- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 45(4); 2021 > Article
-
ReviewGuideline/Fact Sheet 2021 Clinical Practice Guidelines for Diabetes Mellitus in Korea
-
Kyu Yeon Hur1
 , Min Kyong Moon2, Jong Suk Park3, Soo-Kyung Kim4, Seung-Hwan Lee5, Jae-Seung Yun5, Jong Ha Baek6, Junghyun Noh7, Byung-Wan Lee3, Tae Jung Oh8, Suk Chon9, Ye Seul Yang5, Jang Won Son5, Jong Han Choi10, Kee Ho Song10, Nam Hoon Kim11, Sang Yong Kim12, Jin Wha Kim12, Sang Youl Rhee9, You-Bin Lee1, Sang-Man Jin1, Jae Hyeon Kim1, Chong Hwa Kim13, Dae Jung Kim14, SungWan Chun15, Eun-Jung Rhee16, Hyun Min Kim17, Hyun Jung Kim18, Donghyun Jee19, Jae Hyun Kim20, Won Seok Choi21, Eun-Young Lee5, Kun-Ho Yoon5, Seung-Hyun Ko5
, Min Kyong Moon2, Jong Suk Park3, Soo-Kyung Kim4, Seung-Hwan Lee5, Jae-Seung Yun5, Jong Ha Baek6, Junghyun Noh7, Byung-Wan Lee3, Tae Jung Oh8, Suk Chon9, Ye Seul Yang5, Jang Won Son5, Jong Han Choi10, Kee Ho Song10, Nam Hoon Kim11, Sang Yong Kim12, Jin Wha Kim12, Sang Youl Rhee9, You-Bin Lee1, Sang-Man Jin1, Jae Hyeon Kim1, Chong Hwa Kim13, Dae Jung Kim14, SungWan Chun15, Eun-Jung Rhee16, Hyun Min Kim17, Hyun Jung Kim18, Donghyun Jee19, Jae Hyun Kim20, Won Seok Choi21, Eun-Young Lee5, Kun-Ho Yoon5, Seung-Hyun Ko5 , Committee of Clinical Practice Guidelines, Korean Diabetes Association
, Committee of Clinical Practice Guidelines, Korean Diabetes Association -
Diabetes & Metabolism Journal 2021;45(4):461-481.
DOI: https://doi.org/10.4093/dmj.2021.0156
Published online: July 30, 2021
1Division of Endocrinology and Metabolism, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
2Department of Internal Medicine, Seoul Metropolitan Government Seoul National University Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea
3Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
4Division of Endocrinology and Metabolism, Department of Internal Medicine, CHA Bundang Medical Center, CHA University, Seongnam, Korea
5Division of Endocrinology and Metabolism, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
6Division of Endocrinology & Metabolism, Department of Medicine, Gyeongsang National University Changwon Hospital, Gyeongsang National University College of Medicine, Changwon, Korea
7Division of Endocrinology and Metabolism, Department of Internal Medicine, Inje University Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea
8Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
9Department of Endocrinology and Metabolism, Kyung Hee University College of Medicine, Kyung Hee University Hospital, Seoul, Korea
10Division of Endocrinology and Metabolism, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea
11Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea
12Division of Endocrinology and Metabolism, Department of Internal Medicine, Chosun University College of Medicine, Gwangju, Korea
13Division of Endocrinology & Metabolism, Department of Internal Medicine, Sejong General Hospital, Bucheon, Korea
14Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea
15Department of Internal Medicine, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea
16Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
17Division of Endocrinology and Metabolism, Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea
18Institute for Evidence-based Medicine, Cochrane Korea, Department of Preventive Medicine, Korea University College of Medicine, Seoul, Korea
19Division of Vitreous and Retina, Department of Ophthalmology, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
20Department of Pediatrics, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
21Division of Infectious Diseases, Department of Internal Medicine, Korea University College of Medicine, Korea University Ansan Hospital, Ansan, Korea
-
Corresponding author: Seung-Hyun Ko
 Division of Endocrinology & Metabolism, Department of Internal Medicine, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, 93 Jungbu-daero, Paldal-gu, Suwon 16247, Korea E-mail: kosh@catholic.ac.kr
Division of Endocrinology & Metabolism, Department of Internal Medicine, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, 93 Jungbu-daero, Paldal-gu, Suwon 16247, Korea E-mail: kosh@catholic.ac.kr
Copyright © 2021 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- ABSTRACT
- INTRODUCTION
- DIAGNOSIS OF DIABETES MELLITUS
- SCREENING AND PREVENTION OF DIABETES
- GLYCEMIC, BLOOD PRESSURE, AND LIPID CONTROL TARGETS IN T2DM
- OBESITY MANAGEMENT IN T2DM
- ANTIHYPERGLYCEMIC THERAPY FOR ADULT PATIENTS WITH TYPE 1 DIABETES MELLITUS
- ANTIHYPERGLYCEMIC THERAPY FOR ADULT PATIENTS WITH T2DM
- DIABETIC KIDNEY DISEASE (DIABETIC NEPHROPATHY)
- DIABETIC NEUROPATHY AND FOOT CARE
- DIABETIC RETINOPATHY
- NAFLD IN T2DM
- CGM SYSTEM AND INSULIN PUMP USE
- VACCINATION FOR PATIENTS WITH T2DM
- CONCLUSIONS
- NOTES
- REFERENCES
Figure & Data
References
Citations

- Impact of Subclinical Atrial Function on the Prognosis of Patients With Atrial Fibrillation and Metabolic Syndrome
Hyun-Jin Kim
CardioMetabolic Syndrome Journal.2024; 4(1): 36. CrossRef - A Multicenter, Randomized, Open-Label Study to Compare the Effects of Gemigliptin Add-on or Escalation of Metformin Dose on Glycemic Control and Safety in Patients with Inadequately Controlled Type 2 Diabetes Mellitus Treated with Metformin and SGLT-2 Inh
