
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Previous issues
- Page Path
- HOME > Browse > Previous issues
Review
- Guideline/Fact Sheet
- Screening for Prediabetes and Diabetes in Korean Nonpregnant Adults: A Position Statement of the Korean Diabetes Association, 2022
- Kyung Ae Lee, Dae Jung Kim, Kyungdo Han, Suk Chon, Min Kyong Moon, on Behalf of the Committee of Clinical Practice Guideline of Korean Diabetes Association
- Diabetes Metab J. 2022;46(6):819-826. Published online November 24, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0364
- 4,263 View
- 268 Download
- 4 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
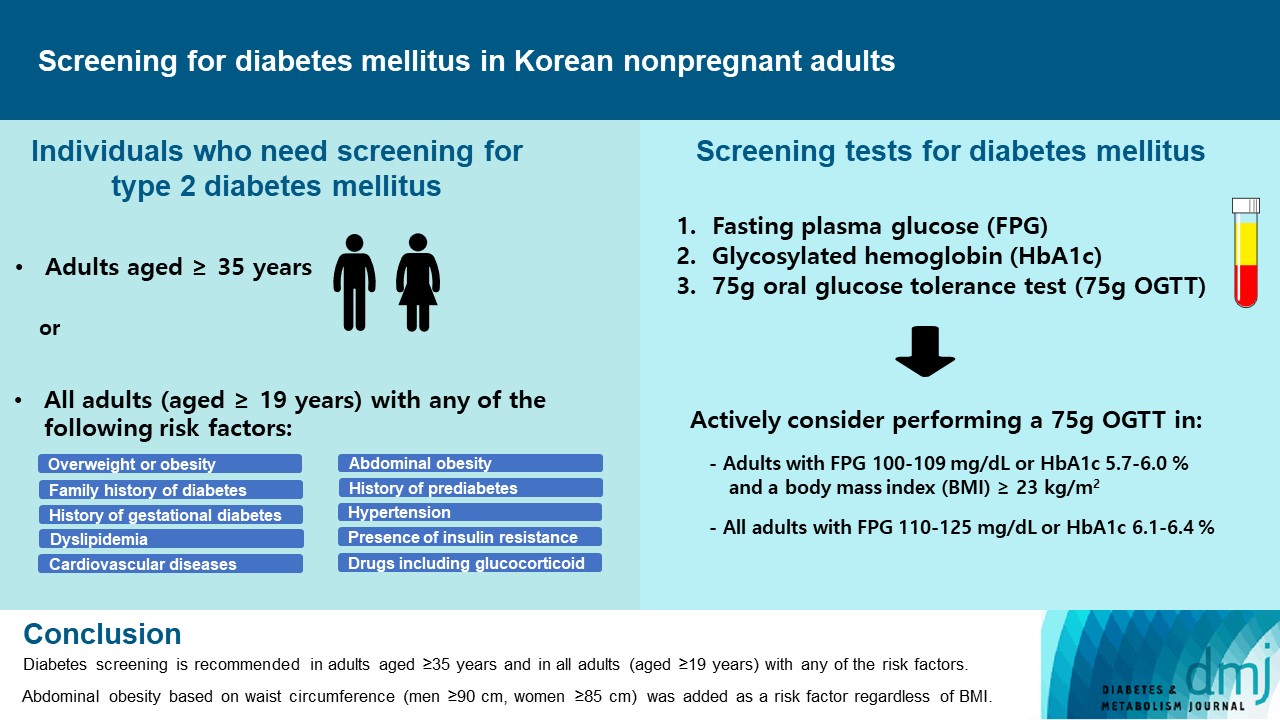
ePub - Diabetes screening serves to identify individuals at high-risk for diabetes who have not yet developed symptoms and to diagnose diabetes at an early stage. Globally, the prevalence of diabetes is rapidly increasing. Furthermore, obesity and/or abdominal obesity, which are major risk factors for type 2 diabetes mellitus (T2DM), are progressively increasing, particularly among young adults. Many patients with T2DM are asymptomatic and can accompany various complications at the time of diagnosis, as well as chronic complications develop as the duration of diabetes increases. Thus, proper screening and early diagnosis are essential for diabetes care. Based on reports on the changing epidemiology of diabetes and obesity in Korea, as well as growing evidence from new national cohort studies on diabetes screening, the Korean Diabetes Association has updated its clinical practice recommendations regarding T2DM screening. Diabetes screening is now recommended in adults aged ≥35 years regardless of the presence of risk factors, and in all adults (aged ≥19) with any of the risk factors. Abdominal obesity based on waist circumference (men ≥90 cm, women ≥85 cm) was added to the list of risk factors.
