
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Previous issues
- Page Path
- HOME > Browse > Previous issues
- Basic Research
- Application of Animal Models in Diabetic Cardiomyopathy
- Wang-Soo Lee, Jaetaek Kim
- Diabetes Metab J. 2021;45(2):129-145. Published online March 25, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0285
- 9,153 View
- 332 Download
- 9 Web of Science
- 14 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 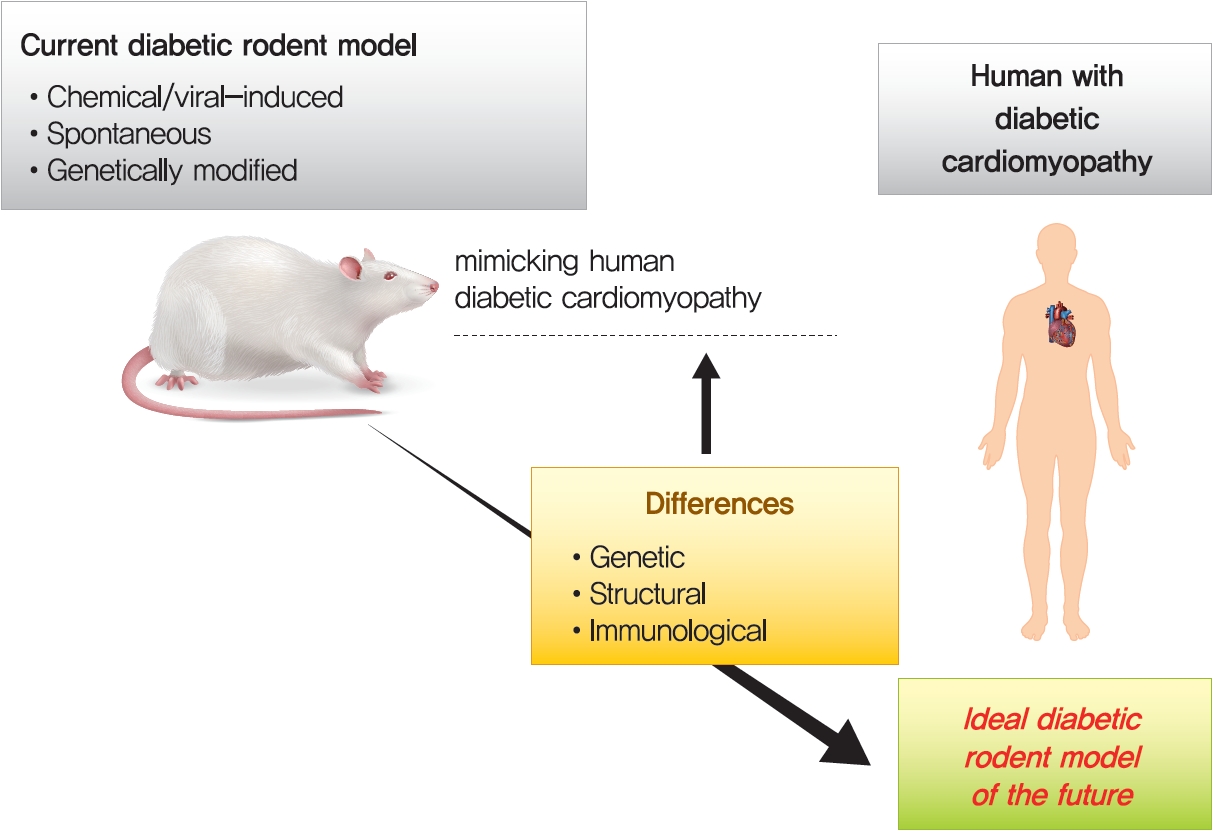
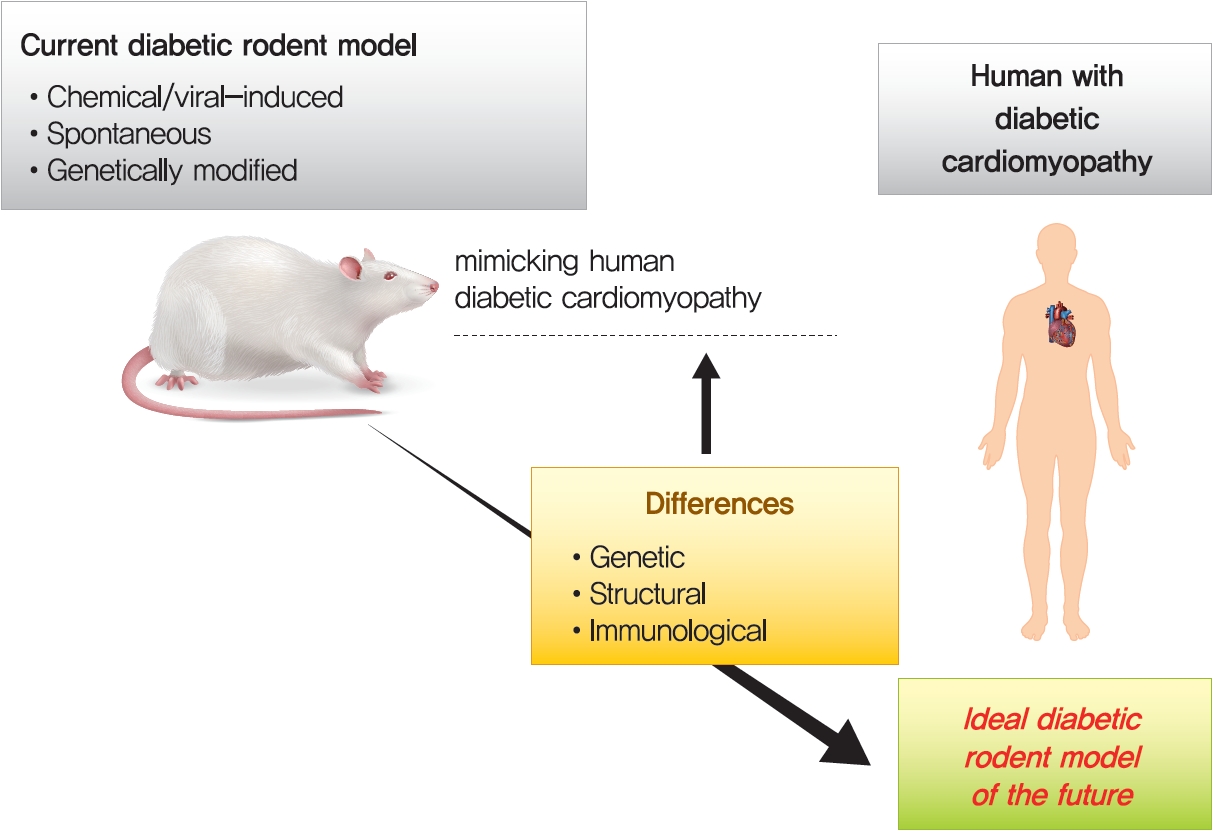
- Diabetic heart disease is a growing and important public health risk. Apart from the risk of coronary artery disease or hypertension, diabetes mellitus (DM) is a well-known risk factor for heart failure in the form of diabetic cardiomyopathy (DiaCM). Currently, DiaCM is defined as myocardial dysfunction in patients with DM in the absence of coronary artery disease and hypertension. The underlying pathomechanism of DiaCM is partially understood, but accumulating evidence suggests that metabolic derangements, oxidative stress, increased myocardial fibrosis and hypertrophy, inflammation, enhanced apoptosis, impaired intracellular calcium handling, activation of the renin-angiotensin-aldosterone system, mitochondrial dysfunction, and dysregulation of microRNAs, among other factors, are involved. Numerous animal models have been used to investigate the pathomechanisms of DiaCM. Despite some limitations, animal models for DiaCM have greatly advanced our understanding of pathomechanisms and have helped in the development of successful disease management strategies. In this review, we summarize the current pathomechanisms of DiaCM and provide animal models for DiaCM according to its pathomechanisms, which may contribute to broadening our understanding of the underlying mechanisms and facilitating the identification of possible new therapeutic targets.
-
Citations
Citations to this article as recorded by- Chitosan Versus Dapagliflozin in a Diabetic Cardiomyopathy Mouse Model
Georgică Târtea, Aurel Popa-Wagner, Veronica Sfredel, Smaranda Ioana Mitran, Alexandra Oltea Dan, Anca-Maria Țucă, Alexandra Nicoleta Preda, Victor Raicea, Eugen Țieranu, Dragoș Cozma, Radu Vătășescu
International Journal of Molecular Sciences.2024; 25(4): 2118. CrossRef - Mitochondrial energy metabolism in diabetic cardiomyopathy: Physiological adaption, pathogenesis, and therapeutic targets
Wanlin Ye, Kun Han, Maodi Xie, Sheyu Li, Guo Chen, Yanyan Wang, Tao Li
Chinese Medical Journal.2024; 137(8): 936. CrossRef - Liraglutide Attenuates Diabetic Cardiomyopathy via the ILK/PI3K/AKT/PTEN Signaling Pathway in Rats with Streptozotocin-Induced Type 2 Diabetes Mellitus
Shatha M. Alobaid, Rahaf M. Alshahrani, Asma S. Alonazi, Nawal M. Alrasheed, Maha A. Alamin, Tahani K. Alshammari, Anfal F. Bin Dayel, Doaa M. Elnagar, Rana R. Alotaibi, Lama A. Almuthnabi, Dalia H. Almasud, Shahad E. Al-Ammar, Shahad O. Almadhi, Reema A.
Pharmaceuticals.2024; 17(3): 374. CrossRef - An Overview of Diabetic Cardiomyopathy
Abdul Quaiyoom, Ranjeet Kumar
Current Diabetes Reviews.2024;[Epub] CrossRef - Evaluation and Management of Patients With Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
International Journal of Heart Failure.2023; 5(1): 1. CrossRef - Evaluation and Management of Patients with Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 10. CrossRef - Machine learning for spatial stratification of progressive cardiovascular dysfunction in a murine model of type 2 diabetes mellitus
Andrya J. Durr, Anna S. Korol, Quincy A. Hathaway, Amina Kunovac, Andrew D. Taylor, Saira Rizwan, Mark V. Pinti, John M. Hollander, Yoshihiro Fukumoto
PLOS ONE.2023; 18(5): e0285512. CrossRef - Hyperglycemic memory in diabetic cardiomyopathy
Jiabing Zhan, Chen Chen, Dao Wen Wang, Huaping Li
Frontiers of Medicine.2022; 16(1): 25. CrossRef - Murine Models of Obesity
Tânia Martins, Catarina Castro-Ribeiro, Sílvia Lemos, Tiago Ferreira, Elisabete Nascimento-Gonçalves, Eduardo Rosa, Paula Alexandra Oliveira, Luís Miguel Antunes
Obesities.2022; 2(2): 127. CrossRef - The Role of Mitochondria in Metabolic Syndrome–Associated Cardiomyopathy
Jiayu Li, Jingye Li, Yijun Chen, Wenyu Hu, Xuhe Gong, Hui Qiu, Hui Chen, Yanguo Xin, Hongwei Li, Tao Li
Oxidative Medicine and Cellular Longevity.2022; 2022: 1. CrossRef - Guidelines on models of diabetic heart disease
Lisa C. Heather, Anne D. Hafstad, Ganesh V. Halade, Romain Harmancey, Kimberley M. Mellor, Paras K. Mishra, Erin E. Mulvihill, Miranda Nabben, Michinari Nakamura, Oliver J. Rider, Matthieu Ruiz, Adam R. Wende, John R. Ussher
American Journal of Physiology-Heart and Circulatory Physiology.2022; 323(1): H176. CrossRef - Extracellular vesicle therapy for non-ischemic heart failure: A systematic review of preclinical studies
Ramana Vaka, Sophie Van Remortel, Valentina Ly, Darryl R. Davis
Extracellular Vesicle.2022; 1: 100009. CrossRef - Effect of a Six-week Endurance Exercise Program and Empagliflozin Consumption on Some Structural and Functional Indices of the Heart in Male Diabetic Rats
Eftekhar Mohammadi, Mohammad Fathi, Farzaneh Chehel Cheraghi, Afshin Nazari
journal of ilam university of medical sciences.2022; 30(3): 1. CrossRef - Cardiac Phosphodiesterases Are Differentially Increased in Diabetic Cardiomyopathy
Rita Hanna, Wared Nour-Eldine, Youakim Saliba, Carole Dagher-Hamalian, Pia Hachem, Pamela Abou-Khalil, Delphine Mika, Audrey Varin, Magali Samia El Hayek, Laëtitia Pereira, Nassim Farès, Grégoire Vandecasteele, Aniella Abi-Gerges
Life Sciences.2021; 283: 119857. CrossRef
- Chitosan Versus Dapagliflozin in a Diabetic Cardiomyopathy Mouse Model
- Cardiovascular Risk/Epidemiology
- Epidemiology, Pathophysiology, Diagnosis and Treatment of Heart Failure in Diabetes
- Jin Joo Park
- Diabetes Metab J. 2021;45(2):146-157. Published online March 25, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0282
- Correction in: Diabetes Metab J 2021;45(5):796
- 13,750 View
- 1,205 Download
- 51 Web of Science
- 54 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
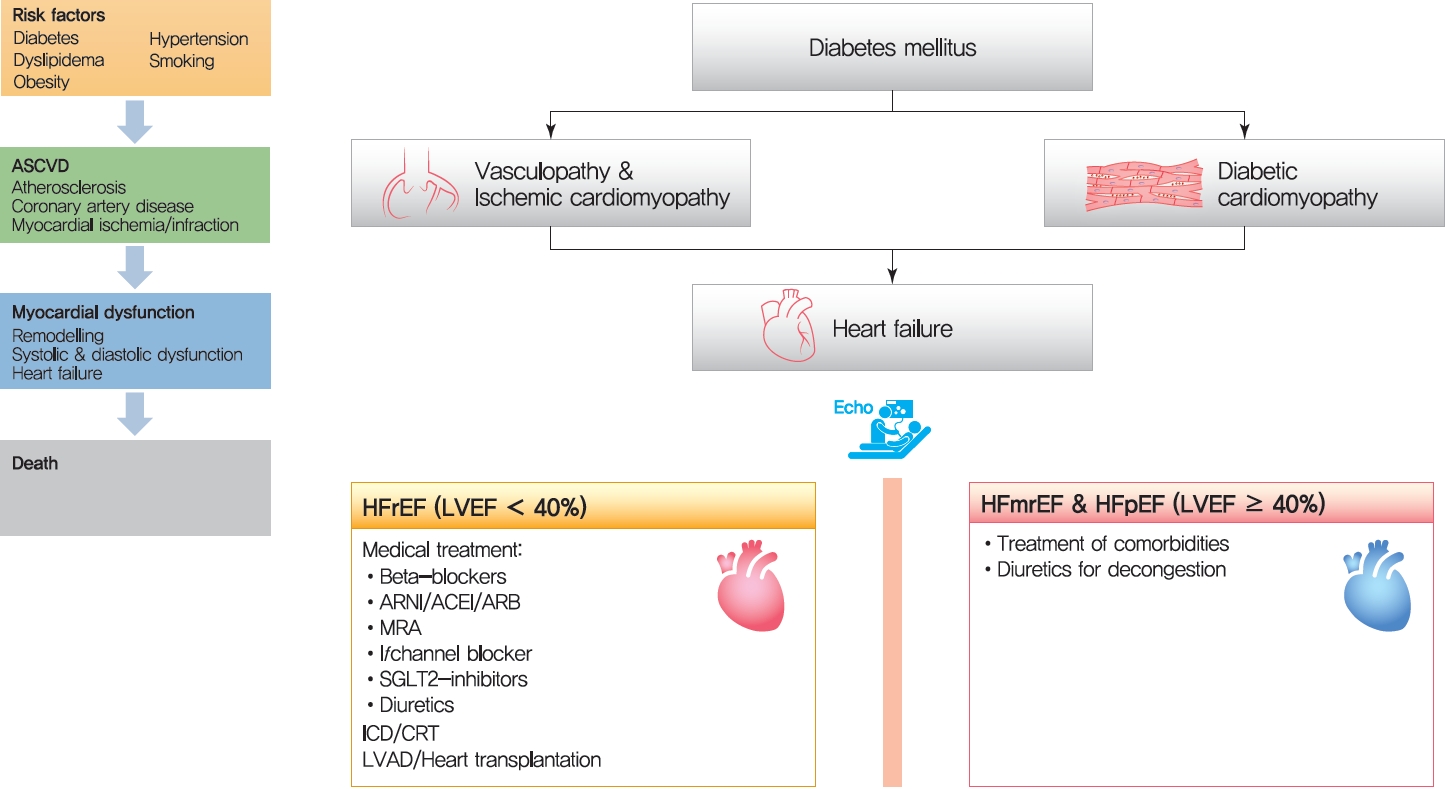
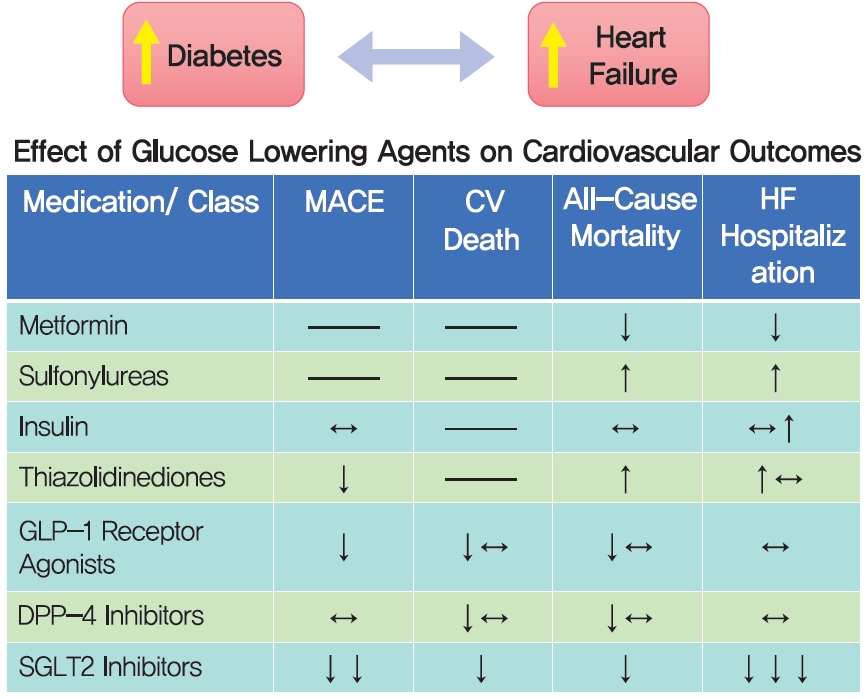
- The cardiovascular disease continuum begins with risk factors such as diabetes mellitus (DM), progresses to vasculopathy and myocardial dysfunction, and finally ends with cardiovascular death. Diabetes is associated with a 2- to 4-fold increased risk for heart failure (HF). Moreover, HF patients with DM have a worse prognosis than those without DM. Diabetes can cause myocardial ischemia via micro- and macrovasculopathy and can directly exert deleterious effects on the myocardium. Hyperglycemia, hyperinsulinemia, and insulin resistance can cause alterations in vascular homeostasis. Then, reduced nitric oxide and increased reactive oxygen species levels favor inflammation leading to atherothrombotic progression and myocardial dysfunction. The classification, diagnosis, and treatment of HF for a patient with and without DM remain the same. Until now, drugs targeting neurohumoral and metabolic pathways improved mortality and morbidity in HF with reduced ejection fraction (HFrEF). Therefore, all HFrEF patients should receive guideline-directed medical therapy. By contrast, drugs modulating neurohumoral activity did not improve survival in HF with preserved ejection fraction (HFpEF) patients. Trials investigating whether sodium-glucose cotransporter-2 inhibitors are effective in HFpEF are on-going. This review will summarize the epidemiology, pathophysiology, and treatment of HF in diabetes.
