
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Lifestyle
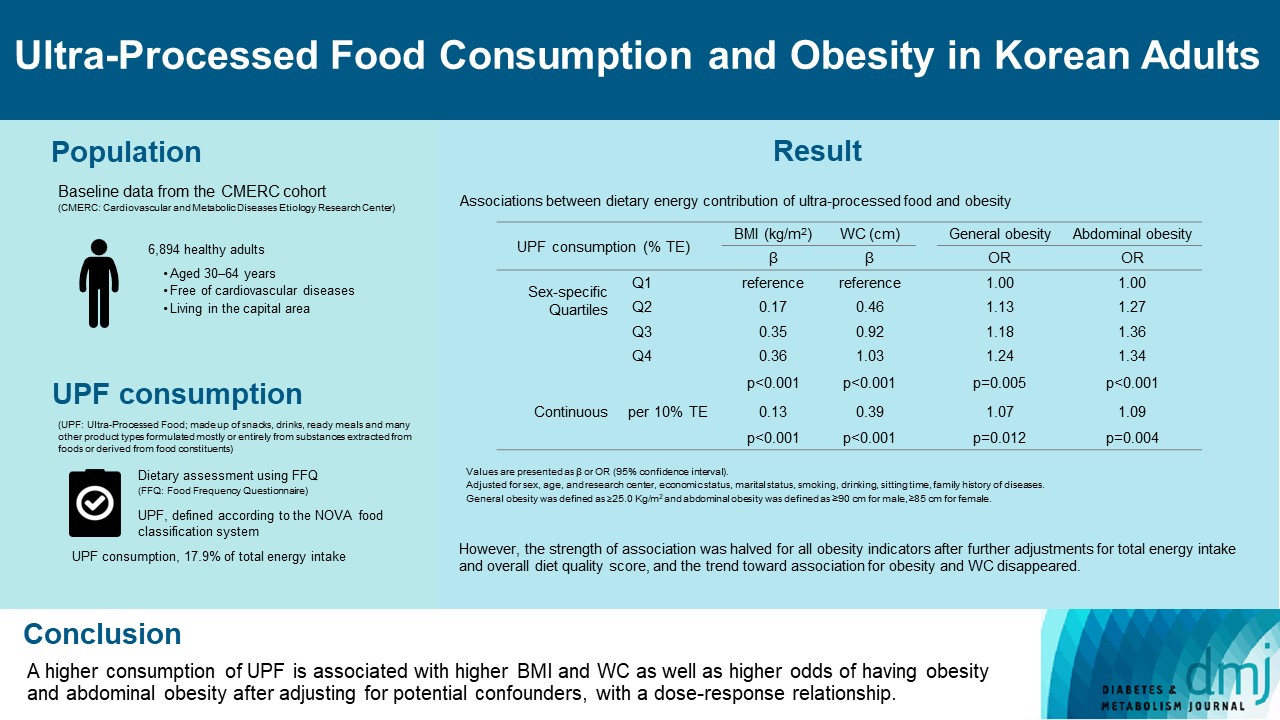
- Ultra-Processed Food Consumption and Obesity in Korean Adults
- Jee-Seon Shim, Kyoung Hwa Ha, Dae Jung Kim, Hyeon Chang Kim
- Diabetes Metab J. 2023;47(4):547-558. Published online April 26, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0026
- 2,854 View
- 139 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
This study aimed to investigate the association between consumption of ultra-processed foods (UPF) and obesity in Korean adults.
Methods
We included the Cardiovascular and Metabolic Diseases Etiology Research Center cohort study baseline data of adults aged 30 to 64 years who completed a validated food frequency questionnaire. UPF was defined using the NOVA food classification. Multivariable linear and logistic regression analyses were performed to assess the association of dietary energy contribution of UPF with obesity indicators (body mass index [BMI], obesity, waist circumference [WC], and abdominal obesity).
Results
Consumption of UPF accounted for 17.9% of total energy intake and obesity and abdominal obesity prevalence was 35.4% and 30.2%, respectively. Compared with those in the lowest quartile of UPF consumption, adults in the highest quartile had greater BMI (β=0.36; 95% confidence interval [CI], 0.15 to 0.56), WC (β=1.03; 95% CI, 0.46 to 1.60), higher odds of having obesity (odds ratio [OR], 1.24; 95% CI, 1.07 to 1.45), and abdominal obesity (OR, 1.34; 95% CI, 1.14 to 1.57), after adjusting for sociodemographic characteristics, health-related behaviors, and family history of diseases. Dose-response associations between UPF consumption and obesity indicators were consistently found (all P trend <0.01). However, the strength of association was halved for all obesity indicators after further adjustments for total energy intake and overall diet quality score, and the trend toward association for obesity and WC disappeared.
Conclusion
Our finding supports the evidence that consumption of UPF is positively associated with obesity among Korean adults. -
Citations
Citations to this article as recorded by- Ultra-processed food consumption and increased risk of metabolic syndrome in Korean adults: A cross-sectional analysis of the KNHANES 2016–2020
Hansol Park, Youngmi Lee, Jinah Hwang, Yujin Lee
Nutrition.2024; 122: 112374. CrossRef - Diet quality partially mediates the association between ultraprocessed food consumption and adiposity indicators
Jee‐Seon Shim, Kyoung Hwa Ha, Dae Jung Kim, Hyeon Chang Kim
Obesity.2023; 31(9): 2430. CrossRef - Development of a Semi-Quantitative Food-Frequency Questionnaire for Korean Adults with Obesity
Jina Chung, Seoeun Ahn, Hyojee Joung, Sangah Shin
Nutrients.2023; 15(22): 4848. CrossRef
- Ultra-processed food consumption and increased risk of metabolic syndrome in Korean adults: A cross-sectional analysis of the KNHANES 2016–2020
- Complications
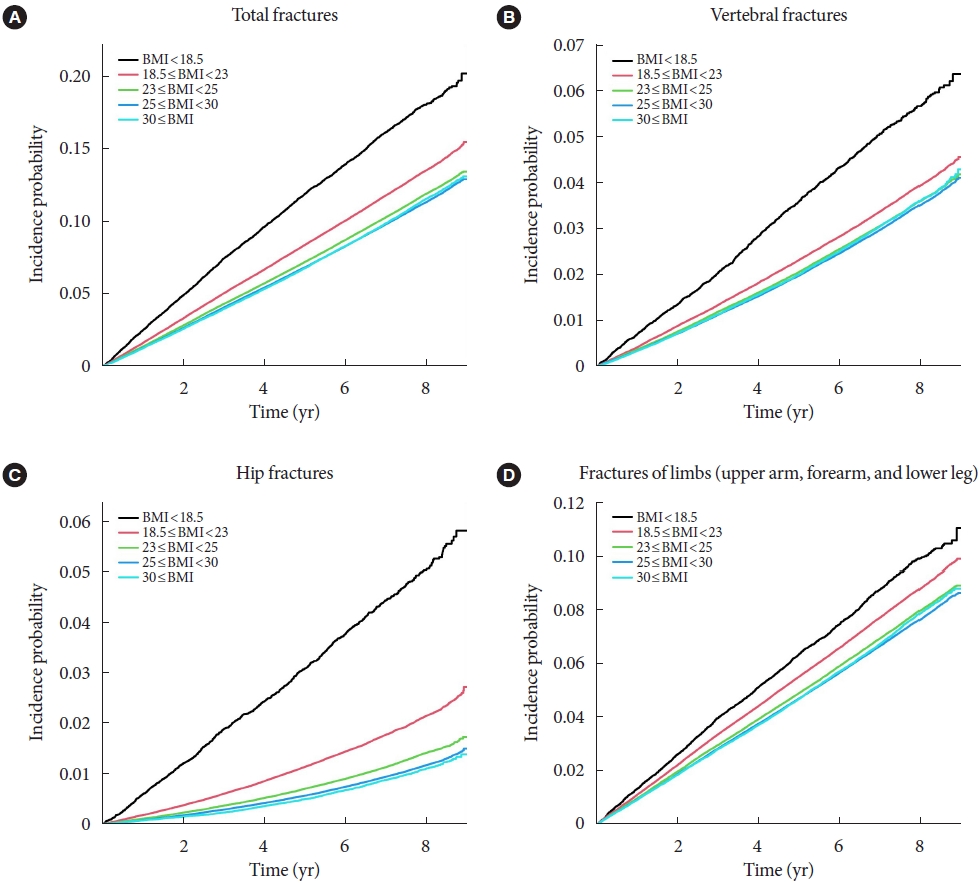
- Association of Body Mass Index and Fracture Risk Varied by Affected Bones in Patients with Diabetes: A Nationwide Cohort Study
- Se-Won Lee, Kyungdo Han, Hyuk-Sang Kwon
- Diabetes Metab J. 2023;47(2):242-254. Published online January 19, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0001
- 2,899 View
- 164 Download
- 5 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Body mass index (BMI) is a risk factor for the type 2 diabetes (T2DM), and T2DM accompanies various complications, such as fractures. We investigated the effects of BMI and T2DM on fracture risk and analyzed whether the association varied with fracture locations.
Methods
This study is a nationwide population-based cohort study that included all people with T2DM (n=2,746,078) who received the National Screening Program during 2009–2012. According to the anatomical location of the fracture, the incidence rate and hazard ratio (HR) were analyzed by dividing it into four categories: vertebra, hip, limbs, and total fracture.
Results
The total fracture had higher HR in the underweight group (HR, 1.268; 95% CI, 1.228 to 1.309) and lower HR in the obese group (HR, 0.891; 95% CI, 0.882 to 0.901) and the morbidly obese group (HR, 0.873; 95% CI, 0.857 to 0.89), compared to reference (normal BMI group). Similar trends were observed for HR of vertebra fracture. The risk of hip fracture was most prominent, the risk of hip fracture increased in the underweight group (HR, 1.896; 95% CI, 1.178 to 2.021) and decreased in the obesity (HR, 0.643; 95% CI, 0.624 to 0.663) and morbidly obesity group (HR, 0.627; 95% CI, 0.591 to 0.665). Lastly, fracture risk was least affected by BMI for limbs.
Conclusion
In T2DM patients, underweight tends to increase fracture risk, and overweight tends to lower fracture risk, but association between BMI and fracture risk varied depending on the affected bone lesions. -
Citations
Citations to this article as recorded by- Dysuricemia—A New Concept Encompassing Hyperuricemia and Hypouricemia
Naoyuki Otani, Motoshi Ouchi, Einosuke Mizuta, Asuka Morita, Tomoe Fujita, Naohiko Anzai, Ichiro Hisatome
Biomedicines.2023; 11(5): 1255. CrossRef - Association of Body Mass Index and Fracture Risk Varied by Affected Bones in Patients with Diabetes: A Nationwide Cohort Study (Diabetes Metab J 2023;47:242-54)
Se-Won Lee, Kyungdo Han, Hyuk-Sang Kwon
Diabetes & Metabolism Journal.2023; 47(3): 439. CrossRef - Association of Body Mass Index and Fracture Risk Varied by Affected Bones in Patients with Diabetes: A Nationwide Cohort Study (Diabetes Metab J 2023;47:242-54)
So Young Park
Diabetes & Metabolism Journal.2023; 47(3): 437. CrossRef - Effect of SGLT2 inhibitors on fractures, BMD, and bone metabolism markers in patients with type 2 diabetes mellitus: a systematic review and meta-analysis
Xin Wang, Fengyi Zhang, Yufeng Zhang, Jiayi Zhang, Yingli Sheng, Wenbo Wang, Yujie Li
Osteoporosis International.2023; 34(12): 2013. CrossRef
- Dysuricemia—A New Concept Encompassing Hyperuricemia and Hypouricemia
- Complication
- Waist Circumference and Body Mass Index Variability and Incident Diabetic Microvascular Complications: A Post Hoc Analysis of ACCORD Trial
- Daniel Nyarko Hukportie, Fu-Rong Li, Rui Zhou, Jia-Zhen Zheng, Xiao-Xiang Wu, Xian-Bo Wu
- Diabetes Metab J. 2022;46(5):767-780. Published online May 10, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0258
- 3,772 View
- 220 Download
- 7 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Obesity is associated with adverse health events among diabetic patients, however, the relationship between obesity fluctuation and risk of microvascular complications among this specific population is unclear. We aimed to examine the effect of waist circumference (WC) and body mass index (BMI) variability on the risk of diabetic microvascular outcome
Methods
Annually recorded anthropometric data in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study was used to examine the association of WC and BMI variability defined as variability independent of mean, with the risk of microvascular outcomes, including neuropathy, nephropathy, and retinopathy. Cox proportional hazards models were used to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) (Trial registration: ClinicalTrials.gov., no. NCT00000620).
Results
There were 4,031, 5,369, and 2,601 cases of neuropathy, nephropathy, and retinopathy during a follow-up period of 22,524, 23,941, and 23,850 person-years, respectively. Higher levels of WC and BMI variability were associated with an increased risk of neuropathy. Compared with the lowest quartile, the fully-adjusted HR (95% CI) for the highest quartile of WC and BMI variability for neuropathy risk were 1.21 (1.05 to 1.40) and 1.16 (1.00 to 1.33), respectively. Also, higher quartiles of BMI variability but not WC variability were associated with increased risk of nephropathic events. The fully-adjusted HR (95% CI) for the highest quartile compared with the lowest quartile of BMI variability was 1.31 (1.18 to 1.46). However, the results for retinopathic events were all insignificant.
Conclusion
Among participants with type 2 diabetes mellitus, WC and BMI variability were associated with a higher risk of neuropathic events, whereas BMI variability was associated with an increased risk of nephropathic events. -
Citations
Citations to this article as recorded by- Association of body mass index and blood pressure variability with 10-year mortality and renal disease progression in type 2 diabetes
Stephen Fava, Sascha Reiff
Acta Diabetologica.2024;[Epub] CrossRef - Waist Circumference and Body Mass Index Variability and Incident Diabetic Microvascular Complications: A Post Hoc Analysis of ACCORD Trial (Diabetes Metab J 2022;46:767-80)
Yun Kyung Cho
Diabetes & Metabolism Journal.2023; 47(1): 147. CrossRef - Waist Circumference and Body Mass Index Variability and Incident Diabetic Microvascular Complications: A Post Hoc Analysis of ACCORD Trial (Diabetes Metab J 2022;46:767-80)
Daniel Nyarko Hukportie, Fu-Rong Li, Rui Zhou, Jia-Zhen Zheng, Xiao-Xiang Wu, Xian-Bo Wu
Diabetes & Metabolism Journal.2023; 47(1): 150. CrossRef - Weight variability and diabetes complications
Francesco Prattichizzo, Chiara Frigé, Rosalba La Grotta, Antonio Ceriello
Diabetes Research and Clinical Practice.2023; 199: 110646. CrossRef - Risk Factors for Diabetic Retinopathy in Latin America (Mexico) and the World: A Systematic Review and Meta-Analysis
Oscar Vivanco-Rojas, Sonia López-Letayf, Valentina Londoño-Angarita, Fátima Sofía Magaña-Guerrero, Beatriz Buentello-Volante, Yonathan Garfias
Journal of Clinical Medicine.2023; 12(20): 6583. CrossRef - Effects of body weight variability on risks of macro- and microvascular outcomes in individuals with type 2 diabetes: The Rio de Janeiro type 2 diabetes cohort
Claudia R.L. Cardoso, Nathalie C. Leite, Gil F. Salles
Diabetes Research and Clinical Practice.2023; 205: 110992. CrossRef - Correlation Between the Variability of Different Obesity Indices and Diabetic Kidney Disease: A Retrospective Cohort Study Based on Populations in Taiwan
Zhenzhen Sun, Kun Wang, Chuan Yun, Fang Bai, Xiaodan Yuan, Yaujiunn Lee, Qingqing Lou
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 2791. CrossRef - Unraveling shared risk factors for diabetic foot ulcer: a comprehensive Mendelian randomization analysis
Kangli Yin, Tianci Qiao, Yongkang Zhang, Jiarui Liu, Yuzhen Wang, Fei Qi, Junlin Deng, Cheng Zhao, Yongcheng Xu, Yemin Cao
BMJ Open Diabetes Research & Care.2023; 11(6): e003523. CrossRef
- Association of body mass index and blood pressure variability with 10-year mortality and renal disease progression in type 2 diabetes
- Metabolic Risk/Epidemiology
- Impact of Older Age Adiposity on Incident Diabetes: A Community-Based Cohort Study in China
- Anthony Chen, Weiju Zhou, Jian Hou, Alan Nevill, Yuanlin Ding, Yuhui Wan, Rebecca Jester, Xia Qin, Zhi Hu, Ruoling Chen
- Diabetes Metab J. 2022;46(5):733-746. Published online April 29, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0215
- 4,001 View
- 197 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Obesity classifications vary globally and the impact of older age adiposity on incident diabetes has not been well-studied.