-
Citations
Citations to this article as recorded by- Oxidative Balance Score and New-Onset Type 2 Diabetes Mellitus in Korean Adults without Non-Alcoholic Fatty Liver Disease: Korean Genome and Epidemiology Study-Health Examinees (KoGES-HEXA) Cohort
Mid-Eum Moon, Dong Hyuk Jung, Seok-Jae Heo, Byoungjin Park, Yong Jae Lee
Antioxidants.2024; 13(1): 107. CrossRef - Efficacy and Safety of Once-Weekly Semaglutide Versus Once-Daily Sitagliptin as Metformin Add-on in a Korean Population with Type 2 Diabetes
Byung-Wan Lee, Young Min Cho, Sin Gon Kim, Seung-Hyun Ko, Soo Lim, Amine Dahaoui, Jin Sook Jeong, Hyo Jin Lim, Jae Myung Yu
Diabetes Therapy.2024; 15(2): 547. CrossRef - Triglyceride-glucose index predicts type 2 diabetes mellitus more effectively than oral glucose tolerance test-derived insulin sensitivity and secretion markers
Min Jin Lee, Ji Hyun Bae, Ah Reum Khang, Dongwon Yi, Mi Sook Yun, Yang Ho Kang
Diabetes Research and Clinical Practice.2024; 210: 111640. CrossRef - Cumulative muscle strength and risk of diabetes: A prospective cohort study with mediation analysis
Shanhu Qiu, Xue Cai, Yan Liang, Wenji Chen, Duolao Wang, Zilin Sun, Bo Xie, Tongzhi Wu
Diabetes Research and Clinical Practice.2023; 197: 110562. CrossRef - Revisiting the Diabetes Crisis in Korea: Call for Urgent Action
Jun Sung Moon
The Journal of Korean Diabetes.2023; 24(1): 1. CrossRef - 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - 2023 Clinical Practice Guidelines for Diabetes
Min Kyong Moon
The Journal of Korean Diabetes.2023; 24(3): 120. CrossRef
- Oxidative Balance Score and New-Onset Type 2 Diabetes Mellitus in Korean Adults without Non-Alcoholic Fatty Liver Disease: Korean Genome and Epidemiology Study-Health Examinees (KoGES-HEXA) Cohort
Editorial
- Oldies but Goodies: Thiazolidinedione as an Insulin Sensitizer with Cardioprotection
- Eun-Hee Cho
- Diabetes Metab J. 2022;46(6):827-828. Published online November 24, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0372
- 1,731 View
- 153 Download
- 3 Web of Science
- 3 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Diabetes: a review of its pathophysiology, and advanced methods of mitigation
Sarika Gupta, Nitin Sharma, Sandeep Arora, Saurabh Verma
Current Medical Research and Opinion.2024; : 1. CrossRef - Lobeglitazone, a novel thiazolidinedione, for secondary prevention in patients with ischemic stroke: a nationwide nested case-control study
Joonsang Yoo, Jimin Jeon, Minyoul Baik, Jinkwon Kim
Cardiovascular Diabetology.2023;[Epub] CrossRef - Molecular Processes Involved in the Shared Pathways between Cardiovascular Diseases and Diabetes
Julita Tokarek, Emilian Budny, Maciej Saar, Kamila Stańczak, Ewa Wojtanowska, Ewelina Młynarska, Jacek Rysz, Beata Franczyk
Biomedicines.2023; 11(10): 2611. CrossRef
- Diabetes: a review of its pathophysiology, and advanced methods of mitigation
Original Articles
- Basic Research
- Peroxisomal Fitness: A Potential Protective Mechanism of Fenofibrate against High Fat Diet-Induced Non-Alcoholic Fatty Liver Disease in Mice
- Songling Jiang, Md Jamal Uddin, Xiaoying Yu, Lingjuan Piao, Debra Dorotea, Goo Taeg Oh, Hunjoo Ha
- Diabetes Metab J. 2022;46(6):829-842. Published online June 24, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0274
- 4,905 View
- 292 Download
- 7 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Non-alcoholic fatty liver disease (NAFLD) has been increasing in association with the epidemic of obesity and diabetes. Peroxisomes are single membrane-enclosed organelles that play a role in the metabolism of lipid and reactive oxygen species. The present study examined the role of peroxisomes in high-fat diet (HFD)-induced NAFLD using fenofibrate, a peroxisome proliferator-activated receptor α (PPARα) agonist.
Methods
Eight-week-old male C57BL/6J mice were fed either a normal diet or HFD for 12 weeks, and fenofibrate (50 mg/kg/day) was orally administered along with the initiation of HFD.
Results
HFD-induced liver injury as measured by increased alanine aminotransferase, inflammation, oxidative stress, and lipid accumulation was effectively prevented by fenofibrate. Fenofibrate significantly increased the expression of peroxisomal genes and proteins involved in peroxisomal biogenesis and function. HFD-induced attenuation of peroxisomal fatty acid oxidation was also significantly restored by fenofibrate, demonstrating the functional significance of peroxisomal fatty acid oxidation. In Ppara deficient mice, fenofibrate failed to maintain peroxisomal biogenesis and function in HFD-induced liver injury.
Conclusion
The present data highlight the importance of PPARα-mediated peroxisomal fitness in the protective effect of fenofibrate against NAFLD. -
Citations
Citations to this article as recorded by- Pharmacological potential of ginseng and ginsenosides in nonalcoholic fatty liver disease and nonalcoholic steatohepatitis
Young-Su Yi
Journal of Ginseng Research.2024; 48(2): 122. CrossRef - Fenofibrate alleviates NAFLD by enhancing the PPARα/PGC-1α signaling pathway coupling mitochondrial function
Xuemei Wang, Jieying Wang, Cao Ying, Yuan Xing, Xuan Su, Ke Men
BMC Pharmacology and Toxicology.2024;[Epub] CrossRef - Role of Fenofibrate Use in Dyslipidemia and Related Comorbidities in the Asian Population: A Narrative Review
Chaicharn Deerochanawong, Sin Gon Kim, Yu-Cheng Chang
Diabetes & Metabolism Journal.2024; 48(2): 184. CrossRef - Current Therapeutical Approaches Targeting Lipid Metabolism in NAFLD
Manuela Vitulo, Elisa Gnodi, Giulia Rosini, Raffaella Meneveri, Roberto Giovannoni, Donatella Barisani
International Journal of Molecular Sciences.2023; 24(16): 12748. CrossRef - PPARα agonist fenofibrate prevents postoperative cognitive dysfunction by enhancing fatty acid oxidation in mice
Tiantian Liu, Xinlu Chen, Ziqi Wei, Xue Han, Yujia Liu, Zhengliang Ma, Tianjiao Xia, Xiaoping Gu
Translational Neuroscience.2023;[Epub] CrossRef - Fenofibrate enhances lipid deposition via modulating PPARγ, SREBP-1c, and gut microbiota in ob/ob mice fed a high-fat diet
Ying Zhang, Xiu-Bin Jia, Yun-Chao Liu, Wen-Qian Yu, Yan-Hong Si, Shou-Dong Guo
Frontiers in Nutrition.2022;[Epub] CrossRef
- Pharmacological potential of ginseng and ginsenosides in nonalcoholic fatty liver disease and nonalcoholic steatohepatitis
- Drug/Regimen
- Comparison of Serum Ketone Levels and Cardiometabolic Efficacy of Dapagliflozin versus Sitagliptin among Insulin-Treated Chinese Patients with Type 2 Diabetes Mellitus
- Chi-Ho Lee, Mei-Zhen Wu, David Tak-Wai Lui, Darren Shing-Hei Chan, Carol Ho-Yi Fong, Sammy Wing-Ming Shiu, Ying Wong, Alan Chun-Hong Lee, Joanne King-Yan Lam, Yu-Cho Woo, Karen Siu-Ling Lam, Kelvin Kai-Hang Yiu, Kathryn Choon-Beng Tan
- Diabetes Metab J. 2022;46(6):843-854. Published online April 28, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0319
- 4,992 View
- 257 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Insulin-treated patients with long duration of type 2 diabetes mellitus (T2DM) are at increased risk of ketoacidosis related to sodium-glucose co-transporter 2 inhibitor (SGLT2i). The extent of circulating ketone elevation in these patients remains unknown. We conducted this study to compare the serum ketone response between dapagliflozin, an SGLT2i, and sitagliptin, a dipeptidyl peptidase-4 inhibitor, among insulin-treated T2DM patients.