-
Citations
Citations to this article as recorded by- Efficacy of Platelet-Rich Plasma in the Treatment of Diabetic Foot Ulcers: A Systematic Review and Meta-Analysis
Yundong Peng, JiePing Wang, Xinyao Liu, Yanqing Zhou, Shaohui Jia, Jinrong Xu, Cheng Zheng
Annals of Vascular Surgery.2024; 98: 365. CrossRef - Diabetic Cardiomyopathy: 2023 Update by the International Multidisciplinary Board of Experts
Ashot Avagimyan, Federica Fogacci, Nana Pogosova, Lev Kakrurskiy, Eugenia Kogan, Olga Urazova, Zhanna Kobalava, Liudmila Mikhaleva, Rositsa Vandysheva, Gioeva Zarina, Artem Trofimenko, Grizelda Navasardyan, Lusine Mkrtchyan, Mattia Galli, Zinaida Jndoyan,
Current Problems in Cardiology.2024; 49(1): 102052. CrossRef - Emerging Biomarkers in the Laboratory and in Practice: A Novel Approach to Diagnosing Heart Failure in Diabetes
Rachel E. Aaron, Tiffany Tian, G. Alexander Fleming, David B. Sacks, James L. Januzzi, Rodica Pop-Busui, Ibrahim A. Hashim, Alan H. B. Wu, Ambarish Pandey, David C. Klonoff
Journal of Diabetes Science and Technology.2024;[Epub] CrossRef - Research Progress on the Relationship between HbA1c and Diabetes Complicated with Chronic Heart Failure
·依沙 迪达尔
Advances in Clinical Medicine.2024; 14(01): 1117. CrossRef - Association Between Use of Sodium-Glucose Cotransporter-2 Inhibitors or Angiotensin Receptor-Neprilysin Inhibitor and the Risk of Atherosclerotic Cardiovascular Disease With Coexisting Diabetes and Heart Failure
Ya-Wen Lin, Chun-Hsiang Lin, Cheng-Li Lin, Che-Huei Lin, Ming-Hung Lin
Journal of Cardiovascular Pharmacology and Therapeutics.2024;[Epub] CrossRef - The Role of Epicardial Adipose Tissue in Acute Coronary Syndromes, Post-Infarct Remodeling and Cardiac Regeneration
Kamil Krauz, Marcel Kempiński, Paweł Jańczak, Karol Momot, Maciej Zarębiński, Izabela Poprawa, Małgorzata Wojciechowska
International Journal of Molecular Sciences.2024; 25(7): 3583. CrossRef - Molecular mechanisms of metabolic dysregulation in diabetic cardiomyopathy
Yue Zeng, Yilang Li, Wenyue Jiang, Ning Hou
Frontiers in Cardiovascular Medicine.2024;[Epub] CrossRef - Association between nonalcoholic fatty liver disease and left ventricular diastolic dysfunction: A 7-year retrospective cohort study of 3,496 adults using serial echocardiography
Gyuri Kim, Tae Yang Yu, Jae Hwan Jee, Ji Cheol Bae, Mira Kang, Jae Hyeon Kim
Diabetes & Metabolism.2024; : 101534. CrossRef - SGLT2 Inhibitors in the Cardiovascular Disease
Jin Joo Park
The Journal of Korean Diabetes.2024; 25(1): 26. CrossRef - Metabolic Alteration Bridging the Prediabetic State and Colorectal Cancer
Antonino Colloca, Isabella Donisi, Camilla Anastasio, Maria Luisa Balestrieri, Nunzia D’Onofrio
Cells.2024; 13(8): 663. CrossRef - Inflammation in diabetes complications: molecular mechanisms and therapeutic interventions
Lu Zhao, Haoran Hu, Lin Zhang, Zheting Liu, Yunchao Huang, Qian Liu, Liang Jin, Meifei Zhu, Ling Zhang
MedComm.2024;[Epub] CrossRef - Methods to predict heart failure in diabetes patients
Alexander E. Berezin, Tetiana A Berezina, Uta C. Hoppe, Michael Lichtenauer, Alexander A. Berezin
Expert Review of Endocrinology & Metabolism.2024; : 1. CrossRef - Association between Dapagliflozin, Cardiac Biomarkers and Cardiac Remodeling in Patients with Diabetes Mellitus and Heart Failure
Andrew Xanthopoulos, Nikolaos Katsiadas, Spyridon Skoularigkis, Dimitrios E. Magouliotis, Niki Skopeliti, Sotirios Patsilinakos, Alexandros Briasoulis, Filippos Triposkiadis, John Skoularigis
Life.2023; 13(8): 1778. CrossRef - Empagliflozin for Patients with Heart Failure and Type 2 Diabetes Mellitus: Clinical Evidence in Comparison with Other Sodium-Glucose Co-transporter-2 Inhibitors and Potential Mechanism
Bo Liang, Rui Li, Peng Zhang, Ning Gu
Journal of Cardiovascular Translational Research.2023; 16(2): 327. CrossRef - Causes and Determinants of Heart Failure Readmissions Post Transcutaneous Aortic Valve Replacement: A Systematic Review and Meta-Analysis
Farah Yasmin, Muhammad Aamir, Abdul Moeed, Kinza Iqbal, Aymen Iqbal, Muhammad Sohaib Asghar, Waqas Ullah, Indranee Rajapreyar, Yevgeniy Brailovsky
Current Problems in Cardiology.2023; 48(1): 101428. CrossRef - Discussion of a study on the role of EMS in prognosis of elderly patients with AHF
Qingzhuo Yang, Hui Wu, Di Liu, Yunzhao Li, Gang Zhou, Dong Zhang, Yanfang Liu, Yi Li
International Journal of Cardiology.2023; 377: 91. CrossRef - The management correlation between metabolic index, cardiovascular health, and diabetes combined with cardiovascular disease
Yi Zhang, Chao Liu, Yijing Xu, Yanlei Wang, Fang Dai, Honglin Hu, Tian Jiang, Yunxia Lu, Qiu Zhang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Evaluation and Management of Patients With Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
International Journal of Heart Failure.2023; 5(1): 1. CrossRef - Evaluation and Management of Patients with Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 10. CrossRef - Lower Circulating Cell-Free Mitochondrial DNA Is Associated with Heart Failure in Type 2 Diabetes Mellitus Patients
Tetiana A. Berezina, Mykola P. Kopytsya, Olga V. Petyunina, Alexander A. Berezin, Zeljko Obradovic, Lukas Schmidbauer, Michael Lichtenauer, Alexander E. Berezin
Cardiogenetics.2023; 13(1): 15. CrossRef - Novel model predicts diastolic cardiac dysfunction in type 2 diabetes
Mingyu Hao, Xiaohong Huang, Xueting Liu, Xiaokang Fang, Haiyan Li, Lingbo Lv, Liming Zhou, Tiecheng Guo, Dewen Yan
Annals of Medicine.2023; 55(1): 766. CrossRef - Cholinergic drugs reduce metabolic inflammation and diabetic myocardial injury by regulating the gut bacterial component lipopolysaccharide‐induced ERK/Egr‐1 pathway
Qing Wu, Ming Zhao, Dongling Li, Xi He, Weijin Zang
The FASEB Journal.2023;[Epub] CrossRef - Ferroptosis: roles and molecular mechanisms in diabetic cardiomyopathy
Yangting Zhao, Binjing Pan, Xiaoyu Lv, Chongyang Chen, Kai Li, Yawen Wang, Jingfang Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Cardiorenal syndrome and diabetes: an evil pairing
Ana Belén Méndez Fernández, Ander Vergara Arana, Aleix Olivella San Emeterio, Maria Antonieta Azancot Rivero, Toni Soriano Colome, Maria Jose Soler Romeo
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Therapeutic Potential of Hibiscus sabdariffa Linn. in Attenuating Cardiovascular Risk Factors
Syaifuzah Sapian, Asma Ali Ibrahim Mze, Fatin Farhana Jubaidi, Nor Anizah Mohd Nor, Izatus Shima Taib, Zariyantey Abd Hamid, Satirah Zainalabidin, Nur Najmi Mohamad Anuar, Haliza Katas, Jalifah Latip, Juriyati Jalil, Nur Faizah Abu Bakar, Siti Balkis Budi
Pharmaceuticals.2023; 16(6): 807. CrossRef - Exploring the prospect of intrinsic wave propagation in evaluating myocardial stiffness among patients with type 2 diabetes
Qiao Cheng, Xiao Huang, Xinying Fan, Jie Sun, Jun Zhang, Qiaoying Tang, Youbin Deng, Xiaojun Bi
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - The multidimensional prognostic index (MPI) predicts long-term mortality in old type 2 diabetes mellitus patients: a 13-year follow-up study
F. Salis, E. Cossu, A. Mandas
Journal of Endocrinological Investigation.2023; 47(1): 191. CrossRef - PRDM16 exerts critical role in myocardial metabolism and energetics in type 2 diabetes induced cardiomyopathy
Tongtong Hu, Qingqing Wu, Qi Yao, Jiabin Yu, Kebing Jiang, Ying Wan, Qizhu Tang
Metabolism.2023; 146: 155658. CrossRef - Empagliflozin Reduces Interleukin-6 Levels in Patients with Heart Failure
Michael Gotzmann, Pauline Henk, Ulrik Stervbo, Arturo Blázquez-Navarro, Andreas Mügge, Nina Babel, Timm H. Westhoff
Journal of Clinical Medicine.2023; 12(13): 4458. CrossRef - Features of the course and complications of acute myocardial infarction in type 2 diabetes mellitus
M. N. Zatsepina, F. O. Ushanova, T. L. Bogacheva
FOCUS. Endocrinology.2023; 4(2): 42. CrossRef - Admission triglyceride-glucose index is predictor of long-term mortality and appropriate implantable cardiac defibrillator therapy in patients with heart failure
Kazım S Özcan, Mert İ Hayıroğlu, Tufan Çınar
Biomarkers in Medicine.2023; 17(10): 487. CrossRef - Emerging Roles of Phospholipase C Beta Isozymes as Potential Biomarkers in Cardiac Disorders
Antonietta Fazio, Camilla Evangelisti, Alessandra Cappellini, Sara Mongiorgi, Foteini-Dionysia Koufi, Irene Neri, Maria Vittoria Marvi, Michele Russo, Alessandra Ghigo, Lucia Manzoli, Roberta Fiume, Stefano Ratti
International Journal of Molecular Sciences.2023; 24(17): 13096. CrossRef - Research progress of dihydromyricetin in the treatment of diabetes mellitus
Ziyuan Wang, Zhuoran Cao, Zhiying Yue, Zhengfeng Yang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Assessment of subclinical left ventricular myocardial systolic dysfunction in type 2 diabetes mellitus patients with or without hypertension by global and segmental myocardial work
Guang-An Li, Jun Huang, Xiao Sheng, Li Fan
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Managing heart failure in diabetics with dual acting sotagliflozin—A review
Kushal Seni, Pooja A Chawla
Health Sciences Review.2023; 9: 100130. CrossRef - Association between triglyceride glucose-body mass index and heart failure in subjects with diabetes mellitus or prediabetes mellitus: a cross-sectional study
Shuping Yang, Xiangxiang Shi, Wanlu Liu, Zhaokai Wang, Ruoshui Li, Xianzhi Xu, Chaofan Wang, Lei Li, Ruili Wang, Tongda Xu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Influence of Sociodemographic Variables and Healthy Habits on the Values of Insulin Resistance Indicators in 386,924 Spanish Workers
Miguel Mestre Font, Carla Busquets-Cortés, José Ignacio Ramírez-Manent, Pilar Tomás-Gil, Hernán Paublini, Ángel Arturo López-González
Nutrients.2023; 15(24): 5122. CrossRef - The effect of dapagliflozin on ventricular arrhythmias, cardiac arrest, or sudden death in people with heart failure: a tick in another box for sodium-glucose cotransporter 2 inhibitors
Theocharis Koufakis, George Giannakoulas, Pantelis Zebekakis, Kalliopi Kotsa
Expert Opinion on Pharmacotherapy.2022; 23(3): 321. CrossRef - The peculiar role of vitamin D in the pathophysiology of cardiovascular and neurodegenerative diseases
Milijana Janjusevic, Giulia Gagno, Alessandra Lucia Fluca, Laura Padoan, Antonio Paolo Beltrami, Gianfranco Sinagra, Rita Moretti, Aneta Aleksova
Life Sciences.2022; 289: 120193. CrossRef - Mechanisms of cardiac dysfunction in diabetic cardiomyopathy: molecular abnormalities and phenotypical variants
Francesca Romana Prandi, Isabella Evangelista, Domenico Sergi, Alberto Palazzuoli, Francesco Romeo
Heart Failure Reviews.2022; 28(3): 597. CrossRef - Modern Approaches to Treatment of Chronic Heart Failure in Patients with Type 2 Diabetes Mellitus
Yu. G. Gorb, S. A. Serik, O. V. Tkachenko, V. V. Ryabukha
Ukraïnsʹkij žurnal medicini, bìologìï ta sportu.2022; 7(1): 14. CrossRef - Metabonomic Characteristics of Myocardial Diastolic Dysfunction in Type 2 Diabetic Cardiomyopathy Patients
Mingyu Hao, Jianxin Deng, Xiaohong Huang, Haiyan Li, Huiting Ou, Xiangsheng Cai, Jiajie She, Xueting Liu, Ling Chen, Shujuan Chen, Wenlan Liu, Dewen Yan
Frontiers in Physiology.2022;[Epub] CrossRef - Serum Levels of Irisin Predict Cumulative Clinical Outcomes in Heart Failure Patients With Type 2 Diabetes Mellitus
Alexander A. Berezin, Michael Lichtenauer, Elke Boxhammer, Ivan M. Fushtey, Alexander E. Berezin
Frontiers in Physiology.2022;[Epub] CrossRef - Heart Failure: An Underappreciated Complication of Diabetes. A Consensus Report of the American Diabetes Association
Rodica Pop-Busui, James L. Januzzi, Dennis Bruemmer, Sonia Butalia, Jennifer B. Green, William B. Horton, Colette Knight, Moshe Levi, Neda Rasouli, Caroline R. Richardson
Diabetes Care.2022; 45(7): 1670. CrossRef - Von Willebrand factor (vWF) in patients with heart failure with preserved ejection fraction (HFpEF): A retrospective observational study
Mayila Abudoukelimu, Bayinsilema Ba, Yan Kai Guo, Jie Xu
Medicine.2022; 101(31): e29854. CrossRef - Why Does the Intravenous Iron Supplementation Not Work in Heart Failure Patients on Hemodialysis?
