
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Previous issues
- Page Path
- HOME > Browse > Previous issues
- Drug/Regimen
- The History of Insulin Therapy in Korea
- Jun Sung Moon, Jong Chul Won, Young Min Cho
- Diabetes Metab J. 2021;45(5):623-628. Published online September 30, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0171

- 4,039 View
- 136 Download
- 1 Web of Science
- 1 Crossref
- Drug/Regimen
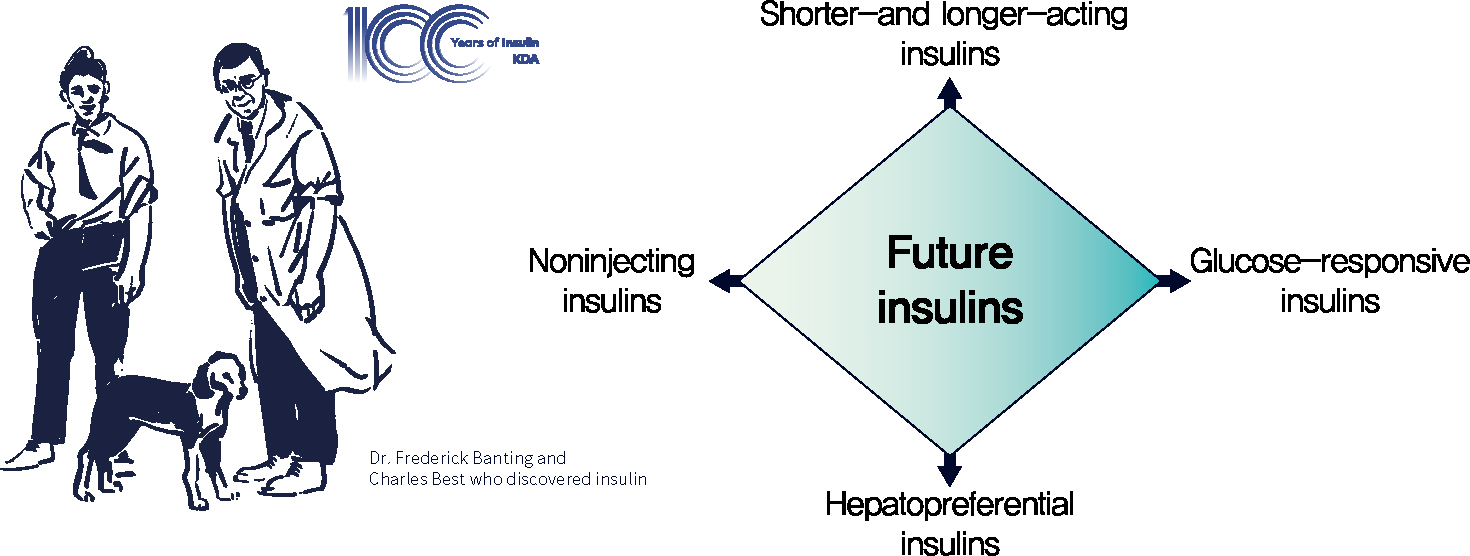
- A Century of Progress in Diabetes Care with Insulin: A History of Innovations and Foundation for the Future
- Seung-Hwan Lee, Kun-Ho Yoon
- Diabetes Metab J. 2021;45(5):629-640. Published online September 30, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0163
- 8,519 View
- 452 Download
- 13 Web of Science
- 15 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 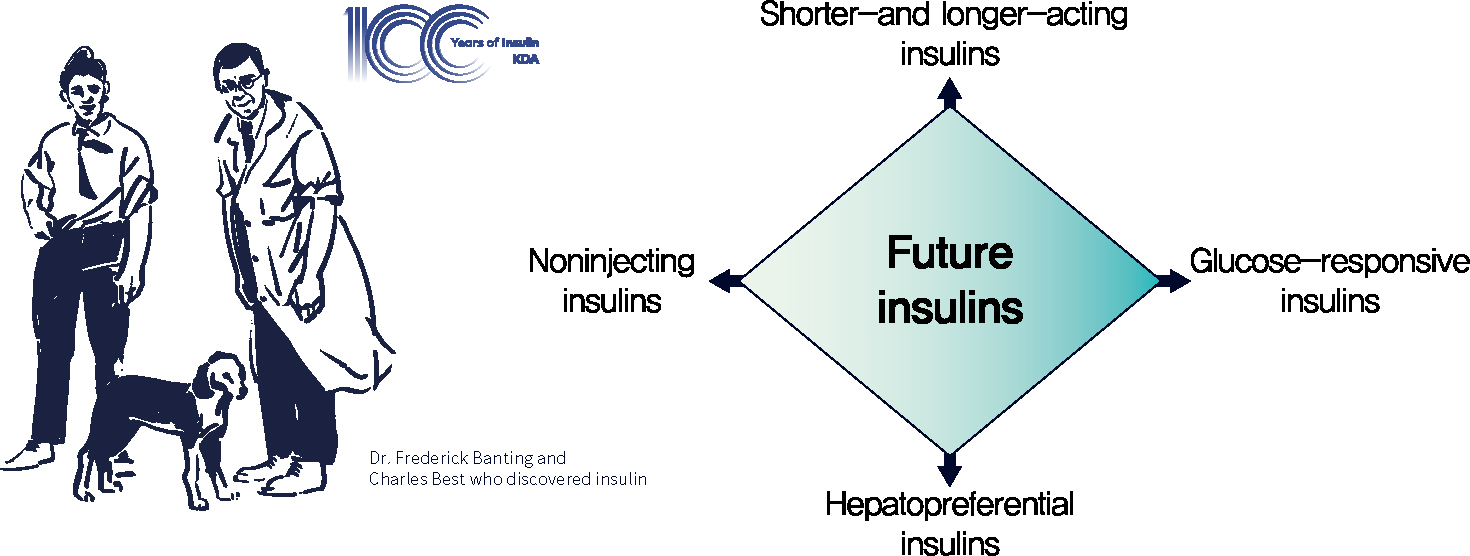
- The year 2021 marks the 100th anniversary of the discovery of insulin, which has greatly changed the lives of people with diabetes and become a cornerstone of advances in medical science. A rapid bench-to-bedside application of the lifesaving pancreatic extract and its immediate commercialization was the result of a promising idea, positive drive, perseverance, and collaboration of Banting and colleagues. As one of the very few proteins isolated in a pure form at that time, insulin also played a key role in the development of important methodologies and in the beginning of various fields of modern science. Since its discovery, insulin has evolved continuously to optimize the care of people with diabetes. Since the 1980s, recombinant DNA technology has been employed to engineer insulin analogs by modifying their amino acid sequence, which has resulted in the production of insulins with various profiles that are currently used. However, unmet needs in insulin treatment still exist, and several forms of future insulins are under development. In this review, we discuss the past, present, and future of insulin, including a history of ceaseless innovations and collective intelligence. We believe that this story will be a solid foundation and an unerring guide for the future.
-
Citations
Citations to this article as recorded by- Antidiabetic Potential of Phytochemicals Found in Vernonia amygdalina
Archna Talwar, Neha Chakraborty, Manaal Zahera, Shruti Anand, Irshad Ahmad, Samra Siddiqui, Avni Nayyar, Ashanul Haque, Mohd Saeed, Ponnurengam Malliappan Sivakumar
Journal of Chemistry.2024; 2024: 1. CrossRef - Insulin’s Legacy: A Century of Breakthroughs and Innovation
Somar Hadid, Emily Zhang, William H. Frishman, Erika Brutsaert
Cardiology in Review.2024;[Epub] CrossRef - Investigation on Quality Characteristics and Antidiabetic Properties of Mulberry Leaf Fu Brick Tea
Yuanyuan Shao, Ling Lin, Wei Xu, Zhihua Gong, Jinfeng Li, Jun Zhang, Xinpei Yan, Zhonghua Liu, Wenjun Xiao, Miguel Rebollo-Hernanz
Journal of Food Biochemistry.2024; 2024: 1. CrossRef - Prandial Insulins: A Person-Centered Choice
Bhawna Attri, Lakshmi Nagendra, Deep Dutta, Sahana Shetty, Shehla Shaikh, Sanjay Kalra, Saptarshi Bhattacharya
Current Diabetes Reports.2024;[Epub] CrossRef - Konjac Glucomannan: An Emerging Specialty Medical Food to Aid in the Treatment of Type 2 Diabetes Mellitus
Yimeng Fang, Jiahui Ma, Pengyu Lei, Lei Wang, Junying Qu, Jing Zhao, Fan Liu, Xiaoqing Yan, Wei Wu, Libo Jin, Hao Ji, Da Sun
Foods.2023; 12(2): 363. CrossRef - Glucose-Responsive Silk Fibroin Microneedles for Transdermal Delivery of Insulin
Guohongfang Tan, Fujian Jiang, Tianshuo Jia, Zhenzhen Qi, Tieling Xing, Subhas C. Kundu, Shenzhou Lu
Biomimetics.2023; 8(1): 50. CrossRef - Network pharmacology-based screening of the active ingredients and mechanisms of Cymbaria daurica against diabetes mellitus
Ruyu Shi, Dongxue Chen, Mingyue Ji, Baochang Zhou, Ziyan Zhang, Chunhong Zhang, Minhui Li
Food Science and Human Wellness.2023; 12(6): 2001. CrossRef - Type 1 Diabetes Overview and Perioperative Management
Grace B. Nelson, Kathryn M. Sumpter
Orthopedic Clinics of North America.2023; 54(3): 287. CrossRef - In Vitro BioTransformation (ivBT): Definitions, Opportunities, and Challenges
Yi-Heng P. Job Zhang, Zhiguang Zhu, Chun You, Lingling Zhang, Kuanqing Liu
Synthetic Biology and Engineering.2023; 1(2): 1. CrossRef - The effect of insulin analogs in people with type 1 diabetes at increased risk of severe hypoglycemia
Sofie Broeng-Mikkelgaard, Julie Maria Bøggild Brøsen, Peter Lommer Kristensen, Birger Thorsteinsson, Ulrik Pedersen-Bjergaard
Frontiers in Pharmacology.2023;[Epub] CrossRef - Biologic Medications: An Overview of Important Therapies in Children and Adolescents
Melissa S. Tesher
Pediatric Annals.2022;[Epub] CrossRef - A Sixty-Year Research and Development of Trichosanthin, a Ribosome-Inactivating Protein
Jia-Qi Lu, Kam-Bo Wong, Pang-Chui Shaw
Toxins.2022; 14(3): 178. CrossRef - Extra-Glycemic Effects of Anti-Diabetic Medications: Two Birds with One Stone?
Eun-Jung Rhee
Endocrinology and Metabolism.2022; 37(3): 415. CrossRef - Les biothérapies en pédiatrie
R. Duclaux-Loras, A. Belot
Perfectionnement en Pédiatrie.2022; 5(3): 193. CrossRef - Dynamic Detection of HbA1c Using a Silicon Nanowire Field Effect Tube Biosensor
Hang Chen, Lijuan Deng, Jialin Sun, Hang Li, Xiaoping Zhu, Tong Wang, Yanfeng Jiang
Biosensors.2022; 12(11): 916. CrossRef
- Antidiabetic Potential of Phytochemicals Found in Vernonia amygdalina
- Technology/Device
- Assessment of Insulin Secretion and Insulin Resistance in Human
- So Young Park, Jean-François Gautier, Suk Chon
- Diabetes Metab J. 2021;45(5):641-654. Published online September 30, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0220

- 14,124 View
- 878 Download
- 47 Web of Science
- 23 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 
- The impaired insulin secretion and increased insulin resistance (or decreased insulin sensitivity) play a major role in the pathogenesis of all types of diabetes mellitus (DM). It is very important to assess the pancreatic β-cell function and insulin resistance/ sensitivity to determine the type of DM and to plan an optimal management and prevention strategy for DM. So far, various methods and indices have been developed to assess the β-cell function and insulin resistance/sensitivity based on static, dynamic test and calculation of their results. In fact, since the metabolism of glucose and insulin is made through a complex process related with various stimuli in several tissues, it is difficult to fully reflect the real physiology. In order to solve the theoretical and practical difficulties, research on new index is still in progress. Also, it is important to select the appropriate method and index for the purpose of use and clinical situation. This review summarized a variety of traditional methods and indices to evaluate pancreatic β-cell function and insulin resistance/sensitivity and introduced novel indices.
