
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 42(6); 2018 > Article
-
Original ArticleEpidemiology Association of Thigh Muscle Mass with Insulin Resistance and Incident Type 2 Diabetes Mellitus in Japanese Americans
-
Seung Jin Han1,2
 , Edward J. Boyko2,3, Soo-Kyung Kim4, Wilfred Y. Fujimoto3, Steven E. Kahn3,5, Donna L. Leonetti6
, Edward J. Boyko2,3, Soo-Kyung Kim4, Wilfred Y. Fujimoto3, Steven E. Kahn3,5, Donna L. Leonetti6 -
Diabetes & Metabolism Journal 2018;42(6):488-495.
DOI: https://doi.org/10.4093/dmj.2018.0022
Published online: September 5, 2018
1Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea.
2Seattle Epidemiologic Research and Information Center, VA Puget Sound Health Care System, Seattle, WA, USA.
3Department of Medicine, University of Washington School of Medicine, Seattle, WA, USA.
4Department of Internal Medicine, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam, Korea.
5Hospital and Specialty Medicine Service, VA Puget Sound Health Care System, Seattle, WA, USA.
6Department of Anthropology, University of Washington, Seattle, WA, USA.
- Corresponding author: Seung Jin Han. Department of Endocrinology and Metabolism, Ajou University School of Medicine, 164 World cup-ro, Yeongtong-gu, Suwon 16499, Korea. hsj@ajou.ac.kr
Copyright © 2018 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations

- Shape phenotype of thigh fat and muscle and risk of major adverse cardiovascular events after fragility hip fracture
Sheen‐Woo Lee, Seung‐Chan Kim, Jeong‐Eun Yi
Journal of Cachexia, Sarcopenia and Muscle.2024; 15(1): 331. CrossRef - CD36 gene variant rs1761667(G/A) as a biomarker in obese type 2 diabetes mellitus cases
Ashwin Kumar Shukla, Amreen Shamsad, Atar Singh Kushwah, Shalini Singh, Kauser Usman, Monisha Banerjee
Egyptian Journal of Medical Human Genetics.2024;[Epub] CrossRef - Association between macro- and microvascular damage and sarcopenia index in individuals with type 2 diabetes mellitus
Hui Xu, Qun-Yan Xiang, Jun-Kun Zhan, Yi Wang, Yan-Jiao Wang, Shuang Li, You-Shuo Liu
Applied Physiology, Nutrition, and Metabolism.2024;[Epub] CrossRef - More appendicular lean mass relative to body mass index is associated with lower incident diabetes in middle-aged adults in the CARDIA study
Melanie S. Haines, Aaron Leong, Bianca C. Porneala, Victor W. Zhong, Cora E. Lewis, Pamela J. Schreiner, Karen K. Miller, James B. Meigs, Mercedes R. Carnethon
Nutrition, Metabolism and Cardiovascular Diseases.2023; 33(1): 105. CrossRef - Involvement of the fecal amino acid profile in a clinical and anthropometric study of Mexican patients with insulin resistance and type 2 diabetes mellitus
Mayra Paloma Macías-Acosta, Lorena Valerdi-Contreras, Ericka Denise Bustos-Angel, Rudy Antonio García-Reyes, Monserrat Alvarez-Zavala, Marisela González-Ávila
Amino Acids.2022; 54(1): 47. CrossRef - Association of serum creatinine levels and risk of type 2 diabetes mellitus in Korea: a case control study
Do Kyeong Song, Young Sun Hong, Yeon-Ah Sung, Hyejin Lee
