
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Cardiovascular Risk/Epidemiology
- The Role of Echocardiography in Evaluating Cardiovascular Diseases in Patients with Diabetes Mellitus
- Sun Hwa Lee, Jae-Hyeong Park
- Diabetes Metab J. 2023;47(4):470-483. Published online July 27, 2023
- DOI: https://doi.org/10.4093/dmj.2023.0036

- 2,729 View
- 293 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Patients with diabetes mellitus are highly susceptible to cardiovascular complications, which are directly correlated with cardiovascular morbidity and mortality. In addition to coronary artery disease, there is growing awareness of the risk and prevalence of heart failure (HF) in patients with diabetes. Echocardiography is an essential diagnostic modality commonly performed in patients with symptoms suggestive of cardiovascular diseases (CVD), such as dyspnea or chest pain, to establish or rule out the cause of symptoms. Conventional echocardiographic parameters, such as left ventricular ejection fraction, are helpful not only for diagnosing CVD but also for determining severity, treatment strategy, prognosis, and response to treatment. Echocardiographic myocardial strain, a novel echocardiographic technique, enables the detection of early changes in ventricular dysfunction before HF symptoms develop. This article aims to review the role of echocardiography in evaluating CVD in patients with diabetes mellitus and how to use it in patients with suspected cardiac diseases.
-
Citations
Citations to this article as recorded by- Increased Blood Pressure Variability Over a 16-Year Period Is Associated With Left Ventricular Diastolic Dysfunction in a Population-Based Cohort
Jae-Hyeong Park, Soon-Ki Ahn, Goo-Yeong Cho, Ki-Chul Sung, Seung Ku Lee, Seong Hwan Kim, Chol Shin
American Journal of Hypertension.2024; 37(3): 168. CrossRef - Biomarkers and subclinical left ventricular dysfunction in patients with type 2 diabetes without clinical manifestations of cardiovascular diseases
T. G. Utina, D. U. Akasheva, D. V. Korsunsky, O. N. Dzhioeva, O. M. Drapkina
Cardiovascular Therapy and Prevention.2024; 23(1): 3914. CrossRef - Cardiovascular risk assessment in inflammatory bowel disease with coronary calcium score
Waqar Arif Rasool Chaudhry, Muhammad Ashfaq, Parvinder Kaur, Mahendra Kumar, Maria Faraz, Jahanzeb Malik, Amin Mehmoodi
Annals of Medicine & Surgery.2024; 86(3): 1496. CrossRef
- Increased Blood Pressure Variability Over a 16-Year Period Is Associated With Left Ventricular Diastolic Dysfunction in a Population-Based Cohort
- Cardiovascular Risk/Epidemiology
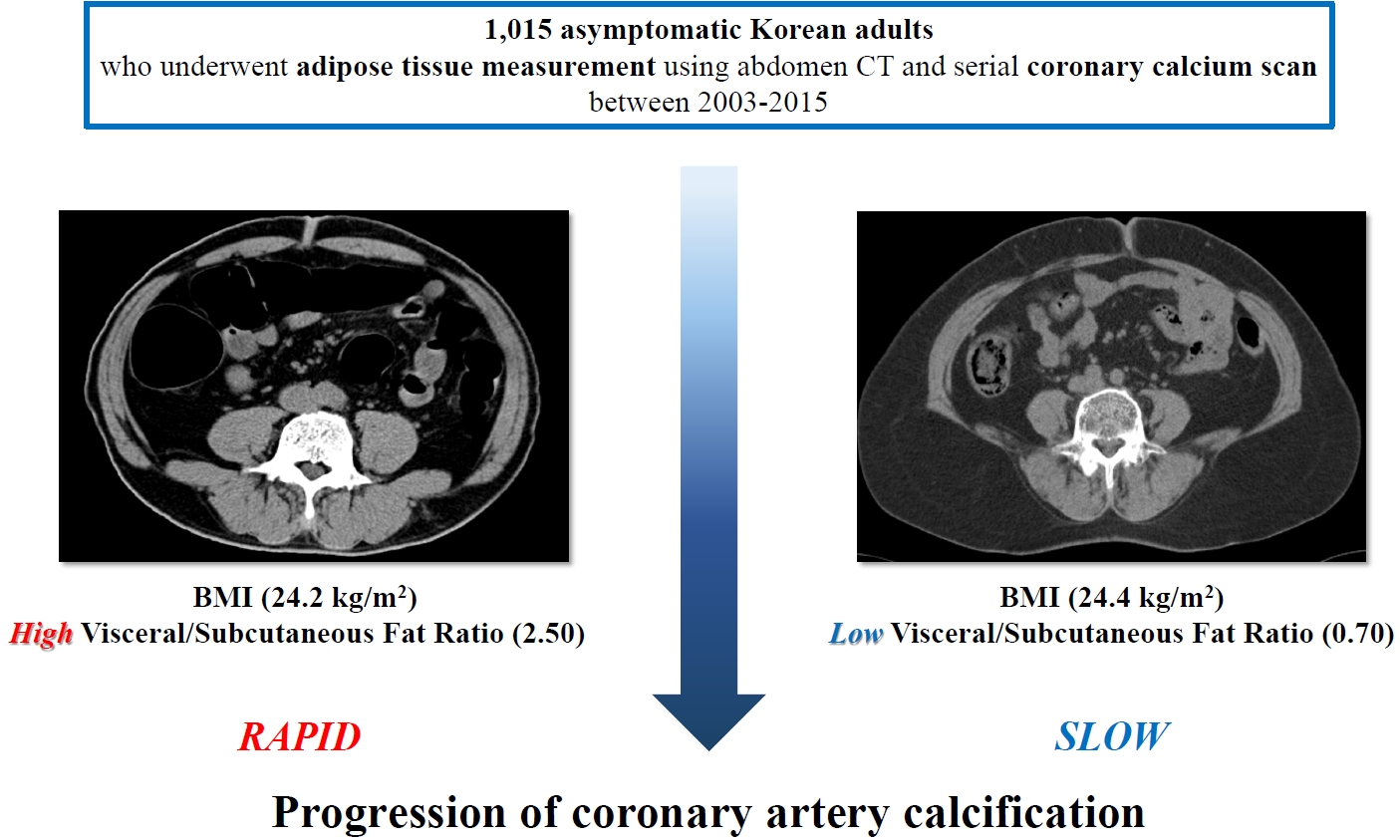
- Clinical Significance of Body Fat Distribution in Coronary Artery Calcification Progression in Korean Population
- Heesun Lee, Hyo Eun Park, Ji Won Yoon, Su-Yeon Choi
- Diabetes Metab J. 2021;45(2):219-230. Published online October 28, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0161
- Correction in: Diabetes Metab J 2021;45(6):974
- 6,498 View
- 257 Download
- 8 Web of Science
- 7 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 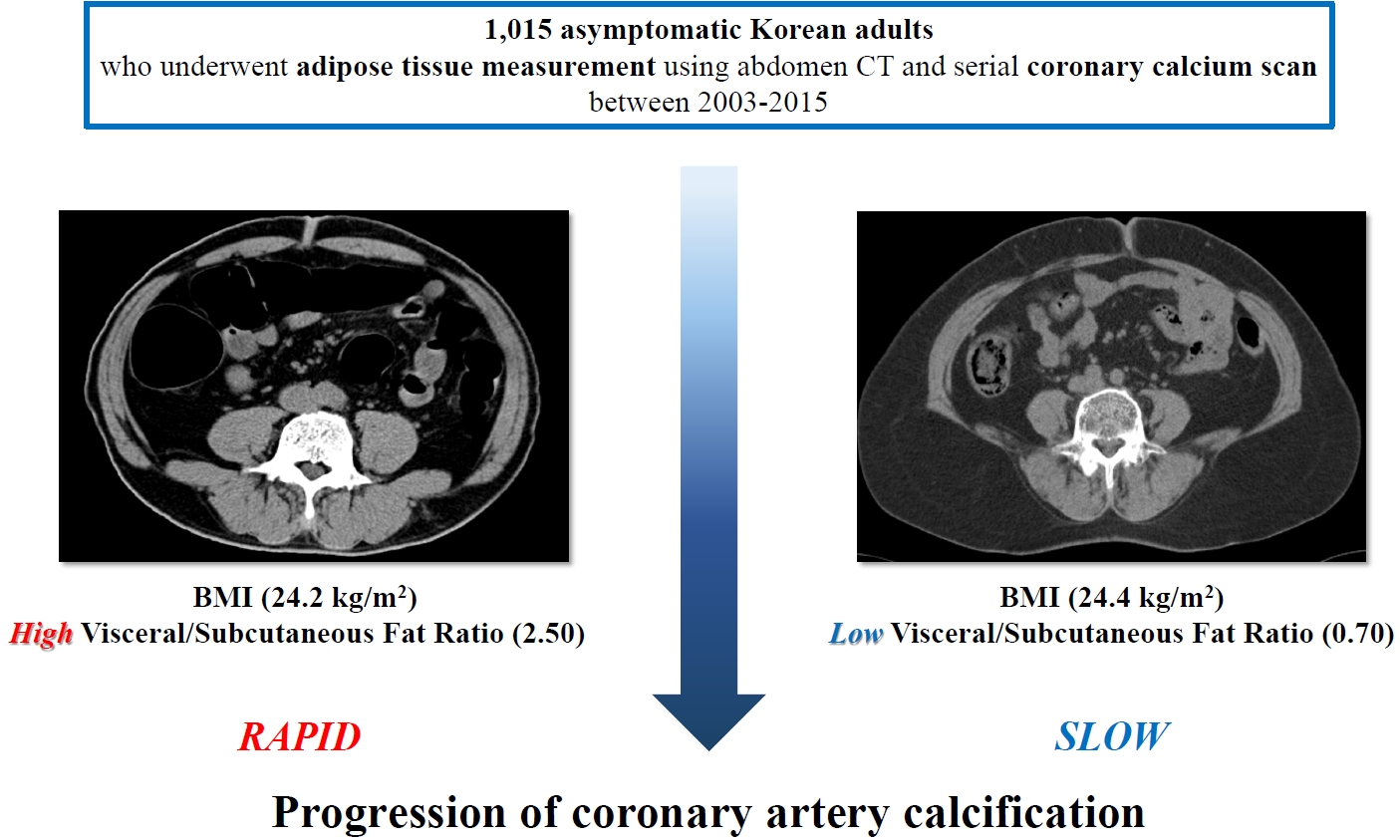
- Background
Although obesity differs according to ethnicity, it is globally established as a solid risk factor for cardiovascular disease. However, it is not fully understood how obesity parameters affect the progression of coronary artery calcification (CAC) in Korean population. We sought to evaluate the association of obesity-related parameters including visceral adipose tissue (VAT) measurement and CAC progression.
