
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Cardiovascular Risk/Epidemiology
- Intensified Multifactorial Intervention in Patients with Type 2 Diabetes Mellitus
- Takayoshi Sasako, Toshimasa Yamauchi, Kohjiro Ueki
- Diabetes Metab J. 2023;47(2):185-197. Published online January 12, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0325
- 5,073 View
- 358 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
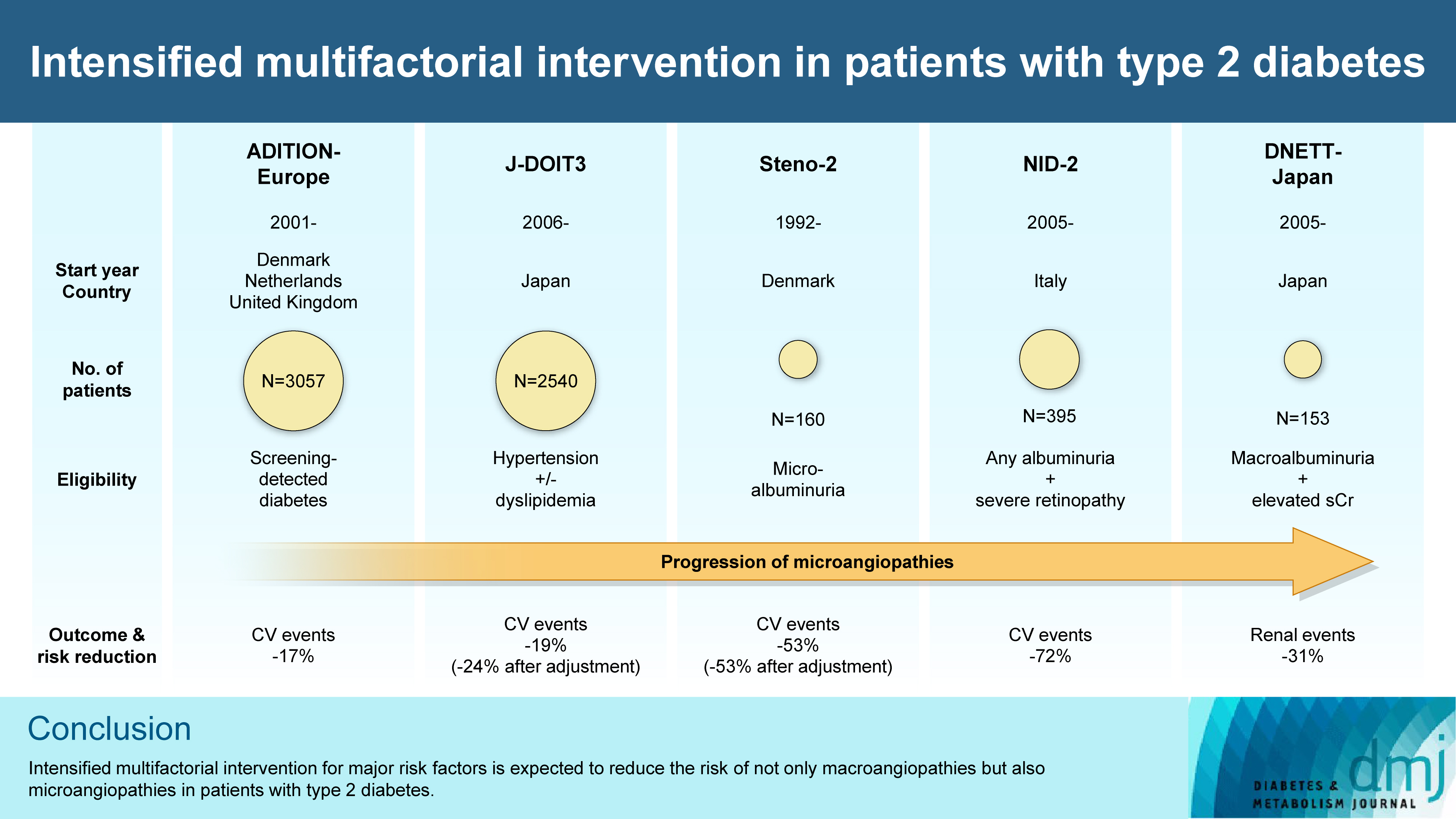
ePub - In the management of diabetes mellitus, one of the most important goals is to prevent its micro- and macrovascular complications, and to that end, multifactorial intervention is widely recommended. Intensified multifactorial intervention with pharmacotherapy for associated risk factors, alongside lifestyle modification, was first shown to be efficacious in patients with microalbuminuria (Steno-2 study), then in those with less advanced microvascular complications (the Anglo-Danish-Dutch Study of Intensive Treatment In People with Screen Detected Diabetes in Primary Care [ADDITION]-Europe and the Japan Diabetes Optimal Treatment study for 3 major risk factors of cardiovascular diseases [J-DOIT3]), and in those with advanced microvascular complications (the Nephropathy In Diabetes-Type 2 [NID-2] study and Diabetic Nephropathy Remission and Regression Team Trial in Japan [DNETT-Japan]). Thus far, multifactorial intervention led to a reduction in cardiovascular and renal events, albeit not necessarily significant. It should be noted that not only baseline characteristics but also the control status of the risk factors and event rates during intervention among the patients widely varied from one trial to the next. Further evidence is needed for the efficacy of multifactorial intervention in a longer duration and in younger or elderly patients. Moreover, now that new classes of antidiabetic drugs are available, it should be addressed whether strict and safe glycemic control, alongside control of other risk factors, could lead to further risk reductions in micro- and macrovascular complications, thereby decreasing all-cause mortality in patients with type 2 diabetes mellitus.
-
Citations
Citations to this article as recorded by- Exploring mechanisms underlying diabetes comorbidities and strategies to prevent vascular complications
Takayoshi Sasako
Diabetology International.2024; 15(1): 34. CrossRef - Targeting ERS-mitophagy in hippocampal neurons to explore the improvement of memory by tea polyphenols in aged type 2 diabetic rats
Wenjuan Feng, Chenhui Lv, Le Cheng, Xin Song, Xuemin Li, Haoran Xie, Shuangzhi Chen, Xi Wang, Lushan Xue, Cheng Zhang, Jie Kou, Lili Wang, Haifeng Zhao
Free Radical Biology and Medicine.2024; 213: 293. CrossRef - Risk of Dementia Among Patients With Diabetes in a Multidisciplinary, Primary Care Management Program
Kailu Wang, Shi Zhao, Eric Kam-Pui Lee, Susan Zi-May Yau, Yushan Wu, Chi-Tim Hung, Eng-Kiong Yeoh
JAMA Network Open.2024; 7(2): e2355733. CrossRef - Causes of In-Hospital Death and Pharmaceutical Associations with Age of Death during a 10-Year Period (2011–2020) in Individuals with and without Diabetes at a Japanese Community General Hospital
Minae Hosoki, Taiki Hori, Yousuke Kaneko, Kensuke Mori, Saya Yasui, Seijiro Tsuji, Hiroki Yamagami, Saki Kawata, Tomoyo Hara, Shiho Masuda, Yukari Mitsui, Kiyoe Kurahashi, Takeshi Harada, Shingen Nakamura, Toshiki Otoda, Tomoyuki Yuasa, Akio Kuroda, Itsur
Journal of Clinical Medicine.2024; 13(5): 1283. CrossRef - External validation of a minimal-resource model to predict reduced estimated glomerular filtration rate in people with type 2 diabetes without diagnosis of chronic kidney disease in Mexico: a comparison between country-level and regional performance
Camilla Sammut-Powell, Rose Sisk, Ruben Silva-Tinoco, Gustavo de la Pena, Paloma Almeda-Valdes, Sonia Citlali Juarez Comboni, Susana Goncalves, Rory Cameron
Frontiers in Endocrinology.2024;[Epub] CrossRef - Gut Microbiota Targeted Approach by Natural Products in Diabetes Management: An Overview
Priyanka Sati, Praveen Dhyani, Eshita Sharma, Dharam Chand Attri, Arvind Jantwal, Rajni Devi, Daniela Calina, Javad Sharifi-Rad
Current Nutrition Reports.2024;[Epub] CrossRef - Cardiovascular Risk Reduction in Type 2 Diabetes: Further Insights into the Power of Weight Loss and Exercise
Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(3): 302. CrossRef - Sarcopenia: Loss of mighty armor against frailty and aging
Takayoshi Sasako, Kohjiro Ueki
Journal of Diabetes Investigation.2023; 14(10): 1145. CrossRef
- Exploring mechanisms underlying diabetes comorbidities and strategies to prevent vascular complications
- Pathophysiology
- Blood Pressure Target in Type 2 Diabetes Mellitus
- Hyun-Jin Kim, Kwang-il Kim, on Behalf of the Policy Committee of Korean Society of Hypertension
- Diabetes Metab J. 2022;46(5):667-674. Published online September 19, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0215

- 6,126 View
- 504 Download
- 5 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The prevalence of diabetes mellitus continues to increase worldwide, and it is a well-established cardiovascular risk factor. Hypertension is also an important cardiovascular risk factor to be controlled and is common among patients with diabetes mellitus. Optimal blood pressure (BP) goals have been the subject of great debate in the management of hypertension among patients with diabetes mellitus. This review provides detailed results from randomized controlled trials and meta-analyses of clinical outcomes according to the target BP in patients with type 2 diabetes mellitus. In addition, the target BP in patients with diabetes mellitus recommended by different guidelines was summarized and presented. A target BP of <140/90 mm Hg is recommended for patients with hypertension and diabetes mellitus, and BP should be controlled to <130/80 mm Hg in patients with diabetes mellitus who have high-risk clinical features. We hope that this review will be helpful to clinicians and patients by promoting the understanding and appropriate application of BP control in the comprehensive management of patients with diabetes mellitus.
