Bruce A. Chase, Sylwia Pocica, Roberta Frigerio, Katerina Markopoulou, Demetrius M. Maraganore, Navamon Aunaetitrakul, Alexander Epshteyn, Alexandru C. Barboi
Clinical Autonomic Research.2023; 33(6): 903. CrossRef - Autonomic symptoms and associated factors in patients with chronic heart failure
Hellen Da Silva, Sofie Pardaens, Marc Vanderheyden, Johan De Sutter, Heleen Demeyer, Michel De Pauw, Laurent Demulier, Jan Stautemas, Patrick Calders
Acta Cardiologica.2023; 78(2): 203. CrossRef - Incretins and microvascular complications of diabetes: neuropathy, nephropathy, retinopathy and microangiopathy
Jonathan Goldney, Jack A. Sargeant, Melanie J. Davies
Diabetologia.2023; 66(10): 1832. CrossRef - Functional and morphometric assessment of small-fibre damage in late-onset hereditary transthyretin amyloidosis with polyneuropathy: the controversial relation between small-fibre-related symptoms and diagnostic test findings
Eleonora Galosi, Luca Leonardi, Pietro Falco, Giuseppe Di Pietro, Alessandra Fasolino, Nicoletta Esposito, Caterina Leone, Giulia Di Stefano, Maurizio Inghilleri, Marco Luigetti, Antonini Giovanni, Andrea Truini
Amyloid.2023; 30(1): 59. CrossRef - In vivo molecular imaging of cardiac angiogenesis in persons with and without type 2 diabetes: A cross‐sectional 68 Ga‐RGD‐PET study
Jens Christian Laursen, Ida Kirstine Bull Rasmussen, Emilie Hein Zobel, Philip Hasbak, Lene Holmvang, Christian Stevns Hansen, Bernt Johan von Scholten, Marie Frimodt‐Møller, Peter Rossing, Tine Willum Hansen, Andreas Kjaer, Rasmus Sejersten Ripa
Diabetic Medicine.2023;[Epub] CrossRef - Cardiac innervations in diabetes mellitus—Anatomical evidence of neuropathy
Natalija Filipović, Maja Marinović Guić, Vana Košta, Katarina Vukojević
The Anatomical Record.2023; 306(9): 2345. CrossRef - Clinical Predictors of Pacing Device Implantation in Implantable Cardiac Monitor Recipients for Unexplained Syncope
Reina Tonegawa-Kuji, Yuko Y. Inoue, Michikazu Nakai, Koshiro Kanaoka, Yoko Sumita, Yuichiro Miyazaki, Akinori Wakamiya, Keiko Shimamoto, Nobuhiko Ueda, Kenzaburo Nakajima, Naoya Kataoka, Mitsuru Wada, Kenichiro Yamagata, Kohei Ishibashi, Koji Miyamoto, Sa
CJC Open.2023; 5(4): 259. CrossRef - Cardiovascular autonomic reflex tests using a handheld device in the diagnosis of cardiovascular autonomic neuropathy in patients with schizophrenia
Laura Blok-Husum, Milka Ane Rank Brcelic, Hanin Kawa Farman Kawal Bassi, Svend Eggert Jensen, Rene Ernst Nielsen, Kristian Kragholm, Jesper Fleischer, Esben Laugesen, Christoffer Polcwiartek
American Heart Journal Plus: Cardiology Research and Practice.2023; 26: 100252. CrossRef - Causal association between vitamin D and diabetic neuropathy: a Mendelian randomization analysis
Wei Huang, Lei Gu, Jingwen Wang, Yiqi Wang, Fangzheng Cao, Tianyu Jin, Yifan Cheng
Endocrine.2023; 80(2): 328. CrossRef - Diabetes Mellitus and Heart Failure: Epidemiology, Pathophysiologic Mechanisms, and the Role of SGLT2 Inhibitors
Panagiotis Theofilis, Evangelos Oikonomou, Konstantinos Tsioufis, Dimitris Tousoulis
Life.2023; 13(2): 497. CrossRef - Sex differences and sex steroids influence on the presentation and severity of cardiovascular autonomic neuropathy of patients with type 1 diabetes
Lía Nattero-Chávez, María Insenser, Alejandra Quintero Tobar, Elena Fernández-Durán, Beatriz Dorado Avendaño, Tom Fiers, Jean-Marc Kaufman, Manuel Luque-Ramírez, Héctor F. Escobar-Morreale
Cardiovascular Diabetology.2023;[Epub] CrossRef - Early Gastrointestinal Neuropathy Assessed by Wireless Motility Capsules in Adolescents with Type 1 Diabetes
Vinni Faber Rasmussen, Mathilde Thrysøe, Páll Karlsson, Esben Thyssen Vestergaard, Kurt Kristensen, Ann-Margrethe Rønholt Christensen, Jens Randel Nyengaard, Astrid Juhl Terkelsen, Christina Brock, Klaus Krogh
Journal of Clinical Medicine.2023; 12(5): 1925. CrossRef - Heart rate variability in people with metabolic syndrome
Kostiantyn Apykhtin, Svitlana Drozdovska, Olha Hurenko, Anastasiia Nahorna, Anatoly Pisaruk, Yuliia Panchenko, Olena Andrieieva
Ageing & Longevity.2023; (1 2023): 1. CrossRef - Heart rate variability in people with metabolic syndrome
Kostiantyn Apykhtin, Svitlana Drozdovska, Olha Hurenko, Anastasiia Nahorna, Anatoly Pisaruk, Yuliia Panchenko, Olena Andrieieva
JOURNAL OF THE NATIONAL ACADEMY OF MEDICAL SCIENCES OF UKRAINE.2023; (1 2023): 1. CrossRef - Potential of electronic devices for detection of health problems in older adults at home: A systematic review and meta-analysis
Yu-ting Cao, Xin-xin Zhao, Yi-ting Yang, Shi-jie Zhu, Liang-dong Zheng, Ting Ying, Zhou Sha, Rui Zhu, Tao Wu
Geriatric Nursing.2023; 51: 54. CrossRef - Diabetes mellitus in der Akut- und Notfallmedizin
Leo Benning, Julian Krehl, Felix Patricius Hans
Notfallmedizin up2date.2023; 18(01): 45. CrossRef - Correlation between Heart rate recovery and Left Atrial phasic functions evaluated by 2D speckle-tracking Echocardiography after Acute Myocardial infarction
Behruz Mashayekhi, Reza Mohseni-Badalabadi, Ali Hosseinsabet, Tahereh Ahmadian
BMC Cardiovascular Disorders.2023;[Epub] CrossRef - Pancreatic sympathetic innervation disturbance in type 1 diabetes
Senlin Li, Huimin Yuan, Keshan Yang, Qing Li, Ming Xiang
Clinical Immunology.2023; 250: 109319. CrossRef - A Nonrandomized Trial of the Effects of Passive Simulated Jogging on Short-Term Heart Rate Variability in Type 2 Diabetic Subjects
Jose A. Adams, Jose R. Lopez, Veronica Banderas, Marvin A. Sackner, Mark Yorek
Journal of Diabetes Research.2023; 2023: 1. CrossRef - Evaluating treatment options for cardiovascular autonomic neuropathy in patients with diabetes mellitus: a systematic review
Jasmine KaiLi Goh, Leroy Koh
Diabetology International.2023; 14(3): 224. CrossRef - Autonomic neuropathic symptoms in patients with diabetes: practical tools for screening in daily routine
Ana Raquel Souza de Azevedo Vieira, Lara Benigno Porto-Dantas, Flaviene Alves do Prado Romani, Patrícia Souza Carvalho, Rodica Pop-Busui, Hermelinda Cordeiro Pedrosa
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - “Arterial stiffness is not associated with changes in the circadian pattern of blood pressure in patients with type 1 diabetes mellitus and cardiovascular autonomic dysfunction”
Lía Nattero-Chávez, Ane Bayona Cebada, Elena Fernández-Durán, Alejandra Quintero Tobar, Beatriz Dorado Avendaño, Héctor Escobar-Morreale, Manuel Luque-Ramírez
Diabetes and Vascular Disease Research.2023; 20(3): 147916412311736. CrossRef - Frontiers in diagnostic and therapeutic approaches in diabetic sensorimotor neuropathy (DSPN)
Sanjeev Sharma, Gerry Rayman
Frontiers in Endocrinology.2023;[Epub] CrossRef - In Type 2 Diabetes Mellitus, normalization of hemoglobin A1c accompanies reduced sensitivity to pressure at the sternum
Jens Faber, Søren Ballegaard, Nanna Ørsted, Ebbe Eldrup, Benny Karpatschof, Finn Gyntelberg, Sofie Korsgaard Hecquet, Albert Gjedde
Frontiers in Neuroscience.2023;[Epub] CrossRef - Functional status associated with postural dizziness, but not postural hypotension, in older adults: a community-based study
Hsiang-Ju Cheng, Zih-Jie Sun, Feng-Hwa Lu, Yi-Ching Yang, Chih-Jen Chang, Jin-Shang Wu
BMC Geriatrics.2023;[Epub] CrossRef - Effects of baricitinib, empagliflozin, linagliptin and telmisartan on cardiovascular autonomic neuropathy in type 1 diabetes: An exploratory, randomized, open‐label, crossover trial