Methods
This retrospective observational cohort study investigated 1,015 asymptomatic Korean subjects who underwent serial CAC scoring by computed tomography (CT) with at least 1-year interval and adipose tissue measurement using non-contrast CT at baseline for a routine checkup between 2003 and 2015. CAC progression, the main outcome, was defined as a difference of ≥2.5 between the square roots of the baseline and follow-up CAC scores using Agatston units.
Results
During follow-up (median 39 months), 37.5% of subjects showed CAC progression of a total population (56.4 years, 80.6% male). Body mass index (BMI) ≥25 kg/m2, increasing waist circumferences (WC), and higher VAT/subcutaneous adipose tissue (SAT) area ratio were independently associated with CAC progression. Particularly, predominance of VAT over SAT at ≥30% showed the strongest prediction for CAC progression (adjusted hazard ratio, 2.20; P<0.001) and remained of prognostic value regardless of BMI or WC status. Further, it provided improved risk stratification of CAC progression beyond known prognosticators.
Conclusion
Predominant VAT area on CT is the strongest predictor of CAC progression regardless of BMI or WC in apparently healthy Korean population. Assessment of body fat distribution may be helpful to identify subjects at higher risk. -
Citations
Citations to this article as recorded by- Gender-specific abdominal fat distribution and insulin resistance associated with organophosphate esters and phthalate metabolites exposure
Xiaoliu Shi, Wanyue Wang, Jiafan Feng, Xiaochun Ma, Mengting Xu, Cui Wang
Environmental Pollution.2024; 349: 123959. CrossRef - The association between C-reactive protein and coronary artery calcification: a systematic review and meta-analysis
Amirhossein Tajani, Masoumeh Sadeghi, Navid Omidkhoda, Amir Hooshang Mohammadpour, Sara Samadi, Vahid Jomehzadeh
BMC Cardiovascular Disorders.2024;[Epub] CrossRef - Visceral adipose tissue is an independent predictor and mediator of the progression of coronary calcification: a prospective sub-analysis of the GEA study
Neftali Eduardo Antonio-Villa, Juan Gabriel Juárez-Rojas, Rosalinda Posadas-Sánchez, Juan Reyes-Barrera, Aida Medina-Urrutia
Cardiovascular Diabetology.2023;[Epub] CrossRef - Deep learning-based prediction for significant coronary artery stenosis on coronary computed tomography angiography in asymptomatic populations
Heesun Lee, Bong Gyun Kang, Jeonghee Jo, Hyo Eun Park, Sungroh Yoon, Su-Yeon Choi, Min Joo Kim
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Relationship between a novel non–insulin-based metabolic score for insulin resistance (METS‐IR) and coronary artery calcification
Zhenwei Wang, Xiaofang Hui, Xu Huang, Jingjie Li, Naifeng Liu
BMC Endocrine Disorders.2022;[Epub] CrossRef - Association Between Abdominal Adipose Tissue Distribution and Risk of Endometrial Cancer: A Case-Control Study
Yuan Cheng, Zhongyu Wang, Xiaoxuan Jia, Rong Zhou, Jianliu Wang
Clinical Medicine Insights: Oncology.2022; 16: 117955492211407. CrossRef - Sex differences in cardiovascular risk may be related to sex differences in diet patterns: a narrative review
A. M. Tindall, V. A. Stallings
Annals of Human Biology.2021; 48(6): 517. CrossRef
- Gender-specific abdominal fat distribution and insulin resistance associated with organophosphate esters and phthalate metabolites exposure
- Cardiovascular Risk/Epidemiology
- Impact of Diabetes Control on Subclinical Atherosclerosis: Analysis from Coronary Computed Tomographic Angiography Registry
- Gyung-Min Park, Chang Hoon Lee, Seung-Whan Lee, Sung-Cheol Yun, Young-Hak Kim, Yong-Giun Kim, Ki-Bum Won, Soe Hee Ann, Shin-Jae Kim, Dong Hyun Yang, Joon-Won Kang, Tae-Hwan Lim, Eun Hee Koh, Woo Je Lee, Min-Seon Kim, Joong-Yeol Park, Hong-Kyu Kim, Jaewon Choe, Sang-Gon Lee
- Diabetes Metab J. 2020;44(3):470-479. Published online November 22, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0073
- 8,672 View
- 69 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background There are limited data on the impact of diabetes control on the risk of subclinical coronary atherosclerosis.
Methods We analyzed 6,434 consecutive asymptomatic individuals without previous history of coronary artery disease who underwent coronary computed tomographic angiography (CCTA) (mean age, 53.7±7.6 years and 4,694 men [73.0%]). The degree and extent of subclinical coronary atherosclerosis were assessed by CCTA, and ≥50% diameter stenosis was defined as significant. A cardiac event was defined as a composite of all-cause death, myocardial infarction, unstable angina, or coronary revascularization. Study participants were categorized as normal (
n =5,319), controlled diabetes (glycosylated hemoglobin [HbA1c] <7%,n =747), or uncontrolled diabetes (HbA1c ≥7%,n =368), respectively.Results Compared with normal individuals, there were no statistically significant differences in the risk of for any atherosclerotic plaque (odds ratio [OR], 1.16; 95% confidence interval [CI], 0.98 to 1.38;
P =0.086) and significant coronary artery stenosis (OR, 1.08; 95% CI, 0.82 to 1.42;P =0.583) in controlled diabetic individuals. In contrast, uncontrolled diabetic individuals had consistently higher risks of any atherosclerotic plaque (OR, 2.16; 95% CI, 1.70 to 2.75;P <0.001) and significant coronary artery stenosis (OR, 3.34; 95% CI, 2.52 to 4.43;P <0.001) than normal individuals. During a follow-up of median 5.4 years, there was no significant difference in cardiac events between normal and controlled diabetic individuals (P =0.365). However, uncontrolled diabetes was associated with an increased risk of cardiac events compared with normal individuals (P <0.001) and controlled diabetic individuals (P =0.023).Conclusion Asymptomatic uncontrolled diabetes was associated with significant subclinical coronary atherosclerosis with subsequent high risk for cardiac events.
-
Citations
Citations to this article as recorded by- Carotid Ultrasound Abnormalities of People Living With HIV in Kunming, China: Multiple Correspondence Analysis Approach to Identify Influencing Factors
Shuishui Pan, Haiyan Fu, Zhiqiong Ai, Chongxi Li, Jinsong Bai
International Journal of STD & AIDS.2023; 34(10): 710. CrossRef - Differential Impact of Degree of Hypertension on Subclinical Coronary Atherosclerosis in Asymptomatic Subjects With and Without Diabetes Mellitus
Hyun Woo Park, Sangyong Jo, Kyung Sun Park, Hyeji Lee, Young-Jee Jeon, Sangwoo Park, Soe Hee Ann, Yong-Giun Kim, Seong Hoon Choi, Woon Jung Kwon, Young-Rak Cho, Jon Suh, Gyung-Min Park
The American Journal of Cardiology.2023; 203: 343. CrossRef - Exosomal MALAT1 Derived from High Glucose-Treated Macrophages Up-Regulates Resistin Expression via miR-150-5p Downregulation
Kou-Gi Shyu, Bao-Wei Wang, Wei-Jen Fang, Chun-Ming Pan, Chiu-Mei Lin
International Journal of Molecular Sciences.2022; 23(3): 1095. CrossRef - Comparison of Framingham risk score and pooled cohort equations for the prediction of coronary atherosclerosis in patients who meet the target LDL-C level of Korean dyslipidemia guideline
Su Bin Kim, Hae Won Jung
Medicine.2022; 101(47): e31816. CrossRef - Time to Reach Target Glycosylated Hemoglobin Is Associated with Long-Term Durable Glycemic Control and Risk of Diabetic Complications in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A 6-Year Observational Study
Kyoung Jin Kim, Jimi Choi, Jae Hyun Bae, Kyeong Jin Kim, Hye Jin Yoo, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2021; 45(3): 368. CrossRef - Frequency and Significance of Right Bundle Branch Block and Subclinical Coronary Atherosclerosis in Asymptomatic Individuals
Hyeji Lee, Young-Jee Jeon, Byung Ju Kang, Tae Young Lee, Eun Ji Park, Sangwoo Park, Soe Hee Ann, Yong-Giun Kim, Yongjik Lee, Seong Hoon Choi, Gyung-Min Park
The American Journal of Cardiology.2021; 158: 30. CrossRef - The association between glucose-related variables and plaque morphology in patients with ST-segment elevated myocardial infarction
Jinxin Liu, Shanjie Wang, Can Cui, Hengxuan Cai, Rong Sun, Weili Pan, Shaohong Fang, Bo Yu
Cardiovascular Diabetology.2020;[Epub] CrossRef - Choosing Antithrombotic Therapy in Patients with Coronary Heart Disease and Type 2 Diabetes Mellitus: How to Reduce the Risk of Death
N. A. Koziolova, P. G. Karavaev, A. S. Veklich
Kardiologiia.2020; 60(4): 109. CrossRef
- Carotid Ultrasound Abnormalities of People Living With HIV in Kunming, China: Multiple Correspondence Analysis Approach to Identify Influencing Factors
- Complications
- Serum Total Bilirubin Levels Provide Additive Risk Information over the Framingham Risk Score for Identifying Asymptomatic Diabetic Patients at Higher Risk for Coronary Artery Stenosis
- Jaechan Leem, Eun Hee Koh, Jung Eun Jang, Chang-Yun Woo, Jin Sun Oh, Min Jung Lee, Joon-Won Kang, Tae-Hwan Lim, Chang Hee Jung, Woo Je Lee, Joong-Yeol Park, Ki-Up Lee
- Diabetes Metab J. 2015;39(5):414-423. Published online October 22, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.5.414
- 4,232 View
- 30 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The diagnosis of coronary artery disease (CAD) is often delayed in patients with type 2 diabetes. Serum total bilirubin levels are inversely associated with CAD. However, no studies have examined whether this can be used as a biochemical marker for identifying asymptomatic diabetic patients at higher risk for having obstructive CAD.
