
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 35(4); 2011 > Article
-
Original ArticleManagement of Blood Pressure in Patients with Type 2 Diabetes Mellitus: A Nationwide Survey in Korean
- Mi Hae Seo1, Woo Je Lee2, Cheol Young Park1, Sung Rae Kim3, Joong Yeol Park2, Kun-Ho Yoon3, Moon Kyu Lee4, Sung Woo Park1
-
Diabetes & Metabolism Journal 2011;35(4):348-353.
DOI: https://doi.org/10.4093/dmj.2011.35.4.348
Published online: August 31, 2011
1Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
2Department of Internal Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
3Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea.
4Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- Corresponding author: Sung Woo Park. Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, 108 Pyeong-dong, Jongno-gu, Seoul 110-746, Korea. sungwoo0913.park@samsung.com
Copyright © 2011 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- Hypertension is common in patients with type 2 diabetes, affecting up to 60% of patients. The Korean Diabetes Association performed a nationwide survey about prevalence, awareness and control of hypertension among diabetic Koreans.
-
Methods
- The current survey included 3,859 diabetic patients recruited from 43 hospitals in Korea. Age, gender, height, weight and blood pressure (BP) were measured by standard methods. Data on fasting plasma glucose, glycosylated hemoglobin (HbA1c), awareness of hypertension, and compliance of antihypertensive medication were collected via interview and reviewed using patient medical records.
-
Results
- A total of 57.5% of all patients were >60 years old. Their mean HbA1c was 7.6±1.5%. Among antihypertensive medication users, 39.9% had <130 mm Hg and <80 mm Hg, whereas 60.1% had ≥130 mm Hg or ≥80 mm Hg. The answer "BP is under good control" was given by 75.1% of the antihypertensive medication users. Out of these patients, 26.4% had <130 mm Hg and <80 mm Hg, whereas 73.6% had ≥130 mm Hg or ≥80 mm Hg. A total of 75.5% of antihypertensive medication users answered that they had taken their antihypertensive medication every day for the past 2 weeks. "Forgetfulness" was most frequently the reason of non-compliance for patients that did not take their antihypertensive medication regularly.
-
Conclusion
- Approximately one third of the patients with diabetes were found to reach target blood pressure control in the 43 hospitals across Korea. Stricter control is needed to reduce severe complications of diabetes in Korea.
- An epidemic of type 2 diabetes (T2DM) is a great concern in the Asian population [1]. Kim et al. [2] reported that the age-adjusted prevalence of diabetes was 7.6% (men, 8.1% ; women 7.5%). Hypertension is extremely common in patients with T2DM, affecting up to 60% of patients [3], consequently adding significantly to its overall morbidity and mortality [4,5]. United Kingdom Prospective Diabetes Study (UKPDS) showed that strict blood pressure (BP) control in patients with hypertension and T2DM achieved a clinically important reduction in the risk of macrovascular and microvascular complications in T2DM [6]. Andros et al. [7] showed that the proportion of patients with diabetes who had uncontrolled hypertension was still high and remains an important health concern accounting for a large economic burden on the United States. Therefore, the adequate control of BP has important clinical and prognostic relevance in reducing economic burden in subjects with type 2 diabetes.
- Recently, Lim et al. [8] reported that the prevalence of hypertension among Korean diabetes was 60.4%. However, there is limited current epidemiologic data on the prevalence, awareness and control of hypertension among diabetic Koreans. Here, we analyzed trends in the prevalence, awareness, treatment, and control of hypertension in Korea, and determined whether there were further improvements in hypertension control according to the current treatment goals.
INTRODUCTION
- Study participants
- This study was a survey conducted in July to October 2010. The participants were diabetic patients who visited one of the endocrinology clinics in 43 hospitals across Korea, and had no mental impairments that could interfere with the survey. The survey was administered to a total of 3,895 participants that agreed to take the survey.
- The survey was approved by the independent Ethics Committee/Institutional Review Board at each study site, and written informed consent was obtained from all participants. The study was performed according to the Good Clinical Practice Guidelines and the Declaration of Helsinki.
- Clinical data collection
- The participants were interviewed individually by nurses who fully understood the survey questions and were trained to conduct the interviews. The interviewer explained the purpose of the survey and asked the participant for his/her consent. A consent form was read and signed by the participant before proceeding with the survey.
- The survey questionnaires were developed by an organizing committee representing the Korean Diabetes Association. The survey for patients with diabetes had 3 categories and 11 questions. Eight questions assessed general characteristics (sex, age, height, weight) and clinical characteristics (fasting glucose concentration, glycated hemoglobin level [HbA1c], treatment modality of diabetes, and presence of complications. A further 3 questions pertained to the status of current hypertension management (awareness of target BP, compliance of antihypertensive medication, type of antihypertensive medication). The body mass index (BMI) was calculated as the weight in kilograms divided by the height in square meters.