Jens Christian Laursen, Viktor Rotbain Curovic, Marjolein Y. A. M. Kroonen, Niels Jongs, Emilie H. Zobel, Tine W. Hansen, Marie Frimodt‐Møller, Gozewijn D. Laverman, Adriaan Kooy, Frederik Persson, Hiddo J. L. Heerspink, Christian Stevns Hansen, Peter Ros
Diabetes, Obesity and Metabolism.2023; 25(10): 3064. CrossRef - The Retinal Nerve Fiber Layer Thickness Is Associated with Systemic Neurodegeneration in Long-Term Type 1 Diabetes
Christina Brock, Anne-Marie Wegeberg, Thomas Arendt Nielsen, Bassam Karout, Per M. Hellström, Asbjørn Mohr Drewes, Henrik Vorum
Translational Vision Science & Technology.2023; 12(6): 23. CrossRef - The Use of Empirical Mode Decomposition on Heart Rate Variability Signals to Assess Autonomic Neuropathy Progression in Type 2 Diabetes
Sandra Cossul, Felipe Rettore Andreis, Mateus Andre Favretto, Jefferson Luiz Brum Marques
Applied Sciences.2023; 13(13): 7824. CrossRef - Topical capsaicin for the management of painful diabetic neuropathy: a narrative systematic review
Brandon Goodwin, Maanas Chiplunkar, Ryan Salerno, Kylon Coombs, Umar Sannoh, Vrushank Shah, Nicholas Averell, Usmaan Al-Shebab, Deanna Janora
Pain Management.2023; 13(5): 309. CrossRef - Adynamic response to cold pain reflects dysautonomia in type 1 diabetes and polyneuropathy
Thomas Arendt Nielsen, Søren Lundbye-Christensen, Yoanna Krasimirova Dimitrova, Sam Riahi, Birgitte Brock, Asbjørn Mohr Drewes, Christina Brock
Scientific Reports.2023;[Epub] CrossRef - Autonomic Nerve Function Tests in Patients with Diabetes
Heung Yong Jin, Tae Sun Park
The Journal of Korean Diabetes.2023; 24(2): 71. CrossRef - Understanding the role of hyperglycemia and the molecular mechanism associated with diabetic neuropathy and possible therapeutic strategies
Mandeep Kaur, Sakshi Misra, Priyanka Swarnkar, Preeti Patel, Balak Das Kurmi, Ghanshyam Das Gupta, Amrita Singh
Biochemical Pharmacology.2023; 215: 115723. CrossRef - A three-month physical training program improves cardiovascular autonomic function in patients with metabolic syndrome with and without diabetes – a pilot study
Anna Vágvölgyi, Judit Erzsébet Ábrahám, Éva Máthéné Köteles, Andrea Korom, Mária Barnai, Mónika Szűcs, Andrea Orosz, Péter Kempler, Adrienn Menyhárt, Attila Nemes, Tamás Várkonyi, István Baczkó, István Kósa, Csaba Lengyel
Frontiers in Endocrinology.2023;[Epub] CrossRef - Cardiovascular autonomic neuropathy in patients with type 2 diabetes with and without sensorimotor polyneuropathy
Emil Peters, Mustapha Itani, Alexander G. Kristensen, Astrid Juhl Terkelsen, Thomas Krøigård, Hatice Tankisi, Troels S. Jensen, Nanna B. Finnerup, Sandra Sif Gylfadottir
Journal of the Peripheral Nervous System.2023; 28(3): 450. CrossRef - Cardiac Autonomic Neuropathy in Prediabetes: A Case-Control Study
Pavan Gujjar, Y. S. Ravikumar, Lakshmi Nagendra, Hiya Boro, Saptarshi Bhattacharya
Indian Journal of Endocrinology and Metabolism.2023; 27(4): 325. CrossRef - Diabetic Neuropathies
Melissa A. Elafros, Brian C. Callaghan
CONTINUUM: Lifelong Learning in Neurology.2023; 29(5): 1401. CrossRef - Determinants of the heart rate variability in type 1 diabetes mellitus
Máté Hajdu, Konstandia Garmpis, Vivien Vértes, Noémi Vorobcsuk-Varga, Gergő Attila Molnár, László Hejjel, István Wittmann, Réka Faludi
Frontiers in Endocrinology.2023;[Epub] CrossRef - The Effect of Exercise on Cardiovascular Autonomic Nervous Function in Patients with Diabetes: A Systematic Review
Hidetaka Hamasaki
Healthcare.2023; 11(19): 2668. CrossRef - Influence of Fibrinogen/Albumin Ratio and Fibrinogen/Pre-Albumin Ratio on Cardiac Autonomic Neuropathy in Type 2 Diabetes
Subei Zhao, Zheng Yang, Meng Yu, Linyu Xiang, Yuhuan Lv, Chunyan Tian, Rong Li
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 3249. CrossRef - In Ischemic Heart Disease, Reduced Sensitivity to Pressure at the Sternum Accompanies Lower Mortality after Five Years: Evidence from a Randomized Controlled Trial
Søren Ballegaard, Jens Faber, Christian Selmer, Finn Gyntelberg, Svend Kreiner, Benny Karpatschof, Tobias Wirenfeldt Klausen, Åke Hjalmarson, Albert Gjedde
Journal of Clinical Medicine.2023; 12(24): 7585. CrossRef - Assessment of the relationship of systemic vascular dysfunction and cardiac autonomic neuropathy (CAN) with diabetic retinopathy
KJ Hari Prakash, Sucheta Parija, Manisha Kar
Journal of Family Medicine and Primary Care.2023; 12(12): 3236. CrossRef - Autonomic Neuropathy in Ambulatory Type 2 Diabetes Mellitus Patients: A Single-arm Prospective, Observational Study
Kaustav Saha, Shatavisa Mukherjee, Animesh Maiti, Santanu Kumar Tripathi
Journal of the Practice of Cardiovascular Sciences.2023; 9(3): 178. CrossRef - Insomnia and type 2 diabetes: how to help the patient. Modern view of a neurologist
E. S. Akarachkova, O. V. Kotova, V. L. Klimov, D. I. Lebedeva
FOCUS. Endocrinology.2023; 4(4): 12. CrossRef - Carvedilol improves heart rate variability indices, biomarkers but not cardiac nerve density in streptozotocin-induced T2DM model of diabetic cardiac autonomic neuropathy
Olawale Mathias Akinlade, Bamidele Owoyele, Olufemi Ayodele Soladoye
Journal of Basic and Clinical Physiology and Pharmacology.2022; 33(2): 213. CrossRef - Cardiovascular autonomic responses during head-up tilt test in newly diagnosed type 2 diabetes
Esteban Jorge-Galarza, Margarita Torres-Tamayo, María del Rocío Martínez-Alvarado, Berenice Peña-Aparicio, Carmen González-Salazar, Juan Reyes-Barrera, Manuel Sierra-Beltrán, Erika Fajardo-Flores, Andrey Kostin, J. Antonio González-Hermosillo
Irish Journal of Medical Science (1971 -).2022; 191(5): 2077. CrossRef - Cardiovascular autonomic neuropathy and incident diabetic kidney disease in patients with type 2 diabetes
Ji Eun Jun, Min Sun Choi, Jae Hyeon Kim
Diabetes Research and Clinical Practice.2022; 184: 109181. CrossRef - Kardiovaskuläre Risiken in der 4.–6. Lebensdekade mit Diabetes mellitus Typ 1
Young Hee Lee-Barkey, Bernd Stratmann, Diethelm Tschöpe
Der Diabetologe.2022; 18(2): 131. CrossRef - Mechanisms of cardiac dysfunction in diabetic cardiomyopathy: molecular abnormalities and phenotypical variants
Francesca Romana Prandi, Isabella Evangelista, Domenico Sergi, Alberto Palazzuoli, Francesco Romeo
Heart Failure Reviews.2022; 28(3): 597. CrossRef - Comparison of Risk Assessment Strategies for Patients with Diabetes Mellitus and Stable Chest Pain: A Coronary Computed Tomography Angiography Study
Jia Zhao, Shuo Wang, Pengyu Zhao, Yong Huo, Chunjie Li, Jia Zhou, Pawel Kleczynski
Journal of Diabetes Research.2022; 2022: 1. CrossRef - BOND study: a randomised double-blind, placebo-controlled trial over 12 months to assess the effects of benfotiamine on morphometric, neurophysiological and clinical measures in patients with type 2 diabetes with symptomatic polyneuropathy
Gidon J Bönhof, Gundega Sipola, Alexander Strom, Christian Herder, Klaus Strassburger, Birgit Knebel, Claudia Reule, Jan-Christoph Wollmann, Andrea Icks, Hadi Al-Hasani, Michael Roden, Oliver Kuss, Dan Ziegler
BMJ Open.2022; 12(2): e057142. CrossRef - Pragmatic Clinic-Based Investigation of Glycemic Variability in Patients With Type 1 Diabetes in Routine Clinical Practice and Its Association With Cardiovascular Autonomic Neuropathy: A Pilot Study
Lucianne R.M. Tannus, Marilia B. Gomes
Endocrine Practice.2022; 28(5): 465. CrossRef - Longitudinal effects of one‐leg standing time on neuropathy outcomes in association with glycemic control in non‐elderly patients with type 2 diabetes
Kazuhiro Sugimoto, Takashi Sozu, Takehiko Hoshino, Yuko Watanabe, Akira Tamura, Toshiro Yamazaki, Setsu Ohta, Susumu Suzuki, Takuro Shimbo