Methods We performed a cross-sectional study of 460 consecutive asymptomatic patients with type 2 diabetes. All patients underwent coronary computed tomographic angiography, and their serum total bilirubin levels were measured. Obstructive CAD was defined as ≥50% diameter stenosis in at least one coronary artery.
Results Serum total bilirubin tertiles showed an inverse association with the prevalence of obstructive CAD. In multivariate logistic regression analysis, the odds ratio for the highest versus the lowest tertile of total bilirubin was 0.227 (95% confidence interval [CI], 0.130 to 0.398), and an increment of 1 µmol/L in serum total bilirubin level was associated with a 14.6% decrease in obstructive CAD after adjustment for confounding variables. Receiver operating characteristic curve analysis showed that the area under the curve for the Framingham Risk Score (FRS) plus serum total bilirubin level was 0.712 (95% CI, 0.668 to 0.753), which is significantly greater than that of the FRS alone (
P =0.0028).Conclusion Serum total bilirubin level is inversely associated with obstructive CAD and provides additive risk information over the FRS. Serum total bilirubin may be helpful for identifying asymptomatic patients with type 2 diabetes who are at higher risk for obstructive CAD.
-
Citations
Citations to this article as recorded by- DECREASE IN SERUM BILIRUBIN AS AN UNFAVORABLE MARKER OF CARDIOVASCULAR DISORDERS
L. M. Strilchuk, O. O. Zimba, I. B. Zhakun
Eastern Ukrainian Medical Journal.2020; 8(3): 268. CrossRef - Contemporary diagnostic algorithm for coronary artery disease: achievements and prospects
A. S. Akselrod, D. Yu. Shchekochikhin, E. S. Tebenkova, A. V. Zhelankin, D. A. Stonogina, E. A. Syrkina, S. K. Ternovoy
Kardiologiya i serdechno-sosudistaya khirurgiya.2019; 12(5): 418. CrossRef - Pharmacological actions and therapeutic potentials of bilirubin in islet transplantation for the treatment of diabetes
Qing Yao, Xue Jiang, Longfa Kou, Adelaide T. Samuriwo, He-Lin Xu, Ying-Zheng Zhao
Pharmacological Research.2019; 145: 104256. CrossRef - Evaluation of genetic effect of NOS3 and G×E interaction on the variability of serum bilirubin in a Han Chinese population
Yingshui Yao, Zhengmei Fang, Song Yang, Hailong Zhao, Yanchun Chen, Yuelong Jin, Xianghai Zhao, Lijun Zhu, Yuanrui Tian, Chong Shen
Nitric Oxide.2017; 70: 25. CrossRef - Supplementation with Phycocyanobilin, Citrulline, Taurine, and Supranutritional Doses of Folic Acid and Biotin—Potential for Preventing or Slowing the Progression of Diabetic Complications
Mark McCarty
Healthcare.2017; 5(1): 15. CrossRef - Effect of bilirubin concentration on the risk of diabetic complications: A meta-analysis of epidemiologic studies
Bo Zhu, Xiaomei Wu, Yifei Bi, Yang Yang
Scientific Reports.2017;[Epub] CrossRef - Role of Bilirubin in Diabetic Vascular Complications: Can Bilirubin Predict More than Just Liver Disease?
Jun Sung Moon
Diabetes & Metabolism Journal.2015; 39(5): 384. CrossRef
- DECREASE IN SERUM BILIRUBIN AS AN UNFAVORABLE MARKER OF CARDIOVASCULAR DISORDERS
- Predictive Factors for Efficacy of Dipeptidyl Peptidase-4 Inhibitors in Patients with Type 2 Diabetes Mellitus
- Shusuke Yagi, Ken-ichi Aihara, Masashi Akaike, Daiju Fukuda, Hotimah Masdan Salim, Masayoshi Ishida, Tomomi Matsuura, Takayuki Ise, Koji Yamaguchi, Takashi Iwase, Hirotsugu Yamada, Takeshi Soeki, Tetsuzo Wakatsuki, Michio Shimabukuro, Toshio Matsumoto, Masataka Sata
- Diabetes Metab J. 2015;39(4):342-347. Published online July 21, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.4.342
- 3,992 View
- 54 Download
- 18 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Predictive factors for the efficacy of dipeptidyl peptidase-4 (DPP-4) inhibitors for lowering glycosylated hemoglobin (HbA1c) remain unclear in patients with type 2 diabetes mellitus. The aim of this study is therefore to clarify predictive factors of the efficacy of DPP-4 inhibitors for lowering HbA1c after 12 months of treatment.
Methods A total of 191 consecutive type 2 diabetic patients (male sex 55%, mean age, 68.3±35.8 years), who had been treated with DPP-4 inhibitors for 12 months, were enrolled in this study and evaluated retrospectively.
Results After 12 months of DPP-4 inhibitor treatment, random blood glucose level, and HbA1c level, decreased from 167±63 to 151±49 mg/dL (
P <0.01), and from 7.5%±1.3% to 6.9%±0.9% (P <0.01) respectively, without severe side effects. Multiple regression analysis showed that predictors of DPP-4 inhibitor treatment efficacy in lowering HbA1c level after 12 months were a decrease in HbA1c level after 3 months of treatment, a high baseline HbA1c level, a low baseline body mass index, and the absence of coronary artery disease.Conclusion Most suitable candidates for treatment with DPP-4 inhibitors are diabetics who are not obese and do not have coronary artery disease. In addition, long-term efficacy of DPP-4 inhibitors can be predicted by decrement of HbA1c after 3 months of treatment.