Methods
We examined a random sample of 2,809 participants aged ≥60 years in China, who were free of diabetes at baseline and were followed up for up to 10 years to document diabetes (n=178). The incidence of diabetes was assessed in relation to different cut-off points of body mass index (BMI) and waist circumference (WC) in multiple adjusted Cox regression models.
Results
The diabetic risk in the cohort increased linearly with the continuous and quartile variables of BMI and WC. The BMI-World Health Organization (WHO) and BMI-China criteria analysis did not show such a linear relationship, however, the BMI-Asian/Hong Kong criteria did; adjusted hazards ratio (HR) was 0.42 (95% confidence interval [CI], 0.20 to 0.90) in BMI <20 kg/m2, 1.46 (95% CI, 0.99 to 2.14) in 23–≤26 kg/m2, and 1.63 (95% CI, 1.09 to 2.45) in ≥26 kg/m2. The WC-China criteria revealed a slightly better prediction of diabetes (adjusted HRs were 1.79 [95% CI, 1.21 to 2.66] and 1.87 [95% CI, 1.22 to 2.88] in central obese action levels 1 and 2) than the WC-WHO. The combination of the BMI-Asian/Hong Kong with WC-China demonstrated the strongest prediction. There were no gender differences in the impact of adiposity on diabetes.
Conclusion
In older Chinese, BMI-Asian/Hong Kong criteria is a better predictor of diabetes than other BMI criterion. Its combination with WC-China improved the prediction of adiposity to diabetes, which would help manage bodyweight in older age to reduce the risk of diabetes. -
Citations
Citations to this article as recorded by- Association of air pollution with dementia: a systematic review with meta-analysis including new cohort data from China
Jie Tang, Anthony Chen, Fan He, Martin Shipley, Alan Nevill, Hugh Coe, Zhi Hu, Tao Zhang, Haidong Kan, Eric Brunner, Xuguang Tao, Ruoling Chen
Environmental Research.2023; 223: 115048. CrossRef - Impact of fish consumption on all-cause mortality in older people with and without dementia: a community-based cohort study
Aishat T. Bakre, Anthony Chen, Xuguang Tao, Jian Hou, Yuyou Yao, Alain Nevill, James J. Tang, Sabine Rohrmann, Jindong Ni, Zhi Hu, John Copeland, Ruoling Chen
European Journal of Nutrition.2022; 61(7): 3785. CrossRef
- Association of air pollution with dementia: a systematic review with meta-analysis including new cohort data from China
- Metabolic Risk/Epidemiology
- Influence of Pre-Pregnancy Underweight Body Mass Index on Fetal Abdominal Circumference, Estimated Weight, and Pregnancy Outcomes in Gestational Diabetes Mellitus
- Minji Kim, Kyu-Yeon Hur, Suk-Joo Choi, Soo-Young Oh, Cheong-Rae Roh
- Diabetes Metab J. 2022;46(3):499-505. Published online January 24, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0059

- 5,017 View
- 201 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - This study aimed to determine the influence of pre-pregnancy body mass index on pregnancy outcomes in gestational diabetes mellitus (GDM), comparing underweight patients with GDM with normal weight patients with GDM. Maternal baseline characteristics, ultrasonographic results, and pregnancy and neonatal outcomes were reviewed in 946 women with GDM with singleton pregnancies. Underweight patients with GDM showed a benign course in most aspects during pregnancy, except for developing a higher risk of giving birth to small for gestational age neonates. Underweight women with GDM required less insulin treatment, had a higher rate of vaginal delivery, and had a lower rate of cesarean delivery. In addition, their neonates were more likely to have fetal abdominal circumference and estimated fetal weight below the 10th percentile both at the time of GDM diagnosis and before delivery. Notably, their risk for preeclampsia and macrosomia were lower. Collectively, our data suggest that underweight women with GDM may require a different approach in terms of diagnosis and management throughout their pregnancy.
-
Citations
Citations to this article as recorded by- Challenges in the management of gestational diabetes mellitus in anorexia nervosa
Rija Siddiqui, Carrie J McAdams
Psychiatry Research Case Reports.2024; 3(1): 100215. CrossRef - Obesity Is Associated With Higher Risk of Adverse Maternal and Neonatal Outcomes Than Supervised Gestational Diabetes
Namju Seo, You Min Lee, Ye-jin Kim, Ji-hee Sung, Kyu-Yeon Hur, Suk-Joo Choi, Cheong-Rae Roh, Soo-young Oh
Journal of Korean Medical Science.2023;[Epub] CrossRef - Maternal pre-pregnancy obesity modifies the association between first-trimester thyroid hormone sensitivity and gestational Diabetes Mellitus: a retrospective study from Northern China
Honglin Sun, Yibo Zhou, Jia Liu, Ying Wang, Guang Wang
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef
- Challenges in the management of gestational diabetes mellitus in anorexia nervosa
- Metabolic Risk/Epidemiology
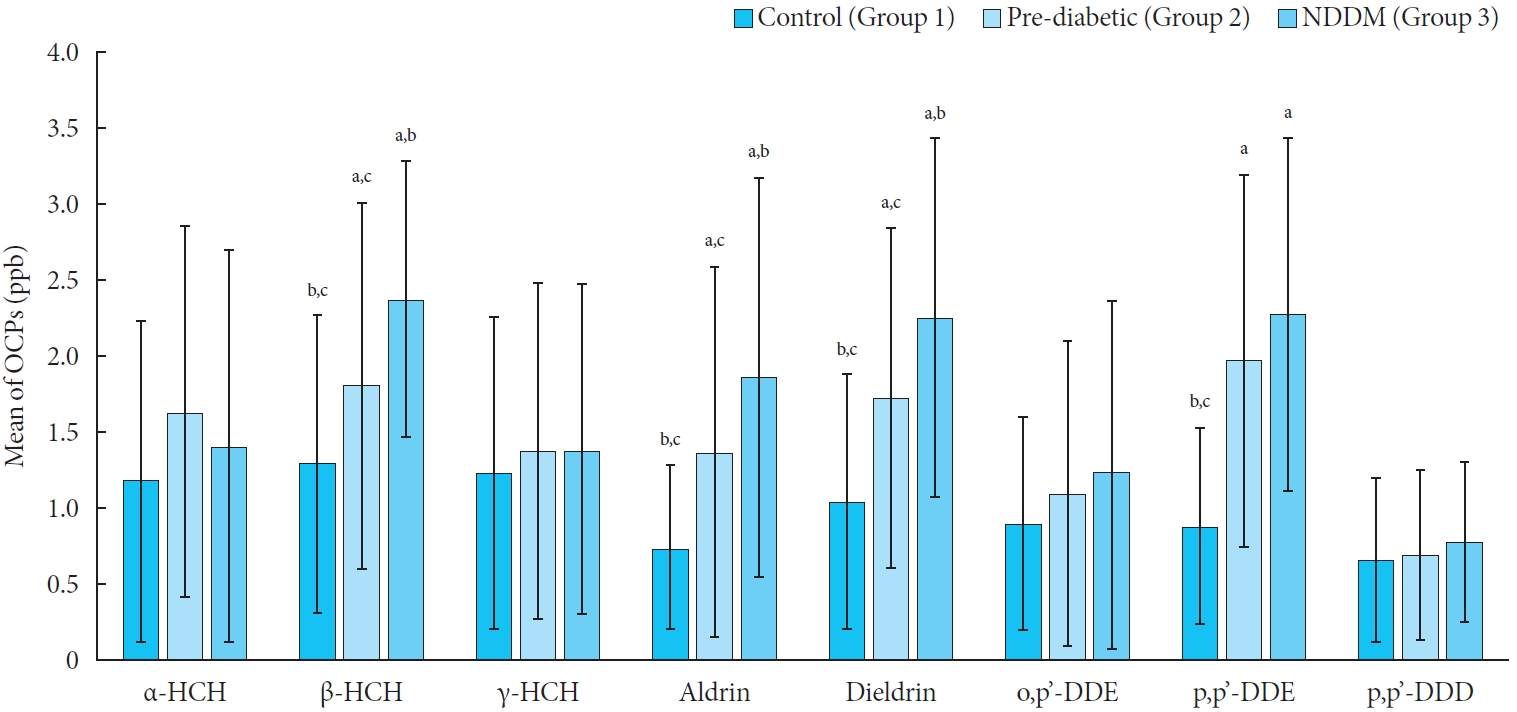
- Level of Organochlorine Pesticide in Prediabetic and Newly Diagnosed Diabetes Mellitus Patients with Varying Degree of Glucose Intolerance and Insulin Resistance among North Indian Population
- Shipra Tyagi, Brijesh Kumar Mishra, Tusha Sharma, Neha Tawar, Abdul Jamil Urfi, Basu Dev Banerjee, Sri Venkata Madhu
- Diabetes Metab J. 2021;45(4):558-568. Published online January 15, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0093
- 4,872 View
- 143 Download
- 10 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Organochlorine pesticides (OCPs) exposure may induce an endocrine disruption which may lead to the risk of developing diabetes through alteration and disturbance of glucose metabolism, insulin resistance, and destruction of β-cells. The present study determines the recent trend of OCPs residue in blood samples and their association with the known risk factors responsible for developing the risk of diabetes among the North Indian population.
Methods
Blood sample of 300 patients (100 each of normal glucose tolerance [NGT], prediabetes and newly detected diabetes mellitus [DM]) between the age group of 30 to 70 years were collected. OCPs residue in whole blood samples was analyzed by using gas chromatography equipped with a 63Ni selective electron capture detector.
Results
Significantly higher levels of β-hexachlorocyclohexane (HCH), dieldrin, and p,p’-dichloro-diphenyl-dichloroethylene (DDE) were found in the prediabetes and newly detected DM groups as compared to NGT group. Insulin resistance showed to be significantly positive correlation with β-HCH and dieldrin. Also, fasting and postprandial glucose levels were significantly positively correlated with levels of β-HCH, dieldrin, and p,p’-DDE. Further, when OCPs level was adjusted for age and body mass index (BMI), it was found that β-HCH, dieldrin, and p,p’-DDE levels in blood increases the risk of diabetes by 2.70, 2.83, and 2.55 times respectively. Moreover, when we adjust OCPs level based on BMI categories (BMI <23, ≥23, and ≤25, and >25 kg/m2); β-HCH and p,p’-DDE showed a significant risk of developing newly detected DM with BMI >25 and ≥23 and ≤25 kg/m2.
Conclusion
The OCPs level present in the environment may be responsible for biological, metabolic, and endocrine disruptions within the human body which may increase the risk of developing newly detected DM. Hence, OCPs exposure can play a crucial role in the etiology of diabetes. -
Citations
Citations to this article as recorded by- Combined effects of organochlorine pesticides on type 2 diabetes mellitus: Insights from endocrine disrupting effects of hormones
Jiayu Shi, Dandan Wei, Cuicui Ma, Jintian Geng, Mengzhen Zhao, Jian Hou, Wenqian Huo, Tao Jing, Chongjian Wang, Zhenxing Mao
Environmental Pollution.2024; 341: 122867. CrossRef - Associations of chronic exposure to a mixture of pesticides and type 2 diabetes mellitus in a Chinese elderly population
Tian Chen, Xiaohua Liu, Jianghua Zhang, Lulu Wang, Jin Su, Tao Jing, Ping Xiao
Chemosphere.2024; 351: 141194. CrossRef - Application of In Vitro Models for Studying the Mechanisms Underlying the Obesogenic Action of Endocrine-Disrupting Chemicals (EDCs) as Food Contaminants—A Review
Monika Kowalczyk, Jakub P. Piwowarski, Artur Wardaszka, Paulina Średnicka, Michał Wójcicki, Edyta Juszczuk-Kubiak
International Journal of Molecular Sciences.2023; 24(2): 1083. CrossRef - The diabetogenic effects of pesticides: Evidence based on epidemiological and toxicological studies
Yile Wei, Linping Wang, Jing Liu
Environmental Pollution.2023; 331: 121927. CrossRef - Pesticides and insulin resistance-related metabolic diseases: Evidences and mechanisms
Ali Arab, Sara Mostafalou
Pesticide Biochemistry and Physiology.2023; 195: 105521. CrossRef - Circulating organochlorine pesticide levels, genetic predisposition and the risk of incident type 2 diabetes
Chengyong Jia, Shiyang Zhang, Xu Cheng, Peiwen Li, Jun An, Xin Zhang, Wending Li, Yali Xu, Handong Yang, Tao Jing, Huan Guo, Meian He
Environmental Pollution.2023; 337: 122541. CrossRef - Targets for pollutants in rat and human pancreatic beta-cells: The effect of prolonged exposure to sub-lethal concentrations of hexachlorocyclohexane isomers on the expression of function- and survival-related proteins
Nela Pavlíková, Jan Šrámek, Martin Jaček, Jan Kovář, Vlasta Němcová
Environmental Toxicology and Pharmacology.2023; 104: 104299. CrossRef - Association of Organochlorine Pesticides With Genetic Markers of Endoplasmic Reticulum Stress in Type 2 Diabetes Mellitus: A Case–Control Study Among the North-Indian Population
Neha Tawar, Basu Dev Banerjee, Sri Venkata Madhu, Vivek Agrawal, Sanjay Gupta
Frontiers in Endocrinology.2022;[Epub] CrossRef - Acaricidal and insecticidal efficacy of new esters derivatives of a natural coumarin osthole
Xijie Shan, Min Lv, Jingru Wang, Yujia Qin, Hui Xu
Industrial Crops and Products.2022; 182: 114855. CrossRef - Association between organochlorine pesticides and nonalcoholic fatty liver disease in the National Health and Nutrition Examination Survey 2003–2004
Hyunji Sang, Kyu-Na Lee, Chang Hee Jung, Kyungdo Han, Eun Hee Koh
Scientific Reports.2022;[Epub] CrossRef
- Combined effects of organochlorine pesticides on type 2 diabetes mellitus: Insights from endocrine disrupting effects of hormones
- Cardiovascular Risk/Epidemiology
-
- Associations among Obesity Degree, Glycemic Status, and Risk of Heart Failure in 9,720,220 Korean Adults
- Eun-Jung Rhee, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Yang-Hyun Kim, Won-Young Lee
- Diabetes Metab J. 2020;44(4):592-601. Published online April 20, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0104
- Correction in: Diabetes Metab J 2020;44(5):783

- 6,636 View
- 142 Download
- 16 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background Recent studies suggest an association between diabetes and increased risk of heart failure (HF). However, the associations among obesity status, glycemic status, and risk of HF are not known. In this study, we analyzed whether the risk of HF increases in participants according to baseline glycemic status and whether this increased risk is associated with obesity status.