Methods
This was a randomized, open-label, active comparator-controlled study involving 60 insulin-treated T2DM patients. Participants were randomized 1:1 for 24-week of dapagliflozin 10 mg daily or sitagliptin 100 mg daily. Serum β-hydroxybutyrate (BHB) levels were measured at baseline, 12 and 24 weeks after intervention. Comprehensive cardiometabolic assessments were performed with measurements of high-density lipoprotein cholesterol (HDL-C) cholesterol efflux capacity (CEC), vibration-controlled transient elastography and echocardiography.
Results
Among these 60 insulin-treated participants (mean age 58.8 years, diabetes duration 18.2 years, glycosylated hemoglobin 8.87%), as compared with sitagliptin, serum BHB levels increased significantly after 24 weeks of dapagliflozin (P=0.045), with a median of 27% increase from baseline. Change in serum BHB levels correlated significantly with change in free fatty acid levels. Despite similar glucose lowering, dapagliflozin led to significant improvements in body weight (P=0.006), waist circumference (P=0.028), HDL-C (P=0.041), CEC (P=0.045), controlled attenuation parameter (P=0.007), and liver stiffness (P=0.022). Average E/e’, an echocardiographic index of left ventricular diastolic dysfunction, was also significantly lower at 24 weeks in participants treated with dapagliflozin (P=0.037).
Conclusion
Among insulin-treated T2DM patients with long diabetes duration, compared to sitagliptin, dapagliflozin modestly increased ketone levels and was associated with cardiometabolic benefits. -
Citations
Citations to this article as recorded by- Serum thrombospondin‐2 level changes with liver stiffness improvement in patients with type 2 diabetes
Jimmy Ho Cheung Mak, David Tak‐Wai Lui, Carol Ho‐Yi Fong, Chloe Yu‐Yan Cheung, Ying Wong, Alan Chun‐Hong Lee, Ruby Lai‐Chong Hoo, Aimin Xu, Kathryn Choon‐Beng Tan, Karen Siu‐Ling Lam, Chi‐Ho Lee
Clinical Endocrinology.2024; 100(3): 230. CrossRef - SGLT-2 inhibitors as novel treatments of multiple organ fibrosis
Junpei Hu, Jianhui Teng, Shan Hui, Lihui Liang
Heliyon.2024; 10(8): e29486. CrossRef - Effect of sodium-glucose cotransporter protein-2 inhibitors on left ventricular hypertrophy in patients with type 2 diabetes: A systematic review and meta-analysis
Yao Wang, Yujie Zhong, Zhehao Zhang, Shuhao Yang, Qianying Zhang, Bingyang Chu, Xulin Hu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Effects of SGLT2 inhibitors on hepatic fibrosis and steatosis: A systematic review and meta-analysis
Peipei Zhou, Ying Tan, Zhenning Hao, Weilong Xu, Xiqiao Zhou, Jiangyi Yu
Frontiers in Endocrinology.2023;[Epub] CrossRef - The impact of sodium-glucose Cotransporter-2 inhibitors on lipid profile: A meta-analysis of 28 randomized controlled trials
Gang Fan, Dian long Guo, Hong Zuo
European Journal of Pharmacology.2023; 959: 176087. CrossRef
- Serum thrombospondin‐2 level changes with liver stiffness improvement in patients with type 2 diabetes
- Drug/Regimen
- A Real-World Study of Long-Term Safety and Efficacy of Lobeglitazone in Korean Patients with Type 2 Diabetes Mellitus
- Bo-Yeon Kim, Hyuk-Sang Kwon, Suk Kyeong Kim, Jung-Hyun Noh, Cheol-Young Park, Hyeong-Kyu Park, Kee-Ho Song, Jong Chul Won, Jae Myung Yu, Mi Young Lee, Jae Hyuk Lee, Soo Lim, Sung Wan Chun, In-Kyung Jeong, Choon Hee Chung, Seung Jin Han, Hee-Seok Kim, Ju-Young Min, Sungrae Kim
- Diabetes Metab J. 2022;46(6):855-865. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0264
- 6,690 View
- 296 Download
- 6 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Thiazolidinediones (TZDs) have been associated with various safety concerns including weight gain, bladder cancer, and congestive heart failure (CHF). This study evaluated the efficacy and safety of lobeglitazone, a novel TZD in patients with type 2 diabetes mellitus (T2DM) in real practice.
Methods
In this non-interventional, multi-center, retrospective, and observational study conducted at 15 tertiary or secondary referral hospitals in Korea, a total of 2,228 patients with T2DM who received lobeglitazone 0.5 mg for more than 1 year were enrolled.
Results
Overall adverse events (AEs) occurred in 381 patients (17.10%) including edema in 1.97% (n=44). Cerebrovascular and cardiovascular diseases were identified in 0.81% (n=18) and 0.81% (n=18), respectively. One case of CHF was reported as an AE. Edema occurred in 1.97% (n=44) of patients. Hypoglycemia occurred in 2.47% (n=55) of patients. Fracture occurred in 1.17% (n=26) of all patients. Lobeglitazone significantly decreased HbA1c level, resulting in a mean treatment difference of -1.05%± 1.35% (P<0.001), and decreased total cholesterol, triglyceride, and low-density lipoprotein cholesterol. However, it increased high-density lipoprotein cholesterol, regardless of statin administration. The patients who received lobeglitazone 0.5 mg showed an apparent reduction in glycosylated hemoglobin (HbA1c) from baseline during the first 6 months of treatment. The HbA1c levels remained stable between months 6 and 42.