-
Citations
Citations to this article as recorded by- Endogenous GLP-1 levels play an important role in determining the efficacy of DPP-IV Inhibitors in both prediabetes and type 2 diabetes
Shiau Chin Chong, Norlela Sukor, Sarah Anne Robert, Kim Fong Ng, Nor Azmi Kamaruddin
Frontiers in Endocrinology.2022;[Epub] CrossRef - Dipeptidyl peptidase‐4 inhibitor, anagliptin, alters hepatic insulin clearance in relation to the glycemic status in Japanese individuals with type 2 diabetes
Takahiro Abe, Yasuhiro Matsubayashi, Sayaka Muragishi, Akihiro Yoshida, Hideki Suganami, Kenichi Furusawa, Kazuya Fujihara, Shiro Tanaka, Kohei Kaku, Hirohito Sone
Journal of Diabetes Investigation.2021; 12(10): 1805. CrossRef - Effects of omarigliptin on glucose variability and oxidative stress in type 2 diabetes patients: A prospective study
Makoto Ohara, Hiroe Nagaike, Tomoki Fujikawa, Yo Kohata, Maiho Ogawa, Takemasa Omachi, Risa Sasajima, Hirotoshi Chiba, Toshimasa Ara, Ayuka Sugawara, Munenori Hiromura, Michishige Terasaki, Yusaku Mori, Tomoyasu Fukui, Tsutomu Hirano, Hiroki Yokoyama, Sho
Diabetes Research and Clinical Practice.2021; 179: 108999. CrossRef - Factors associated with the glucose‐lowering efficacy of sitagliptin in Japanese patients with type 2 diabetes mellitus: Pooled analysis of Japanese clinical trials
Naoko Tajima, Jun‐ichi Eiki, Taro Okamoto, Kotoba Okuyama, Masaru Kawashima, Samuel S Engel
Journal of Diabetes Investigation.2020; 11(3): 640. CrossRef - Efficacy and safety of evogliptin versus sitagliptin as add on to metformin alone in a combined russian-korean population. Evo-combi trial
Alina Y. Babenko, Anna A. Mosikian, Igor E. Makarenko, Victoriya V. Leusheva, Evgeny V. Shlyakhto
Diabetes mellitus.2018; 21(4): 241. CrossRef - Predictors for the Treatment Effect of Sodium Glucose Co-transporter 2 Inhibitors in Patients with Type 2 Diabetes Mellitus
Shusuke Yagi, Ken-ichi Aihara, Takeshi Kondo, Kiyoe Kurahashi, Sumiko Yoshida, Itsuro Endo, Daiju Fukuda, Yutaka Nakaya, Kin-ichiro Suwaki, Takashi Takeji, Toshihiro Wada, Hotimah Masdan Salim, Saori Hama, Tomomi Matsuura, Takayuki Ise, Kenya Kusunose, Ko
Advances in Therapy.2018; 35(1): 124. CrossRef - Ethnic Differences in Efficacy and Safety of Alogliptin: A Systematic Review and Meta-Analysis
Yuli Cai, Tianshu Zeng, Zhongyuan Wen, Lulu Chen
Diabetes Therapy.2018; 9(1): 177. CrossRef - Effectiveness prediction of Evogliptin treatment in type 2 diabetes mellitus in russian-korean population
Anna A. Mosikian, Alina Y. Babenko, Yulia A. Sevastyanova, Roman V. Drai, Evgenij V. Shlyakhto
Diabetes mellitus.2018; 21(5): 333. CrossRef - Efficacy and Safety of Linagliptin in 2681 Asian Patients Stratified by Age, Obesity, and Renal Function: A Pooled Analysis of Randomized Clinical Trials
Guang Ning, Tushar Bandgar, Uwe Hehnke, Jisoo Lee, Juliana C. N. Chan
Advances in Therapy.2017; 34(9): 2150. CrossRef - Potential regulatory mechanisms of lncRNA in diabetes and its complications
Shui-Dong Feng, Ji-Hua Yang, Chao Hua Yao, Si-Si Yang, Ze-Mei Zhu, Di Wu, Hong-Yan Ling, Liang Zhang
Biochemistry and Cell Biology.2017; 95(3): 361. CrossRef - Baseline Body Mass Index and the Efficacy of Hypoglycemic Treatment in Type 2 Diabetes: A Meta-Analysis
Xiaoling Cai, Wenjia Yang, Xueying Gao, Lingli Zhou, Xueyao Han, Linong Ji, Francesco Giorgino
PLOS ONE.2016; 11(12): e0166625. CrossRef - Efficacy of hypoglycemic treatment in type 2 diabetes stratified by age or diagnosed age: a meta-analysis
Xiaoling Cai, Wenjia Yang, Yifei Chen, Xueying Gao, Lingli Zhou, Simin Zhang, Xueyao Han, Linong Ji
Expert Opinion on Pharmacotherapy.2016; 17(12): 1591. CrossRef - Pharmacokinetic, pharmacodynamic and clinical evaluation of saxagliptin in type 2 diabetes
Rose Anderson, Jennifer Hayes, Jeffrey W. Stephens
Expert Opinion on Drug Metabolism & Toxicology.2016; 12(4): 467. CrossRef - Letter: Predictive Factors for Efficacy of Dipeptidyl Peptidase-4 Inhibitors in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2015;39:342-7)
Ye An Kim
Diabetes & Metabolism Journal.2015; 39(5): 444. CrossRef - Response: Predictive Factors for Efficacy of Dipeptidyl Peptidase-4 Inhibitors in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2015;39:342-7)
Shusuke Yagi, Ken-ichi Aihara, Masataka Sata
Diabetes & Metabolism Journal.2015; 39(5): 446. CrossRef
- Endogenous GLP-1 levels play an important role in determining the efficacy of DPP-IV Inhibitors in both prediabetes and type 2 diabetes
- Assessment of the Association between Mean Hemoglobin A1c Levels for 5 Years and Coronary Artery Disease by Coronary Angiography in Nondiabetic Patients
- Jae-Joon Kim, Ji-Hoon Kang, Ja-Jun Goo, Kyoung-Nyoun Kim, Ja-Young Lee, Mi-kyung Kim, Tae Ik Kim
- Diabetes Metab J. 2014;38(1):58-63. Published online February 19, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.1.58
- 3,969 View
- 27 Download
- 4 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The effects of glucose on cardiovascular events or mortality in nondiabetic patients has been recently reported. However, since atherosclerosis can be formed over a long period of time, it is necessary to devote several years to unveil the relationship between the two factors. Here, we attempted to find out the relationship between the mean hemoglobin A1c (HbA1c) level and HbA1c variability for 5 years and coronary artery disease (CAD) by using coronary angiography (CAG) to assess nondiabetic patients.
Methods We reviewed patients who performed CAG who were followed up for at least 5 years after the initial diagnosis. The fasting blood test was performed annually for glucose and HbA1c level. CAD was defined as more than 50% of luminal narrowing. The severity of CAD was divided into two groups depending on whether no vessels were involved or one more vessel were involved (CAD(-) or CAD(+), respectively).
Results The patients in CAD(+) group had higher mean HbA1c level for 5 years than CAD(-) group (5.71±0.40 vs. 5.86±0.68;
P =0.04). Mean HbA1c was a significant predictor for CAD in multiple regression (odds ratio, 2.224;P =0.028). The percentage of patients with CAD was significantly higher in patients with >6.2% of mean HbA1c levels compared to patients with <6.2% of mean HbA1c levels (P <0.019).Conclusion When the mean HbA1c levels were above 6.2%, the risk of CAD was higher. Also this study shows that HbA1c level can be one of the predictors for CAD even if the patients do not have diabetes.
-
Citations
Citations to this article as recorded by- Impact of a comprehensive cardiac rehabilitation programme versus coronary revascularisation in patients with stable angina pectoris: study protocol for the PRO-FIT randomised controlled trial
Joyce M. Heutinck, Iris A. De Koning, Tom Vromen, Robert-Jan M. Van Geuns, Dick H.J. Thijssen, Hareld M.C. Kemps, Eddy M. Adang, Johanna M. Geleijnse, Pieter van Gorp, Arnoud W. J. van ‘t Hof, Veronica R. Janssen, Harald T. Jorstad, Roderik A. Kraaijenhag
BMC Cardiovascular Disorders.2023;[Epub] CrossRef - Evaluation of HbA1c as a prognostic biomarker of cardiovascular events and mortality in nondiabetic patients: Methodological considerations
Denis Monneret
Atherosclerosis.2015; 242(1): 19. CrossRef
- Impact of a comprehensive cardiac rehabilitation programme versus coronary revascularisation in patients with stable angina pectoris: study protocol for the PRO-FIT randomised controlled trial
- Diagnostic Accuracy of 64-Slice MDCT Coronary Angiography for the Assessment of Coronary Artery Disease in Korean Patients with Type 2 Diabetes
- Jun Sung Moon, Ji Sung Yoon, Kyu Chang Won, Ihn-Ho Cho, Hyoung Woo Lee
- Diabetes Metab J. 2013;37(1):54-62. Published online February 15, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.1.54
- 3,661 View
- 29 Download
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background A 64-slice multidetector computed tomography (MDCT) is well known to be a useful noninvasive form of angiography for the general population, but not for certain patients with diabetes. The aim of this study was to investigate the diagnostic accuracy and usefulness of 64-slice MDCT coronary angiography for detecting coronary artery disease in Korean patients with type 2 diabetes mellitus (T2DM).
Methods A total of 240 patients were included, 74 of whom had type 2 diabetes (M:F=40:33; 41.8±9.5 years). We compared significant coronary stenosis (>50% luminal narrowing) in MDCT with invasive coronary angiography (ICA) by segment, artery, and patient. We also evaluated the influence of obesity and coronary calcium score on MDCT accuracy.
Results Of the 4,064 coronary segments studied, 4,062 segments (T2DM=1,109) were assessed quantitatively by both MDCT and ICA, and 706 segments (T2DM=226) were detected as a significant lesion by ICA in all patients. Sensitivity, specificity, as well as positive and negative predictive values for the presence of significant stenosis in T2DM were: by segment, 89.4%, 96.4%, 85.8%, and 97.4%, respectively; by artery (
n =222), 95.1%, 92.9%, 94.4%, and 93.8%, respectively; by patients (n =74), 98.4%, 100.0%, 98.4%, and 90.0%, respectively. Regardless of presence of diabetes, there was no significant difference in diagnostic accuracy. Obesity (≥25 kg/m2) and coronary calcium score did not also affect the diagnostic accuracy of MDCT.Conclusion The 64-slice MDCT coronary angiography was found to have similar diagnostic accuracy with ICA, regardless of diabetes. These results suggest MDCT may be helpful to reduce unnecessary invasive studies for patients with diabetes.
-
Citations
Citations to this article as recorded by- Can Radiation Dose Burden of CT Angiography be Reduced While Still Accurately Diagnosing Etiology of Acute Chest Pain?
