
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 45(2); 2021 > Article
-
Brief ReportCardiovascular risk/Epidemiology Clinical Impact of Dysglycemia in Patients with an Acute Myocardial Infarction
-
Jae-Wook Chung1
 , Yeong-Seon Park1, Jeong-Eon Seo1, Yeseul Son1, Cheol-Woo Oh1, Chan-Hee Lee1,2
, Yeong-Seon Park1, Jeong-Eon Seo1, Yeseul Son1, Cheol-Woo Oh1, Chan-Hee Lee1,2 , Jong-Ho Nam1,2, Jung-Hee Lee1,2, Jang-Won Son1,2, Ung Kim1,2, Jong-Seon Park1,2, Kyu-Chang Won1,3, Dong-Gu Shin1,2
, Jong-Ho Nam1,2, Jung-Hee Lee1,2, Jang-Won Son1,2, Ung Kim1,2, Jong-Seon Park1,2, Kyu-Chang Won1,3, Dong-Gu Shin1,2 -
Diabetes & Metabolism Journal 2021;45(2):270-274.
DOI: https://doi.org/10.4093/dmj.2019.0164
Published online: April 16, 2020
1Yeungnam University College of Medicine, Daegu, Korea
2Division of Cardiology, Department of Internal Medicine, Yeungnam University Medical Center, Daegu, Korea
3Division of Endocrinology, Department of Internal Medicine, Yeungnam University Medical Center, Daegu, Korea
-
Corresponding author: Chan-Hee Lee
 Division of Cardiology, Department of Internal Medicine, Yeungnam University Medical Center, Yeungnam University College of Medicine, 170 Hyunchoong-ro, Nam-gu, Daegu 42415, Korea. chanheebox@naver.com
Division of Cardiology, Department of Internal Medicine, Yeungnam University Medical Center, Yeungnam University College of Medicine, 170 Hyunchoong-ro, Nam-gu, Daegu 42415, Korea. chanheebox@naver.com
Copyright © 2021 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- This study aimed to determine the impact of dysglycemia on myocardial injury and cardiac dysfunction in acute myocardial infarctions (AMIs). From 2005 to 2016, a total of 1,593 patients with AMIs who underwent percutaneous coronary intervention were enrolled. The patients were classified into five groups according to the admission glucose level: ≤80, 81 to 140, 141 to 200, 201 to 260, and ≥261 mg/dL. The clinical and echocardiographic parameters and 30-day mortality were analyzed. The peak troponin I and white blood cell levels had a positive linear relationship to the admission glucose level. The left ventricular ejection fraction had an inverted U-shape trend, and the E/E' ratio was U-shaped based on euglycemia. The 30-day mortality also increased as the admission glucose increased, and the cut-off value for predicting the mortality was 202.5 mg/dL. Dysglycemia, especially hyperglycemia, appears to be associated with myocardial injury and could be another adjunctive parameter for predicting mortality in patients with AMIs.
- Hyperglycemia on admission is a common feature of the early phase of an acute myocardial infarction (AMI) with or without diabetes [1], and is also a prognostic factor of the mortality rate [234]. However, an association between dysglycemia and myocardial injury or the cardiac dysfunction, which eventually leads to death, is unclear in AMI patients. In the current study, we aimed to determine the impact of dysglycemia on myocardial injury, the cardiac function, and 30-day mortality in AMI patients that underwent percutaneous coronary intervention (PCI).
INTRODUCTION
- From October 2005 to January 2016, a total of 1,593 consecutive patients with an AMI who underwent a PCI at Yeungnam University Medical Center were enrolled. AMIs were diagnosed if the patients met the following criteria: (1) at least one positive cardiac biochemical marker of ischemia and (2) typical symptoms compatible with myocardial ischemia or new ischemic electrocardiographic changes, or imaging evidence of a new loss of viable myocardium, or new regional wall motion abnormality. This study was approved by the Institutional Review Board of the Yeungnam University Medical Center (No. 2019-08-037). Written informed consent by the patients was waived due to a retrospective nature of our study.