Conclusion
Lobeglitazone has long-term safety profile, good glycemic-lowering effect and long-term durability of glycemic control in real-world clinical settings. -
Citations
Citations to this article as recorded by- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
Deep Dutta, Saptarshi Bhattacharya, Manoj Kumar, Priyankar K. Datta, Ritin Mohindra, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102697. CrossRef - Efficacy and safety of lobeglitazone, a new Thiazolidinedione, as compared to the standard of care in type 2 diabetes mellitus: A systematic review and meta-analysis
Shashank R. Joshi, Saibal Das, Suja Xaviar, Shambo Samrat Samajdar, Indranil Saha, Sougata Sarkar, Shatavisa Mukherjee, Santanu Kumar Tripathi, Jyotirmoy Pal, Nandini Chatterjee
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102703. CrossRef - Will lobeglitazone rival pioglitazone? A systematic review and critical appraisal
Kalyan Kumar Gangopadhyay, Awadhesh Kumar Singh
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(4): 102747. CrossRef - Lobeglitazone
Reactions Weekly.2023; 1948(1): 262. CrossRef - Lobeglitazone, a novel thiazolidinedione, for secondary prevention in patients with ischemic stroke: a nationwide nested case-control study
Joonsang Yoo, Jimin Jeon, Minyoul Baik, Jinkwon Kim
Cardiovascular Diabetology.2023;[Epub] CrossRef - Lobeglitazone and Its Therapeutic Benefits: A Review
Balamurugan M, Sarumathy S, Robinson R
Cureus.2023;[Epub] CrossRef - Oldies but Goodies: Thiazolidinedione as an Insulin Sensitizer with Cardioprotection
Eun-Hee Cho
Diabetes & Metabolism Journal.2022; 46(6): 827. CrossRef
- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
- Type 1 Diabetes
- Abnormal Responses in Cognitive Impulsivity Circuits Are Associated with Glycosylated Hemoglobin Trajectories in Type 1 Diabetes Mellitus and Impaired Metabolic Control
- Helena Jorge, Isabel C. Duarte, Sandra Paiva, Ana Paula Relvas, Miguel Castelo-Branco
- Diabetes Metab J. 2022;46(6):866-878. Published online March 22, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0307
- 4,391 View
- 173 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Risky health decisions and impulse control profiles may impact on metabolic control in type 1 diabetes mellitus (T1DM). We hypothesize that the neural correlates of cognitive impulsivity and decision-making in T1DM relate to metabolic control trajectories.
Methods
We combined functional magnetic resonance imaging (fMRI), measures of metabolic trajectories (glycosylated hemoglobin [HbA1c] over multiple time points) and behavioral assessment using a cognitive impulsivity paradigm, the Balloon Analogue Risk Task (BART), in 50 participants (25 T1DM and 25 controls).
Results
Behavioral results showed that T1DM participants followed a rigid conservative risk strategy along the iterative game. Imaging group comparisons showed that patients showed larger activation of reward related, limbic regions (nucleus accumbens, amygdala) and insula (interoceptive saliency network) in initial game stages. Upon game completion differences emerged in relation to error monitoring (anterior cingulate cortex [ACC]) and inhibitory control (inferior frontal gyrus). Importantly, activity in the saliency network (ACC and insula), which monitors interoceptive states, was related with metabolic trajectories, which was also found for limbic/reward networks. Parietal and posterior cingulate regions activated both in controls and patients with adaptive decision-making, and positively associated with metabolic trajectories.
Conclusion
We found triple converging evidence when comparing metabolic trajectories, patients versus controls or risk averse (non-learners) versus patients who learned by trial and error. Dopaminergic reward and saliency (interoceptive and error monitoring) circuits show a tight link with impaired metabolic trajectories and cognitive impulsivity in T1DM. Activity in parietal and posterior cingulate are associated with adaptive trajectories. This link between reward-saliency-inhibition circuits suggests novel strategies for patient management. -
Citations
Citations to this article as recorded by- The usefulness of an intervention with a serious video game as a complementary approach to cognitive behavioural therapy in eating disorders: A pilot randomized clinical trial for impulsivity management
Cristina Vintró‐Alcaraz, Núria Mallorquí‐Bagué, María Lozano‐Madrid, Giulia Testa, Roser Granero, Isabel Sánchez, Janet Treasure, Susana Jiménez‐Murcia, Fernando Fernández‐Aranda
European Eating Disorders Review.2023; 31(6): 781. CrossRef - Adaptations of the balloon analog risk task for neuroimaging settings: a systematic review
Charline Compagne, Juliana Teti Mayer, Damien Gabriel, Alexandre Comte, Eloi Magnin, Djamila Bennabi, Thomas Tannou
Frontiers in Neuroscience.2023;[Epub] CrossRef - Trust-based health decision-making recruits the neural interoceptive saliency network which relates to temporal trajectories of Hemoglobin A1C in Diabetes Type 1
Helena Jorge, Isabel C. Duarte, Miguel Melo, Ana Paula Relvas, Miguel Castelo-Branco
Brain Imaging and Behavior.2023; 18(1): 171. CrossRef
- The usefulness of an intervention with a serious video game as a complementary approach to cognitive behavioural therapy in eating disorders: A pilot randomized clinical trial for impulsivity management
- Metabolic Risk/Epidemiology
- Sex Differences in the Effects of CDKAL1 Variants on Glycemic Control in Diabetic Patients: Findings from the Korean Genome and Epidemiology Study
- Hye Ah Lee, Hyesook Park, Young Sun Hong
- Diabetes Metab J. 2022;46(6):879-889. Published online February 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0265
- 65,535 View
- 178 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Using long-term data from the Korean Genome and Epidemiology Study, we defined poor glycemic control and investigated possible risk factors, including variants related to type 2 diabetes mellitus (T2DM). In addition, we evaluated interaction effects among risk factors for poor glycemic control.