-
Citations
Citations to this article as recorded by- Recent evidence on target blood pressure in patients with hypertension
Hack-Lyoung Kim
Cardiovascular Prevention and Pharmacotherapy.2024; 6(1): 17. CrossRef - Using Generative AI to Improve the Performance and Interpretability of Rule-Based Diagnosis of Type 2 Diabetes Mellitus
Leon Kopitar, Iztok Fister, Gregor Stiglic
Information.2024; 15(3): 162. CrossRef - Additive interaction of family medical history of diabetes with hypertension on the diagnosis of diabetes among older adults in India: longitudinal ageing study in India
Waquar Ahmed
BMC Public Health.2024;[Epub] CrossRef - Emerging roles of interferon-stimulated gene-15 in age-related telomere attrition, the DNA damage response, and cardiovascular disease
María González-Amor, Beatriz Dorado, Vicente Andrés
Frontiers in Cell and Developmental Biology.2023;[Epub] CrossRef - Effects of Diabetes and Voluntary Exercise on IgA Concentration and Polymeric Immunoglobulin Receptor Expression in the Submandibular Gland of Rats
Jaebum Park, Yuko Yamamoto, Kouki Hidaka, Satoko Wada-Takahashi, Shun-suke Takahashi, Toshiya Morozumi, Nobuhisa Kubota, Makiko Saita, Juri Saruta, Wakako Sakaguchi, Masahiro To, Tomoko Shimizu, Yuko Mikuni-Takagaki, Keiichi Tsukinoki
Medicina.2023; 59(4): 789. CrossRef - A diabetes update
Zachary Bloomgarden
Journal of Diabetes.2023; 15(7): 542. CrossRef - CARDIOPROTECTIVE AND METABOLIC EFFECTS OF ANTIHYPERTENSIVE THERAPY IN PATIENTS WITH SUCH COMORBIDITIES AS ARTERIAL HYPERTENSION, TYPE 2 DIABETES MELLITUS, AND OBESITY
I. P. Dunaieva, N. O. Kravchun, І. A. Ilchenko
Bulletin of Problems Biology and Medicine.2023; 1(2): 211. CrossRef - Hypertensive Heart Failure
Filippos Triposkiadis, Pantelis Sarafidis, Alexandros Briasoulis, Dimitrios E. Magouliotis, Thanos Athanasiou, John Skoularigis, Andrew Xanthopoulos
Journal of Clinical Medicine.2023; 12(15): 5090. CrossRef - 2023 Clinical Practice Guidelines for Diabetes
Min Kyong Moon
The Journal of Korean Diabetes.2023; 24(3): 120. CrossRef
- Recent evidence on target blood pressure in patients with hypertension
- Cardiovascular Risk/Epidemiology
- Association between Variability of Metabolic Risk Factors and Cardiometabolic Outcomes
- Min Jeong Park, Kyung Mook Choi
- Diabetes Metab J. 2022;46(1):49-62. Published online January 27, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0316