Jin Joo Park
CardioMetabolic Syndrome Journal.2022; 2(2): 176. CrossRef - Severe hypoglycemia and risk of hospitalization for heart failure in adults with diabetes treated with oral medications with or without insulin: A population-based study
You-Bin Lee, Yoon-Jong Bae, Hoseob Kim, Jiyun Park, So Yoon Kwon, So Hee Park, Gyuri Kim, Kyu Yeon Hur, Jae Hyeon Kim, Sang-Man Jin
Diabetes Research and Clinical Practice.2022; 192: 110083. CrossRef - Blood Pressure Target in Type 2 Diabetes Mellitus
Hyun-Jin Kim, Kwang-il Kim
Diabetes & Metabolism Journal.2022; 46(5): 667. CrossRef - Application Value of Systemic Inflammatory Indexes in the Clinical Evaluation of Patients with Heart Failure with Preserved Ejection Fraction (HFpEF)
Ruxin Wang, Juan Wu, Haowen Ye, Xiaofang Zhang, Lihong Wang
Medicina.2022; 58(10): 1473. CrossRef - HFpEF and Atrial Fibrillation: The Enigmatic Interplay of Dysmetabolism, Biomarkers, and Vascular Endothelial Dysfunction
Jure Bosanac, Lara Straus, Marko Novaković, Daniel Košuta, Mojca Božič Mijovski, Jerneja Tasič, Borut Jug, Azizah Ugusman
Disease Markers.2022; 2022: 1. CrossRef - The importance of caveolin as a target in the prevention and treatment of diabetic cardiomyopathy
Weiyi Xia, Xia Li, Qingping Wu, Aimin Xu, Liangqing Zhang, Zhengyuan Xia
Frontiers in Immunology.2022;[Epub] CrossRef - Microvascular Burden and Incident Heart Failure Among Middle-Aged and Older Adults With Type 1 or Type 2 Diabetes
Fu-Rong Li, Daniel Nyarko Hukportie, Jing Yang, Huan-Huan Yang, Guo-Chong Chen, Xian-Bo Wu
Diabetes Care.2022; 45(12): 2999. CrossRef - C-reactive protein and statins in heart failure with reduced and preserved ejection fraction
Jin Joo Park, Minjae Yoon, Hyoung-Won Cho, Hyun-Jai Cho, Kye Hun Kim, Dong Heon Yang, Byung-Su Yoo, Seok-Min Kang, Sang Hong Baek, Eun-Seok Jeon, Jae-Joong Kim, Myeong-Chan Cho, Shung Chull Chae, Byung-Hee Oh, Dong-Ju Choi
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Pharmacological treatment of type 2 diabetes in elderly patients with heart failure: randomized trials and beyond
Angela Sciacqua, Elena Succurro, Giuseppe Armentaro, Sofia Miceli, Daniele Pastori, Giuseppe Rengo, Giorgio Sesti
Heart Failure Reviews.2021; 28(3): 667. CrossRef
- Efficacy of Platelet-Rich Plasma in the Treatment of Diabetic Foot Ulcers: A Systematic Review and Meta-Analysis
- Cardiovascular Risk/Epidemiology
- Diabetes Management in Patients with Heart Failure
- Jia Shen, Barry H. Greenberg
- Diabetes Metab J. 2021;45(2):158-172. Published online March 25, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0296
- 8,096 View
- 493 Download
- 6 Web of Science
- 9 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 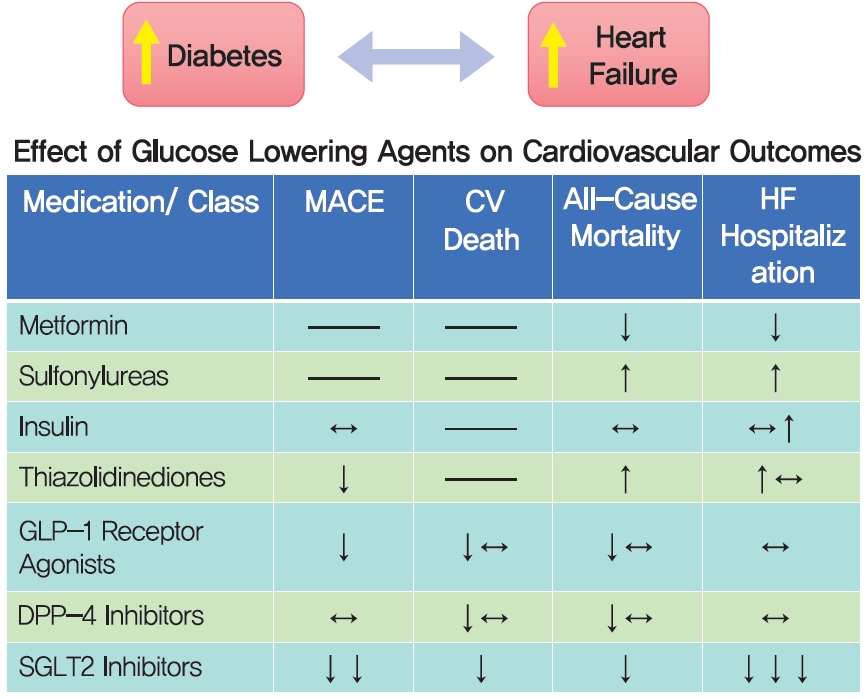
- Diabetes and heart failure (HF) are common diseases, each affecting large segments of the world population. Moreover, prevalence rates for both are expected to rise dramatically over coming decades. The high prevalence rates of both diseases and wellrecognized association of diabetes as a risk factor for HF make it inevitable that both diseases co-exist in a large number of patients, complicating their management and increasing the risk of a poor outcome. Management of diabetes has been shown to impact clinical events in patients with HF and there is emerging evidence that agents used to treat diabetes can reduce HF events, even in non-diabetic patients. In this review we summarize the clinical course and treatment of patients with type 2 diabetes mellitus (T2DM) and HF and review the efficacy and safety of pharmacological agents in patients with T2DM at risk for HF and those with established disease.
-
Citations
Citations to this article as recorded by- Letter to Editor From Banerjee et al: “Glucagon-Like Peptide-1 Receptor Agonists Across the Spectrum of Heart Failure”
Mainak Banerjee, Indira Maisnam, Satinath Mukhopadhyay
The Journal of Clinical Endocrinology & Metabolism.2024; 109(2): e873. CrossRef - Evaluation and Management of Patients With Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
International Journal of Heart Failure.2023; 5(1): 1. CrossRef - Prevalence and management of hyperkalemia in chronic kidney disease and heart failure patients in the Gulf Cooperation Council (GCC)
Ali AlSahow, Mohammad AbdulShafy, Saeed Al‐Ghamdi, Harith AlJoburi, Osama AlMogbel, Fadel Al‐Rowaie, Nizar Attallah, Feras Bader, Hisham Hussein, Mohamed Hassan, Khaldoun Taha, Matthew R. Weir, Faiez Zannad
The Journal of Clinical Hypertension.2023; 25(3): 251. CrossRef - Evaluation and Management of Patients with Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 10. CrossRef - Prescription appropriateness of anti-diabetes drugs in elderly patients hospitalized in a clinical setting: evidence from the REPOSI Register
Elena Succurro, Alessio Novella, Alessandro Nobili, Federica Giofrè, Franco Arturi, Angela Sciacqua, Francesco Andreozzi, Antonello Pietrangelo, Giorgio Sesti, Francesco Perticone, Francesco Violi, Salvatore Corrao, Alessandra Marengoni, Mauro Tettamanti,
Internal and Emergency Medicine.2023; 18(4): 1049. CrossRef - Re-evaluation of dipeptidyl peptidase-4 inhibitors in patients with heart failure and diabetes mellitus
Jiaoran Li, Yanping Liu, Panpan Hao
Diabetes Research and Clinical Practice.2023; 202: 110798. CrossRef - Managing heart failure in diabetics with dual acting sotagliflozin—A review
Kushal Seni, Pooja A Chawla
Health Sciences Review.2023; 9: 100130. CrossRef - Effect of Integrated Care on Patients With Atrial Fibrillation: A Systematic Review of Randomized Controlled Trials
Yi Li, Wenjing Zhao, Jun Huang, Murui Zheng, Peng Hu, Jiahai Lu, Hai Deng, Xudong Liu
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Pharmacological treatment of type 2 diabetes in elderly patients with heart failure: randomized trials and beyond
Angela Sciacqua, Elena Succurro, Giuseppe Armentaro, Sofia Miceli, Daniele Pastori, Giuseppe Rengo, Giorgio Sesti
Heart Failure Reviews.2021; 28(3): 667. CrossRef
- Letter to Editor From Banerjee et al: “Glucagon-Like Peptide-1 Receptor Agonists Across the Spectrum of Heart Failure”
- Skeletal Muscle Should Not Be Overlooked
- Ji A Seo
- Diabetes Metab J. 2021;45(2):173-174. Published online March 25, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0024
- 3,285 View
- 123 Download
- Metabolic Risk/Epidemiology
- Insulin Resistance Increases Serum Immunoglobulin E Sensitization in Premenopausal Women
- Seung Eun Lee, Ji Yeon Baek, Kyungdo Han, Eun Hee Koh
- Diabetes Metab J. 2021;45(2):175-182. Published online April 14, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0150
- 6,195 View
- 123 Download
- 1 Web of Science
- 1 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 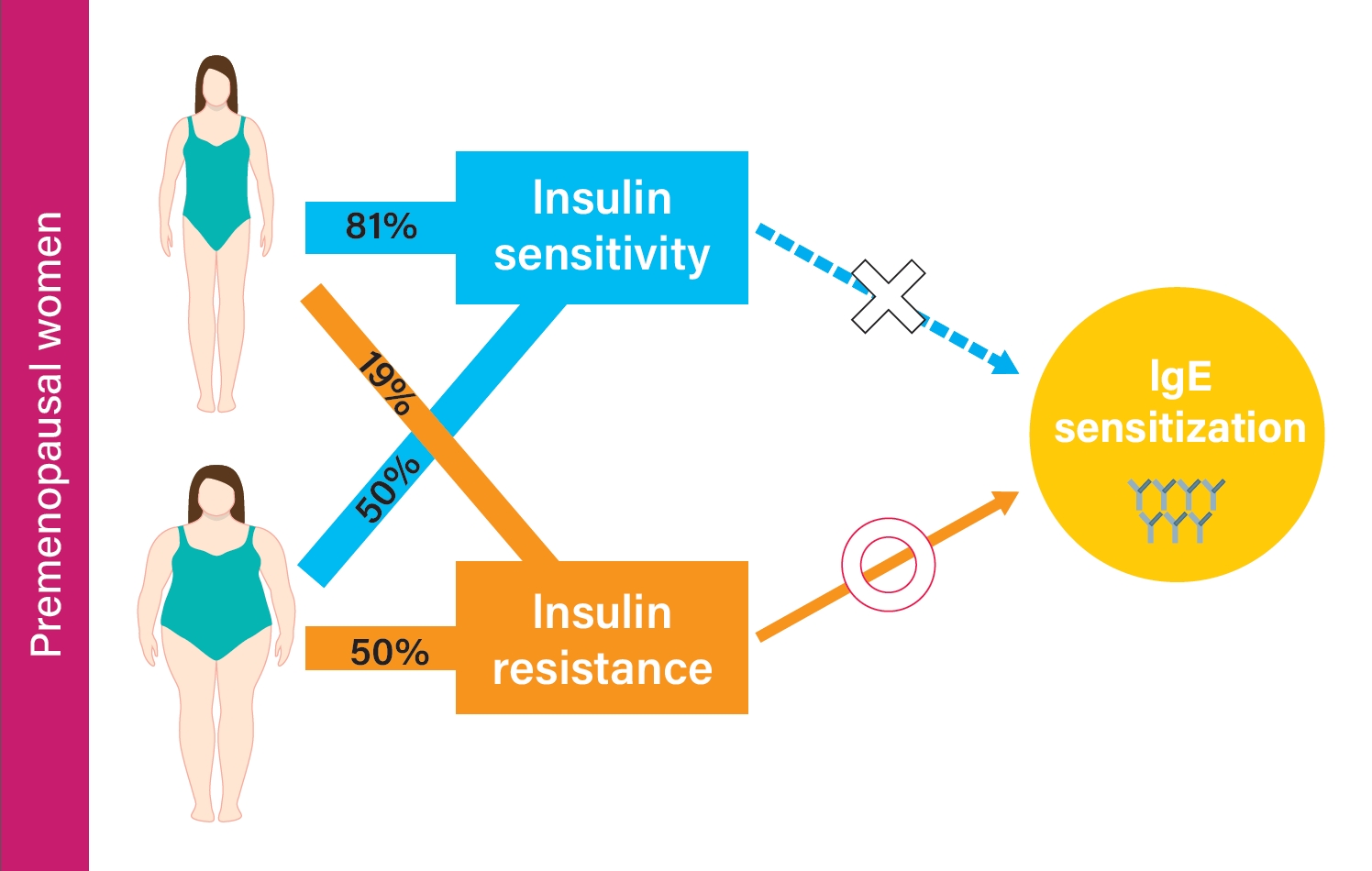
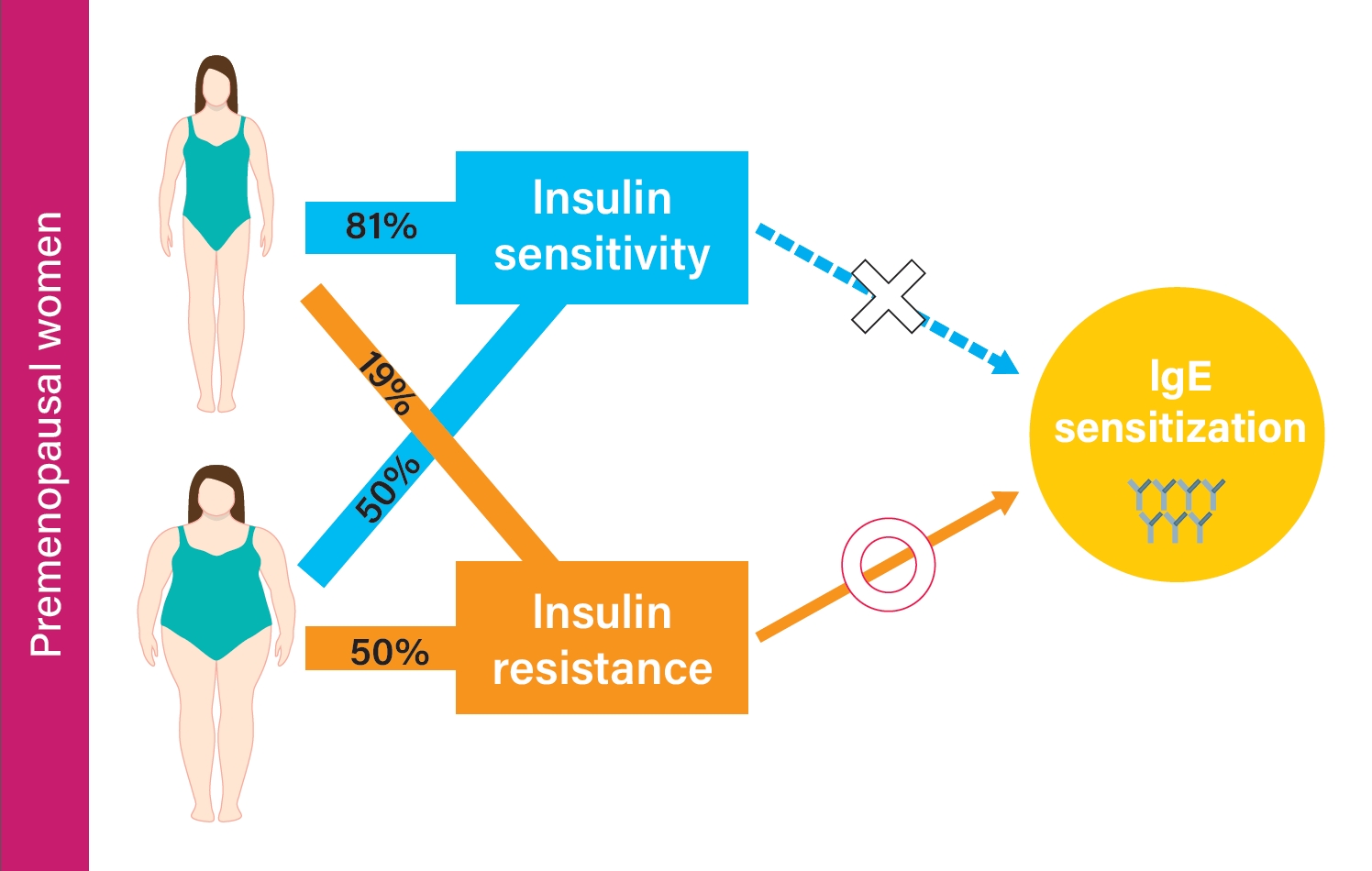
Background Although studies have shown that obesity is associated with aeroallergen sensitization (atopy), controversy still exists. We aimed to investigate the association between metabolic status, obesity, and atopy stratified by sex and menopausal status.
Methods A total of 1,700 adults from the 2010 Korean National Health and Nutrition Examination Survey were classified into metabolically healthy nonobese (MHNO), metabolically unhealthy nonobese (MUNO), metabolically healthy obese (MHO), and metabolically unhealthy obese (MUO) by body mass index and insulin resistance. Atopy was defined as a positive response to at least one aeroallergen. Multiple regression analysis was used to evaluate the risk of immunoglobulin E (IgE) elevation or atopy in relation to the degree of metabolic abnormality and obesity.