- Each question was delivered by an interviewer and cross-checked with the medical records of the participant. The purpose of the survey questionnaires was to identify patients experiencing hypertension with diabetes awareness and their drug compliance. All of the information gathered from this survey remained confidential and was used for research purposes only.
- Definition of hypertension and assessment of BP
- Hypertension was defined as systolic BP (SBP) of at least 130 mm Hg or diastolic BP (DBP) of at least 80 mm Hg in persons with diabetes mellitus or self-reported use of medication for lowering BP [9]. Control of BP in persons with diabetes mellitus was defined as having a BP that was lower than 130 mm Hg systolic and lower than 80 mm Hg diastolic [9]. Patients were labeled as uncontrolled hypertension if the mean of three measures of SBP was ≥130 mm Hg and/or DBP was ≥80 mm Hg. BP was taken following recommendations of the Join National Committee (JNC 7) [10].
- During this time two BP measures were taken in an interval of at least 5 minutes after patients were maintained on their mediation. Measurements began after 5 minutes of quiet rest and were made with a mercury sphygmomanometer with the patient seated. A cuff of suitable size was used. The SBP was taken at Korotkoff phase I and the DBP was taken at Korotkoff phase V [11]. Following that, we calculated BP as the average of two measurements. We also assessed the percentage of the entire population and those with hypertension who were utilizing angiotensin-converting enzyme inhibitors (ACEIs), angiotensin II receptor blockers (ARBs) and other anti-hypertensive medications at the time of chart review. All data are presented as means±standard deviation or number (%). All analyses were performed using SPSS version 18.0 software (SPSS Inc., Chicago, IL, USA).
METHODS
- General characteristics of the survey population
- Of the total 3,895 participants, 48.6% were male and 51.4% were female. A total of 57.5% of all patients were over 60 years old. The proportion of participants in their under-40s, 40s, 50s, 60s, and over-70s were 3.7%, 10.8%, 28.2%, 32.6%, and 24.9%, respectively. The average BMI was 24.6±3.5 kg/m2. Patients who had BMI>25 kg/m2 represented 67.3% of the total participants. The level of BMI decreased according to increasing age. Interestingly, in diabetic patients that were under 40 years old (under-40s), the proportion of BMI>30 kg/m2 was reported as 19.1%, and was higher than that of the other age groups (data not shown).
- The mean value of HbA1c was 7.6±1.5% and 58.4% of all participants achieved the target goal (HbA1c <7.0%) of the ADA guideline [9]. The mean SBP was 127.0±16.6 mm Hg, whereas the mean DBP was 77.0±10.6 mm Hg. In the category of ≥130 mm Hg systolic or ≥80 mm Hg diastolic, the prevalence of not taking antihypertensive drugs or taking them was 23.8% and 37.5%, respectively (Table 1).
- Awareness of target BP and control of BP
- Table 2 indicates the awareness of target BP in diabetic patients. When asked about the awareness of target BP in diabetic patients, 62.5% of participants answered that they had known about their target BP. Out of all patients, the awareness of target BP in diabetic patients (≤120 mm Hg or ≤80 mm Hg) was 47.3% and non-diabetic patients (≤130 mm Hg or ≤80 mm Hg) was 57.3%.
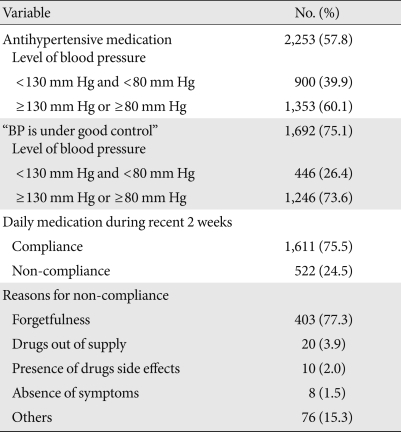
- Prevalence and compliance of antihypertensive medication with diabetes
- Among antihypertensive medication users, 39.9% had <130 mm Hg and <80 mm Hg whereas 60.1% had ≥130 mm Hg and ≥80 mm Hg. The answer "BP is under good control" was given by 75.1% of the antihypertensive medication users, and of these patients, 26.4% were in the <130 mm Hg and <80 mm Hg group, compared to 73.6% in the ≥130 mm Hg or ≥80 mm Hg group. When we analyzed compliance of antihypertensive medication during the past 2 weeks, 75.5% of antihypertensive medication users answered that they had taken antihypertensive medication every day in recent 2 weeks (Table 3). Otherwise, 24.5% were non-compliant and did not take antihypertensive medication regularly. Reasons for non-compliance included forgetfulness, drugs side effects, shortage of drugs and the asymptomatic nature of hypertension, and the frequency of each is shown in Table 3.