Journal of Diabetes Investigation.2022; 13(6): 1039. CrossRef - Thermal quantitative sensory testing as a screening tool for cardiac autonomic neuropathy in patients with diabetes mellitus
Veronika Potockova, Sarka Mala, Lucie Hoskovcova, Vaclav Capek, Tomas Nedelka, Lucie Riedlbauchova, Daniel Baumgartner, Livie Mensova, Radim Mazanec
Brain and Behavior.2022;[Epub] CrossRef - Cardiovascular Autonomic Reflex Tests and 7 Heart Rate Variability Indices for Early Diagnosis of Cardiovascular Autonomic Neuropathy in Type 2 Diabetes Individuals
Yeelen Ballesteros Atala, Mozânia Reis De Matos, Denise Engelbrecht Zantut-Wittmann, Alejandro Rosell Castillo, Daniele P Santos-Bezerra, Maria Lucia Correa-Giannella, Maria Cândida Ribeiro Parisi
Current Diabetes Reviews.2022;[Epub] CrossRef - Design, synthesis, in vitro and in silico studies of naproxen derivatives as dual lipoxygenase and α-glucosidase inhibitors
Asma Sardar, Obaid-ur-Rahman Abid, Saima Daud, M. Fakhar-e-Alam, Muhammad Hussnain Siddique, Muhammad Ashraf, Wardah Shahid, Syeda Abida Ejaz, M. Atif, Shafiq Ahmad, Sulman Shafeeq, Muhammad Afzal
Journal of Saudi Chemical Society.2022; 26(3): 101468. CrossRef - Clinical manifestations and evaluation of cardiac autonomic neuropathy in diabetes mellitus and metabolic syndrome
L. S. Moshkhoeva, A. N. Barinov
Neurology, Neuropsychiatry, Psychosomatics.2022; 14(2): 71. CrossRef - The relationship between vitamin B12 levels and electrocardiographic ventricular repolarization markers
Emre Yılmaz, Devrim Kurt, Aslı Vural, Ertan Aydın, Sencer Çamcı, Ercan Aydın
Nutrición Hospitalaria.2022;[Epub] CrossRef - The effect of liraglutide on cardiac autonomic function in type 2 diabetes: A prespecified secondary analysis from the LIRAFLAME randomized, double‐blinded, placebo‐controlled trial
Suvanjaa Sivalingam, Emilie Hein Zobel, Christian S. Hansen, Rasmus S. Ripa, Bernt J. von Scholten, Viktor Rotbain Curovic, Andreas Kjaer, Jacob K. Jensen, Tine W. Hansen, Peter Rossing
Diabetes, Obesity and Metabolism.2022; 24(8): 1638. CrossRef - Heart Rate Variability and Chronic Kidney Disease in Patients with Type 2 Diabetes
Wei Shi, Jing Zhang, Dan Chen, Xiaolei Chen, Wei Duan, Hongmei Zhang, Fahd Abd Algalil
Applied Bionics and Biomechanics.2022; 2022: 1. CrossRef - Spectrum of cardiac autonomic neuropathy in patients with type 2 diabetes mellitus: A North India perspective
PrativaPriyadarshani Sethi, Basavraj Jatteppanavar, Ravi Kant, Monika Pathania, MukeshChand Bairwa
Journal of Cardio-diabetes and metabolic disorders.2022; 2(1): 23. CrossRef - Cardiac Autonomic Dysfunction Is Associated With Risk of Diabetic Kidney Disease Progression in Type 2 Diabetes Mellitus
Haixia Zeng, Jianmo Liu, Zheng Chen, Peng Yu, Jianping Liu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Diagnostic Tools, Biomarkers, and Treatments in Diabetic polyneuropathy
and Cardiovascular Autonomic Neuropathy
Gidon J. Bönhof, Christian Herder, Dan Ziegler
Current Diabetes Reviews.2022;[Epub] CrossRef - Triglyceride glucose index is related with cardiac autonomic dysfunction in patients with metabolic syndrome
Akif Serhat Balcıoğlu, Ekrem Aksu, Ahmet Çağrı Aykan
Kardiologiia.2022; 62(6): 45. CrossRef - Pathogenesis of Distal Symmetrical Polyneuropathy in Diabetes
Sasha Smith, Pasha Normahani, Tristan Lane, David Hohenschurz-Schmidt, Nick Oliver, Alun Huw Davies
Life.2022; 12(7): 1074. CrossRef - Correlation between impaired hemodynamic response and cardiopulmonary fitness in middle-aged type 2 diabetes mellitus patients: a case–control study
Jinjin Xie, Lianhua Yin, Jia Huang, Ying Xu, Yannan Chen, Jiawei Qin, Zhizhen Liu, Jing Tao
European Journal of Applied Physiology.2022; 122(10): 2295. CrossRef - Higher frequency of cardiovascular autonomic neuropathy in youth with type 2 compared to type 1 diabetes: Role of cardiometabolic risk factors
Benjamin J. Varley, Megan L. Gow, Yoon Hi Cho, Paul Benitez‐Aguirre, Janine Cusumano, Alison Pryke, Albert Chan, Vallimayil Velayutham, Kim C. Donaghue, Maria E. Craig
Pediatric Diabetes.2022; 23(7): 1073. CrossRef - The role of protein kinase C in diabetic microvascular complications
Deng Pan, Lin Xu, Ming Guo
Frontiers in Endocrinology.2022;[Epub] CrossRef - Effect of SGLT-2 inhibitors on cardiac autonomic function in type 2 diabetes mellitus: a meta-analysis of randomized controlled trials
Dimitrios Patoulias, Alexandra Katsimardou, Nikolaos Fragakis, Christodoulos Papadopoulos, Michael Doumas
Acta Diabetologica.2022; 60(1): 1. CrossRef - Association between blood glucose levels and autonomic symptoms in Peru
Gabriel Angeles-Zurita, Margorie Narro-Fuentes, Antonio Bernabe-Ortiz
Primary Care Diabetes.2022; 16(5): 709. CrossRef - Clinical scoring systems for the risk of cardiovascular autonomic neuropathy in type 1 and type 2 diabetes: A simple tool
Marika Menduni, Cinzia D'Amato, Martina Leoni, Valentina Izzo, Mariateresa Staltari, Carla Greco, Andrea Abbatepassero, Giuseppe Seminara, Ilenia D'Ippolito, Davide Lauro, Vincenza Spallone
Journal of the Peripheral Nervous System.2022; 27(4): 259. CrossRef - Vagus nerve stimulation as a novel treatment for systemic lupus erythematous: study protocol for a randomised, parallel-group, sham-controlled investigator-initiated clinical trial, the SLE-VNS study
Amanda Hempel Zinglersen, Ida Lynghøj Drange, Katrine Aagaard Myhr, Andreas Fuchs, Mogens Pfeiffer-Jensen, Christina Brock, Søren Jacobsen
BMJ Open.2022; 12(9): e064552. CrossRef - To the interpretation of frequency components of the heart rate variability
N. V. Kuzmenko, V. A. Tsyrlin, M. G. Pliss
Translational Medicine.2022; 9(3): 35. CrossRef - Protein pyrrole adducts are associated with elevated glucose indices and clinical features of diabetic diffuse neuropathies
Xiao Chen, Zhuyi Jiang, Lianjing Zhang, Wei Liu, Xiaohu Ren, Luling Nie, Desheng Wu, Zhiwei Guo, Weimin Liu, Xifei Yang, Yan Wu, Zhen Liang, Peter Spencer, Jianjun Liu
Journal of Diabetes.2022; 14(10): 646. CrossRef - Cardiac Autonomic Neuropathy in Type 1 and 2 Diabetes: Epidemiology, Pathophysiology, and Management
Scott Williams, Siddig Abdel Raheim, Muhammad Ilyas Khan, Umme Rubab, Prathap Kanagala, Sizheng Steven Zhao, Anne Marshall, Emily Brown, Uazman Alam
Clinical Therapeutics.2022; 44(10): 1394. CrossRef - Pathophysiological and clinical aspects of the circadian rhythm of arterial stiffness in diabetes mellitus: A minireview
Victoria A. Serhiyenko, Ludmila M. Serhiyenko, Volodymyr B. Sehin, Alexandr A. Serhiyenko
Endocrine Regulations.2022; 56(4): 284. CrossRef - Heart rate-corrected QT interval prolongation is associated with decreased heart rate variability in patients with type 2 diabetes
Seon-Ah Cha
Medicine.2022; 101(45): e31511. CrossRef - Effect of the Glucagon-Like Peptide-1 Receptor Agonists on Autonomic Function in Subjects with Diabetes: A Systematic Review and Meta-Analysis
Carla Greco, Daniele Santi, Giulia Brigante, Chiara Pacchioni, Manuela Simoni
Diabetes & Metabolism Journal.2022; 46(6): 901. CrossRef - Diabetes-Induced Cardiac Autonomic Neuropathy: Impact on Heart Function and Prognosis
Susumu Z. Sudo, Tadeu L. Montagnoli, Bruna de S. Rocha, Aimeé D. Santos, Mauro P. L. de Sá, Gisele Zapata-Sudo
Biomedicines.2022; 10(12): 3258. CrossRef - The Relationship Between Orthostatic Hypotension and Vitamin D Deficiency in Patients with Uncontrolled Type 2 Diabetes Mellitus
Ece YİĞİT, Ridvan SİVRİTEPE, Dilay KARABULUT, Umut KARABULUT