-
Citations
Citations to this article as recorded by- Polyphenol-Rich Extract of Fermented Chili Pepper Alleviates Insulin Resistance in HepG2 Cells via Regulating INSR, PTP1B, PPAR-γ, and AMPK Pathways
Tao Wang, Meiqi Li, Shengbao Cai, Linyan Zhou, Xiaosong Hu, Junjie Yi
Fermentation.2023; 9(2): 84. CrossRef - 2,3-Dihydrosorbicillin and chrysopanol stimulate insulin secretion in INS-1 cells
Dahae Lee, Jaekyung Kim, Sungyoul Choi, Jinwon Choi, Jin Woo Lee, Ki Sung Kang, Sang Hee Shim
Bioorganic & Medicinal Chemistry Letters.2023; 83: 129186. CrossRef - Insulin: A connection between pancreatic β cells and the hypothalamus
Brenda De la Cruz Concepción, Yaccil Adilene Flores Cortez, Martha Isela Barragán Bonilla, Juan Miguel Mendoza Bello, Monica Espinoza Rojo
World Journal of Diabetes.2023; 14(2): 76. CrossRef - The Metabolic Score for Insulin Resistance (METS-IR) Predicts Cardiovascular Disease and Its Subtypes in Patients with Hypertension and Obstructive Sleep Apnea
Wenbo Yang, Xintian Cai, Junli Hu, Wen Wen, Heizhati Mulalibieke, Xiaoguang Yao, Ling Yao, Qing Zhu, Jing Hong, Qin Luo, Shasha Liu, Nanfang Li
Clinical Epidemiology.2023; Volume 15: 177. CrossRef - Association between dietary patterns and biomarkers in connection with diabetes mellitus in adolescents: A systematic review
Bernardo Paz Barboza, Camila Tureck, Liliana Paula Bricarello, Mariane de Almeida Alves, Anabelle Retondario, Amanda de Moura Souza, Ricardo Fernandes, Francisco de Assis Guedes de Vasconcelos
Nutrition, Metabolism and Cardiovascular Diseases.2023; 33(4): 685. CrossRef - PNPLA3 rs738409 risk genotype decouples TyG index from HOMA2-IR and intrahepatic lipid content
Ákos Nádasdi, Viktor Gál, Tamás Masszi, Anikó Somogyi, Gábor Firneisz
Cardiovascular Diabetology.2023;[Epub] CrossRef - Ethnic Variability in Glucose and Insulin Response to Rice Among Healthy Overweight Adults: A Randomized Cross-Over Study
Amena Sadiya, Vidya Jakapure, Vijay Kumar
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 993. CrossRef - Familial partial lipodystrophy type 2 and obesity, two adipose tissue pathologies with different inflammatory profiles
Guillaume Treiber, Marie-Paule Gonthier, Alice Guilleux, Samir Medjane, Oriane Bonfanti, Muriel Cogne, Olivier Meilhac, Estelle Nobecourt
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Discriminant Model for Insulin Resistance in Type 2 Diabetic Patients
Erislandis López-Galán, Rafael Barrio-Deler, Manuel Alejandro Fernández-Fernández, Yaquelin Del Toro-Delgado, Isaac Enrique Peñuela-Puente, Miguel Enrique Sánchez-Hechavarría, Mario Eugenio Muñoz-Bustos, Gustavo Alejandro Muñoz-Bustos
Medicina.2023; 59(5): 839. CrossRef - Mechanisms of Oxidative Stress in Metabolic Syndrome
Sepiso K. Masenga, Lombe S. Kabwe, Martin Chakulya, Annet Kirabo
International Journal of Molecular Sciences.2023; 24(9): 7898. CrossRef - Estimated Glucose Disposal Rate Predicts Renal Progression in Type 2 Diabetes Mellitus: A Retrospective Cohort Study
Juan Peng, Aimei Li, Liangqingqing Yin, Qi Yang, Jinting Pan, Bin Yi
Journal of the Endocrine Society.2023;[Epub] CrossRef - Transfer RNA Mutation Associated with Type 2 Diabetes Mellitus
Fanny Rizki Rahmadanthi, Iman Permana Maksum
Biology.2023; 12(6): 871. CrossRef - Honokiol improves endothelial function in type 2 diabetic rats via alleviating oxidative stress and insulin resistance
An He, Huilin Yu, Yu Hu, Huiling Chen, Xiang Li, Jian Shen, Rongjuan Zhuang, Yi Chen, Bryan Richard Sasmita, Minghao Luo, Dingyi Lv
Biochemical and Biophysical Research Communications.2022; 600: 109. CrossRef - Relationship of Vitamin A and Thyroid Function in Individuals With Obesity and After Laparoscopic Sleeve Gastrectomy
Bingwei Ma, Peng Yang, Jingyang Gao, Lei Du, Chunjun Sheng, Taofeek Usman, Xingchun Wang, Shen Qu
Frontiers in Nutrition.2022;[Epub] CrossRef - Efficacy of Personalized Diabetes Self-care Using an Electronic Medical Record–Integrated Mobile App in Patients With Type 2 Diabetes: 6-Month Randomized Controlled Trial
Eun Young Lee, Seon-Ah Cha, Jae-Seung Yun, Sun-Young Lim, Jin-Hee Lee, Yu-Bae Ahn, Kun-Ho Yoon, Min Kyung Hyun, Seung-Hyun Ko
Journal of Medical Internet Research.2022; 24(7): e37430. CrossRef - Acyclovir alleviates insulin resistance via activating PKM1 in diabetic mice
Zhuozhou Hu, Jing Zhou, Liang Han, Xiangxiang Li, Chun Li, Tongyu Wu, Jingjing Liu, Wenyang Zhao, Jia Kang, Xinping Chen
Life Sciences.2022; 304: 120725. CrossRef - Identifying Glucose Metabolism Status in Nondiabetic Japanese Adults Using Machine Learning Model with Simple Questionnaire
Tomoki Uchida, Takeshi Kanamori, Takanori Teramoto, Yuji Nonaka, Hiroki Tanaka, Satoshi Nakamura, Norihito Murayama, Rajesh Kaluri
Computational and Mathematical Methods in Medicine.2022; 2022: 1. CrossRef - Elevated triglyceride-glucose (TyG) index predicts impaired islet β-cell function: A hospital-based cross-sectional study
Zi Chen, Jie Wen
Frontiers in Endocrinology.2022;[Epub] CrossRef - Maternal Glycaemic and Insulinemic Status and Newborn DNA Methylation: Findings in Women With Overweight and Obesity
Marion Lecorguillé, Fionnuala M McAuliffe, Patrick J Twomey, Karien Viljoen, John Mehegan, Cecily C Kelleher, Matthew Suderman, Catherine M Phillips
The Journal of Clinical Endocrinology & Metabolism.2022; 108(1): 85. CrossRef - Acanthosis Nigricans: Pointer of Endocrine Entities
Andreea-Maria Radu, Mara Carsote, Mihai Cristian Dumitrascu, Florica Sandru
Diagnostics.2022; 12(10): 2519. CrossRef - Relationship between Insulin Resistance Risk Scales and Non-Alcoholic Fatty Liver Disease and Liver Fibrosis Scales in 219,477 Spanish Workers
José Ignacio Ramírez-Manent, Emilio Martínez-Almoyna, Carlos López, Carla Busquets-Cortés, Hilda González San Miguel, Ángel Arturo López-González
Metabolites.2022; 12(11): 1093. CrossRef - Investigation of Insulin Secretion in Glucose Tolerance Test by the Intake of Novel Imeglimin (Twymeeg)
Hiroshi BANDO, Hiroko OGAWA, Hirohisa URASAKI, Shinji NAGAHIRO, Hiroko URASAKI, Miwako NAKANISHI, Osami WATANABE
Asploro Journal of Biomedical and Clinical Case Reports.2022; 5(3): 113. CrossRef - Evaluation and Screening of Hypoglycemic Activity of Total Ginsenosides GBE-5 Fraction From Panax Ginseng Berry Based on UHPLC–MS Metabolomics
Heyu Wang, Yu Tong, Anqi Wang, Ying Li, Bofan Lu, Hui Li, Lili Jiao, Wei Wu
Frontiers in Nutrition.2022;[Epub] CrossRef
- Polyphenol-Rich Extract of Fermented Chili Pepper Alleviates Insulin Resistance in HepG2 Cells via Regulating INSR, PTP1B, PPAR-γ, and AMPK Pathways
- Pathophysiology
- Rho-Kinase as a Therapeutic Target for Nonalcoholic Fatty Liver Diseases
- Inês Sousa-Lima, Hyun Jeong Kim, John Jones, Young-Bum Kim
- Diabetes Metab J. 2021;45(5):655-674. Published online September 30, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0197
- 5,769 View
- 171 Download
- 7 Web of Science
- 7 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 
- Nonalcoholic fatty liver disease (NAFLD) is a major public health problem and the most common form of chronic liver disease, affecting 25% of the global population. Although NAFLD is closely linked with obesity, insulin resistance, and type 2 diabetes mellitus, knowledge on its pathogenesis remains incomplete. Emerging data have underscored the importance of Rho-kinase (Rho-associated coiled-coil-containing kinase [ROCK]) action in the maintenance of normal hepatic lipid homeostasis. In particular, pharmacological blockade of ROCK in hepatocytes or hepatic stellate cells prevents the progression of liver diseases such as NAFLD and fibrosis. Moreover, mice lacking hepatic ROCK1 are protected against obesity-induced fatty liver diseases by suppressing hepatic de novo lipogenesis. Here we review the roles of ROCK as an indispensable regulator of obesity-induced fatty liver disease and highlight the key cellular pathway governing hepatic lipid accumulation, with focus on de novo lipogenesis and its impact on therapeutic potential. Consequently, a comprehensive understanding of the metabolic milieu linking to liver dysfunction triggered by ROCK activation may help identify new targets for treating fatty liver diseases such as NAFLD.
-
Citations
Citations to this article as recorded by- THE ROLE OF N6-METHYLADENOSINE METHYLTRANSFERASE RBM15 IN NONALCOHOLIC FATTY LIVER DISEASE
Shiqing Li, Shengyi Lian, Wei Cheng, Tao Zhang, Xiaobing Gong
Shock.2024; 61(2): 311. CrossRef - Exploring the potential of drug repurposing for liver diseases: A comprehensive study
Fares E.M. Ali, Mustafa Ahmed Abdel-Reheim, Emad H.M. Hassanein, Mostafa K. Abd El-Aziz, Hanan S. Althagafy, Khalid S.A. Badran
Life Sciences.2024; : 122642. CrossRef - Targeting of G-protein coupled receptor 40 alleviates airway hyperresponsiveness through RhoA/ROCK1 signaling pathway in obese asthmatic mice
Xixi Lin, Like Wang, Xiaojie Lu, Yuanyuan Zhang, Rongying Zheng, Ruijie Chen, Weixi Zhang
Respiratory Research.2023;[Epub] CrossRef - Selectivity matters: selective ROCK2 inhibitor ameliorates established liver fibrosis via targeting inflammation, fibrosis, and metabolism
Alexandra Zanin-Zhorov, Wei Chen, Julien Moretti, Melanie S. Nyuydzefe, Iris Zhorov, Rashmi Munshi, Malavika Ghosh, Cindy Serdjebi, Kelli MacDonald, Bruce R. Blazar, Melissa Palmer, Samuel D. Waksal
Communications Biology.2023;[Epub] CrossRef - Insight Into Rho Kinase Isoforms in Obesity and Energy Homeostasis
Lei Wei, Jianjian Shi
Frontiers in Endocrinology.2022;[Epub] CrossRef - Paeoniflorin alleviates liver injury in hypercholesterolemic rats through the ROCK/AMPK pathway
Tong Liu, Ning Zhang, Lingya Kong, Sijie Chu, Ting Zhang, Guangdi Yan, Donglai Ma, Jun Dai, Zhihong Ma
Frontiers in Pharmacology.2022;[Epub] CrossRef - Fasudil Increased the Sensitivity to Gefitinib in NSCLC by Decreasing Intracellular Lipid Accumulation
Tingting Liao, Jingjing Deng, Wenjuan Chen, Juanjuan Xu, Guanghai Yang, Mei Zhou, Zhilei Lv, Sufei Wang, Siwei Song, Xueyun Tan, Zhengrong Yin, Yumei Li, Yang Jin
Cancers.2022; 14(19): 4709. CrossRef
- THE ROLE OF N6-METHYLADENOSINE METHYLTRANSFERASE RBM15 IN NONALCOHOLIC FATTY LIVER DISEASE
- Drug/Regimen
- Efficacy and Safety of Treatment with Quadruple Oral Hypoglycemic Agents in Uncontrolled Type 2 Diabetes Mellitus: A Multi-Center, Retrospective, Observational Study