Methods
Among 436 subjects with newly diagnosed diabetes, poor glycemic control was defined based on glycosylated hemoglobin trajectory patterns by group-based trajectory modeling. For the variants related to T2DM, genetic risk scores (GRSs) were calculated and divided into quartiles. Risk factors for poor glycemic control were assessed using a logistic regression model.
Results
Of the subjects, 43% were in the poor-glycemic-control group. Body mass index (BMI) and triglyceride (TG) were associated with poor glycemic control. The risk for poor glycemic control increased by 11.0% per 1 kg/m2 increase in BMI and by 3.0% per 10 mg/dL increase in TG. The risk for GRS with poor glycemic control was sex-dependent (Pinteraction=0.07), and a relationship by GRS quartiles was found in females but not in males. Moreover, the interaction effect was found to be significant on both additive and multiplicative scales. The interaction effect was evident in the variants of cyclin-dependent kinase 5 regulatory subunit-associated protein 1-like (CDKAL1).
Conclusion
Females with risk alleles of variants in CDKAL1 associated with T2DM had a higher risk for poor glycemic control than males. -
Citations
Citations to this article as recorded by- Hepatic Cdkal1 deletion regulates HDL catabolism and promotes reverse cholesterol transport
Dan Bi An, Soo-jin Ann, Seungmin Seok, Yura Kang, Sang-Hak Lee
Atherosclerosis.2023; 375: 21. CrossRef
- Hepatic Cdkal1 deletion regulates HDL catabolism and promotes reverse cholesterol transport
- Metabolic Risk/Epidemiology
- Higher Muscle Mass Protects Women with Gestational Diabetes Mellitus from Progression to Type 2 Diabetes Mellitus
- Yujin Shin, Joon Ho Moon, Tae Jung Oh, Chang Ho Ahn, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
- Diabetes Metab J. 2022;46(6):890-900. Published online April 28, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0334
- 4,742 View
- 228 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We evaluated whether postpartum muscle mass affects the risk of type 2 diabetes mellitus (T2DM) in Korean women with gestational diabetes mellitus (GDM).
Methods
A total of 305 women with GDM (mean age, 34.9 years) was prospectively evaluated for incident prediabetes and T2DM from 2 months after delivery and annually thereafter. Appendicular skeletal muscle mass (ASM) was assessed with bioelectrical impedance analysis at the initial postpartum visit, and ASM, either divided by body mass index (BMI) or squared height, and the absolute ASM were used as muscle mass indices. The risk of incident prediabetes and T2DM was assessed according to tertiles of these indices using a logistic regression model.
Results
After a mean follow-up duration of 3.3 years, the highest ASM/BMI tertile group had a 61% lower risk of incident prediabetes and T2DM compared to the lowest tertile group, and this remained significant after we adjusted for covariates (adjusted odds ratio, 0.37; 95% confidence interval [CI], 0.15 to 0.92; P=0.032). Equivalent findings were observed in normal weight women (BMI <23 kg/m2), but this association was not significant for overweight women (BMI ≥23 kg/m2). Absolute ASM or ASM/height2 was not associated with the risk of postpartum T2DM.
Conclusion
A higher muscle mass, as defined by the ASM/BMI index, was associated with a lower risk of postpartum prediabetes and T2DM in Korean women with GDM. -
Citations
Citations to this article as recorded by- More appendicular lean mass relative to body mass index is associated with lower incident diabetes in middle-aged adults in the CARDIA study
Melanie S. Haines, Aaron Leong, Bianca C. Porneala, Victor W. Zhong, Cora E. Lewis, Pamela J. Schreiner, Karen K. Miller, James B. Meigs, Mercedes R. Carnethon
Nutrition, Metabolism and Cardiovascular Diseases.2023; 33(1): 105. CrossRef - The Association of the Triglyceride and Muscle to Fat Ratio During Early Pregnancy with the Development of Gestational Diabetes Mellitus
Fang Wang, Yuan-Yuan Bao, Kang Yu
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 3187. CrossRef - Correlation of body composition in early pregnancy on gestational diabetes mellitus under different body weights before pregnancy
Li Xintong, Xu Dongmei, Zhang Li, Cao Ruimin, Hao Yide, Cui Lingling, Chen Tingting, Guo Yingying, Li Jiaxin
Frontiers in Endocrinology.2022;[Epub] CrossRef
- More appendicular lean mass relative to body mass index is associated with lower incident diabetes in middle-aged adults in the CARDIA study
- Complications
- Effect of the Glucagon-Like Peptide-1 Receptor Agonists on Autonomic Function in Subjects with Diabetes: A Systematic Review and Meta-Analysis
- Carla Greco, Daniele Santi, Giulia Brigante, Chiara Pacchioni, Manuela Simoni
- Diabetes Metab J. 2022;46(6):901-911. Published online April 12, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0314
- 4,468 View
- 266 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
In addition to the metabolic effects in diabetes, glucagon-like peptide 1 receptor (GLP-1R) agonists lead to a small but substantial increase in heart rate (HR). However, the GLP-1R actions on the autonomic nervous system (ANS) in diabetes remain debated. Therefore, this meta-analysis evaluates the effect of GLP-1R agonist on measures of ANS function in diabetes.
Methods
According to the Cochrane Collaboration and Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement, we conducted a meta-analysis considering clinical trials in which the autonomic function was evaluated in diabetic subjects chronically treated with GLP-1R agonists. The outcomes were the change of ANS function measured by heart rate variability (HRV) and cardiac autonomic reflex tests (CARTs).
Results
In the studies enrolled, HR significantly increased after treatment (P<0.001), whereas low frequency/high frequency ratio did not differ (P=0.410); no changes in other measures of HRV were detected. Considering CARTs, only the 30:15 value derived from lying-to-standing test was significantly lower after treatment (P=0.002), but only two studies reported this measurement. No differences in other CARTs outcome were observed.