Hae Jin Kim, Jung Hyun Noh, Min Kyong Moon, Sung Hee Choi, Seung-Hyun Ko, Eun-Jung Rhee, Kyu Yeon Hur, In-Kyung Jeong, Mark Yorek
Journal of Diabetes Research.2024; 2024: 1. CrossRef - Efficacy and Safety of Once-Weekly Semaglutide Versus Once-Daily Sitagliptin as Metformin Add-on in a Korean Population with Type 2 Diabetes
Byung-Wan Lee, Young Min Cho, Sin Gon Kim, Seung-Hyun Ko, Soo Lim, Amine Dahaoui, Jin Sook Jeong, Hyo Jin Lim, Jae Myung Yu
Diabetes Therapy.2024; 15(2): 547. CrossRef - Real-World Continuous Glucose Monitoring Data from a Population with Type 1 Diabetes in South Korea: Nationwide Single-System Analysis
Ji Yoon Kim, Sang-Man Jin, Sarah B. Andrade, Boyang Chen, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2024;[Epub] CrossRef - Association between Dyslipidemia and Glycated Hemoglobin in a Population-Based Study
Purum Kang, Ka Young Kim, Hye Young Shin
Metabolites.2024; 14(2): 92. CrossRef - Outcomes of Various Classes of Oral Antidiabetic Drugs on Nonalcoholic Fatty Liver Disease
Heejoon Jang, Yeonjin Kim, Dong Hyeon Lee, Sae Kyung Joo, Bo Kyung Koo, Soo Lim, Woojoo Lee, Won Kim
JAMA Internal Medicine.2024; 184(4): 375. CrossRef - View on Metformin: Antidiabetic and Pleiotropic Effects, Pharmacokinetics, Side Effects, and Sex-Related Differences
Guglielmina Froldi
Pharmaceuticals.2024; 17(4): 478. CrossRef - Comparison between a tubeless, on-body automated insulin delivery system and a tubeless, on-body sensor-augmented pump in type 1 diabetes: a multicentre randomised controlled trial
Ji Yoon Kim, Sang-Man Jin, Eun Seok Kang, Soo Heon Kwak, Yeoree Yang, Jee Hee Yoo, Jae Hyun Bae, Jun Sung Moon, Chang Hee Jung, Ji Cheol Bae, Sunghwan Suh, Sun Joon Moon, Sun Ok Song, Suk Chon, Jae Hyeon Kim
Diabetologia.2024;[Epub] CrossRef - Inhibition of sodium-glucose cotransporter-2 and liver-related complications in individuals with diabetes: a Mendelian randomization and population-based cohort study
Sung Won Chung, Hye-Sung Moon, Hyunjae Shin, Hyein Han, Sehoon Park, Heejin Cho, Jeayeon Park, Moon Haeng Hur, Min Kyung Park, Sung-Ho Won, Yun Bin Lee, Eun Ju Cho, Su Jong Yu, Dong Ki Kim, Jung-Hwan Yoon, Jeong-Hoon Lee, Yoon Jun Kim
Hepatology.2024;[Epub] CrossRef - Health and Productivity Benefits with Early Intensified Treatment in Patients with Type 2 Diabetes: Results from Korea
Foteini Tsotra, Ankur Malhotra, Platon Peristeris, Ioannis Athanasiou, Malina Müller, Giovanni Bader
INQUIRY: The Journal of Health Care Organization, Provision, and Financing.2024;[Epub] CrossRef - Efficacy of intermittent short‐term use of a real‐time continuous glucose monitoring system in non‐insulin–treated patients with type 2 diabetes: A randomized controlled trial
Sun Joon Moon, Kyung‐Soo Kim, Woo Je Lee, Mi Yeon Lee, Robert Vigersky, Cheol‐Young Park
Diabetes, Obesity and Metabolism.2023; 25(1): 110. CrossRef - Therapeutic Effects of Switching to Anagliptin from Other DPP-4 Inhibitors in T2DM Patients with Inadequate Glycemic Control: A Non-interventional, Single-Arm, Open-Label, Multicenter Observational Study
Sang-Yong Kim, Sungrae Kim
Diabetes Therapy.2023; 14(1): 109. CrossRef - Low Skeletal Muscle Mass Accompanied by Abdominal Obesity Additively Increases the Risk of Incident Type 2 Diabetes
Ji Eun Jun, Seung-Eun Lee, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Jae Hwan Jee, Jae Hyeon Kim
The Journal of Clinical Endocrinology & Metabolism.2023; 108(5): 1173. CrossRef - Diabetes screening in South Korea: a new estimate of the number needed to screen to detect diabetes
Kyoung Hwa Ha, Kyung Ae Lee, Kyung-Do Han, Min Kyong Moon, Dae Jung Kim
The Korean Journal of Internal Medicine.2023; 38(1): 93. CrossRef - Justicia carnea extracts ameliorated hepatocellular damage in streptozotocin-induced type 1 diabetic male rats via decrease in oxidative stress, inflammation and increasing other risk markers
John Adeolu Falode, Oluwaseun Igbekele Ajayi, Tolulope Victoria Isinkaye, Akinwunmi Oluwaseun Adeoye, Basiru Olaitan Ajiboye, Bartholomew I. C. Brai
Biomarkers.2023; 28(2): 177. CrossRef - Sex differences in the impact of diabetes mellitus on tuberculosis recurrence: a retrospective national cohort study
Dararat Eksombatchai, Dawoon Jeong, Jeongha Mok, Doosoo Jeon, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Hongjo Choi, Young Ae Kang
International Journal of Infectious Diseases.2023; 127: 1. CrossRef - The Predictive Ability of C-Peptide in Distinguishing Type 1 Diabetes From Type 2 Diabetes: A Systematic Review and Meta-Analysis
Sajid Iqbal, Abdulrahim Abu Jayyab, Ayah Mohammad Alrashdi, Silvia Reverté-Villarroya
Endocrine Practice.2023; 29(5): 379. CrossRef - Anagliptin twice‐daily regimen improves glycaemic variability in subjects with type 2 diabetes: A double‐blind, randomized controlled trial
Yong‐ho Lee, Doo‐Man Kim, Jae Myung Yu, Kyung Mook Choi, Sin Gon Kim, Kang Seo Park, Hyun‐Shik Son, Choon Hee Chung, Kyu Jeung Ahn, Soon Hee Lee, Ki‐Ho Song, Su Kyoung Kwon, Hyeong Kyu Park, Kyu Chang Won, Hak Chul Jang