- We classified all patients into five groups according to the initial plasma glucose level on admission: Group 1 (hypoglycemic, n= 5), ≤80 mg/dL; Group 2 (euglycemic, n=634), 81 to 140 mg/dL; Group 3 (mild hyperglycemic, n=492), 141 to 200 mg/dL; Group 4 (moderate hyperglycemic, n=229), 201 to 260 mg/dL; and Group 5 (severe hyperglycemic, n=233), ≥261 mg/dL. The plasma glucose was the random, non-fasting glucose level at the time of hospital admission, and cut-off levels of 140 and 200 mg/dL were used according to the diagnostic criteria of impaired glucose tolerance in the American Diabetes Association (ADA) guidelines [5], and then each group was stratified at an interval of 60 mg/dL, referring to the grouping methods in the previous study about the admission glucose and mortality in the Korea Acute Myocardial Infarction Registry [6]. Diabetes mellitus (DM) was defined by the patient-reported history, medical records, or a glycosylated hemoglobin (HbA1c) value of ≥6.5% or an oral glucose tolerance test during the admission period according to the ADA guidelines. The clinical, laboratory, and echocardiographic parameters and 30-day mortality were analyzed.
- All statistical analyses were performed using IBM SPSS version 20.0 (IBM Co., Armonk, NY, USA). Continuous variables were compared using a one-way analysis of variance, Kruskal-Wallis test, independent Student's t-test, or Mann-Whitney U test. Categorical variables were compared using chi-square statistics or a Fisher's exact probability test. A P value <0.05 was considered statistically significant.
METHODS
- The mean age was 64.9±12.0 years (Table 1). The mean admission glucose level was 68.4 mg/dL in Group 1, 116.6 mg/dL in Group 2, 166.1 mg/dL in Group 3, 225.2 mg/dL in Group 4, and 348.4 mg/dL in Group 5, respectively.
- We analyzed the relationships between the admission glucose and serum N-terminal probrain natriuretic peptide (NT-proBNP), peak troponin I, and peak aspartate aminotransferase (AST) levels and the white blood cell (WBC) count during the admission period (Table 2). The troponin I and WBC levels exhibited a positive linear relationship to the admission glucose level (P<0.001), but the NT-proBNP level (the highest value of 5,295.8 pg/mL was observed in Group 1) and AST levels did not. In the echocardiographic parameters, the left ventricular ejection fraction (LVEF) had a trend of an inverted U-shape, while the transmitral Doppler early filling velocity to tissue Doppler early diastolic mitral annular velocity (E/E') ratio exhibited a U-shape trend based on Group 2.
- In a subgroup analysis, all patients were divided into diabetic (n=551) and nondiabetic groups (n=1,042) (Table 2). In the nondiabetic groups, the troponin I, AST, and WBC levels had a positive linear relationship to admission glucose level. The troponin I and AST levels were higher in nondiabetics than diabetics in Group 5 (P=0.033 and P<0.001, respectively).
- Among 1,593 patients, 69 (4.3%) died within 30 days. The 30-day mortality increased according to the groups (1.9% for Group 2, 2.8% for Group 3, 6.1% for Group 4, and 12.4% for Group 5, P<0.001) excluding Group 1. The cut-off value for predicting the 30-day mortality was 202.5 mg/dL (area under the curve 0.703, sensitivity 0.623, specificity 0.741, P<0.001). Forty out of 1,042 nondiabetics and 29 of 551 diabetics died within 30-days. In the nondiabetic groups, there was a linear correlation between the admission glucose level and 30-day mortality. Of note, in Group 5, the 30-day mortality in nondiabetics was higher than that in diabetics (P<0.001). The cut-off value for predicting the 30-day mortality was 174.5 mg/dL in nondiabetics and 208.5 mg/dL in diabetics.