- Jun Sung Moon, Sunghwan Suh, Sang Soo Kim, Heung Yong Jin, Jeong Mi Kim, Min Hee Jang, Kyung Ae Lee, Ju Hyung Lee, Seung Min Chung, Young Sang Lyu, Jin Hwa Kim, Sang Yong Kim, Jung Eun Jang, Tae Nyun Kim, Sung Woo Kim, Eonju Jeon, Nan Hee Cho, Mi-Kyung Kim, Hye Soon Kim, Il Seong Nam-Goong, Eun Sook Kim, Jin Ook Chung, Dong-Hyeok Cho, Chang Won Lee, Young Il Kim, Dong Jin Chung, Kyu Chang Won, In Joo Kim, Tae Sun Park, Duk Kyu Kim, Hosang Shon
- Diabetes Metab J. 2021;45(5):675-683. Published online August 12, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0107
- 35,343 View
- 367 Download
- 9 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 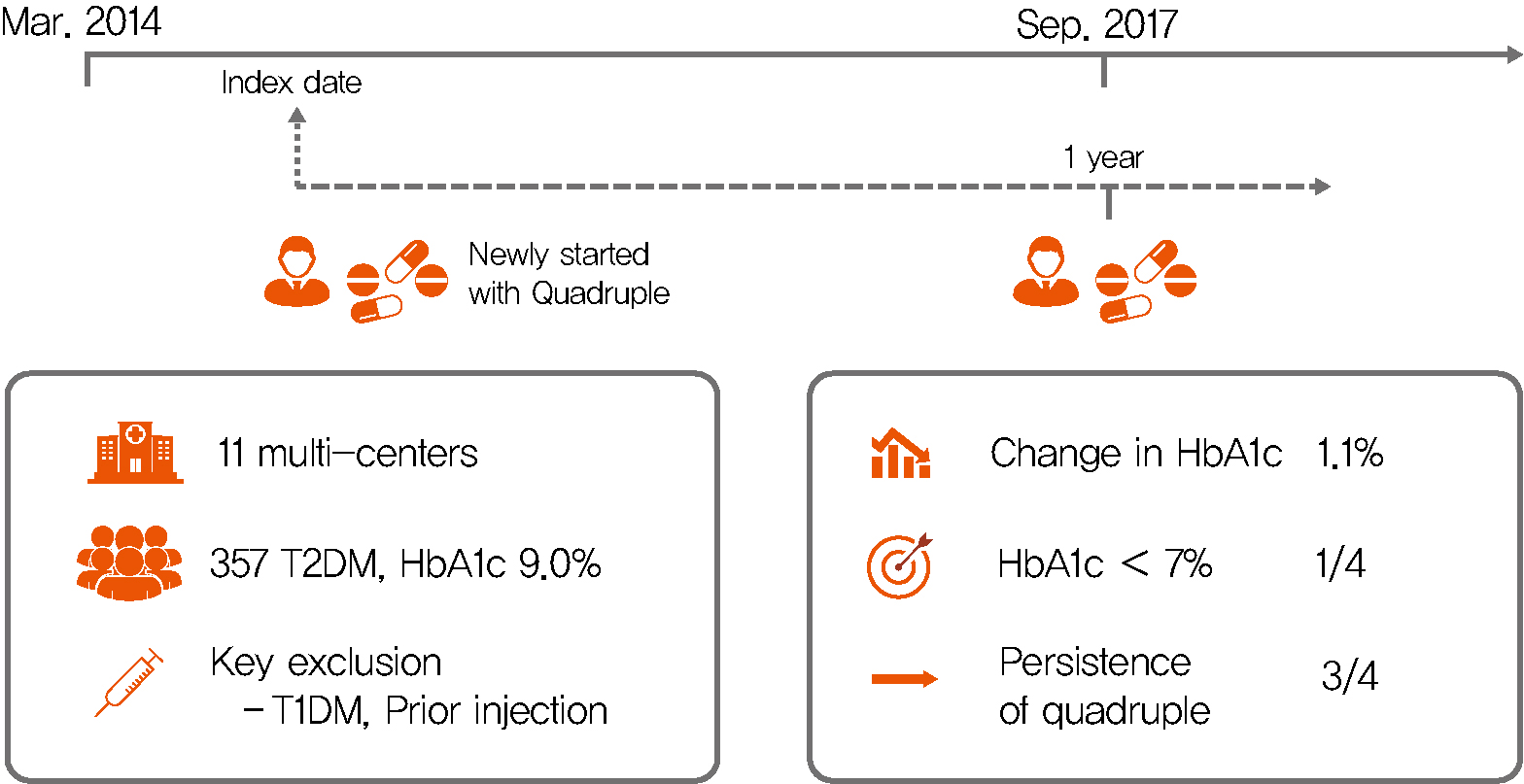
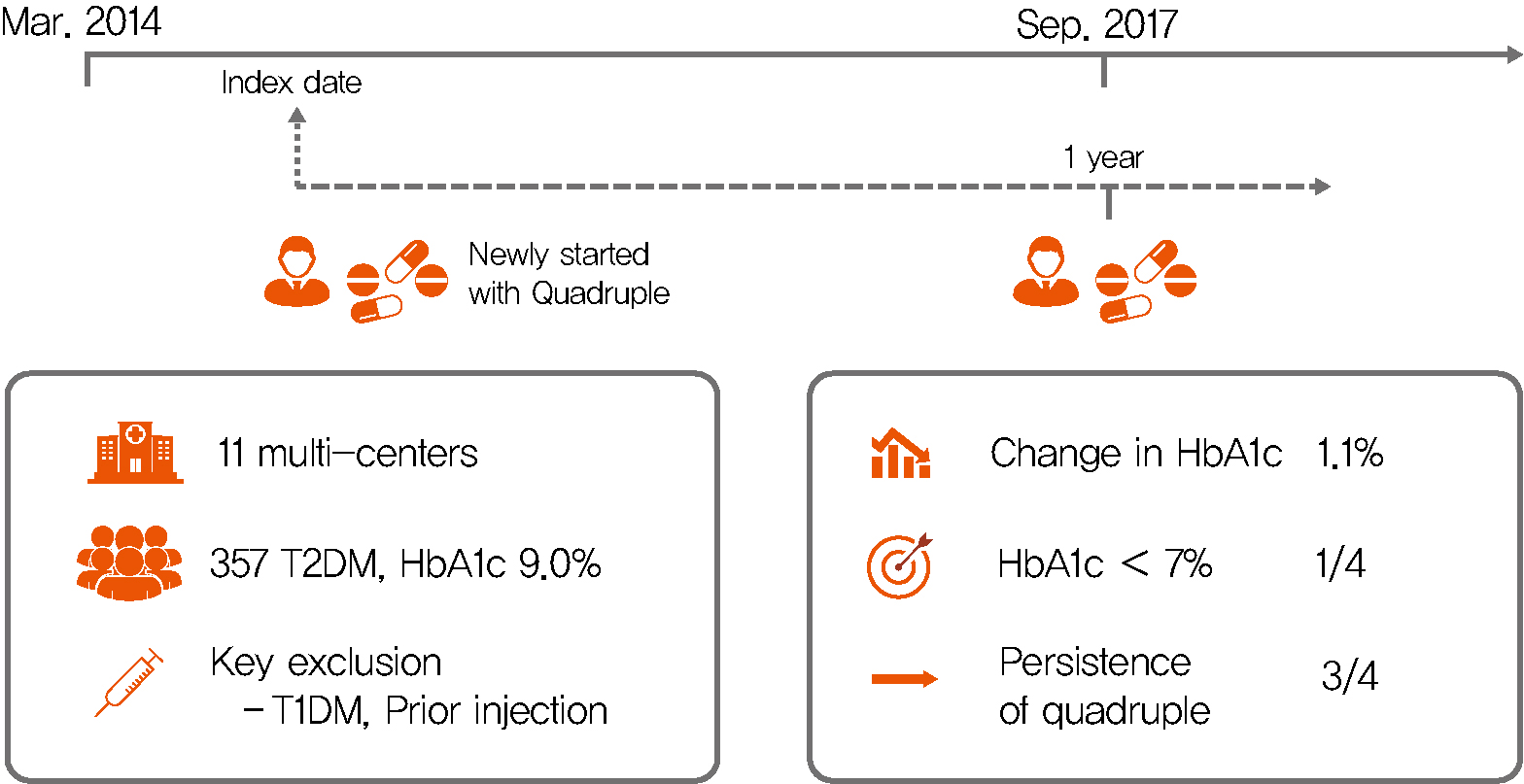
Background Only few studies have shown the efficacy and safety of glucose-control strategies using the quadruple drug combination. Therefore, the aim of the present study was to investigate the usefulness of the quadruple combination therapy with oral hypoglycemic agents (OHAs) in patients with uncontrolled type 2 diabetes mellitus (T2DM).
Methods From March 2014 to December 2018, data of patients with T2DM, who were treated with quadruple hypoglycemic medications for over 12 months in 11 hospitals in South Korea, were reviewed retrospectively. We compared glycosylated hemoglobin (HbA1c) levels before and 12 months after quadruple treatment with OHAs. The safety, maintenance rate, and therapeutic patterns after failure of the quadruple therapy were also evaluated.
Results In total, 357 patients were enrolled for quadruple OHA therapy, and the baseline HbA1c level was 9.0%±1.3% (74.9±14.1 mmol/mol). After 12 months, 270 patients (75.6%) adhered to the quadruple therapy and HbA1c was significantly reduced from 8.9%±1.2% to 7.8%±1.3% (mean change, −1.1%±1.2%;
P <0.001). The number of patients with HbA1c <7% increased significantly from 5 to 68 (P <0.005). In addition, lipid profiles and liver enzyme levels were also improved whereas no changes in body weight. There was no significant safety issue in patients treated with quadruple OHA therapy.Conclusion This study shows the therapeutic efficacy of the quadruple OHA regimen T2DM and demonstrates that it can be an option for the management of T2DM patients who cannot use insulin or reject injectable therapy.
-
Citations
Citations to this article as recorded by- Estimating Type 2 Diabetes Prevalence: A Model of Drug Consumption Data
Rita Oliveira, Matilde Monteiro-Soares, José Pedro Guerreiro, Rúben Pereira, António Teixeira-Rodrigues
Pharmacy.2024; 12(1): 18. CrossRef - Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
Kyung-Soo Kim, Kyung Ah Han, Tae Nyun Kim, Cheol-Young Park, Jung Hwan Park, Sang Yong Kim, Yong Hyun Kim, Kee Ho Song, Eun Seok Kang, Chul Sik Kim, Gwanpyo Koh, Jun Goo Kang, Mi Kyung Kim, Ji Min Han, Nan Hee Kim, Ji Oh Mok, Jae Hyuk Lee, Soo Lim, Sang S
Diabetes & Metabolism.2023; 49(4): 101440. CrossRef - Effectiveness and safety of teneligliptin added to patients with type 2 diabetes inadequately controlled by oral triple combination therapy: A multicentre, randomized, double‐blind, and placebo‐controlled study
Minyoung Lee, Woo‐je Lee, Jae Hyeon Kim, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2022; 24(6): 1105. CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - Glycaemic control with add‐on thiazolidinedione or a sodium‐glucose co‐transporter‐2 inhibitor in patients with type 2 diabetes after the failure of an oral triple antidiabetic regimen: A 24‐week, randomized controlled trial
Jaehyun Bae, Ji Hye Huh, Minyoung Lee, Yong‐Ho Lee, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2021; 23(2): 609. CrossRef
- Estimating Type 2 Diabetes Prevalence: A Model of Drug Consumption Data
- Complications
- High Incidence of Chronic Kidney Disease among Iranian Diabetic Adults: Using CKD-EPI and MDRD Equations for Estimated Glomerular Filtration Rate
- Seyyed Saeed Moazzeni, Reyhane Hizomi Arani, Mitra Hasheminia, Maryam Tohidi, Fereidoun Azizi, Farzad Hadaegh
- Diabetes Metab J. 2021;45(5):684-697. Published online March 16, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0109
- 5,821 View
- 157 Download
- 13 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To investigate the population based incidence rate of chronic kidney disease (CKD) and its potential risk factors among Iranian diabetic adults during over 14 years of follow-up.
Methods
Two different equations (Chronic Kidney Disease Epidemiology Collaboration [CKD-EPI] and Modification of Diet in Renal Disease [MDRD]) were applied for the calculating the estimated glomerular filtration rate (eGFR). Among a total of 1,374 diabetic Tehranian adults, 797 and 680 individuals were eligible for CKD-EPI and MDRD analyses, respectively. CKD was defined as eGFR lower than 60 mL/min/1.73 m2. Multivariable Cox proportional hazard models were used to estimate the hazard ratios (HRs) and 95% confidence intervals (CI) for all potential risk factors.
Results
The incidence rates (95% CI) of CKD per 1,000 person-years were 43.84 (39.49 to 48.66) and 55.80 (50.29 to 61.91) based on CKD-EPI and MDRD equations, respectively. Being older, a history of cardiovascular disease, and having lower levels of eGFR were significant risk factors in both equations. Moreover, in CKD-EPI, using glucose-lowering medications and hypertension, and in MDRD, female sex and fasting plasma glucose ≥10 mmol/L were also independent risk factors. Regarding the discrimination index, CKD-EPI equation showed a higher range of C-index for the predicted probability of incident CKD in the full-adjusted model, compared to MDRD equation (0.75 [0.72 to 0.77] vs. 0.69 [0.66 to 0.72]).
Conclusion
We found an incidence rate of more than 4%/year for CKD development among our Iranian diabetic population. Compared to MDRD, it can be suggested that CKD-EPI equation can be a better choice to use for prediction models of incident CKD among the Iranian diabetic populations. -
Citations
Citations to this article as recorded by- The Effect of the Holy Quran Recitation on Inflammatory Markers in Hemodialysis Patients in Iran: A Randomized Clinical Trial
Maedeh Teimourzadeh, Hassan Babamohamadi, Maliheh Yarmohamadi, Raheb Ghorbani, Harold G. Koenig
Journal of Religion and Health.2024;[Epub] CrossRef - Prevalence of anemia and its associated factors among patients with type 2 diabetes mellitus in a referral diabetic clinic in the north of Iran
Reyhane Hizomi Arani, Farima Fakhri, Mohammad Naeimi Tabiee, Fatemeh Talebi, Zahra Talebi, Negin Rashidi, Maryam Zahedi
BMC Endocrine Disorders.2023;[Epub] CrossRef - The association between fasting plasma glucose variability and incident eGFR decline: evidence from two cohort studies
Niloofar Deravi, Yasaman Sharifi, Fatemeh Koohi, Seyed Saeed Tamehri Zadeh, Soroush Masrouri, Fereidoun Azizi, Farzad Hadaegh
BMC Public Health.2023;[Epub] CrossRef - Low LncRNA LUCAT1 Expression Assists in the Diagnosis of Chronic Heart Failure and Predicts Poor Prognosis
Jian Wang, Xujin Wu, Li Wang, Chengyong Zhao
International Heart Journal.2023; 64(3): 409. CrossRef - Comparison of eGFR formulas (CKD-EPI and MDRD) in patients with multiple myeloma
Osman ERİNÇ, Soner YEŞİLYURT, Meliha NALCACİ
Cukurova Medical Journal.2023; 48(2): 336. CrossRef - Comparison and evaluation of the 2009 and 2021 chronic kidney disease-epidemiological collaboration equations among Jordanian patients with type 2 diabetes mellitus
Randa I. Farah, Abdulrahman Alhajahjeh, Oraib Al-farahid, Hana Abuzaid, Dana Hiasat, Rama Rayyan, Laith Bdier, Izzat AlAwwa, Kamel Ajlouni
Acta Diabetologica.2023; 61(2): 169. CrossRef - Effect of teaching health-promoting behaviors on the care burden of family caregivers of hemodialysis patients: a four-group clinical trial
Mehrdad Hayati, Razieh Bagherzadeh, Mehdi Mahmudpour, Fatemeh Heidari, Hakimeh Vahedparast
BMC Nursing.2023;[Epub] CrossRef - Impact of social and clinical factors on the diagnostic delay of chronic kidney disease: an evaluation study
Mousa Ghelichi-Ghojogh, Mohammad fararouei, Mozhgan Seif, Bahram Shahryari, Maryam Pakfetrat
International Urology and Nephrology.2022; 54(7): 1603. CrossRef - Chronic kidney disease and its health-related factors: a case-control study
Mousa Ghelichi-Ghojogh, Mohammad Fararouei, Mozhgan Seif, Maryam Pakfetrat
BMC Nephrology.2022;[Epub] CrossRef - Incidence and risk factors of severe non‐proliferative/proliferative diabetic retinopathy: More than a decade follow up in the Tehran Lipids and Glucose Study
Mahsa Sardarinia, Samaneh Asgari, Reyhane Hizomi Arani, Fatemeh Eskandari, Fereidoun Azizi, Davood Khalili, Farzad Hadaegh
Journal of Diabetes Investigation.2022; 13(2): 317. CrossRef - Pathophysiologic Mechanisms and Potential Biomarkers in Diabetic Kidney Disease
Chan-Young Jung, Tae-Hyun Yoo
Diabetes & Metabolism Journal.2022; 46(2): 181. CrossRef - Prevalence of chronic kidney diseases and its determinants among Iranian adults: results of the first phase of Shahedieh cohort study
Ali Dehghani, Sadegh Alishavandi, Nader Nourimajalan, Hossein Fallahzadeh, Vahid Rahmanian
BMC Nephrology.2022;[Epub] CrossRef - Construct a classification decision tree model to select the optimal equation for estimating glomerular filtration rate and estimate it more accurately
Zhenliang Fan, Qiaorui Yang, Zhuohan Xu, Ke Sun, Mengfan Yang, Riping Yin, Dongxue Zhao, Junfen Fan, Hongzhen Ma, Yiwei Shen, Hong Xia
Scientific Reports.2022;[Epub] CrossRef - Novel biomarkers for diabetic kidney disease
Chan-Young Jung, Tae-Hyun Yoo
Kidney Research and Clinical Practice.2022; 41(Suppl 2): S46. CrossRef - Prevalence and Associated Factors of Kidney Dysfunction in Patients with Hypertension and/or Diabetes Mellitus from a Primary Care Population in Northwest China
Mengyue Lin, Mulalibieke Heizhati, Lin Wang, Lin Gan, Mei Li, Wenbo Yang, Ling Yao, Zhongrong Wang, Zhikang Yang, Reyila Abudoyreyimu, Zihao Wu, Nanfang Li
International Journal of General Medicine.2021; Volume 14: 7567. CrossRef
- The Effect of the Holy Quran Recitation on Inflammatory Markers in Hemodialysis Patients in Iran: A Randomized Clinical Trial
- Complications
- Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
- Eugene Han, Mi Kyung Kim, Byoung Kuk Jang, Hye Soon Kim
- Diabetes Metab J. 2021;45(5):698-707. Published online February 2, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0118
- 5,406 View
- 197 Download
- 11 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
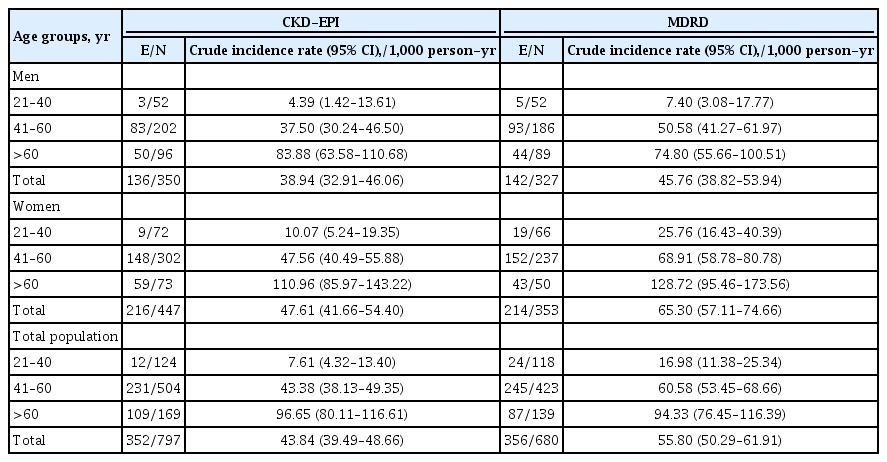
This study aimed to investigate the association between hepatic steatosis burden and albuminuria in Korean patients with type 2 diabetes mellitus (T2DM) and nonalcoholic fatty liver disease (NAFLD).