Diabetes, Obesity and Metabolism.2023; 25(5): 1174. CrossRef - Implementation of five machine learning methods to predict the 52-week blood glucose level in patients with type 2 diabetes
Xiaomin Fu, Yuhan Wang, Ryan S. Cates, Nan Li, Jing Liu, Dianshan Ke, Jinghua Liu, Hongzhou Liu, Shuangtong Yan
Frontiers in Endocrinology.2023;[Epub] CrossRef - Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - The Efficacy of Treatment Intensification by Quadruple Oral Therapy Compared to GLP-1RA Therapy in Poorly Controlled Type 2 Diabetes Mellitus Patients: A Real-world Data Study
Minyoung Kim, Hosu Kim, Kyong Young Kim, Soo Kyoung Kim, Junghwa Jung, Jong Ryeal Hahm, Jaehoon Jung, Jong Ha Baek
Diabetes & Metabolism Journal.2023; 47(1): 135. CrossRef - Safety and Effectiveness of Empagliflozin in Korean Patients with Type 2 Diabetes Mellitus: Results from a Nationwide Post-Marketing Surveillance
Jun Sung Moon, Nam Hoon Kim, Jin Oh Na, Jae Hyoung Cho, In-Kyung Jeong, Soon Hee Lee, Ji-Oh Mok, Nan Hee Kim, Dong Jin Chung, Jinhong Cho, Dong Woo Lee, Sun Woo Lee, Kyu Chang Won
Diabetes & Metabolism Journal.2023; 47(1): 82. CrossRef - Evaluation and Management of Patients With Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
International Journal of Heart Failure.2023; 5(1): 1. CrossRef - Influenza vaccination trend and related factors among patients with diabetes in Korea: Analysis using a nationwide database
Dong-Hwa Lee, Bumhee Yang, Seonhye Gu, Eung-Gook Kim, Youlim Kim, Hyung Koo Kang, Yeong Hun Choe, Hyun Jeong Jeon, Seungyong Park, Hyun Lee
Frontiers in Endocrinology.2023;[Epub] CrossRef - Optimal Low-Density Lipoprotein Cholesterol Level for Primary Prevention in Koreans with Type 2 Diabetes Mellitus
Ji Yoon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2023; 47(1): 42. CrossRef - Evaluation and Management of Patients with Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 10. CrossRef - Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Association between Low-Density Lipoprotein Cholesterol Level and Cardiovascular Outcomes in Korean Adults: A Nationwide Cohort Study
Junghyun Noh, Min Kyong Moon, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong
Diabetes & Metabolism Journal.2023; 47(1): 59. CrossRef - Analysis of the Incidence of Type 2 Diabetes, Requirement of Insulin Treatment, and Diabetes-Related Complications among Patients with Cancer
Su Jung Lee, Chulho Kim, Hyunjae Yu, Dong-Kyu Kim
Cancers.2023; 15(4): 1094. CrossRef - The 2022 focused update of the 2018 Korean Hypertension Society Guidelines for the management of hypertension
Hack-Lyoung Kim, Eun Mi Lee, Shin Young Ahn, Kwang-il Kim, Hyeon Chang Kim, Ju Han Kim, Hae-Young Lee, Jang Hoon Lee, Jong-Moo Park, Eun Joo Cho, Sungha Park, Jinho Shin, Young-Kwon Kim
Clinical Hypertension.2023;[Epub] CrossRef - Consistency of 1-day and 3-day average dietary intake and the relationship of dietary intake with blood glucose, hbA1c, BMI, and lipids in patients with type 2 diabetes
DaeEun Lee, Haejung Lee, Sangeun Lee, MinJin Lee, Ah Reum Khang
Journal of Korean Biological Nursing Science.2023; 25(1): 20. CrossRef - Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
Kyung-Soo Kim, Kyung Ah Han, Tae Nyun Kim, Cheol-Young Park, Jung Hwan Park, Sang Yong Kim, Yong Hyun Kim, Kee Ho Song, Eun Seok Kang, Chul Sik Kim, Gwanpyo Koh, Jun Goo Kang, Mi Kyung Kim, Ji Min Han, Nan Hee Kim, Ji Oh Mok, Jae Hyuk Lee, Soo Lim, Sang S
Diabetes & Metabolism.2023; 49(4): 101440. CrossRef - Effect of olmesartan and amlodipine on serum angiotensin-(1–7) levels and kidney and vascular function in patients with type 2 diabetes and hypertension
Kyuho Kim, Ji Hye Moon, Chang Ho Ahn, Soo Lim
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Menopausal hormone therapy and the risk of type 2 diabetes mellitus: Health Insurance Database in South Korea–based retrospective cohort study
Jin-Sung Yuk, Jung Min Kim
Menopause.2023; 30(5): 497. CrossRef - Intensified Multifactorial Intervention in Patients with Type 2 Diabetes Mellitus
Takayoshi Sasako, Toshimasa Yamauchi, Kohjiro Ueki
Diabetes & Metabolism Journal.2023; 47(2): 185. CrossRef - Association between antidiabetic drugs and the incidence of atrial fibrillation in patients with type 2 diabetes: A nationwide cohort study in South Korea
Sunyoung Kim, So Young Park, Bongseong Kim, Chanyang Min, Wonyoung Cho, Dong Keon Yon, Joo Young Kim, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee, Sang Youl Rhee
Diabetes Research and Clinical Practice.2023; 198: 110626. CrossRef - Totally robotic Roux-en-Y gastric bypass in a morbidly obese patient in Korea: a case report
Ji Won Seo, Kyong-Hwa Jun
Journal of Minimally Invasive Surgery.2023; 26(1): 40. CrossRef - Effect of diabetes-specific oral nutritional supplements with allulose on weight and glycemic profiles in overweight or obese type 2 diabetic patients
Jihye Tak, Minkyung Bok, Hyunkyung Rho, Ju Hyun Park, Yunsook Lim, Suk Chon, Hyunjung Lim
Nutrition Research and Practice.2023; 17(2): 241. CrossRef - Associations Between Modifiable Risk Factors and Changes in Glycemic Status Among Individuals With Prediabetes