Results In premenopausal women, total IgE was positively correlated with obesity and insulin resistance. MUNO participants had a higher risk of having elevated total IgE compared to MHNO participants (odds ratio [OR], 2.271; 95% confidence interval [CI], 1.201 to 4.294), while MHO participants did not show a significant difference (OR, 1.435; 95% CI, 0.656 to 3.137) in premenopausal women. MUNO, but not MHO was also associated with atopy (OR, 2.157; 95% CI, 1.284 to 3.625). In men and postmenopausal women, there was no significant difference between metabolic status, obesity, and atopy among groups.
Conclusion Increased insulin resistance is associated with total IgE and atopy in premenopausal women but not in postmenopausal women or men.
-
Citations
Citations to this article as recorded by- Is There a Relationship between Insulin Resistance and Eosinophil, Inflammatory Parameters Neutrophil to lymphocyte ratio, C-Reactive Protein Values?
Meltem YİĞİT, Özgür OLUKMAN
Medical Records.2024; 6(1): 32. CrossRef
- Is There a Relationship between Insulin Resistance and Eosinophil, Inflammatory Parameters Neutrophil to lymphocyte ratio, C-Reactive Protein Values?
- Metabolic Risk/Epidemiology
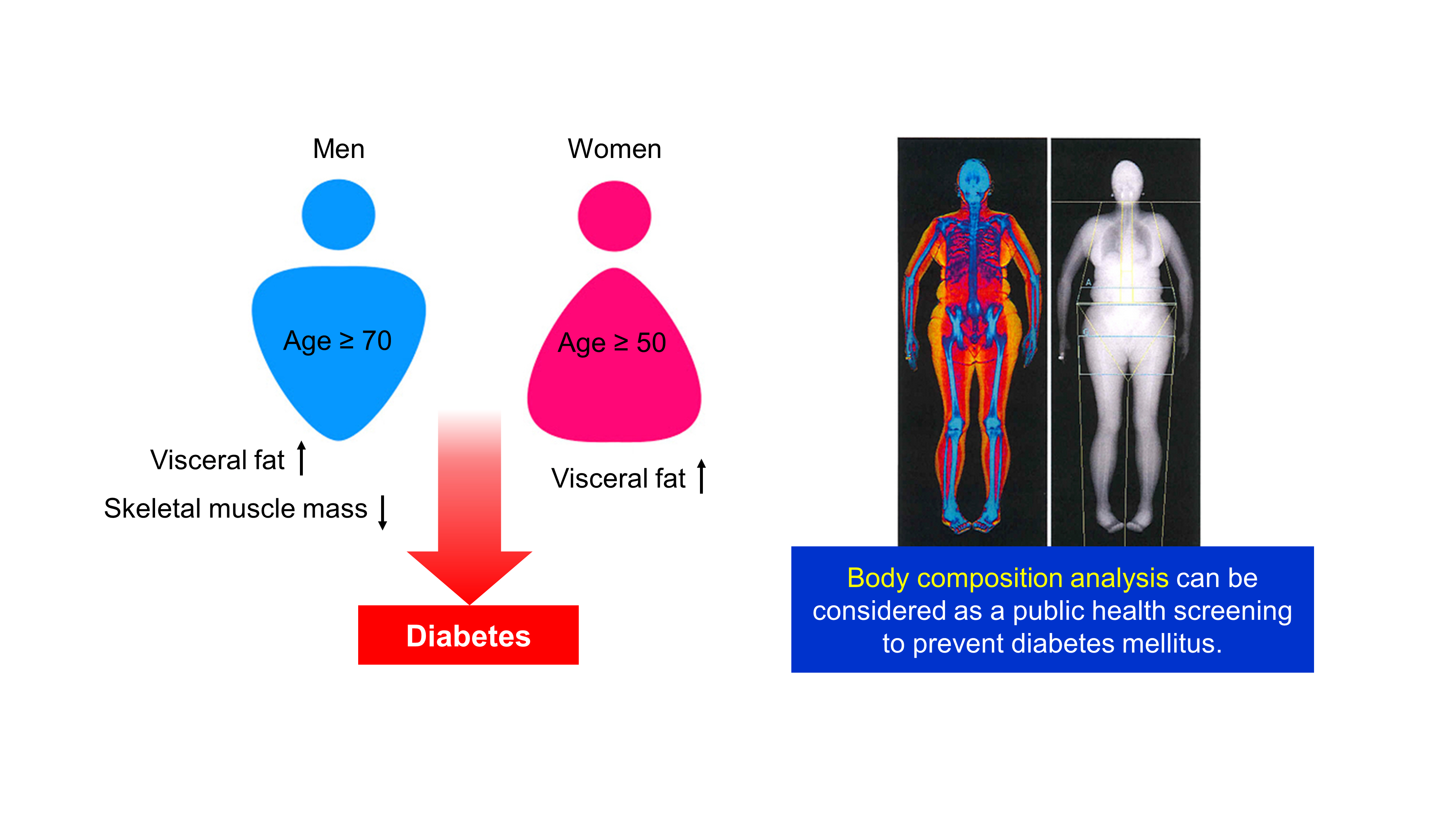
- Age- and Sex-Related Differential Associations between Body Composition and Diabetes Mellitus
- Eun Roh, Soon Young Hwang, Jung A Kim, You-Bin Lee, So-hyeon Hong, Nam Hoon Kim, Ji A Seo, Sin Gon Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
- Diabetes Metab J. 2021;45(2):183-194. Published online June 16, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0171
- 7,441 View
- 236 Download
- 3 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 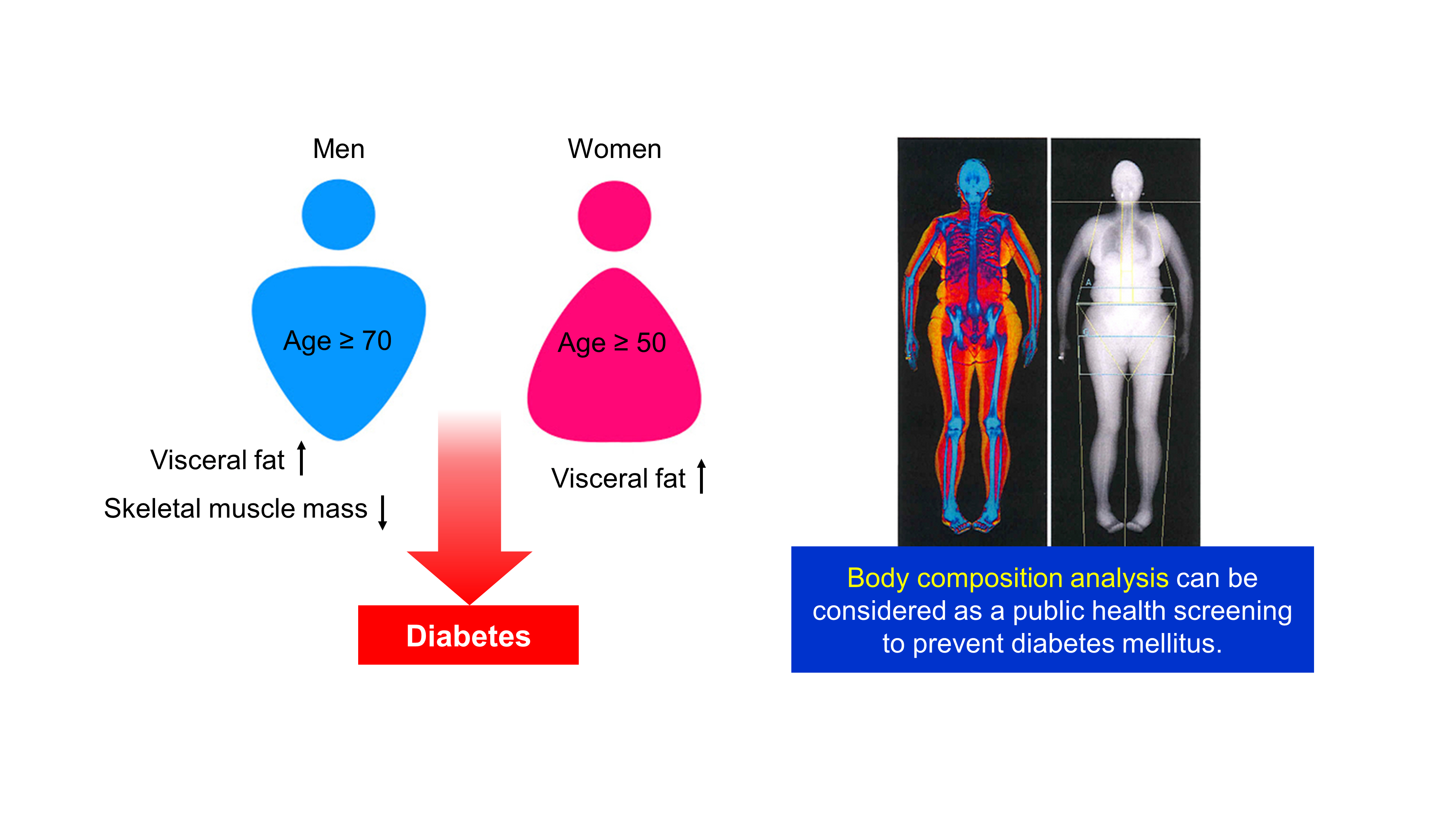
Background The age- and sex-related differences on the impacts of body composition on diabetes mellitus (DM) remain uncertain.
Methods The fourth and fifth Korea National Health and Nutrition Examination Survey included 15,586 subjects over 30 years of age who completed dual-energy X-ray absorptiometry. We conducted a cross-sectional study to investigate whether muscle mass index (MMI), defined as appendicular skeletal muscle divided by body mass index (BMI), and fat mass index (FMI), defined as trunk fat mass divided by BMI, were differently associated with DM according to age and sex.
Results In multivariate logistic regression, the risk for DM significantly increased across quartiles of FMI in men aged ≥70. Meanwhile, MMI showed a protective association with DM in men of the same age. The odds ratios (ORs) for the highest quartile versus the lowest quartile of FMI and MMI were 3.116 (95% confidence interval [CI], 1.405 to 6.914) and 0.295 (95% CI, 0.157 to 0.554), respectively. In women, the ORs of DM was significantly different across FMI quartiles in those over age 50. The highest quartile of FMI exhibited increased ORs of DM in subjects aged 50 to 69 (OR, 1.891; 95% CI, 1.229 to 2.908) and ≥70 (OR, 2.275; 95% CI, 1.103 to 4.69) compared to lowest quartile. However, MMI was not significantly associated with DM in women of all age groups.
Conclusion Both FMI and MMI were independent risk factors for DM in men aged 70 years or more. In women over 50 years, FMI was independently associated with DM. There was no significant association between MMI and DM in women.
-
Citations
Citations to this article as recorded by- Research Progress on Correlation between Body Composition Changes and Disease Pro-gression of Type 2 Diabetes
敏 张
Advances in Clinical Medicine.2024; 14(03): 936. CrossRef - Low Skeletal Muscle Mass Accompanied by Abdominal Obesity Additively Increases the Risk of Incident Type 2 Diabetes
Ji Eun Jun, Seung-Eun Lee, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Jae Hwan Jee, Jae Hyeon Kim
The Journal of Clinical Endocrinology & Metabolism.2023; 108(5): 1173. CrossRef - Is imaging-based muscle quantity associated with risk of diabetes? A meta-analysis of cohort studies
Shanhu Qiu, Xue Cai, Yang Yuan, Bo Xie, Zilin Sun, Tongzhi Wu
Diabetes Research and Clinical Practice.2022; 189: 109939. CrossRef - Whole and segmental body composition changes during mid-follicular and mid-luteal phases of the menstrual cycle in recreationally active young women
Şükran Nazan Koşar, Yasemin Güzel, Mehmet Gören Köse, Ayşe Kin İşler, Tahir Hazır
Annals of Human Biology.2022; 49(2): 124. CrossRef - Body Composition and Diabetes
Hye Jin Yoo
The Journal of Korean Diabetes.2021; 22(4): 238. CrossRef
- Research Progress on Correlation between Body Composition Changes and Disease Pro-gression of Type 2 Diabetes
- Metabolic Risk/Epidemiology
- Plasma Targeted Metabolomics Analysis for Amino Acids and Acylcarnitines in Patients with Prediabetes, Type 2 Diabetes Mellitus, and Diabetic Vascular Complications
- Xin Li, Yancheng Li, Yuanhao Liang, Ruixue Hu, Wenli Xu, Yufeng Liu
- Diabetes Metab J. 2021;45(2):195-208. Published online March 9, 2021
- DOI: https://doi.org/10.4093/dmj.2019.0209

- 6,251 View
- 201 Download
- 12 Web of Science
- 12 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- Background
We hypothesized that specific amino acids or acylcarnitines would have benefits for the differential diagnosis of diabetes. Thus, a targeted metabolomics for amino acids and acylcarnitines in patients with diabetes and its complications was carried out.
Methods
A cohort of 54 normal individuals and 156 patients with type 2 diabetes mellitus and/or diabetic complications enrolled from the First Affiliated Hospital of Jinzhou Medical University was studied. The subjects were divided into five main groups: normal individuals, impaired fasting glucose, overt diabetes, diabetic microvascular complications, and diabetic peripheral vascular disease. The technique of tandem mass spectrometry was applied to obtain the plasma metabolite profiles. Metabolomics multivariate statistics were applied for the metabolic data analysis and the differential metabolites determination.
Results
A total of 10 cross-comparisons within diabetes and its complications were designed to explore the differential metabolites. The results demonstrated that eight comparisons existed and yielded significant metabolic differences. A total number of 24 differential metabolites were determined from six selected comparisons, including up-regulated amino acids, down-regulated medium-chain and long-chain acylcarnitines. Altered differential metabolites provided six panels of biomarkers, which were helpful in distinguishing diabetic patients.
Conclusion
Our results demonstrated that the biomarker panels consisted of specific amino acids and acylcarnitines which could reflect the metabolic variations among the different stages of diabetes and might be useful for the differential diagnosis of prediabetes, overt diabetes and diabetic complications. -
Citations
Citations to this article as recorded by- Liquid Biopsy: A Game Changer for Type 2 Diabetes
Gratiela Gradisteanu Pircalabioru, Madalina Musat, Viviana Elian, Ciprian Iliescu
International Journal of Molecular Sciences.2024; 25(5): 2661. CrossRef - Identification of FGF13 as a Potential Biomarker and Target for Diagnosis of Impaired Glucose Tolerance
Qi Chen, Fangyu Li, Yuanyuan Gao, Fengying Yang, Li Yuan
International Journal of Molecular Sciences.2023; 24(2): 1807. CrossRef - Quantitative, Targeted Analysis of Gut Microbiota Derived Metabolites Provides Novel Biomarkers of Early Diabetic Kidney Disease in Type 2 Diabetes Mellitus Patients
Lavinia Balint, Carmen Socaciu, Andreea Iulia Socaciu, Adrian Vlad, Florica Gadalean, Flaviu Bob, Oana Milas, Octavian Marius Cretu, Anca Suteanu-Simulescu, Mihaela Glavan, Silvia Ienciu, Maria Mogos, Dragos Catalin Jianu, Ligia Petrica
Biomolecules.2023; 13(7): 1086. CrossRef - Unlocking the Potential: Amino Acids’ Role in Predicting and Exploring Therapeutic Avenues for Type 2 Diabetes Mellitus
Yilan Ding, Shuangyuan Wang, Jieli Lu
Metabolites.2023; 13(9): 1017. CrossRef - Untargeted metabolomics reveals dynamic changes in metabolic profiles of rat supraspinatus tendon at three different time points after diabetes induction
Kuishuai Xu, Liang Zhang, Tianrui Wang, Zhongkai Ren, Tengbo Yu, Yingze Zhang, Xia Zhao
Frontiers in Endocrinology.2023;[Epub] CrossRef - Acylcarnitines: Can They Be Biomarkers of Diabetic Nephropathy?