Methods
We recruited 100 patients with both T2DM and NAFLD, but without chronic kidney disease. Albuminuria was defined as a spot urinary albumin-to-creatinine ratio (ACR) ≥30 mg/g. Transient elastography was performed, and the steatosis burden was quantified by controlled attenuation parameter (CAP) with significant steatosis defined as CAP >302 dB/m.
Results
The prevalence of significant steatosis and albuminuria was 56.0% and 21.0%, respectively. Subjects with significant steatosis were significantly younger and had a significantly shorter duration of T2DM, greater waist circumference, and higher body mass index, total cholesterol, triglyceride, and low density lipoprotein cholesterol levels, than subjects without severe NAFLD (all P<0.05). Albuminuria was higher in patients with significant steatosis than in patients without significant steatosis (32.1% vs. 6.8%, P=0.002). Urinary ACR showed a correlation with CAP (r=0.331, P=0.001), and multiple linear regression analysis revealed a significant association between a high degree of albuminuria and high CAP value (r=0.321, P=0.001). Additionally, multivariate logistic regression analysis demonstrated the independent association between urinary ACR and significant steatosis after adjustment for confounding factors including age, body mass index, duration of T2DM, low density lipoprotein level, and renin-angiotensin system blocker use (odds ratio, 1.88; 95% confidence interval, 1.31 to 2.71; P=0.001).
Conclusion
T2DM patients with NAFLD had a higher prevalence of albuminuria, which correlated with their steatosis burden. -
Citations
Citations to this article as recorded by- A Novel Anthropometric Parameter, Weight-Adjusted Waist Index Represents Sarcopenic Obesity in Newly Diagnosed Type 2 Diabetes Mellitus
Min Jeong Park, Soon Young Hwang, Nam Hoon Kim, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
Journal of Obesity & Metabolic Syndrome.2023; 32(2): 130. CrossRef - Significance of Diabetic Kidney Disease Biomarkers in Predicting Metabolic-Associated Fatty Liver Disease
Jaehyun Bae, Byung-Wan Lee
Biomedicines.2023; 11(7): 1928. CrossRef - Non-alcoholic fatty liver disease and sarcopenia is associated with the risk of albuminuria independent of insulin resistance, and obesity
Eugene Han, Mi Kyung Kim, Seung-Soon Im, Byoung Kuk Jang, Hye Soon Kim
Journal of Diabetes and its Complications.2022; 36(8): 108253. CrossRef - Development and implementation of patient-level prediction models of end-stage renal disease for type 2 diabetes patients using fast healthcare interoperability resources
San Wang, Jieun Han, Se Young Jung, Tae Jung Oh, Sen Yao, Sanghee Lim, Hee Hwang, Ho-Young Lee, Haeun Lee
Scientific Reports.2022;[Epub] CrossRef - Beyond Liver Disease: Non-Alcoholic Fatty Liver Disease and Advanced Liver Fibrosis in Kidney Disease
Eugene Han
Diabetes & Metabolism Journal.2022; 46(4): 564. CrossRef - Muscle fat contents rather than muscle mass determines nonalcoholic steatohepatitis and liver fibrosis in patients with severe obesity
Eugene Han, Mi Kyung Kim, Hye Won Lee, Seungwan Ryu, Hye Soon Kim, Byoung Kuk Jang, Youngsung Suh
Obesity.2022; 30(12): 2440. CrossRef - Decreased Serum Osteocalcin is an Independent Risk Factor for Metabolic Dysfunction-Associated Fatty Liver Disease in Type 2 Diabetes
Yu-Jie Wang, Chun-Hua Jin, Jiang-Feng Ke, Jun-Wei Wang, Yi-Lin Ma, Jun-Xi Lu, Mei-Fang Li, Lian-Xi Li
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 3717. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2021;45:698-707)
Eugene Han, Hye Soon Kim
Diabetes & Metabolism Journal.2021; 45(6): 972. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2021;45:698-707)
Mi-kyung Kim
Diabetes & Metabolism Journal.2021; 45(6): 968. CrossRef - Liver fibrosis indices are related to diabetic peripheral neuropathy in individuals with type 2 diabetes
Kyuho Kim, Tae Jung Oh, Hyen Chung Cho, Yun Kyung Lee, Chang Ho Ahn, Bo Kyung Koo, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
Scientific Reports.2021;[Epub] CrossRef
- A Novel Anthropometric Parameter, Weight-Adjusted Waist Index Represents Sarcopenic Obesity in Newly Diagnosed Type 2 Diabetes Mellitus
- Complications
- Screening Tools Based on Nomogram for Diabetic Kidney Diseases in Chinese Type 2 Diabetes Mellitus Patients
- Ganyi Wang, Biyao Wang, Gaoxing Qiao, Hao Lou, Fei Xu, Zhan Chen, Shiwei Chen
- Diabetes Metab J. 2021;45(5):708-718. Published online April 13, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0117

- 6,912 View
- 141 Download
- 5 Web of Science
- 6 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- Background
The influencing factors of diabetic kidney disease (DKD) in Chinese patients with type 2 diabetes mellitus (T2DM) were explored to develop and validate a DKD diagnostic tool based on nomogram approach for patients with T2DM.
Methods
A total of 2,163 in-hospital patients with diabetes diagnosed from March 2015 to March 2017 were enrolled. Specified logistic regression models were used to screen the factors and establish four different diagnostic tools based on nomogram according to the final included variables. Discrimination and calibration were used to assess the performance of screening tools.
Results
Among the 2,163 participants with diabetes (1,227 men and 949 women), 313 patients (194 men and 120 women) were diagnosed with DKD. Four different screening equations (full model, laboratory-based model 1 [LBM1], laboratory-based model 2 [LBM2], and simplified model) showed good discriminations and calibrations. The C-indexes were 0.8450 (95% confidence interval [CI], 0.8202 to 0.8690) for full model, 0.8149 (95% CI, 0.7892 to 0.8405) for LBM1, 0.8171 (95% CI, 0.7912 to 0.8430) for LBM2, and 0.8083 (95% CI, 0.7824 to 0.8342) for simplified model. According to Hosmer-Lemeshow goodness-of-fit test, good agreement between the predicted and observed DKD events in patients with diabetes was observed for full model (χ2=3.2756, P=0.9159), LBM1 (χ2=7.749, P=0.4584), LBM2 (χ2=10.023, P=0.2634), and simplified model (χ2=12.294, P=0.1387).