BMC Endocrine Disorders.2022;[Epub] CrossRef - The Relationship Between Fat-Free Mass and Glucose Metabolism in Children and Adolescents: A Systematic Review and Meta-Analysis
Lijun Wu, Fangfang Chen, Junting Liu, Dongqing Hou, Tao Li, Yiren Chen, Zijun Liao
Frontiers in Pediatrics.2022;[Epub] CrossRef - Is imaging-based muscle quantity associated with risk of diabetes? A meta-analysis of cohort studies
Shanhu Qiu, Xue Cai, Yang Yuan, Bo Xie, Zilin Sun, Tongzhi Wu
Diabetes Research and Clinical Practice.2022; 189: 109939. CrossRef - Effects of Exercise Intervention on Type 2 Diabetes Patients With Abdominal Obesity and Low Thigh Circumference (EXTEND): Study Protocol for a Randomized Controlled Trial
Dan Liu, Ying Zhang, Liang Wu, Jingyi Guo, Xiangtian Yu, Huasheng Yao, Rui Han, Tianshu Ma, Yuchan Zheng, Qiongmei Gao, Qichen Fang, Yan Zhao, Yanan Zhao, Biao Sun, Weiping Jia, Huating Li
Frontiers in Endocrinology.2022;[Epub] CrossRef - Association between diabetic peripheral neuropathy and sarcopenia: A systematic review and meta‐analysis
Thapat Wannarong, Persen Sukpornchairak, Weerakit Naweera, Christopher D. Geiger, Patompong Ungprasert
Geriatrics & Gerontology International.2022; 22(9): 785. CrossRef - Synergistic Interaction between Hyperuricemia and Abdominal Obesity as a Risk Factor for Metabolic Syndrome Components in Korean Population
Min Jin Lee, Ah Reum Khang, Yang Ho Kang, Mi Sook Yun, Dongwon Yi
Diabetes & Metabolism Journal.2022; 46(5): 756. CrossRef - HOMA-IR as a predictor of Health Outcomes in Patients with Metabolic Risk Factors: A Systematic Review and Meta-analysis
José G. González-González, Jorge R. Violante-Cumpa, Miguel Zambrano-Lucio, Erick Burciaga-Jimenez, Patricia L. Castillo-Morales, Mariano Garcia-Campa, Ricardo César Solis, Alejandro D González-Colmenero, René Rodríguez-Gutiérrez
High Blood Pressure & Cardiovascular Prevention.2022; 29(6): 547. CrossRef - Maternal height as a predictor of glucose intolerance in the postpartum and its relationship with maternal pre-gestational weight
Catarina Cidade-Rodrigues, Filipe M. Cunha, Catarina Chaves, Fabiana Castro, Catarina Pereira, Sílvia Paredes, Margarida Silva-Vieira, Anabela Melo, Odete Figueiredo, Cláudia Nogueira, Ana Morgado, Mariana Martinho, Maria C. Almeida, Margarida Almeida
Archives of Gynecology and Obstetrics.2022; 307(2): 601. CrossRef - Correlation of body composition in early pregnancy on gestational diabetes mellitus under different body weights before pregnancy
Li Xintong, Xu Dongmei, Zhang Li, Cao Ruimin, Hao Yide, Cui Lingling, Chen Tingting, Guo Yingying, Li Jiaxin
Frontiers in Endocrinology.2022;[Epub] CrossRef - Relationship between low skeletal muscle mass, sarcopenic obesity and left ventricular diastolic dysfunction in Korean adults
Jee Hee Yoo, Sung Woon Park, Ji Eun Jun, Sang‐Man Jin, Kyu Yeon Hur, Moon‐Kyu Lee, Mira Kang, Gyuri Kim, Jae Hyeon Kim
Diabetes/Metabolism Research and Reviews.2021;[Epub] CrossRef - Skeletal Muscle and Metabolic Health: How Do We Increase Muscle Mass and Function in People with Type 2 Diabetes?
