- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 38(2); 2014 > Article
-
Original ArticleClinical Care/Education The Appropriateness of the Length of Insulin Needles Based on Determination of Skin and Subcutaneous Fat Thickness in the Abdomen and Upper Arm in Patients with Type 2 Diabetes
- Kang Hee Sim1, Moon Sook Hwang2, Sun Young Kim1, Hye Mi Lee1, Ji Yeun Chang3, Moon Kyu Lee4
-
Diabetes & Metabolism Journal 2014;38(2):120-133.
DOI: https://doi.org/10.4093/dmj.2014.38.2.120
Published online: April 18, 2014
1Department of Nursing, Samsung Medical Center, Seoul, Korea.
2Department of Nursing Science, Woo Suk University, Wanju, Korea.
3Department of Internal Medicine, Seoul St. Mary's Hospital, Seoul, Korea.
4Division of Endocrinology and Metabolism, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- Corresponding author: Moon Sook Hwang. Department of Nursing Science, WooSuk University, 443 Samnye-ro, Wanju-gun 565-701, Korea. msyellow45@hanmail.net
Copyright © 2014 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- Longer needle and complicated insulin injection technique such as injecting at a 45-degree angle and making skinfolds may decrease patient compliance to insulin injection therapy. In this light, shorter insulin needles have been recently developed. However, it is necessary to ascertain that such shorter needles are appropriate for Korean patients with diabetes as well.
-
Methods
- First, the diverse demographic and diabetic features of 156 Korean adults with diabetes were collected by a questionnaire and a device unit of body fat measurement. The skin and subcutaneous fat thicknesses of each subject were measured by Ultrasound device with a 7- to 12-MHz probe. Data were analyzed using analysis of variance and multiple linear regression.
-
Results
- The mean skin thickness was 2.29±0.37 mm in the abdomen and 2.00±0.34 mm in the upper arms, and the mean subcutaneous fat thickness was to 10.15±6.54 mm in the abdomen and 5.50±2.68 mm in the upper arms. Our analysis showed that the factors affecting the skin thickness of the abdomen and upper arms were gender and body mass index (BMI), whereas the factors influencing the subcutaneous fat thickness in the abdomen were gender and BMI, and the factors influencing the subcutaneous fat thickness in the upper arms were gender, BMI, and age. Insulin fluids may not appear to be intradermally injected into the abdomen and upper arms at any needle lengths. The risk of intramuscular injection is likely to increase with longer insulin needles and lower BMI.
-
Conclusion
- It is recommended to fully inform the patients about the lengths of needles for insulin injections. As for the recommended needle length, the findings of this study indicate that needles as short as 4 mm are sufficient to deliver insulin for Korean patients with diabetes.
- Insulin treatments are necessary for sugar control not only in type 1 diabetes mellitus (T1DM) patients, but also in type 2 diabetes mellitus (T2DM) patients. As for insulin injections, an intramuscular injection leads to a faster absorption than the desirable rate, while intradermal injection causes insulin leakage and pain, for which reasons insulin must be injected not into the muscles, dermis, and nerves, but into the subcutaneous tissue [1]. However the subcutaneous tissue thickness of patients varies depending on the age, gender, body mass index (BMI), and parts of the body [2,3], and the injected subcutaneous area depends on the length of a needle [4]. Therefore, before an insulin injection, the injection site, the subcutaneous fat thickness, the injection method, the length of the needle, and other psychological factors must be considered.
- Yet, nurses constantly trained patients to inject insulin to diabetic patients with needles of the same length, regardless of the skin and subcutaneous adipose layer thicknesses [4], and most patients inject insulin themselves with the syringes that they were trained with. Currently 8-mm needle syringes are used to inject insulin in clinical settings, and because these needles are long, people are trained to either inject insulin at 45-degree angle or after making skinfolds.