Methods We analyzed the risk of HF according to baseline glycemic status (normoglycemia, impaired fasting glucose [IFG], and diabetes) in 9,720,220 Koreans who underwent Korean National Health Screening in 2009 without HF at baseline with a median follow-up period of 6.3 years. The participants were divided into five and six groups according to baseline body mass index (BMI) and waist circumference, respectively.
Results Participants with IFG and those with diabetes showed a 1.08- and 1.86-fold increased risk of HF, respectively, compared to normoglycemic participants. Compared to the normal weight group (BMI, 18.5 to 22.9 kg/m2), the underweight group (BMI <18.5 kg/m2) showed a 1.7-fold increased risk of HF, and those with BMI ≥30 kg/m2 showed a 1.1-fold increased risk of HF, suggesting a J-shaped association with BMI. When similar analyses were performed for different glycemic statuses, the J-shaped association between BMI and HF risk was consistently observed in both groups with and without diabetes.
Conclusion Participants with IFG and diabetes showed a significantly increased HF risk compared to normoglycemic participants. This increased risk of HF was mostly prominent in underweight and class II obese participants than in participants with normal weight.
-
Citations
Citations to this article as recorded by- Association between underweight and risk of heart failure in diabetes patients
Tae Kyung Yoo, Kyung‐Do Han, Eun‐Jung Rhee, Won‐Young Lee
Journal of Cachexia, Sarcopenia and Muscle.2024; 15(2): 671. CrossRef - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - Research on obesity using the National Health Information Database: recent trends
Eun-Jung Rhee
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 35. CrossRef - Impact of mental disorders on the risk of heart failure among Korean patients with diabetes: a cohort study
Tae Kyung Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Diabetology.2023;[Epub] CrossRef - Differential Impact of Obesity on the Risk of Diabetes Development in Two Age Groups: Analysis from the National Health Screening Program
Tae Kyung Yoo, Kyung-Do Han, Yang-Hyun Kim, Ga Eun Nam, Sang Hyun Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2023; 47(6): 846. CrossRef - Characterization of the oxidative stress and inflammatory markers in metabolically healthy obese individuals
Hazhmat Ali
Al-Kufa University Journal for Biology.2023; 15(3): 28. CrossRef - The Influence of Obesity and Metabolic Health on Vascular Health
Eun-Jung Rhee
Endocrinology and Metabolism.2022; 37(1): 1. CrossRef - Changes in Patterns of Physical Activity and Risk of Heart Failure in Newly Diagnosed Diabetes Mellitus Patients
Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2022; 46(2): 327. CrossRef - Evaluating Triglyceride and Glucose Index as a Simple and Easy-to-Calculate Marker for All-Cause and Cardiovascular Mortality
Kyung-Soo Kim, Sangmo Hong, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
Journal of General Internal Medicine.2022; 37(16): 4153. CrossRef - Impact of hypoglycemia at the time of hospitalization for heart failure from emergency department on major adverse cardiovascular events in patients with and without type 2 diabetes
Seon-Ah Cha, Jae-Seung Yun, Gee-Hee Kim, Yu-Bae Ahn
Cardiovascular Diabetology.2022;[Epub] CrossRef - Insulin resistance and heart failure with preserved ejection fraction. Pathogenetic and therapeutic crossroads
O. V. Tsygankova, N. E. Evdokimova, V. V. Veretyuk, L. D. Latyntseva, A. S. Ametov
Diabetes mellitus.2022; 25(6): 535. CrossRef - The association between metabolic syndrome and heart failure in middle-aged male and female: Korean population-based study of 2 million individuals
Tae-Eun Kim, Hyeongsu Kim, JiDong Sung, Duk-Kyung Kim, Myoung-Soon Lee, Seong Woo Han, Hyun-Joong Kim, Sung Hea Kim, Kyu-Hyung Ryu
Epidemiology and Health.2022; 44: e2022078. CrossRef - Diabetes and Heart Failure
Eun-Jung Rhee
The Journal of Korean Diabetes.2021; 22(1): 12. CrossRef - Prediabetes and the risk of heart failure: A meta‐analysis
Xiaoyan Cai, Xiong Liu, Lichang Sun, Yiting He, Sulin Zheng, Yang Zhang, Yuli Huang
Diabetes, Obesity and Metabolism.2021; 23(8): 1746. CrossRef - Diabetes and Heart Failure
Eun-Jung Rhee
Cardiovascular Prevention and Pharmacotherapy.2021; 3(2): 21. CrossRef - Effects of Lipid Overload on Heart in Metabolic
Diseases
An Yan, Guinan Xie, Xinya Ding, Yi Wang, Liping Guo
Hormone and Metabolic Research.2021; 53(12): 771. CrossRef - Obesity Degree and Glycemic Status: Factors That Should Be Considered in Heart Failure
Hye Soon Kim
Diabetes & Metabolism Journal.2020; 44(4): 529. CrossRef - Letter: Associations among Obesity Degree, Glycemic Status, and Risk of Heart Failure in 9,720,220 Korean Adults (Diabetes Metab J 2020;44:592-601)
Darae Kim
Diabetes & Metabolism Journal.2020; 44(5): 777. CrossRef - Response: Associations among Obesity Degree, Glycemic Status, and Risk of Heart Failure in 9,720,220 Korean Adults (Diabetes Metab J 2020;44:592-601)
Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2020; 44(5): 781. CrossRef
- Association between underweight and risk of heart failure in diabetes patients
- Genetics
- Severity of Nonalcoholic Fatty Liver Disease in Type 2 Diabetes Mellitus: Relationship between Nongenetic Factors and PNPLA3/HSD17B13 Polymorphisms
- Mattia Bellan, Cosimo Colletta, Matteo Nazzareno Barbaglia, Livia Salmi, Roberto Clerici, Venkata Ramana Mallela, Luigi Mario Castello, Giuseppe Saglietti, Gian Piero Carnevale Schianca, Rosalba Minisini, Mario Pirisi
- Diabetes Metab J. 2019;43(5):700-710. Published online July 29, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0201
- 4,927 View
- 76 Download
- 16 Web of Science
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The prevalence of nonalcoholic fatty liver disease (NAFLD) in patients with type 2 diabetes mellitus (T2DM) is high, though its severity is often underestimated. Our aim is to provide an estimate of the prevalence of severe NAFLD in T2DM and identify its major predictors.
Methods T2DM patients (
n =328) not previously known to have NAFLD underwent clinical assessment, transient elastography with measure of liver stiffness (LS) and controlled attenuation parameter (CAP), and genotyping for patatin like phospholipase domain containing 3 (PNPLA3 ) and 17β-hydroxysteroid-dehydrogenase type 13 (HSD17B13 ).Results Median LS was 6.1 kPa (4.9 to 8.6). More than one-fourth patients had advanced liver disease, defined as LS ≥7.9 kPa (
n =94/238, 29%), and had a higher body mass index (BMI) than those with a LS <7.9 kPa. Carriage of the G allele in thePNPLA3 gene was associated with higher LS, being 5.9 kPa (4.7 to 7.7) in C/C homozygotes, 6.1 kPa (5.2 to 8.7) in C/G heterozygotes, and 6.8 kPa (5.8 to 9.2) in G/G homozygotes (P =0.01). This trend was absent in patients with ≥1 mutatedHSD17B13 allele. In a multiple linear regression model, BMI andPNPLA3 genotype predicted LS, while age, gender, disease duration, and glycosylated hemoglobin did not fit into the model. None of these variables was confirmed to be predictive among carriers of at least oneHSD17B13 mutated allele. There was no association between CAP and polymorphisms ofPNPLA3 orHSD17B13 .Conclusion Advanced NAFLD is common among T2DM patients. LS is predicted by both BMI and
PNPLA3 polymorphism, the effect of the latter being modulated by mutatedHSD17B13 .-
Citations
Citations to this article as recorded by- miRNA and lncRNA as potential tissue biomarkers in hepatocellular carcinoma
Venkata Ramana Mallela, Marie Rajtmajerová, Andriy Trailin, Václav Liška, Kari Hemminki, Filip Ambrozkiewicz
Non-coding RNA Research.2024; 9(1): 24. CrossRef - 17-Beta-Hydroxysteroid Dehydrogenase 13 Loss of Function Does Not Confer Protection to Nonalcoholic Fatty Liver Disease in Indian Population
Bale Govardhan, V. Kulkarni Anand, Padaki Nagaraja Rao, P. Balachandran Menon, Sharma Mithun, Mitnala Sasikala, T.R. Sowmya, Sekaran Anuradha, C. Pawar Smita, D. Nageshwar Reddy, Vishnubhotla Ravikanth
Journal of Clinical and Experimental Hepatology.2024; 14(4): 101371. CrossRef - Review article: the role of HSD17B13 on global epidemiology, natural history, pathogenesis and treatment of NAFLD
Maral Amangurbanova, Daniel Q. Huang, Rohit Loomba
Alimentary Pharmacology & Therapeutics.2023; 57(1): 37. CrossRef - Identification of shared genetic architecture between non-alcoholic fatty liver disease and type 2 diabetes: A genome-wide analysis
Yajing Tan, Qian He, Kei Hang Katie Chan
Frontiers in Endocrinology.2023;[Epub] CrossRef - Polymorphisms of HSD17B13, GCKR, HFE, and CP as factors of the development of non-alcoholic fatty liver disease and comorbid diseases
O. V. Smirnova, D. V. Lagutinskaya
Meditsinskiy sovet = Medical Council.2023; (8): 119. CrossRef - Global prevalence of non-alcoholic fatty liver disease in type 2 diabetes mellitus: an updated systematic review and meta-analysis
Elina En Li Cho, Chong Zhe Ang, Jingxuan Quek, Clarissa Elysia Fu, Lincoln Kai En Lim, Zane En Qi Heng, Darren Jun Hao Tan, Wen Hui Lim, Jie Ning Yong, Rebecca Zeng, Douglas Chee, Benjamin Nah, Cosmas Rinaldi Adithya Lesmana, Aung Hlaing Bwa, Khin Maung W
Gut.2023; 72(11): 2138. CrossRef - HSD17B13 and other liver fat-modulating genes predict development of hepatocellular carcinoma among HCV-positive cirrhotics with and without viral clearance after DAA treatment
Michela E. Burlone, Mattia Bellan, Matteo N. Barbaglia, Ginevra Mocchetti, Venkata R. Mallela, Rosalba Minisini, Cristina Rigamonti, Mario Pirisi
Clinical Journal of Gastroenterology.2022; 15(2): 301. CrossRef - Influence of Type 2 Diabetes in the Association of PNPLA3 rs738409 and TM6SF2 rs58542926 Polymorphisms in NASH Advanced Liver Fibrosis
Pablo Gabriel-Medina, Roser Ferrer-Costa, Francisco Rodriguez-Frias, Andreea Ciudin, Salvador Augustin, Jesus Rivera-Esteban, Juan M. Pericàs, David Martinez Selva
Biomedicines.2022; 10(5): 1015. CrossRef - Triglyceride and glucose index is a simple and easy‐to‐calculate marker associated with nonalcoholic fatty liver disease
Kyung‐Soo Kim, Sangmo Hong, Hong‐Yup Ahn, Cheol‐Young Park
Obesity.2022; 30(6): 1279. CrossRef - Prevalence of elevated liver stiffness in patients with type 1 and type 2 diabetes: A systematic review and meta-analysis
Stefano Ciardullo, Gianluca Perseghin
Diabetes Research and Clinical Practice.2022; 190: 109981. CrossRef - Associations of Hydroxysteroid 17-beta Dehydrogenase 13 Variants with Liver Histology in Chinese Patients with Metabolic-associated Fatty Liver Disease
Wen-Yue Liu, Mohammed Eslam, Kenneth I. Zheng, Hong-Lei Ma, Rafael S. Rios, Min-Zhi Lv, Gang Li, Liang-Jie Tang, Pei-Wu Zhu, Xiao-Dong Wang, Christopher D. Byrne, Giovanni Targher, Jacob George, Ming-Hua Zheng
Journal of Clinical and Translational Hepatology.2021; 000(000): 000. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Eugene Han, Mi Kyung Kim, Byoung Kuk Jang, Hye Soon Kim
Diabetes & Metabolism Journal.2021; 45(5): 698. CrossRef - Genetic Polymorphisms and Clinical Features in Diabetic Patients With Fatty Liver: Results From a Single-Center Experience in Southern Italy
Rosanna Villani, Grazia Pia Magnati, Giuseppe De Girolamo, Moris Sangineto, Antonino Davide Romano, Tommaso Cassano, Gaetano Serviddio
Frontiers in Medicine.2021;[Epub] CrossRef - Interplay of PNPLA3 and HSD17B13 Variants in Modulating the Risk of Hepatocellular Carcinoma among Hepatitis C Patients
Carla De Benedittis, Mattia Bellan, Martina Crevola, Elena Boin, Matteo Nazzareno Barbaglia, Venkata Ramana Mallela, Paolo Ravanini, Elisa Ceriani, Stefano Fangazio, Pier Paolo Sainaghi, Michela Emma Burlone, Rosalba Minisini, Mario Pirisi
Gastroenterology Research and Practice.2020; 2020: 1. CrossRef - Toward Genetic Prediction of Nonalcoholic Fatty Liver Disease Trajectories: PNPLA3 and Beyond
Marcin Krawczyk, Roman Liebe, Frank Lammert
Gastroenterology.2020; 158(7): 1865. CrossRef - The effect of liraglutide on nonalcoholic fatty liver disease in type 2 diabetes mellitus
Xueyang Zhang, Ran Bai, Yong Jia, Junwei Zong, Yongbo Wang, Yanan Dong
International Journal of Diabetes in Developing Countries.2020; 40(4): 491. CrossRef - Lifestyle and silymarin: a fight against liver damage in NAFLD associated - prediabetic disease
Cosimo Colletta, Alessandro Colletta, Giuseppe Placentino
Journal of Diabetes & Metabolic Disorders.2020; 19(2): 883. CrossRef
- miRNA and lncRNA as potential tissue biomarkers in hepatocellular carcinoma
- Obesity and Metabolic Syndrome
- The Association between Z-Score of Log-Transformed A Body Shape Index and Cardiovascular Disease in Korea
- Wankyo Chung, Jung Hwan Park, Hye Soo Chung, Jae Myung Yu, Shinje Moon, Dong Sun Kim
- Diabetes Metab J. 2019;43(5):675-682. Published online April 26, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0169
- 7,747 View
- 59 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background In order to overcome the limitations of body mass index (BMI) and waist circumference (WC), the z-score of the log-transformed A Body Shape Index (LBSIZ) has recently been introduced. In this study, we analyzed the relationship between the LBSIZ and cardiovascular disease (CVD) in a Korean representative sample.