Sherine M. Sharara, Scott R. Monnin, Manolo Rubio, Rami N. Khouzam, Samar R. Ragheb
Current Problems in Cardiology.2021; 46(4): 100766. CrossRef - Assessment of high sensitivity C-reactive protein and coronary plaque characteristics by computed tomography in patients with and without diabetes mellitus
Hai-Ting Zhou, De-Li Zhao, Guo-Kun Wang, Tian-Zuo Wang, Hong-Wei Liang, Jin-Ling Zhang
BMC Cardiovascular Disorders.2020;[Epub] CrossRef - Triglyceride Glucose-Waist Circumference Better Predicts Coronary Calcium Progression Compared with Other Indices of Insulin Resistance: A Longitudinal Observational Study
Yun Kyung Cho, Jiwoo Lee, Hwi Seung Kim, Eun Hee Kim, Min Jung Lee, Dong Hyun Yang, Joon-Won Kang, Chang Hee Jung, Joong-Yeol Park, Hong-Kyu Kim, Woo Je Lee
Journal of Clinical Medicine.2020; 10(1): 92. CrossRef - The impact of non-alcoholic fatty liver disease and metabolic syndrome on the progression of coronary artery calcification
Yun Kyung Cho, Yu Mi Kang, Jee Hee Yoo, Jiwoo Lee, Seung Eun Lee, Dong Hyun Yang, Joon-Won Kang, Joong-Yeol Park, Chang Hee Jung, Hong-Kyu Kim, Woo Je Lee
Scientific Reports.2018;[Epub] CrossRef - Effects of Low-density Lipoprotein Cholesterol on Coronary Artery Calcification Progression According to High-density Lipoprotein Cholesterol Levels
Da Young Lee, Ji Hyun Kim, Se Eun Park, Cheol-young Park, Ki-won Oh, Sung-woo Park, Eun-Jung Rhee, Won-young Lee
Archives of Medical Research.2017; 48(3): 284. CrossRef - 2013 ACC/AHA Cholesterol Guideline Versus 2004 NCEP ATP III Guideline in the Prediction of Coronary Artery Calcification Progression in a Korean Population
Yun Kyung Cho, Chang Hee Jung, Yu Mi Kang, Jenie Yoonoo Hwang, Eun Hee Kim, Dong Hyun Yang, Joon‐Won Kang, Joong‐Yeol Park, Hong‐Kyu Kim, Woo Je Lee
Journal of the American Heart Association.2016;[Epub] CrossRef - Imaging Quality Evaluation of Low Tube Voltage Coronary CT Angiography Using Low Concentration Contrast Medium
Chengzhong Zhang, Yuejun Yu, Zaixian Zhang, Qingguo Wang, Linfeng Zheng, Yan Feng, Zhiguo Zhou, Guixiang Zhang, Kangan Li, Zhuoli Zhang
PLOS ONE.2015; 10(3): e0120539. CrossRef - 2013 ACC/AHA versus 2004 NECP ATP III Guidelines in the Assignment of Statin Treatment in a Korean Population with Subclinical Coronary Atherosclerosis
Chang Hee Jung, Min Jung Lee, Yu Mi Kang, Dong Hyun Yang, Joon-Won Kang, Eun Hee Kim, Duk-Woo Park, Joong-Yeol Park, Hong-Kyu Kim, Woo Je Lee, Yingmei Feng
PLOS ONE.2015; 10(9): e0137478. CrossRef - Serum Total Bilirubin Levels Provide Additive Risk Information over the Framingham Risk Score for Identifying Asymptomatic Diabetic Patients at Higher Risk for Coronary Artery Stenosis
Jaechan Leem, Eun Hee Koh, Jung Eun Jang, Chang-Yun Woo, Jin Sun Oh, Min Jung Lee, Joon-Won Kang, Tae-Hwan Lim, Chang Hee Jung, Woo Je Lee, Joong-Yeol Park, Ki-Up Lee
Diabetes & Metabolism Journal.2015; 39(5): 414. CrossRef - Association between serum gamma-glutamyltransferase and the progression of coronary artery calcification
Yun Kyung Cho, Yu Mi Kang, Jenie Yoonoo Hwang, Eun Hee Kim, Dong Hyun Yang, Joon-Won Kang, Joong-Yeol Park, Woo Je Lee, Hong-Kyu Kim, Chang Hee Jung
Atherosclerosis.2015; 243(1): 300. CrossRef - Role of Bilirubin in Diabetic Vascular Complications: Can Bilirubin Predict More than Just Liver Disease?
Jun Sung Moon
Diabetes & Metabolism Journal.2015; 39(5): 384. CrossRef - The Association of Rate of Weight Gain During Early Adulthood With the Prevalence of Subclinical Coronary Artery Disease in Recently Diagnosed Type 2 Diabetes: The MAXWEL-CAD Study
Soo Lim, Sung Hee Choi, Kyoung Min Kim, Sang Il Choi, Eun Ju Chun, Min Joo Kim, Kyong Soo Park, Hak Chul Jang, Naveed Sattar
Diabetes Care.2014; 37(9): 2491. CrossRef - Retraction: Diagnostic Accuracy of 64-Slice MDCT Coronary Angiography for the Assessment of Coronary Artery Disease in Korean Patients with Type 2 Diabetes
Jun Sung Moon, Ji Sung Yoon, Kyu Chang Won, Ihn-Ho Cho, Hyoung Woo Lee
Diabetes & Metabolism Journal.2013; 37(3): 217. CrossRef
- Can Radiation Dose Burden of CT Angiography be Reduced While Still Accurately Diagnosing Etiology of Acute Chest Pain?
- Metabolic Syndrome versus Framingham Risk Score for Association of Self-Reported Coronary Heart Disease: The 2005 Korean Health and Nutrition Examination Survey
- Hye Mi Kang, Dong-Jun Kim
- Diabetes Metab J. 2012;36(3):237-244. Published online June 14, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.3.237
- 3,329 View
- 27 Download
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Several studies in Western populations have indicated that metabolic syndrome (MetS) is inferior to the Framingham risk score (FRS) in predicting coronary heart disease (CHD). However there has been no study about the predictability of MetS vs. FRS for CHD in Korea.
Methods Among the 43,145 persons from the third Korea National Health and Nutrition Examination Survey in 2005, laboratory test and nutritional survey data from 5,271 persons were examined. Participants were also asked to recall a physician's diagnosis of CHD.
Results The median age was 46 (range, 20 to 78) in men (
n =2,257) and 44 (range, 20 to 78) years in women (n =3,014). Prevalence of self-reported CHD was 1.7% in men and 2.1% in women. Receiver operating characteristic curves and their respective area under the curve (AUC) were used to compare the ability of the FRS and the number of components of MetS to predict self-reported CHD in each sex. In men, AUC of FRS was significantly larger than that of MetS (0.767 [0.708 to 0.819] vs. 0.677 [0.541 to 0.713],P <0.01). In women, AUC of FRS was comparable to that of MetS (0.777 [0.728 to 0.826] vs. 0.733 [0.673 to 0.795]), and was not significant.Conclusion The data suggested that FRS was more closely associated with CHD compared to MetS in Korean men.
-
Citations
Citations to this article as recorded by- Intakes of Milk and Soymilk and Cardiovascular Disease Risk in Korean Adults: A Study Based on the 2012~2016 Korea National Health and Nutrition Examination Survey
Ae Wha Ha, Woo Kyoung Kim, Sun Hyo Kim
Journal of the Korean Society of Food Science and Nutrition.2023; 52(5): 522. CrossRef - Cow’s Milk Intake and Risk of Coronary Heart Disease in Korean Postmenopausal Women
Ae-Wha Ha, Woo-Kyoung Kim, Sun-Hyo Kim
Nutrients.2022; 14(5): 1092. CrossRef - Prognostic Modelling Studies of Coronary Heart Disease—A Systematic Review of Conventional and Genetic Risk Factor Studies
Nayla Nasr, Beáta Soltész, János Sándor, Róza Adány, Szilvia Fiatal
Journal of Cardiovascular Development and Disease.2022; 9(9): 295. CrossRef - Framingham Risk Score Assessment in Subjects with Pre-diabetes and Diabetes: A Cross-Sectional Study in Korea
Hyuk Sang Kwon, Kee Ho Song, Jae Myung Yu, Dong Sun Kim, Ho Sang Shon, Kyu Jeung Ahn, Sung Hee Choi, Seung Hyun Ko, Won Kim, Kyoung Hwa Lee, Il Seong Nam-Goong, Tae Sun Park
Journal of Obesity & Metabolic Syndrome.2021; 30(3): 261. CrossRef - Cardiometabolic risk prediction algorithms for young people with psychosis: a systematic review and exploratory analysis
B. I. Perry, R. Upthegrove, O. Crawford, S. Jang, E. Lau, I. McGill, E. Carver, P. B. Jones, G. M. Khandaker
Acta Psychiatrica Scandinavica.2020; 142(3): 215. CrossRef - Metabolic Syndrome and Mortality in Continuous Ambulatory Peritoneal Dialysis Patients: A 5-Year Prospective Cohort Study
WenLong Gu, Chunyan Yi, Xueqing Yu, Xiao Yang
Kidney and Blood Pressure Research.2019; 44(5): 1026. CrossRef - Comparison Between Metabolic Syndrome and the Framingham Risk Score as Predictors of Cardiovascular Diseases Among Kazakhs in Xinjiang
Wenwen Yang, Rulin Ma, Xianghui Zhang, Heng Guo, Jia He, Lei Mao, Lati Mu, Yunhua Hu, Yizhong Yan, Jiaming Liu, Jiaolong Ma, Shugang Li, Yusong Ding, Mei Zhang, Jingyu Zhang, Shuxia Guo
Scientific Reports.2018;[Epub] CrossRef - Prediction of Coronary Heart Disease Risk in Korean Patients with Diabetes Mellitus