RESULTS
- In this study, we chose the laboratory parameters, including the serum NT-proBNP, peak troponin I [78], and AST level [9], during admission as a marker of myocardial injury and the WBC count as a marker of myocardial inflammation [10]. Further, we also chose representative echocardiographic parameters, including the LVEF as a marker of the systolic cardiac function, and the E/E' ratio as a marker of the diastolic function [1112].
- Previous studies reported that hyperglycemia is related to myocardial injury by analyzing the effects of a high admission glucose level on the LVEF at admission and discharge [13]. In this study, it was significant in that the factors more directly reflecting myocardial injury were used to demonstrate the connection between the blood glucose level and myocardial injury. This research also showed that a high admission glucose level during an AMI was related to a higher short-term mortality. As a result, the blood glucose level had the possibility of being used as an assisting factor for predicting myocardial injury and the short-term mortality during AMIs owing to the advantage it has in being able to be measured easily compared to the other factors.
- In our research, severe hyperglycemia (Group 5) in the AMI patients was associated with a greater 30-day mortality in the nondiabetic group than diabetic group (P<0.001). Also, the troponin I and AST levels were higher in the nondiabetics, which meant the cardiac injury during hyperglycemia was more severe and stressful in nondiabetics than diabetics. Additionally, the mortality could be low in diabetics because the threshold of the blood glucose causing cell damage might increase in diabetics [14].
- This study had several limitations. First, this study was a single center and retrospective study based on AMI patients with a PCI. Therefore, this data did not include patients who did not receive a PCI or who already died in the emergency room. Second, there was the possibility of other factors that could have affected the admission glucose level such as the food intake, meal time intervals, and amount of food. Finally, there was a limited number of patients in Group 1, so it was hard to assess the relationship between hypoglycemia and myocardial injury or dysfunction. Although the diabetic patients with admission hypoglycemia had the highest NT-proBNP level and E/E' ratio and worst LVEF in the subgroup analysis, we could not perform a mortality analysis because of the scanty number of patients in that subgroup.
- In conclusion, dysglycemia, especially hyperglycemia, appears to be associated with myocardial injury, and could be another adjunctive parameter for predicting the mortality in patients with an AMI.
DISCUSSION
-
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
-
AUTHOR CONTRIBUTIONS
Conception or design: C.H.L.
Acquisition, analysis, or interpretation of data: J.W.C., Y.S.P., J.E.S., Y.S., C.W.O., J.H.N., J.H,L., J.W.S., U.K., J.S.P., K.C.W., D.G.S.
Drafting the work or revising: J.W.C., C.H.L.
Final approval of the manuscript: C.H.L.
-
FUNDING
None
NOTES
-
Acknowledgements
- None.