Ebaa Al-Ozairi, Dalal Alsaeed, Dherar Alroudhan, Nia Voase, Amal Hasan, Jason M R Gill, Naveed Sattar, Paul Welsh, Cindy M Gray, Jirapitcha Boonpor, Carlos Celis-Morales, Stuart R Gray
The Journal of Clinical Endocrinology & Metabolism.2021; 106(2): 309. CrossRef - Association of the triglyceride and glucose index with low muscle mass: KNHANES 2008–2011
Jung A. Kim, Soon Young Hwang, Ji Hee Yu, Eun Roh, So-hyeon Hong, You-Bin Lee, Nam Hoon Kim, Hye Jin Yoo, Ji A. Seo, Nan Hee Kim, Sin Gon Kim, Sei Hyun Baik, Kyung Mook Choi
Scientific Reports.2021;[Epub] CrossRef - ADAS-viewer: web-based application for integrative analysis of multi-omics data in Alzheimer’s disease
Seonggyun Han, Jaehang Shin, Hyeim Jung, Jane Ryu, Habtamu Minassie, Kwangsik Nho, Insong Koh, Younghee Lee
npj Systems Biology and Applications.2021;[Epub] CrossRef - Relative associations of abdominal and thigh compositions with cardiometabolic diseases in African Caribbean men
Curtis Tilves, Joseph M. Zmuda, Allison L. Kuipers, Sangeeta Nair, John Jeffrey Carr, James G. Terry, Shyamal Peddada, Victor Wheeler, Iva Miljkovic
Obesity Science & Practice.2021; 7(6): 738. CrossRef - Changes in creatinine‐to‐cystatin C ratio over 4 years, risk of diabetes, and cardiometabolic control: The China Health and Retirement Longitudinal Study
Shanhu Qiu, Xue Cai, Yang Yuan, Bo Xie, Zilin Sun, Tongzhi Wu
Journal of Diabetes.2021; 13(12): 1025. CrossRef - Associations Between Glucose Tolerance, Insulin Secretion, Muscle and Fat Mass in Cystic Fibrosis
Bibi Uhre Nielsen, Daniel Faurholt-Jepsen, Peter Sandor Oturai, Tavs Qvist, Rikke Krogh-Madsen, Terese Lea Katzenstein, James Shaw, Christian Ritz, Tacjana Pressler, Thomas Peter Almdal, Inger Hee Mabuza Mathiesen
Clinical Medicine Insights: Endocrinology and Diabetes.2021; 14: 117955142110382. CrossRef - Total and regional fat‐to‐muscle mass ratio measured by bioelectrical impedance and risk of incident type 2 diabetes
Ningjian Wang, Ying Sun, Haojie Zhang, Chi Chen, Yuying Wang, Jihui Zhang, Fangzhen Xia, Christian Benedict, Xiao Tan, Yingli Lu
Journal of Cachexia, Sarcopenia and Muscle.2021; 12(6): 2154. CrossRef - How was the Diabetes Metabolism Journal added to MEDLINE?
Hye Jin Yoo
Science Editing.2020; 7(2): 201. CrossRef - An update on nutrient modulation in the management of disease-induced muscle wasting: evidence from human studies
Matthew S. Brook, Daniel J. Wilkinson, Philip J. Atherton
Current Opinion in Clinical Nutrition & Metabolic Care.2020; 23(3): 174. CrossRef - The functional nutritional and regulatory activities of calcium supplementation from eggshell for obesity disorders management
Marwa El‐Zeftawy, Samar Abd‐El Mohsen Ali, Sally Salah, Hani S. Hafez