Salma Nabila, Ji-Eun Kim, Jaesung Choi, JooYong Park, Aesun Shin, Sang-Ah Lee, Jong-koo Lee, Daehee Kang, Ji-Yeob Choi
Diabetes Care.2023; 46(3): 535. CrossRef - Efficacy and safety of enavogliflozin, a novel SGLT2 inhibitor, in Korean people with type 2 diabetes: A 24‐week, multicentre, randomized, double‐blind, placebo‐controlled, phase III trial
Soo Heon Kwak, Kyung Ah Han, Kyung‐Soo Kim, Jae Myung Yu, EunSook Kim, Jong Chul Won, Jun Goo Kang, Choon Hee Chung, Seungjoon Oh, Sung Hee Choi, Kyu Chang Won, Sin Gon Kim, Seung Ah Cho, Bo Young Cho, Kyong Soo Park
Diabetes, Obesity and Metabolism.2023; 25(7): 1865. CrossRef - Adjusting the Use of Glucose-Lowering Agents in the Real-World Clinical Management of People with Type 2 Diabetes: A Narrative Review
Siew Pheng Chan, Lee-Ling Lim, Juliana C. N. Chan, David R. Matthews
Diabetes Therapy.2023; 14(5): 823. CrossRef - The association of perfluoroalkyl substances (PFAS) exposure and kidney function in Korean adolescents using data from Korean National Environmental Health Survey (KoNEHS) cycle 4 (2018–2020): a cross-sectional study
Jisuk Yun, Eun-Chul Jang, Soon-Chan Kwon, Young-Sun Min, Yong-Jin Lee
Annals of Occupational and Environmental Medicine.2023;[Epub] CrossRef - A Comparison of the Pharmacokinetics and Safety of Dapagliflozin Formate, an Ester Prodrug of Dapagliflozin, to Dapagliflozin Propanediol Monohydrate in Healthy Subjects
Hyun Chul Kim, Sangmi Lee, Siyoung Sung, Eunjin Kim, In-Jin Jang, Jae-Yong Chung
Drug Design, Development and Therapy.2023; Volume 17: 1203. CrossRef - Efficacy and safety of monotherapy with enavogliflozin in Korean patients with type 2 diabetes mellitus: Results of a 12‐week, multicentre, randomized, double‐blind, placebo‐controlled, phase 2 trial
Ye Seul Yang, Kyung Wan Min, Seok‐O Park, Kyung‐Soo Kim, Jae Myung Yu, Eun‐Gyoung Hong, Sung Rae Cho, Kyu Chang Won, Yong Hyun Kim, Seungjoon Oh, Sung Hee Choi, Gwanpyo Koh, Wan Huh, Su Young Kim, Kyong Soo Park
Diabetes, Obesity and Metabolism.2023; 25(8): 2096. CrossRef - An Integrated Digital Health Care Platform for Diabetes Management With AI-Based Dietary Management: 48-Week Results From a Randomized Controlled Trial
You-Bin Lee, Gyuri Kim, Ji Eun Jun, Hyunjin Park, Woo Je Lee, You-Cheol Hwang, Jae Hyeon Kim
Diabetes Care.2023; 46(5): 959. CrossRef - Performance of Simple Fibrosis Score in Non-Alcoholic Fatty Liver Disease with and without Type 2 Diabetes
Seung Min Chung, Min Kyu Kang, Jun Sung Moon, Jung Gil Park
Endocrinology and Metabolism.2023; 38(2): 277. CrossRef - Correlation analysis of cancer incidence after pravastatin treatment
Jin Yu, Raeun Kim, Jiwon Shinn, Man Young Park, Hun-Sung Kim
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 61. CrossRef - Comparison of the effects of gemigliptin versus glimepiride on cardiac function in patients with type 2 diabetes uncontrolled with metformin: The gemi‐heart study
Seung Min Chung, Jun Sung Moon, Jun Hwa Hong, In‐Chang Hwang, Soo Lim
Diabetes, Obesity and Metabolism.2023; 25(8): 2181. CrossRef - The era of continuous glucose monitoring and its expanded role in type 2 diabetes
Jin Yu, Jae‐Hyoung Cho, Seung‐Hwan Lee
Journal of Diabetes Investigation.2023; 14(7): 841. CrossRef - Impact of continuous glucose monitoring on glycemic control and its derived metrics in type 1 diabetes: a longitudinal study
So Hyun Cho, Seohyun Kim, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Gyuri Kim, Jae Hyeon Kim
Frontiers in Endocrinology.2023;[Epub] CrossRef - Impact of mental disorders on the risk of heart failure among Korean patients with diabetes: a cohort study
Tae Kyung Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Diabetology.2023;[Epub] CrossRef - Asia-Pacific consensus recommendations for application of continuous glucose monitoring in diabetes management
Alice P.S. Kong, Soo Lim, Seung-Hyun Yoo, Linong Ji, Liming Chen, Yuqian Bao, Ester Yeoh, Siew-Pheng Chan, Chih-Yuan Wang, Viswanathan Mohan, Neale Cohen, Margaret J. McGill, Stephen M. Twigg
Diabetes Research and Clinical Practice.2023; 201: 110718. CrossRef - Chronic disease management program applied to type 2 diabetes patients and prevention of diabetic complications: a retrospective cohort study using nationwide data
Min Kyung Hyun, Jang Won Lee, Seung-Hyun Ko
BMC Public Health.2023;[Epub] CrossRef - Fatty Liver & Diabetes Statistics in Korea: Nationwide Data 2009 to 2017
Eugene Han, Kyung-Do Han, Yong-ho Lee, Kyung-Soo Kim, Sangmo Hong, Jung Hwan Park, Cheol-Young Park
Diabetes & Metabolism Journal.2023; 47(3): 347. CrossRef - Opening the Precision Diabetes Care through Digital Healthcare
Joonyub Lee, Jin Yu, Kun-Ho Yoon
Diabetes & Metabolism Journal.2023; 47(3): 307. CrossRef - Glycemia according to the Use of Continuous Glucose Monitoring among Adults with Type 1 Diabetes Mellitus in Korea: A Real-World Study
You-Bin Lee, Minjee Kim, Jae Hyeon Kim
Diabetes & Metabolism Journal.2023; 47(3): 405. CrossRef - Navigating the Seas of Glycemic Control: The Role of Continuous Glucose Monitoring in Type 1 Diabetes Mellitus
Jun Sung Moon