Methods Data were collected from the Korea National Health and Nutrition Examination VI to V. The association between CVD and obesity indices was analyzed using a receiver operating characteristic curve. The cut-off value for the LBSIZ was estimated using the Youden index, and the odds ratio (OR) for CVD was determined via multivariate logistic regression analysis. ORs according to the LBSIZ value were analyzed using restricted cubic spline regression plots.
Results A total of 31,227 Korean healthy adults were analyzed. Area under the curve (AUC) of LBSIZ against CVD was 0.686 (95% confidence interval [CI], 0.671 to 0.702), which was significantly higher than the AUC of BMI (0.583; 95% CI, 0.567 to 0.599) or WC (0.646; 95% CI, 0.631 to 0.661) (
P <0.001). Similar results were observed for stroke and coronary artery diseases. The cut-off value for the LBSIZ was 0.35 (sensitivity, 64.5%; specificity, 64%; OR, 1.29, 95% CI, 1.12 to 1.49). Under restricted cubic spline regression, LBSIZ demonstrated that OR started to increase past the median value.Conclusion The findings of this study suggest that the LBSIZ might be more strongly associated with CVD risks compared to BMI or WC. These outcomes would be helpful for CVD risk assessment in clinical settings, especially the cut-off value of the LBSIZ suggested in this study.
-
Citations
Citations to this article as recorded by- Body Shape Index and Cardiovascular Risk in Individuals With Obesity
Nazlı Hacıağaoğlu, Can Öner, Hüseyin Çetin, Engin Ersin Şimşek
Cureus.2022;[Epub] CrossRef - Association between body shape index and risk of mortality in the United States
Heysoo Lee, Hye Soo Chung, Yoon Jung Kim, Min Kyu Choi, Yong Kyun Roh, Wankyo Chung, Jae Myung Yu, Chang-Myung Oh, Shinje Moon
Scientific Reports.2022;[Epub] CrossRef - Utility of the Z-score of log-transformed A Body Shape Index (LBSIZ) in the assessment for sarcopenic obesity and cardiovascular disease risk in the United States
Wankyo Chung, Jung Hwan Park, Hye Soo Chung, Jae Myung Yu, Dong Sun Kim, Shinje Moon
Scientific Reports.2019;[Epub] CrossRef
- Body Shape Index and Cardiovascular Risk in Individuals With Obesity
- Obesity and Metabolic Syndrome
-
- The Risk of Myocardial Infarction and Ischemic Stroke According to Waist Circumference in 21,749,261 Korean Adults: A Nationwide Population-Based Study
- Jung-Hwan Cho, Eun-Jung Rhee, Se-Eun Park, Hyemi Kwon, Jin-Hyung Jung, Kyung-Do Han, Yong-Gyu Park, Hye Soon Park, Yang-Hyun Kim, Soon-Jib Yoo, Won-Young Lee
- Diabetes Metab J. 2019;43(2):206-221. Published online December 27, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0039
- 5,606 View
- 102 Download
- 22 Web of Science
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Waist circumference (WC) is a well-known obesity index that predicts cardiovascular disease (CVD). We studied the relationship between baseline WC and development of incident myocardial infarction (MI) and ischemic stroke (IS) using a nationwide population-based cohort, and evaluated if its predictability is better than body mass index (BMI).
Methods Our study included 21,749,261 Koreans over 20 years of age who underwent the Korean National Health Screening between 2009 and 2012. The occurrence of MI or IS was investigated until the end of 2015 using National Health Insurance Service data.
Results A total of 127,289 and 181,637 subjects were newly diagnosed with MI and IS. The incidence rate and hazard ratio of MI and IS increased linearly as the WC level increased, regardless of adjustment for BMI. When the analyses were performed according to 11 groups of WC, the lowest risk of MI was found in subjects with WC of 70 to 74.9 and 65 to 69.9 cm in male and female, and the lowest risk of IS in subjects with WC of 65 to 69.9 and 60 to 64.9 cm in male and female, respectively. WC showed a better ability to predict CVD than BMI with smaller Akaike information criterion. The optimal WC cutoffs were 84/78 cm for male/female for predicting MI, and 85/78 cm for male/female for predicting IS.
Conclusion WC had a significant linear relationship with the risk of MI and IS and the risk began to increase from a WC that was lower than expected.
-
Citations
Citations to this article as recorded by- Usefulness of New Criteria for Metabolic Syndrome Optimized for Prediction of Cardiovascular Diseases in Japanese
Yurie Yamazaki, Kazuya Fujihara, Takaaki Sato, Mayuko Harada Yamada, Yuta Yaguchi, Yasuhiro Matsubayashi, Takaho Yamada, Satoru Kodama, Kiminori Kato, Hitoshi Shimano, Hirohito Sone
Journal of Atherosclerosis and Thrombosis.2024; 31(4): 382. CrossRef - Association between body composition and subsequent cardiovascular diseases among 5-year breast cancer survivors
Ji Soo Kim, Jihun Song, Seulggie Choi, Sung Min Kim, Young Jun Park, Sun Jae Park, Yoosun Cho, Yun Hwan Oh, Seogsong Jeong, Kyae Hyung Kim, Sang Min Park
Nutrition, Metabolism and Cardiovascular Diseases.2024;[Epub] CrossRef - Body mass index, waist circumference and cardiovascular diseases in transitional ages (40 and 66 years)
Jung Eun Yoo, Kyungdo Han, Jin‐Hyung Jung, Yang‐Im Hur, Yang Hyun Kim, Eun Sook Kim, Jang Won Son, Eun‐Jung Rhee, Won‐Young Lee, Ga Eun Nam
Journal of Cachexia, Sarcopenia and Muscle.2023; 14(1): 369. CrossRef - Risk factors for stroke among anthropometric indices and lipid profiles in the Korean population: a large-scale cross-sectional study
Mi Hong Yim, Young Ju Jeon, Bum Ju Lee
Scientific Reports.2023;[Epub] CrossRef - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - Research on obesity using the National Health Information Database: recent trends
Eun-Jung Rhee
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 35. CrossRef - Association between the weight-adjusted waist index and stroke: a cross-sectional study
Jiayi Ye, Yanjie Hu, Xinrong Chen, Zhe Yin, Xingzhu Yuan, Liping Huang, Ka Li
BMC Public Health.2023;[Epub] CrossRef - Increased risk of ischemic stroke associated with elevated gamma-glutamyl transferase level in adult cancer survivors: a population-based cohort study
Kyuwoong Kim, Hyeyun Jung, Edvige Di Giovanna, Tae Joon Jun, Young-Hak Kim
Scientific Reports.2023;[Epub] CrossRef - Changes in body composition and subsequent cardiovascular disease risk among 5-year breast cancer survivors
Ji Soo Kim, Jihun Song, Seulggie Choi, Sang Min Park
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Association between Stroke and Abdominal Obesity in the Middle-Aged and Elderly Korean Population: KNHANES Data from 2011–2019
Jong Yeon Kim, Sung Min Cho, Youngmin Yoo, Taesic Lee, Jong Koo Kim
International Journal of Environmental Research and Public Health.2022; 19(10): 6140. CrossRef - Prevalence of metabolic syndrome and related factors in a large sample of antipsychotic naïve patients with first-episode psychosis: Baseline results from the PAFIP cohort
Nathalia Garrido-Torres, Miguel Ruiz-Veguilla, Luis Alameda, Manuel Canal-Rivero, María Juncal Ruiz, Marcos Gómez-Revuelta, Rosa Ayesa-Arriola, Ana Rubio-García, Benedicto Crespo-Facorro, Javier Vázquez-Bourgon
Schizophrenia Research.2022; 246: 277. CrossRef - Development and validation of risk prediction models for stroke and mortality among patients with type 2 diabetes in northern China
X. Shao, H. Liu, F. Hou, Y. Bai, Z. Cui, Y. Lin, X. Jiang, P. Bai, Y. Wang, Y. Zhang, C. Lu, H. Liu, S. Zhou, P. Yu
Journal of Endocrinological Investigation.2022; 46(2): 271. CrossRef - Neck circumference for predicting the occurrence of future cardiovascular events: A 7.6-year longitudinal study
Tingting Hu, Yun Shen, Weijie Cao, Yiting Xu, Yufei Wang, Xiaojing Ma, Yuqian Bao
Nutrition, Metabolism and Cardiovascular Diseases.2022; 32(12): 2830. CrossRef - A prospective study of waist circumference trajectories and incident cardiovascular disease in China: the Kailuan Cohort Study
Liang Wang, Yujin Lee, Yuntao Wu, Xinyuan Zhang, Cheng Jin, Zhe Huang, Yixin Wang, Zhiyi Wang, Penny Kris-Etherton, Shouling Wu, Xiang Gao
The American Journal of Clinical Nutrition.2021; 113(2): 338. CrossRef - The Repeatedly Elevated Fatty Liver Index Is Associated With Increased Mortality: A Population-Based Cohort Study
Chang-Hoon Lee, Kyung-Do Han, Da Hye Kim, Min-Sun Kwak
Frontiers in Endocrinology.2021;[Epub] CrossRef - Obesity Degree and Glycemic Status: Factors That Should Be Considered in Heart Failure
Hye Soon Kim
Diabetes & Metabolism Journal.2020; 44(4): 529. CrossRef - Exposure-weighted scoring for metabolic syndrome and the risk of myocardial infarction and stroke: a nationwide population-based study
Eun Young Lee, Kyungdo Han, Da Hye Kim, Yong-Moon Park, Hyuk-Sang Kwon, Kun-Ho Yoon, Mee Kyoung Kim, Seung-Hwan Lee
Cardiovascular Diabetology.2020;[Epub] CrossRef - Predicting the Development of Myocardial Infarction in Middle-Aged Adults with Type 2 Diabetes: A Risk Model Generated from a Nationwide Population-Based Cohort Study in Korea
Seung-Hwan Lee, Kyungdo Han, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim
Endocrinology and Metabolism.2020; 35(3): 636. CrossRef - Obesity Fact Sheet in Korea, 2018: Data Focusing on Waist Circumference and Obesity-Related Comorbidities
Ga Eun Nam, Yang-Hyun Kim, Kyungdo Han, Jin-Hyung Jung, Yong Gyu Park, Kwan-Woo Lee, Eun-Jung Rhee, Jang Won Son, Seong-Su Lee, Hyuk-Sang Kwon, Won-Young Lee, Soon Jib Yoo
Journal of Obesity & Metabolic Syndrome.2019; 28(4): 236. CrossRef - Simply the Best: Anthropometric Indices for Predicting Cardiovascular Disease
Jie-Eun Lee
Diabetes & Metabolism Journal.2019; 43(2): 156. CrossRef - Association and Interaction Analysis of Lipid Accumulation Product with Impaired Fasting Glucose Risk: A Cross-Sectional Survey
Jian Song, Xue Chen, Yuhong Jiang, Jing Mi, Yuyuan Zhang, Yingying Zhao, Xuesen Wu, Huaiquan Gao
Journal of Diabetes Research.2019; 2019: 1. CrossRef - Letter: Association of Z-Score of the Log-Transformed A Body Shape Index with Cardiovascular Disease in People Who Are Obese but Metabolically Healthy: The Korea National Health and Nutrition Examination Survey 2007-2010 (J Obes Metab Syndr 2018;27:158-65
Eun-Jung Rhee
Journal of Obesity & Metabolic Syndrome.2019; 28(2): 139. CrossRef - Response: The Differential Association between Muscle Strength and Diabetes Mellitus According to the Presence or Absence of Obesity (J Obes Metab Syndr 2019;28:46-52)
Bo Kyung Koo
Journal of Obesity & Metabolic Syndrome.2019; 28(4): 297. CrossRef
- Usefulness of New Criteria for Metabolic Syndrome Optimized for Prediction of Cardiovascular Diseases in Japanese
- Epidemiology
- Association of Thigh Muscle Mass with Insulin Resistance and Incident Type 2 Diabetes Mellitus in Japanese Americans
- Seung Jin Han, Edward J. Boyko, Soo-Kyung Kim, Wilfred Y. Fujimoto, Steven E. Kahn, Donna L. Leonetti
- Diabetes Metab J. 2018;42(6):488-495. Published online September 5, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0022
- 4,595 View
- 63 Download
- 34 Web of Science
- 34 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Skeletal muscle plays a major role in glucose metabolism. We investigated the association between thigh muscle mass, insulin resistance, and incident type 2 diabetes mellitus (T2DM) risk. In addition, we examined the role of body mass index (BMI) as a potential effect modifier in this association.
Methods This prospective study included 399 Japanese Americans without diabetes (mean age 51.6 years) who at baseline had an estimation of thigh muscle mass by computed tomography and at baseline and after 10 years of follow-up a 75-g oral glucose tolerance test and determination of homeostasis model assessment of insulin resistance (HOMA-IR). We fit regression models to examine the association between thigh muscle area and incidence of T2DM and change in HOMA-IR, both measured over 10 years.
Results Thigh muscle area was inversely associated with future HOMA-IR after adjustment for age, sex, BMI, HOMA-IR, fasting plasma glucose, total abdominal fat area, and thigh subcutaneous fat area at baseline (
P =0.033). The 10-year cumulative incidence of T2DM was 22.1%. A statistically significant interaction between thigh muscle area and BMI was observed, i.e., greater thigh muscle area was associated with lower risk of incident T2DM for subjects at lower levels of BMI, but this association diminished at higher BMI levels.Conclusion Thigh muscle mass area was inversely associated with future insulin resistance. Greater thigh muscle area predicts a lower risk of incident T2DM for leaner Japanese Americans.