Online Türk Sağlık Bilimleri Dergisi.2022; 7(2): 313. CrossRef - A study of heart rate variability in diabetic mellitus patients
Srinivasa Jayachandra, Satyanath Reddy Kodidala
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(3): 153. CrossRef - The prevalence of cardiac autonomic neuropathy in prediabetes: a systematic review
Aikaterini Eleftheriadou, Scott Williams, Sarah Nevitt, Emily Brown, Rebecca Roylance, John P. H. Wilding, Daniel J. Cuthbertson, Uazman Alam
Diabetologia.2021; 64(2): 288. CrossRef - Risk of cardiac autonomic neuropathy in latent autoimmune diabetes in adults is similar to type 1 diabetes and lower compared to type 2 diabetes: A cross‐sectional study
Ernesto Maddaloni, Chiara Moretti, Rossella Del Toro, Sara Sterpetti, Maria Vittoria Ievolella, Gabriele Arnesano, Rocky Strollo, Silvia Irina Briganti, Luca D'Onofrio, Paolo Pozzilli, Raffaella Buzzetti
Diabetic Medicine.2021;[Epub] CrossRef - Effects of lunar cycle on fasting plasma glucose, heart rate and blood pressure in type 2 diabetic patients
Sutanu Dutta Chowdhury, Subhasish Pramanik, Koena Bhattacharjee, Lakshmi Kanta Mondal
Chronobiology International.2021; 38(2): 270. CrossRef - Intensive Risk Factor Management and Cardiovascular Autonomic Neuropathy in Type 2 Diabetes: The ACCORD Trial
Yaling Tang, Hetal Shah, Carlos Roberto Bueno Junior, Xiuqin Sun, Joanna Mitri, Maria Sambataro, Luisa Sambado, Hertzel C. Gerstein, Vivian Fonseca, Alessandro Doria, Rodica Pop-Busui
Diabetes Care.2021; 44(1): 164. CrossRef - Decreased glomerular filtration rate and increased albuminuria for identification of cardiovascular autonomic neuropathy in subjects with and without diabetes
Ying-Chuen Lai, Hung-Yuan Li, Yi-Dier Jiang, Tien-Jyun Chang, Lee-Ming Chuang
Autonomic Neuroscience.2021; 230: 102757. CrossRef - Exposures influencing the developing central autonomic nervous system
Sarah D. Schlatterer, Adre J. du Plessis
Birth Defects Research.2021; 113(11): 845. CrossRef - Vitamin B12 Supplementation in Diabetic Neuropathy: A 1-Year, Randomized, Double-Blind, Placebo-Controlled Trial
Triantafyllos Didangelos, Eleni Karlafti, Evangelia Kotzakioulafi, Eleni Margariti, Parthena Giannoulaki, Georgios Batanis, Solomon Tesfaye, Kοnstantinos Kantartzis
Nutrients.2021; 13(2): 395. CrossRef - The Association Between Continuous Glucose Monitoring-Derived Metrics and Cardiovascular Autonomic Neuropathy in Outpatients with Type 2 Diabetes
Min Young Kim, Gyuri Kim, Ji Yun Park, Min Sun Choi, Ji Eun Jun, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2021; 23(6): 434. CrossRef - Insulin resistance is independently associated with cardiovascular autonomic neuropathy in type 2 diabetes
Yingshan Liu, Yu Peng, Jing Jin, Yanshan Chen, Chuna Chen, Zhenguo Chen, Haishan Huang, Lingling Xu
Journal of Diabetes Investigation.2021; 12(9): 1651. CrossRef - SGLT2 inhibitors and the autonomic nervous system in diabetes: A promising challenge to better understand multiple target improvement
Vincenza Spallone, Paul Valensi
Diabetes & Metabolism.2021; 47(4): 101224. CrossRef - Reduction of Pressure Pain Sensitivity as Novel Non-pharmacological Therapeutic Approach to Type 2 Diabetes: A Randomized Trial
Jens Faber, Ebbe Eldrup, Christian Selmer, Caroline Pichat, Sofie Korsgaard Hecquet, Torquil Watt, Svend Kreiner, Benny Karpatschof, Finn Gyntelberg, Søren Ballegaard, Albert Gjedde
Frontiers in Neuroscience.2021;[Epub] CrossRef - Relationship between cardiac autonomic neuropathy and cardio-metabolic risk profile in adults with type 1 diabetes
M. Serdarova, R. Dimova, N. Chakarova, G. Grozeva, A. Todorova, T. Tankova
Diabetes Research and Clinical Practice.2021; 174: 108721. CrossRef - Differences and Similarities in Neuropathy in Type 1 and 2 Diabetes: A Systematic Review
Mar Sempere-Bigorra, Iván Julián-Rochina, Omar Cauli
Journal of Personalized Medicine.2021; 11(3): 230. CrossRef - Assessment of Gastrointestinal Autonomic Dysfunction: Present and Future Perspectives
Ditte S. Kornum, Astrid J. Terkelsen, Davide Bertoli, Mette W. Klinge, Katrine L. Høyer, Huda H. A. Kufaishi, Per Borghammer, Asbjørn M. Drewes, Christina Brock, Klaus Krogh
Journal of Clinical Medicine.2021; 10(7): 1392. CrossRef - Diabetic heart disease: A clinical update
Jake Rajbhandari, Cornelius James Fernandez, Mayuri Agarwal, Beverly Xin Yi Yeap, Joseph M Pappachan
World Journal of Diabetes.2021; 12(4): 383. CrossRef - Novel and Emerging Electrophysiological Biomarkers of Diabetic Neuropathy and Painful Diabetic Neuropathy
Anne Marshall, Uazman Alam, Andreas Themistocleous, Nigel Calcutt, Andrew Marshall
Clinical Therapeutics.2021; 43(9): 1441. CrossRef - Cardiac Autonomic Neuropathy Is Not Reversed by Euglycemia Following Islet Transplantation
Tejas Deshmukh, Peter Emerson, Patricia Anderson, Eddy Kizana, Philip J. O’Connell, D. Jane Holmes-Walker, James J.H. Chong
Transplantation.2021; 105(5): 1125. CrossRef - Attenuation of Muscle Mass and Density Is Associated With Poor Outcomes Among Patients Undergoing Major Gynecologic Surgery: A Retrospective Cohort Study
Lu Che, Yan Zhang, Jiawen Yu, Li Xu, Yuguang Huang
Anesthesia & Analgesia.2021; 132(6): 1692. CrossRef - Association of Urinary N-Acetyl-β-D-Glucosaminidase with Cardiovascular Autonomic Neuropathy in Type 1 Diabetes Mellitus without Nephropathy
Min Sun Choi, Ji Eun Jun, Sung Woon Park, Jee Hee Yoo, Jiyeon Ahn, Gyuri Kim, Sang-Man Jin, Kyu Yeon Hur, Moon-Kyu Lee, Jae Hyeon Kim
Diabetes & Metabolism Journal.2021; 45(3): 349. CrossRef - Pathogenesis, diagnosis and clinical management of diabetic sensorimotor peripheral neuropathy
Gordon Sloan, Dinesh Selvarajah, Solomon Tesfaye
Nature Reviews Endocrinology.2021; 17(7): 400. CrossRef - Heart Rate Variability as a Potential Non-invasive Marker of Blood Glucose Level
L. R. Jarman, J. L. Elliott, T. Lees, R. Clifton-Bligh, A. M. Simpson, N. Nassif, S. Lal
Human Physiology.2021; 47(2): 209. CrossRef - Cardiovascular autonomic neuropathy in diabetes: Pathophysiology, clinical assessment and implications
Alice Duque, Mauro Felippe Felix Mediano, Andrea De Lorenzo, Luiz Fernando Rodrigues Jr
World Journal of Diabetes.2021; 12(6): 855. CrossRef - Gaussian process-based kernel as a diagnostic model for prediction of type 2 diabetes mellitus risk using non-linear heart rate variability features
R. Shashikant, Uttam Chaskar, Leena Phadke, Chetankumar Patil
Biomedical Engineering Letters.2021; 11(3): 273. CrossRef - Possible Preventative/Rehabilitative Role of Gliflozins in OSA and T2DM. A Systematic Literature Review-Based Hypothesis
Vincenzo Maria Monda, Francesca Porcellati, Felice Strollo, Alessandro Fucili, Marcello Monesi, Ersilia Satta, Sandro Gentile
Advances in Therapy.2021; 38(8): 4195. CrossRef - Characteristics of cardiovascular autonomic dysfunction and association with quality of life in patients with systemic lupus erythematosus
Amanda Hempel Zinglersen, Katrine Kjær Iversen, Henrik Christian Bidstrup Leffers, Esben Laugesen, Jesper Fleischer, Søren Jacobsen
Lupus Science & Medicine.2021; 8(1): e000507. CrossRef - Impaired vagal adaptation to an exercise task in women with gestational diabetes mellitus versus women with uncomplicated pregnancies
Marieta P. Theodorakopoulou, Areti Triantafyllou, Andreas Zafeiridis, Afroditi Κ. Boutou, Iris Grigoriadou, Evangelia Kintiraki, Stella Douma, Dimitrios G. Goulis, Konstantina Dipla