- 5,682 View
- 221 Download
- 5 Web of Science
- 7 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 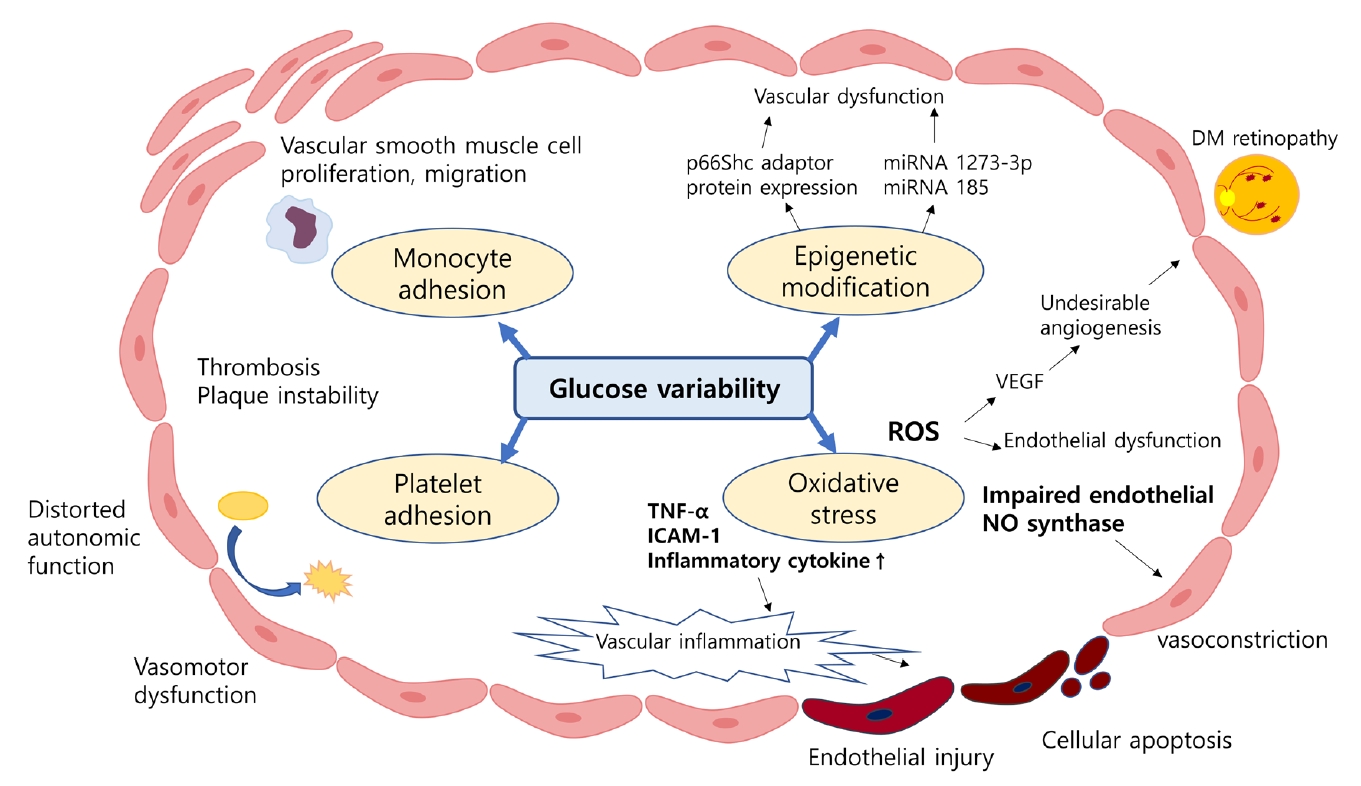
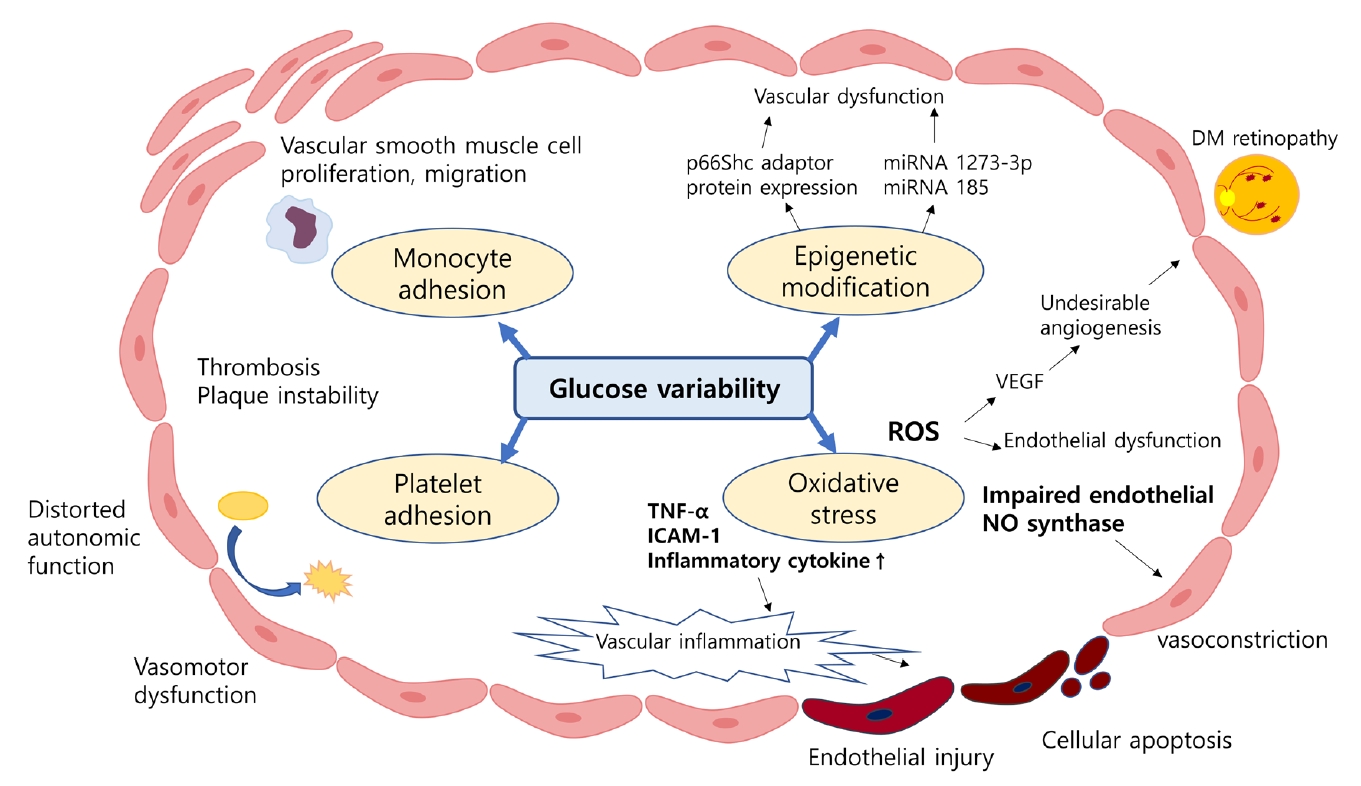
- Despite strenuous efforts to reduce cardiovascular disease (CVD) risk by improving cardiometabolic risk factors, such as glucose and cholesterol levels, and blood pressure, there is still residual risk even in patients reaching treatment targets. Recently, researchers have begun to focus on the variability of metabolic variables to remove residual risks. Several clinical trials and cohort studies have reported a relationship between the variability of metabolic parameters and CVDs. Herein, we review the literature regarding the effect of metabolic factor variability and CVD risk, and describe possible mechanisms and potential treatment perspectives for reducing cardiometabolic risk factor variability.
-
Citations
Citations to this article as recorded by- Long-term variability in physiological measures in relation to mortality and epigenetic aging: prospective studies in the USA and China
Hui Chen, Tianjing Zhou, Shaowei Wu, Yaying Cao, Geng Zong, Changzheng Yuan
BMC Medicine.2023;[Epub] CrossRef - Dose–response relationship between physical activity and cardiometabolic risk in obese children and adolescents: A pre-post quasi-experimental study
Zekai Chen, Lin Zhu
Frontiers in Physiology.2023;[Epub] CrossRef - Association of body weight change with all-cause and cause-specific mortality: A nationwide population-based study
So Yoon Kwon, Gyuri Kim, Jungkuk Lee, Jiyun Park, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Diabetes Research and Clinical Practice.2023; 199: 110666. CrossRef - Association between lipid variability and the risk of mortality in cancer patients not receiving lipid-lowering agents
Seohyun Kim, Gyuri Kim, So Hyun Cho, Rosa Oh, Ji Yoon Kim, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Frontiers in Oncology.2023;[Epub] CrossRef - Association between visit-to-visit lipid variability and risk of ischemic heart disease: a cohort study in China
Yonghao Wu, Peng Shen, Lisha Xu, Zongming Yang, Yexiang Sun, Luhua Yu, Zhanghang Zhu, Tiezheng Li, Dan Luo, Hongbo Lin, Liming Shui, Mengling Tang, Mingjuan Jin, Kun Chen, Jianbing Wang
Endocrine.2023;[Epub] CrossRef - Variability of Metabolic Risk Factors: Causative Factor or Epiphenomenon?