-
Citations
Citations to this article as recorded by- Shape phenotype of thigh fat and muscle and risk of major adverse cardiovascular events after fragility hip fracture
Sheen‐Woo Lee, Seung‐Chan Kim, Jeong‐Eun Yi
Journal of Cachexia, Sarcopenia and Muscle.2024; 15(1): 331. CrossRef - CD36 gene variant rs1761667(G/A) as a biomarker in obese type 2 diabetes mellitus cases
Ashwin Kumar Shukla, Amreen Shamsad, Atar Singh Kushwah, Shalini Singh, Kauser Usman, Monisha Banerjee
Egyptian Journal of Medical Human Genetics.2024;[Epub] CrossRef - Association between macro- and microvascular damage and sarcopenia index in individuals with type 2 diabetes mellitus
Hui Xu, Qun-Yan Xiang, Jun-Kun Zhan, Yi Wang, Yan-Jiao Wang, Shuang Li, You-Shuo Liu
Applied Physiology, Nutrition, and Metabolism.2024;[Epub] CrossRef - More appendicular lean mass relative to body mass index is associated with lower incident diabetes in middle-aged adults in the CARDIA study
Melanie S. Haines, Aaron Leong, Bianca C. Porneala, Victor W. Zhong, Cora E. Lewis, Pamela J. Schreiner, Karen K. Miller, James B. Meigs, Mercedes R. Carnethon
Nutrition, Metabolism and Cardiovascular Diseases.2023; 33(1): 105. CrossRef - Involvement of the fecal amino acid profile in a clinical and anthropometric study of Mexican patients with insulin resistance and type 2 diabetes mellitus
Mayra Paloma Macías-Acosta, Lorena Valerdi-Contreras, Ericka Denise Bustos-Angel, Rudy Antonio García-Reyes, Monserrat Alvarez-Zavala, Marisela González-Ávila
Amino Acids.2022; 54(1): 47. CrossRef - Association of serum creatinine levels and risk of type 2 diabetes mellitus in Korea: a case control study
Do Kyeong Song, Young Sun Hong, Yeon-Ah Sung, Hyejin Lee
BMC Endocrine Disorders.2022;[Epub] CrossRef - The Relationship Between Fat-Free Mass and Glucose Metabolism in Children and Adolescents: A Systematic Review and Meta-Analysis
Lijun Wu, Fangfang Chen, Junting Liu, Dongqing Hou, Tao Li, Yiren Chen, Zijun Liao
Frontiers in Pediatrics.2022;[Epub] CrossRef - Is imaging-based muscle quantity associated with risk of diabetes? A meta-analysis of cohort studies
Shanhu Qiu, Xue Cai, Yang Yuan, Bo Xie, Zilin Sun, Tongzhi Wu
Diabetes Research and Clinical Practice.2022; 189: 109939. CrossRef - Effects of Exercise Intervention on Type 2 Diabetes Patients With Abdominal Obesity and Low Thigh Circumference (EXTEND): Study Protocol for a Randomized Controlled Trial
Dan Liu, Ying Zhang, Liang Wu, Jingyi Guo, Xiangtian Yu, Huasheng Yao, Rui Han, Tianshu Ma, Yuchan Zheng, Qiongmei Gao, Qichen Fang, Yan Zhao, Yanan Zhao, Biao Sun, Weiping Jia, Huating Li
Frontiers in Endocrinology.2022;[Epub] CrossRef - Association between diabetic peripheral neuropathy and sarcopenia: A systematic review and meta‐analysis
Thapat Wannarong, Persen Sukpornchairak, Weerakit Naweera, Christopher D. Geiger, Patompong Ungprasert
Geriatrics & Gerontology International.2022; 22(9): 785. CrossRef - Synergistic Interaction between Hyperuricemia and Abdominal Obesity as a Risk Factor for Metabolic Syndrome Components in Korean Population
Min Jin Lee, Ah Reum Khang, Yang Ho Kang, Mi Sook Yun, Dongwon Yi
Diabetes & Metabolism Journal.2022; 46(5): 756. CrossRef - HOMA-IR as a predictor of Health Outcomes in Patients with Metabolic Risk Factors: A Systematic Review and Meta-analysis
José G. González-González, Jorge R. Violante-Cumpa, Miguel Zambrano-Lucio, Erick Burciaga-Jimenez, Patricia L. Castillo-Morales, Mariano Garcia-Campa, Ricardo César Solis, Alejandro D González-Colmenero, René Rodríguez-Gutiérrez
High Blood Pressure & Cardiovascular Prevention.2022; 29(6): 547. CrossRef - Maternal height as a predictor of glucose intolerance in the postpartum and its relationship with maternal pre-gestational weight
Catarina Cidade-Rodrigues, Filipe M. Cunha, Catarina Chaves, Fabiana Castro, Catarina Pereira, Sílvia Paredes, Margarida Silva-Vieira, Anabela Melo, Odete Figueiredo, Cláudia Nogueira, Ana Morgado, Mariana Martinho, Maria C. Almeida, Margarida Almeida
Archives of Gynecology and Obstetrics.2022; 307(2): 601. CrossRef - Correlation of body composition in early pregnancy on gestational diabetes mellitus under different body weights before pregnancy
Li Xintong, Xu Dongmei, Zhang Li, Cao Ruimin, Hao Yide, Cui Lingling, Chen Tingting, Guo Yingying, Li Jiaxin
Frontiers in Endocrinology.2022;[Epub] CrossRef - Relationship between low skeletal muscle mass, sarcopenic obesity and left ventricular diastolic dysfunction in Korean adults
Jee Hee Yoo, Sung Woon Park, Ji Eun Jun, Sang‐Man Jin, Kyu Yeon Hur, Moon‐Kyu Lee, Mira Kang, Gyuri Kim, Jae Hyeon Kim
Diabetes/Metabolism Research and Reviews.2021;[Epub] CrossRef - Skeletal Muscle and Metabolic Health: How Do We Increase Muscle Mass and Function in People with Type 2 Diabetes?
Ebaa Al-Ozairi, Dalal Alsaeed, Dherar Alroudhan, Nia Voase, Amal Hasan, Jason M R Gill, Naveed Sattar, Paul Welsh, Cindy M Gray, Jirapitcha Boonpor, Carlos Celis-Morales, Stuart R Gray
The Journal of Clinical Endocrinology & Metabolism.2021; 106(2): 309. CrossRef - Association of the triglyceride and glucose index with low muscle mass: KNHANES 2008–2011
Jung A. Kim, Soon Young Hwang, Ji Hee Yu, Eun Roh, So-hyeon Hong, You-Bin Lee, Nam Hoon Kim, Hye Jin Yoo, Ji A. Seo, Nan Hee Kim, Sin Gon Kim, Sei Hyun Baik, Kyung Mook Choi
Scientific Reports.2021;[Epub] CrossRef - ADAS-viewer: web-based application for integrative analysis of multi-omics data in Alzheimer’s disease
Seonggyun Han, Jaehang Shin, Hyeim Jung, Jane Ryu, Habtamu Minassie, Kwangsik Nho, Insong Koh, Younghee Lee
npj Systems Biology and Applications.2021;[Epub] CrossRef - Relative associations of abdominal and thigh compositions with cardiometabolic diseases in African Caribbean men
Curtis Tilves, Joseph M. Zmuda, Allison L. Kuipers, Sangeeta Nair, John Jeffrey Carr, James G. Terry, Shyamal Peddada, Victor Wheeler, Iva Miljkovic
Obesity Science & Practice.2021; 7(6): 738. CrossRef - Changes in creatinine‐to‐cystatin C ratio over 4 years, risk of diabetes, and cardiometabolic control: The China Health and Retirement Longitudinal Study
Shanhu Qiu, Xue Cai, Yang Yuan, Bo Xie, Zilin Sun, Tongzhi Wu
Journal of Diabetes.2021; 13(12): 1025. CrossRef - Associations Between Glucose Tolerance, Insulin Secretion, Muscle and Fat Mass in Cystic Fibrosis
Bibi Uhre Nielsen, Daniel Faurholt-Jepsen, Peter Sandor Oturai, Tavs Qvist, Rikke Krogh-Madsen, Terese Lea Katzenstein, James Shaw, Christian Ritz, Tacjana Pressler, Thomas Peter Almdal, Inger Hee Mabuza Mathiesen
Clinical Medicine Insights: Endocrinology and Diabetes.2021; 14: 117955142110382. CrossRef - Total and regional fat‐to‐muscle mass ratio measured by bioelectrical impedance and risk of incident type 2 diabetes
Ningjian Wang, Ying Sun, Haojie Zhang, Chi Chen, Yuying Wang, Jihui Zhang, Fangzhen Xia, Christian Benedict, Xiao Tan, Yingli Lu
Journal of Cachexia, Sarcopenia and Muscle.2021; 12(6): 2154. CrossRef - How was the Diabetes Metabolism Journal added to MEDLINE?
Hye Jin Yoo
Science Editing.2020; 7(2): 201. CrossRef - An update on nutrient modulation in the management of disease-induced muscle wasting: evidence from human studies
Matthew S. Brook, Daniel J. Wilkinson, Philip J. Atherton
Current Opinion in Clinical Nutrition & Metabolic Care.2020; 23(3): 174. CrossRef - The functional nutritional and regulatory activities of calcium supplementation from eggshell for obesity disorders management
Marwa El‐Zeftawy, Samar Abd‐El Mohsen Ali, Sally Salah, Hani S. Hafez
Journal of Food Biochemistry.2020;[Epub] CrossRef - Dose‐response associations between serum creatinine and type 2 diabetes mellitus risk: A Chinese cohort study and meta‐analysis of cohort studies
Pei Qin, Yanmei Lou, Liming Cao, Jing Shi, Gang Tian, Dechen Liu, Qionggui Zhou, Chunmei Guo, Quanman Li, Yang Zhao, Feiyan Liu, Xiaoyan Wu, Ranran Qie, Minghui Han, Shengbing Huang, Ping Zhao, Changyi Wang, Jianping Ma, Xiaolin Peng, Shan Xu, Hongen Chen
Journal of Diabetes.2020; 12(8): 594. CrossRef - Caloric restriction in heart failure: A systematic review
Vittorio Emanuele Bianchi
Clinical Nutrition ESPEN.2020; 38: 50. CrossRef - Association between the Thigh Muscle and Insulin Resistance According to Body Mass Index in Middle-Aged Korean Adults
Ji Eun Heo, Jee-Seon Shim, Hokyou Lee, Hyeon Chang Kim
Diabetes & Metabolism Journal.2020; 44(3): 446. CrossRef - Joint impact of muscle mass and waist circumference on type 2 diabetes in Japanese middle‐aged adults: The Circulatory Risk in Communities Study (CIRCS)
Mikako Yasuoka, Isao Muraki, Hironori Imano, Hiroshige Jinnouchi, Yasuhiko Kubota, Mina Hayama‐Terada, Mitsumasa Umesawa, Kazumasa Yamagishi, Tetsuya Ohira, Akihiko Kitamura, Takeo Okada, Masahiko Kiyama, Hiroyasu Iso
Journal of Diabetes.2020; 12(9): 677. CrossRef - Catch-Up Growth in Children Born Small for Gestational Age Related to Body Composition and Metabolic Risk at Six Years of Age in the UK
M. Loredana Marcovecchio, Samantha Gorman, Laura P.E. Watson, David B. Dunger, Kathryn Beardsall
Hormone Research in Paediatrics.2020; 93(2): 119. CrossRef - Response: Association of Thigh Muscle Mass with Insulin Resistance and Incident Type 2 Diabetes Mellitus in Japanese Americans (Diabetes Metab J 2018;42:488–95)
Seung Jin Han, Edward J. Boyko
Diabetes & Metabolism Journal.2019; 43(1): 125. CrossRef - Berberine chloride ameliorated PI3K/Akt‐p/SIRT‐1/PTEN signaling pathway in insulin resistance syndrome induced in rats
Marwa El‐Zeftawy, Doaa Ghareeb, Eman R. ElBealy, Rasha Saad, Salma Mahmoud, Nihal Elguindy, Attalla F. El‐kott, Mohamed El‐Sayed
Journal of Food Biochemistry.2019;[Epub] CrossRef - Letter: Association of Thigh Muscle Mass with Insulin Resistance and Incident Type 2 Diabetes Mellitus in Japanese Americans (Diabetes Metab J 2018;42:488–95)
Nan Hee Cho, Hye Soon Kim
Diabetes & Metabolism Journal.2019; 43(1): 123. CrossRef - Asian Indians With Prediabetes Have Similar Skeletal Muscle Mass and Function to Those With Type 2 Diabetes
Sucharita Sambashivaiah, Stephen D. R. Harridge, Nidhi Sharma, Sumithra Selvam, Priyanka Rohatgi, Anura V. Kurpad
Frontiers in Nutrition.2019;[Epub] CrossRef
- Shape phenotype of thigh fat and muscle and risk of major adverse cardiovascular events after fragility hip fracture
- Obesity and Metabolic Syndrome
- Associations between Body Mass Index and Chronic Kidney Disease in Type 2 Diabetes Mellitus Patients: Findings from the Northeast of Thailand
- Sojib Bin Zaman, Naznin Hossain, Muntasirur Rahman
- Diabetes Metab J. 2018;42(4):330-337. Published online August 21, 2018
- DOI: https://doi.org/10.4093/dmj.2017.0052
- 3,825 View
- 55 Download
- 11 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Chronic kidney disease (CKD) has emerged as a public health burden globally. Obesity and long-term hyperglycaemia can initiate the renal vascular complications in patients with type 2 diabetes mellitus (T2DM). This study aimed to investigate the association of body mass index (BMI) with the CKD in patients with T2DM.
Methods This study has used retrospective medical records, biochemical reports, and anthropometric measurements of 3,580 T2DM patients which were collected between January to December 2015 from a district hospital in Thailand. CKD was defined according to the measurement of estimated glomerular filtration rate (<60 mL/min/1.73 m2). Multiple logistic regression analysis was used to explore the association between BMI and CKD in patients with T2DM.
Results The mean age of the participants was 60.86±9.67 years, 53.68% had poor glycaemic control, and 45.21% were overweight. About one-in-four (23.26%) T2DM patients had CKD. The mean BMI of non-CKD group was slightly higher (25.30 kg/m2 vs. 24.30 kg/m2) when compared with CKD patients. Multivariable analysis showed that older age, female sex, hypertension, and microalbuminuria were associated with the presence of CKD. No association was observed between CKD and poorly controlled glycosylated hemoglobin or hypercholesterolemia. Adjusted analysis further showed overweight and obesity were negatively associated with CKD (adjusted odds ratio [AOR], 0.73; 95% confidence interval [CI], 0.58 to 0.93) and (AOR, 0.53; 95% CI, 0.35 to 0.81), respectively.
Conclusion The negative association of BMI with CKD could reflect the reverse causality. Lower BMI might not lead a diabetic patient to develop CKD, but there are possibilities that CKD leads the patient to experience reduced BMI.