Diabetes & Metabolism Journal.2023; 47(3): 345. CrossRef - Lost in translation: assessing the nomenclature change for diabetic kidney disease in Japan
Tetsuya Babazono, Tatsumi Moriya
Diabetology International.2023; 14(4): 319. CrossRef - Effects of dapagliflozin compared with glimepiride on body composition in Asian patients with type 2 diabetes inadequately controlled with metformin: The BEYOND study
Hyeong Kyu Park, Kyoung‐Ah Kim, Kyung‐Wan Min, Tae‐Seo Sohn, In Kyung Jeong, Chul Woo Ahn, Nan‐Hee Kim, Ie Byung Park, Ho Chan Cho, Choon Hee Chung, Sung Hee Choi, Kang Seo Park, Seoung‐Oh Yang, Kwan Woo Lee
Diabetes, Obesity and Metabolism.2023; 25(9): 2743. CrossRef - Topic Modeling Analysis of Diabetes-Related Health Information during the Coronavirus Disease Pandemic
Soyoon Min, Jeongwon Han
Healthcare.2023; 11(13): 1871. CrossRef - Screening Test for Evaluation of Cardiovascular Disease in Patients with Diabetes
Ji-Oh Mok, Chan-Hee Jung
The Journal of Korean Diabetes.2023; 24(2): 76. CrossRef - Paradigm Shift in Management of Hyperglycemia in Patients with Type 2 Diabetes: Glucocentric versus Organ Protection
Jong Chul Won
The Journal of Korean Diabetes.2023; 24(2): 59. CrossRef - Association between type 2 diabetes mellitus and depression among Korean midlife women: a cross-sectional analysis study
You Lee Yang, Eun-Ok Im, Yunmi Kim
BMC Nursing.2023;[Epub] CrossRef - Fibrotic Burden in the Liver Differs Across Metabolic Dysfunction-Associated Fatty Liver Disease Subtypes
Tae Seop Lim, Ho Soo Chun, Soon Sun Kim, Ja Kyung Kim, Minjong Lee, Hyo Jung Cho, Seung Up Kim, Jae Youn Cheong
Gut and Liver.2023; 17(4): 610. CrossRef - Association between the number of pregnancies and cardiac target organ damages: a cross-sectional analysis of data from the Korean women’s chest pain registry (KoROSE)
Hack-Lyoung Kim, Hyun-Jin Kim, Mina Kim, Sang Min Park, Hyun Ju Yoon, Young Sup Byun, Seong-Mi Park, Mi-Seung Shin, Kyung-Soon Hong, Myung-A Kim
BMC Women's Health.2023;[Epub] CrossRef - Exercise therapy for diabetes mellitus
Chaiho Jeong, Tae-Seo Sohn
Journal of the Korean Medical Association.2023; 66(7): 427. CrossRef - Medical nutrition therapy for diabetes mellitus
Suk Chon
Journal of the Korean Medical Association.2023; 66(7): 421. CrossRef - Identification of individuals at risk of hepatocellular carcinoma: screening for clinically significant liver fibrosis in patients with T2DM
Tina Reinson, Ryan M Buchanan, Christopher D Byrne
Expert Review of Endocrinology & Metabolism.2023; 18(5): 355. CrossRef - Additive impact of diabetes and sarcopenia on all-cause and cardiovascular mortality: A longitudinal nationwide population-based study
Eyun Song, Soon Young Hwang, Min Jeong Park, Ahreum Jang, Kyeong Jin Kim, Ji Hee Yu, Nam Hoon Kim, Hye Jin Yoo, Ji A. Seo, Sin Gon Kim, Nan Hee Kim, Sei Hyun Baik, Kyung Mook Choi
Metabolism.2023; 148: 155678. CrossRef - Exposure to perfluoroalkyl and polyfluoroalkyl substances and risk of stroke in adults: a meta-analysis
Min Cheol Chang, Seung Min Chung, Sang Gyu Kwak
Reviews on Environmental Health.2023;[Epub] CrossRef - Risk of Pancreatic Cancer and Use of Dipeptidyl Peptidase 4 Inhibitors in Patients with Type 2 Diabetes: A Propensity Score-Matching Analysis
Mee Kyoung Kim, Kyungdo Han, Hyuk-Sang Kwon, Soon Jib Yoo
Endocrinology and Metabolism.2023; 38(4): 426. CrossRef - Incident infection risks depending on oral antidiabetic exposure in insulin-treated type 2 diabetes patients
Sanghwa Park, Jiseon Jeong, Yunna Woo, Yeo Jin Choi, Sooyoung Shin
Scientific Reports.2023;[Epub] CrossRef - Dyslipidemia Fact Sheet in South Korea, 2022
Eun-Sun Jin, Jee-Seon Shim, Sung Eun Kim, Jae Hyun Bae, Shinae Kang, Jong Chul Won, Min-Jeong Shin, Heung Yong Jin, Jenny Moon, Hokyou Lee, Hyeon Chang Kim, In-Kyung Jeong
Journal of Lipid and Atherosclerosis.2023; 12(3): 237. CrossRef - Diabetes Mellitus in the Elderly Adults in Korea: Based on Data from the Korea National Health and Nutrition Examination Survey 2019 to 2020
Seung-Hyun Ko, Kyung Do Han, Yong-Moon Park, Jae-Seung Yun, Kyuho Kim, Jae-Hyun Bae, Hyuk-Sang Kwon, Nan-Hee Kim
Diabetes & Metabolism Journal.2023; 47(5): 643. CrossRef - Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): A State-of-the-Art Review
Wah-Kheong Chan, Kee-Huat Chuah, Ruveena Bhavani Rajaram, Lee-Ling Lim, Jeyakantha Ratnasingam, Shireene Ratna Vethakkan
Journal of Obesity & Metabolic Syndrome.2023; 32(3): 197. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk Factors
Ye Seul Yang
The Journal of Korean Diabetes.2023; 24(3): 135. CrossRef - Dyslipidemia Fact Sheet in South Korea, 2022
Eun-Sun Jin, Jee-Seon Shim, Sung Eun Kim, Jae Hyun Bae, Shinae Kang, Jong Chul Won, Min-Jeong Shin, Heung Yong Jin, Jenny Moon, Hokyou Lee, Hyeon Chang Kim, In-Kyung Jeong
Diabetes & Metabolism Journal.2023; 47(5): 632. CrossRef - 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - Riesgo residual. Conclusiones
Ángel Cequier, José Luis Zamorano
Revista Española de Cardiología Suplementos.2023; 23: 25. CrossRef - Intake of Fruit and Glycemic Control in Korean Patients with Diabetes Mellitus Using the Korea National Health and Nutrition Examination Survey