Conclusion
LBM1, LBM2, and simplified model exhibited excellent predictive performance and availability and could be recommended for screening DKD cases among Chinese patients with diabetes. -
Citations
Citations to this article as recorded by- Development of Serum Lactate Level-Based Nomograms for Predicting Diabetic Kidney Disease in Type 2 Diabetes Mellitus Patients
Chunxia Jiang, Xiumei Ma, Jiao Chen, Yan Zeng, Man Guo, Xiaozhen Tan, Yuping Wang, Peng Wang, Pijun Yan, Yi Lei, Yang Long, Betty Yuen Kwan Law, Yong Xu
Diabetes, Metabolic Syndrome and Obesity.2024; Volume 17: 1051. CrossRef - Changes in urinary exosomal protein CALM1 may serve as an early noninvasive biomarker for diagnosing diabetic kidney disease
Tao Li, Tian ci Liu, Na Liu, Man Zhang
Clinica Chimica Acta.2023; 547: 117466. CrossRef - Developing screening tools to estimate the risk of diabetic kidney disease in patients with type 2 diabetes mellitus
Xu Cao, Xiaomei Pei
Technology and Health Care.2023; : 1. CrossRef - Development and validation of a novel nomogram to predict diabetic kidney disease in patients with type 2 diabetic mellitus and proteinuric kidney disease
Hui Zhuan Tan, Jason Chon Jun Choo, Stephanie Fook-Chong, Yok Mooi Chin, Choong Meng Chan, Chieh Suai Tan, Keng Thye Woo, Jia Liang Kwek
International Urology and Nephrology.2022; 55(1): 191. CrossRef - Nomogram-Based Chronic Kidney Disease Prediction Model for Type 1 Diabetes Mellitus Patients Using Routine Pathological Data
Nakib Hayat Chowdhury, Mamun Bin Ibne Reaz, Sawal Hamid Md Ali, Shamim Ahmad, María Liz Crespo, Andrés Cicuttin, Fahmida Haque, Ahmad Ashrif A. Bakar, Mohammad Arif Sobhan Bhuiyan
Journal of Personalized Medicine.2022; 12(9): 1507. CrossRef - Development and assessment of diabetic nephropathy prediction model using hub genes identified by weighted correlation network analysis
Xuelian Zhang, Yao Wang, Zhaojun Yang, Xiaoping Chen, Jinping Zhang, Xin Wang, Xian Jin, Lili Wu, Xiaoyan Xing, Wenying Yang, Bo Zhang
Aging.2022; 14(19): 8095. CrossRef
- Development of Serum Lactate Level-Based Nomograms for Predicting Diabetic Kidney Disease in Type 2 Diabetes Mellitus Patients
- Metabolic Risk/Epidemiology
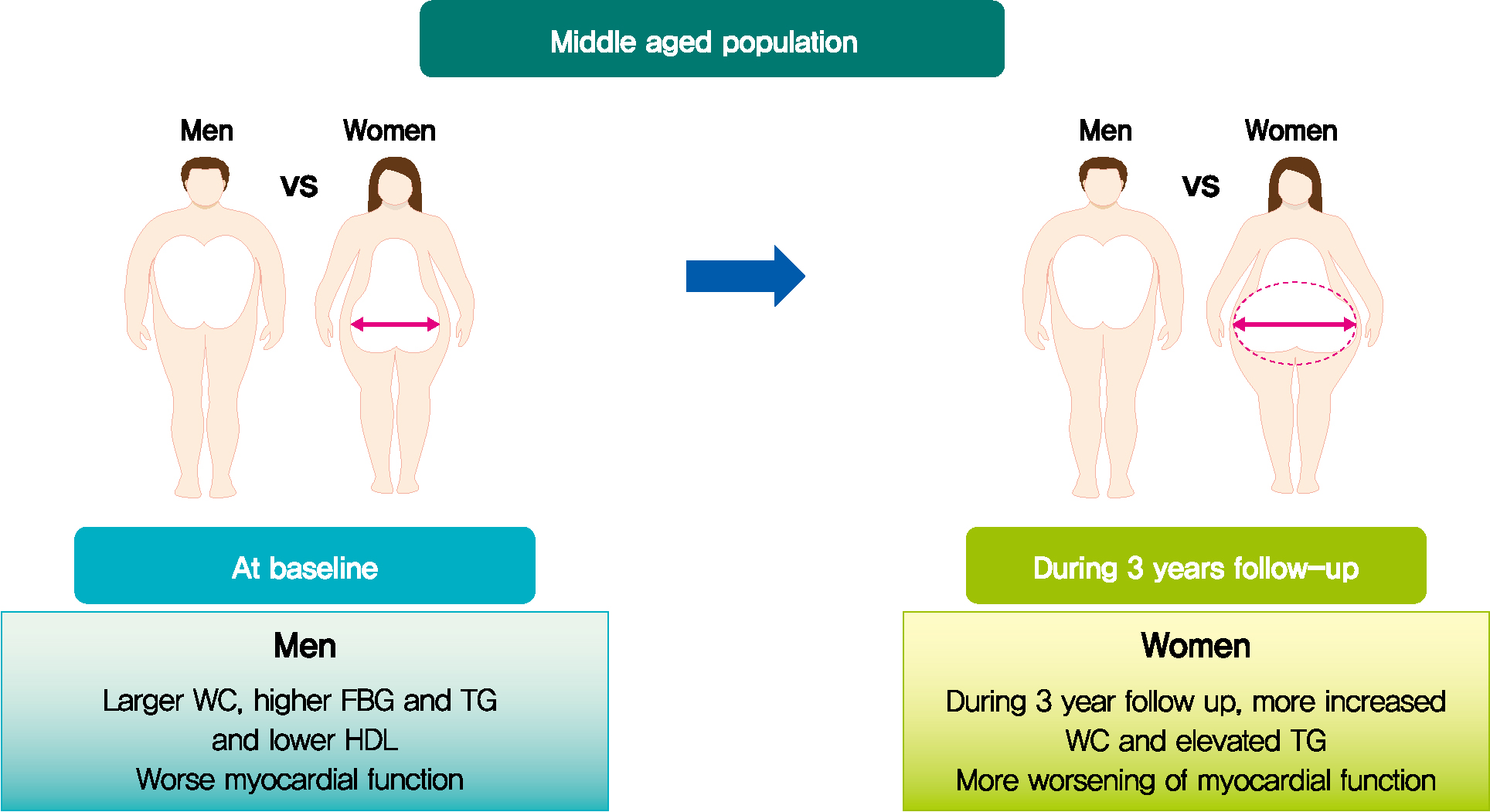
- Longitudinal Change in Myocardial Function and Clinical Parameters in Middle-Aged Subjects: A 3-Year Follow-up Study
- Dong-Hyuk Cho, Hyung Joon Joo, Mi-Na Kim, Hee-Dong Kim, Do-Sun Lim, Seong-Mi Park
- Diabetes Metab J. 2021;45(5):719-729. Published online June 15, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0132
- 4,238 View
- 108 Download
- 2 Web of Science
- 2 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 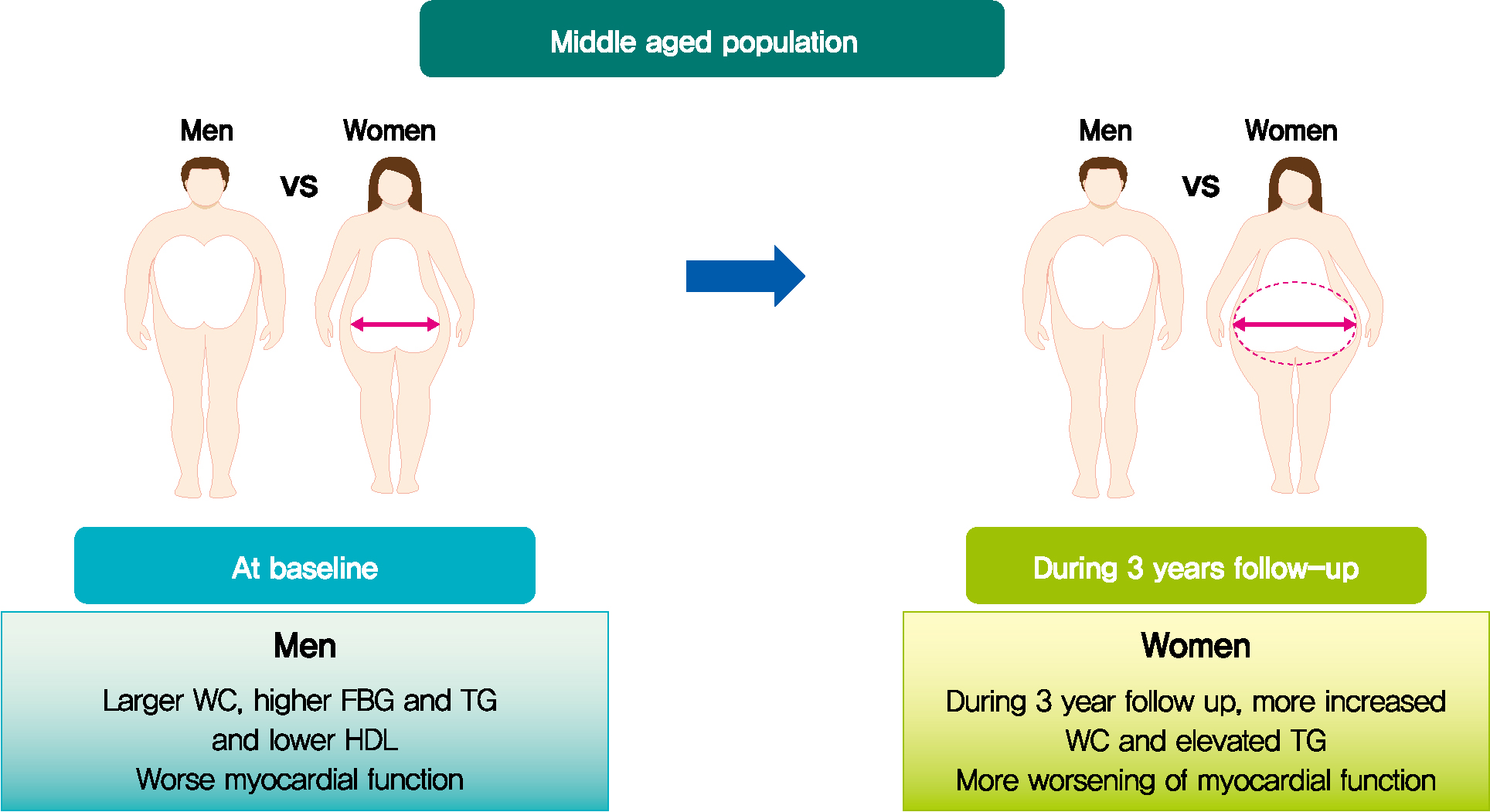
- Background
Metabolic syndrome (MetS) is closely associated with the aging process. However, changes in metabolic conditions and cardiac function that occur in middle aged population remain unclear. We evaluated longitudinal changes in metabolic parameters and cardiac function during a 3-year period in subjects with suspected MetS.
Methods
We studied 191 participants with suspected MetS at baseline and after 3 years. Anthropometric parameters, including waist circumference (WC), and metabolic parameters, including fasting blood glucose and lipid profile were measured. Conventional echocardiography with two-dimensional speckle tracking was performed.
Results
Mean age was 56.2±4.4 years, and there were 97 women (50.8%). Men had increased WC and triglycerides (TG) (WC 91.2±6.8 cm vs. 84.0±8.0 cm, P<0.001; TG 184.4±116.3 mg/dL vs. 128.2±53.6 mg/dL, P<0.001), and reduced global longitudinal strain (GLS) (–15.4%±2.1% vs. –17.1%±2.0%, P<0.001) compared to women. After 3.4 years, values of WC and TG did not change in men but increased in women (all P<0.05). The absolute value of left ventricular (LV) GLS did not change in men but was reduced in women (P=0.011). Change in TG was independently associated with worsening of LV GLS only in women (standardized β, –0.309; 95% confidence interval, –0.130 to –0.009; P=0.025).
Conclusion
In middle aged population, a vulnerable period for metabolic disturbance, cardiac remodeling tended to progress, which was prominent in women. Progression of adiposity and dyslipidemia after menopause may accelerate subclinical cardiac remodeling in middle-aged women. Lifestyle modification and medical interventions may help prevent further cardiac dysfunction in these subjects. -
Citations
Citations to this article as recorded by- Positive additive interaction effects of age, sex, obesity, and metabolic syndrome on left ventricular dysfunction
Dan Zhou, Zhongwen Ye, Zhiqiang Nie, Chaolei Chen, Songyuan Luo, Mengqi Yan, Jiabin Wang, Yingqing Feng
Journal of Diabetes.2024;[Epub] CrossRef - Lung-Heart Outcomes and Mortality through the 2020 COVID-19 Pandemic in a Prospective Cohort of Breast Cancer Radiotherapy Patients
Vincent Vinh-Hung, Olena Gorobets, Nele Adriaenssens, Hilde Van Parijs, Guy Storme, Dirk Verellen, Nam P. Nguyen, Nicolas Magne, Mark De Ridder
Cancers.2022; 14(24): 6241. CrossRef
- Positive additive interaction effects of age, sex, obesity, and metabolic syndrome on left ventricular dysfunction
- Metabolic Risk/Epidemiology
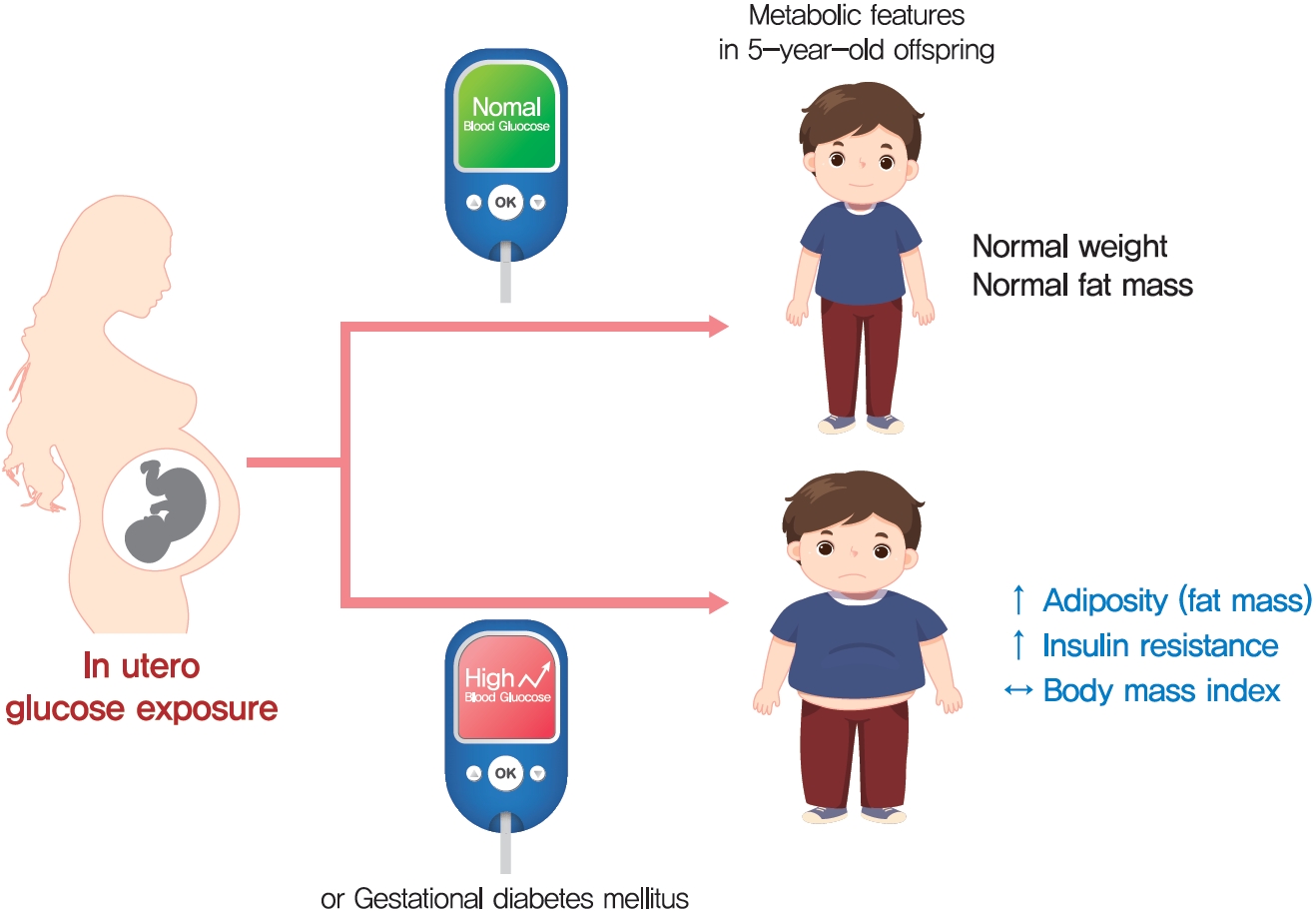
- Maternal Hyperglycemia during Pregnancy Increases Adiposity of Offspring
- Hye Rim Chung, Joon Ho Moon, Jung Sub Lim, Young Ah Lee, Choong Ho Shin, Joon-Seok Hong, Soo Heon Kwak, Sung Hee Choi, Hak Chul Jang
- Diabetes Metab J. 2021;45(5):730-738. Published online February 22, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0154
- 5,717 View
- 180 Download
- 6 Web of Science
- 6 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 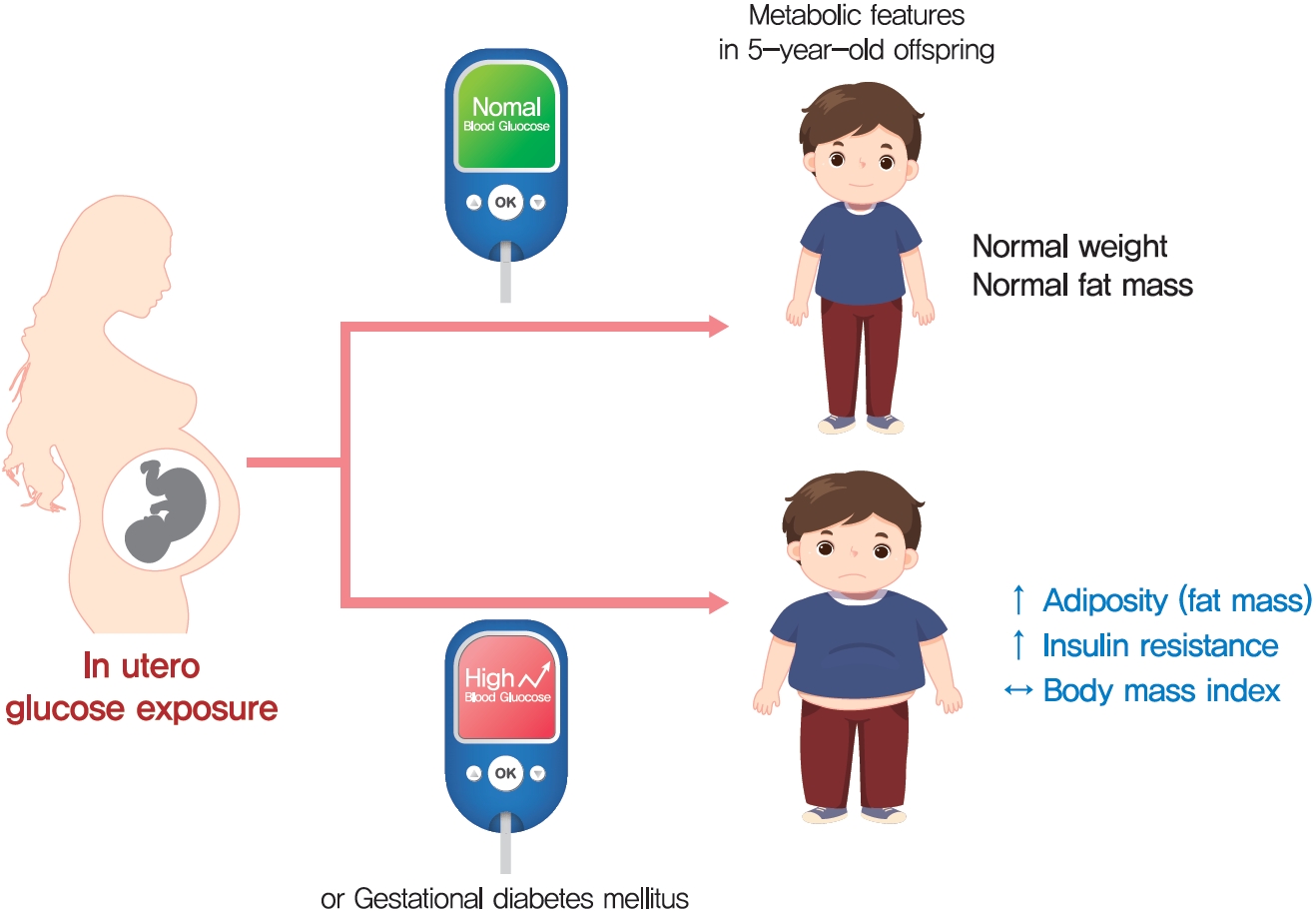
- Background
The effect of intrauterine hyperglycemia on fat mass and regional fat proportion of the offspring of mothers with gestational diabetes mellitus (OGDM) remains to be determined.