-
Citations
Citations to this article as recorded by- Prevalence and predictors of chronic kidney disease among type 2 diabetic patients worldwide, systematic review and meta-analysis
Eneyew Talie Fenta, Habitu Birhan Eshetu, Natnael Kebede, Eyob Ketema Bogale, Amare Zewdie, Tadele Derbew Kassie, Tadele Fentabil Anagaw, Elyas Melaku Mazengia, Sintayehu Shiferaw Gelaw
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Profile of Obesity and Comorbidities and their Correlation among Hemodialysis Patients, Elbasan
Brunilda Elezi, Skender Topi, Erjona Abazaj
Open Access Macedonian Journal of Medical Sciences.2022; 10(E): 225. CrossRef - Association of eNOS and MCP-1 Genetic Variants with Type 2 Diabetes and Diabetic Nephropathy Susceptibility: A Case–Control and Meta-Analysis Study
Priyanka Raina, Ruhi Sikka, Himanshu Gupta, Kawaljit Matharoo, Surinder Kumar Bali, Virinder Singh, AJS Bhanwer
Biochemical Genetics.2021; 59(4): 966. CrossRef - New Pandemic: Obesity and Associated Nephropathy
Isha Sharma, Yingjun Liao, Xiaoping Zheng, Yashpal S. Kanwar
Frontiers in Medicine.2021;[Epub] CrossRef - Associations between obesity, weight change and decreased renal function in Korean type 2 diabetic patients: a longitudinal follow-up study
Bo-Yeon Kim, Dug-Hyun Choi, Chan-Hee Jung, Ji-Oh Mok, Chul-Hee Kim
BMC Endocrine Disorders.2021;[Epub] CrossRef - The burden of chronic kidney disease among people with diabetes by insurance schemes: Findings from a primary referral hospital in Thailand
Sojib Bin Zaman, Rajat Das Gupta, Putthikrai Pramual, Raihan Kabir Khan, Chinakorn Sujimongkol, Naznin Hossain, Mohammad Rifat Haider, Md. Nazmul Karim, Gulam Muhammed Kibria, Sheikh Mohammdad Shariful Islam
Diabetes Epidemiology and Management.2021; 4: 100026. CrossRef - Association between body mass index and estimated glomerular filtration rate in patients with chronic kidney disease of unknown aetiology in Sri Lanka
M. R. D. L. Kulathunga, M. A. A. Wijayawardena, Ravi Naidu, S. J. Wimalawansa, A. W. Wijeratne
Environmental Geochemistry and Health.2020; 42(9): 2645. CrossRef - The prevalence of diabetic chronic kidney disease in adult Greek subjects with type 2 diabetes mellitus: A series from hospital-based diabetes clinics
Ilias N. Migdalis, Nikolaos Papanas, Athanasios E. Raptis, Ioannis M. Ioannidis, Alexios E. Sotiropoulos, George D. Dimitriadis
Diabetes Research and Clinical Practice.2020; 166: 108243. CrossRef - Underweight Increases the Risk of End-Stage Renal Diseases for Type 2 Diabetes in Korean Population: Data From the National Health Insurance Service Health Checkups 2009–2017
Yang-Hyun Kim, Jun Goo Kang, Seong Jin Lee, Kyung-do Han, Sung-Hee Ihm, Kyung-Hwan Cho, Yong-Gyu Park
Diabetes Care.2020; 43(5): 1118. CrossRef - Prevalence and risk factors of chronic kidney disease among Palestinian type 2 diabetic patients: a cross-sectional study
Zaher Nazzal, Zakaria Hamdan, Dunia Masri, Oday Abu-Kaf, Mohammad Hamad
BMC Nephrology.2020;[Epub] CrossRef - Effects of Variability in Blood Pressure, Glucose, and Cholesterol Concentrations, and Body Mass Index on End-Stage Renal Disease in the General Population of Korea
Mee Kyoung Kim, Kyungdo Han, Hun-Sung Kim, Yong-Moon Park, Hyuk-Sang Kwon, Kun-Ho Yoon, Seung-Hwan Lee
Journal of Clinical Medicine.2019; 8(5): 755. CrossRef
- Prevalence and predictors of chronic kidney disease among type 2 diabetic patients worldwide, systematic review and meta-analysis
- Epidemiology
- The Evidence for an Obesity Paradox in Type 2 Diabetes Mellitus
- Seung Jin Han, Edward J. Boyko
- Diabetes Metab J. 2018;42(3):179-187. Published online May 31, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0055
- 6,332 View
- 122 Download
- 61 Web of Science
- 61 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Although overweight/obesity is a major risk factor for the development of type 2 diabetes mellitus, there is increasing evidence that overweight or obese patients with type 2 diabetes mellitus experience lower mortality compared with patients of normal weight. This paradoxical finding, known as the “obesity paradox,” occurs in other chronic diseases, and in type 2 diabetes mellitus is particularly perplexing given that lifestyle intervention with one goal being weight reduction is an important feature of the management of this condition. We summarize in this review the findings from clinical and epidemiologic studies that have investigated the association between overweight and obesity (usually assessed using body mass index [BMI]) and mortality in type 2 diabetes mellitus and discuss potential causes of the obesity paradox. We conclude that most studies show evidence of an obesity paradox, but important conflicting findings still exist. We also evaluate if potential bias might explain the obesity paradox in diabetes, including, for example, the presence of confounding factors, measurement error due to use of BMI as an index of obesity, and reverse causation.
-
Citations
Citations to this article as recorded by- Association between the weight-adjusted waist index and the odds of type 2 diabetes mellitus in United States adults: a cross-sectional study
Dongdong Zheng, Suzhen Zhao, Dan Luo, Feng Lu, Zhishen Ruan, Xiaokang Dong, Wenjing Chen
Frontiers in Endocrinology.2024;[Epub] CrossRef - Racial and Ethnic Disparities in Primary Prevention of Cardiovascular Disease
Mohammad R. Ali, Hadjer Nacer, Claire A. Lawson, Kamlesh Khunti
Canadian Journal of Cardiology.2024;[Epub] CrossRef - Independent and interactive associations of heart rate and obesity with type 2 diabetes mellites: A population‐based study
Tianxin Zhu, Qingyu Chen, Hongxing Chen, Lili You, Dan Liu, Xiaoyun Zhang, Feng Li, Hongshi Wu, Juying Tang, Diaozhu Lin, Kan Sun, Li Yan, Meng Ren
Journal of Diabetes.2024;[Epub] CrossRef - Two‐sided roles of adipose tissue: Rethinking the obesity paradox in various human diseases from a new perspective
Jing Pan, Jianqiong Yin, Lu Gan, Jianxin Xue
Obesity Reviews.2023;[Epub] CrossRef - Lean or diabetic subtypes predict increased all-cause and disease-specific mortality in metabolic-associated fatty liver disease
Goh Eun Chung, Su Jong Yu, Jeong-Ju Yoo, Yuri Cho, Kyu-na Lee, Dong Wook Shin, Donghee Kim, Yoon Jun Kim, Jung-Hwan Yoon, Kyungdo Han, Eun Ju Cho
BMC Medicine.2023;[Epub] CrossRef - Dynamic changes in prevalence of type 2 diabetes along with associated factors in Bangladesh: Evidence from two national cross-sectional surveys (BDHS 2011 and BDHS 2017–18)
Sabiha Shirin Sara, Ashis Talukder, Ka Yiu Lee, Nayan Basak, Shaharior Rahman Razu, Iqramul Haq, Chuton Deb Nath
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(2): 102706. CrossRef - Association of dietary intake with body mass index and glycemic profile among newly diagnosed patients with type 2 diabetes mellitus
Keddagoda Gamage Piyumi Wasana, Anoja Priyadarshani Attanayake, Thilak Priyantha Weerarathna, Devpura Arachchige Bandumalee Nimalshanthi Amarasekera, Kamani Ayoma Perera Wijewardana Jayatilaka
American Journal of Human Biology.2023;[Epub] CrossRef - Can lipophilic pollutants in adipose tissue explain weight change‐related risk in type 2 diabetes mellitus?
Duk‐Hee Lee, In‐Kyu Lee
Journal of Diabetes Investigation.2023; 14(4): 528. CrossRef - Visceral fat and attribute-based medicine in chronic kidney disease
Hiroshi Kataoka, Kosaku Nitta, Junichi Hoshino
Frontiers in Endocrinology.2023;[Epub] CrossRef - A primary care delivered, technology supported lifestyle program for Type 2 Diabetes Management: An evaluation of changes in metabolic health, feasibility, and acceptability – A pilot interventional study protocol
Pennie J. Taylor, Campbell H. Thompson, Thomas P. Wycherley, Grant D. Brinkworth
Contemporary Clinical Trials Communications.2023; 33: 101152. CrossRef - The medical model of “obesity” and the values behind the guise of health
Kayla R. Mehl
Synthese.2023;[Epub] CrossRef - Elevated MMP-8 levels, inversely associated with BMI, predict mortality in mechanically ventilated patients: an observational multicenter study
Hang Ruan, Shu-sheng Li, Qin Zhang, Xiao Ran
Critical Care.2023;[Epub] CrossRef - Obesity and 30-day case fatality after hyperglycemic crisis hospitalizations in Korea: a national cohort study
Hojun Yoon, Hyun Ho Choi, Giwoong Choi, Sun Ok Song, Kyoung Hwa Ha, Dae Jung Kim
Cardiovascular Prevention and Pharmacotherapy.2023; 5(3): 74. CrossRef - Normal‐weight central obesity and risk of cardiovascular and microvascular events in adults with prediabetes or diabetes: Chinese and British cohorts
Pingting Zhong, Shaoying Tan, Zhuoting Zhu, Ziyu Zhu, Yi Liang, Wenyong Huang, Wei Wang
Diabetes/Metabolism Research and Reviews.2023;[Epub] CrossRef - Overweight and obesity are associated with better survival in STEMI patients with diabetes
Hamza Chaudhry, Ramez Bodair, Ziyad Mahfoud, Soha Dargham, Jassim Al Suwaidi, Hani Jneid, Charbel Abi Khalil
Obesity.2023; 31(11): 2834. CrossRef - Influence of diabetes and obesity on ten-year outcomes after coronary artery bypass grafting in the arterial revascularisation trial
Maria Stefil, Mario Gaudino, Umberto Benedetto, Stephen Gerry, Alastair Gray, Belinda Lees, Bruno Podesser, Lukasz Krzych, Lokeswara Rao Sajja, David Taggart, Marcus Flather
Clinical Research in Cardiology.2023;[Epub] CrossRef - Poor glycaemic control: prevalence, factors and implications for the care of patients with type 2 diabetes in Kinshasa, Democratic Republic of the Congo: a cross-sectional study
Jean-Pierre Fina Lubaki, Olufemi Babatunde Omole, Joel Msafiri Francis
Frontiers in Clinical Diabetes and Healthcare.2023;[Epub] CrossRef - Comparison of obesity indices and triglyceride glucose-related parameters to predict type 2 diabetes mellitus among normal-weight elderly in China
Pan Ke, Xia Wu, Minzhi Xu, Jie Feng, Hongbin Xu, Yong Gan, Chao Wang, Zhenyu Deng, Xiang Liu, Wenning Fu, Qingfeng Tian, Yan He, Lirong Zhong, Heng Jiang, Zuxun Lu
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity.2022; 27(3): 1181. CrossRef - Association Between Obesity and Cardiovascular Disease in Elderly Patients With Diabetes: A Retrospective Cohort Study
Sangmo Hong, Jung Hwan Park, Kyungdo Han, Chang Beom Lee, Dong Sun Kim, Sung Hoon Yu
The Journal of Clinical Endocrinology & Metabolism.2022; 107(2): e515. CrossRef - The Relationship between the Lipid Accumulation Product and Beta-cell Function in Korean Adults with or without Type 2 Diabetes Mellitus: The 2015 Korea National Health and Nutrition Examination Survey
Hye Eun Cho, Seung Bum Yang, Mi Young Gi, Ju Ae Cha, so Young Park, Hyun Yoon
Endocrine Research.2022; 47(2): 80. CrossRef - Body mass index and all-cause mortality in patients with newly diagnosed type 2 diabetes mellitus in South Korea: a retrospective cohort study
Jae-Seok Hong, Hee-Chung Kang
BMJ Open.2022; 12(4): e048784. CrossRef - Social determinants of obesity in American Indian and Alaska Native peoples aged ≥ 50 years
R Turner Goins, Cheryl Conway, Margaret Reid, Luohua Jiang, Jenny Chang, Kimberly R Huyser, Angela G Brega, John F Steiner, Amber L Fyfe-Johnson, Michelle Johnson-Jennings, Vanessa Hiratsuka, Spero M Manson, Joan O’Connell
Public Health Nutrition.2022; 25(8): 2064. CrossRef - Cardiorespiratory Fitness, BMI, Mortality, and Cardiovascular Disease in Adults with Overweight/Obesity and Type 2 Diabetes
ANDREW C. WILLS, ELSA VAZQUEZ ARREOLA, MUIDEEN T. OLAIYA, JEFFREY M. CURTIS, MARGARETA I. HELLGREN, ROBERT L. HANSON, WILLIAM C. KNOWLER
Medicine & Science in Sports & Exercise.2022; 54(6): 994. CrossRef - Spline Longitudinal Multi-response Model for the Detection of Lifestyle-
Based Changes in Blood Glucose of Diabetic Patients
Anna Islamiyati
Current Diabetes Reviews.2022;[Epub] CrossRef - The obesity paradox: Retinopathy, obesity, and circulating risk markers in youth with type 2 diabetes in the TODAY Study
Lynne L. Levitsky, Kimberly L. Drews, Morey Haymond, Rose A. Glubitosi-Klug, Lorraine E. Levitt Katz, Mihai Mititelu, William Tamborlane, Jeanie B. Tryggestad, Ruth S. Weinstock
Journal of Diabetes and its Complications.2022; 36(11): 108259. CrossRef - Distribution of lean mass and mortality risk in patients with type 2 diabetes