Xiaodie Mu, Min Yang, Peiyao Ling, Aihua Wu, Hua Zhou, Jingting Jiang
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 247. CrossRef - Targeted metabolomics analysis of amino acids and acylcarnitines as risk markers for diabetes by LC–MS/MS technique
Shaghayegh Hosseinkhani, Babak Arjmand, Arezou Dilmaghani-Marand, Sahar Mohammadi Fateh, Hojat Dehghanbanadaki, Niloufar Najjar, Sepideh Alavi-Moghadam, Robabeh Ghodssi-Ghassemabadi, Ensieh Nasli-Esfahani, Farshad Farzadfar, Bagher Larijani, Farideh Razi
Scientific Reports.2022;[Epub] CrossRef - Identification of Insulin Resistance Biomarkers in Metabolic Syndrome Detected by UHPLC-ESI-QTOF-MS
Leen Oyoun Alsoud, Nelson C. Soares, Hamza M. Al-Hroub, Muath Mousa, Violet Kasabri, Nailya Bulatova, Maysa Suyagh, Karem H. Alzoubi, Waseem El-Huneidi, Bashaer Abu-Irmaileh, Yasser Bustanji, Mohammad H. Semreen
Metabolites.2022; 12(6): 508. CrossRef - Serum Untargeted Metabolomics Reveal Potential Biomarkers of Progression of Diabetic Retinopathy in Asians
Zongyi Wang, Jiyang Tang, Enzhong Jin, Yusheng Zhong, Linqi Zhang, Xinyao Han, Jia Liu, Yong Cheng, Jing Hou, Xuan Shi, Huijun Qi, Tong Qian, Li Yuan, Xianru Hou, Hong Yin, Jianhong Liang, Mingwei Zhao, Lvzhen Huang, Jinfeng Qu
Frontiers in Molecular Biosciences.2022;[Epub] CrossRef - Circulating amino acids and acylcarnitines correlated with different CAC score ranges in diabetic postmenopausal women using LC–MS/MS based metabolomics approach
Shaghayegh Hosseinkhani, Pooneh Salari, Fatemeh Bandarian, Mojgan Asadi, Shapour Shirani, Niloufar Najjar, Hojat Dehghanbanadaki, Parvin Pasalar, Farideh Razi
BMC Endocrine Disorders.2022;[Epub] CrossRef - Metabolomic comparison followed by cross-validation of enzyme-linked immunosorbent assay to reveal potential biomarkers of diabetic retinopathy in Chinese with type 2 diabetes
Zongyi Wang, Jiyang Tang, Enzhong Jin, Chi Ren, Siying Li, Linqi Zhang, Yusheng Zhong, Yu Cao, Jianmin Wang, Wei Zhou, Mingwei Zhao, Lvzhen Huang, Jinfeng Qu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Urine Metabolites Enable Fast Detection of COVID-19 Using Mass Spectrometry
Alexandre Varao Moura, Danilo Cardoso de Oliveira, Alex Ap. R. Silva, Jonas Ribeiro da Rosa, Pedro Henrique Dias Garcia, Pedro Henrique Godoy Sanches, Kyana Y. Garza, Flavio Marcio Macedo Mendes, Mayara Lambert, Junier Marrero Gutierrez, Nicole Marino Gra
Metabolites.2022; 12(11): 1056. CrossRef
- Liquid Biopsy: A Game Changer for Type 2 Diabetes
- Metabolic Risk/Epidemiology
-
- Effect of Sarcopenia and Body Shape on Cardiovascular Disease According to Obesity Phenotypes
- Hyun-Woong Cho, Wankyo Chung, Shinje Moon, Ohk-Hyun Ryu, Min Kyung Kim, Jun Goo Kang
- Diabetes Metab J. 2021;45(2):209-218. Published online July 10, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0223
- 8,312 View
- 212 Download
- 21 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background This study aimed to assess the effects of sarcopenia and A Body Shape Index (ABSI) on cardiovascular disease (CVD) risk according to obesity phenotypes.
Methods We used data from the National Health and Nutrition Examination Survey 1999 to 2012. A total of 25,270 adults were included and classified into the following groups: metabolically healthy normal weight (MHNW), metabolically healthy overweight/obese (MHO), metabolically unhealthy normal weight (MUNW), and metabolically unhealthy overweight/obese (MUO). Sarcopenia was defined as the appendicular skeletal mass index <7 kg/m2 in men and <5.5kg/m2 in women. A multivariate logistic regression analysis was performed to evaluate the odds ratio (OR) of sarcopenia and ABSI for CVD events according to the obesity phenotype.
Results The MHNW participants with sarcopenia had higher risk for CVD than those without sarcopenia (OR, 2.69; 95% confidence interval [CI], 1.56 to 4.64). In the analysis with MHNW participants without sarcopenia as a reference, the participants with sarcopenia showed a higher OR for CVD than those without sarcopenia in both MHO (OR in participants without sarcopenia, 3.31; 95% CI, 1.94 to 5.64) (OR in participants with sarcopenia, 8.59; 95% CI, 2.63 to 28.04) and MUO participants (OR in participants without sarcopenia, 5.11; 95% CI, 3.21 to 8.15) (OR in participants with sarcopenia, 8.12; 95% CI, 4.04 to 16.32). Participants within the second and third tertiles of ABSI had higher ORs for CVDs than the counterpart of obesity phenotypes within the first tertile.
Conclusion These results suggest that clinical approaches that consider muscle and body shape are required.
-
Citations
Citations to this article as recorded by- Association of low muscle mass and obesity with increased all‐cause and cardiovascular disease mortality in US adults
Donghyun Kim, Junghoon Lee, Raekil Park, Chang‐Myung Oh, Shinje Moon
Journal of Cachexia, Sarcopenia and Muscle.2024; 15(1): 240. CrossRef - Metabolic-associated fatty liver disease and sarcopenia: A double whammy
Aditya Viswanath, Sherouk Fouda, Cornelius James Fernandez, Joseph M Pappachan
World Journal of Hepatology.2024; 16(2): 152. CrossRef - Association of Myosteatosis with Nonalcoholic Fatty Liver Disease, Severity, and Liver Fibrosis Using Visual Muscular Quality Map in Computed Tomography
Hwi Seung Kim, Jiwoo Lee, Eun Hee Kim, Min Jung Lee, In Young Bae, Woo Je Lee, Joong-Yeol Park, Hong-Kyu Kim, Chang Hee Jung
Diabetes & Metabolism Journal.2023; 47(1): 104. CrossRef - Additive impact of diabetes and sarcopenia on all-cause and cardiovascular mortality: A longitudinal nationwide population-based study
Eyun Song, Soon Young Hwang, Min Jeong Park, Ahreum Jang, Kyeong Jin Kim, Ji Hee Yu, Nam Hoon Kim, Hye Jin Yoo, Ji A. Seo, Sin Gon Kim, Nan Hee Kim, Sei Hyun Baik, Kyung Mook Choi
Metabolism.2023; 148: 155678. CrossRef - Association between a body shape index and abdominal aortic calcification in general population: A cross-sectional study
Wei Li, Zhenwei Wang, Min Li, Jing Xie, Jing Gong, Naifeng Liu
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Metabolic Impact of Frailty Changes Diabetes Trajectory
Alan J. Sinclair, Ahmed H. Abdelhafiz
Metabolites.2023; 13(2): 295. CrossRef - Association between sarcopenic obesity and poor muscle quality based on muscle quality map and abdominal computed tomography
Yun Kyung Cho, Han Na Jung, Eun Hee Kim, Min Jung Lee, Joong‐Yeol Park, Woo Je Lee, Hong‐Kyu Kim, Chang Hee Jung
Obesity.2023; 31(6): 1547. CrossRef - Metabolic Characteristics of Frail Older People with Diabetes Mellitus—A Systematic Search for Phenotypes
Ahmed H. Abdelhafiz, Grace L. Keegan, Alan J. Sinclair
Metabolites.2023; 13(6): 705. CrossRef - Risk of Cardiovascular Diseases Among Different Metabolic Obesity Phenotypes: A Prospective Observational Study
Xiaowei Liu, Chan Yang, Yuanyuan Dang, Zhenqi Chang, Juan Li, Yi Zhao, Yuhong Zhang
Metabolic Syndrome and Related Disorders.2023; 21(6): 306. CrossRef - Effect of Hypoxia Conditioning on Body Composition in Middle-Aged and Older Adults: A Systematic Review and Meta-Analysis
Zhijian He, Lijun Qiang, Yusheng Liu, Wenfeng Gao, Tao Feng, Yang Li, Bing Yan, Olivier Girard
Sports Medicine - Open.2023;[Epub] CrossRef - Association Between a Body Shape Index and Subclinical Carotid Atherosclerosis in Population Free of Cardiovascular and Cerebrovascular Diseases
Xiaotian Ma, Lihong Chen, Wenchao Hu, Lanjie He
Journal of Atherosclerosis and Thrombosis.2022; 29(8): 1140. CrossRef - Impact of Sarcopenia on the Severity of the Liver Damage in Patients With Non-alcoholic Fatty Liver Disease
Vittoria Zambon Azevedo, Cristina Alina Silaghi, Thomas Maurel, Horatiu Silaghi, Vlad Ratziu, Raluca Pais
Frontiers in Nutrition.2022;[Epub] CrossRef - Identification of sarcopenic obesity in adults undergoing orthopaedic surgery: Relationship between “a body shape index” (ABSI) and fat-free mass. A cross -sectional study
Ana Tomažič, Boštjan Žvanut, Lilijana Vouk Grbac, Mihaela Jurdana, Fatih Özden
PLOS ONE.2022; 17(6): e0269956. CrossRef - Associations of Dynapenic Obesity and Sarcopenic Obesity with the Risk of Complications in COVID-19
Laura Pérez-Campos Mayoral, Carlos Alberto Matias-Cervantes, Eduardo Pérez-Campos, Carlos Romero Díaz, Luis Ángel Laguna Barrios, María del Socorro Pina Canseco, Margarito Martínez Cruz, Eduardo Pérez-Campos Mayoral, Carlos Josué Solórzano Mata, Francisco
International Journal of Molecular Sciences.2022; 23(15): 8277. CrossRef - Sex Differences in Adiposity and Cardiovascular Diseases
Haoyun Li, Daniels Konja, Luyao Wang, Yu Wang
International Journal of Molecular Sciences.2022; 23(16): 9338. CrossRef - The Applicability of the ESPEN and EASO-Defined Diagnostic Criteria for Sarcopenic Obesity in Japanese Patients after Stroke: Prevalence and Association with Outcomes
Yoshihiro Yoshimura, Hidetaka Wakabayashi, Fumihiko Nagano, Ayaka Matsumoto, Sayuri Shimazu, Ai Shiraishi, Yoshifumi Kido, Takahiro Bise
Nutrients.2022; 14(19): 4205. CrossRef - The value of combining the simple anthropometric obesity parameters, Body Mass Index (BMI) and a Body Shape Index (ABSI), to assess the risk of non-alcoholic fatty liver disease
Maobin Kuang, Guotai Sheng, Chong Hu, Song Lu, Nan Peng, Yang Zou
Lipids in Health and Disease.2022;[Epub] CrossRef - Sarcopenia and cardiovascular disease in patients with and without kidney disease: what do we know?
Ozkan Gungor, Mustafa Sevinc, Sena Ulu, Ismail Kocyigit
International Urology and Nephrology.2022; 55(5): 1161. CrossRef - Skeletal Muscle Should Not Be Overlooked
Ji A Seo
Diabetes & Metabolism Journal.2021; 45(2): 173. CrossRef - The Role of Sarcopenic Obesity in Cancer and Cardiovascular Disease: A Synthesis of the Evidence on Pathophysiological Aspects and Clinical Implications
Erika Aparecida Silveira, Rômulo Roosevelt da Silva Filho, Maria Claudia Bernardes Spexoto, Fahimeh Haghighatdoost, Nizal Sarrafzadegan, Cesar de Oliveira
International Journal of Molecular Sciences.2021; 22(9): 4339. CrossRef
- Association of low muscle mass and obesity with increased all‐cause and cardiovascular disease mortality in US adults
- Cardiovascular Risk/Epidemiology
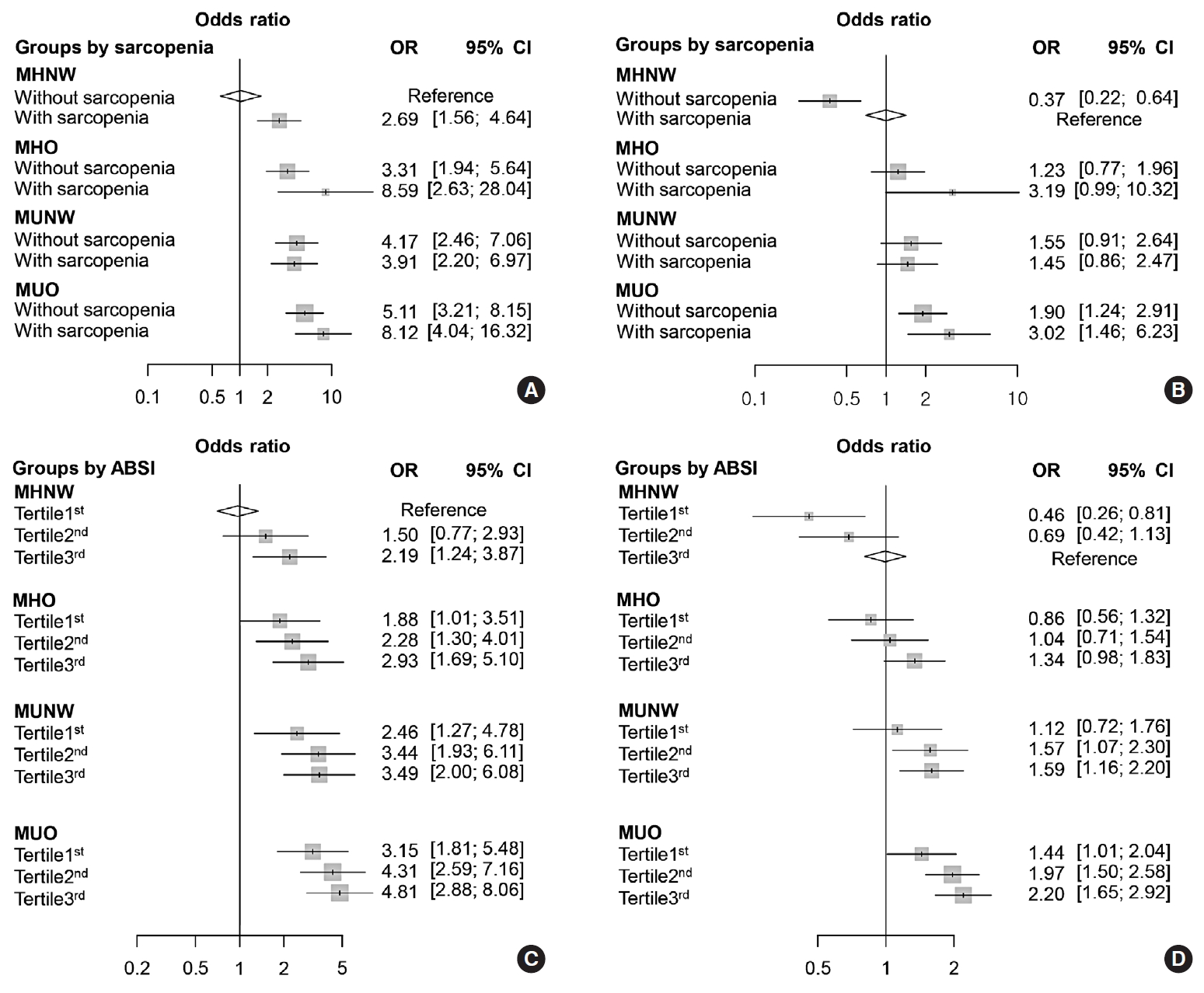
- Clinical Significance of Body Fat Distribution in Coronary Artery Calcification Progression in Korean Population
- Heesun Lee, Hyo Eun Park, Ji Won Yoon, Su-Yeon Choi
- Diabetes Metab J. 2021;45(2):219-230. Published online October 28, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0161
- Correction in: Diabetes Metab J 2021;45(6):974
- 6,502 View
- 257 Download
- 8 Web of Science
- 7 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 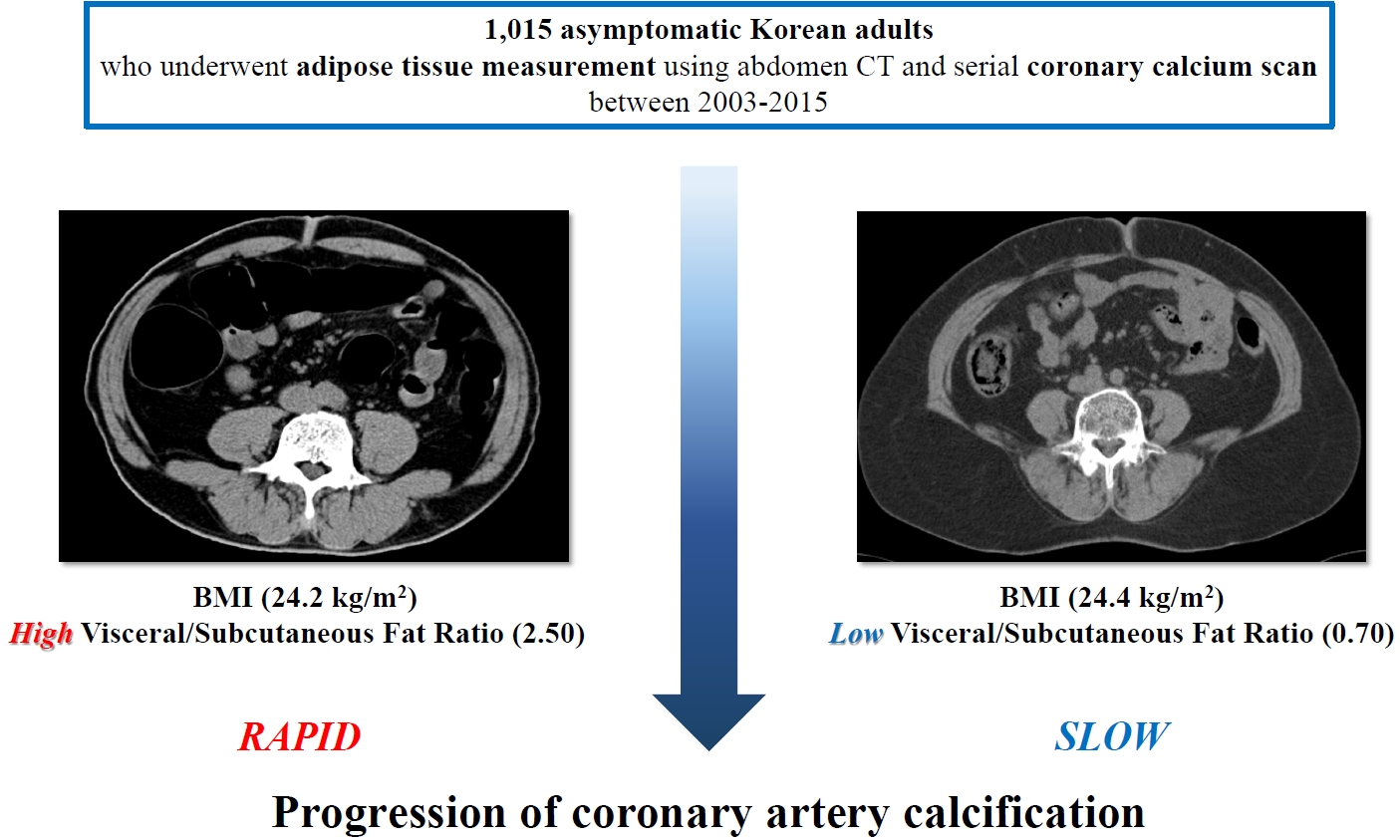
- Background
Although obesity differs according to ethnicity, it is globally established as a solid risk factor for cardiovascular disease. However, it is not fully understood how obesity parameters affect the progression of coronary artery calcification (CAC) in Korean population. We sought to evaluate the association of obesity-related parameters including visceral adipose tissue (VAT) measurement and CAC progression.