- Usage pattern of antihypertensive medication among antihypertensive medication users
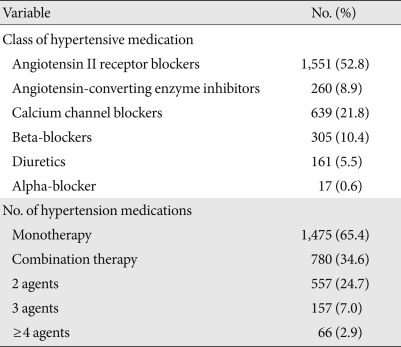
- The proportion of diabetic patients taking antihypertensive medication out of all participants was 57.8%. Antihypertensive medications were classified into one of six categories: ACEIs, ARBs, calcium channel blockers, beta-blockers, diuretics and alpha-blockers. A majority of antihypertensive classification was on angiotensin II receptor blockers 52.8%. The proportion of angiotensin-converting enzyme inhibitors, calcium channel blockers and beta-blockers was 8.9%, 21.8%, and 10.4%, respectively (Table 4).
- Of patients with antihypertensive medication, the proportion of monotherapy, 2 agent combinations, 3 agent combinations and more than 4 agent combinations were 65.4%, 24.7%, 7.0%, 2.9%, respectively. One third of combination therapy was on ARB and hydrochlorothiazide (data not shown).
RESULTS
- Our study is the first epidemiologic study of prevalence, awareness and control of hypertension among diabetic Koreans. We found that the prevalence of patients that did not achieve target BP goal with diabetes was over 60%. These results imply that majority of type 2 diabetic hypertensive patients still do not have control of their BP. Our study also showed that most participants were in good control with regards to BP, and of these patients, a majority were in the uncontrolled BP category. These respondents suggested that there was a difference between BP control in clinical practice and patient thoughts. Therefore, to achieve a target BP with diabetes, clinicians need to inform their patients of target BP, to reduce severe complications that may rise with diabetes in Korea.
- Patient knowledge and awareness of hypertension was significantly associated with compliance to medication for hypertension. A report suggested that patients who knew about the importance of compliance had a significantly higher compliance rate than patients who had been ignorant of that aspect [12]. Our study showed that there is a difference between antihypertensive medication compliance and BP control. Thus, to achieve target BP control with diabetes, clinicians should inform patients about the importance of target BP control.
- Controlling BP was significantly effective in reducing the risk of cardiovascular events and mortality in diabetic patients [9,13,14]. Also, current guidelines recommend lowering BP to <130/80 mm Hg in patients with diabetes [9,10,15,16]. Therefore, untreated or poorly controlled hypertension in diabetic patients is an important health problem. The disease, patients, and clinician factors all contribute to poor BP control in diabetes [17]. However, achieving the target BP largely depends on patient compliance with therapy [17]. In this study, the diabetic patients with hypertension who did not achieve the target were more obese, younger and showed poor compliance with antihypertensive medication. Thus, clinicians should clearly distinguish these patients and establish intensive control measures.
- The results of this study were similar with findings of other recently published studies [7,18,19]. These recent studies also found that 80% to 83% of diabetic patients with hypertension received drug therapy but a range of only 12% to 35% of patients controlled their BP below 130/80 mm Hg depending on various data sources [7,18,19]. However, in our study, about two-thirds of patient utilizing antihypertensive drug therapy still did not meet the goal for BP control, suggesting that these patients should be treated more rigorously to achieve controlled BP.
- Both ADA and JNC 7 recommended a ACEIs or ARBs as a first line therapy in hypertension with diabetes [9,10]. It is very difficult to achieve BP targets with monotherapy, and most patients require a combination of two or three drugs to get to target [9,10]. In combination therapy with a RAAS blocker, ADA suggests a low dose of a thiazide diuretic [9]. Our survey was consistent with these recent studies, and a majority of antihypertensive medication users were on ARBs (52.8%). One-third of combination therapy was on ARBs and hydrochlorothiazide (data not shown).