Hye Jin Yoo
Diabetes & Metabolism Journal.2022; 46(2): 257. CrossRef - Long-Term Variability in Physiological Measures in Relation to Mortality and Epigenetic Aging: Prospective Studies in the US and China
Hui Chen, Tianjing Zhou, Shaowei Wu, Yaying Cao, Geng Zong, Changzheng Yuan
SSRN Electronic Journal .2022;[Epub] CrossRef
- Long-term variability in physiological measures in relation to mortality and epigenetic aging: prospective studies in the USA and China
- Cardiovascular Risk/Epidemiology
- Appraisal of Guidelines for the Management of Blood Pressure in Patients with Diabetes Mellitus: The Consensuses, Controversies and Gaps
- Menghui Liu, Shaozhao Zhang, Xiaohong Chen, Yue Guo, Xiangbin Zhong, Zhenyu Xiong, Yifen Lin, Huimin Zhou, Yiquan Huang, Zhengzhipeng Zhang, Lichun Wang, Xiaodong Zhuang, Xinxue Liao
- Diabetes Metab J. 2021;45(5):753-764. Published online April 23, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0134
- 4,866 View
- 143 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
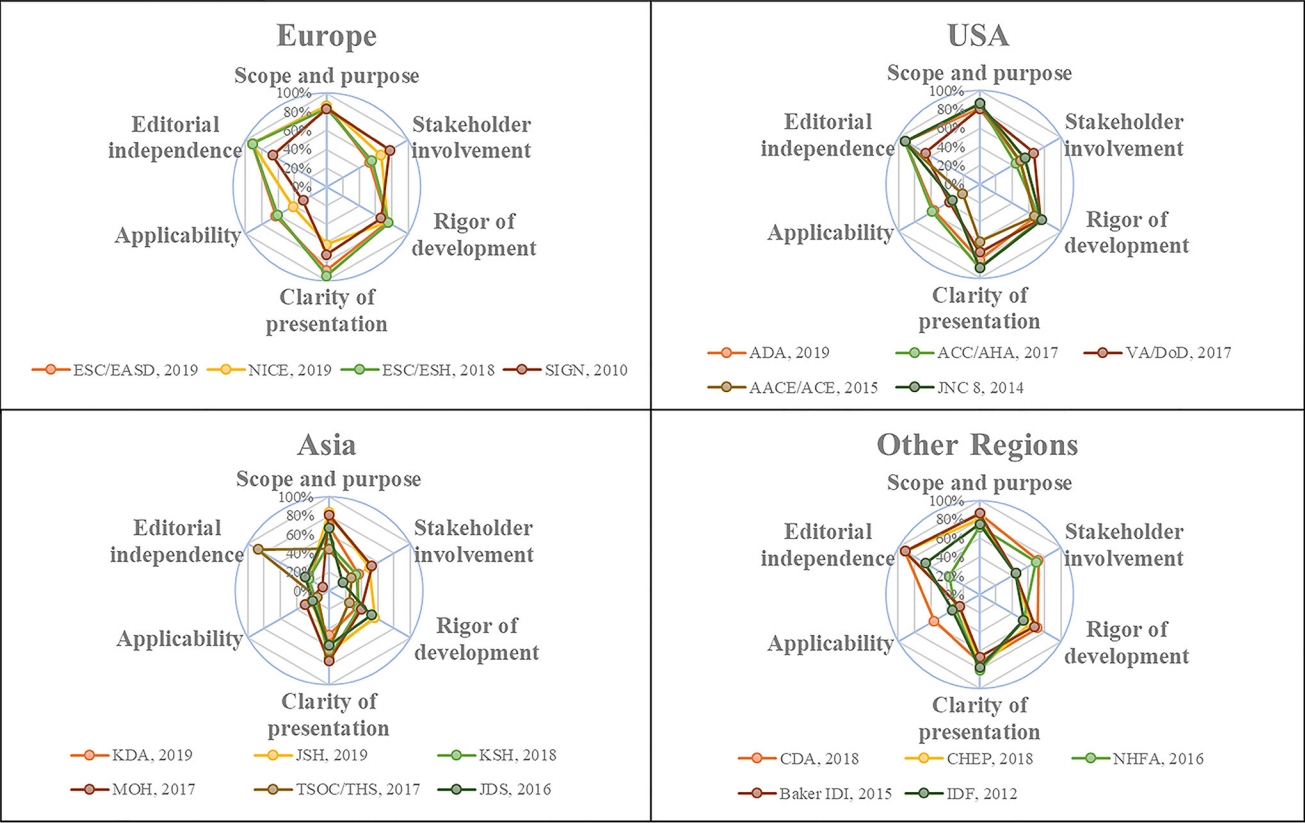
ePub - Background
Currently available guidelines contain conflicting recommendations on the management of blood pressure (BP) in patients with diabetes mellitus (DM). Therefore, it is necessary to appraise the guidelines and summarize the agreements and differences among recommendations.
Methods
Four databases and the websites of guideline organizations were searched for guidelines regarding BP targets and thresholds for pharmacologic therapy in DM patients, and the included guidelines were appraised with the Appraisal of Guidelines for Research and Evaluation (AGREE) II instrument.
Results
In 6,498 records identified, 20 guidelines met our inclusion criteria with 64.0% AGREE II scores (interquartile range, 48.5% to 72.0%). The scores of the European and American guidelines were superior to those of the Asian guidelines (both adjusted P<0.001). Most of the guidelines advocated systolic BP targets <130 mm Hg (12 guidelines, 60%) and diastolic BP targets <80 mm Hg (14 guidelines, 70%) in DM patients. Approximately half of the guidelines supported systolic BP thresholds >140 mm Hg (10 guidelines, 50%) and diastolic BP thresholds >90 mm Hg (nine guidelines, 45%). The tiny minority of the guidelines provided the relevant recommendations regarding the lower limit of official BP targets and the ambulatory BP monitoring (ABPM)/home BP monitoring (HBPM) targets and thresholds in DM patients.
Conclusion
The lower official BP targets (<130/80 mm Hg) in patients with DM are advocated by most of the guidelines, but they contain conflicting recommendations on the official BP thresholds. Moreover, the gaps regarding the lower limit of official BP targets and the ABPM/HBPM targets and thresholds need to be considered by future study.
- Metabolic Risk/Epidemiology
- Association between Higher Blood Pressure and Risk of Diabetes Mellitus in Middle-Aged and Elderly Chinese Adults
- Xue Yang, Jian Chen, An Pan, Jason H.Y. Wu, Fei Zhao, Yue Xie, Yi Wang, Yi Ye, Xiong-Fei Pan, Chun-Xia Yang
- Diabetes Metab J. 2020;44(3):436-445. Published online November 14, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0081
- 4,821 View
- 83 Download
- 10 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background To examine the prospective association between higher blood pressure (BP) and risk of type 2 diabetes mellitus (T2DM) in middle-aged and elderly Chinese adults.
Methods A total of 9,642 middle-aged and elderly Chinese adults (≥45 years old; 47.30% men) without diabetes from the China Health and Retirement Longitudinal Study were included for analyses. Participants were categorized into three groups: normal BP, prehypertension, and hypertension, according to the 2010 Chinese Guidelines for the Management of Hypertension. The incidence of T2DM was determined by self-reported physician diagnosis during two follow-up surveys conducted in 2013 to 2014 and 2015 to 2016.
Results During the 4-year follow-up, 429 participants (4.45%) developed T2DM, including 3.51% of the men and 5.29% of the women. The incidence rates of T2DM were 2.57%, 3.75%, and 6.71% in the normal BP, prehypertension, and hypertension groups, respectively. After adjustment for age, sex, education level, residence, smoking status, alcohol consumption, body mass index, waist circumference, and dyslipidemia, both prehypertension (odds ratio [OR], 1.32; 95% confidence interval [CI], 0.98 to 1.77) and hypertension (OR, 2.02; 95% CI, 1.54 to 2.64) were associated with increased risk of T2DM, compared to those with a normal BP. The ORs associated with T2DM were 1.08 (95% CI, 1.03 to 1.13) for an increase of 10 mm Hg in systolic BP and 1.06 (95% CI, 1.01 to 1.10) for an increase of 5 mm Hg in diastolic BP.
Conclusion Higher BP is a risk factor for T2DM in middle-aged and elderly Chines. It may be a potential target for diabetes prevention.