Bo Kyung Koo, Sohee Oh, Yoon Ji Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2018; 7(2): 110. CrossRef - Epidemiology and cardiovascular comorbidities in patients with psoriasis: A Korean nationwide population‐based cohort study
Eui Hyun Oh, Young Suck Ro, Jeong Eun Kim
The Journal of Dermatology.2017; 44(6): 621. CrossRef - Pattern of Thyroid Dysfunction in Patients with Metabolic Syndrome and Its Relationship with Components of Metabolic Syndrome
Prabin Gyawali, Jyoti Shrestha Takanche, Raj Kumar Shrestha, Prem Bhattarai, Kishor Khanal, Prabodh Risal, Rajendra Koju
Diabetes & Metabolism Journal.2015; 39(1): 66. CrossRef - The Effects of Menopause on the Metabolic Syndrome in Korean Women
SoYoun Bang, IlGu Cho
Journal of the Korea Academia-Industrial cooperation Society.2015; 16(4): 2704. CrossRef - Evaluation of Nutrient Intake and Food Variety in Korean Male Adults according to Framingham Risk Score
Mi-Kyeong Choi, Yun-Jung Bae
The Korean Journal of Food And Nutrition.2014; 27(3): 484. CrossRef - Cardiometabolic implication of sarcopenia: The Korea National Health and Nutrition Examination Study (KNHANES) 2008–2010
Kyoung Min Kim, Soo Lim, Sung Hee Choi, Jung Hee Kim, Chan Soo Shin, Kyong Soo Park, Hak Chul Jang
IJC Metabolic & Endocrine.2014; 4: 63. CrossRef - Different tools for estimating cardiovascular risk in Brazilian postmenopausal women
Eliana A. P. Nahas, Aline M. Andrade, Mayra C. Jorge, Claudio L. Orsatti, Flavia B. Dias, Jorge Nahas-Neto
Gynecological Endocrinology.2013; 29(10): 921. CrossRef - Hemoglobin A1c Is Positively Correlated with Framingham Risk Score in Older, Apparently Healthy Nondiabetic Korean Adults
Ji Hye Shin, Ji In Kang, Yun Jung, Young Min Choi, Hyun Jung Park, Jung Hae So, Jin Hwa Kim, Sang Yong Kim, Hak Yeon Bae
Endocrinology and Metabolism.2013; 28(2): 103. CrossRef - Cardiovascular Disease Risk of Bus Drivers in a City of Korea
Seung Shin, Chul Lee, Han Song, Sul Kim, Hyun Lee, Min Jung, Sang Yoo
Annals of Occupational and Environmental Medicine.2013; 25(1): 34. CrossRef
- Intakes of Milk and Soymilk and Cardiovascular Disease Risk in Korean Adults: A Study Based on the 2012~2016 Korea National Health and Nutrition Examination Survey
- Relationship between Chemerin Levels and Cardiometabolic Parameters and Degree of Coronary Stenosis in Korean Patients with Coronary Artery Disease
- Yu-Jin Hah, Nam-Keong Kim, Mi-Kyung Kim, Hye-Soon Kim, Seung-Ho Hur, Hyuck-Jun Yoon, Yoon-Nyun Kim, Keun-Gyu Park
- Diabetes Metab J. 2011;35(3):248-254. Published online June 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.3.248
- 24,768 View
- 30 Download
- 40 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Chemerin is a novel adipokine that is associated with inflammation and adipogenesis. However, it remains unclear whether chemerin is involved in patients with cardiovascular disease. We investigated whether the serum chemerin levels of Korean patients with coronary artery disease correlated with specific cardiometabolic parameters.
Methods In total, 131 patients, all of whom had coronary artery stenosis exceeding 50%, participated in this study. Their serum chemerin levels and cardiometabolic parameters were measured. The serum chemerin levels of two groups of patients were compared; those with one stenotic vessel (
n =68) and those with multiple stenotic vessels, including left main coronary artery disease (n =63).Results Serum chemerin levels correlated positively with the degree of coronary artery stenosis and fasting glucose, triglyceride, total cholesterol, low density lipoprotein cholesterol, and high sensitive C-reactive protein levels. The group with multiple stenotic vessels, including left main disease, had higher chemerin levels than the group with one stenotic vessel (
t =-2.129,P =0.035). Multiple binary logistic regression showed chemerin was not an independent risk factor of multiple vessel disease (odds ratio, 1.018; confidence interval, 0.997 to 1.040;P =0.091).Conclusion Serum chemerin levels have a significant correlation with several cardiometabolic risk factors and the degree of coronary artery stenosis in Korean patients with coronary artery disease. However, multiple binary logistic regression showed chemerin was not an independent risk factor of multiple vessel disease. Additional investigations are necessary to fully elucidate the role of chemerin in cardiovascular disease.
-
Citations
Citations to this article as recorded by- Adipokine chemerin overexpression in trophoblasts leads to dyslipidemia in pregnant mice: implications for preeclampsia
Lunbo Tan, Zijun Ouyang, Zhilong Chen, Fen Sun, Haichun Guo, Feng Wang, Monique Mulder, Yuan Sun, Xifeng Lu, Jian V. Zhang, A. H. Jan Danser, Koen Verdonk, Xiujun Fan, Qing Yang
Lipids in Health and Disease.2023;[Epub] CrossRef - Chemerin Levels in Acute Coronary Syndrome: Systematic Review and Meta-Analysis
Abdulrahman Ismaiel, Mohammad Zeeshan Ashfaq, Daniel-Corneliu Leucuta, Mohamed Ismaiel, Dilara Ensar Ismaiel, Stefan-Lucian Popa, Dan L Dumitrascu
Laboratory Medicine.2022; 53(6): 552. CrossRef - Prognostic value of plasma adipokine chemerin in patients with coronary artery disease
Bo Wang, Wenxin Kou, Shuya Ji, Rongrong Shen, Hongwei Ji, Jianhui Zhuang, Yifan Zhao, Bo Li, Wenhui Peng, Xuejing Yu, Hailing Li, Yawei Xu
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Role of Chemerin in Cardiovascular Diseases
Mirjana T. Macvanin, Manfredi Rizzo, Jelena Radovanovic, Alper Sonmez, Francesco Paneni, Esma R. Isenovic
Biomedicines.2022; 10(11): 2970. CrossRef - Chemerin in inflammatory diseases
Xin Su, Ye Cheng, Guoming Zhang, Bin Wang
Clinica Chimica Acta.2021; 517: 41. CrossRef - Chemerin activity in selected pathological states of human body – A systematic review
Magdalena Acewicz, Irena Kasacka
Advances in Medical Sciences.2021; 66(2): 270. CrossRef - Chemerin in atherosclerosis
Jia-Xiang Sun, Chi Zhang, Zhe-Bin Cheng, Mu-Yao Tang, Yi-Zhang Liu, Jie-Feng Jiang, Xuan Xiao, Liang Huang
Clinica Chimica Acta.2021; 520: 8. CrossRef - Serum Chemerin Concentration Is Associated with Proinflammatory Status in Chronic Coronary Syndrome
Anna Szpakowicz, Malgorzata Szpakowicz, Magda Lapinska, Marlena Paniczko, Slawomir Lawicki, Andrzej Raczkowski, Marcin Kondraciuk, Emilia Sawicka, Malgorzata Chlabicz, Marcin Kozuch, Maciej Poludniewski, Slawomir Dobrzycki, Irina Kowalska, Karol Kaminski
Biomolecules.2021; 11(8): 1149. CrossRef - Novo Efeito Cardioprotetor da L-Carnitina em Camundongos Obesos Diabéticos: Regulação da Expressão de Quemerina e CMKLRI no Coração e Tecidos Adiposos
Rezvan Amiri, Mohammad Reza Tabandeh, Seyed Ahmad Hosseini
Arquivos Brasileiros de Cardiologia.2021; 117(4): 715. CrossRef - The role of adipokines in the regulation of cardiovascular function
A. V. Karpushev, V. B. Mikhailova
"Arterial’naya Gipertenziya" ("Arterial Hypertension").2020; 25(5): 448. CrossRef - The associations among RARRES2 rs17173608 gene polymorphism, serum chemerin, and non-traditional lipid profile in patients with metabolic syndrome
Marwa A. Dahpy, Marwa K. Khairallah, Nashwa Mostafa A. Azoz, Ghada M. Ezzat
Egyptian Journal of Medical Human Genetics.2020;[Epub] CrossRef - Serum chemerin as a predictor of left ventricle hypertrophy in patients with coronary artery disease
NohaHasssanin Hanboly, Yasser Sharaf, Mervat Al-Anany, Essam Saeed
Nigerian Journal of Cardiology.2019; 16(1): 25. CrossRef - Association of Circulating Chemerin With Subclinical Parameters of Atherosclerosis
Stephanie Zylla, Marcus Dörr, Henry Völzke, Ulf Schminke, Stephan B. Felix, Matthias Nauck, Nele Friedrich
Arteriosclerosis, Thrombosis, and Vascular Biology.2018; 38(7): 1656. CrossRef - Six weeks of combined aerobic and resistance exercise using outdoor exercise machines improves fitness, insulin resistance, and chemerin in the Korean elderly: A pilot randomized controlled trial
Dong-Il Kim, Dong Hoon Lee, Sunghyun Hong, Sung-won Jo, Young-shin Won, Justin Y. Jeon
Archives of Gerontology and Geriatrics.2018; 75: 59. CrossRef - Relationship between serum chemerin levels and insulin resistance index and cardio–respiratory function in non–active obese and lean men