Eunju Yoon, Ji Cheol Bae, Sunghwan Suh
Endocrinology and Metabolism.2023; 38(5): 538. CrossRef - 2023 Clinical Practice Guidelines for Diabetes
Min Kyong Moon
The Journal of Korean Diabetes.2023; 24(3): 120. CrossRef - Cumulative effect of impaired fasting glucose on the risk of dementia in middle-aged and elderly people: a nationwide cohort study
Jin Yu, Kyu-Na Lee, Hun-Sung Kim, Kyungdo Han, Seung-Hwan Lee
Scientific Reports.2023;[Epub] CrossRef - Coleus forskohlii Root Extract (ForcslimTM) as a Prospective Antidiabetic Agent: In vitro Glucose Uptake Stimulation and α-Amylase Inhibitory Effects
Firoz Hirehal Hussain Mi, Channangihalli Thimmegowda Sadashiva, Neethumol Benny, Sreedrisya Ayippakkari Kuttiattu, Ravi Subban
International Journal of Pharmacology.2023; 19(5): 730. CrossRef - Comparison of on-Statin Lipid and Lipoprotein Levels for the Prediction of First Cardiovascular Event in Type 2 Diabetes Mellitus
Ji Yoon Kim, Jimi Choi, Sin Gon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2023; 47(6): 837. CrossRef - Differential Impact of Obesity on the Risk of Diabetes Development in Two Age Groups: Analysis from the National Health Screening Program
Tae Kyung Yoo, Kyung-Do Han, Yang-Hyun Kim, Ga Eun Nam, Sang Hyun Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2023; 47(6): 846. CrossRef - Associations of omega-3 fatty acids vs. fenofibrate with adverse cardiovascular outcomes in people with metabolic syndrome: propensity matched cohort study
Nam Hoon Kim, Ji Yoon Kim, Jimi Choi, Sin Gon Kim
European Heart Journal - Cardiovascular Pharmacotherapy.2023;[Epub] CrossRef - Strategies to Maintain the Remission of Diabetes Following Metabolic Surgery
Mi Kyung Kim, Hye Soon Kim
Journal of Metabolic and Bariatric Surgery.2023; 12(2): 26. CrossRef - East Asian perspectives in metabolic and bariatric surgery
Tae Jung Oh, Hyuk‐Joon Lee, Young Min Cho
Journal of Diabetes Investigation.2022; 13(5): 756. CrossRef - Recent Updates to Clinical Practice Guidelines for Diabetes Mellitus
Jin Yu, Seung-Hwan Lee, Mee Kyoung Kim
Endocrinology and Metabolism.2022; 37(1): 26. CrossRef - Association between Physical Exercise and Glycated Hemoglobin Levels in Korean Patients Diagnosed with Diabetes
Il Yun, Hye Jin Joo, Yu Shin Park, Eun-Cheol Park
International Journal of Environmental Research and Public Health.2022; 19(6): 3280. CrossRef - Effectiveness and safety of teneligliptin added to patients with type 2 diabetes inadequately controlled by oral triple combination therapy: A multicentre, randomized, double‐blind, and placebo‐controlled study
Minyoung Lee, Woo‐je Lee, Jae Hyeon Kim, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2022; 24(6): 1105. CrossRef - Trends of severe hypoglycemia in patients with type 2 diabetes in Korea: A longitudinal nationwide cohort study
Jae‐Seung Yun, Kyungdo Han, Seung‐Hyun Ko
Journal of Diabetes Investigation.2022; 13(8): 1438. CrossRef - GLP-1 receptor agonists in diabetic kidney disease: current evidence and future directions
Ji Hee Yu, So Young Park, Da Young Lee, Nan Hee Kim, Ji A Seo
Kidney Research and Clinical Practice.2022; 41(2): 136. CrossRef - Cardiorenal Risk Profiles Among Data-Driven Type 2 Diabetes Sub-Phenotypes: A Post-Hoc Analysis of the China Health and Nutrition Survey
Hui Gao, Kan Wang, Wensui Zhao, Jianlin Zhuang, Yu Jiang, Lei Zhang, Qingping Liu, Fariba Ahmadizar
Frontiers in Endocrinology.2022;[Epub] CrossRef - Individualized Medical Nutrition Therapy for Diabetic Patients according to Diabetes Medication
Juyeon Park
The Journal of Korean Diabetes.2022; 23(1): 50. CrossRef - Critical shear stress of red blood cells as a novel integrated biomarker for screening chronic kidney diseases in cases of type 2 diabetes
Il Rae Park, Jimi Choi, Eun Young Ha, Seung Min Chung, Jun Sung Moon, Sehyun Shin, Sin Gon Kim, Kyu Chang Won
Clinical Hemorheology and Microcirculation.2022; 81(4): 293. CrossRef - Effects of exercise on reducing diabetes risk in Korean women according to menopausal status
Jung-Hwan Cho, Hye-Mi Kwon, Se-Eun Park, Ju-Hwan Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Prevention and Pharmacotherapy.2022; 4(2): 75. CrossRef - Novel Glycemic Index Based on Continuous Glucose Monitoring to Predict Poor Clinical Outcomes in Critically Ill Patients: A Pilot Study
Eun Yeong Ha, Seung Min Chung, Il Rae Park, Yin Young Lee, Eun Young Choi, Jun Sung Moon
Frontiers in Endocrinology.2022;[Epub] CrossRef - Free Versus Fixed-Ratio Combination of Basal Insulin and GLP-1 Receptor Agonists in Type 2 Diabetes Uncontrolled With GLP-1 Receptor Agonists: A Systematic Review and Indirect Treatment Comparison
Han Na Jung, Yun Kyung Cho, Se Hee Min, Hwi Seung Kim, Ye-Jee Kim, Joong-Yeol Park, Woo Je Lee, Chang Hee Jung
Frontiers in Endocrinology.2022;[Epub] CrossRef - Obesity, hypertension, diabetes mellitus, and hypercholesterolemia in Korean adults before and during the COVID-19 pandemic: a special report of the 2020 Korea National Health and Nutrition Examination Survey
Ga Bin Lee, Yoonjung Kim, Suyeon Park, Hyeon Chang Kim, Kyungwon Oh