Methods
The body composition of OGDM (n=25) and offspring of normoglycemic mothers (n=49) was compared using dualenergy X-ray absorptiometry at age 5 years. The relationship between maternal glucose concentration during a 100 g oral glucose tolerance test (OGTT) and regional fat mass or proportion was analyzed after adjusting for maternal prepregnancy body mass index (BMI).
Results
BMI was comparable between OGDM and control (median, 16.0 kg/m2 vs. 16.1 kg/m2 ). Total, truncal, and leg fat mass were higher in OGDM compared with control (3,769 g vs. 2,245 g, P=0.004; 1,289 g vs. 870 g, P=0.017; 1,638 g vs. 961 g, P=0.002, respectively), whereas total lean mass was lower in OGDM (15,688 g vs. 16,941 g, P=0.001). Among OGDM, total and truncal fat mass were correlated with fasting and 3-hour glucose concentrations of maternal 100 g OGTT during pregnancy (total fat mass, r=0.49, P=0.018 [fasting], r=0.473, P=0.023 [3-hour]; truncal fat mass, r=0.571, P=0.004 [fasting], r=0.558, P=0.006 [3-hour]), but there was no correlation between OGDM leg fat mass and maternal OGTT during pregnancy. Regional fat indices were not correlated with concurrent maternal 75 g OGTT values.
Conclusion
Intrauterine hyperglycemia is associated with increased fat mass, especially truncal fat, in OGDM aged 5 years. -
Citations
Citations to this article as recorded by- Advances in free fatty acid profiles in gestational diabetes mellitus
Haoyi Du, Danyang Li, Laura Monjowa Molive, Na Wu
Journal of Translational Medicine.2024;[Epub] CrossRef - High-fat diet during pregnancy lowers fetal weight and has a long-lasting adverse effect on brown adipose tissue in the offspring
Mihoko Yamaguchi, Jun Mori, Nozomi Nishida, Satoshi Miyagaki, Yasuhiro Kawabe, Takeshi Ota, Hidechika Morimoto, Yusuke Tsuma, Shota Fukuhara, Takehiro Ogata, Takuro Okamaura, Naoko Nakanishi, Masahide Hamaguchi, Hisakazu Nakajima, Michiaki Fukui, Tomoko I
Journal of Developmental Origins of Health and Disease.2023; 14(2): 261. CrossRef - Prediction of gestational diabetes mellitus in Asian women using machine learning algorithms
Byung Soo Kang, Seon Ui Lee, Subeen Hong, Sae Kyung Choi, Jae Eun Shin, Jeong Ha Wie, Yun Sung Jo, Yeon Hee Kim, Kicheol Kil, Yoo Hyun Chung, Kyunghoon Jung, Hanul Hong, In Yang Park, Hyun Sun Ko
Scientific Reports.2023;[Epub] CrossRef - Effects of early standardized management on the growth trajectory of offspring with gestational diabetes mellitus at 0–5 years old: a preliminary longitudinal study
Bingbing Guo, Jingjing Pei, Yin Xu, Yajie Wang, Xinye Jiang
Scientific Reports.2023;[Epub] CrossRef - Gestational Diabetes Mellitus: Diagnostic Approaches and Maternal-Offspring Complications
Joon Ho Moon, Hak Chul Jang
Diabetes & Metabolism Journal.2022; 46(1): 3. CrossRef - Increased Pro-Inflammatory T Cells, Senescent T Cells, and Immune-Check Point Molecules in the Placentas of Patients With Gestational Diabetes Mellitus
Yea Eun Kang, Hyon-Seung Yi, Min-Kyung Yeo, Jung Tae Kim, Danbit Park, Yewon Jung, Ok Soon Kim, Seong Eun Lee, Ji Min Kim, Kyong Hye Joung, Ju Hee Lee, Bon Jeong Ku, Mina Lee, Hyun Jin Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef
- Advances in free fatty acid profiles in gestational diabetes mellitus
- Metabolic Risk/Epidemiology
-
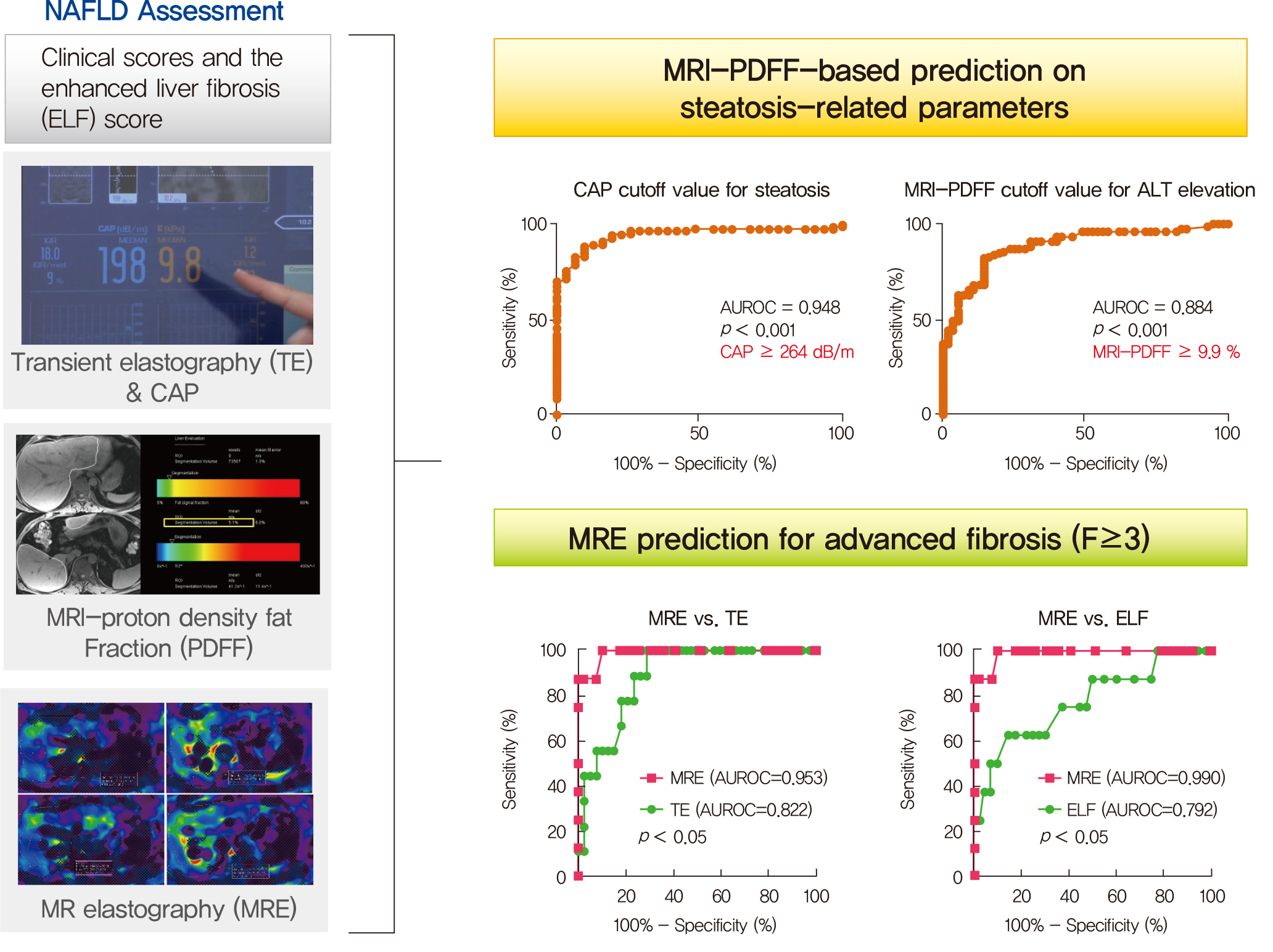
- Magnetic Resonance-Based Assessments Better Capture Pathophysiologic Profiles and Progression in Nonalcoholic Fatty Liver Disease
- Seung Joon Choi, Seong Min Kim, Yun Soo Kim, Oh Sang Kwon, Seung Kak Shin, Kyoung Kon Kim, Kiyoung Lee, Ie Byung Park, Cheol Soo Choi, Dong Hae Chung, Jaehun Jung, MunYoung Paek, Dae Ho Lee
- Diabetes Metab J. 2021;45(5):739-752. Published online October 28, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0137
- 8,704 View
- 218 Download
- 13 Web of Science
- 15 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 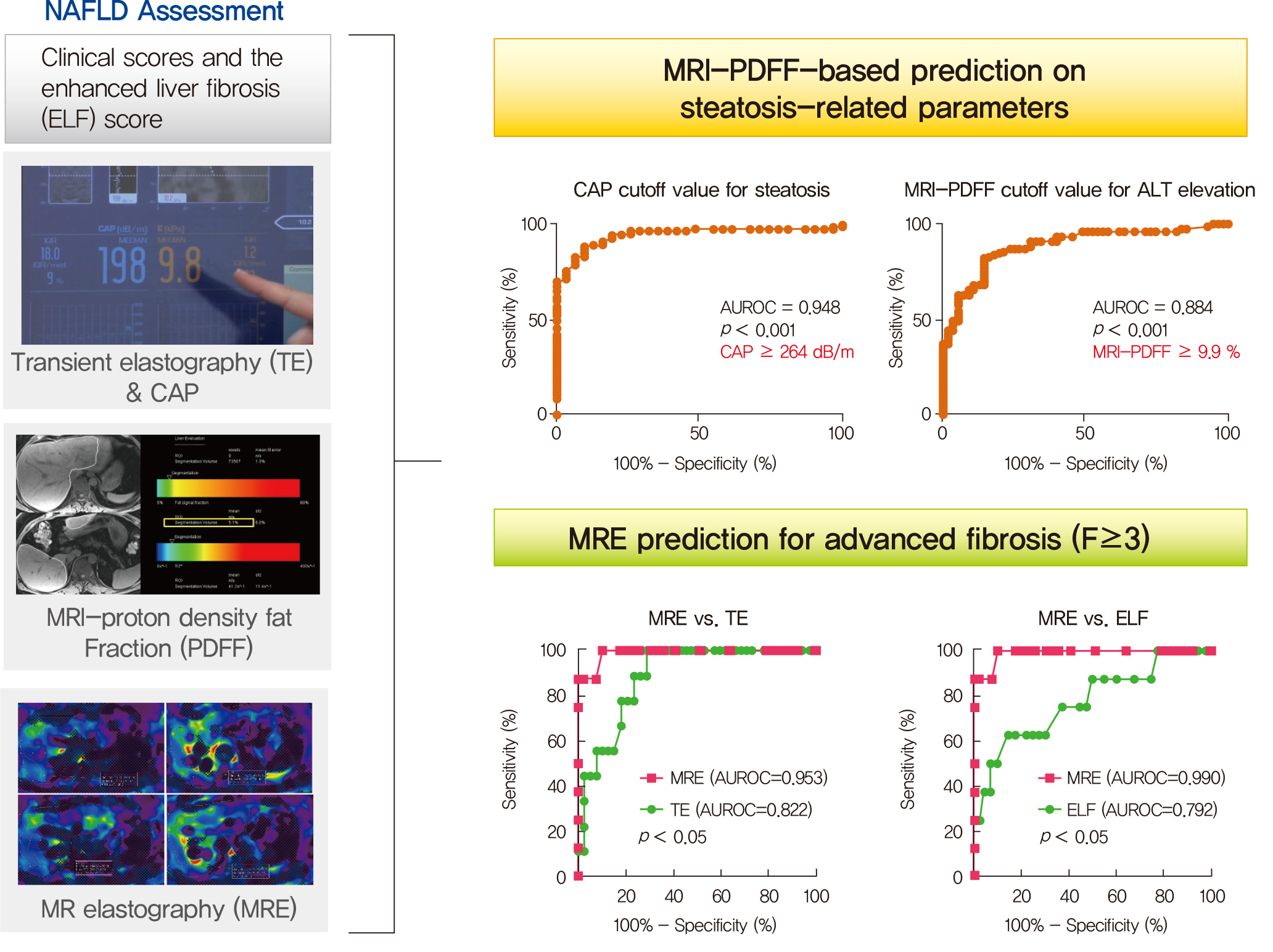
- Background
Several noninvasive tools are available for the assessment of nonalcoholic fatty liver disease (NAFLD) including clinical and blood biomarkers, transient elastography (TE), and magnetic resonance imaging (MRI) techniques, such as proton density fat fraction (MRI-PDFF) and magnetic resonance elastography (MRE). In the present study, we aimed to evaluate whether magnetic resonance (MR)-based examinations better discriminate the pathophysiologic features and fibrosis progression in NAFLD than other noninvasive methods.
Methods
A total of 133 subjects (31 healthy volunteers and 102 patients with NAFLD) were subjected to clinical and noninvasive NAFLD evaluation, with additional liver biopsy in some patients (n=54).
Results
MRI-PDFF correlated far better with hepatic fat measured by MR spectroscopy (r=0.978, P<0.001) than with the TE controlled attenuation parameter (CAP) (r=0.727, P<0.001). In addition, MRI-PDFF showed stronger correlations with various pathophysiologic parameters for cellular injury, glucose and lipid metabolism, and inflammation, than the TE-CAP. The MRI-PDFF and TE-CAP cutoff levels associated with abnormal elevation of serum alanine aminotransferase were 9.9% and 270 dB/m, respectively. The MRE liver stiffness measurement (LSM) showed stronger correlations with liver enzymes, platelets, complement component 3, several clinical fibrosis scores, and the enhanced liver fibrosis (ELF) score than the TE-LSM. In an analysis of only biopsied patients, MRE performed better in discriminating advanced fibrosis with a cutoff value of 3.9 kPa than the TE (cutoff 8.1 kPa) and ELF test (cutoff 9.2 kPa).