ACKNOWLEDGMENTS
- 1. Oswald GA, Corcoran S, Yudkin JS. Prevalence and risks of hyperglycaemia and undiagnosed diabetes in patients with acute myocardial infarction. Lancet 1984;1:1264-1267.ArticlePubMed
- 2. Pinto DS, Skolnick AH, Kirtane AJ, Murphy SA, Barron HV, Giugliano RP, et al. TIMI Study Group. U-shaped relationship of blood glucose with adverse outcomes among patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol 2005;46:178-180.ArticlePubMed
- 3. Capes SE, Hunt D, Malmberg K, Gerstein HC. Stress hyperglycaemia and increased risk of death after myocardial infarction in patients with and without diabetes: a systematic overview. Lancet 2000;355:773-778.ArticlePubMed
- 4. Kosiborod M, Inzucchi SE, Goyal A, Krumholz HM, Masoudi FA, Xiao L, et al. Relationship between spontaneous and iatrogenic hypoglycemia and mortality in patients hospitalized with acute myocardial infarction. JAMA 2009;301:1556-1564.ArticlePubMed
- 5. American Diabetes Association. 2. Classification and diagnosis of diabetes. Diabetes Care 2016;39 Suppl 1:S13-S22.ArticlePubMedPDF
- 6. Lee SA, Cho SJ, Jeong MH, Kim YJ, Kim CJ, Cho MC, et al. KAMIR/KorMI Registry. Hypoglycemia at admission in patients with acute myocardial infarction predicts a higher 30-day mortality in patients with poorly controlled type 2 diabetes than in well-controlled patients. Diabetes Care 2014;37:2366-2373.ArticlePubMedPDF
- 7. Kontos MC, Shah R, Fritz LM, Anderson FP, Tatum JL, Ornato JP, et al. Implication of different cardiac troponin I levels for clinical outcomes and prognosis of acute chest pain patients. J Am Coll Cardiol 2004;43:958-965.ArticlePubMed
- 8. Antman EM, Tanasijevic MJ, Thompson B, Schactman M, McCabe CH, Cannon CP, et al. Cardiac-specific troponin I levels to predict the risk of mortality in patients with acute coronary syndromes. N Engl J Med 1996;335:1342-1349.ArticlePubMed
- 9. Lofthus DM, Stevens SR, Armstrong PW, Granger CB, Mahaffey KW. Pattern of liver enzyme elevations in acute ST-elevation myocardial infarction. Coron Artery Dis 2012;23:22-30.ArticlePubMed
- 10. Sabatine MS, Morrow DA, Cannon CP, Murphy SA, Demopoulos LA, DiBattiste PM, et al. Relationship between baseline white blood cell count and degree of coronary artery disease and mortality in patients with acute coronary syndromes: a TACTICS-TIMI 18 (Treat Angina with Aggrastat and determine Cost of Therapy with an Invasive or Conservative Strategy: Thrombolysis in Myocardial Infarction 18 trial) substudy. J Am Coll Cardiol 2002;40:1761-1768.PubMed
- 11. Thune JJ, Solomon SD. Left ventricular diastolic function following myocardial infarction. Curr Heart Fail Rep 2006;3:170-174.ArticlePubMedPDF
- 12. Kettunen RV, Leppaluoto J, Jounela A, Vuolteenaho O. Plasma N-terminal atrial natriuretic peptide in acute myocardial infarction. Am Heart J 1994;127:1449-1455.ArticlePubMed
- 13. Ishihara M, Inoue I, Kawagoe T, Shimatani Y, Kurisu S, Nishioka K, et al. Impact of acute hyperglycemia on left ventricular function after reperfusion therapy in patients with a first anterior wall acute myocardial infarction. Am Heart J 2003;146:674-678.ArticlePubMed
- 14. Ishihara M, Kojima S, Sakamoto T, Kimura K, Kosuge M, Asada Y, et al. Japanese Acute Coronary Syndrome Study (JACSS) Investigators. Comparison of blood glucose values on admission for acute myocardial infarction in patients with versus without diabetes mellitus. Am J Cardiol 2009;104:769-774.ArticlePubMed
REFERENCES
Values are presented as mean±standard deviation or number (%).
BMI, body mass index; STEMI, ST-segment elevation myocardial infarction; NSTEMI, non-ST-segment elevation myocardial infarction; DM, diabetes mellitus; BP, blood pressure; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; HbA1c, glycosylated hemoglobin.