-
Citations
Citations to this article as recorded by- Leveraging IgG N-glycosylation to infer the causality between T2D and hypertension
Haotian Wang, Yuan Li, Weijie Cao, Jie Zhang, Mingyang Cao, Xiaoni Meng, Di Liu, Youxin Wang
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Externalizing traits: Shared causalities for COVID-19 and Alzheimer's dementia using Mendelian randomization analysis
Haotian Wang, Mingyang Cao, Yingjun Xi, Weijie Cao, Xiaoyu Zhang, Xiaoni Meng, Deqiang Zheng, Lijuan Wu, Wei Wang, Di Liu, Youxin Wang, Shibu Yooseph
PNAS Nexus.2023;[Epub] CrossRef - Causal Paradigm Between Common Comorbidities of Cardiovascular and Metabolism-Related Diseases in Elderly: Evidence from Cross-Sectional and Mendelian Randomization Studies
Junwang Gu, Qi Wang, Xuanhui Wu, Han Zhang, Chunmei Wu, Wei Qiu
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 2953. CrossRef - Hypertension, Arterial Stiffness, and Diabetes: a Prospective Cohort Study
Xue Tian, Yingting Zuo, Shuohua Chen, Yijun Zhang, Xiaoli Zhang, Qin Xu, Shouling Wu, Anxin Wang
Hypertension.2022; 79(7): 1487. CrossRef - Integrated analysis of probability of type 2 diabetes mellitus with polymorphisms and methylation of SLC30A8 gene: a nested case-control study
Fulan Hu, Yanyan Zhang, Pei Qin, Yang Zhao, Dechen Liu, Qionggui Zhou, Gang Tian, Quanman Li, Chunmei Guo, Xiaoyan Wu, Ranran Qie, Shengbing Huang, Minghui Han, Yang Li, Dongsheng Hu, Ming Zhang
Journal of Human Genetics.2022; 67(11): 651. CrossRef - Understanding Frailty: Probabilistic Causality between Components and Their Relationship with Death through a Bayesian Network and Evidence Propagation
Ricardo Ramírez-Aldana, Juan Carlos Gomez-Verjan, Carmen García-Peña, Luis Miguel Gutiérrez-Robledo, Lorena Parra-Rodríguez
Electronics.2022; 11(19): 3001. CrossRef - Novel lipid indicators and the risk of type 2 diabetes mellitus among Chinese hypertensive patients: findings from the Guangzhou Heart Study
Hai Deng, Peng Hu, Huoxing Li, Huanning Zhou, Xiuyi Wu, Maohua Yuan, Xueru Duan, Miaochan Lao, Chuchu Wu, Murui Zheng, Xiang Qian Lao, Wenjing Zhao, Xudong Liu
Cardiovascular Diabetology.2022;[Epub] CrossRef - Trends and Comparisons of Blood Pressure and Fasting Plasma Glucose in Patients with Hypertension, Diabetes, and Comorbidity: 4-Year Follow-Up Data
Luxinyi Xu, Xiaotong Wen, Ying Yang, Dan Cui
Risk Management and Healthcare Policy.2022; Volume 15: 2221. CrossRef - Policyholder cluster divergence based differential premium in diabetes insurance
Benjiang Ma, Qing Tang, Yifang Qin, Muhammad Farhan Bashir
Managerial and Decision Economics.2021; 42(7): 1793. CrossRef - Association of hypertension and incident diabetes in Chinese adults: a retrospective cohort study using propensity-score matching
Yang Wu, Haofei Hu, Jinlin Cai, Runtian Chen, Xin Zuo, Heng Cheng, Dewen Yan
BMC Endocrine Disorders.2021;[Epub] CrossRef
- Leveraging IgG N-glycosylation to infer the causality between T2D and hypertension
- Epidemiology
- Association of Visit-to-Visit Variability of Blood Pressure with Cardiovascular Disease among Type 2 Diabetes Mellitus Patients: A Cohort Study
- Zhe-Bin Yu, Die Li, Xue-Yu Chen, Pei-Wen Zheng, Hong-Bo Lin, Meng-Ling Tang, Ming-Juan Jin, Jian-Bing Wang, Kun Chen
- Diabetes Metab J. 2019;43(3):350-367. Published online March 6, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0108
- 5,250 View
- 81 Download
- 10 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Increasing evidence has shown that visit-to-visit variability (VVV) of blood pressure (BP) is associated with an increased risk of cardiovascular disease (CVD). The objective of this study was to evaluate the impact of VVV of systolic blood pressure (SBP) and diastolic blood pressure (DBP) on the risk of CVD among patients with type 2 diabetes mellitus (T2DM) in China.
Methods We conducted a retrospective cohort study of 10,163 T2DM patients who were not previously diagnosed with CVD from January 2008 to December 2012 in Ningbo, China. The VVV of BP was calculated using five metrics, including standard deviation (SD), coefficient of variation (CV), variation independent of mean, average real variability, and successive variability (SV) of measurements, obtained over a 24-month measurement period. Hazard ratios and 95% confidence intervals (CIs) were estimated by Cox proportional hazards regression models for the associations of variability in BP with risk of CVD.
Results A total of 894 CVD events were observed during a median follow-up of 49.5 months. The hazard ratio in the highest quintile of SD of SBP was 1.24 (95% CI, 1.01 to 1.52) compared with patients in the lowest quintile. The association between higher VVV of DBP and risk of CVD was not consistent across different metrics and sensitivity analyses.
Conclusion Higher VVV of SBP was associated with an increased risk of CVD, irrespective of the mean SBP level. Future studies are needed to confirm these findings.
-
Citations
Citations to this article as recorded by- Association between Variability of Metabolic Risk Factors and Cardiometabolic Outcomes
Min Jeong Park, Kyung Mook Choi
Diabetes & Metabolism Journal.2022; 46(1): 49. CrossRef - Joint effect of blood pressure and glycemic variation on the risk of cardiovascular morbidity and mortality in persons with type 2 diabetes
Cheng-Chieh Lin, Chia-Ing Li, Ya-Ling Juan, Chiu-Shong Liu, Chih-Hsueh Lin, Shing-Yu Yang, Tsai-Chung Li
Metabolism.2022; 136: 155308. CrossRef - Visit‐to‐visit variability of blood pressure and risk of macrovascular and microvascular complications in patients with type 2 diabetes: A Chinese primary‐care cohort study
Ying Deng, Yin Liu, Shengchao Zhang, Hanbing Yu, Xiaozhou Zeng, Rongrong An, Zhenyuan Chen, Na Sun, Xiaoxv Yin, Yue Dong
Journal of Diabetes.2022; 14(11): 767. CrossRef - Visit‑to‑visit blood pressure variability is associated with arterial stiffness in Chinese adults: A prospective analysis
Yuwen Zhang, Lizhan Bie, Mian Li, Tiange Wang, Min Xu, Jieli Lu, Shuangyuan Wang, Jie Zhang, Yufang Bi, Weiqing Wang, Guang Ning, Yuhong Chen, Yu Xu
The Journal of Clinical Hypertension.2021; 23(4): 802. CrossRef - Variability of risk factors and diabetes complications
Antonio Ceriello, Francesco Prattichizzo
Cardiovascular Diabetology.2021;[Epub] CrossRef - Effectiveness of statin intensive therapy in type 2 diabetes mellitus with high visit-to-visit blood pressure variability
Shota Ikeda, Keisuke Shinohara, Nobuyuki Enzan, Shouji Matsushima, Takeshi Tohyama, Kouta Funakoshi, Junji Kishimoto, Hiroshi Itoh, Issei Komuro, Hiroyuki Tsutsui
Journal of Hypertension.2021; 39(7): 1435. CrossRef - Prognostic importance of visit-to-visit blood pressure variability for micro- and macrovascular outcomes in patients with type 2 diabetes: The Rio de Janeiro Type 2 Diabetes Cohort Study
Claudia R. L. Cardoso, Nathalie C. Leite, Gil F. Salles
Cardiovascular Diabetology.2020;[Epub] CrossRef - Impact of visit-to-visit variability in blood pressure on coronary plaque as assessed by integrated backscatter intravascular ultrasound
Yuta Kato, Atsushi Iwata, Makito Futami, Motoki Yamashita, Eiji Shigemoto, Takashi Kuwano, Makoto Sugihara, Shin-Ichiro Miura
Clinical and Experimental Hypertension.2020; 42(7): 608. CrossRef - VISIT-TO-VISIT BLOOD PRESSURE VARIABILITY IN RURAL MALES WITH ARTERIAL HYPERTENSION: ASSOCIATION WITH NON-VALVULAR ATRIAL FIBRILLATION
T.I. Nimtsovych, A.M. Kravchenko, O.Yu. Mishcheniuk, К.О. Mikhaliev, T.Ya. Chursina
Клінічна та профілактична медицина.2020; (2): 90. CrossRef - VISIT-TO-VISIT BLOOD PRESSURE VARIABILITY AND TARGET ORGAN DAMAGE IN RURAL DWELLERS WITH UNCOMPLICATED ARTERIAL HYPERTENSION
Tetiana I. Nimtsovych, Anatolii M. Kravchenko, Olha Yu. Mishcheniuk, Tamara Ya. Chursina, Кyrylo О. Mikhaliev, Viktor P. Polovyi
Wiadomości Lekarskie.2020; 73(12): 2591. CrossRef - HDL-Cholesterol, Its Variability, and the Risk of Diabetes: A Nationwide Population-Based Study
Seung-Hwan Lee, Hun-Sung Kim, Yong-Moon Park, Hyuk-Sang Kwon, Kun-Ho Yoon, Kyungdo Han, Mee Kyoung Kim
The Journal of Clinical Endocrinology & Metabolism.2019; 104(11): 5633. CrossRef
- Association between Variability of Metabolic Risk Factors and Cardiometabolic Outcomes
- Higher Prevalence and Awareness, but Lower Control Rate of Hypertension in Patients with Diabetes than General Population: The Fifth Korean National Health and Nutrition Examination Survey in 2011
- Seung-Hyun Ko, Hyuk-Sang Kwon, Dae Jung Kim, Jae Hyeon Kim, Nan Hee Kim, Chul Sik Kim, Kee-Ho Song, Jong Chul Won, Soo Lim, Sung Hee Choi, Kyungdo Han, Yong-Moon Park, Bong-Yun Cha
- Diabetes Metab J. 2014;38(1):51-57. Published online February 19, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.1.51
- 3,829 View
- 29 Download
- 28 Web of Science
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We investigated the prevalence, awareness, treatment, and control rate of hypertension in Korean adults with diabetes using nationally representative data.