Journal of Food Biochemistry.2020;[Epub] CrossRef - Dose‐response associations between serum creatinine and type 2 diabetes mellitus risk: A Chinese cohort study and meta‐analysis of cohort studies
Pei Qin, Yanmei Lou, Liming Cao, Jing Shi, Gang Tian, Dechen Liu, Qionggui Zhou, Chunmei Guo, Quanman Li, Yang Zhao, Feiyan Liu, Xiaoyan Wu, Ranran Qie, Minghui Han, Shengbing Huang, Ping Zhao, Changyi Wang, Jianping Ma, Xiaolin Peng, Shan Xu, Hongen Chen
Journal of Diabetes.2020; 12(8): 594. CrossRef - Caloric restriction in heart failure: A systematic review
Vittorio Emanuele Bianchi
Clinical Nutrition ESPEN.2020; 38: 50. CrossRef - Association between the Thigh Muscle and Insulin Resistance According to Body Mass Index in Middle-Aged Korean Adults
Ji Eun Heo, Jee-Seon Shim, Hokyou Lee, Hyeon Chang Kim
Diabetes & Metabolism Journal.2020; 44(3): 446. CrossRef - Joint impact of muscle mass and waist circumference on type 2 diabetes in Japanese middle‐aged adults: The Circulatory Risk in Communities Study (CIRCS)
Mikako Yasuoka, Isao Muraki, Hironori Imano, Hiroshige Jinnouchi, Yasuhiko Kubota, Mina Hayama‐Terada, Mitsumasa Umesawa, Kazumasa Yamagishi, Tetsuya Ohira, Akihiko Kitamura, Takeo Okada, Masahiko Kiyama, Hiroyasu Iso
Journal of Diabetes.2020; 12(9): 677. CrossRef - Catch-Up Growth in Children Born Small for Gestational Age Related to Body Composition and Metabolic Risk at Six Years of Age in the UK
M. Loredana Marcovecchio, Samantha Gorman, Laura P.E. Watson, David B. Dunger, Kathryn Beardsall
Hormone Research in Paediatrics.2020; 93(2): 119. CrossRef - Response: Association of Thigh Muscle Mass with Insulin Resistance and Incident Type 2 Diabetes Mellitus in Japanese Americans (Diabetes Metab J 2018;42:488–95)
Seung Jin Han, Edward J. Boyko
Diabetes & Metabolism Journal.2019; 43(1): 125. CrossRef - Berberine chloride ameliorated PI3K/Akt‐p/SIRT‐1/PTEN signaling pathway in insulin resistance syndrome induced in rats
Marwa El‐Zeftawy, Doaa Ghareeb, Eman R. ElBealy, Rasha Saad, Salma Mahmoud, Nihal Elguindy, Attalla F. El‐kott, Mohamed El‐Sayed
Journal of Food Biochemistry.2019;[Epub] CrossRef - Letter: Association of Thigh Muscle Mass with Insulin Resistance and Incident Type 2 Diabetes Mellitus in Japanese Americans (Diabetes Metab J 2018;42:488–95)
Nan Hee Cho, Hye Soon Kim
Diabetes & Metabolism Journal.2019; 43(1): 123. CrossRef - Asian Indians With Prediabetes Have Similar Skeletal Muscle Mass and Function to Those With Type 2 Diabetes
Sucharita Sambashivaiah, Stephen D. R. Harridge, Nidhi Sharma, Sumithra Selvam, Priyanka Rohatgi, Anura V. Kurpad
Frontiers in Nutrition.2019;[Epub] CrossRef

 KDA
KDA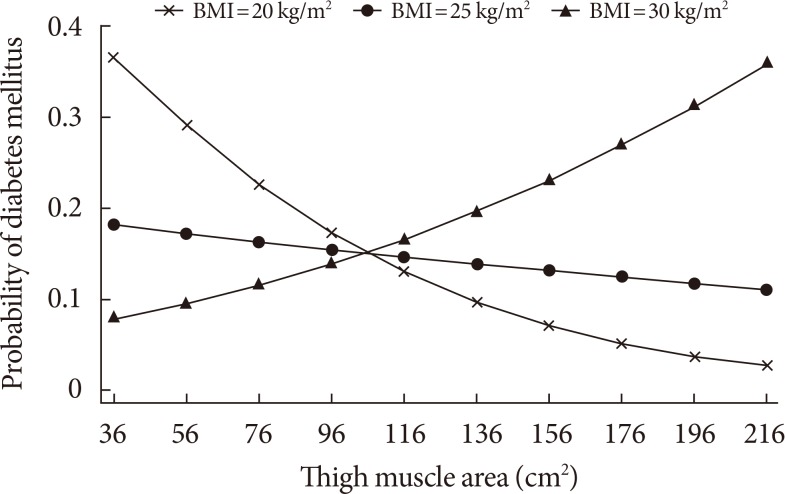
 PubReader
PubReader Cite
Cite