Conclusion
The meta-analysis confirms the HR increase but seems to exclude an alteration of the sympatho-vagal balance due to chronic treatment with GLP-1R agonists in diabetes, considering the available measures of ANS function. -
Citations
Citations to this article as recorded by- Liraglutide does not increase heart rate of diabetic patients during acute myocardial infarction
Qianyi Li, Chunxuan Wu, Shiqun Sun, Lingchao Yang, Yanyan Li, Yixin Niu, Li Zhang, Wei Li, Ying Yu
Journal of Diabetes.2024;[Epub] CrossRef - Hormonal Gut–Brain Signaling for the Treatment of Obesity
Eun Roh, Kyung Mook Choi
International Journal of Molecular Sciences.2023; 24(4): 3384. CrossRef - Effects of new hypoglycemic drugs on cardiac remodeling: a systematic review and network meta-analysis
Yi-lin Huang, Xiao-zhuo Xu, Jing Liu, Pin-yao Wang, Xue-li Wang, Hong-lin Feng, Cheng-jiang Liu, Xu Han
BMC Cardiovascular Disorders.2023;[Epub] CrossRef - Obesity and hypertension: Obesity medicine association (OMA) clinical practice statement (CPS) 2023
Tiffany Lowe Clayton, Angela Fitch, Harold Edward Bays
Obesity Pillars.2023; 8: 100083. CrossRef - Incretins and microvascular complications of diabetes: neuropathy, nephropathy, retinopathy and microangiopathy
Jonathan Goldney, Jack A. Sargeant, Melanie J. Davies
Diabetologia.2023; 66(10): 1832. CrossRef - Diabetes-Induced Cardiac Autonomic Neuropathy: Impact on Heart Function and Prognosis
Susumu Z. Sudo, Tadeu L. Montagnoli, Bruna de S. Rocha, Aimeé D. Santos, Mauro P. L. de Sá, Gisele Zapata-Sudo
Biomedicines.2022; 10(12): 3258. CrossRef
- Liraglutide does not increase heart rate of diabetic patients during acute myocardial infarction
- Others
- Influence of Maternal Diabetes on the Risk of Neurodevelopmental Disorders in Offspring in the Prenatal and Postnatal Periods
- Verónica Perea, Xavier Urquizu, Maite Valverde, Marina Macias, Anna Carmona, Esther Esteve, Gemma Escribano, Nuria Pons, Oriol Giménez, Teresa Gironés, Andreu Simó-Servat, Andrea Domenech, Núria Alonso-Carril, Carme Quirós, Antonio J. Amor, Eva López, Maria José Barahona
- Diabetes Metab J. 2022;46(6):912-922. Published online April 29, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0340
- 4,804 View
- 249 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study aimed to evaluate the influence of maternal diabetes in the risk of neurodevelopmental disorders in offspring in the prenatal and postnatal periods.
Methods
This cohort study included singleton gestational diabetes mellitus (GDM) pregnancies >22 weeks’ gestation with live newborns between 1991 and 2008. The control group was randomly selected and matched (1:2) for maternal age, weeks of gestation and birth year. Cox regression models estimated the effect of GDM on the risk of attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder (ASD), and maternal type 2 diabetes mellitus (T2DM). Moreover, interaction between maternal T2DM and GDM-ADHD relationship was evaluated.
Results
Children (n=3,123) were included (1,073 GDM; 2,050 control group). The median follow-up was 18.2 years (interquartile range, 14.2 to 22.3) (n=323 with ADHD, n=36 with ASD, and n=275 from women who developed T2DM). GDM exposure was associated with ADHD (hazard ratio [HR]crude, 1.67; 95% confidence interval [CI], 1.33 to 2.07) (HRadjusted, 1.64; 95% CI, 1.31 to 2.05). This association remained significant regardless of the treatment (diet or insulin) and diagnosis after 26 weeks of gestation. Children of mothers who developed T2DM presented higher rates of ADHD (14.2 vs. 10%, P=0.029). However, no interaction was found when T2DM was included in the GDM and ADHD models (P>0.05). GDM was not associated with an increased risk of ASD (HRadjusted, 1.46; 95% CI, 0.74 to 2.84).
Conclusion
Prenatal exposure to GDM increases the risk of ADHD in offspring, regardless of GDM treatment complexity. However, postnatal exposure to maternal T2DM was not related to the development of ADHD. -
Citations
Citations to this article as recorded by- Effects of a Diabetic Microenvironment on Neurodegeneration: Special Focus on Neurological Cells
Vishal Chavda, Dhananjay Yadav, Snehal Patel, Minseok Song
Brain Sciences.2024; 14(3): 284. CrossRef - Maternal Diabetes Deregulates the Expression of Mecp2 via miR-26b-5p in Mouse Embryonic Neural Stem Cells
Sukanya Shyamasundar, Seshadri Ramya, Deepika Kandilya, Dinesh Kumar Srinivasan, Boon Huat Bay, Suraiya Anjum Ansari, S Thameem Dheen
Cells.2023; 12(11): 1516. CrossRef - Evaluating the prospects of using gestational diabetes mellitus model to find means of pharmacological correction of the disorders in rat offspring
A. S. Solomina, A. V. Rodina, K. S. Kachalov, A. D. Zakharov, A. D. Durnev
Pharmacokinetics and Pharmacodynamics.2023; (2): 45. CrossRef - Hair and cord blood element levels and their relationship with air pollution, dietary intake, gestational diabetes mellitus, and infant neurodevelopment
Yin-Yin Xia, Jamie V. de Seymour, Xiao-Jia Yang, Lin-Wei Zhou, Yue Liu, Yang Yang, Kathryn L. Beck, Cathryn A. Conlon, Toby Mansell, Boris Novakovic, Richard Saffery, Ting-Li Han, Hua Zhang, Philip N. Baker
Clinical Nutrition.2023; 42(10): 1875. CrossRef - Role of Excessive Weight Gain During Gestation in the Risk of ADHD in Offspring of Women With Gestational Diabetes
Verónica Perea, Andreu Simó-Servat, Carmen Quirós, Nuria Alonso-Carril, Maite Valverde, Xavier Urquizu, Antonio J Amor, Eva López, Maria-José Barahona
The Journal of Clinical Endocrinology & Metabolism.2022; 107(10): e4203. CrossRef
- Effects of a Diabetic Microenvironment on Neurodegeneration: Special Focus on Neurological Cells
- Others
- Fasting Glucose Variability and the Risk of Dementia in Individuals with Diabetes: A Nationwide Cohort Study
- Da Young Lee, Jaeyoung Kim, Sanghyun Park, So Young Park, Ji Hee Yu, Ji A Seo, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Kyungdo Han, Nan Hee Kim
- Diabetes Metab J. 2022;46(6):923-935. Published online May 24, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0346
- 5,602 View
- 254 Download
- 6 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We investigated whether fasting glucose (FG) variability could predict the risk of dementia.