Methods Using data of 5,105 adults from the fifth Korea National Health and Nutrition Examination Survey in 2011 (4,389 nondiabetes mellitus [non-DM]), 242 newly diagnosed with DM (new-DM), and 474 previously diagnosed with DM (known-DM), we analyzed the prevalence of hypertension (mean systolic blood pressure ≥140 mm Hg, diastolic blood pressure ≥90 mm Hg, or use of antihypertensive medication) and control rate of hypertension (blood pressure [BP] <130/80 mm Hg).
Results The prevalence of hypertension in diabetic adults was 54.6% (44.4% in new-DM and 62.6% in known-DM,
P <0.0001 andP <0.0001, respectively) compared with non-DM adults (26.2%). Compared to non-DM, awareness (85.7%,P <0.001) and treatment (97.0%,P =0.020) rates were higher in known-DM, whereas no differences were found between new-DM and non-DM. Control rate among all hypertensive subjects was lower in new-DM (14.9%), compared to non-DM (35.1%,P <0.001) and known-DM (33.3%,P =0.004). Control rate among treated subjects was also lower in new-DM (25.2%), compared to non-DM (68.4%,P <0.0001) and known-DM (39.9%,P <0.0001).Conclusion Higher prevalence and low control rate of hypertension in adults with diabetes suggest that stringent efforts are needed to control BP in patients with diabetes, particularly in newly diagnosed diabetic patients.
-
Citations
Citations to this article as recorded by- Comorbidities of diabetes and hypertension in Vietnam: current burden, trends over time, and correlated factors
Thi Hoang Lan Vu, Thi Tu Quyen Bui, Quoc Bao Tran, Quynh Nga Pham, Duc Truong Lai, Tu Hoang Le, Van Minh Hoang
BMC Public Health.2023;[Epub] CrossRef - Diabetes Fact Sheets in Korea, 2020: An Appraisal of Current Status
Chan-Hee Jung, Jang Won Son, Shinae Kang, Won Jun Kim, Hun-Sung Kim, Hae Soon Kim, Mihae Seo, Hye-Jung Shin, Seong-Su Lee, Su Jin Jeong, Yongin Cho, Seung Jin Han, Hyang Mi Jang, Mira Rho, Shinbi Lee, Mihyun Koo, Been Yoo, Jung-Wha Moon, Hye Young Lee, Ja
Diabetes & Metabolism Journal.2021; 45(1): 1. CrossRef - Time Trends in Comorbidity and Management of Hypertension and Self-reported Diabetes: A 15-Year Nationwide Longitudinal Study in China
Yixuan Li, Xiaomin Sun, Junxiang Wei, Jing Wu, Youfa Wang
American Journal of Hypertension.2021; 34(8): 810. CrossRef - Impact of Sociodemographic Characteristics, Lifestyle, and Obesity on Coexistence of Diabetes and Hypertension: A Structural Equation Model Analysis amongst Chinese Adults
Wenwen Wu, Jie Diao, Jinru Yang, Donghan Sun, Ying Wang, Ziling Ni, Fen Yang, Xiaodong Tan, Ling Li, Li Li, Lanfranco D Elia
International Journal of Hypertension.2021; 2021: 1. CrossRef - Real-World Effectiveness and Safety of a Single-Pill Combination of Olmesartan/Amlodipine/Hydrochlorothiazide in Korean Patients with Essential Hypertension (RESOLVE): A Large, Observational, Retrospective, Cohort Study
Sung-Ji Park, Si Jae Rhee
Advances in Therapy.2020; 37(8): 3500. CrossRef - Comprehensive Identification of Key Genes Involved in Development of Diabetes Mellitus-Related Atherogenesis Using Weighted Gene Correlation Network Analysis
Qi Huang, Guoxiong Deng, Rongguo Wei, Qiaoye Wang, Donghua Zou, Jinru Wei
Frontiers in Cardiovascular Medicine.2020;[Epub] CrossRef - Risk of hypertension among different metabolic phenotypes: a systematic review and meta-analysis of prospective cohort studies
Atieh Mirzababaei, Hadis Mozaffari, Sakineh Shab-Bidar, Alireza Milajerdi, Kurosh Djafarian
Journal of Human Hypertension.2019; 33(5): 365. CrossRef - Diabetes Fact Sheet in Korea, 2016: An Appraisal of Current Status
Jong Chul Won, Jae Hyuk Lee, Jae Hyeon Kim, Eun Seok Kang, Kyu Chang Won, Dae Jung Kim, Moon-Kyu Lee
Diabetes & Metabolism Journal.2018; 42(5): 415. CrossRef - Evaluation of an association between long sleep duration and periodontal disease among men and women using nationally representative data
Kyungdo Han, Yong-Moon Park, Jun-Beom Park
Gaceta Sanitaria.2018; 32(2): 143. CrossRef - Association between oral health behavior and periodontal disease among Korean adults
Kyungdo Han, Jun-Beom Park
Medicine.2017; 96(7): e6176. CrossRef - Age threshold for moderate and severe periodontitis among Korean adults without diabetes mellitus, hypertension, metabolic syndrome, and/or obesity
Kyungdo Han, Jun-Beom Park
Medicine.2017; 96(33): e7835. CrossRef - Clinical Course and Risk Factors of Diabetic Retinopathy in Patients with Type 2 Diabetes Mellitus in Korea
Jae-Seung Yun, Tae-Seok Lim, Seon-Ah Cha, Yu-Bae Ahn, Ki-Ho Song, Jin A Choi, Jinwoo Kwon, Donghyun Jee, Yang Kyung Cho, Yong-Moon Park, Seung-Hyun Ko
Diabetes & Metabolism Journal.2016; 40(6): 482. CrossRef - Different effect of alcohol consumption on hypertension according to metabolic health status
H K Yang, K Han, Y-M Park, H-S Kwon, K-H Yoon, S-H Lee
Journal of Human Hypertension.2016; 30(10): 591. CrossRef - Differential Association of Metabolic Risk Factors with Open Angle Glaucoma according to Obesity in a Korean Population
Hyun-Ah Kim, Kyungdo Han, Yun-Ah Lee, Jin A Choi, Yong-Moon Park
Scientific Reports.2016;[Epub] CrossRef - Low skeletal muscle mass is associated with non-alcoholic fatty liver disease in Korean adults: the Fifth Korea National Health and Nutrition Examination Survey
Hee Yeon Kim, Chang Wook Kim, Chung-Hwa Park, Jong Young Choi, Kyungdo Han, Anwar T Merchant, Yong-Moon Park
Hepatobiliary & Pancreatic Diseases International.2016; 15(1): 39. CrossRef - Diabetic Cardiovascular Autonomic Neuropathy Predicts Recurrent Cardiovascular Diseases in Patients with Type 2 Diabetes
Seon-Ah Cha, Jae-Seung Yun, Tae-Seok Lim, Kyoungil Min, Ki-Ho Song, Ki-Dong Yoo, Yong-Moon Park, Yu-Bae Ahn, Seung-Hyun Ko, James M Wright
PLOS ONE.2016; 11(10): e0164807. CrossRef - Lipoprotein(a) predicts the development of diabetic retinopathy in people with type 2 diabetes mellitus