Mehdi Abbaszadegan, Farhad Kouhi achachluie
Advances in Obesity, Weight Management & Control.2018;[Epub] CrossRef - Serum levels of chemerin, apelin, vaspin, and omentin-1 in obese type 2 diabetic Egyptian patients with coronary artery stenosis
Tarek M.K. Motawi, Soliman G. Mahdy, Maha M. El-Sawalhi, Eman N. Ali, Rania Farag A. El-Telbany
Canadian Journal of Physiology and Pharmacology.2018; 96(1): 38. CrossRef - Plasma CXCL1 levels and TRAF3IP2 variants in patients with myocardial infarction
Safoora Pordel, Mahdi Sajedi Khanian, Mohammad Hossein Karimi, Hossein Nikoo, Mehrnoosh Doroudchi
Journal of Clinical Laboratory Analysis.2018;[Epub] CrossRef - Serum Chemerin Levels are Associated with Visceral Adiposity, Independent of Waist Circumference, in Newly Diagnosed Type 2 Diabetic Subjects
Dae Young Cheon, Jun Goo Kang, Seong Jin Lee, Sung Hee Ihm, Eun Jig Lee, Moon Gi Choi, Hyung Joon Yoo, Chul Sik Kim
Yonsei Medical Journal.2017; 58(2): 319. CrossRef - The comparison of chemerin, adiponectin and lipid profile indices in obese and non-obese adolescents
Zahra Maghsoudi, Roya Kelishadi, Mohammad Javad Hosseinzadeh-Attar
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2016; 10(2): S43. CrossRef - Chemerin processing in the myocardium: A mechanism in search of a function
Michael V.G. Latronico, Gianluigi Condorelli
Journal of Molecular and Cellular Cardiology.2016; 100: 21. CrossRef - Chemerin as an independent predictor of cardiovascular event risk
Sinan İnci, Gökhan Aksan, Pınar Doğan
Therapeutic Advances in Endocrinology and Metabolism.2016; 7(2): 57. CrossRef - Chemerin level in pregnancies complicated by preeclampsia and its relation with disease severity and neonatal outcomes
Orkun Cetin, Zehra Kurdoglu, Mertihan Kurdoglu, H. Guler Sahin
Journal of Obstetrics and Gynaecology.2016; : 1. CrossRef - Chemerin in renal dysfunction and cardiovascular disease
Mario Bonomini, Assunta Pandolfi
Vascular Pharmacology.2016; 77: 28. CrossRef - High plasma chemerin is associated with renal dysfunction and predictive for cardiovascular events — Insights from phenotype and genotype characterization
Andreas Leiherer, Axel Muendlein, Elena Kinz, Alexander Vonbank, Philipp Rein, Peter Fraunberger, Cornelia Malin, Christoph H. Saely, Heinz Drexel
Vascular Pharmacology.2016; 77: 60. CrossRef - Chemerin plays a protective role by regulating human umbilical vein endothelial cell-induced nitric oxide signaling in preeclampsia
Liqiong Wang, Tianli Yang, Yiling Ding, Yan Zhong, Ling Yu, Mei Peng
Endocrine.2015; 48(1): 299. CrossRef - Evaluation of the salivary levels of visfatin, chemerin, and progranulin in periodontal inflammation
Erkan Özcan, N. Işıl Saygun, Muhittin A. Serdar, Nezahat Kurt
Clinical Oral Investigations.2015; 19(4): 921. CrossRef - Elevated serum chemerin in Chinese women with hyperandrogenic PCOS
LiQiong Wang, Yan Zhong, YiLing Ding, XiaoBo Shi, Jian Huang, FuFan Zhu
Gynecological Endocrinology.2014; 30(10): 746. CrossRef - Chemerin reduces vascular nitric oxide/cGMP signalling in rat aorta: a link to vascular dysfunction in obesity?
Karla Bianca Neves, Núbia S. Lobato, Rhéure Alves Moreira Lopes, Fernando P. Filgueira, Camila Ziliotto Zanotto, Ana Maria Oliveira, Rita C. Tostes
Clinical Science.2014; 127(2): 111. CrossRef - Chemerin levels as predictor of acute coronary events: A case–control study nested within the veterans affairs normative aging study
Konstantinos N. Aronis, Ayse Sahin-Efe, John P. Chamberland, Avron Spiro, Pantel Vokonas, Christos S. Mantzoros
Metabolism.2014; 63(6): 760. CrossRef - The predictive value of the first-trimester maternal serum chemerin level for pre-eclampsia
Qiu-Lian Xu, Min Zhu, Yan Jin, Nan Wang, Hai-Xia Xu, Li-Mei Quan, Shan-Shan Wang, Shan-Shan Li
Peptides.2014; 62: 150. CrossRef - Evaluation of Circulating Adipokines and Abdominal Obesity as Predictors of Significant Myocardial Ischemia Using Gated Single-Photon Emission Computed Tomography
Chi-Sheng Hung, Yen-Wen Wu, Jei-Yie Huang, Pei-Ying Hsu, Ming-Fong Chen, Xin-Liang Ma
PLoS ONE.2014; 9(5): e97710. CrossRef - Towards an integrative approach to understanding the role of chemerin in human health and disease
J. L. Rourke, H. J. Dranse, C. J. Sinal
Obesity Reviews.2013; 14(3): 245. CrossRef - The association between chemerin and homeostasis assessment of insulin resistance at baseline and after weight reduction via lifestyle modifications in young obese adults
Mi Kyung Lee, Sang Hui Chu, Duk Chul Lee, Ki Yong An, Ji-Hye Park, Dong Il Kim, Jiyoung Kim, Sunghyun Hong, Jee Aee Im, Ji Won Lee, Justin Y. Jeon
Clinica Chimica Acta.2013; 421: 109. CrossRef - Elevated Chemerin Levels in Pakistani Men: An Interrelation with Metabolic Syndrome Phenotypes
Syeda Sadia Fatima, Kiymet Bozaoglu, Rehana Rehman, Faiza Alam, Abdul Shakoor Memon, Pascale Chavatte-Palmer
PLoS ONE.2013; 8(2): e57113. CrossRef - Chemerin: a potential endocrine link between obesity and type 2 diabetes
Alexandra A. Roman, Sebastian D. Parlee, Christopher J. Sinal
Endocrine.2012; 42(2): 243. CrossRef - Elastase and Tryptase Govern TNFα-Mediated Production of Active Chemerin by Adipocytes
Sebastian D. Parlee, Jenna O. McNeil, Shanmugam Muruganandan, Christopher J. Sinal, Kerry B. Goralski, Charaf Benarafa
PLoS ONE.2012; 7(12): e51072. CrossRef - Potential association between coronary artery disease and the inflammatory biomarker YKL-40 in asymptomatic patients with type 2 diabetes mellitus
Hyun Min Kim, Byung-Wan Lee, Young-Mi Song, Won Jin Kim, Hyuk-Jae Chang, Dong-Hoon Choi, Hee Tae Yu, EunSeok Kang, Bong Soo Cha, Hyun Chul Lee
Cardiovascular Diabetology.2012;[Epub] CrossRef - The association of serum chemerin level with risk of coronary artery disease in Chinese adults
Qun Yan, Yifei Zhang, Jie Hong, Weiqiong Gu, Meng Dai, Juan Shi, Ying Zhai, Weiqing Wang, Xiaoying Li, Guang Ning
Endocrine.2012; 41(2): 281. CrossRef - Epidemiology of Micro- and Macrovascular Complications of Type 2 Diabetes in Korea
Jung Hee Kim, Dae Jung Kim, Hak Chul Jang, Sung Hee Choi
Diabetes & Metabolism Journal.2011; 35(6): 571. CrossRef - Chemerin: A Novel Link between Inflammation and Atherosclerosis?
Eun-Jung Rhee
Diabetes & Metabolism Journal.2011; 35(3): 216. CrossRef
- Adipokine chemerin overexpression in trophoblasts leads to dyslipidemia in pregnant mice: implications for preeclampsia
- Lack of Association between Serum Cystatin C Levels and Coronary Artery Disease in Diabetic Patients
- Eun Hee Kim, Ji Hee Yu, Sang Ah Lee, Eui Young Kim, Won Gu Kim, Seung Hun Lee, Eun Hee Cho, Eun Hee Koh, Woo Je Lee, Min-Seon Kim, Joong-Yeol Park, Ki-Up Lee
- Korean Diabetes J. 2010;34(2):95-100. Published online April 30, 2010
- DOI: https://doi.org/10.4093/kdj.2010.34.2.95
- 4,413 View
- 31 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Serum cystatin C level is a more sensitive marker of renal dysfunction than serum creatinine level. Serum cystatin C level was recently reported to predict the development of cardiovascular disease. This study was performed to evaluate whether the cystatin C level is associated with coronary artery disease (CAD), independent of diabetic nephropathy.
Methods We conducted a case-control study to assess the relationship between serum cystatin C level and coronary artery disease in diabetic patients. Among 460 diabetic patients, 38 diabetic patients had CAD. The control group consisted of 38 diabetic patients who were matched to cases by age, sex, and presence/absence of diabetic nephropathy. Serum cystatin C level was measured in stored samples.
Results Serum cystatin C level was significantly higher in patients with diabetic nephropathy, both in CAD and non-CAD patients. However, serum cystatin C level did not differ between CAD and non-CAD patients, regardless of diabetic nephropathy.
Conclusion Serum cystatin C level is a marker of renal dysfunction, but not coronary artery disease, in diabetic patients.