Conclusion
Our results suggest that MRI-based assessment of NAFLD is the best non-invasive tool that captures the histologic, pathophysiologic and metabolic features of the disease. -
Citations
Citations to this article as recorded by- A Novel Score Based on Controlled Attenuation Parameter Accurately Predicts Hepatic Steatosis in Individuals With Metabolic Dysfunction Associated Steatotic Liver Disease: A Derivation and Independent Validation Study
Zi-Ming An, Qiao-Hong Liu, Xin-Jian Ye, Qian Zhang, Hua-Fu Pei, Xin Xin, Jie Yuan, Qian Huang, Kun Liu, Fang Lu, Zhi-Han Yan, Yu Zhao, Yi-Yang Hu, Ming-Hua Zheng, Qin Feng
Clinical and Translational Gastroenterology.2024; 15(3): e00680. CrossRef - Imaging Methods Applicable in the Diagnostics of Alzheimer’s Disease, Considering the Involvement of Insulin Resistance
Petra Hnilicova, Ema Kantorova, Stanislav Sutovsky, Milan Grofik, Kamil Zelenak, Egon Kurca, Norbert Zilka, Petra Parvanovova, Martin Kolisek
International Journal of Molecular Sciences.2023; 24(4): 3325. CrossRef - Polyunsaturated and Saturated Oxylipin Plasma Levels Allow Monitoring the Non-Alcoholic Fatty Liver Disease Progression to Severe Stages
Miguel D. Ferrer, Clara Reynés, Margalida Monserrat-Mesquida, Magdalena Quetglas-Llabrés, Cristina Bouzas, Silvia García, David Mateos, Miguel Casares, Cristina Gómez, Lucía Ugarriza, Josep A. Tur, Antoni Sureda, Antoni Pons
Antioxidants.2023; 12(3): 711. CrossRef - An individual patient data meta-analysis to determine cut-offs for and confounders of NAFLD-fibrosis staging with magnetic resonance elastography
Jia-xu Liang, Javier Ampuero, Hao Niu, Kento Imajo, Mazen Noureddin, Jaideep Behari, Dae Ho Lee, Richard L. Ehman, Fredrik Rorsman, Johan Vessby, Juan R. Lacalle, Ferenc E. Mózes, Michael Pavlides, Quentin M. Anstee, Stephen A. Harrison, Javier Castell, R
Journal of Hepatology.2023; 79(3): 592. CrossRef - Relationship between controlled attenuated parameter and magnetic resonance imaging–proton density fat fraction for evaluating hepatic steatosis in patients with NAFLD
Ziming An, Qiaohong Liu, Wenli Zeng, Yan Wang, Qian Zhang, Huafu Pei, Xin Xin, Shuohui Yang, Fang Lu, Yu Zhao, Yiyang Hu, Qin Feng
Hepatology Communications.2022; 6(8): 1975. CrossRef - Noninvasive imaging of hepatic dysfunction: A state-of-the-art review
Ting Duan, Han-Yu Jiang, Wen-Wu Ling, Bin Song
World Journal of Gastroenterology.2022; 28(16): 1625. CrossRef - Diagnosis and Pathogenesis of Sarcopenia in Chronic Liver Disease Using Liver Magnetic Resonance Imaging
Atsushi Nakamura, Tsubasa Yoshimura, Tomomi Sato, Takeshi Ichikawa
Cureus.2022;[Epub] CrossRef - Plasma Aldo-Keto Reductase Family 1 Member B10 as a Biomarker Performs Well in the Diagnosis of Nonalcoholic Steatohepatitis and Fibrosis
Aron Park, Seung Joon Choi, Sungjin Park, Seong Min Kim, Hye Eun Lee, Minjae Joo, Kyoung Kon Kim, Doojin Kim, Dong Hae Chung, Jae Been Im, Jaehun Jung, Seung Kak Shin, Byung-Chul Oh, Cheolsoo Choi, Seungyoon Nam, Dae Ho Lee
International Journal of Molecular Sciences.2022; 23(9): 5035. CrossRef - Contribution of a genetic risk score to ethnic differences in fatty liver disease
Maddie J. Kubiliun, Jonathan C. Cohen, Helen H. Hobbs, Julia Kozlitina
Liver International.2022; 42(10): 2227. CrossRef - Plasma Metabolomics and Machine Learning-Driven Novel Diagnostic Signature for Non-Alcoholic Steatohepatitis
Moongi Ji, Yunju Jo, Seung Joon Choi, Seong Min Kim, Kyoung Kon Kim, Byung-Chul Oh, Dongryeol Ryu, Man-Jeong Paik, Dae Ho Lee
Biomedicines.2022; 10(7): 1669. CrossRef - Updated S2k Clinical Practice Guideline on Non-alcoholic Fatty Liver Disease (NAFLD) issued by the German Society of Gastroenterology, Digestive and Metabolic Diseases (DGVS) – April 2022 – AWMF Registration No.: 021–025
Zeitschrift für Gastroenterologie.2022; 60(09): e733. CrossRef - Aktualisierte S2k-Leitlinie nicht-alkoholische Fettlebererkrankung der Deutschen Gesellschaft für Gastroenterologie, Verdauungs- und Stoffwechselkrankheiten (DGVS) – April 2022 – AWMF-Registernummer: 021–025
E. Roeb, A. Canbay, H. Bantel, J. Bojunga, J. de Laffolie, M. Demir, U. W. Denzer, A. Geier, W. P. Hofmann, C. Hudert, T. Karlas, M. Krawczyk, T. Longerich, T. Luedde, M. Roden, J. Schattenberg, M. Sterneck, A. Tannapfel, P. Lorenz, F. Tacke
Zeitschrift für Gastroenterologie.2022; 60(09): 1346. CrossRef - Ultrasound Methods for the Assessment of Liver Steatosis: A Critical Appraisal
Dorotea Bozic, Kristian Podrug, Ivana Mikolasevic, Ivica Grgurevic
Diagnostics.2022; 12(10): 2287. CrossRef - Significance of liver fat loss in chronic liver disease: Usefulness of hepatic proton density fat fraction measurement by magnetic resonance imaging in evaluating malnutrition
Atsushi Nakamura, Haruka Okada, Tsubasa Yoshimura, Manami Deguchi, Yuei Hosokawa, Tomomi Satoh, Takeshi Ichikawa, Keiji Okuyama, Yoshihiro Yoshioka, Hitoshi Asakura
Kanzo.2021; 62(9): 525. CrossRef - Screening for nonalcoholic fatty liver disease-when, who and how?
Christoph G Dietrich, Monika Rau, Andreas Geier
World Journal of Gastroenterology.2021; 27(35): 5803. CrossRef
- A Novel Score Based on Controlled Attenuation Parameter Accurately Predicts Hepatic Steatosis in Individuals With Metabolic Dysfunction Associated Steatotic Liver Disease: A Derivation and Independent Validation Study
- Cardiovascular Risk/Epidemiology
- Appraisal of Guidelines for the Management of Blood Pressure in Patients with Diabetes Mellitus: The Consensuses, Controversies and Gaps
- Menghui Liu, Shaozhao Zhang, Xiaohong Chen, Yue Guo, Xiangbin Zhong, Zhenyu Xiong, Yifen Lin, Huimin Zhou, Yiquan Huang, Zhengzhipeng Zhang, Lichun Wang, Xiaodong Zhuang, Xinxue Liao
- Diabetes Metab J. 2021;45(5):753-764. Published online April 23, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0134
- 4,866 View
- 143 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Currently available guidelines contain conflicting recommendations on the management of blood pressure (BP) in patients with diabetes mellitus (DM). Therefore, it is necessary to appraise the guidelines and summarize the agreements and differences among recommendations.
Methods
Four databases and the websites of guideline organizations were searched for guidelines regarding BP targets and thresholds for pharmacologic therapy in DM patients, and the included guidelines were appraised with the Appraisal of Guidelines for Research and Evaluation (AGREE) II instrument.
Results
In 6,498 records identified, 20 guidelines met our inclusion criteria with 64.0% AGREE II scores (interquartile range, 48.5% to 72.0%). The scores of the European and American guidelines were superior to those of the Asian guidelines (both adjusted P<0.001). Most of the guidelines advocated systolic BP targets <130 mm Hg (12 guidelines, 60%) and diastolic BP targets <80 mm Hg (14 guidelines, 70%) in DM patients. Approximately half of the guidelines supported systolic BP thresholds >140 mm Hg (10 guidelines, 50%) and diastolic BP thresholds >90 mm Hg (nine guidelines, 45%). The tiny minority of the guidelines provided the relevant recommendations regarding the lower limit of official BP targets and the ambulatory BP monitoring (ABPM)/home BP monitoring (HBPM) targets and thresholds in DM patients.
Conclusion
The lower official BP targets (<130/80 mm Hg) in patients with DM are advocated by most of the guidelines, but they contain conflicting recommendations on the official BP thresholds. Moreover, the gaps regarding the lower limit of official BP targets and the ABPM/HBPM targets and thresholds need to be considered by future study.
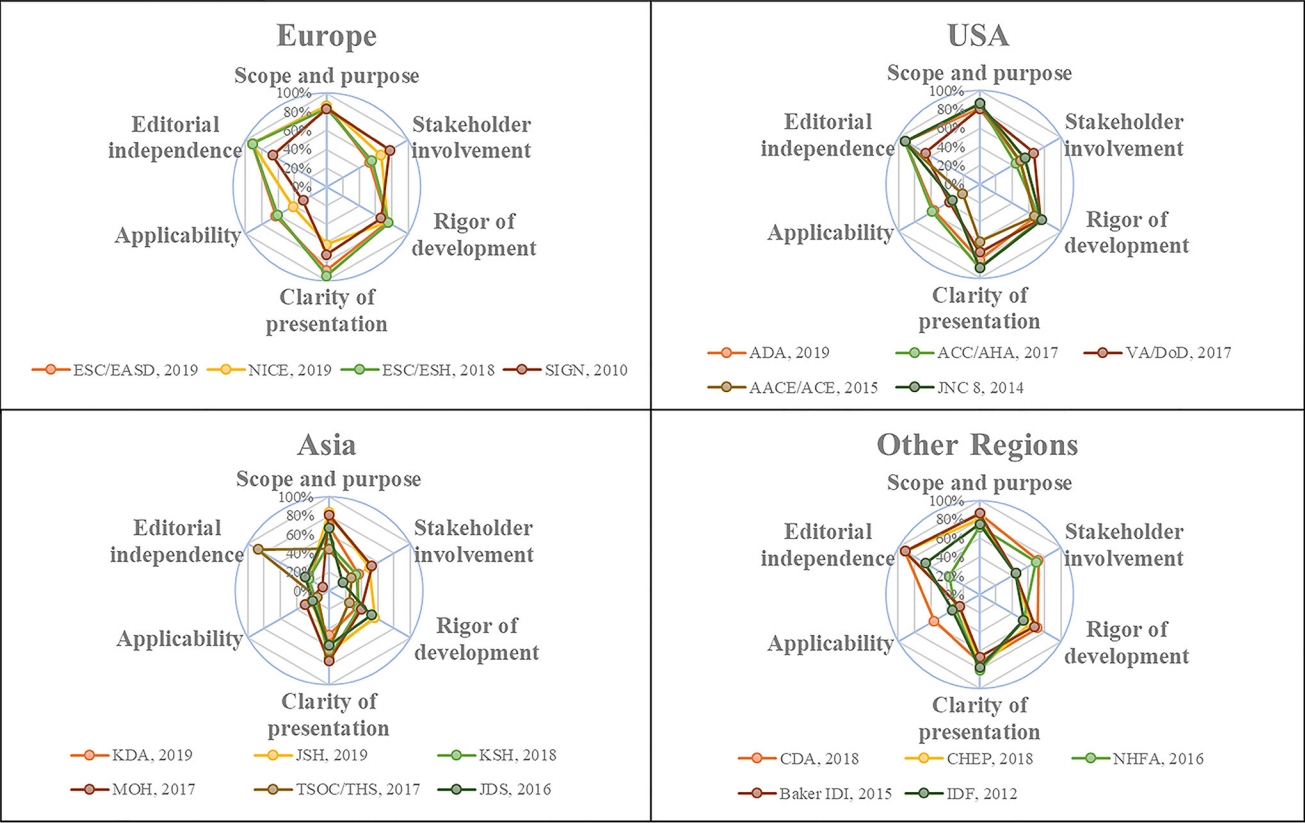
- COVID-19
- Effects of Social Distancing on Diabetes Management in Older Adults during COVID-19 Pandemic
- Soo Myoung Shin, Tae Jung Oh, Sung Hee Choi, Hak Chul Jang
- Diabetes Metab J. 2021;45(5):765-772. Published online August 30, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0096
- 5,954 View
- 191 Download
- 9 Web of Science
- 9 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 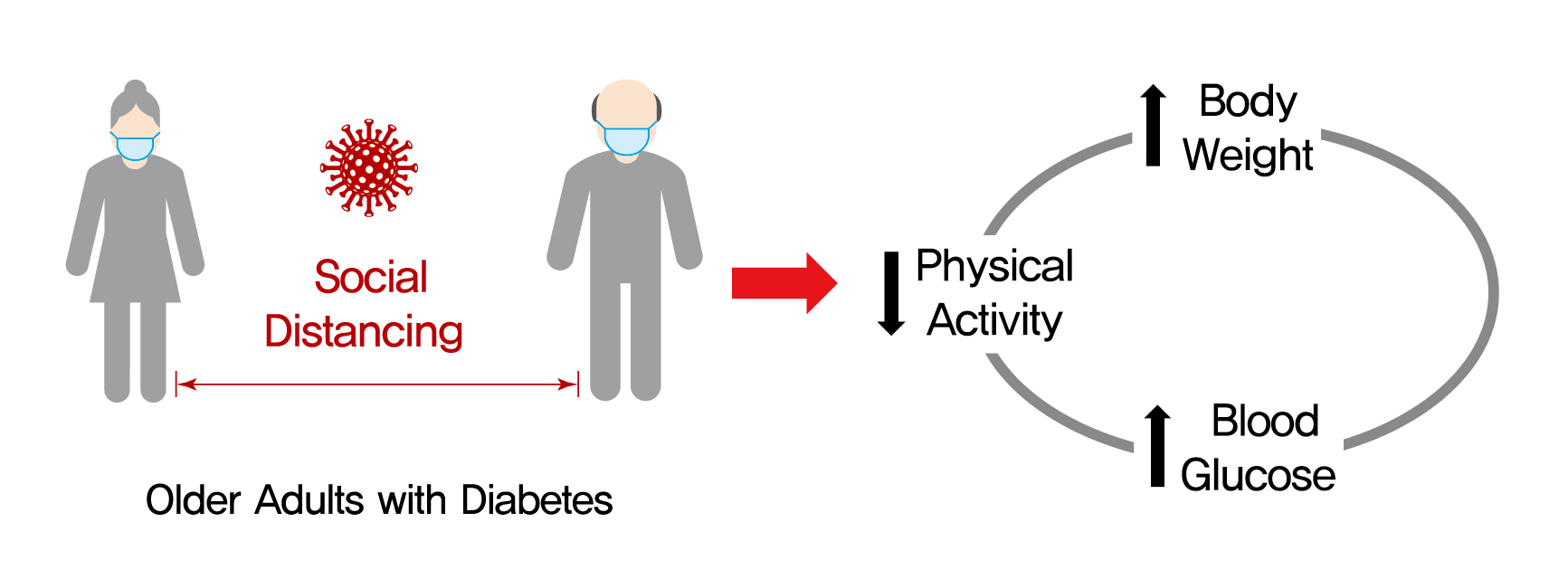
- Background
On March 22, 2020, intense social distancing (SD) was implemented in Korea to prevent the spread of coronavirus disease 19 (COVID-19). This study examined the impact of SD on diabetes control in older adults with diabetes.