- The present study had some limitations. First, we used survey-based data with a limited questionnaire, resulting in the analysis being limited only to this particular dataset. In particular for age, this survey did not include duration of diabetes and exact age, but just a questionnaire for the under-40s, 40s, 50s, 60s, and over-70s. Second, only diabetes patients who visited 43 university hospitals were selected. The characteristics of patients in a primary clinic may be very different from those in a tertiary hospital. Therefore, the results cannot be generalized to people with other diseases or to the general population. Third, although an average of up to two BP measurements were obtained under the same standardized conditions, there was the possibility of misclassification of individuals. However, the method of BP measurement in these surveys was consistent with the JNC 7 standard, which recommended the classification of hypertension based on an average of two or more measured [20]. Fourth, participants who were in this survey were not randomized with enrollment.
- In conclusion, our survey found that the majority of patients with diabetes did not reach target BP control in 43 hospitals across Korea. The results showed that the prevalence of diabetic patients with uncontrolled hypertension was still high and remained an important public health concern in Korea. In the survey results from the diabetic patients, we found that stricter control is needed to reduce severe complication of diabetes in Korea.
DISCUSSION
-
Acknowledgements
- This study was partially supported by an unrestricted grant from Astrazeneca Pharmaceuticals Corporation in South Korea.
ACKNOWLEDGMENTS
- 1. Ramachandran A, Ma RC, Snehalatha C. Diabetes in Asia. Lancet 2010;375:408-418. ArticlePubMed
- 2. Kim SM, Lee JS, Lee J, Na JK, Han JH, Yoon DK, Baik SH, Choi DS, Choi KM. Prevalence of diabetes and impaired fasting glucose in Korea: Korean National Health and Nutrition Survey 2001. Diabetes Care 2006;29:226-231. PubMed
- 3. Aubert R. Diabetes in America. 1995. 2nd ed. Bethesda: National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Disease.
- 4. National High Blood Pressure Education Program Working Group report on hypertension in diabetes. Hypertension 1994;23:145-158. ArticlePubMed
- 5. Park Y, Lee H, Koh CS, Min H, Yoo K, Kim Y, Shin Y. Prevalence of diabetes and IGT in Yonchon County, South Korea. Diabetes Care 1995;18:545-548. ArticlePubMedPDF
- 6. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317:703-713. ArticlePubMedPMC
- 7. Andros V, Egger A, Dua U. Blood pressure goal attainment according to JNC 7 guidelines and utilization of antihypertensive drug therapy in MCO patients with type 1 or type 2 diabetes. J Manag Care Pharm 2006;12:303-309. ArticlePubMed
- 8. Lim S, Kim DJ, Jeong IK, Son HS, Chung CH, Koh G, Lee DH, Won KC, Park JH, Park TS, Ahn J, Kim J, Park KG, Ko SH, Ahn YB, Lee I. A nationwide survey about the current status of glycemic control and complications in diabetic patients in 2006: The Committee of the Korean Diabetes Association on the Epidemiology of Diabetes Mellitus. Korean Diabetes J 2009;33:48-57.Article
- 9. American Diabetes Association. Standards of medical care in diabetes--2011. Diabetes Care 2011;34(Suppl 1):S11-S61. ArticlePubMedPMCPDF
- 10. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National High Blood Pressure Education Program Coordinating Committee. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560-2572. ArticlePubMed
- 11. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ. Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. National Heart, Lung, and Blood Institute. National High Blood Pressure Education Program Coordinating Committee. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003;42:1206-1252. ArticlePubMed
- 12. Khalil SA, Elzubier AG. Drug compliance among hypertensive patients in Tabuk, Saudi Arabia. J Hypertens 1997;15:561-565. ArticlePubMed
- 13. Adler AI, Stratton IM, Neil HA, Yudkin JS, Matthews DR, Cull CA, Wright AD, Turner RC, Holman RR. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ 2000;321:412-419. ArticlePubMedPMC