Hormones.2021; 20(4): 753. CrossRef - Cardioprotective Effects of Sodium-glucose Cotransporter 2 Inhibitors Regardless of Type 2 Diabetes Mellitus: A Meta-analysis
Lucas Silva Sousa, Felipe de Araújo Nascimento, Juliano Rocha, Michelle Rocha-Parise
International Journal of Cardiovascular Sciences.2021;[Epub] CrossRef - Management of diabetic neuropathy
Simona Cernea, Itamar Raz
Metabolism.2021; 123: 154867. CrossRef - Large fibre, small fibre and autonomic neuropathy in adolescents with type 1 diabetes: A systematic review
Vinni Faber Rasmussen, Troels Staehelin Jensen, Hatice Tankisi, Páll Karlsson, Esben Thyssen Vestergaard, Kurt Kristensen, Jens Randel Nyengaard, Astrid Juhl Terkelsen
Journal of Diabetes and its Complications.2021; 35(11): 108027. CrossRef - Cardiovascular Risk Management in Type 1 Diabetes
I. H. Teoh, P. Elisaus, J. D. Schofield
Current Diabetes Reports.2021;[Epub] CrossRef - Disturbances in the intraventricular conduction system in teenagers with type 1 diabetes. A pilot study
Agnieszka Zubkiewicz-Kucharska, Anna Noczyńska, Małgorzata Sobieszczańska, Małgorzata Poręba, Joanna Chrzanowska, Rafał Poręba, Monika Seifert, Anna Janocha, Krystyna Laszki-Szcząchor
Journal of Diabetes and its Complications.2021; 35(11): 108043. CrossRef - Peripheral and Autonomic Neuropathy Status of Young Patients With Type 1 Diabetes Mellitus at the Time of Transition From Pediatric Care to Adult-Oriented Diabetes Care
Anna Vágvölgyi, Ágnes Maróti, Mónika Szűcs, Csongor Póczik, Dóra Urbán-Pap, István Baczkó, Attila Nemes, Éva Csajbók, Krisztián Sepp, Péter Kempler, Andrea Orosz, Tamás Várkonyi, Csaba Lengyel
Frontiers in Endocrinology.2021;[Epub] CrossRef - Pancreatic exocrine insufficiency in diabetes is associated with autonomic dysfunction
Dag André Sangnes, Elisabeth Sandvik Bergmann, Rose Marie Moss, Trond Engjom, Eirik Søfteland
Scandinavian Journal of Gastroenterology.2021; 56(10): 1222. CrossRef - Dependence of Heart Rate Variability Indices on the Mean Heart Rate in Women with Well-Controlled Type 2 Diabetes
Adriana Robles-Cabrera, José M. Torres-Arellano, Ruben Fossion, Claudia Lerma
Journal of Clinical Medicine.2021; 10(19): 4386. CrossRef - Normative data on cardiovascular autonomic function in Greenlandic Inuit
Marie Mathilde Bjerg Christensen, Christian Stevns Hansen, Jesper Fleischer, Dorte Vistisen, Stine Byberg, Trine Larsen, Jens Christian Laursen, Marit Eika Jørgensen
BMJ Open Diabetes Research & Care.2021; 9(1): e002121. CrossRef - What Is in the Field for Genetics and Epigenetics of Diabetic Neuropathy: The Role of MicroRNAs
V. Spallone, C. Ciccacci, A. Latini, P. Borgiani, Karim Gariani
Journal of Diabetes Research.2021; 2021: 1. CrossRef - Evaluation and treatment of peripheral nervous system dysfunction in patients with prediabetes
O. E. Zinovyeva, T. M. Ostroumova, M. V. Koniashova, N. A. Gorbachev
Neurology, Neuropsychiatry, Psychosomatics.2021; 13(5): 116. CrossRef - Manifestazioni cliniche della neuropatia autonomica diabetica: valutazione dei sintomi
Carla Greco, Chiara Pacchioni, Manuela Simoni
L'Endocrinologo.2021; 22(6): 514. CrossRef - Perspectives of glycemic variability in diabetic neuropathy: a comprehensive review
Xiaochun Zhang, Xue Yang, Bao Sun, Chunsheng Zhu
Communications Biology.2021;[Epub] CrossRef - The Association Between Cardiovascular Autonomic Function and Changes in Kidney and Myocardial Function in Type 2 Diabetes and Healthy Controls
Jens Christian Laursen, Ida Kirstine B. Rasmussen, Emilie H. Zobel, Philip Hasbak, Bernt Johan von Scholten, Lene Holmvang, Rasmus S. Ripa, Christian S. Hansen, Marie Frimodt-Moeller, Andreas Kjaer, Peter Rossing, Tine W. Hansen
Frontiers in Endocrinology.2021;[Epub] CrossRef - Dependence of heart rate variability on indicators of type 1 diabetes mellitus control.
N. O. Pertseva, O. V. Gurzhiy, K. I. Moshenets
Medicni perspektivi (Medical perspectives).2020; 25(1): 88. CrossRef - Efficacy and safety of evogliptin treatment in patients with type 2 diabetes: A multicentre, active‐controlled, randomized, double‐blind study with open‐label extension (the EVERGREEN study)
Gyuri Kim, Soo Lim, Hyuk‐Sang Kwon, Ie B. Park, Kyu J. Ahn, Cheol‐Young Park, Su K. Kwon, Hye S. Kim, Seok W. Park, Sin G. Kim, Min K. Moon, Eun S. Kim, Choon H. Chung, Kang S. Park, Mikyung Kim, Dong J. Chung, Chang B. Lee, Tae H. Kim, Moon‐Kyu Lee
Diabetes, Obesity and Metabolism.2020; 22(9): 1527. CrossRef - Diabetes mellitus and comorbidities: A bad romance
Niki Katsiki, Dimitrios Tousoulis
Hellenic Journal of Cardiology.2020; 61(1): 23. CrossRef - Features of the glucose influence on the heart activity and the changes in the potentials of the stomach and the intestines at the heart insufficiency conditions
V. V. Soltanov, L. M. Komarovskaya
Doklady of the National Academy of Sciences of Belarus.2020; 63(6): 736. CrossRef - Living Day to Day
Gerald Kayingo, Virginia McCoy Hass
Physician Assistant Clinics.2020; 5(2): 213. CrossRef - Source specific PM2.5 associated with heart rate variability in the elderly with coronary heart disease: A community-based panel study
Xi Chen, Bing Qiu, Qinpei Zou, Tian Qiu, Runkui Li, Ashley Truong, Yanmin Qi, Tao Liu, Limin Han, Tiebing Liu, Junrui Chang, Qi Sun, Ying Zhu, Dongqun Xu
Chemosphere.2020; 260: 127399. CrossRef - The Association of Autonomic Nervous System Function With Ischemic Stroke, and Treatment Strategies
Mengxi Zhao, Ling Guan, Yilong Wang
Frontiers in Neurology.2020;[Epub] CrossRef - Cardiac diabetic autonomic neuropathy
L. T. Akhmedzhanova, T. A. Belyakova, Yu. A. Podkovko, Yu. M. Shor
Medical Council.2020; (21): 94. CrossRef - Diabetes, and its treatment, as an effector of autonomic nervous system circuits and its functions
Liliana Espinoza, Carie R Boychuk
Current Opinion in Pharmacology.2020; 54: 18. CrossRef - Morning blood pressure surge is associated with autonomic neuropathy and peripheral vascular disease in patients with diabetes
Federica Di Gennaro, Cinzia D’Amato, Roberto Morganti, Carla Greco, Susanna Longo, Diana Corradini, Davide Lauro, Vincenza Spallone
Journal of Human Hypertension.2020; 34(7): 495. CrossRef - The Compound Expression of HSP90 and INOS in the Testis of Diabetic Rats as Cellular and Pathologic Adverse Effects of Diabetes
Ali Alsarhan, Kawther Faisal Amawi, Inas Saleh Al-Mazari, Hashem Abu Hurirah, Ahed J. Alkhatib
Analytical Cellular Pathology.2020; 2020: 1. CrossRef - Heart rate variability features from nonlinear cardiac dynamics in identification of diabetes using artificial neural network and support vector machine
Yogender Aggarwal, Joyani Das, Papiya Mitra Mazumder, Rohit Kumar, Rakesh Kumar Sinha
Biocybernetics and Biomedical Engineering.2020; 40(3): 1002. CrossRef - Distal Symmetric and Cardiovascular Autonomic Neuropathies in Brazilian Individuals with Type 2 Diabetes Followed in a Primary Health Care Unit: A Cross-Sectional Study
Mozania Reis de Matos, Daniele Pereira Santos-Bezerra, Cristiane das Graças Dias Cavalcante, Jacira Xavier de Carvalho, Juliana Leite, Jose Antonio Januario Neves, Sharon Nina Admoni, Marisa Passarelli, Maria Candida Parisi, Maria Lucia Correa-Giannella
International Journal of Environmental Research and Public Health.2020; 17(9): 3232. CrossRef - Awareness of hypoglycemia and spectral analysis of heart rate variability in type 1 diabetes
Ticiana Paes, L. Clemente Rolim, Celso Sallum Filho, João Roberto de Sa, Sérgio A. Dib
Journal of Diabetes and its Complications.2020; 34(8): 107617. CrossRef - Is there cardiac autonomic neuropathy in prediabetes?