Epidemiology and Health.2022; 44: e2022041. CrossRef - Adherence to healthy lifestyle behaviors as a preventable risk factor for severe hypoglycemia in people with type 2 diabetes: A longitudinal nationwide cohort study
Jae‐Seung Yun, Kyungdo Han, Yong‐Moon Park, Eugene Han, Yong‐ho Lee, Seung‐Hyun Ko
Journal of Diabetes Investigation.2022; 13(9): 1533. CrossRef - Diabetes Fact Sheet in Korea 2021
Jae Hyun Bae, Kyung-Do Han, Seung-Hyun Ko, Ye Seul Yang, Jong Han Choi, Kyung Mook Choi, Hyuk-Sang Kwon, Kyu Chang Won
Diabetes & Metabolism Journal.2022; 46(3): 417. CrossRef - Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hyperte
Jong Han Choi, Jee-Hyun Kang, Suk Chon
Diabetes & Metabolism Journal.2022; 46(3): 377. CrossRef - Effect of Carbohydrate-Restricted Diets and Intermittent Fasting on Obesity, Type 2 Diabetes Mellitus, and Hypertension Management: Consensus Statement of the Korean Society for the Study of Obesity, Korean Diabetes Association, and Korean Society of Hype
Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim
Diabetes & Metabolism Journal.2022; 46(3): 355. CrossRef - Effect of carbohydrate-restricted diets and intermittent fasting on obesity, type 2 diabetes mellitus, and hypertension management: consensus statement of the Korean Society for the Study of obesity, Korean Diabetes Association, and Korean Society of Hype
Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim
Clinical Hypertension.2022;[Epub] CrossRef - Efficacy of Personalized Diabetes Self-care Using an Electronic Medical Record–Integrated Mobile App in Patients With Type 2 Diabetes: 6-Month Randomized Controlled Trial
Eun Young Lee, Seon-Ah Cha, Jae-Seung Yun, Sun-Young Lim, Jin-Hee Lee, Yu-Bae Ahn, Kun-Ho Yoon, Min Kyung Hyun, Seung-Hyun Ko
Journal of Medical Internet Research.2022; 24(7): e37430. CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - Hypoglycemic agents and glycemic variability in individuals with type 2 diabetes: A systematic review and network meta-analysis
SuA Oh, Sujata Purja, Hocheol Shin, Minji Kim, Eunyoung Kim
Diabetes and Vascular Disease Research.2022; 19(3): 147916412211068. CrossRef - Tolerability and Effectiveness of Switching to Dulaglutide in Patients With Type 2 Diabetes Inadequately Controlled With Insulin Therapy
Youngsook Kim, Ji Hye Huh, Minyoung Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Frontiers in Endocrinology.2022;[Epub] CrossRef - Factors Influencing the Utilization of Diabetes Complication Tests Under the COVID-19 Pandemic: Machine Learning Approach
Haewon Byeon
Frontiers in Endocrinology.2022;[Epub] CrossRef - Association of prediabetes with death and diabetic complications in older adults: the pros and cons of active screening for prediabetes
Giwoong Choi, Hojun Yoon, Hyun Ho Choi, Kyoung Hwa Ha, Dae Jung Kim
Age and Ageing.2022;[Epub] CrossRef - Recent information on test utilization and intraindividual change in anti-glutamic acid decarboxylase antibody in Korea: a retrospective study
Rihwa Choi, Wonseo Park, Gayoung Chun, Jiwon Lee, Sang Gon Lee, Eun Hee Lee
BMJ Open Diabetes Research & Care.2022; 10(3): e002739. CrossRef - Extra-Glycemic Effects of Anti-Diabetic Medications: Two Birds with One Stone?
Eun-Jung Rhee
Endocrinology and Metabolism.2022; 37(3): 415. CrossRef - Pharmacological Treatment of Nonalcoholic Fatty Liver Disease: Antidiabetic Agents
Kyung-Soo Kim
The Journal of Korean Diabetes.2022; 23(2): 83. CrossRef - Maintaining Physical Activity Is Associated with Reduced Major Adverse Cardiovascular Events in People Newly Diagnosed with Diabetes
Duhoe Kim, Jaehun Seo, Kyoung Hwa Ha, Dae Jung Kim
Journal of Obesity & Metabolic Syndrome.2022; 31(2): 187. CrossRef - Effect of Carbohydrate-Restricted Diets and Intermittent Fasting on Obesity, Type 2 Diabetes Mellitus, and Hypertension Management: Consensus Statement of the Korean Society for the Study of Obesity, Korean Diabetes Association, and Korean Society of Hype
Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim
Journal of Obesity & Metabolic Syndrome.2022; 31(2): 100. CrossRef - Advanced Glycation End Products and Their Effect on Vascular Complications in Type 2 Diabetes Mellitus
Jeongmin Lee, Jae-Seung Yun, Seung-Hyun Ko
Nutrients.2022; 14(15): 3086. CrossRef - Severe hypoglycemia as a risk factor for cardiovascular outcomes in patients with type 2 diabetes: is it preventable?
Seung-Hyun Ko
Cardiovascular Prevention and Pharmacotherapy.2022; 4(3): 106. CrossRef - New, Novel Lipid-Lowering Agents for Reducing Cardiovascular Risk: Beyond Statins
Kyuho Kim, Henry N. Ginsberg, Sung Hee Choi
Diabetes & Metabolism Journal.2022; 46(4): 517. CrossRef - Current status of obesity treatment in Korea: based on the 2020 Korean Society for the Study of Obesity guidelines for obesity management
Eun-Jung Rhee
Journal of the Korean Medical Association.2022; 65(7): 388. CrossRef - Experiences of Using Wearable Continuous Glucose Monitors in Adults With Diabetes: A Qualitative Descriptive Study
Hee Sun Kang, Hyang Rang Park, Chun-Ja Kim, Savitri Singh-Carlson
The Science of Diabetes Self-Management and Care.2022; 48(5): 362. CrossRef - 젊은 2형 당뇨병 환자의 관리
재현 배