Methods
Adults aged 60 to 90 years with type 2 diabetes mellitus who were physically and mentally independent were recruited. Participants who had complete blood chemistry data from April to July 2019 (pre-SD era) and April to July 2020 (SD era) were enrolled. Data were obtained about physical activity, nutrition, sarcopenia, and psychological and mental health from questionnaires in April to July 2020. Calf circumference was measured.
Results
In total, 246 people (100 men, 146 women; mean age, 73.8±5.7 years) participated in this study. The levels of glycated hemoglobin (HbA1c, 7.4%±1.0% vs. 7.1%±0.8%, P<0.001), fasting glucose (142.2±16.7 mg/dL vs. 132.0±27.7 mg/dL, P<0.001), and body weight (62.6±9.4 kg vs. 61.8±10.1 kg, P<0.01) were higher in the SD era than in the pre-SD era. Total physical activity was lower in the SD era (2,584.6±2,624.1 MET-min/week–1 vs. 1,987.3±2,295.0 MET-min/week–1, P<0.001). A larger increase in HbA1c level was associated with increased body weight and decreased physical activity.
Conclusion
SD had negative effects on diabetes management in older adults with diabetes. Fasting glucose and HbA1c levels and body weight increased during the SD era. Participants with reduced physical activity gained more weight and had higher blood glucose levels. Given that the COVID-19 pandemic is ongoing, health professionals and diabetes educators should monitor changes in lifestyle factors in older adults with diabetes. -
Citations
Citations to this article as recorded by- Preliminary efficacy of a technology-based physical activity intervention for older Korean adults during the COVID-19 pandemic
Soonhyung Kwon, Oejin Shin, Rosalba Hernandez
Educational Gerontology.2024; 50(1): 27. CrossRef - Obesity and weight change during the COVID‐19 pandemic in children and adults: A systematic review and meta‐analysis
Laura N. Anderson, Yulika Yoshida‐Montezuma, Nora Dewart, Ezza Jalil, Jayati Khattar, Vanessa De Rubeis, Sarah Carsley, Lauren E. Griffith, Lawrence Mbuagbaw
Obesity Reviews.2023;[Epub] CrossRef - Changes in lifestyle-related behaviour during the COVID-19 pandemic in Japan: a questionnaire survey for examinees who underwent an annual health check-up
Miyako Kishimoto, Kayo Masuko, Sumie Yamamoto, Retsu Fujita, Shoko Nakamura, Masato Odawara, Mikio Zeniya
Journal of International Medical Research.2023;[Epub] CrossRef - Glycaemic monitoring and control among high-risk patients with type 2 diabetes in Australian general practice during COVID-19
Kirrilee Jane Barlow, Paul P Fahey, Evan Atlantis
Family Medicine and Community Health.2023; 11(3): e002271. CrossRef - Social isolation, loneliness and subsequent risk of major adverse cardiovascular events among individuals with type 2 diabetes mellitus
Yannis Yan Liang, Yilin Chen, Hongliang Feng, Huachen Xue, Yu Nie, Qi-Yong H Ai, Jiacheng Ma, Lulu Yang, Jihui Zhang, Sizhi Ai
General Psychiatry.2023; 36(6): e101153. CrossRef - Stress, Depression, and Unhealthy Behavior Changes among Patients with Diabetes during COVID-19 in Korea
Hae Ran Kim, Jeong-Soon Kim
Healthcare.2022; 10(2): 303. CrossRef - Reply to comment on “Unexpected decline in glycated hemoglobin level after emergency COVID‐19 measures in three robust older Japanese women with prediabetes/mild type 2 diabetes”
Tazuo Okuno, Osamu Iritani, Kumie Kodera, Daisuke Hama, Asami Kane, Kozue Morigaki, Toshio Terai, Norie Maeno, Shigeto Morimoto
Geriatrics & Gerontology International.2022; 22(7): 541. CrossRef - Anxiety, Distress and Stress among Patients with Diabetes during COVID-19 Pandemic: A Systematic Review and Meta-Analysis
Rubén A. García-Lara, José L. Gómez-Urquiza, María José Membrive-Jiménez, Almudena Velando-Soriano, Monserrat E. Granados-Bolivar, José L. Romero-Béjar, Nora Suleiman-Martos
Journal of Personalized Medicine.2022; 12(9): 1412. CrossRef - Prevalence of Depression and Related Factors among Patients with Chronic Disease during the COVID-19 Pandemic: A Systematic Review and Meta-Analysis
Rubén A. García-Lara, Nora Suleiman-Martos, María J. Membrive-Jiménez, Victoria García-Morales, Miguel Quesada-Caballero, Isabel M. Guisado-Requena, José L. Gómez-Urquiza
Diagnostics.2022; 12(12): 3094. CrossRef
- Preliminary efficacy of a technology-based physical activity intervention for older Korean adults during the COVID-19 pandemic
- Basic Research
-
- The Effects of Exercise and Restriction of Sugar-Sweetened Beverages on Muscle Function and Autophagy Regulation in High-Fat High-Sucrose-Fed Obesity Mice
- Didi Zhang, Ji Hyun Lee, Hyung Eun Shin, Seong Eun Kwak, Jun Hyun Bae, Liang Tang, Wook Song
- Diabetes Metab J. 2021;45(5):773-786. Published online March 25, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0157
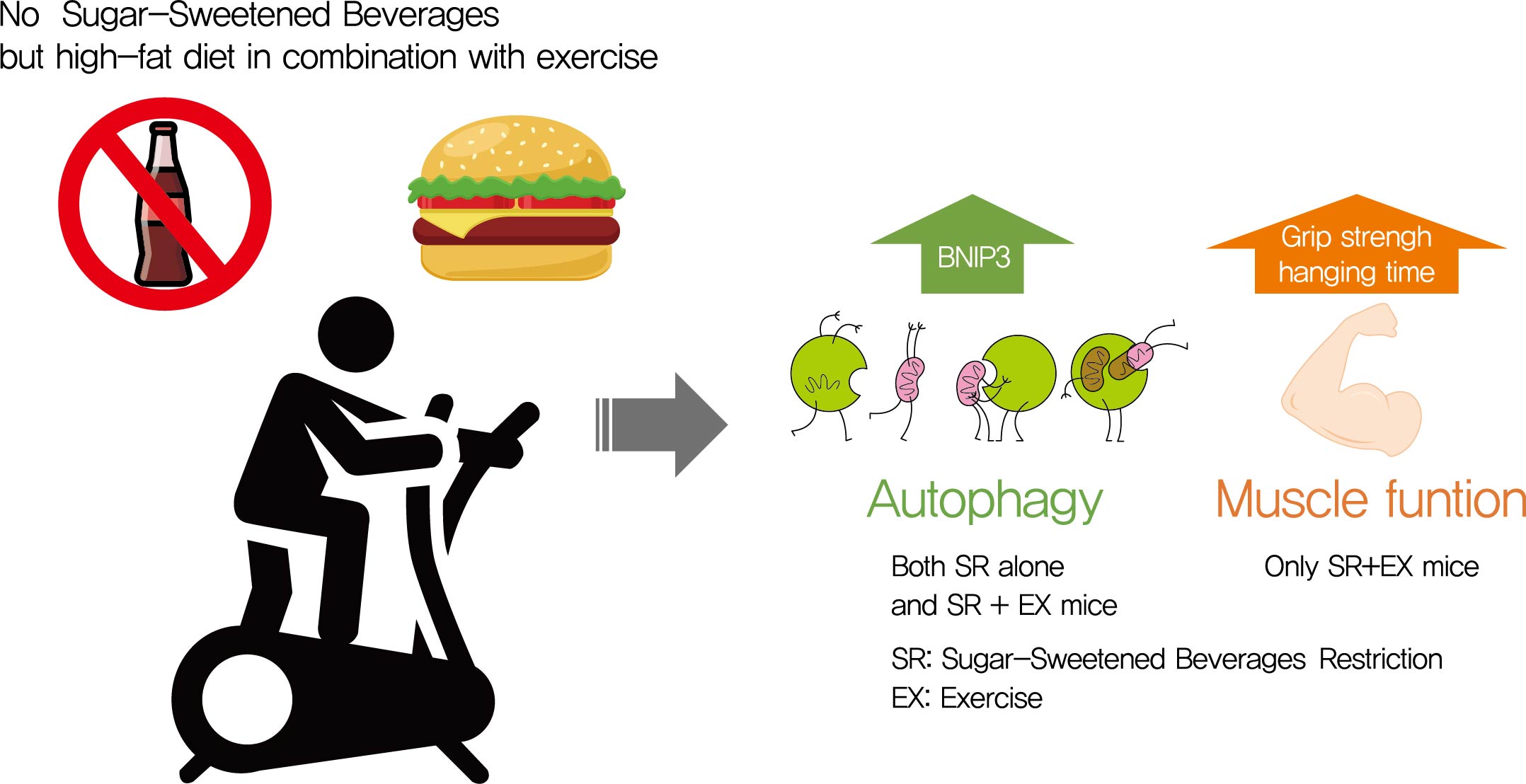
- 7,075 View
- 252 Download
- 5 Web of Science
- 6 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- Background
Autophagy maintains muscle mass and healthy skeletal muscles. Several recent studies have associated sugar-sweetened beverage (SSB) consumption with diseases. We investigated whether muscle dysfunction due to obesity could be restored by SSB restriction (SR) alone or in combination with exercise (EX) training.
Methods
Obese mice were subjected to SR combined with treadmill EX. Intraperitoneal glucose tolerance test, grip strength test, hanging time test, and body composition analysis were performed. Triglyceride (TG) and total cholesterol (TC) serum concentrations and TG concentrations in quadriceps muscles were analyzed. Western blot and reverse transcription-quantitative polymerase chain reaction helped analyze autophagy-related protein and mRNA expression, respectively.
Results
SR alone had no significant effect on fasting blood glucose levels, glucose tolerance, and muscle function. However, it had effect on serum TC, serum TG, and BCL2 interacting protein 3 expression. SR+EX improved glucose tolerance and muscle function and increased serum TC utilization than SR alone. SR+EX reduced P62 levels, increased glucose transporter type 4 and peroxisome proliferator-activated receptor γ coactivator-1α protein expression, and improved grip strength relative to the high-fat and high-sucrose liquid (HFHS) group, and this was not observed in the HFHS+EX group.
Conclusion
SR induced mitophagy-related protein expression in quadriceps, without affecting muscle function. And, the combination of SR and EX activated mitophagy-related proteins and improved muscle function. -
Citations
Citations to this article as recorded by- Mitochondrial Dysfunction, Oxidative Stress, and Inter-Organ Miscommunications in T2D Progression
Rajakrishnan Veluthakal, Diana Esparza, Joseph M. Hoolachan, Rekha Balakrishnan, Miwon Ahn, Eunjin Oh, Chathurani S. Jayasena, Debbie C. Thurmond
International Journal of Molecular Sciences.2024; 25(3): 1504. CrossRef - The association between healthy beverage index and sarcopenia in Iranian older adults: a case-control study
Marzieh Mahmoodi, Zainab Shateri, Mehran Nouri, Mohebat Vali, Nasrin Nasimi, Zahra Sohrabi, Mohammad Hossein Dabbaghmanesh, Maede Makhtoomi
BMC Geriatrics.2024;[Epub] CrossRef - Interplay of skeletal muscle and adipose tissue: sarcopenic obesity
Min Jeong Park, Kyung Mook Choi
Metabolism.2023; 144: 155577. CrossRef - Association between sugar-sweetened beverage consumption frequency and muscle strength: results from a sample of Chinese adolescents
Yunjie Zhang, Pan Xu, Yongjing Song, Nan Ma, Jinkui Lu
BMC Public Health.2023;[Epub] CrossRef - Muscle strength and prediabetes progression and regression in middle‐aged and older adults: a prospective cohort study
Shanhu Qiu, Xue Cai, Yang Yuan, Bo Xie, Zilin Sun, Duolao Wang, Tongzhi Wu
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(2): 909. CrossRef - INTENSITY OF FREE RADICAL PROCESSES IN RAT SKELETAL MUSCLES UNDER THE CONDITIONS OF DIFFERENT DIETARY SUPPLY WITH NUTRIENTS
O.M. Voloshchuk, Н.P. Kopylchuk
Fiziolohichnyĭ zhurnal.2022; 68(4): 48. CrossRef
- Mitochondrial Dysfunction, Oxidative Stress, and Inter-Organ Miscommunications in T2D Progression
- Clinical Impact of Dysglycemia in Patients with an Acute Myocardial Infarction (Diabetes Metab J 2021;45:270-4)
- Bo-Yeon Kim
- Diabetes Metab J. 2021;45(5):787-788. Published online September 30, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0061
- 2,732 View
- 82 Download

 KDA
KDA


 First
First Prev
Prev