Li Ding, Yuxin Fan, Jingting Qiao, Jing He, Ruodan Wang, Qing He, Jingqiu Cui, Zhongshu Ma, Fangqiu Zheng, Hua Gao, Chenlin Dai, Hongyan Wei, Jun Li, Yuming Cao, Gang Hu, Ming Liu
Primary Care Diabetes.2022; 16(6): 824. CrossRef - Current Knowledge on the Pathophysiology of Lean/Normal-Weight Type 2 Diabetes
Teresa Salvatore, Raffaele Galiero, Alfredo Caturano, Luca Rinaldi, Livio Criscuolo, Anna Di Martino, Gaetana Albanese, Erica Vetrano, Christian Catalini, Celestino Sardu, Giovanni Docimo, Raffaele Marfella, Ferdinando Carlo Sasso
International Journal of Molecular Sciences.2022; 24(1): 658. CrossRef - The obesity paradox and diabetes
Giovanni Gravina, Federica Ferrari, Grazia Nebbiai
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity.2021; 26(4): 1057. CrossRef - Implicating the effect of ketogenic diet as a preventive measure to obesity and diabetes mellitus
Sachin Kumar, Tapan Behl, Monika Sachdeva, Aayush Sehgal, Shilpa Kumari, Arun Kumar, Gagandeep Kaur, Harlokesh Narayan Yadav, Simona Bungau
Life Sciences.2021; 264: 118661. CrossRef - Diagnosis of obesity based on body composition‐associated health risks—Time for a change in paradigm
Anja Bosy‐Westphal, Manfred J. Müller
Obesity Reviews.2021;[Epub] CrossRef - Body mass index and clinical outcomes in patients with intracerebral haemorrhage: results from the China Stroke Center Alliance
Zhentang Cao, Xinmin Liu, Zixiao Li, Hongqiu Gu, Yingyu Jiang, Xingquan Zhao, Yongjun Wang
Stroke and Vascular Neurology.2021; 6(3): 424. CrossRef - Obesity and Overweight Are Associated with Minimal Extrathyroidal Extension, Multifocality and Bilaterality of Papillary Thyroid Cancer
Krzysztof Kaliszewski, Dorota Diakowska, Marta Rzeszutko, Jerzy Rudnicki
Journal of Clinical Medicine.2021; 10(5): 970. CrossRef - Obesity paradox in patients with cardiovascular diseases and diabetes mellitus type 2 (analytical review)
Margarita P. Zaikina, Valentina A. Kapustina, Stanislav I. Savel'ev
HEALTH CARE OF THE RUSSIAN FEDERATION.2021; 65(2): 135. CrossRef - Risk factors for adverse outcomes among 35 879 veterans with and without diabetes after diagnosis with COVID-19
Pandora L Wander, Elliott Lowy, Lauren A Beste, Luis Tulloch-Palomino, Anna Korpak, Alexander C Peterson, Bessie A Young, Edward J Boyko
BMJ Open Diabetes Research & Care.2021; 9(1): e002252. CrossRef - Obesity and glycemic control among people with type 2 diabetes in the United States: A retrospective cohort study using insurance claims data
Kristina S. Boye, Maureen J. Lage, Vivian Thieu, Shraddha Shinde, Shivanie Dhamija, Jay Patrick Bae
Journal of Diabetes and its Complications.2021; 35(9): 107975. CrossRef - Differential effects of body mass index on domain-specific cognitive outcomes after stroke
Minwoo Lee, Mi Sun Oh, San Jung, Ju-Hun Lee, Chul-Ho Kim, Min Uk Jang, Young Eun Kim, Hee-Joon Bae, Jaeseol Park, Yeonwook Kang, Byung-Chul Lee, Jae-Sung Lim, Kyung-Ho Yu
Scientific Reports.2021;[Epub] CrossRef - Associations between traditional and non-traditional anthropometric indices and cardiometabolic risk factors among inpatients with type 2 diabetes mellitus: a cross-sectional study
Sahar Golabi, Sajad Ajloo, Fatemeh Maghsoudi, Maryam Adelipour, Mahshid Naghashpour
Journal of International Medical Research.2021; 49(10): 030006052110499. CrossRef - Impact of preexisting type 2 diabetes mellitus and antidiabetic drugs on all-cause and cause-specific mortality among Medicaid-insured women diagnosed with breast cancer
Wayne R. Lawrence, Akiko S. Hosler, Margaret Gates Kuliszewski, Matthew C. Leinung, Xiuling Zhang, Maria J. Schymura, Francis P. Boscoe
Cancer Epidemiology.2020; 66: 101710. CrossRef - Serum Adiponectin and Progranulin Level in Patients with Benign Thyroid Nodule or Papillary Thyroid Cancer
Hyemi Kwon, Se Eun Park, Ji-Sup Yun, Cheol-Young Park
Endocrinology and Metabolism.2020; 35(2): 396. CrossRef - Obesity, sleep apnea, and cancer
Isaac Almendros, Miguel A. Martinez-Garcia, Ramon Farré, David Gozal
International Journal of Obesity.2020; 44(8): 1653. CrossRef - Association of Body Mass Index With Clinical Outcomes in Patients With Atrial Fibrillation: A Report From the FANTASIIA Registry
Vicente Bertomeu‐Gonzalez, José Moreno‐Arribas, María Asunción Esteve‐Pastor, Inmaculada Roldán‐Rabadán, Javier Muñiz, Paula Raña‐Míguez, Martín Ruiz‐Ortiz, Ángel Cequier, Vicente Bertomeu‐Martínez, Lina Badimón, Manuel Anguita, Gregory Y. H. Lip, Francis
Journal of the American Heart Association.2020;[Epub] CrossRef - Risk of type 2 diabetes according to the cumulative exposure to metabolic syndrome or obesity: A nationwide population‐based study
You‐Bin Lee, Da Hye Kim, Seon Mee Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Yong Gyu Park, Kyungdo Han, Hye Jin Yoo
Journal of Diabetes Investigation.2020; 11(6): 1583. CrossRef - Gut microbiota of obese and diabetic Thai subjects and interplay with dietary habits and blood profiles
Lucsame Gruneck, Niwed Kullawong, Kongkiat Kespechara, Siam Popluechai
PeerJ.2020; 8: e9622. CrossRef Multistate Models to Predict Development of Late Complications of Type 2 Diabetes in an Open Cohort Study
Roqayeh Aliyari, Ebrahim Hajizadeh, Ashraf Aminorroaya, Farshad Sharifi, Iraj Kazemi, Ahmad-Reza Baghestani
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 1863. CrossRef- Early weaning induces short‐ and long‐term effects on pancreatic islets in Wistar rats of both sexes
Carla Bruna Pietrobon, Rosiane Aparecida Miranda, Iala Milene Bertasso, Paulo Cezar de Freitas Mathias, Maria Lúcia Bonfleur, Sandra Lucinei Balbo, Marise Auxiliadora de Barros Reis, Márcia Queiroz Latorraca, Vanessa Cristina Arantes, Elaine de Oliveira,
The Journal of Physiology.2020; 598(3): 489. CrossRef - A negative impact of recent weight loss on in-hospital mortality is not modified by overweight and obesity
Rocco Barazzoni, Isabella Sulz, Karin Schindler, Stephan C. Bischoff, Gianluca Gortan Cappellari, Michael Hiesmayr
Clinical Nutrition.2020; 39(8): 2510. CrossRef - Body mass index and mortality among middle-aged Japanese individuals with diagnosed diabetes: The Japan Public Health Center-based prospective study (JPHC study)
Chiho Yamazaki, Atsushi Goto, Motoki Iwasaki, Norie Sawada, Shino Oba, Mitsuhiko Noda, Hiroyasu Iso, Hiroshi Koyama, Shoichiro Tsugane
Diabetes Research and Clinical Practice.2020; 164: 108198. CrossRef Is the Obesity Paradox in Type 2 Diabetes Due to Artefacts of Biases? An Analysis of Pooled Cohort Data from the Heinz Nixdorf Recall Study and the Study of Health in Pomerania
Bernd Kowall, Andreas Stang, Raimund Erbel, Susanne Moebus, Astrid Petersmann, Antje Steveling, Karl-Heinz Jöckel, Henry Völzke
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 1989. CrossRef- Associations between BMI, waist circumference, central obesity and outcomes in type II diabetes mellitus: The ACCORD Trial
Charles A. German, Brian Laughey, Alain G. Bertoni, Joseph Yeboah
Journal of Diabetes and its Complications.2020; 34(3): 107499. CrossRef - Trends in mechanical ventilation use and mortality over time in patients receiving mechanical ventilation in Spain from 2001 to 2015.
Javier de-Miguel-Díez, Rodrigo Jiménez-García, Valentín Hernández-Barrera, Jose J Zamorano-Leon, Rosa Villanueva-Orbaiz, Romana Albaladejo-Vicente, Ana López-de-Andrés
European Journal of Internal Medicine.2020; 74: 67. CrossRef - Type 2 diabetes mellitus: pathogenesis and genetic diagnosis
D. Himanshu, Wahid Ali, Mohd Wamique
Journal of Diabetes & Metabolic Disorders.2020; 19(2): 1959. CrossRef - Prevalence and factors associated with overweight and obesity among patients with type 2 diabetes mellitus in Uganda—a descriptive retrospective study
Salome Tino, Billy N Mayanja, Michael Charles Mubiru, Emmanuel Eling, Edward Ddumba, Pontiano Kaleebu, Moffat Nyirenda
BMJ Open.2020; 10(11): e039258. CrossRef - Nutrition Therapy in Critically Ill Overweight Elderly Patient with Heart Failure, Myocardial Infarction, Pneumonia, and Chronic Kidney Disease
Christina RUSLI, Agussalim BUKHARI, Nurpudji A. TASLIM, Suryani AS’AD, Haerani RASYID
Journal of Nutritional Science and Vitaminology.2020; 66(Supplement): S25. CrossRef - Obesity and childhood asthma
Jason E. Lang
Current Opinion in Pulmonary Medicine.2019; 25(1): 34. CrossRef - Why primary obesity is a disease?
Antonino De Lorenzo, Santo Gratteri, Paola Gualtieri, Andrea Cammarano, Pierfrancesco Bertucci, Laura Di Renzo
Journal of Translational Medicine.2019;[Epub] CrossRef - Impaired compensatory hyperinsulinemia among nonobese type 2 diabetes patients: a cross-sectional study
Jit Sarkar, Sujay Krishna Maity, Abhishek Sen, Titli Nargis, Dipika Ray, Partha Chakrabarti
Therapeutic Advances in Endocrinology and Metabolism.2019; 10: 204201881988902. CrossRef - Sedentary behaviour is associated with diabetes mellitus in adults: findings of a cross-sectional analysis from the Brazilian National Health System
Ítalo Ribeiro Lemes, Xuemei Sui, Bruna Camilo Turi-Lynch, Duck-chul Lee, Steven N Blair, Rômulo Araújo Fernandes, Jamile Sanches Codogno, Henrique Luiz Monteiro
Journal of Public Health.2019; 41(4): 742. CrossRef - Obesity Paradox in Chronic Liver Diseases: Product of Bias or a Real Thing?
Ines Bilic Curcic, Maja Cigrovski Berkovic, Lucija Kuna, Hrvoje Roguljic, Robert Smolic, Silvija Canecki Varzic, Lucija Virovic Jukic, Martina Smolic
Journal of Clinical and Translational Hepatology.2019; 7(3): 1. CrossRef - From the Obesity Tsunami to the Diabetes Avalanche: Primordial Prevention of the Diabesity-Related Cardiovascular Epidemic by Diabeto-Cardiologists
Mustafa Karakurt, Burak Acar, Ozcan Ozeke, Mustafa Bilal Ozbay, Yasin Ozen, Sefa Unal, Mustafa Karanfil, Cagri Yayla, Serkan Cay, Orhan Maden, Dursun Aras, Serkan Topaloglu, Sinan Aydogdu, Zehra Golbasi
Angiology.2019; 70(4): 371. CrossRef - Increased Plasma Dipeptidyl Peptidase-4 (DPP4) Activity Is an Obesity-Independent Parameter for Glycemic Deregulation in Type 2 Diabetes Patients
Jit Sarkar, Titli Nargis, Om Tantia, Sujoy Ghosh, Partha Chakrabarti
Frontiers in Endocrinology.2019;[Epub] CrossRef - INVESTIGATING INDIVIDUAL FACTORS RELATED TO READMISSION OF PATIENTS WITH TYPE 2 DIABETES- A CROSS-SECTIONAL STUDY
Valiallah Dashtpour, Mehran Hesaraki, Mahnaz Abavisani, Mahdieh Sari, Sudabeh Ahmadidarrehsima
Journal of Evolution of Medical and Dental Sciences.2018; 7(53): 5604. CrossRef
- Association between the weight-adjusted waist index and the odds of type 2 diabetes mellitus in United States adults: a cross-sectional study
- Obesity and Metabolic Syndrome
- Association between Blood Mercury Level and Visceral Adiposity in Adults
- Jong Suk Park, Kyoung Hwa Ha, Ka He, Dae Jung Kim
- Diabetes Metab J. 2017;41(2):113-120. Published online December 21, 2016
- DOI: https://doi.org/10.4093/dmj.2017.41.2.113
- 4,839 View
- 45 Download
- 38 Web of Science
- 39 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Few studies have examined the association between mercury exposure and obesity. The aim of this study is to investigate the association between blood mercury concentrations and indices of obesity in adults.
Methods A total of 200 healthy subjects, aged 30 to 64 years, who had no history of cardiovascular or malignant disease, were examined. Anthropometric and various biochemical profiles were measured. Visceral adipose tissue (VAT) was measured using dual-energy X-ray absorptiometry (DXA).
Results All subjects were divided into three groups according to blood mercury concentrations. Compared with the subjects in the lowest tertile of mercury, those in the highest tertile were more likely to be male; were current alcohol drinkers and smokers; had a higher body mass index (BMI), waist circumference (WC), and VAT; had higher levels of blood pressure, fasting glucose, and insulin resistance; and consumed more fish. The blood mercury concentration was significantly associated with anthropometric parameters, showing relationships with BMI, WC, and VAT. After adjusting for multiple risk factors, the odds ratios (ORs) for high mercury concentration was significantly higher in the highest VAT tertile than in the lowest VAT tertile (OR, 2.66; 95% confidence interval, 1.05 to 6.62;
P <0.05).Conclusion The blood mercury concentration was significantly associated with VAT in healthy adults. Further studies are warranted to confirm our findings.