Jae-Seung Yun, Tae-Seok Lim, Seon-Ah Cha, Yu-Bae Ahn, Ki-Ho Song, Jin A. Choi, Jinwoo Kwon, Donghyun Jee, Yang Kyung Cho, Yong-Moon Park, Seung-Hyun Ko
Journal of Clinical Lipidology.2016; 10(2): 426. CrossRef - Elevated lipoprotein(a) levels predict cardiovascular disease in type 2 diabetes mellitus: a 10-year prospective cohort study
Tae-Seok Lim, Jae-Seung Yun, Seon-Ah Cha, Ki-Ho Song, Ki-Dong Yoo, Yu-Bae Ahn, Yong-Moon Park, Seung-Hyun Ko
The Korean Journal of Internal Medicine.2016; 31(6): 1110. CrossRef - The association of incident hypertension with metabolic health and obesity status: definition of metabolic health does not matter
Yu Mi Kang, Chang Hee Jung, Jung Eun Jang, Jenie Yoonoo Hwang, Eun Hee Kim, Joong‐Yeol Park, Hong‐Kyu Kim, Woo Je Lee
Clinical Endocrinology.2016; 85(2): 207. CrossRef - The association between abnormal heart rate variability and new onset of chronic kidney disease in patients with type 2 diabetes: A ten-year follow-up study
Jae-Seung Yun, Yu-Bae Ahn, Ki-Ho Song, Ki-Dong Yoo, Hyung-Wook Kim, Yong-Moon Park, Seung-Hyun Ko
Diabetes Research and Clinical Practice.2015; 108(1): 31. CrossRef - Obesity as a Potential Risk Factor for Blepharoptosis: The Korea National Health and Nutrition Examination Survey 2008-2010
Ji-Sun Paik, Su-Kyung Jung, Kyung-Do Han, Sang-Duck Kim, Yong-Moon Park, Suk-Woo Yang, Michele Madigan
PLOS ONE.2015; 10(7): e0131427. CrossRef - Cost-effectiveness analysis of low density lipoprotein cholesterol-lowering therapy in hypertensive patients with type 2 diabetes in Korea: single-pill regimen (amlodipine/atorvastatin) versus double-pill regimen (amlodipine+atorvastatin)
Ji-Hyun Park, Yong-Ho Lee, Su-Kyoung Ko, Bong-Soo Cha
Epidemiology and Health.2015; 37: e2015010. CrossRef - Early Renal Abnormalities as an Indicator of Cardiovascular Risk in Type 2 Diabetes
Francesca Viazzi, Barbara Bonino, Elena Ratto, Salvatore De Cosmo, Roberto Pontremoli
High Blood Pressure & Cardiovascular Prevention.2014; 21(4): 257. CrossRef
- Comorbidities of diabetes and hypertension in Vietnam: current burden, trends over time, and correlated factors
- Management of Blood Pressure in Patients with Type 2 Diabetes Mellitus: A Nationwide Survey in Korean
- Mi Hae Seo, Woo Je Lee, Cheol Young Park, Sung Rae Kim, Joong Yeol Park, Kun-Ho Yoon, Moon Kyu Lee, Sung Woo Park
- Diabetes Metab J. 2011;35(4):348-353. Published online August 31, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.4.348
- 3,822 View
- 33 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Hypertension is common in patients with type 2 diabetes, affecting up to 60% of patients. The Korean Diabetes Association performed a nationwide survey about prevalence, awareness and control of hypertension among diabetic Koreans.
Methods The current survey included 3,859 diabetic patients recruited from 43 hospitals in Korea. Age, gender, height, weight and blood pressure (BP) were measured by standard methods. Data on fasting plasma glucose, glycosylated hemoglobin (HbA1c), awareness of hypertension, and compliance of antihypertensive medication were collected via interview and reviewed using patient medical records.
Results A total of 57.5% of all patients were >60 years old. Their mean HbA1c was 7.6±1.5%. Among antihypertensive medication users, 39.9% had <130 mm Hg and <80 mm Hg, whereas 60.1% had ≥130 mm Hg or ≥80 mm Hg. The answer "BP is under good control" was given by 75.1% of the antihypertensive medication users. Out of these patients, 26.4% had <130 mm Hg and <80 mm Hg, whereas 73.6% had ≥130 mm Hg or ≥80 mm Hg. A total of 75.5% of antihypertensive medication users answered that they had taken their antihypertensive medication every day for the past 2 weeks. "Forgetfulness" was most frequently the reason of non-compliance for patients that did not take their antihypertensive medication regularly.
Conclusion Approximately one third of the patients with diabetes were found to reach target blood pressure control in the 43 hospitals across Korea. Stricter control is needed to reduce severe complications of diabetes in Korea.
-
Citations
Citations to this article as recorded by- Value of ambulatory blood pressure measurement in diagnosing hypotension in hypertensive diabetic patients with medication-controlled BP
Kamal Alghalayini
JRSM Cardiovascular Disease.2020; 9: 204800402093088. CrossRef - Association between blood pressure and target organ damage in patients with chronic kidney disease and hypertension: results of the APrODiTe study
Ran-hui Cha, Sejoong Kim, Sun Ae Yoon, Dong-Ryeol Ryu, Ji Eun Oh, Sang-Youb Han, Eun Young Lee, Dong Ki Kim, Yon Su Kim
Hypertension Research.2014; 37(2): 172. CrossRef - Blood Pressure Control According to the Prevalence of Diabetes in Renal Transplant Recipients
E. Zbroch, J. Malyszko, I. Glowinska, D. Maciorkowska, G. Kobus, M. Mysliwiec
Transplantation Proceedings.2013; 45(1): 200. CrossRef - Prevalence, awareness, treatment and control of hypertension in adults with diagnosed diabetes: The Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV)
H-S Lee, S-S Lee, I-Y Hwang, Y-J Park, S-H Yoon, K Han, J-W Son, S-H Ko, Y G Park, H W Yim, W-C Lee, Y-M Park
Journal of Human Hypertension.2013; 27(6): 381. CrossRef - Multi-Institutional Analysis of Localized Renal Cell Carcinoma that Demonstrates the Impact of Diabetic Status on Prognosis After Nephrectomy
Yun-Sok Ha, Won Tae Kim, Seok-Joong Yun, Sang-Cheol Lee, Wun-Jae Kim, Yong Hyun Park, Seok Ho Kang, Sung-Hoo Hong, Seok-Soo Byun, Yong-June Kim
Annals of Surgical Oncology.2013; 20(11): 3662. CrossRef
- Value of ambulatory blood pressure measurement in diagnosing hypotension in hypertensive diabetic patients with medication-controlled BP
- Effect of Valsartan on Blood Pressure and Urinary Albumin Excretion in Hypertensive Type 2 Diabetic Patients: An Open-Label, Multicenter Study.