| Variable | Group 1 | Group 2 | Group 3 | Group 4 | Group 5 | P value | |
|---|---|---|---|---|---|---|---|
| <80 mg/dL (n=5) | 81–140 mg/dL (n=634) | 141–200 mg/dL (n=492) | 201–260 mg/dL (n=229) | >260 mg/dL (n=233) | |||
| NT-proBNP, pq/mL | |||||||
| Total | 5,295.8 | 1,424.5 | 1,931.8 | 2,260.2 | 4,170.1 | <0.001 | |
| DMa | 12,911.5 | 2,308.2 | 3,181.5 | 2,797.4 | 4,616.5 | 0.009 | |
| Non-DMb | 218.7 | 1,301.2 | 1,397.3 | 1,530.3 | 2,109.3 | 0.698 | |
| P valuec | <0.001 | 0.012 | <0.001 | 0.002 | 0.005 | ||
| Troponin I, ng/mL | |||||||
| Total | 10.9 | 30.1 | 49.5 | 48.3 | 51.8 | <0.001 | |
| DM | 5.7 | 25.2 | 40.7 | 44.5 | 47.5 | 0.071 | |
| Non-DM | 14.3 | 30.7 | 53.3 | 53.5 | 71.9 | <0.001 | |
| P value | 0.088 | 0.591 | 0.169 | 0.374 | 0.033 | ||
| AST, IU/L | |||||||
| Total | 49.6 | 120.3 | 201.5 | 233.8 | 254.6 | 0.055 | |
| DM | 35.0 | 89.5 | 122.5 | 127.2 | 194.7 | 0.187 | |
| Non-DM | 59.3 | 124.6 | 235.3 | 380.5 | 533.1 | 0.002 | |
| P value | 0.210 | 0.191 | 0.108 | 0.005 | <0.001 | ||
| WBC, K/μL | |||||||
| Total | 7.1 | 9.7 | 10.5 | 11.0 | 12.7 | <0.001 | |
| DM | 6.9 | 9.3 | 10.2 | 10.7 | 12.2 | <0.001 | |
| Non-DM | 7.3 | 9.7 | 10.6 | 11.4 | 15.0 | <0.001 | |
| P value | 0.440 | 0.599 | 0.444 | 0.645 | 0.132 | ||
| LVEF, % | |||||||
| Total | 51.6 | 52.3 | 49.2 | 49.4 | 46.1 | <0.001 | |
| DM | 44.0 | 50.0 | 48.2 | 49.2 | 45.8 | 0.023 | |
| Non-DM | 56.7 | 52.6 | 49.7 | 49.7 | 47.8 | <0.001 | |
| P value | 0.136 | 0.802 | 0.399 | 0.525 | 0.729 | ||
| E/E’ ratio | |||||||
| Total | 16.2 | 12.1 | 12.6 | 13.6 | 15.1 | <0.001 | |
| DM | 23.4 | 13.9 | 13.6 | 13.9 | 15.3 | 0.046 | |
| Non-DM | 11.4 | 11.9 | 12.1 | 13.2 | 14.3 | 0.037 | |
| P value | 0.342 | <0.001 | 0.054 | 0.707 | 0.808 | ||
| Mortality, % | |||||||
| Total | 0.0 | 1.9 | 2.8 | 6.1 | 12.4 | <0.001 | |
| DM | 0.0 | 2.6 | 2.0 | 5.3 | 8.9 | <0.001 | |
| Non-DM | 0.0 | 1.8 | 3.2 | 7.3 | 29.3 | 0.055 | |
| P value | - | 0.751 | 0.410 | 0.482 | <0.001 | ||
NT-proBNP, N-terminal probrain natriuretic peptide; DM, diabetes mellitus; AST, aspartate aminotransferase; WBC, white blood cell count; LVEF, left ventricular ejection fraction; E/E’, the ratio of transmitral Doppler early filling velocity to tissue Doppler early diastolic mitral annular velocity.
a n=551,
b n=1,042,
c P value between the DM and non-DM groups.