-
Citations
Citations to this article as recorded by- Exposure to Metal Mixtures and Overweight or Obesity Among Chinese Adults
Gaojie Fan, Qing Liu, Mingyang Wu, Jianing Bi, Xiya Qin, Qing Fang, Zhengce Wan, Yongman Lv, Youjie Wang, Lulu Song
Biological Trace Element Research.2023; 201(8): 3697. CrossRef - Methylmercury drives lipid droplet formation and adipokine expression during the late stages of adipocyte differentiation in 3T3-L1 cells
Yasukazu Takanezawa, Yui Kashiwano, Ryosuke Nakamura, Yuka Ohshiro, Shimpei Uraguchi, Masako Kiyono
Toxicology.2023; 486: 153446. CrossRef - Expression Profiling of Adipogenic and Anti-Adipogenic MicroRNA Sequences following Methylmercury Exposure in Caenorhabditis elegans
Giancarlo Garofalo, Tyson Nielsen, Samuel Caito
Toxics.2023; 11(11): 934. CrossRef - Report of the Scientific Committee of the Spanish Agency for Food Safety and Nutrition (AESAN) on the available evidence in relation to the potential obesogenic activity of certain chemical compounds that may be present in foods
Ana María Rivas Velasco, Irene Bretón Lesmes, Araceli Díaz Perales, Ángel Gil Izquierdo, María José González Muñoz, Victoria Moreno Arribas, María del Puy Portillo Baquedano, Silvia Pichardo Sánchez
Food Risk Assess Europe.2023;[Epub] CrossRef - Lead, mercury, and cadmium exposures are associated with obesity but not with diabetes mellitus: Korean National Environmental Health Survey (KoNEHS) 2015–2017
Min Kyong Moon, Inae Lee, Aram Lee, Hyunwoong Park, Min Joo Kim, Sunmi Kim, Yoon Hee Cho, Sooyeon Hong, Jiyoung Yoo, Gi Jeong Cheon, Kyungho Choi, Young Joo Park, Jeongim Park
Environmental Research.2022; 204: 111888. CrossRef - The Effect of Mixture of Heavy Metals on Obesity in Individuals ≥50 Years of Age
Hai Nguyen Duc, Hojin Oh, Min-Sun Kim
Biological Trace Element Research.2022; 200(8): 3554. CrossRef - MicroRNA Expression Influences Methylmercury-Induced Lipid Accumulation and Mitochondrial Toxicity in Caenorhabditis elegans
Tyson Nielsen, Nicole Crawford, Megan Martell, Belal Khalil, Farooq Imtiaz, Jennifer L. Newell-Caito, Samuel Caito
Chemical Research in Toxicology.2022; 35(1): 77. CrossRef - Relationship Between Serum Levels of Arsenic, Cadmium, and Mercury and Body Mass Index and Fasting Plasma Glucose in a Mexican Adult Population
Héctor Hernández-Mendoza, Héctor Edmundo Álvarez-Loredo, Elizabeth Teresita Romero-Guzmán, Darío Gaytán-Hernández, Consuelo Chang-Rueda, Israel Martínez-Navarro, Bertha Irene Juárez-Flores, María Judith Rios-Lugo
Biological Trace Element Research.2022; 200(12): 4916. CrossRef - Heavy metal-induced lipogenic gene aberration, lipid dysregulation and obesogenic effect: a review
Yang Zhou, Frank Peprah Addai, Xinshuang Zhang, Yuelin Liu, Yinfeng Wang, Feng Lin, Alex Tuffour, Jie Gu, Guangxiang Liu, Haifeng Shi
Environmental Chemistry Letters.2022; 20(3): 1611. CrossRef - Differential fat accumulation in early adulthood according to adolescent‐BMI and heavy metal exposure
Larissa Betanzos‐Robledo, Martha M. Téllez‐Rojo, Hector Lamadrid‐Figueroa, Ernesto Roldan‐Valadez, Karen E. Peterson, Erica C. Jansen, Nil Basu, Alejandra Cantoral
New Directions for Child and Adolescent Development.2022; 2022(181-182): 37. CrossRef - The Association of Mercury and ALT with Obesity in Korean Adults: Using Data from the Korea National Health and Nutrition Examination Survey for 11 Years (KNHANES 2005, 2008~2017)
Sang Shin Pyo
Korean Journal of Clinical Laboratory Science.2022; 54(3): 192. CrossRef - Plasma titanium level is positively associated with metabolic syndrome: A survey in China’s heavy metal polluted regions
Miao Huang, Jingyuan Chen, Guangyu Yan, Yiping Yang, Dan Luo, Xiang Chen, Meian He, Hong Yuan, Zhijun Huang, Yao Lu
Ecotoxicology and Environmental Safety.2021; 208: 111435. CrossRef - Relationship Between Elevated Hair Mercury Levels, Essential Element Status, and Metabolic Profile in Overweight and Obese Adults
Anatoly V. Skalny, Jung-Su Chang, Igor P. Bobrovnitsky, Philippe Yu Kopylov, Margarita G. Skalnaya, Shih-Yi Huang, Monica Maria Bastos Paoliello, Ekaterina S. Ivanova, Weu Wang, Alexey A. Tinkov
Biological Trace Element Research.2021; 199(8): 2874. CrossRef - Associations between metabolic syndrome and four heavy metals: A systematic review and meta-analysis
Ping Xu, Aiping Liu, Fengna Li, Alexey A. Tinkov, Longjian Liu, Ji-Chang Zhou
Environmental Pollution.2021; 273: 116480. CrossRef - Cadmium, lead and mercury in the blood of psoriatic and vitiligo patients and their possible associations with dietary habits
Marta Wacewicz-Muczyńska, Katarzyna Socha, Jolanta Soroczyńska, Marek Niczyporuk, Maria H. Borawska
Science of The Total Environment.2021; 757: 143967. CrossRef - Crude oil and public health issues in Niger Delta, Nigeria: Much ado about the inevitable
Orish Ebere Orisakwe
Environmental Research.2021; 194: 110725. CrossRef - Mercury in the human adrenal medulla could contribute to increased plasma noradrenaline in aging
Roger Pamphlett, Stephen Kum Jew, Philip A. Doble, David P. Bishop
Scientific Reports.2021;[Epub] CrossRef - Multiple metal exposure and obesity: A prospective cohort study of adults living along the Yangtze River, China
Qi Zhong, Qi-rong Qin, Wan-jun Yang, Jia-liu He, Jin-liang Zhu, Zhen-yu Zhu, Fen Huang
Environmental Pollution.2021; 285: 117150. CrossRef - Association between Blood Mercury Levels and Non-Alcoholic Fatty Liver Disease in Non-Obese Populations: The Korean National Environmental Health Survey (KoNEHS) 2012–2014
Yun-Jung Yang, Eun-Jung Yang, Kyongjin Park, Subin Oh, Taehyen Kim, Yeon-Pyo Hong
International Journal of Environmental Research and Public Health.2021; 18(12): 6412. CrossRef - Hair Lead, Aluminum, and Other Toxic Metals in Normal-Weight and Obese Patients with Coronary Heart Disease
Anatoly V. Skalny, Philippe Yu Kopylov, Monica M. B. Paoliello, Jung-Su Chang, Michael Aschner, Igor P. Bobrovnitsky, Jane C.-J. Chao, Jan Aaseth, Sergei N. Chebotarev, Alexey A. Tinkov
International Journal of Environmental Research and Public Health.2021; 18(15): 8195. CrossRef - Methylmercury chronic exposure affects the expression of DNA single-strand break repair genes, induces oxidative stress, and chromosomal abnormalities in young dyslipidemic APOE knockout mice
Cássia R. Roque, Letícia R. Sampaio, Mayumi N. Ito, Daniel V. Pinto, Juan S.R. Caminha, Paulo I.G. Nunes, Ramon S. Raposo, Flávia A. Santos, Cláudia C. Windmöller, Maria Elena Crespo-Lopez, Jacqueline I. Alvarez-Leite, Reinaldo B. Oriá, Ronald F. Pinheiro
Toxicology.2021; 464: 152992. CrossRef - Methylmercury-Induced Metabolic Alterations in Caenorhabditis elegans Are Diet-Dependent
Nicole Crawford, Megan Martell, Tyson Nielsen, Belal Khalil, Farooq Imtiaz, Etienne Nguidjo, Jennifer Newell-Caito, Julia Bornhorst, Tanja Schwerdtle, Samuel Caito
Toxics.2021; 9(11): 287. CrossRef - Antioxidant status in relation to heavy metals induced oxidative stress in patients with polycystic ovarian syndrome (PCOS)
Manal Abudawood, Hajera Tabassum, Atheer H. Alanazi, Fatmah Almusallam, Feda Aljaser, Mir Naiman Ali, Naif D. Alenzi, Samyah T. Alanazi, Manal A. Alghamdi, Ghadah H. Altoum, Manar A. Alzeer, Majed O. Alotaibi, Arwa Abudawood, Hazem K. Ghneim, Lulu Abdulla
Scientific Reports.2021;[Epub] CrossRef - Association of Blood Mercury Levels with the Risks of Overweight and High Waist-to-Height Ratio in Children and Adolescents: Data from the Korean National Health and Nutrition Examination Survey
Ky Young Cho
Children.2021; 8(12): 1087. CrossRef - The sex-specific effects of blood lead, mercury, and cadmium levels on hepatic steatosis and fibrosis: Korean nationwide cross-sectional study
Seung Min Chung, Jun Sung Moon, Ji Sung Yoon, Kyu Chang Won, Hyoung Woo Lee
Journal of Trace Elements in Medicine and Biology.2020; 62: 126601. CrossRef - Elevated blood mercury level has a non-linear association with infertility in U.S. women: Data from the NHANES 2013–2016
Fangfang Zhu, Chi Chen, Yingxuan Zhang, Si Chen, Xian Huang, Jingwei Li, Yanxi Wang, Xiaorong Liu, Gaopi Deng, Jie Gao
Reproductive Toxicology.2020; 91: 53. CrossRef - Methylmercury Induces Metabolic Alterations in Caenorhabditis elegans: Role for C/EBP Transcription Factor
Samuel W Caito, Jennifer Newell-Caito, Megan Martell, Nicole Crawford, Michael Aschner
Toxicological Sciences.2020; 174(1): 112. CrossRef - Association of Fish Consumption and Mercury Exposure During Pregnancy With Metabolic Health and Inflammatory Biomarkers in Children
Nikos Stratakis, David V. Conti, Eva Borras, Eduardo Sabido, Theano Roumeliotaki, Eleni Papadopoulou, Lydiane Agier, Xavier Basagana, Mariona Bustamante, Maribel Casas, Shohreh F. Farzan, Serena Fossati, Juan R. Gonzalez, Regina Grazuleviciene, Barbara He
JAMA Network Open.2020; 3(3): e201007. CrossRef - Elemental Analysis of Aging Human Pituitary Glands Implicates Mercury as a Contributor to the Somatopause
Roger Pamphlett, Stephen Kum Jew, Philip A. Doble, David P. Bishop
Frontiers in Endocrinology.2019;[Epub] CrossRef - Mercury leads to features of polycystic ovary syndrome in rats
Eduardo Merlo, Ingridy R.G. Schereider, Maylla R. Simões, Dalton V. Vassallo, Jones B. Graceli
Toxicology Letters.2019; 312: 45. CrossRef - In utero exposure to mercury and childhood overweight or obesity: counteracting effect of maternal folate status
Guoying Wang, Jessica DiBari, Eric Bind, Andrew M. Steffens, Jhindan Mukherjee, Tami R. Bartell, David C. Bellinger, Xiumei Hong, Yuelong Ji, Mei-Cheng Wang, Marsha Wills-Karp, Tina L. Cheng, Xiaobin Wang
BMC Medicine.2019;[Epub] CrossRef - Mercury Is Taken Up Selectively by Cells Involved in Joint, Bone, and Connective Tissue Disorders
Roger Pamphlett, Stephen Kum Jew
Frontiers in Medicine.2019;[Epub] CrossRef - Cohort Profile: The Cardiovascular and Metabolic Diseases Etiology Research Center Cohort in Korea
Jee-Seon Shim, Bo Mi Song, Jung Hyun Lee, Seung Won Lee, Ji Hye Park, Dong Phil Choi, Myung Ha Lee, Kyoung Hwa Ha, Dae Jung Kim, Sungha Park, Won-Woo Lee, Yoosik Youm, Eui-Cheol Shin, Hyeon Chang Kim
Yonsei Medical Journal.2019; 60(8): 804. CrossRef - Chronic mercury at low doses impairs white adipose tissue plasticity
Danize Aparecida Rizzetti, Patricia Corrales, Janaina Trindade Piagette, José Antonio Uranga-Ocio, Gema Medina-Gomez, Franck Maciel Peçanha, Dalton Valentim Vassallo, Marta Miguel, Giulia Alessandra Wiggers
Toxicology.2019; 418: 41. CrossRef - Associations of cumulative exposure to heavy metal mixtures with obesity and its comorbidities among U.S. adults in NHANES 2003–2014
Xin Wang, Bhramar Mukherjee, Sung Kyun Park
Environment International.2018; 121: 683. CrossRef - Blood mercury concentration in relation to metabolic and weight phenotypes using the KNHANES 2011–2013 data
Kayoung Lee
International Archives of Occupational and Environmental Health.2018; 91(2): 185. CrossRef - The association of total blood mercury levels and overweight among Korean adolescents: analysis of the Korean National Health and Nutrition Examination Survey (KNHANES) 2010–2013
Yi-Yeon Shin, In-Kyung Ryu, Mi-Jung Park, Shin-Hye Kim
Korean Journal of Pediatrics.2018; 61(4): 121. CrossRef - Heavy Metal Exposure and Metabolic Syndrome: Evidence from Human and Model System Studies
Antonio Planchart, Adrian Green, Cathrine Hoyo, Carolyn J. Mattingly
Current Environmental Health Reports.2018; 5(1): 110. CrossRef - Association between Blood Mercury Level and Visceral Adiposity in Adults
Seong-Su Moon
Diabetes & Metabolism Journal.2017; 41(2): 96. CrossRef
- Exposure to Metal Mixtures and Overweight or Obesity Among Chinese Adults
- The Relationship between the Level of Fatness and Fitness during Adolescence and the Risk Factors of Metabolic Disorders in Adulthood
- Yoonsuk Jekal, Ji Eun Yun, Sang Wook Park, Sun Ha Jee, Justin Y Jeon
- Korean Diabetes J. 2010;34(2):126-134. Published online April 30, 2010
- DOI: https://doi.org/10.4093/kdj.2010.34.2.126
- 3,170 View
- 27 Download
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The purpose of the current study was to investigate the association between the level of obesity and physical fitness (PF) during adolescence and the risk factors of metabolic disorders during adulthood.
Methods In the current analysis, 3,993 Korean adults (mean age, 38.70 ± 1.69 years) were recruited. The level of body index (BI) and PF were examined during adolescence through high school record, and their health examination data, including systolic blood pressure (SBP), diastolic blood pressure (DBP), fasting glucose (FG), total cholesterol (TC), and current body mass index (BMI) were obtained from National Health Insurance Corporation Data. Gender-specific analyses were administered to compare health exam data across the level of BI, the level of PF, and a mixed level of BI and PF.
Results Most obese males during high school had statistically higher SBP, DBP, FG, and BMI in adulthood, and most obese females had higher BMI, as compared to most lean males or females. Least fit males during high school had statistically higher BMI in adulthood, and least fit females had statistically higher SBP, DBP, FG, TC, and BMI, as compared to most fit males or females. There was a significant relationship between the mixed level of BI and PF and SBP, DBP, TC and current BMI in both genders.
Conclusion Maintaining a healthy level of body weight and PF during adolescence is recommended to prevent the development of metabolic diseases in adulthood.
-
Citations
Citations to this article as recorded by- A cross‐sectional study on the use of big data for the past H1N1 influenza epidemic in obesity after COVID‐19: Focused on the body slimming cream and leptin via DTC gene test
Jinkyung Lee, Ki Han Kwon
Journal of Cosmetic Dermatology.2022; 21(11): 5321. CrossRef - Aerobic fitness in late adolescence and the risk of cancer and cancer-associated mortality in adulthood: A prospective nationwide study of 1.2 million Swedish men
G. Högström, H. Ohlsson, C. Crump, J. Sundquist, K. Sundquist
Cancer Epidemiology.2019; 59: 58. CrossRef - Study Time after School and Habitual Eating Are Associated with Risk for Obesity among Overweight Korean Children: A Prospective Study
Eun Young Lee, Borami Kang, Yeoree Yang, Hae Kyung Yang, Hun-Sung Kim, Sun-Young Lim, Jin-Hee Lee, Seong-Su Lee, Byung-Kyu Suh, Kun-Ho Yoon
Obesity Facts.2018; 11(1): 46. CrossRef - Differences in Dietary Life and Health related Factors According to Obesity in Poor Urban Peruvian Adolescents
Hye-Kyung Chung, Hae-Young Lee, Jin Ri Kim, Eun Woo Nam
Korean Journal of Community Nutrition.2018; 23(4): 302. CrossRef - The influence of aerobic fitness on obesity and its parent-offspring correlations in a cross-sectional study among German families
Ronja Foraita, Mirko Brandes, Frauke Günther, Karin Bammann, Iris Pigeot, Wolfgang Ahrens
BMC Public Health.2015;[Epub] CrossRef - The Effect of Participation in Physical Activity “The Development of Fitness” Class on Physical Fitness and Risk Factors for Metabolic Syndrome of University Students in Korea
김동일, Justin Jeon, 이해동, 박지혜, 홍성현
Korean Journal of Sport Science.2012; 23(3): 478. CrossRef - Epidemiology and prevention of stroke: a worldwide perspective
Elena V Kuklina, Xin Tong, Mary G George, Pooja Bansil
Expert Review of Neurotherapeutics.2012; 12(2): 199. CrossRef - Fitness, Fatness, and Cardiovascular Disease Risk and Outcomes
John M. Jakicic, Anne E. Mishler, Renee Rogers
Current Cardiovascular Risk Reports.2011; 5(2): 113. CrossRef - Epidemiology of Physical Activity Participation and Type 2 Diabetes in Korea
Yoonsuk Jekal, Justin Y Jeon
Journal of Korean Diabetes.2011; 12(1): 13. CrossRef - Relationship Between Trajectories of Trunk Fat Mass Development in Adolescence and Cardiometabolic Risk in Young Adulthood
Lauren B. Sherar, Joe C. Eisenmann, Philip D. Chilibeck, Nazeem Muhajarine, Susanna Martin, Donald A. Bailey, Adam D.G. Baxter‐Jones
Obesity.2011; 19(8): 1699. CrossRef
- A cross‐sectional study on the use of big data for the past H1N1 influenza epidemic in obesity after COVID‐19: Focused on the body slimming cream and leptin via DTC gene test

 KDA
KDA
 First
First Prev
Prev