Lindsay A. Zilliox, James W. Russell
Autonomic Neuroscience.2020; 229: 102722. CrossRef - Chronic Microvascular Complications in Prediabetic States—An Overview
Angelika Baranowska-Jurkun, Wojciech Matuszewski, Elżbieta Bandurska-Stankiewicz
Journal of Clinical Medicine.2020; 9(10): 3289. CrossRef - Cardiac vagal tone as a novel screening tool to recognize asymptomatic cardiovascular autonomic neuropathy: Aspects of utility in type 1 diabetes
Anne-Marie Wegeberg, Elin D Lunde, Sam Riahi, Niels Ejskjaer, Asbjørn M Drewes, Birgitte Brock, Rodica Pop-Busui, Christina Brock
Diabetes Research and Clinical Practice.2020; 170: 108517. CrossRef - Assessment of baroreceptor reflex sensitivity in young obese Saudi males at rest and in response to physiological challenges
Abdullah N. AlShahrani, Lubna I. Al‐Asoom, Ahmed A. Alsunni, Nabil S. Elbahai, Talay Yar
Physiological Reports.2020;[Epub] CrossRef - The relationship between QT interval indices with cardiac autonomic neuropathy in diabetic patients: a case control study
Maryam Vasheghani, Farzaneh Sarvghadi, Mohammad Reza Beyranvand, Habib Emami
Diabetology & Metabolic Syndrome.2020;[Epub] CrossRef - Myocardial ischaemia reperfusion injury and cardioprotection in the presence of sensory neuropathy: Therapeutic options
Péter Bencsik, Kamilla Gömöri, Tamara Szabados, Péter Sántha, Zsuzsanna Helyes, Gábor Jancsó, Péter Ferdinandy, Anikó Görbe
British Journal of Pharmacology.2020; 177(23): 5336. CrossRef - Biological Activity of c-Peptide in Microvascular Complications of Type 1 Diabetes—Time for Translational Studies or Back to the Basics?
Aleksandra Ryk, Aleksandra Łosiewicz, Arkadiusz Michalak, Wojciech Fendler
International Journal of Molecular Sciences.2020; 21(24): 9723. CrossRef - Diabetes and cardiovascular disease: inter-relation of risk factors and treatment
Aman Sharma, Shweta Mittal, Rohan Aggarwal, Meenakshi K. Chauhan
Future Journal of Pharmaceutical Sciences.2020;[Epub] CrossRef - Diabetic Autonomic Neuropathy: A Clinical Update
Jugal Kishor Sharma, Anshu Rohatgi, Dinesh Sharma
Journal of the Royal College of Physicians of Edinburgh.2020; 50(3): 269. CrossRef - Obesity, Metabolic Syndrome and the Risk of Microvascular Complications in Patients with Diabetes mellitus
Niki Katsiki, Panagiotis Anagnostis, Kalliopi Kotsa, Dimitrios G. Goulis, Dimitri P. Mikhailidis
Current Pharmaceutical Design.2019; 25(18): 2051. CrossRef - Cardiac Autonomic Neuropathy in Obesity, the Metabolic Syndrome and Prediabetes: A Narrative Review
Scott M. Williams, Aikaterini Eleftheriadou, Uazman Alam, Daniel J. Cuthbertson, John P. H. Wilding
Diabetes Therapy.2019; 10(6): 1995. CrossRef
- Rectal sensitivity correlated with gastrointestinal‐mediated glucose disposal, but not the incretin effect
- Epidemiology
- The Evidence for an Obesity Paradox in Type 2 Diabetes Mellitus
- Seung Jin Han, Edward J. Boyko
- Diabetes Metab J. 2018;42(3):179-187. Published online May 31, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0055
- 6,346 View
- 122 Download
- 61 Web of Science
- 61 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Although overweight/obesity is a major risk factor for the development of type 2 diabetes mellitus, there is increasing evidence that overweight or obese patients with type 2 diabetes mellitus experience lower mortality compared with patients of normal weight. This paradoxical finding, known as the “obesity paradox,” occurs in other chronic diseases, and in type 2 diabetes mellitus is particularly perplexing given that lifestyle intervention with one goal being weight reduction is an important feature of the management of this condition. We summarize in this review the findings from clinical and epidemiologic studies that have investigated the association between overweight and obesity (usually assessed using body mass index [BMI]) and mortality in type 2 diabetes mellitus and discuss potential causes of the obesity paradox. We conclude that most studies show evidence of an obesity paradox, but important conflicting findings still exist. We also evaluate if potential bias might explain the obesity paradox in diabetes, including, for example, the presence of confounding factors, measurement error due to use of BMI as an index of obesity, and reverse causation.
-
Citations
Citations to this article as recorded by- Association between the weight-adjusted waist index and the odds of type 2 diabetes mellitus in United States adults: a cross-sectional study
Dongdong Zheng, Suzhen Zhao, Dan Luo, Feng Lu, Zhishen Ruan, Xiaokang Dong, Wenjing Chen
Frontiers in Endocrinology.2024;[Epub] CrossRef - Racial and Ethnic Disparities in Primary Prevention of Cardiovascular Disease
Mohammad R. Ali, Hadjer Nacer, Claire A. Lawson, Kamlesh Khunti
Canadian Journal of Cardiology.2024;[Epub] CrossRef - Independent and interactive associations of heart rate and obesity with type 2 diabetes mellites: A population‐based study
Tianxin Zhu, Qingyu Chen, Hongxing Chen, Lili You, Dan Liu, Xiaoyun Zhang, Feng Li, Hongshi Wu, Juying Tang, Diaozhu Lin, Kan Sun, Li Yan, Meng Ren
Journal of Diabetes.2024;[Epub] CrossRef - Two‐sided roles of adipose tissue: Rethinking the obesity paradox in various human diseases from a new perspective
Jing Pan, Jianqiong Yin, Lu Gan, Jianxin Xue
Obesity Reviews.2023;[Epub] CrossRef - Lean or diabetic subtypes predict increased all-cause and disease-specific mortality in metabolic-associated fatty liver disease
Goh Eun Chung, Su Jong Yu, Jeong-Ju Yoo, Yuri Cho, Kyu-na Lee, Dong Wook Shin, Donghee Kim, Yoon Jun Kim, Jung-Hwan Yoon, Kyungdo Han, Eun Ju Cho
BMC Medicine.2023;[Epub] CrossRef - Dynamic changes in prevalence of type 2 diabetes along with associated factors in Bangladesh: Evidence from two national cross-sectional surveys (BDHS 2011 and BDHS 2017–18)
Sabiha Shirin Sara, Ashis Talukder, Ka Yiu Lee, Nayan Basak, Shaharior Rahman Razu, Iqramul Haq, Chuton Deb Nath
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(2): 102706. CrossRef - Association of dietary intake with body mass index and glycemic profile among newly diagnosed patients with type 2 diabetes mellitus
Keddagoda Gamage Piyumi Wasana, Anoja Priyadarshani Attanayake, Thilak Priyantha Weerarathna, Devpura Arachchige Bandumalee Nimalshanthi Amarasekera, Kamani Ayoma Perera Wijewardana Jayatilaka
American Journal of Human Biology.2023;[Epub] CrossRef - Can lipophilic pollutants in adipose tissue explain weight change‐related risk in type 2 diabetes mellitus?