Methods
This cohort study analyzed data from Koreans with diabetes after at least three health examinations by the Korean National Health Insurance Corporation between 2005 and 2010, which included at least one examination between 2009 and 2010. A total of 769,554 individuals were included, excluding those aged <40 years and those with dementia. FG variability was measured using the variability independent of the mean (FG-VIM). The incidence of dementia was defined by the International Classification of Diseases 10th Revision codes and prescription of anti-dementia medication and was subdivided into Alzheimer’s disease (AD) and vascular dementia (VD).
Results
During the 6.9-year follow-up, 54,837, 41,032, and 6,892 cases of all-cause dementia, AD, and VD, respectively, were identified. Cox proportional regression analyses showed that as the FG-VIM quartile increased, the risk of dementia serially increased after adjustment for metabolic factors, income status, and diabetes-related characteristics, including the mean FG. Participants in FG-VIM quartile 4 showed a 18%, 19%, and 17% higher risk for all-cause dementia, AD, and VD, respectively, than those in quartile 1; this particularly included non-obese patients with a longer duration of diabetes, high FG levels, dyslipidemia, and those taking glucose-lowering medications. Conversely, the baseline FG status and dementia showed a U-shaped association.
Conclusion
Increased FG variability over 5 years can predict the risk of dementia in individuals with diabetes in Korea. This finding was more pronounced in patients with less favorable metabolic profiles. -
Citations
Citations to this article as recorded by- Fasting glucose variability and risk of dementia in Parkinson’s disease: a 9-year longitudinal follow-up study of a nationwide cohort
Sung Hoon Kang, Yunjin Choi, Su Jin Chung, Seok-Joo Moon, Chi Kyung Kim, Ji Hyun Kim, Kyungmi Oh, Joon Shik Yoon, Sang Won Seo, Geum Joon Cho, Seong-Beom Koh
Frontiers in Aging Neuroscience.2024;[Epub] CrossRef - Effects of a Diabetic Microenvironment on Neurodegeneration: Special Focus on Neurological Cells
Vishal Chavda, Dhananjay Yadav, Snehal Patel, Minseok Song
Brain Sciences.2024; 14(3): 284. CrossRef - The Association of Glucose Variability and Dementia Incidence in Latinx Adults with Type 2 Diabetes: A Retrospective Study
Heather Cuevas, Elizabeth Muñoz, Divya Nagireddy, Jeeyeon Kim, Grace Ganucheau, Fathia Alomoush
Clinical Nursing Research.2023; 32(2): 249. CrossRef - The effects of long-term cumulative HbA1c exposure on the development and onset time of dementia in the patients with type 2 diabetes mellitus: Hospital based retrospective study (2005–2021)
Sunyoung Cho, Choon Ok Kim, Bong-soo Cha, Eosu Kim, Chung Mo Nam, Min-Gul Kim, Min Soo Park
Diabetes Research and Clinical Practice.2023; 201: 110721. CrossRef - Physiological Mechanisms Inherent to Diabetes Involved in the Development of Dementia: Alzheimer’s Disease
Himan Mohamed-Mohamed, Victoria García-Morales, Encarnación María Sánchez Lara, Anabel González-Acedo, Teresa Pardo-Moreno, María Isabel Tovar-Gálvez, Lucía Melguizo-Rodríguez, Juan José Ramos-Rodríguez
Neurology International.2023; 15(4): 1253. CrossRef - Cumulative effect of impaired fasting glucose on the risk of dementia in middle-aged and elderly people: a nationwide cohort study
Jin Yu, Kyu-Na Lee, Hun-Sung Kim, Kyungdo Han, Seung-Hwan Lee
Scientific Reports.2023;[Epub] CrossRef
- Fasting glucose variability and risk of dementia in Parkinson’s disease: a 9-year longitudinal follow-up study of a nationwide cohort
Short Communications
- Technology/Device
- Comparison of Laser and Conventional Lancing Devices for Blood Glucose Measurement Conformance and Patient Satisfaction in Diabetes Mellitus
- Jung A Kim, Min Jeong Park, Eyun Song, Eun Roh, So Young Park, Da Young Lee, Jaeyoung Kim, Ji Hee Yu, Ji A Seo, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo, Nan Hee Kim
- Diabetes Metab J. 2022;46(6):936-940. Published online March 30, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0293
- 5,269 View
- 256 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Self-monitoring of capillary blood glucose is important for controlling diabetes. Recently, a laser lancing device (LMT-1000) that can collect capillary blood without skin puncture was developed. We enrolled 150 patients with type 1 or 2 diabetes mellitus. Blood sampling was performed on the same finger on each hand using the LMT-1000 or a conventional lancet. The primary outcome was correlation between glucose values using the LMT-1000 and that using a lancet. And we compared the pain and satisfaction of the procedures. The capillary blood sampling success rates with the LMT-1000 and lancet were 99.3% and 100%, respectively. There was a positive correlation (r=0.974, P<0.001) between mean blood glucose levels in the LMT-1000 (175.8±63.0 mg/dL) and conventional lancet samples (172.5±63.6 mg/dL). LMT-1000 reduced puncture pain by 75.0% and increased satisfaction by 80.0% compared to a lancet. We demonstrated considerable consistency in blood glucose measurements between samples from the LMT-1000 and a lancet, but improved satisfaction and clinically significant pain reduction were observed with the LMT-1000 compared to those with a lancet.