Public Health Weekly Report.2022; 15(35): 2474. CrossRef - Real-World Prescription Patterns and Barriers Related to the Use of Sodium-Glucose Cotransporter 2 Inhibitors among Korean Patients with Type 2 Diabetes Mellitus and Cardiovascular Disease
Jong Ha Baek, Ye Seul Yang, Seung-Hyun Ko, Kyung Do Han, Jae Hyeon Kim, Min Kyong Moon, Jong Suk Park, Byung-Wan Lee, Tae Jung Oh, Suk Chon, Jong Han Choi, Kyu Yeon Hur
Diabetes & Metabolism Journal.2022; 46(5): 701. CrossRef - Low-Density Lipoprotein Cholesterol Level, Statin Use and Myocardial Infarction Risk in Young Adults
Heekyoung Jeong, Kyungdo Han, Soon Jib Yoo, Mee Kyoung Kim
Journal of Lipid and Atherosclerosis.2022; 11(3): 288. CrossRef - Blood Pressure Target in Type 2 Diabetes Mellitus
Hyun-Jin Kim, Kwang-il Kim
Diabetes & Metabolism Journal.2022; 46(5): 667. CrossRef - Association of underweight status with the risk of tuberculosis: a nationwide population-based cohort study
Su Hwan Cho, Hyun Lee, Hyuktae Kwon, Dong Wook Shin, Hee-Kyung Joh, Kyungdo Han, Jin Ho Park, Belong Cho
Scientific Reports.2022;[Epub] CrossRef - Exploring the risk factors of impaired fasting glucose in middle-aged population living in South Korean communities by using categorical boosting machine
Haewon Byeon
Frontiers in Endocrinology.2022;[Epub] CrossRef - External validation and clinical application of the predictive model for severe hypoglycemia
Jae-Seung Yun, Kyungdo Han, Soo-Yeon Choi, Seon-Ah Cha, Yu-Bae Ahn, Seung-Hyun Ko
Frontiers in Endocrinology.2022;[Epub] CrossRef - Effect of Euonymus alatus Extracts on Diabetes Related Markers in Pancreatic β-Cells and C57BL/Ksj-db/db Mice
Ye Rin Kim, Eun-young Kim, Seong Uk Lee, Young Wan Kim, Yoon Hee Kim
Journal of the Korean Society of Food Science and Nutrition.2022; 51(9): 894. CrossRef - Muscle fat contents rather than muscle mass determines nonalcoholic steatohepatitis and liver fibrosis in patients with severe obesity
Eugene Han, Mi Kyung Kim, Hye Won Lee, Seungwan Ryu, Hye Soon Kim, Byoung Kuk Jang, Youngsung Suh
Obesity.2022; 30(12): 2440. CrossRef - Correlation between shift work and non-alcoholic fatty liver disease among male workers in the steel manufacturing company of Korea: a cross-sectional study
Kiseok Kim, Yong-Jin Lee, Soon-Chan Kwon, Young-Sun Min, Hyun Kyo Lee, Gwangin Baek, Sang Hyeon Kim, Eun-Chul Jang
Annals of Occupational and Environmental Medicine.2022;[Epub] CrossRef - FGM-based remote intervention for adults with type 1 diabetes: The FRIEND randomized clinical trial
Jinju Lee, Myeong Hoon Lee, Jiyun Park, Kyung-Soo Kim, Soo-Kyung Kim, Yong-Wook Cho, Hyun Wook Han, Young Shin Song
Frontiers in Endocrinology.2022;[Epub] CrossRef - Screening for Prediabetes and Diabetes in Korean Nonpregnant Adults: A Position Statement of the Korean Diabetes Association, 2022
Kyung Ae Lee, Dae Jung Kim, Kyungdo Han, Suk Chon, Min Kyong Moon
Diabetes & Metabolism Journal.2022; 46(6): 819. CrossRef - Blood Pressure Control in Patients with Diabetic Kidney Disease
Yaeni Kim, Won Kim, Jwa-Kyung Kim, Ju Young Moon, Samel Park, Cheol Whee Park, Hoon Suk Park, Sang Heon Song, Tae-Hyun Yoo, So-Young Lee, Eun Young Lee, Jeonghwan Lee, Kyubok Jin, Dae Ryong Cha, Jin Joo Cha, Sang Youb Han
Electrolytes & Blood Pressure.2022; 20(2): 39. CrossRef - The Gangwon Obesity and Metabolic Syndrome Study: Methods and Initial Baseline Data
Yoon Jeong Cho, Sohyun Park, Sung Soo Kim, Hyo Jin Park, Jang Won Son, Tae Kyung Lee, Sangmo Hong, Jee-Hyun Kang, Seon Mee Kim, Yang-Hyun Kim, Won Jun Kim, Young Eun Seo, Yoosuk An, Sang Youl Rhee, Suk Chon, Sookyoung Jeon, Kyungho Park, Bong-Soo Kim, Cha
Journal of Obesity & Metabolic Syndrome.2022; 31(4): 303. CrossRef - Oral Semaglutide, the First Ingestible Glucagon-Like Peptide-1 Receptor Agonist: Could It Be a Magic Bullet for Type 2 Diabetes?
Hwi Seung Kim, Chang Hee Jung
International Journal of Molecular Sciences.2021; 22(18): 9936. CrossRef - Long-term effectiveness and safety of quadruple combination therapy with empagliflozin versus dapagliflozin in patients with type 2 diabetes: 3-year prospective observational study
Eu Jeong Ku, Dong-Hwa Lee, Hyun Jeong Jeon, Tae Keun Oh
Diabetes Research and Clinical Practice.2021; 182: 109123. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2021;45:698-707)
Mi-kyung Kim
Diabetes & Metabolism Journal.2021; 45(6): 968. CrossRef - Incidence and Risk Factors for Progression to Diabetes Mellitus: A Retrospective Cohort Study
Min Kyung Hyun, Jong Heon Park, Kyoung Hoon Kim, Soon-Ki Ahn, Seon Mi Ji
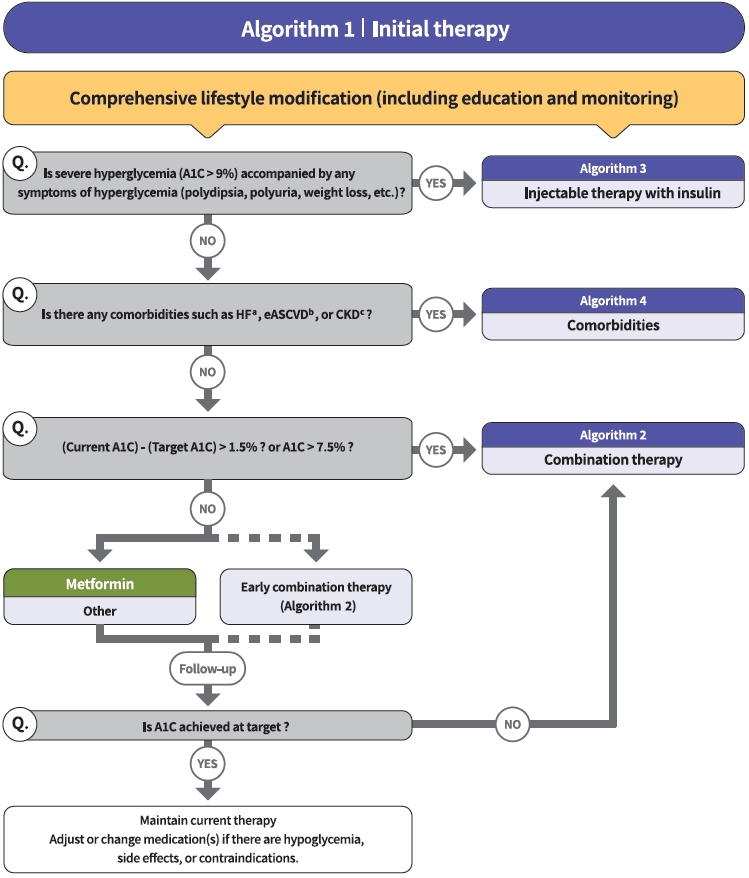
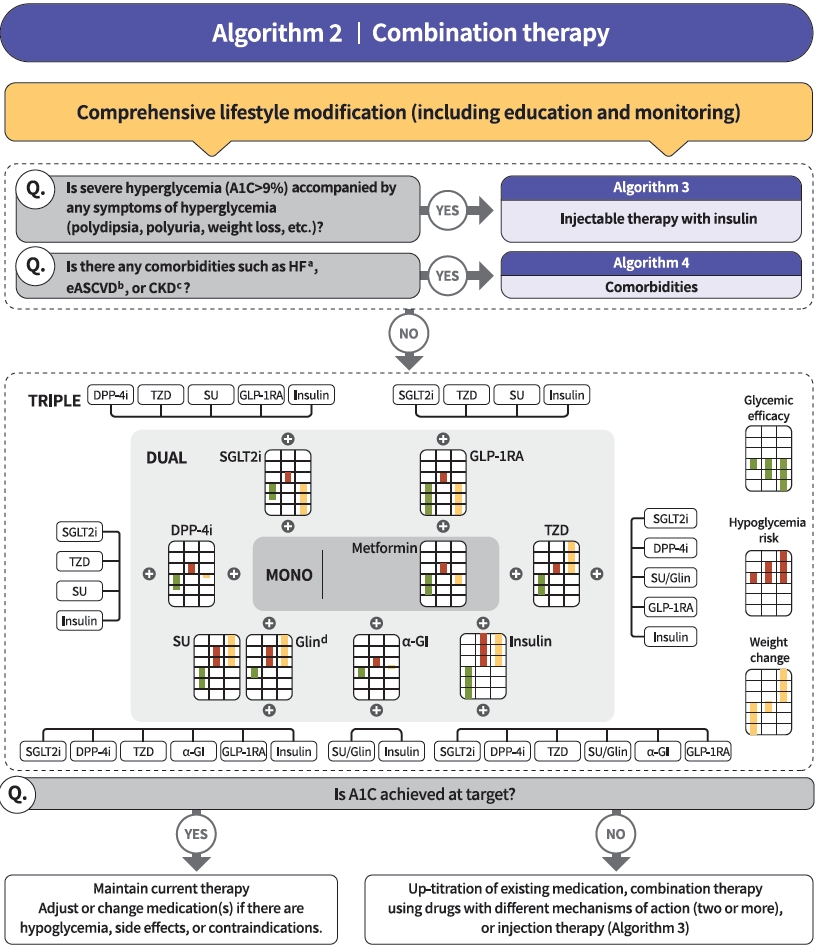
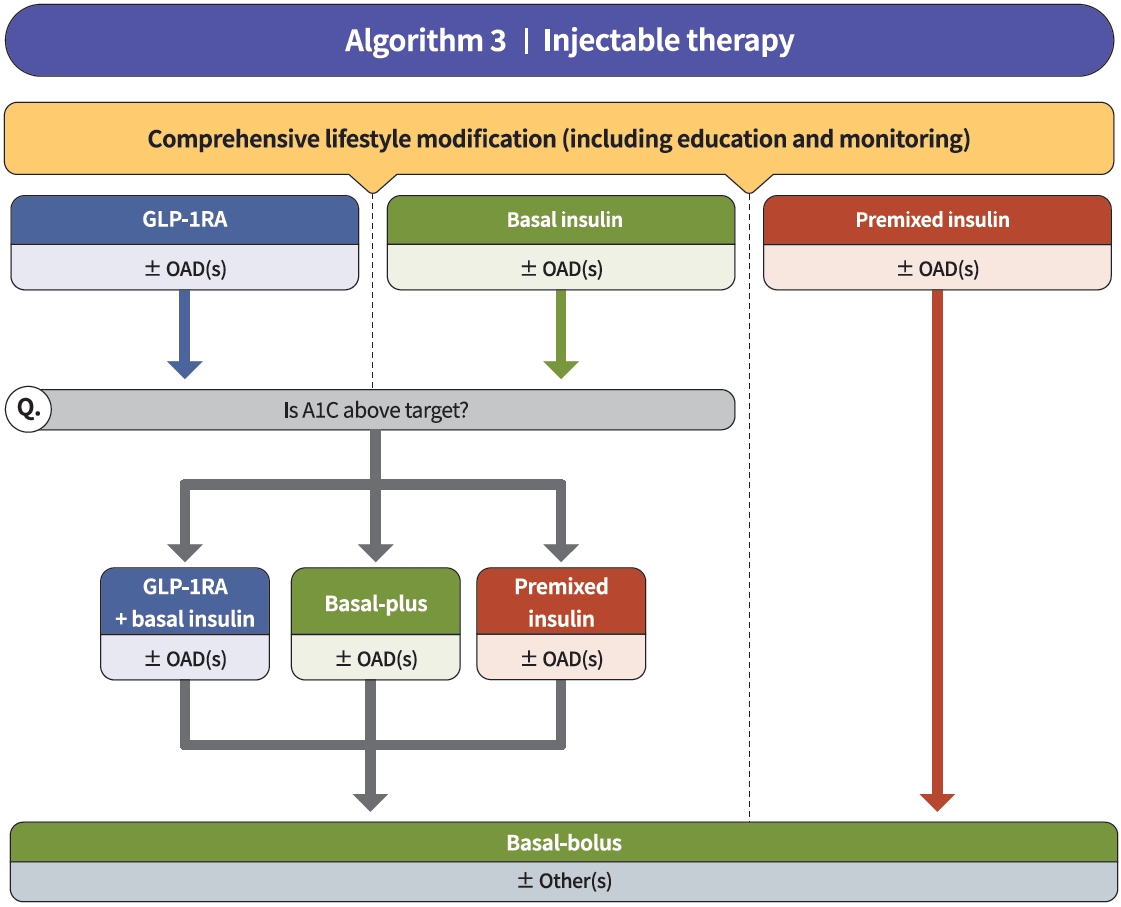
International Journal of Environmental Research and Public Health.2021; 19(1): 123. CrossRef - 2021 Clinical Practice Guidelines for Diabetes: Pharmacotherapy and the Korean Diabetes Association Support System
Kyu Yeon Hur
The Journal of Korean Diabetes.2021; 22(4): 250. CrossRef - 2021 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk
Min Kyong Moon
The Journal of Korean Diabetes.2021; 22(4): 259. CrossRef

 KDA
KDA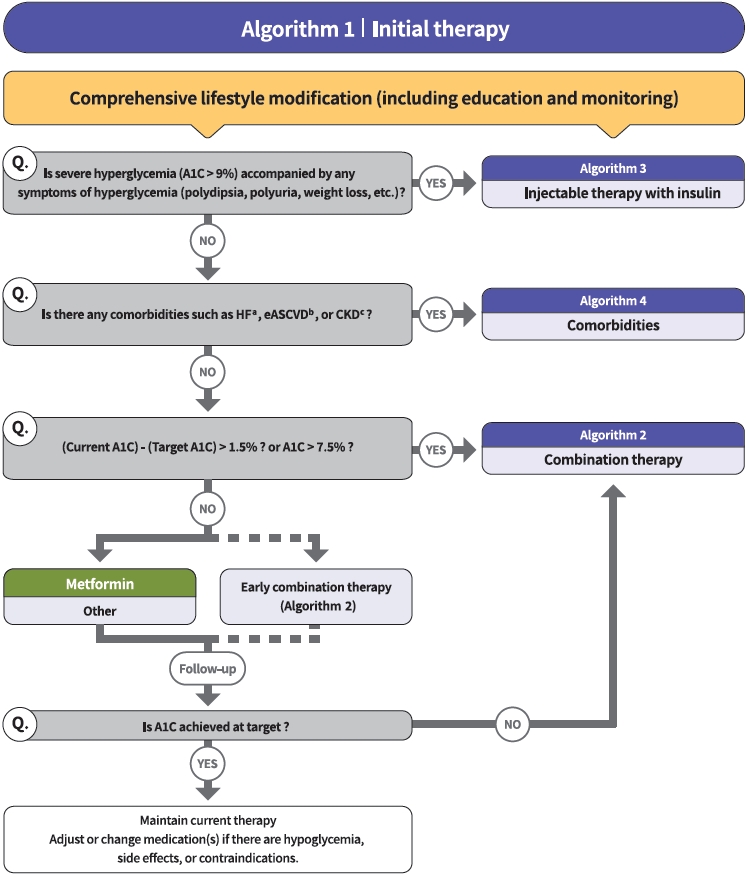

 PubReader
PubReader ePub Link
ePub Link Cite
Cite