-
Citations
Citations to this article as recorded by- Higher Levels of Cystatin C in HIV/AIDS Patients with Metabolic Syndrome
Gordana Dragović, Danica Srdić, Khawla Al Musalhi, Ivan Soldatović, Jovana Kušić, Djordje Jevtović, Devaki Nair
Basic & Clinical Pharmacology & Toxicology.2018; 122(4): 396. CrossRef - The association between serum cystatin C and carotid intima–media thickness in metabolic syndrome patients with normal estimated glomerular filtration rate
Rong Huang, Jingli Gu, Qin Cao, Jiahua Ma, Weiwei Gu, Zhuping Fan
Clinica Chimica Acta.2015; 448: 170. CrossRef - Association of plasma cystatin C levels with angiographically documented coronary artery disease in patients of Indian origin
Aditya Batra, Aditya Kapoor, R.K. Sharma, Nitin Agrawal, Archana Sinha, Sudeep Kumar, Naveen Garg, Satyendra Tewari, Pravin K. Goel
Journal of Cardiology.2012; 59(2): 182. CrossRef - Cystatin C and asymptomatic coronary artery disease in patients with metabolic syndrome and normal glomerular filtration rate
Xie Qing, Wang Furong, Liu Yunxia, Zhang Jian, Wang Xuping, Gao Ling
Cardiovascular Diabetology.2012;[Epub] CrossRef - Response: Lack of Association between Serum Cystatin C Levels and Coronary Artery Disease in Diabetic Patients (Korean Diabetes J 2010;34:95-100)
Eun Hee Kim, Ki-Up Lee
Korean Diabetes Journal.2010; 34(3): 209. CrossRef - Serum Cystatin C as a Biomarker for Predicting Coronary Artery Disease in Diabetes
Jee-Young Oh
Korean Diabetes Journal.2010; 34(2): 84. CrossRef - Letter: Lack of Association between Serum Cystatin C Levels and Coronary Artery Disease in Diabetic Patients (Korean Diabetes J 2010;34:95-100)
Kyu-Chang Won
Korean Diabetes Journal.2010; 34(3): 207. CrossRef
- Higher Levels of Cystatin C in HIV/AIDS Patients with Metabolic Syndrome
- The Association Between Urinary Albumin to Creatinine Ratio and Coronary Artery Calcification in Type 2 Diabetic Patients.
- Ju Young Lee, Yeon Kyung Choi, Hyun Ae Seo, Jae Han Jeon, Jung Eun Lee, Seong Su Moon, Jung Guk Kim, Bo Wan Kim, In Kyu Lee
- Korean Diabetes J. 2009;33(4):289-298. Published online August 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.4.289
- 2,182 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Atherosclerosis, the most common cause of death in type 2 diabetic patients, is closely associated with coronary artery calcium deposition. The coronary calcifications can be easily measured using coronary calcium scoring computed tomography (CT). And microalbuminuria is known as an independent risk factor of cardiovascular disease. So, we examined the association of urinary albumin to creatinine ratio (UACR) and coronary calcification score (CCS) in type 2 diabetic patients. METHODS: Among type 2 diabetic patients who underwent the multidetector CT scanning for the evaluation of CCS at Kyungpook National University Hospital between December 2007 and May 2008, 155 subjects were included. CCS, demographic and laboratory data were assessed. RESULTS: Coronary artery calcifications were identified in 90 patients (51%) and mean, median CCS was 205.8 +/- 476.9, 8.74 (0, 132.0). 60 subjects revealed UACR greater than 30 ug/mg. With the UACR increment, CCS revealed a significant increase (P < 0.001). Age, duration of diabetes, serum Apo A1 level, serum high sensitivity C-reactive protein (hs-CRP) level were also associated with CCS. However, after adjusting for age, UACR and CCS exhibited a significant positive relationship (P = 0.002). CONCLUSION: Increased UACR is associated with coronary artery calcification in type 2 diabetic patients and these results will be useful in early evaluating the presence of macrovascular complications in these patients.
- The Relationship between Serum Retinol-Binding Protein 4 Levels and Coronary Artery Disease in Korean Adults.
- Ji Hoon Kim, Eun Jung Rhee, Eun Suk Choi, Jong Chul Won, Cheol Young Park, Won Young Lee, Ki Won Oh, Byung Jin Kim, Ki Chul Sung, Bum Soo Kim, Jin Ho Kang, Sung Woo Park, Sun Woo Kim, Man Ho Lee, Jung Roe Park
- Korean Diabetes J. 2009;33(2):105-112. Published online April 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.2.105
- 7,735 View
- 16 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
A recently discovered adipokine, retinol-binding protein-4 (RBP-4), is reportedly associated with insulin resistance and metabolic syndrome. This study was performed to analyze the relationship between serum RBP-4 levels and coronary artery disease (CAD) in Korean adults. METHODS: In 235 subjects (mean age 58 years) in whom coronary artery angiograms were performed due to complaints of chest pain, serum RBP-4 levels were measured by enzyme-linked immunosorbent assay. Coronary artery angiograms were performed in all subjects and the severity of CAD was assessed by the number of stenotic vessels. The presence of metabolic syndrome was defined by AHA/NHLBI criteria with body mass index substituted for waist circumference. RESULTS: Coronary angiogram showed that 101 subjects (43%) had normal coronary vessel, 82 subjects (34.9%) had 1-vessel disease, 31 subjects (13.2%) had 2-vessel disease and 21 subjects (8.9%) had 3-vessel disease. Subjects with coronary artery stenosis showed a higher mean age (60.5 +/- 10.0 years), fasting glucose (123.3 mg +/- 45.0 mg/dL) and lower mean value for high-density lipoprotein cholesterol (HDL-C) level (49.0 +/- 13.2 mg/dL), although serum RBP-4 levels were not significantly different between those with and without CAD. Mean age and fasting glucose level increased significantly as the number of stenotic vessels increased, although serum RBP4 level showed no significant differences among the different groups. Among the metabolic parameters, only serum triglyceride levels showed a significant correlation with serum RBP-4 levels. CONCLUSION: There was no difference in mean serum RBP-4 levels between subjects with or without coronary artery disease in Korean adults. Further studies are warranted to draw a clear conclusion on the effect of RBP-4 on atherosclerosis. -
Citations
Citations to this article as recorded by- Retinol binding protein 4 levels relate to the presence and severity of coronary artery disease
Gokay Nar, Sara Sanlialp, Rukiye Nar
Journal of Medical Biochemistry.2021; 40(4): 384. CrossRef
- Retinol binding protein 4 levels relate to the presence and severity of coronary artery disease
- Insulin Resistance and severity of coronary artery diseases in Patients with Coronary Artery Diseases.
- Dae Jung Kim, Jae Hyun Nam, Dong Hoon Choi, Hyeung Jin Kim, Soo Kyung Kim, Se Hwa Kim, Yumie Rhee, Chul Woo Ahn, Bong Soo Cha, Young Duk Song, Sung Kil Lim, Kyeong Rae Kim, Hyun Chul Lee, Kap Bum Huh
- Korean Diabetes J. 2002;26(3):189-198. Published online June 1, 2002
- 1,188 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Insulin resistance (IR) has been identified as a risk factor of atherosclerosis, which may be induced through a mechanism brought about by hypertension, obesity, glucose intolerance and dyslipidemia. The purpose of this study was to investigate the relationship between coronary artery disease (CAD) and insulin resistance. METHODS: Of 92 subjects having undergone coronary angiography 70 with significantly stenotic coronary artery were designated as the CAD group, with the other 22, without stenosis, as the control group. The CAD group was subdivided into 3 smaller groups according to the severity of their CAD; these being 1-vessel disease (group 1, n=31), 2-vessel disease (group 2, n=25), and 3-vessel disease (group 3, n=14). RESULTS: Kitt for patients with CAD was significantly lower than in the control group, and also for those in group 1 compared to groups 2 and 3, 2.72+/-1.29, 2.25+/-0.68 and 2.21+/-0.78%/min, with that of the controls being 3.01+/-1.22%/min p<0.05). There were significant differences between the IR group and the non-IR group in the common carotid artery intima-media thickness (1.09mm vs. 0.87mm, p<0.05), the waist-hip ratio (1.09 vs. 0.93, p<0.05) and the body fat contents (32% vs. 27%, p<0.05).Insulin resistance was assessed by the short insulin tolerance test, and the insulin resistance (IR) group was defined as having a Kitt less than 2.5%/min. CONCLUSION: These results suggest that insulin resistance is an important risk factor for CAD, and is related to the severity of coronary atherosclerosis.
- Clinical and Coronary Angiographic Findings of Coronary Artery Disease in Patients with Noninsulin Dependent Diabetes Mellitus.
- Bon Jeong Ku, Bong Soo An, Jin Ok Jeong, In Whan Seong, Eun Seok Jeon, Min Ho Shong, Heung Kyu Ro, Young Kun Kim
- Korean Diabetes J. 1997;21(3):308-313. Published online January 1, 2001
- 885 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Diabetes mellitus has a major impact on cardiac morbidity and mortality. We analyzed the clinical characteristics and coronary angiographic findings in patients with a coronary artery disease and with noninsulin dependent diabetes mellitus. METHODS: We retrospectively reviewed the clinical and coronary angiographic findings in 74 patients with noninsulin dependent cliabetes mellitus and in 328 non-diabetic patients who had a coronary insufficiency. RESULTS: Significant coronary occlusions and multiple coronary artery diseases were more common in diabetics than in non-diabetics. The patients with noninsulin dependent diabetes mellitus has several limiting factors to perform the successful percutaneous coronary angioplasty, it could be a possible factor for rapid deterioration of coronary insufficiency in patients with diabetes mellitus. Smoking and hypertension significantly increased the incidence of signiftcant coronary occlusions whereas obesity and hypercholesterolemia did not any significant influence on incidence of the significant coronary occlusions. The longer duration of diabetes rnellitus associated with higher incidence of significant coronary occlusions and multiple coronary diseases. CONCLUSION: Significant coronary occlusions and multiple coronary artery diseases were occurred more common in diabetics than in non-diabetics. Coronary angiography should be performed routinely in noninsulin dependent diabetes.

 KDA
KDA
 First
First Prev
Prev