Methods
This retrospective observational cohort study investigated 1,015 asymptomatic Korean subjects who underwent serial CAC scoring by computed tomography (CT) with at least 1-year interval and adipose tissue measurement using non-contrast CT at baseline for a routine checkup between 2003 and 2015. CAC progression, the main outcome, was defined as a difference of ≥2.5 between the square roots of the baseline and follow-up CAC scores using Agatston units.
Results
During follow-up (median 39 months), 37.5% of subjects showed CAC progression of a total population (56.4 years, 80.6% male). Body mass index (BMI) ≥25 kg/m2, increasing waist circumferences (WC), and higher VAT/subcutaneous adipose tissue (SAT) area ratio were independently associated with CAC progression. Particularly, predominance of VAT over SAT at ≥30% showed the strongest prediction for CAC progression (adjusted hazard ratio, 2.20; P<0.001) and remained of prognostic value regardless of BMI or WC status. Further, it provided improved risk stratification of CAC progression beyond known prognosticators.
Conclusion
Predominant VAT area on CT is the strongest predictor of CAC progression regardless of BMI or WC in apparently healthy Korean population. Assessment of body fat distribution may be helpful to identify subjects at higher risk. -
Citations
Citations to this article as recorded by- Gender-specific abdominal fat distribution and insulin resistance associated with organophosphate esters and phthalate metabolites exposure
Xiaoliu Shi, Wanyue Wang, Jiafan Feng, Xiaochun Ma, Mengting Xu, Cui Wang
Environmental Pollution.2024; 349: 123959. CrossRef - The association between C-reactive protein and coronary artery calcification: a systematic review and meta-analysis
Amirhossein Tajani, Masoumeh Sadeghi, Navid Omidkhoda, Amir Hooshang Mohammadpour, Sara Samadi, Vahid Jomehzadeh
BMC Cardiovascular Disorders.2024;[Epub] CrossRef - Visceral adipose tissue is an independent predictor and mediator of the progression of coronary calcification: a prospective sub-analysis of the GEA study
Neftali Eduardo Antonio-Villa, Juan Gabriel Juárez-Rojas, Rosalinda Posadas-Sánchez, Juan Reyes-Barrera, Aida Medina-Urrutia
Cardiovascular Diabetology.2023;[Epub] CrossRef - Deep learning-based prediction for significant coronary artery stenosis on coronary computed tomography angiography in asymptomatic populations
Heesun Lee, Bong Gyun Kang, Jeonghee Jo, Hyo Eun Park, Sungroh Yoon, Su-Yeon Choi, Min Joo Kim
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Relationship between a novel non–insulin-based metabolic score for insulin resistance (METS‐IR) and coronary artery calcification
Zhenwei Wang, Xiaofang Hui, Xu Huang, Jingjie Li, Naifeng Liu
BMC Endocrine Disorders.2022;[Epub] CrossRef - Association Between Abdominal Adipose Tissue Distribution and Risk of Endometrial Cancer: A Case-Control Study
Yuan Cheng, Zhongyu Wang, Xiaoxuan Jia, Rong Zhou, Jianliu Wang
Clinical Medicine Insights: Oncology.2022; 16: 117955492211407. CrossRef - Sex differences in cardiovascular risk may be related to sex differences in diet patterns: a narrative review
A. M. Tindall, V. A. Stallings
Annals of Human Biology.2021; 48(6): 517. CrossRef
- Gender-specific abdominal fat distribution and insulin resistance associated with organophosphate esters and phthalate metabolites exposure
- Genetics
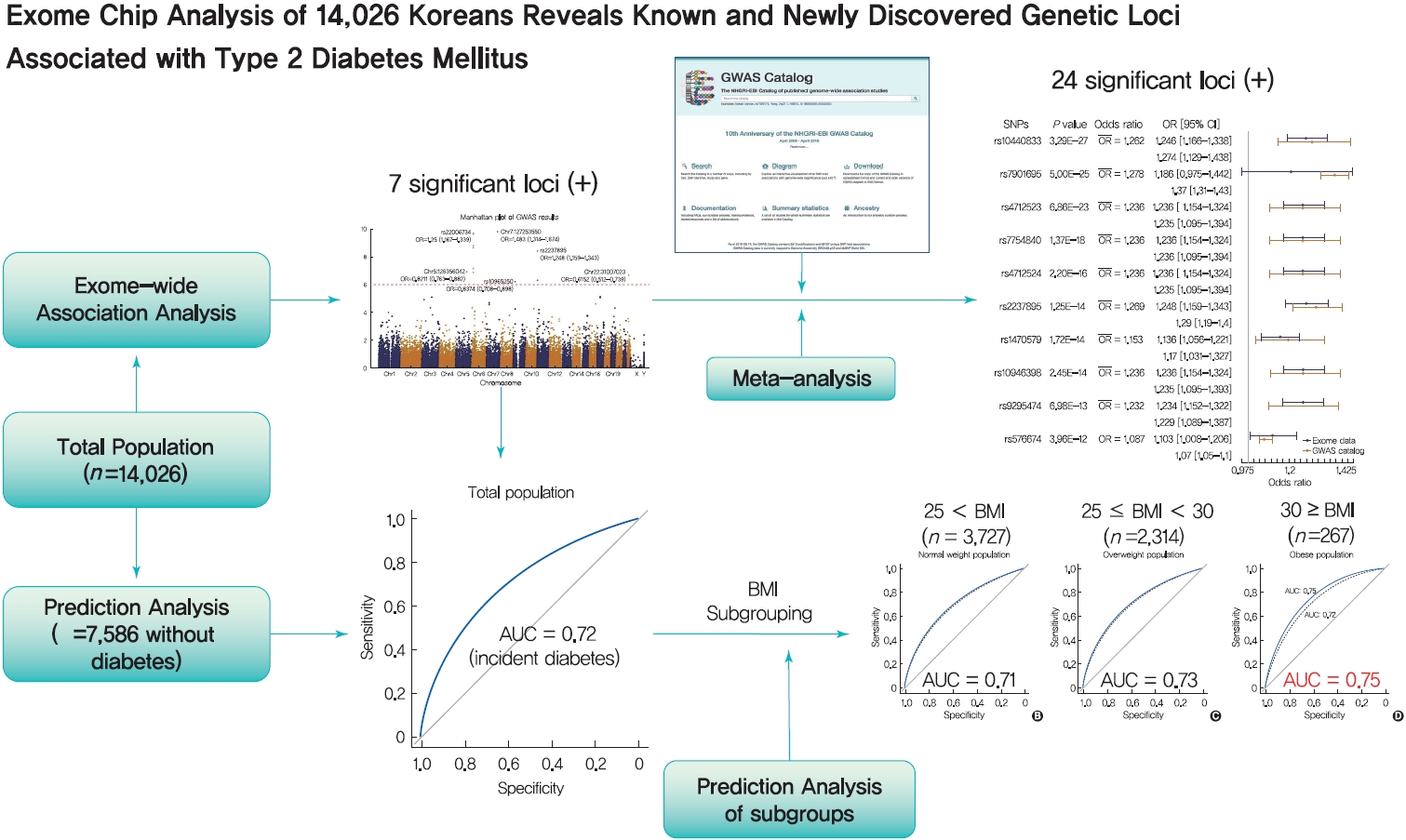
- Exome Chip Analysis of 14,026 Koreans Reveals Known and Newly Discovered Genetic Loci Associated with Type 2 Diabetes Mellitus
- Seong Beom Cho, Jin Hwa Jang, Myung Guen Chung, Sang Cheol Kim
- Diabetes Metab J. 2021;45(2):231-240. Published online July 28, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0163
- 6,215 View
- 195 Download
- 6 Web of Science
- 6 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 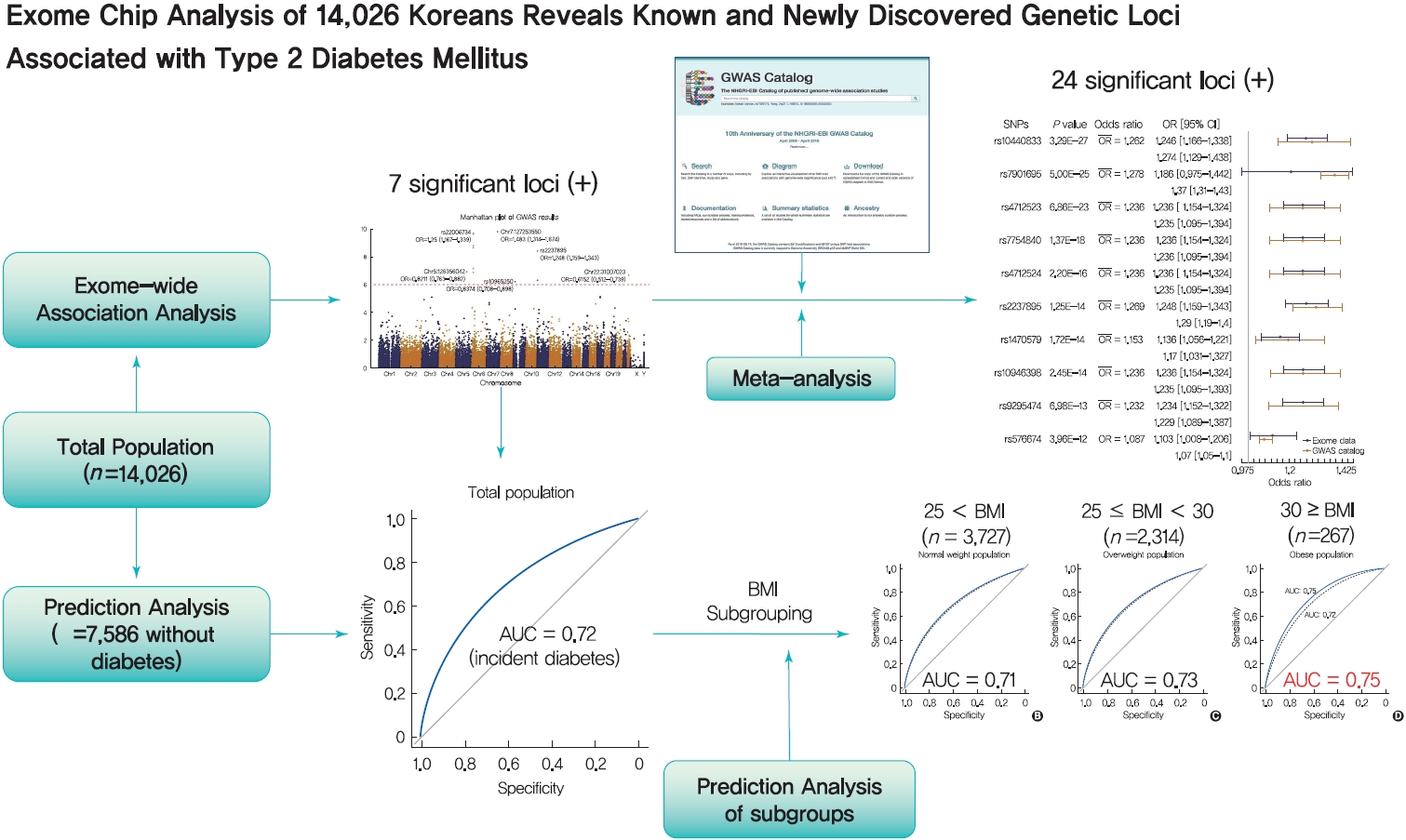
Background Most loci associated with type 2 diabetes mellitus (T2DM) discovered to date are within noncoding regions of unknown functional significance. By contrast, exonic regions have advantages for biological interpretation.
Methods We analyzed the association of exome array data from 14,026 Koreans to identify susceptible exonic loci for T2DM. We used genotype information of 50,543 variants using the Illumina exome array platform.
Results In total, 7 loci were significant with a Bonferroni adjusted
P =1.03×10−6. rs2233580 in paired box gene 4 (PAX4 ) showed the highest odds ratio of 1.48 (P =1.60×10−10). rs11960799 in membrane associated ring-CH-type finger 3 (MARCH3 ) and rs75680863 in transcobalamin 2 (TCN2 ) were newly identified loci. When we built a model to predict the incidence of diabetes with the 7 loci and clinical variables, area under the curve (AUC) of the model improved significantly (AUC=0.72,P <0.05), but marginally in its magnitude, compared with the model using clinical variables (AUC=0.71,P <0.05). When we divided the entire population into three groups—normal body mass index (BMI; <25 kg/m2), overweight (25≤ BMI <30 kg/m2), and obese (BMI ≥30 kg/m2) individuals—the predictive performance of the 7 loci was greatest in the group of obese individuals, where the net reclassification improvement was highly significant (0.51;P =8.00×10−5).Conclusion We found exonic loci having a susceptibility for T2DM. We found that such genetic information is advantageous for predicting T2DM in a subgroup of obese individuals.
-
Citations
Citations to this article as recorded by- Polygenic Risk Score, Lifestyles, and Type 2 Diabetes Risk: A Prospective Chinese Cohort Study
Jia Liu, Lu Wang, Xuan Cui, Qian Shen, Dun Wu, Man Yang, Yunqiu Dong, Yongchao Liu, Hai Chen, Zhijie Yang, Yaqi Liu, Meng Zhu, Hongxia Ma, Guangfu Jin, Yun Qian
Nutrients.2023; 15(9): 2144. CrossRef - Celebrities in the heart, strangers in the pancreatic beta cell: Voltage‐gated potassium channels Kv7.1 and Kv11.1 bridge long QT syndrome with hyperinsulinaemia as well as type 2 diabetes
Anniek F. Lubberding, Christian R. Juhl, Emil Z. Skovhøj, Jørgen K. Kanters, Thomas Mandrup‐Poulsen, Signe S. Torekov
Acta Physiologica.2022;[Epub] CrossRef - Substitution of Carbohydrates for Fats and Risk of Type 2 Diabetes among Korean Middle-Aged Adults: Findings from the Korean Genome and Epidemiology Study
Hye-Ah Lee, Hyesook Park
Nutrients.2022; 14(3): 654. CrossRef - Ethnic-Specific Type 2 Diabetes Risk Factor PAX4 R192H Is Associated with Attention-Specific Cognitive Impairment in Chinese with Type 2 Diabetes
Su Fen Ang, Serena Low, Tze Pin Ng, Clara S.H. Tan, Keven Ang, Ziliang Lim, Wern Ee Tang, Tavintharan Subramaniam, Chee Fang Sum, Su Chi Lim, Nagaendran Kandiah
Journal of Alzheimer's Disease.2022; 88(1): 241. CrossRef - TrustGWAS: A full-process workflow for encrypted GWAS using multi-key homomorphic encryption and pseudorandom number perturbation
Meng Yang, Chuwen Zhang, Xiaoji Wang, Xingmin Liu, Shisen Li, Jianye Huang, Zhimin Feng, Xiaohui Sun, Fang Chen, Shuang Yang, Ming Ni, Lin Li, Yanan Cao, Feng Mu
Cell Systems.2022; 13(9): 752. CrossRef - Sex Differences in the Effects of CDKAL1 Variants on Glycemic Control in Diabetic Patients: Findings from the Korean Genome and Epidemiology Study
Hye Ah Lee, Hyesook Park, Young Sun Hong
Diabetes & Metabolism Journal.2022; 46(6): 879. CrossRef
- Polygenic Risk Score, Lifestyles, and Type 2 Diabetes Risk: A Prospective Chinese Cohort Study
- Genetics
- Enhancer-Gene Interaction Analyses Identified the Epidermal Growth Factor Receptor as a Susceptibility Gene for Type 2 Diabetes Mellitus
- Yang Yang, Shi Yao, Jing-Miao Ding, Wei Chen, Yan Guo
- Diabetes Metab J. 2021;45(2):241-250. Published online June 10, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0204

- 6,010 View
- 104 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background Genetic interactions are known to play an important role in the missing heritability problem for type 2 diabetes mellitus (T2DM). Interactions between enhancers and their target genes play important roles in gene regulation and disease pathogenesis. In the present study, we aimed to identify genetic interactions between enhancers and their target genes associated with T2DM.
Methods We performed genetic interaction analyses of enhancers and protein-coding genes for T2DM in 2,696 T2DM patients and 3,548 controls of European ancestry. A linear regression model was used to identify single nucleotide polymorphism (SNP) pairs that could affect the expression of the protein-coding genes. Differential expression analyses were used to identify differentially expressed susceptibility genes in diabetic and nondiabetic subjects.