Duk‐Hee Lee, In‐Kyu Lee
Journal of Diabetes Investigation.2023; 14(4): 528. CrossRef - Visceral fat and attribute-based medicine in chronic kidney disease
Hiroshi Kataoka, Kosaku Nitta, Junichi Hoshino
Frontiers in Endocrinology.2023;[Epub] CrossRef - A primary care delivered, technology supported lifestyle program for Type 2 Diabetes Management: An evaluation of changes in metabolic health, feasibility, and acceptability – A pilot interventional study protocol
Pennie J. Taylor, Campbell H. Thompson, Thomas P. Wycherley, Grant D. Brinkworth
Contemporary Clinical Trials Communications.2023; 33: 101152. CrossRef - The medical model of “obesity” and the values behind the guise of health
Kayla R. Mehl
Synthese.2023;[Epub] CrossRef - Elevated MMP-8 levels, inversely associated with BMI, predict mortality in mechanically ventilated patients: an observational multicenter study
Hang Ruan, Shu-sheng Li, Qin Zhang, Xiao Ran
Critical Care.2023;[Epub] CrossRef - Obesity and 30-day case fatality after hyperglycemic crisis hospitalizations in Korea: a national cohort study
Hojun Yoon, Hyun Ho Choi, Giwoong Choi, Sun Ok Song, Kyoung Hwa Ha, Dae Jung Kim
Cardiovascular Prevention and Pharmacotherapy.2023; 5(3): 74. CrossRef - Normal‐weight central obesity and risk of cardiovascular and microvascular events in adults with prediabetes or diabetes: Chinese and British cohorts
Pingting Zhong, Shaoying Tan, Zhuoting Zhu, Ziyu Zhu, Yi Liang, Wenyong Huang, Wei Wang
Diabetes/Metabolism Research and Reviews.2023;[Epub] CrossRef - Overweight and obesity are associated with better survival in STEMI patients with diabetes
Hamza Chaudhry, Ramez Bodair, Ziyad Mahfoud, Soha Dargham, Jassim Al Suwaidi, Hani Jneid, Charbel Abi Khalil
Obesity.2023; 31(11): 2834. CrossRef - Influence of diabetes and obesity on ten-year outcomes after coronary artery bypass grafting in the arterial revascularisation trial
Maria Stefil, Mario Gaudino, Umberto Benedetto, Stephen Gerry, Alastair Gray, Belinda Lees, Bruno Podesser, Lukasz Krzych, Lokeswara Rao Sajja, David Taggart, Marcus Flather
Clinical Research in Cardiology.2023;[Epub] CrossRef - Poor glycaemic control: prevalence, factors and implications for the care of patients with type 2 diabetes in Kinshasa, Democratic Republic of the Congo: a cross-sectional study
Jean-Pierre Fina Lubaki, Olufemi Babatunde Omole, Joel Msafiri Francis
Frontiers in Clinical Diabetes and Healthcare.2023;[Epub] CrossRef - Comparison of obesity indices and triglyceride glucose-related parameters to predict type 2 diabetes mellitus among normal-weight elderly in China
Pan Ke, Xia Wu, Minzhi Xu, Jie Feng, Hongbin Xu, Yong Gan, Chao Wang, Zhenyu Deng, Xiang Liu, Wenning Fu, Qingfeng Tian, Yan He, Lirong Zhong, Heng Jiang, Zuxun Lu
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity.2022; 27(3): 1181. CrossRef - Association Between Obesity and Cardiovascular Disease in Elderly Patients With Diabetes: A Retrospective Cohort Study
Sangmo Hong, Jung Hwan Park, Kyungdo Han, Chang Beom Lee, Dong Sun Kim, Sung Hoon Yu
The Journal of Clinical Endocrinology & Metabolism.2022; 107(2): e515. CrossRef - The Relationship between the Lipid Accumulation Product and Beta-cell Function in Korean Adults with or without Type 2 Diabetes Mellitus: The 2015 Korea National Health and Nutrition Examination Survey
Hye Eun Cho, Seung Bum Yang, Mi Young Gi, Ju Ae Cha, so Young Park, Hyun Yoon
Endocrine Research.2022; 47(2): 80. CrossRef - Body mass index and all-cause mortality in patients with newly diagnosed type 2 diabetes mellitus in South Korea: a retrospective cohort study
Jae-Seok Hong, Hee-Chung Kang
BMJ Open.2022; 12(4): e048784. CrossRef - Social determinants of obesity in American Indian and Alaska Native peoples aged ≥ 50 years
R Turner Goins, Cheryl Conway, Margaret Reid, Luohua Jiang, Jenny Chang, Kimberly R Huyser, Angela G Brega, John F Steiner, Amber L Fyfe-Johnson, Michelle Johnson-Jennings, Vanessa Hiratsuka, Spero M Manson, Joan O’Connell
Public Health Nutrition.2022; 25(8): 2064. CrossRef - Cardiorespiratory Fitness, BMI, Mortality, and Cardiovascular Disease in Adults with Overweight/Obesity and Type 2 Diabetes
ANDREW C. WILLS, ELSA VAZQUEZ ARREOLA, MUIDEEN T. OLAIYA, JEFFREY M. CURTIS, MARGARETA I. HELLGREN, ROBERT L. HANSON, WILLIAM C. KNOWLER
Medicine & Science in Sports & Exercise.2022; 54(6): 994. CrossRef - Spline Longitudinal Multi-response Model for the Detection of Lifestyle-
Based Changes in Blood Glucose of Diabetic Patients
Anna Islamiyati
Current Diabetes Reviews.2022;[Epub] CrossRef - The obesity paradox: Retinopathy, obesity, and circulating risk markers in youth with type 2 diabetes in the TODAY Study
Lynne L. Levitsky, Kimberly L. Drews, Morey Haymond, Rose A. Glubitosi-Klug, Lorraine E. Levitt Katz, Mihai Mititelu, William Tamborlane, Jeanie B. Tryggestad, Ruth S. Weinstock
Journal of Diabetes and its Complications.2022; 36(11): 108259. CrossRef - Distribution of lean mass and mortality risk in patients with type 2 diabetes
Li Ding, Yuxin Fan, Jingting Qiao, Jing He, Ruodan Wang, Qing He, Jingqiu Cui, Zhongshu Ma, Fangqiu Zheng, Hua Gao, Chenlin Dai, Hongyan Wei, Jun Li, Yuming Cao, Gang Hu, Ming Liu
Primary Care Diabetes.2022; 16(6): 824. CrossRef - Current Knowledge on the Pathophysiology of Lean/Normal-Weight Type 2 Diabetes
Teresa Salvatore, Raffaele Galiero, Alfredo Caturano, Luca Rinaldi, Livio Criscuolo, Anna Di Martino, Gaetana Albanese, Erica Vetrano, Christian Catalini, Celestino Sardu, Giovanni Docimo, Raffaele Marfella, Ferdinando Carlo Sasso
International Journal of Molecular Sciences.2022; 24(1): 658. CrossRef - The obesity paradox and diabetes
Giovanni Gravina, Federica Ferrari, Grazia Nebbiai
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity.2021; 26(4): 1057. CrossRef - Implicating the effect of ketogenic diet as a preventive measure to obesity and diabetes mellitus
Sachin Kumar, Tapan Behl, Monika Sachdeva, Aayush Sehgal, Shilpa Kumari, Arun Kumar, Gagandeep Kaur, Harlokesh Narayan Yadav, Simona Bungau
Life Sciences.2021; 264: 118661. CrossRef - Diagnosis of obesity based on body composition‐associated health risks—Time for a change in paradigm
Anja Bosy‐Westphal, Manfred J. Müller
Obesity Reviews.2021;[Epub] CrossRef - Body mass index and clinical outcomes in patients with intracerebral haemorrhage: results from the China Stroke Center Alliance
Zhentang Cao, Xinmin Liu, Zixiao Li, Hongqiu Gu, Yingyu Jiang, Xingquan Zhao, Yongjun Wang
Stroke and Vascular Neurology.2021; 6(3): 424. CrossRef - Obesity and Overweight Are Associated with Minimal Extrathyroidal Extension, Multifocality and Bilaterality of Papillary Thyroid Cancer
Krzysztof Kaliszewski, Dorota Diakowska, Marta Rzeszutko, Jerzy Rudnicki
Journal of Clinical Medicine.2021; 10(5): 970. CrossRef - Obesity paradox in patients with cardiovascular diseases and diabetes mellitus type 2 (analytical review)
Margarita P. Zaikina, Valentina A. Kapustina, Stanislav I. Savel'ev
HEALTH CARE OF THE RUSSIAN FEDERATION.2021; 65(2): 135. CrossRef - Risk factors for adverse outcomes among 35 879 veterans with and without diabetes after diagnosis with COVID-19
Pandora L Wander, Elliott Lowy, Lauren A Beste, Luis Tulloch-Palomino, Anna Korpak, Alexander C Peterson, Bessie A Young, Edward J Boyko
BMJ Open Diabetes Research & Care.2021; 9(1): e002252. CrossRef - Obesity and glycemic control among people with type 2 diabetes in the United States: A retrospective cohort study using insurance claims data
Kristina S. Boye, Maureen J. Lage, Vivian Thieu, Shraddha Shinde, Shivanie Dhamija, Jay Patrick Bae
Journal of Diabetes and its Complications.2021; 35(9): 107975. CrossRef - Differential effects of body mass index on domain-specific cognitive outcomes after stroke