- Se Jun Park, Dae Jung Kim, Hae Jin Kim, Soo Yeon Park, Ji A Seo, Nan Hee Kim, Sung Hee Choi, Soo Lim, Hak Chul Jang, Seung Hyun Ko, Ki Ho Song, Yu Bae Ahn, Soo Kyoung Kim, Yong Wook Cho, Jun Goo Kang, Sung Hee Ihm, Cheol Young Park, Sung Woo Park, Dong Hyun Shin, Yong Hyun Kim, Kwan Woo Lee
- Korean Diabetes J. 2008;32(6):513-521. Published online December 1, 2008
- DOI: https://doi.org/10.4093/kdj.2008.32.6.513
- 2,297 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Activation of renin-angiotensin system (RAS) has been an important mechanism of microvascular and macrovascular complications in diabetic patients. It has been reported that RAS blockades reduce the development and progression of diabetic nephropathy. The aim of this study was to evaluate whether valsartan, an angiotensin II receptor blocker (ARB), reduced blood pressure and urinary albumin excretion rate (UAER) in hypertensive type 2 diabetic patients. METHOD: Three hundred forty-seven hypertensive type 2 diabetic patients who had not taken angiotensin converting enzyme inhibitors or ARB for 6 months prior to this study were enrolled. We measured blood pressure and UAER before and after 24 weeks of valsartan treatment. RESULT: Baseline mean systolic and diastolic blood pressure was 143 +/- 15 and 87 +/- 11 mmHg, respectively and the median albumin excretion rate was 27 ug/mg. Reduction in systolic and diastolic blood pressure was 16 mmHg/10 mmHg and the median UAER was 19.3 ug/mg after 24 weeks (P < 0.01, respectively). When we divided the subjects into three groups according to the UAER (normoalbuminuria, microalbuminuria and macroalbuminuria), significant changes were reported in the microalbuminuria and the macroalbuminuria groups. Thirty-eight (42%) patients with microalbuminuria improved to normoalbuminuria and twelve (41%) patients with macroalbuminuria improved to microalbuminuria. We found an association between the improvement of blood pressure and UAER (R = 0.165, P = 0.015). CONCLUSION: We concluded that valsartan reduces urinary albumin excretion and blood pressure in hypertensive type 2 diabetic patients.
- Determinants of 1-Year Changes of Brachial Ankle Pulse Wave Velocity (baPWV) in Patients with Type 2 Diabetes Mellitus.
- Kyung Won Yun, Bo Hyun Kim, Young Pil Bae, Byeong Do Yi, Seung Woo Lee, Hong Kyu Lim, Yeon Sik Ryu, Chang Won Lee
- Korean Diabetes J. 2008;32(4):346-357. Published online August 1, 2008
- DOI: https://doi.org/10.4093/kdj.2008.32.4.346
- 2,356 View
- 19 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Cardiovascular disease is the leading cause of mortality in type 2 diabetes. PWV correlates well with arterial distensibility and stiffness and a useful approach for evaluating the severity of systemic atherosclerosis in adults, and, in particular, the measurement of brachial-ankle PWV (baPWV) has been commonly reported as a simple, noninvasive and practicable method. baPWV was mainly affected by age, SBP and sex. And also, baPWV was affected by many different factors such as body weight, BMI, waist to hip ratio, HbA1c, microalbuminuria, triglyceride, gammaGTP, duration of DM. We evaluated determinants of 1-year changes of baPWV in patients with type 2 DM. METHODS: The study group comprised 189 diabetic patients who measured ankle brachial pressure index (ABI), baPWV at base line and 1-year later. The anthropometric parameters, blood pressure, pulse pressure, fasting plasma glucose (FBS), fasting insulin, A1c, lipid profile, hsCRP, microalbuminuria, AST/ALT, gammaGTP were also checked concurrently. We also analyzed correlation between change of baPWV and subject's medications. We retrospectively analyzed the relationship between the 1-year changes of baPWV and the other factors. All analyses were performed with the SPSS Version 14.0 and P values < 0.05 were considered significant. RESULTS: baPWV change was affected by systolic blood pressure change, diastolic blood pressure change, pulse pressure change, body weight, BMI, triglyceride change, insulin treatment and total cholesterol. Multiple regression analysis of the relationship between change of baPWV and other associated variables shows that the 1-year change of baPWV was significantly associated with the changes of blood pressure and insulin treatment in patients with type 2 DM. CONCLUSION: 1-year change of baPWV was significantly associated with the changes of blood pressure in patients with type 2 DM. -
Citations
Citations to this article as recorded by- Independent association between glycated hemoglobin and arterial stiffness in healthy men
Jin‐Won Noh, Eun‐Jung Kim, Hyun‐Ju Seo, Soo Geun Kim
Journal of Diabetes Investigation.2016; 7(2): 241. CrossRef - Determinants of Follow-up Changes of Brachial Ankle Pulse Wave Velocity in Korean Women
Dae Young Kim, Sung Yeol Kong, Sung Ja Lee, Ha Do Song, Eun Jin Han, Ji Hoon Yang, Ji Yeon Kim, Dong Hyun Lee, Hyun Ho Shin
Journal of the Korean Society of Hypertension.2012; 18(4): 154. CrossRef - Relationships between Cardiac Autonomic Neuropathy and the Brachial-ankle Pulse Wave Velocity in Patients with Type 2 Diabetes
Young Pil Bae, Byeong Do Yi, Bong-Gun Kim, Jong-Hwa Park, Yong Seop Kwon, Ja Young Park, Chang Won Lee, Bo Hyun Kim, Jae-Sik Jang
Endocrinology and Metabolism.2011; 26(1): 44. CrossRef - The Association of Brachial-Ankle Pulse Wave Velocity with Acute Postprandial Hyperglycemia in Korean Prediabetic and Diabetic Subjects
Chul Woo Ahn
Korean Diabetes Journal.2010; 34(5): 284. CrossRef
- Independent association between glycated hemoglobin and arterial stiffness in healthy men
- Clinical Manifestation and Prognostic Factors in Nonketotic Hyperosmolar Coma.
- Bo Wan Kim, Jung Guk Kim, Sung Woo Ha, Hyun Jeong Lee, Jeung Hun Han, Sang Won Jung, Jick Hwa Nam, Si Hyung Park, Soon Hee Lee
- Korean Diabetes J. 1999;23(4):575-584. Published online January 1, 2001
- 951 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Nonketotic hyperosmolar coma is usually a complication of non-insuli#n dependent diabetes and a syndrome of profound dehydration, hyperglycemia and hyperosmolarity. Therefore the patients present a progressive mental change. We evaluated the clinical manifestations of nonketotic hyperosmolar coma to assess the correlation between initial clinical manifestations and responses to treatment in patients with nonketotic hyperosmolar coma. METHODS: We studied 31 patients who had experienced proven nonketotic hyperosmolar coma at Kyungpook National University Hospital from March 1987 to February 1998. We divided nonketotic hyperosmolar coma patients into two groups, tbe complete recovery group and the incomplete recovery group, and compared clinical features and laboratory findings between these two groups. RESULTS: l) A total of 31 patients were studied. Eighteen patients were in the complete recovery group and thirteen patients were in the incomplete recovery group. 2) Mean age was 63.1+10.1 years old, initial blood glucose was 781.8+314.3 mg/dL, effective osmolarity was 342.6+34.9 mosm/L, arterial pH was 7.34. Serum creatinine level was 241.7+130.0 uol/L and BUN was 23.1+12.5 mmol/L. 3) Among clinical features of both groups (complete recovery and incomplete recovery groups), initial systolic blood pressure was 131.4+26.1 mmHg and 104.1+28.6 mmHg, diastolic blood pressure was 90.6+16.5 mmHg and 63.2+17.4 mmHg, and mean arterial blood pressure was 104.2 +18.2 mmHg and 76.8+19.7 mmHg. They revealed a significant difference statistically. 4) Arterial blood pH was 7.40 and 7.25, BUN was 18.4+11.7 mmol/L and 29.5+11.1mmol/L, and WBC count was 13850+4122/ mm and 19823+ 5946/mm. They revealed a significant difference statistically. 5) We also analyzed the significant factors together using multivariate logistic regression analysis. The only significant independent factor responsible for prognosis of nonketotic hyperosmolar coma was initial mean arterial blood pressure. CONCLUSION: Nonketotic hyperosmolar coma occurred more frequently in patients who were older and had abnormal renal function. The prognosis of patients was related with mean arterial blood pressure independently. Mean arterial blood pressure thought to be related to intravascular volume and arterial hypotension seems to reflect dehydration state. In conclusion, prevention and rapid correction of hypotension due to dehydration in older diabetics is the most important treatment to improve the prognosis.

 KDA
KDA
 First
First Prev
Prev