Results We identified one SNP pair, rs4947941×rs7785013, significantly associated with T2DM (combined
P =4.84×10−10). The SNP rs4947941 was annotated as an enhancer, and rs7785013 was located in the epidermal growth factor receptor (EGFR ) gene. This SNP pair was significantly associated withEGFR expression in the pancreas (P =0.033), and the minor allele “A” of rs7785013 decreasedEGFR gene expression and the risk of T2DM with an increase in the dosage of “T” of rs4947941.EGFR expression was significantly upregulated in T2DM patients, which was consistent with the effect of rs4947941×rs7785013 on T2DM andEGFR expression. A functional validation study using the Mouse Genome Informatics (MGI) database showed thatEGFR was associated with diabetes-relevant phenotypes.Conclusion Genetic interaction analyses of enhancers and protein-coding genes suggested that
EGFR may be a novel susceptibility gene for T2DM.-
Citations
Citations to this article as recorded by- Genome-Wide Epistasis Study of Cerebrospinal Fluid Hyperphosphorylated Tau in ADNI Cohort
Dandan Chen, Jin Li, Hongwei Liu, Xiaolong Liu, Chenghao Zhang, Haoran Luo, Yiming Wei, Yang Xi, Hong Liang, Qiushi Zhang
Genes.2023; 14(7): 1322. CrossRef - Investigation of the mechanism of Shen Qi Wan prescription in the treatment of T2DM via network pharmacology and molecular docking
Piaopiao Zhao, Xiaoxiao Zhang, Yuning Gong, Weihua Li, Zengrui Wu, Yun Tang, Guixia Liu
In Silico Pharmacology.2022;[Epub] CrossRef - The Role of the Epidermal Growth Factor Receptor in Diabetic Kidney Disease
Raymond C. Harris
Cells.2022; 11(21): 3416. CrossRef - Co-expression Network Revealed Roles of RNA m6A Methylation in Human β-Cell of Type 2 Diabetes Mellitus
Cong Chen, Qing Xiang, Weilin Liu, Shengxiang Liang, Minguang Yang, Jing Tao
Frontiers in Cell and Developmental Biology.2021;[Epub] CrossRef
- Genome-Wide Epistasis Study of Cerebrospinal Fluid Hyperphosphorylated Tau in ADNI Cohort
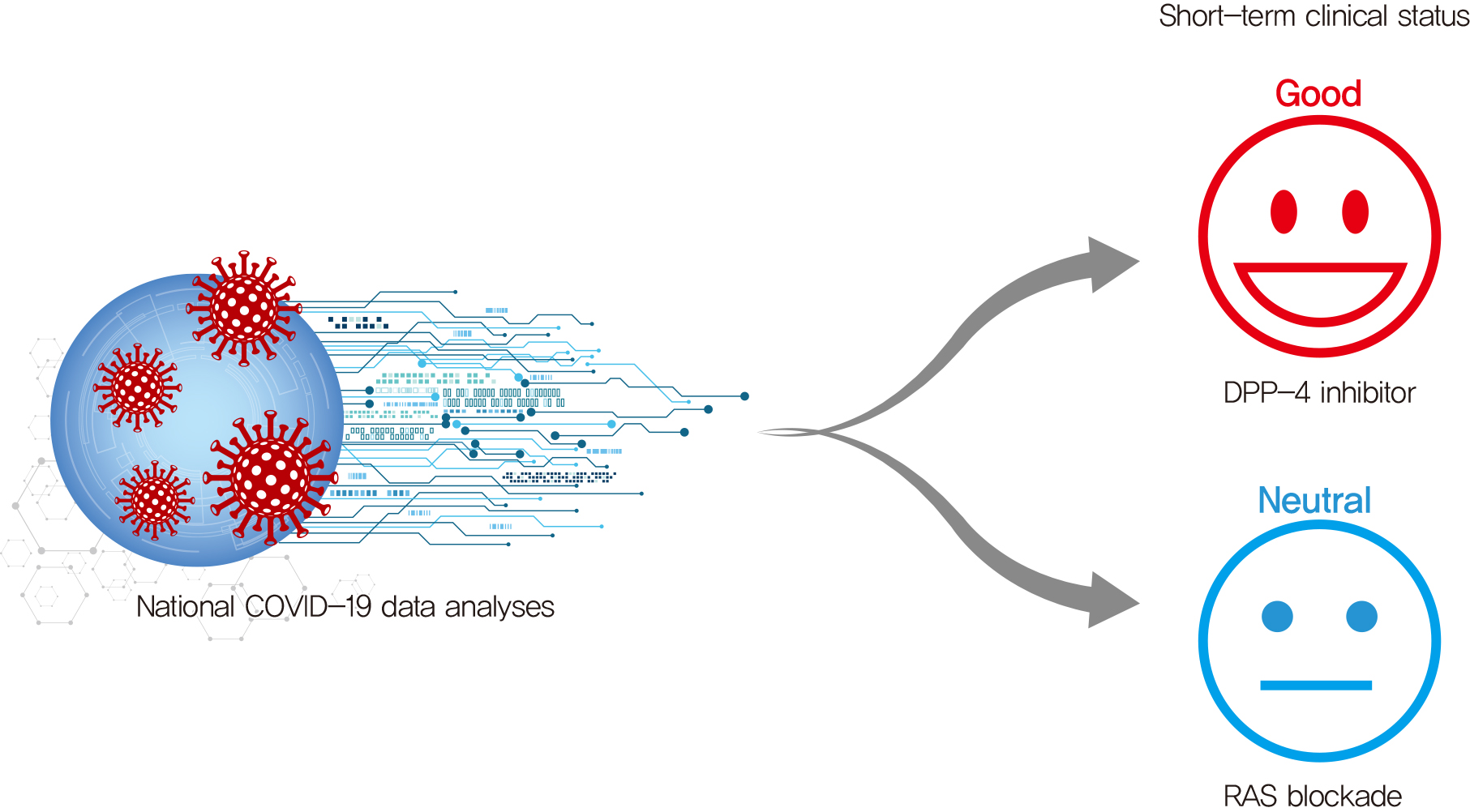
- COVID-19
- Effects of a DPP-4 Inhibitor and RAS Blockade on Clinical Outcomes of Patients with Diabetes and COVID-19
- Sang Youl Rhee, Jeongwoo Lee, Hyewon Nam, Dae-Sung Kyoung, Dong Wook Shin, Dae Jung Kim
- Diabetes Metab J. 2021;45(2):251-259. Published online March 5, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0206
- 7,848 View
- 406 Download
- 33 Web of Science
- 34 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 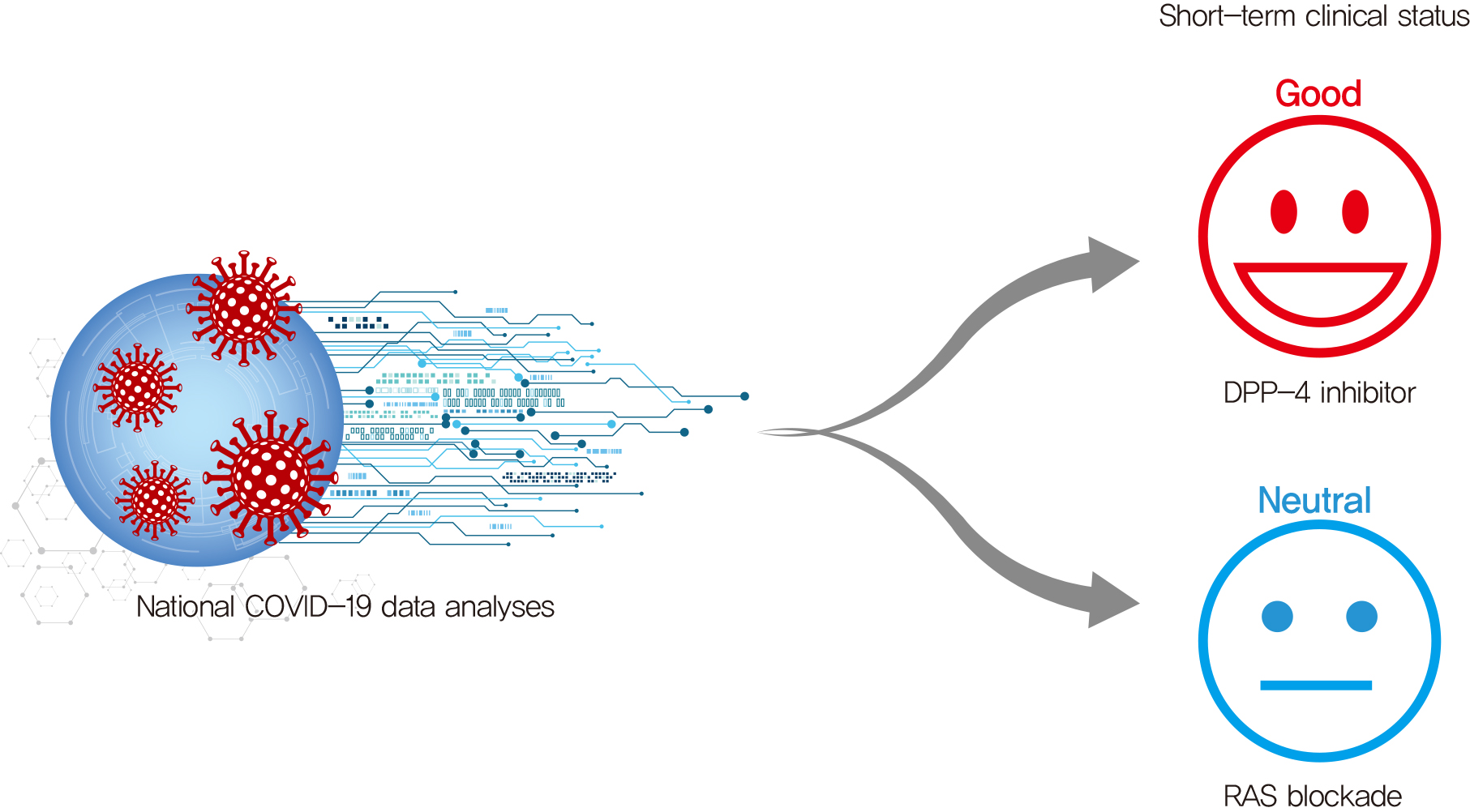
- Background
Dipeptidyl peptidase-4 inhibitor (DPP-4i) and renin-angiotensin system (RAS) blockade are reported to affect the clinical course of coronavirus disease 2019 (COVID-19) in patients with diabetes mellitus (DM).
Methods
As of May 2020, analysis was conducted on all subjects who could confirm their history of claims related to COVID-19 in the National Health Insurance Review and Assessment Service (HIRA) database in Korea. Using this dataset, we compared the short-term prognosis of COVID-19 infection according to the use of DPP-4i and RAS blockade. Additionally, we validated the results using the National Health Insurance Service (NHIS) of Korea dataset.
Results
Totally, data of 67,850 subjects were accessible in the HIRA dataset. Of these, 5,080 were confirmed COVID-19. Among these, 832 subjects with DM were selected for analysis in this study. Among the subjects, 263 (31.6%) and 327 (39.3%) were DPP4i and RAS blockade users, respectively. Thirty-four subjects (4.09%) received intensive care or died. The adjusted odds ratio for severe treatment among DPP-4i users was 0.362 (95% confidence interval [CI], 0.135 to 0.971), and that for RAS blockade users was 0.599 (95% CI, 0.251 to 1.431). These findings were consistent with the analysis based on the NHIS data using 704 final subjects. The adjusted odds ratio for severe treatment among DPP-4i users was 0.303 (95% CI, 0.135 to 0.682), and that for RAS blockade users was 0.811 (95% CI, 0.391 to 1.682).
Conclusion
This study suggests that DPP-4i is significantly associated with a better clinical outcome of patients with COVID-19. -
Citations
Citations to this article as recorded by- The Impact of GLP-1 RAs and DPP-4is on Hospitalisation and Mortality in the COVID-19 Era: A Two-Year Observational Study
Salvatore Greco, Vincenzo M. Monda, Giorgia Valpiani, Nicola Napoli, Carlo Crespini, Fabio Pieraccini, Anna Marra, Angelina Passaro
Biomedicines.2023; 11(8): 2292. CrossRef - Efficacy and Safety of Sitagliptin in the Treatment of COVID-19
Ehab Mudher Mikhael, Siew Chin Ong, Siti Maisharah Sheikh Ghadzi
Journal of Pharmacy Practice.2023; 36(4): 980. CrossRef - DPP-4 Inhibitors as a savior for COVID-19 patients with diabetes
Snehasish Nag, Samanwita Mandal, Oindrila Mukherjee, Suprabhat Mukherjee, Rakesh Kundu
Future Virology.2023; 18(5): 321. CrossRef - Risk phenotypes of diabetes and association with COVID-19 severity and death: an update of a living systematic review and meta-analysis
Sabrina Schlesinger, Alexander Lang, Nikoletta Christodoulou, Philipp Linnerz, Kalliopi Pafili, Oliver Kuss, Christian Herder, Manuela Neuenschwander, Janett Barbaresko, Michael Roden
Diabetologia.2023; 66(8): 1395. CrossRef - ACE2, ACE, DPPIV, PREP and CAT L enzymatic activities in COVID-19: imbalance of ACE2/ACE ratio and potential RAAS dysregulation in severe cases
Raquel Leão Neves, Jéssica Branquinho, Júlia Galanakis Arata, Clarissa Azevedo Bittencourt, Caio Perez Gomes, Michelle Riguetti, Gustavo Ferreira da Mata, Danilo Euclides Fernandes, Marcelo Yudi Icimoto, Gianna Mastroianni Kirsztajn, João Bosco Pesquero
Inflammation Research.2023; 72(8): 1719. CrossRef - Association Between Anti-diabetic Agents and Clinical Outcomes of COVID-19 in Patients with Diabetes: A Systematic Review and Meta-Analysis
Tiantian Han, Shaodi Ma, Chenyu Sun, Huimei Zhang, Guangbo Qu, Yue Chen, Ce Cheng, Eric L. Chen, Mubashir Ayaz Ahmed, Keun Young Kim, Raveena Manem, Mengshi Chen, Zhichun Guo, Hongru Yang, Yue Yan, Qin Zhou
Archives of Medical Research.2022; 53(2): 186. CrossRef - Use of DPP4i reduced odds of clinical deterioration and hyperinflammatory syndrome in COVID-19 patients with type 2 diabetes: Propensity score analysis of a territory-wide cohort in Hong Kong
Carlos K.H. Wong, David T.W. Lui, Angel Y.C. Lui, Ashley C.Y. Kwok, Marshall C.H. Low, Kristy T.K. Lau, Ivan C.H. Au, Xi Xiong, Matthew S.H. Chung, Eric H.Y. Lau, Benjamin J. Cowling
Diabetes & Metabolism.2022; 48(1): 101307. CrossRef - Dipeptidyl peptidase-4 (DPP-IV) inhibitor was associated with mortality reduction in COVID-19 — A systematic review and meta-analysis
Ahmad Fariz Malvi Zamzam Zein, Wilson Matthew Raffaello
Primary Care Diabetes.2022; 16(1): 162. CrossRef - Mortality and Severity in COVID-19 Patients on ACEIs and ARBs—A Systematic Review, Meta-Analysis, and Meta-Regression Analysis
Romil Singh, Sawai Singh Rathore, Hira Khan, Abhishek Bhurwal, Mack Sheraton, Prithwish Ghosh, Sohini Anand, Janaki Makadia, Fnu Ayesha, Kiran S. Mahapure, Ishita Mehra, Aysun Tekin, Rahul Kashyap, Vikas Bansal
Frontiers in Medicine.2022;[Epub] CrossRef - Short- and long-term prognosis of glycemic control in COVID-19 patients with type 2 diabetes
K Zhan, X Zhang, B Wang, Z Jiang, X Fang, S Yang, H Jia, L Li, G Cao, K Zhang, X Ma
QJM: An International Journal of Medicine.2022; 115(3): 131. CrossRef - Decreased circulating dipeptidyl peptidase-4 enzyme activity is prognostic for severe outcomes in COVID-19 inpatients
Ákos Nádasdi, György Sinkovits, Ilona Bobek, Botond Lakatos, Zsolt Förhécz, Zita Z Prohászka, Marienn Réti, Miklós Arató, Gellért Cseh, Tamás Masszi, Béla Merkely, Péter Ferdinandy, István Vályi-Nagy, Zoltán Prohászka, Gábor Firneisz
Biomarkers in Medicine.2022; 16(5): 317. CrossRef - Management von Diabetespatienten in der COVID-19-Pandemie
Charlotte Steenblock, Carlotta Hoffmann, Tilman D. Rachner, Florian Guggenbichler, Ermal Tahirukaj, Sacipi Bejtullah, Vsevolod A. Zinserling, Zsuzanna Varga, Stefan R. Bornstein, Nikolaos Perakakis
Diabetes aktuell.2022; 20(01): 43. CrossRef - Letter: Diabesity Associates with Poor COVID-19 Outcomes among Hospitalized Patients (J Obes Metab Syndr 2021;30:149-54)
Tae Jung Oh
Journal of Obesity & Metabolic Syndrome.2022; 31(1): 86. CrossRef - Glucose-Lowering Agents and COVID-19
Ah Reum Khang
The Journal of Korean Diabetes.2022; 23(1): 1. CrossRef - The Association Between Antidiabetic Agents and Clinical Outcomes of COVID-19 Patients With Diabetes: A Bayesian Network Meta-Analysis
Yidan Chen, Xingfei Lv, Sang Lin, Mohammad Arshad, Mengjun Dai
Frontiers in Endocrinology.2022;[Epub] CrossRef - Drug-Disease Severity and Target-Disease Severity Interaction Networks in COVID-19 Patients
Verena Schöning, Felix Hammann
Pharmaceutics.2022; 14(9): 1828. CrossRef - Role of Dipeptidyl Peptidase-4 (DPP4) on COVID-19 Physiopathology
Alba Sebastián-Martín, Belén G. Sánchez, José M. Mora-Rodríguez, Alicia Bort, Inés Díaz-Laviada
Biomedicines.2022; 10(8): 2026. CrossRef - Anti-Diabetic Drugs GLP-1 Agonists and DPP-4 Inhibitors may Represent
Potential Therapeutic Approaches for COVID-19
Aliah Alshanwani, Tarek Kashour, Amira Badr
Endocrine, Metabolic & Immune Disorders - Drug Targets.2022; 22(6): 571. CrossRef - Dipeptidyl peptidase 4 inhibitors in COVID-19: Beyond glycemic control
Niya Narayanan, Dukhabandhu Naik, Jayaprakash Sahoo, Sadishkumar Kamalanathan
World Journal of Virology.2022; 11(6): 399. CrossRef - Associations Between the Use of Renin–Angiotensin System Inhibitors and the Risks of Severe COVID-19 and Mortality in COVID-19 Patients With Hypertension: A Meta-Analysis of Observational Studies
Xiao-Ce Dai, Zhuo-Yu An, Zi-Yang Wang, Zi-Zhen Wang, Yi-Ren Wang
Frontiers in Cardiovascular Medicine.2021;[Epub] CrossRef - Risk phenotypes of diabetes and association with COVID-19 severity and death: a living systematic review and meta-analysis
Sabrina Schlesinger, Manuela Neuenschwander, Alexander Lang, Kalliopi Pafili, Oliver Kuss, Christian Herder, Michael Roden
Diabetologia.2021; 64(7): 1480. CrossRef - Protecting older patients with cardiovascular diseases from COVID-19 complications using current medications
Mariana Alves, Marília Andreia Fernandes, Gülistan Bahat, Athanase Benetos, Hugo Clemente, Tomasz Grodzicki, Manuel Martínez-Sellés, Francesco Mattace-Raso, Chakravarthi Rajkumar, Andrea Ungar, Nikos Werner, Timo E. Strandberg, Grodzicki, Strandberg
European Geriatric Medicine.2021; 12(4): 725. CrossRef - Cardiometabolic Therapy and Mortality in Very Old Patients With Diabetes Hospitalized due to COVID-19
Jose Manuel Ramos-Rincón, Luis M Pérez-Belmonte, Francisco Javier Carrasco-Sánchez, Sergio Jansen-Chaparro, Mercedes De-Sousa-Baena, José Bueno-Fonseca, Maria Pérez-Aguilar, Coral Arévalo-Cañas, Marta Bacete Cebrian, Manuel Méndez-Bailón, Isabel Fiteni Me
The Journals of Gerontology: Series A.2021; 76(8): e102. CrossRef - Managing diabetes in diabetic patients with COVID: where do we start from?