Figure & Data
References
Citations

- Optimal Low-Density Lipoprotein Cholesterol Levels in Adults Without Diabetes Mellitus: A Nationwide Population-Based Study Including More Than 4 Million Individuals From South Korea
Ji Hye Huh, Sang Wook Park, Tae-Hwa Go, Dae Ryong Kang, Sang-Hak Lee, Jang-Young Kim
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Association of admission hyperglycemia and all-cause mortality in acute myocardial infarction with percutaneous coronary intervention: A dose–response meta-analysis
Shao-Yong Cheng, Hao Wang, Shi-Hua Lin, Jin-Hui Wen, Ling-Ling Ma, Xiao-Ce Dai
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Fenofibrate add-on to statin treatment is associated with low all-cause death and cardiovascular disease in the general population with high triglyceride levels
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Metabolism.2022; 137: 155327. CrossRef - Basic types of the first-day glycemia in acute myocardial infarction: Prognostic, diagnostic, threshold and target glycemia
Goran Koracevic, Milan Djordjevic
Primary Care Diabetes.2021; 15(3): 614. CrossRef - Clinical Impact of Dysglycemia in Patients with an Acute Myocardial Infarction (Diabetes Metab J 2021;45:270-4)
Bo-Yeon Kim
Diabetes & Metabolism Journal.2021; 45(5): 787. CrossRef - Clinical Impact of Dysglycemia in Patients with an Acute Myocardial Infarction (Diabetes Metab J 2021;45:270-4)
Chan-Hee Lee
Diabetes & Metabolism Journal.2021; 45(5): 791. CrossRef - The Effects of Glucose Lowering Agents on the Secondary Prevention of Coronary Artery Disease in Patients with Type 2 Diabetes
Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
Endocrinology and Metabolism.2021; 36(5): 977. CrossRef - Effect of Admission Hyperglycemia on Short-Term Prognosis of Patients with Non-ST Elevation Acute Coronary Syndrome without Diabetes Mellitus
Wei Liu, Zhijuan Li, Shiying Xing, Yanwei Xu, Gaetano Santulli
Journal of Diabetes Research.2021; 2021: 1. CrossRef

 KDA
KDA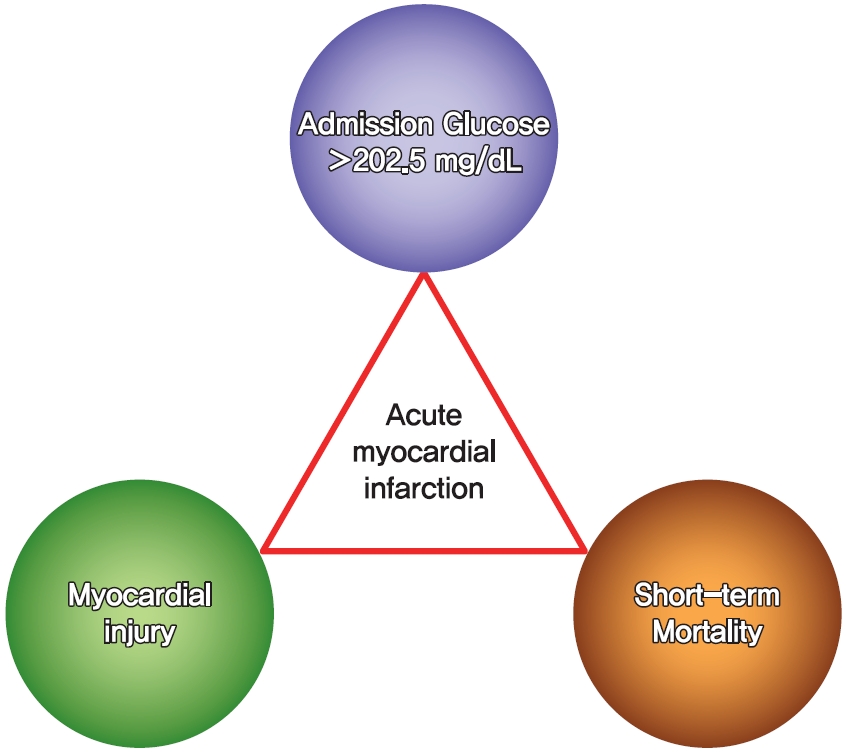
 PubReader
PubReader ePub Link
ePub Link Cite
Cite