Minwoo Lee, Mi Sun Oh, San Jung, Ju-Hun Lee, Chul-Ho Kim, Min Uk Jang, Young Eun Kim, Hee-Joon Bae, Jaeseol Park, Yeonwook Kang, Byung-Chul Lee, Jae-Sung Lim, Kyung-Ho Yu
Scientific Reports.2021;[Epub] CrossRef - Associations between traditional and non-traditional anthropometric indices and cardiometabolic risk factors among inpatients with type 2 diabetes mellitus: a cross-sectional study
Sahar Golabi, Sajad Ajloo, Fatemeh Maghsoudi, Maryam Adelipour, Mahshid Naghashpour
Journal of International Medical Research.2021; 49(10): 030006052110499. CrossRef - Impact of preexisting type 2 diabetes mellitus and antidiabetic drugs on all-cause and cause-specific mortality among Medicaid-insured women diagnosed with breast cancer
Wayne R. Lawrence, Akiko S. Hosler, Margaret Gates Kuliszewski, Matthew C. Leinung, Xiuling Zhang, Maria J. Schymura, Francis P. Boscoe
Cancer Epidemiology.2020; 66: 101710. CrossRef - Serum Adiponectin and Progranulin Level in Patients with Benign Thyroid Nodule or Papillary Thyroid Cancer
Hyemi Kwon, Se Eun Park, Ji-Sup Yun, Cheol-Young Park
Endocrinology and Metabolism.2020; 35(2): 396. CrossRef - Obesity, sleep apnea, and cancer
Isaac Almendros, Miguel A. Martinez-Garcia, Ramon Farré, David Gozal
International Journal of Obesity.2020; 44(8): 1653. CrossRef - Association of Body Mass Index With Clinical Outcomes in Patients With Atrial Fibrillation: A Report From the FANTASIIA Registry
Vicente Bertomeu‐Gonzalez, José Moreno‐Arribas, María Asunción Esteve‐Pastor, Inmaculada Roldán‐Rabadán, Javier Muñiz, Paula Raña‐Míguez, Martín Ruiz‐Ortiz, Ángel Cequier, Vicente Bertomeu‐Martínez, Lina Badimón, Manuel Anguita, Gregory Y. H. Lip, Francis
Journal of the American Heart Association.2020;[Epub] CrossRef - Risk of type 2 diabetes according to the cumulative exposure to metabolic syndrome or obesity: A nationwide population‐based study
You‐Bin Lee, Da Hye Kim, Seon Mee Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Yong Gyu Park, Kyungdo Han, Hye Jin Yoo
Journal of Diabetes Investigation.2020; 11(6): 1583. CrossRef - Gut microbiota of obese and diabetic Thai subjects and interplay with dietary habits and blood profiles
Lucsame Gruneck, Niwed Kullawong, Kongkiat Kespechara, Siam Popluechai
PeerJ.2020; 8: e9622. CrossRef Multistate Models to Predict Development of Late Complications of Type 2 Diabetes in an Open Cohort Study
Roqayeh Aliyari, Ebrahim Hajizadeh, Ashraf Aminorroaya, Farshad Sharifi, Iraj Kazemi, Ahmad-Reza Baghestani
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 1863. CrossRef- Early weaning induces short‐ and long‐term effects on pancreatic islets in Wistar rats of both sexes
Carla Bruna Pietrobon, Rosiane Aparecida Miranda, Iala Milene Bertasso, Paulo Cezar de Freitas Mathias, Maria Lúcia Bonfleur, Sandra Lucinei Balbo, Marise Auxiliadora de Barros Reis, Márcia Queiroz Latorraca, Vanessa Cristina Arantes, Elaine de Oliveira,
The Journal of Physiology.2020; 598(3): 489. CrossRef - A negative impact of recent weight loss on in-hospital mortality is not modified by overweight and obesity
Rocco Barazzoni, Isabella Sulz, Karin Schindler, Stephan C. Bischoff, Gianluca Gortan Cappellari, Michael Hiesmayr
Clinical Nutrition.2020; 39(8): 2510. CrossRef - Body mass index and mortality among middle-aged Japanese individuals with diagnosed diabetes: The Japan Public Health Center-based prospective study (JPHC study)
Chiho Yamazaki, Atsushi Goto, Motoki Iwasaki, Norie Sawada, Shino Oba, Mitsuhiko Noda, Hiroyasu Iso, Hiroshi Koyama, Shoichiro Tsugane
Diabetes Research and Clinical Practice.2020; 164: 108198. CrossRef Is the Obesity Paradox in Type 2 Diabetes Due to Artefacts of Biases? An Analysis of Pooled Cohort Data from the Heinz Nixdorf Recall Study and the Study of Health in Pomerania
Bernd Kowall, Andreas Stang, Raimund Erbel, Susanne Moebus, Astrid Petersmann, Antje Steveling, Karl-Heinz Jöckel, Henry Völzke
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 1989. CrossRef- Associations between BMI, waist circumference, central obesity and outcomes in type II diabetes mellitus: The ACCORD Trial
Charles A. German, Brian Laughey, Alain G. Bertoni, Joseph Yeboah
Journal of Diabetes and its Complications.2020; 34(3): 107499. CrossRef - Trends in mechanical ventilation use and mortality over time in patients receiving mechanical ventilation in Spain from 2001 to 2015.
Javier de-Miguel-Díez, Rodrigo Jiménez-García, Valentín Hernández-Barrera, Jose J Zamorano-Leon, Rosa Villanueva-Orbaiz, Romana Albaladejo-Vicente, Ana López-de-Andrés
European Journal of Internal Medicine.2020; 74: 67. CrossRef - Type 2 diabetes mellitus: pathogenesis and genetic diagnosis
D. Himanshu, Wahid Ali, Mohd Wamique
Journal of Diabetes & Metabolic Disorders.2020; 19(2): 1959. CrossRef - Prevalence and factors associated with overweight and obesity among patients with type 2 diabetes mellitus in Uganda—a descriptive retrospective study
Salome Tino, Billy N Mayanja, Michael Charles Mubiru, Emmanuel Eling, Edward Ddumba, Pontiano Kaleebu, Moffat Nyirenda
BMJ Open.2020; 10(11): e039258. CrossRef - Nutrition Therapy in Critically Ill Overweight Elderly Patient with Heart Failure, Myocardial Infarction, Pneumonia, and Chronic Kidney Disease
Christina RUSLI, Agussalim BUKHARI, Nurpudji A. TASLIM, Suryani AS’AD, Haerani RASYID
Journal of Nutritional Science and Vitaminology.2020; 66(Supplement): S25. CrossRef - Obesity and childhood asthma
Jason E. Lang
Current Opinion in Pulmonary Medicine.2019; 25(1): 34. CrossRef - Why primary obesity is a disease?
Antonino De Lorenzo, Santo Gratteri, Paola Gualtieri, Andrea Cammarano, Pierfrancesco Bertucci, Laura Di Renzo
Journal of Translational Medicine.2019;[Epub] CrossRef - Impaired compensatory hyperinsulinemia among nonobese type 2 diabetes patients: a cross-sectional study
Jit Sarkar, Sujay Krishna Maity, Abhishek Sen, Titli Nargis, Dipika Ray, Partha Chakrabarti
Therapeutic Advances in Endocrinology and Metabolism.2019; 10: 204201881988902. CrossRef - Sedentary behaviour is associated with diabetes mellitus in adults: findings of a cross-sectional analysis from the Brazilian National Health System
Ítalo Ribeiro Lemes, Xuemei Sui, Bruna Camilo Turi-Lynch, Duck-chul Lee, Steven N Blair, Rômulo Araújo Fernandes, Jamile Sanches Codogno, Henrique Luiz Monteiro
Journal of Public Health.2019; 41(4): 742. CrossRef - Obesity Paradox in Chronic Liver Diseases: Product of Bias or a Real Thing?
Ines Bilic Curcic, Maja Cigrovski Berkovic, Lucija Kuna, Hrvoje Roguljic, Robert Smolic, Silvija Canecki Varzic, Lucija Virovic Jukic, Martina Smolic
Journal of Clinical and Translational Hepatology.2019; 7(3): 1. CrossRef - From the Obesity Tsunami to the Diabetes Avalanche: Primordial Prevention of the Diabesity-Related Cardiovascular Epidemic by Diabeto-Cardiologists
Mustafa Karakurt, Burak Acar, Ozcan Ozeke, Mustafa Bilal Ozbay, Yasin Ozen, Sefa Unal, Mustafa Karanfil, Cagri Yayla, Serkan Cay, Orhan Maden, Dursun Aras, Serkan Topaloglu, Sinan Aydogdu, Zehra Golbasi
Angiology.2019; 70(4): 371. CrossRef - Increased Plasma Dipeptidyl Peptidase-4 (DPP4) Activity Is an Obesity-Independent Parameter for Glycemic Deregulation in Type 2 Diabetes Patients
Jit Sarkar, Titli Nargis, Om Tantia, Sujoy Ghosh, Partha Chakrabarti
Frontiers in Endocrinology.2019;[Epub] CrossRef - INVESTIGATING INDIVIDUAL FACTORS RELATED TO READMISSION OF PATIENTS WITH TYPE 2 DIABETES- A CROSS-SECTIONAL STUDY
Valiallah Dashtpour, Mehran Hesaraki, Mahnaz Abavisani, Mahdieh Sari, Sudabeh Ahmadidarrehsima
Journal of Evolution of Medical and Dental Sciences.2018; 7(53): 5604. CrossRef
- Association between the weight-adjusted waist index and the odds of type 2 diabetes mellitus in United States adults: a cross-sectional study

 KDA
KDA
 First
First Prev
Prev