Angelo Avogaro, Benedetta Bonora, Gian Paolo Fadini
Acta Diabetologica.2021; 58(11): 1441. CrossRef - The SARS-CoV-2 receptor angiotensin-converting enzyme 2 (ACE2) in myalgic encephalomyelitis/chronic fatigue syndrome: A meta-analysis of public DNA methylation and gene expression data
João Malato, Franziska Sotzny, Sandra Bauer, Helma Freitag, André Fonseca, Anna D. Grabowska, Luís Graça, Clara Cordeiro, Luís Nacul, Eliana M. Lacerda, Jesus Castro-Marrero, Carmen Scheibenbogen, Francisco Westermeier, Nuno Sepúlveda
Heliyon.2021; 7(8): e07665. CrossRef - Effects of a DPP-4 Inhibitor and RAS Blockade on Clinical Outcomes of Patients with Diabetes and COVID-19 (Diabetes Metab J 2021;45:251-9)
Sang Youl Rhee
Diabetes & Metabolism Journal.2021; 45(4): 619. CrossRef - Effects of a DPP-4 Inhibitor and RAS Blockade on Clinical Outcomes of Patients with Diabetes and COVID-19 (Diabetes Metab J 2021;45:251-9)
Guntram Schernthaner
Diabetes & Metabolism Journal.2021; 45(4): 615. CrossRef - COVID-19 and metabolic disease: mechanisms and clinical management
Charlotte Steenblock, Peter E H Schwarz, Barbara Ludwig, Andreas Linkermann, Paul Zimmet, Konstantin Kulebyakin, Vsevolod A Tkachuk, Alexander G Markov, Hendrik Lehnert, Martin Hrabě de Angelis, Hannes Rietzsch, Roman N Rodionov, Kamlesh Khunti, David Hop
The Lancet Diabetes & Endocrinology.2021; 9(11): 786. CrossRef - Diabetes, Obesity, and COVID-19
Sang Youl Rhee
The Journal of Korean Diabetes.2021; 22(3): 174. CrossRef - Sunlight Exposure and Phototherapy: Perspectives for Healthy Aging in an Era of COVID-19
Toshiaki Nakano, Kuei-Chen Chiang, Chien-Chih Chen, Po-Jung Chen, Chia-Yun Lai, Li-Wen Hsu, Naoya Ohmori, Takeshi Goto, Chao-Long Chen, Shigeru Goto
International Journal of Environmental Research and Public Health.2021; 18(20): 10950. CrossRef - Analysis of influence of background therapy for comorbidities in the period before infection on the risk of the lethal COVID outcome. Data from the international ACTIV SARS-CoV-2 registry («Analysis of chronic non-infectious diseases dynamics after COVID-
E. I. Tarlovskaya, A. G. Arutyunov, A. O. Konradi, Yu. M. Lopatin, A. P. Rebrov, S. N. Tereshchenko, A. I. Chesnikova, H. G. Hayrapetyan, A. P. Babin, I. G. Bakulin, N. V. Bakulina, L. A. Balykova, A. S. Blagonravova, M. V. Boldina, A. R. Vaisberg, A. S.
Kardiologiia.2021; 61(9): 20. CrossRef - Association of clinical characteristics, antidiabetic and cardiovascular agents with diabetes mellitus and COVID-19: a 7-month follow-up cohort study
Marzieh Pazoki, Fatemeh Chichagi, Azar Hadadi, Samira Kafan, Mahnaz Montazeri, Sina Kazemian, Arya Aminorroaya, Mehdi Ebrahimi, Haleh Ashraf, Mojgan Mirabdolhagh Hazaveh, Mohammad Reza Khajavi, Reza Shariat Moharari, Seyed Hamidreza Sharifnia, Shahrokh Ka
Journal of Diabetes & Metabolic Disorders.2021; 20(2): 1545. CrossRef - COVID-19 and Diabetes: A Comprehensive Review of Angiotensin Converting Enzyme 2, Mutual Effects and Pharmacotherapy
Lingli Xie, Ziying Zhang, Qian Wang, Yangwen Chen, Dexue Lu, Weihua Wu
Frontiers in Endocrinology.2021;[Epub] CrossRef - The Roles of Dipeptidyl Peptidase 4 (DPP4) and DPP4 Inhibitors in Different Lung Diseases: New Evidence
Tianli Zhang, Xiang Tong, Shijie Zhang, Dongguang Wang, Lian Wang, Qian Wang, Hong Fan
Frontiers in Pharmacology.2021;[Epub] CrossRef
- The Impact of GLP-1 RAs and DPP-4is on Hospitalisation and Mortality in the COVID-19 Era: A Two-Year Observational Study
- Basic Research
- Umbilical Cord-Mesenchymal Stem Cell-Conditioned Medium Improves Insulin Resistance in C2C12 Cell
- Kyung-Soo Kim, Yeon Kyung Choi, Mi Jin Kim, Jung Wook Hwang, Kyunghoon Min, Sang Youn Jung, Soo-Kyung Kim, Yong-Soo Choi, Yong-Wook Cho
- Diabetes Metab J. 2021;45(2):260-269. Published online July 10, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0191

- 9,502 View
- 206 Download
- 8 Web of Science
- 8 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
Background Umbilical cord-mesenchymal stem cell-conditioned medium (UC-MSC-CM) has emerged as a promising cell-free therapy. The aim of this study was to explore the therapeutic effects of UC-MSC-CM on insulin resistance in C2C12 cell.
Methods Insulin resistance was induced by palmitate. Effects of UC-MSC-CM on insulin resistance were evaluated using glucose uptake, glucose transporter type 4 (GLUT4) translocation, the insulin-signaling pathway, and mitochondrial contents and functions in C2C12 cell.
Results Glucose uptake was improved by UC-MSC-CM. UC-MSC-CM treatment increased only in membranous GLUT4 expression, not in cytosolic GLUT4 expression. It restored the insulin-signaling pathway in insulin receptor substrate 1 and protein kinase B. Mitochondrial contents evaluated by mitochondrial transcription factor A, mitochondrial DNA copy number, and peroxisome proliferator-activated receptor gamma coactivator 1-alpha were increased by UC-MSC-CM. In addition, UC-MSC-CM significantly decreased mitochondrial reactive oxygen species and increased fatty acid oxidation and mitochondrial membrane potential. There was no improvement in adenosine triphosphate (ATP) contents, but ATP synthesis was improved by UC-MSC-CM. Cytokine and active factor analysis of UC-MSC-CM showed that it contained many regulators inhibiting insulin resistance.
Conclusion UC-MSC-CM improves insulin resistance with multiple mechanisms in C2C12 cell.
-
Citations
Citations to this article as recorded by- Neurotransmitters in Type 2 Diabetes and the Control of Systemic and Central Energy Balance
Amnah Al-Sayyar, Maha M. Hammad, Michayla R. Williams, Mohammed Al-Onaizi, Jehad Abubaker, Fawaz Alzaid
Metabolites.2023; 13(3): 384. CrossRef - Neuroprotective Effect of Wharton’s Jelly-Derived Mesenchymal Stem Cell-Conditioned Medium (WJMSC-CM) on Diabetes-Associated Cognitive Impairment by Improving Oxidative Stress, Neuroinflammation, and Apoptosis
Zohre Aghaei, Narges Karbalaei, Mohammad Reza Namavar, Masoud Haghani, Mahboobeh Razmkhah, Mahdi Khorsand Ghaffari, Marzieh Nemati, Andrea Ballini
Stem Cells International.2023; 2023: 1. CrossRef - Mesenchymal-Stem Cell-Derived Conditioned Media Versus Exosomes in the Treatment of Rat Model of Polycystic Ovary: An Attempt to Understand the Underlying Mechanisms (Biochemical and Histological Study)
Soha Abd-elkawy Abd-elwahab, Noura Hassan Khamis, Rehab Ahmed Rifaai, Nashwa Fathy Gamal El-Tahawy, Randa Ahmed Ibrahim
Microscopy and Microanalysis.2023; 29(3): 1244. CrossRef - Therapeutic Potential of Mesenchymal Stem Cell‐Derived Conditioned Medium for Diabetes Mellitus and Related Complications
Basak Isildar, Serbay Ozkan, Meral Koyuturk
Advanced Therapeutics.2023;[Epub] CrossRef - Treatment of type 2 diabetes mellitus with stem cells and antidiabetic drugs: a dualistic and future-focused approach
Priyamvada Amol Arte, Kanchanlata Tungare, Mustansir Bhori, Renitta Jobby, Jyotirmoi Aich
Human Cell.2023; 37(1): 54. CrossRef - Perinatal Stem Cell Therapy to Treat Type 1 Diabetes Mellitus: A Never-Say-Die Story of Differentiation and Immunomodulation
Francesca Paris, Valeria Pizzuti, Pasquale Marrazzo, Andrea Pession, Francesco Alviano, Laura Bonsi
International Journal of Molecular Sciences.2022; 23(23): 14597. CrossRef - Mesenchymal Stem Cell-Derived Apoptotic Bodies: Biological Functions and Therapeutic Potential
Huixue Tang, Huikun Luo, Zihan Zhang, Di Yang
Cells.2022; 11(23): 3879. CrossRef - Human umbilical cord mesenchymal stem cells in type 2 diabetes mellitus: the emerging therapeutic approach
Andreia Gomes, Pedro Coelho, Raquel Soares, Raquel Costa
Cell and Tissue Research.2021; 385(3): 497. CrossRef
- Neurotransmitters in Type 2 Diabetes and the Control of Systemic and Central Energy Balance
- Cardiovascular risk/Epidemiology
- Clinical Impact of Dysglycemia in Patients with an Acute Myocardial Infarction
- Jae-Wook Chung, Yeong-Seon Park, Jeong-Eon Seo, Yeseul Son, Cheol-Woo Oh, Chan-Hee Lee, Jong-Ho Nam, Jung-Hee Lee, Jang-Won Son, Ung Kim, Jong-Seon Park, Kyu-Chang Won, Dong-Gu Shin
- Diabetes Metab J. 2021;45(2):270-274. Published online April 16, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0164

- 5,652 View
- 119 Download
- 8 Web of Science
- 8 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 
This study aimed to determine the impact of dysglycemia on myocardial injury and cardiac dysfunction in acute myocardial infarctions (AMIs). From 2005 to 2016, a total of 1,593 patients with AMIs who underwent percutaneous coronary intervention were enrolled. The patients were classified into five groups according to the admission glucose level: ≤80, 81 to 140, 141 to 200, 201 to 260, and ≥261 mg/dL. The clinical and echocardiographic parameters and 30-day mortality were analyzed. The peak troponin I and white blood cell levels had a positive linear relationship to the admission glucose level. The left ventricular ejection fraction had an inverted
U -shape trend, and the E/E' ratio wasU -shaped based on euglycemia. The 30-day mortality also increased as the admission glucose increased, and the cut-off value for predicting the mortality was 202.5 mg/dL. Dysglycemia, especially hyperglycemia, appears to be associated with myocardial injury and could be another adjunctive parameter for predicting mortality in patients with AMIs.-
Citations
Citations to this article as recorded by- Optimal Low-Density Lipoprotein Cholesterol Levels in Adults Without Diabetes Mellitus: A Nationwide Population-Based Study Including More Than 4 Million Individuals From South Korea
Ji Hye Huh, Sang Wook Park, Tae-Hwa Go, Dae Ryong Kang, Sang-Hak Lee, Jang-Young Kim
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Association of admission hyperglycemia and all-cause mortality in acute myocardial infarction with percutaneous coronary intervention: A dose–response meta-analysis
Shao-Yong Cheng, Hao Wang, Shi-Hua Lin, Jin-Hui Wen, Ling-Ling Ma, Xiao-Ce Dai
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Fenofibrate add-on to statin treatment is associated with low all-cause death and cardiovascular disease in the general population with high triglyceride levels
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Metabolism.2022; 137: 155327. CrossRef - Basic types of the first-day glycemia in acute myocardial infarction: Prognostic, diagnostic, threshold and target glycemia
Goran Koracevic, Milan Djordjevic
Primary Care Diabetes.2021; 15(3): 614. CrossRef - Clinical Impact of Dysglycemia in Patients with an Acute Myocardial Infarction (Diabetes Metab J 2021;45:270-4)
Bo-Yeon Kim
Diabetes & Metabolism Journal.2021; 45(5): 787. CrossRef - Clinical Impact of Dysglycemia in Patients with an Acute Myocardial Infarction (Diabetes Metab J 2021;45:270-4)
Chan-Hee Lee
Diabetes & Metabolism Journal.2021; 45(5): 791. CrossRef - The Effects of Glucose Lowering Agents on the Secondary Prevention of Coronary Artery Disease in Patients with Type 2 Diabetes
Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
Endocrinology and Metabolism.2021; 36(5): 977. CrossRef - Effect of Admission Hyperglycemia on Short-Term Prognosis of Patients with Non-ST Elevation Acute Coronary Syndrome without Diabetes Mellitus
Wei Liu, Zhijuan Li, Shiying Xing, Yanwei Xu, Gaetano Santulli
Journal of Diabetes Research.2021; 2021: 1. CrossRef
- Optimal Low-Density Lipoprotein Cholesterol Levels in Adults Without Diabetes Mellitus: A Nationwide Population-Based Study Including More Than 4 Million Individuals From South Korea
- Impact of Social Distancing Due to Coronavirus Disease 2019 on the Changes in Glycosylated Hemoglobin Level in People with Type 2 Diabetes Mellitus (Diabetes Metab J 2021;45:109-14)
- Junghyun Noh
- Diabetes Metab J. 2021;45(2):275-276. Published online March 25, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0288
- 3,439 View
- 86 Download
- 2 Web of Science
- 1 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Blood hemoglobin A1c might predict adverse differences in heart rate variability in a diabetic population: Evidence from the Midlife in the United States (MIDUS) study
Ying Huang, Hong Chen, Dongxia Hu, Rong Wan
Frontiers in Endocrinology.2022;[Epub] CrossRef
- Blood hemoglobin A1c might predict adverse differences in heart rate variability in a diabetic population: Evidence from the Midlife in the United States (MIDUS) study

 KDA
KDA


 First
First Prev
Prev