- 14. Vijan S, Hayward RA. Treatment of hypertension in type 2 diabetes mellitus: blood pressure goals, choice of agents, and setting priorities in diabetes care. Ann Intern Med 2003;138:593-602. ArticlePubMed
- 15. Mancia G, Laurent S, Agabiti-Rosei E, Ambrosioni E, Burnier M, Caulfield MJ, Cifkova R, Clement D, Coca A, Dominiczak A, Erdine S, Fagard R, Farsang C, Grassi G, Haller H, Heagerty A, Kjeldsen SE, Kiowski W, Mallion JM, Manolis A, Narkiewicz K, Nilsson P, Olsen MH, Rahn KH, Redon J, Rodicio J, Ruilope L, Schmieder RE, Struijker-Boudier HA, van Zwieten PA, Viigimaa M, Zanchetti A. European Society of Hypertension. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. J Hypertens 2009;27:2121-2158. ArticlePubMed
- 16. Rosendorff C, Black HR, Cannon CP, Gersh BJ, Gore J, Izzo JL Jr, Kaplan NM, O'Connor CM, O'Gara PT, Oparil S. American Heart Association Council for High Blood Pressure Research. American Heart Association Council on Clinical Cardiology. American Heart Association Council on Epidemiology and Prevention. Treatment of hypertension in the prevention and management of ischemic heart disease: a scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and Prevention. Circulation 2007;115:2761-2788. ArticlePubMed
- 17. Wang TJ, Vasan RS. Epidemiology of uncontrolled hypertension in the United States. Circulation 2005;112:1651-1662. ArticlePubMed
- 18. Ong KL, Cheung BM, Man YB, Lau CP, Lam KS. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999-2004. Hypertension 2007;49:69-75. ArticlePubMed
- 19. Wong ND, Lopez VA, L'Italien G, Chen R, Kline SE, Franklin SS. Inadequate control of hypertension in US adults with cardiovascular disease comorbidities in 2003-2004. Arch Intern Med 2007;167:2431-2436. ArticlePubMed
- 20. Chaturvedi S. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7): is it really practical? Natl Med J India 2004;17:227
REFERENCES
Figure & Data
References
Citations

- Value of ambulatory blood pressure measurement in diagnosing hypotension in hypertensive diabetic patients with medication-controlled BP
Kamal Alghalayini
JRSM Cardiovascular Disease.2020; 9: 204800402093088. CrossRef - Association between blood pressure and target organ damage in patients with chronic kidney disease and hypertension: results of the APrODiTe study
Ran-hui Cha, Sejoong Kim, Sun Ae Yoon, Dong-Ryeol Ryu, Ji Eun Oh, Sang-Youb Han, Eun Young Lee, Dong Ki Kim, Yon Su Kim
Hypertension Research.2014; 37(2): 172. CrossRef - Blood Pressure Control According to the Prevalence of Diabetes in Renal Transplant Recipients
E. Zbroch, J. Malyszko, I. Glowinska, D. Maciorkowska, G. Kobus, M. Mysliwiec
Transplantation Proceedings.2013; 45(1): 200. CrossRef - Prevalence, awareness, treatment and control of hypertension in adults with diagnosed diabetes: The Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV)
H-S Lee, S-S Lee, I-Y Hwang, Y-J Park, S-H Yoon, K Han, J-W Son, S-H Ko, Y G Park, H W Yim, W-C Lee, Y-M Park
Journal of Human Hypertension.2013; 27(6): 381. CrossRef - Multi-Institutional Analysis of Localized Renal Cell Carcinoma that Demonstrates the Impact of Diabetic Status on Prognosis After Nephrectomy
Yun-Sok Ha, Won Tae Kim, Seok-Joong Yun, Sang-Cheol Lee, Wun-Jae Kim, Yong Hyun Park, Seok Ho Kang, Sung-Hoo Hong, Seok-Soo Byun, Yong-June Kim
Annals of Surgical Oncology.2013; 20(11): 3662. CrossRef
- Related articles
-
- Risk Prediction and Management of Chronic Kidney Disease in People Living with Type 2 Diabetes Mellitus
- Safety of COVID-19 Vaccines among Patients with Type 2 Diabetes Mellitus: Real-World Data Analysis (Diabetes Metab J 2023;47:356-65)
- Safety of COVID-19 Vaccines among Patients with Type 2 Diabetes Mellitus: Real-World Data Analysis (Diabetes Metab J 2023;47:356-65)
- The Risk of Shoulder Adhesive Capsulitis in Individuals with Prediabetes and Type 2 Diabetes Mellitus: A Longitudinal Nationwide Population-Based Study
- The Beneficial Effect of Glycemic Control against Adverse Outcomes in Patients with Type 2 Diabetes Mellitus and Chronic Kidney Disease

 KDA
KDA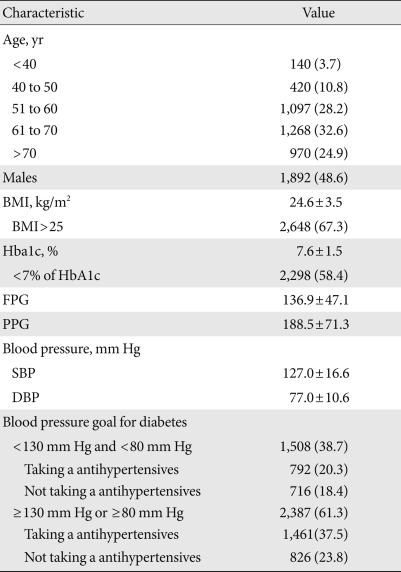

 PubReader
PubReader Cite
Cite