-
Citations
Citations to this article as recorded by- Comparison between a laser-lancing device and automatic incision lancet for capillary blood sampling from the heel of newborn infants: a randomized feasibility trial
Chul Kyu Yun, Eui Kyung Choi, Hyung Jin Kim, Jaeyoung Kim, Byung Cheol Park, Kyuhee Park, Byung Min Choi
Journal of Perinatology.2024;[Epub] CrossRef
- Comparison between a laser-lancing device and automatic incision lancet for capillary blood sampling from the heel of newborn infants: a randomized feasibility trial
- Technology/Device
- A 4-Week, Two-Center, Open-Label, Single-Arm Study to Evaluate the Safety and Efficacy of EOPatch in Well-Controlled Type 1 Diabetes Mellitus
- Jiyun Park, Nammi Park, Sangjin Han, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Woo Je Lee, Jae Hyeon Kim
- Diabetes Metab J. 2022;46(6):941-947. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0299
- 5,168 View
- 269 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - This study evaluated the safety and efficacy of tubeless patch pump called EOPatch in patients with well-controlled type 1 diabetes mellitus (T1DM). This 4-week, two-center, open-label, single-arm study enrolled 10 adult patients diagnosed with T1DM with glycosylated hemoglobin less than 7.5%. The co-primary end points were patch pump usage time for one attachment and number of serious adverse events related to the patch pump. The secondary end points were total amount of insulin injected per patch and changes in glycemic parameters including continuous glucose monitoring data compared to those at study entry. The median usage time per patch was 84.00 hours (interquartile range, 64.50 to 92.50). Serious adverse events did not occur during the trial. Four weeks later, time in range 70 to 180 mg/dL was significantly improved (70.71%±17.14 % vs. 82.96%±9.14%, P=0.01). The times spent below range (<54 mg/dL) and above range (>180 mg/dL) also improved (All P<0.05). Four-week treatment with a tubeless patch pump was safe and led to clinical improvement in glycemic control.
-
Citations
Citations to this article as recorded by- Multilayer track‐etched membrane‐based electroosmotic pump for drug delivery
Qian Yang, Zebo Zhang, Junshu Lin, Boyu Zhu, Rongying Yu, Xinru Li, Bin Su, Bo Zhao
ELECTROPHORESIS.2024; 45(5-6): 433. CrossRef - Comparison between a tubeless, on-body automated insulin delivery system and a tubeless, on-body sensor-augmented pump in type 1 diabetes: a multicentre randomised controlled trial
Ji Yoon Kim, Sang-Man Jin, Eun Seok Kang, Soo Heon Kwak, Yeoree Yang, Jee Hee Yoo, Jae Hyun Bae, Jun Sung Moon, Chang Hee Jung, Ji Cheol Bae, Sunghwan Suh, Sun Joon Moon, Sun Ok Song, Suk Chon, Jae Hyeon Kim
Diabetologia.2024;[Epub] CrossRef - A true continuous healthcare system for type 1 diabetes
Jiyong Kim, Salman Khan, Eun Kyu Kim, Hye-Jun Kil, Bo Min Kang, Hyo Geon Lee, Jin-Woo Park, Jun Young Yoon, Woochul Kim
Nano Energy.2023; 113: 108553. CrossRef
- Multilayer track‐etched membrane‐based electroosmotic pump for drug delivery
- Pathophysiology
- Glutamic Acid Decarboxylase and Tyrosine Phosphatase-Related Islet Antigen-2 Positivity among Children and Adolescents with Diabetes in Korea
- Ka Young Kim, Min Seung Kim, Yun Jeong Lee, Young Ah Lee, Seong Yong Lee, Choong Ho Shin, Jae Hyun Kim
- Diabetes Metab J. 2022;46(6):948-952. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0332
- 4,513 View
- 183 Download
- 3 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Autoantibodies against glutamic acid decarboxylase (GADA), tyrosine phosphatase-related islet antigen 2 (IA2A), insulin (INSA), and islet cells (ICA) are critical for determining the type of diabetes and management strategy in new-onset diabetes mellitus (NODM), but there have been few reports of all diabetes-associated autoantibody (DAA) in Korea. We retrospectively analyzed 193 patients with NODM aged 0 to 18 years who were followed at two tertiary centers in Korea (2017 to 2021). Patients with type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) were 93 (48.2%) and 100 (51.8%), respectively. In T1DM patients, the DAA positivity rate was 94.6%; prevalence of GADA, IA2A, INSA, and ICA was 71.0%, 71.0%, 31.2%, and 10.8%, respectively; and IA2A added 10.7% point autoantibody positivity (83.9% for GADA+INSA+ICA and 94.6% for GADA+INSA+ICA+IA2A). Among the patients with T2DM, 12 (12.0%) were positive for DAA, and all were positive for INSA. These findings suggest that DAA at diagnosis, especially GADA and IA2A, is useful for classifying diabetes in Korean children and adolescents.
-
Citations
Citations to this article as recorded by- Immune-Checkpoint Inhibitors-Induced Type 1 Diabetes Mellitus: From Its Molecular Mechanisms to Clinical Practice
Yun Kyung Cho, Chang Hee Jung
Diabetes & Metabolism Journal.2023; 47(6): 757. CrossRef - Diagnostic and Therapeutic Strategies of Type 2 Diabetes Mellitus in Youth
Hwa Young Kim, Jae Hyun Kim
The Ewha Medical Journal.2022;[Epub] CrossRef
- Immune-Checkpoint Inhibitors-Induced Type 1 Diabetes Mellitus: From Its Molecular Mechanisms to Clinical Practice
Letter
- Advanced Liver Fibrosis Is Associated with Chronic Kidney Disease in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2022;46:630-9)
- Ji Hye Huh
- Diabetes Metab J. 2022;46(6):953-955. Published online November 24, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0374
- [Original]
- 1,780 View
- 113 Download

 KDA
KDA


 First
First Prev
Prev