- Gibney et al. [3] reported that 15% of the content was injected into the muscles when injecting normal saline with 8-mm long needles. In such a way, if diabetic patients are injected with insulin with an 8-mm long needle, a fair amount of the insulin may be injected into the muscular layer. This is more likely in pregnant women who avoid intraperitoneal injections and tend to inject insulin into the upper arm, where creating skinfold is extremely difficult by themselves, and therefore it is much more likely for them to inject insulin into the muscles instead during self-injections. If insulin is injected to the highly vascularized muscles, the absorption rate becomes much quicker, leading to fluctuations in sugar control and hence bringing about predicaments such as difficulties in estimating the reaction to hypoglycemia [5,6], while intracutaneous injections engenders insulin leakage and subsequent skin damage [6]. Therefore, in order to inject insulin into the subcutaneous adipose layer, some measure of injection techniques such as choice of injection site, injection angle, creating skinfolds, etc. are required, but such complexities reduce compliance to insulin injections, for which reason simplifying the injection skills is necessary. Extra care is demanded especially when training the annually increasing number of old diabetic patients [7].
- In this context, usage of short needles that can inject insulin into the subcutaneous adipose layer at right angles are recommended [3,8,9], and recently needles of different lengths have been developed and used such as 4-mm needle syringes. However, obese patients are recommended to use longer needles in order to reach the desired depth [10]. Collectively, measuring the skin and subcutaneous adipose layer thicknesses and identifying by which factors these thicknesses are affected, and therefore selecting the appropriate injection sites and needle length in diabetic patients in need of insulin injections is needed.
- However, no studies have measured the skin and subcutaneous thicknesses of Korean diabetic patients yet, and therefore it is not yet possible to determine which needle length is appropriate. In addition, because insulin is repeatedly injected into a confined area, conditions that lead either to the shrinkage or enlargement of the subcutaneous tissue of the injection sites, such as lipodystrophy, occurs. Therefore, patients are educated to inject insulin at least 2 inches away from the navel, and use the insulin injection chart which they can refer to and circulate around each site with at least a 1- to 2-cm gap between injections [1]. Unfortunately, although most diabetic patients claim to comply with the instructions and circulate in between each injection [11], according to a preliminary investigation of this study, virtually none of the patients used the full injection sites available. Hence, a study that presents the skin and subcutaneous fat thicknesses of all the available injection sites on the abdomen and upper arm should be conducted to provide the patients with stronger evidence to motivate them to circulate around all injection sites.
- Many studies regarding the skin and subcutaneous fat thicknesses [3,12] and insulin syringe needle length [3,5,8,13] have already been published not only from abroad, but endemic studies also exist regarding the skin thickness [14,15], subcutaneous fat thickness [4,16,17,18], and needle length [2]. Even so, a major drawback remains that even if it is the same abdomen or upper arm, the subcutaneous fat thickness can vary depending on where it was measured [17]. Despite this knowledge, other studies claim that a measurement from only one spot on the abdomen and upper arm represents the subcutaneous fat thickness throughout the respective body part. Not only is this insufficient to be used as an back-up evidence to encourage patients to circulate around the injection sites, but not even a single study exist investigating the appropriate insulin syringe needle length.
- The main objective of this research is to inspect the skin, subcutaneous fat, and the total skin and subcutaneous fat thicknesses of the abdominal and upper arm of diabetic patients and elucidate the underlying factors affecting these thicknesses, so that we can determine the availability of using different length needles on the base of measured skin and subcutaneous fat thicknesses.
INTRODUCTION
- Research subjects
- Subjects who were diagnosed with diabetes more than 1 year ago were selected based on the following criteria:
-
Those who do not have any muscular or neural diseases at the sites of insulin injection on the abdomen and upper arm
Those who do not have any skin damage, such as wart, contusion, or brush-burns, at the sites of ultrasound measurements on the abdomen and upper arm
Those who are not using an insulin pump at the sites of ultrasound measurements on the abdomen and upper arm
Those who do not have diseases that may affect the skin thickness, such as malignant tumor or collagen diseases
Those who were not treated with steroids for a prolonged period of time
Those who have fully understood the objectives of this research and can communicate, as well as being able to sign the agreements to participate
- Subjects were chosen from those who have read the brochure attached outside the Department of Internal Medicine in Samsung Medical Center and met our criteria for selection. They were notified of the objectives of this research and were explained that they were able to drop out at any point during the research without any disadvantages, and we obtained signed agreements to participate in the research from the subjects.
- According to the G Power 3 program, in order to acquire a sample number appropriate for the regression analysis that was used in this study, we set the effect size as 0.15, the significance level as 0.05, the test power as 0.95, and the predictive factor as 5, after which we were able to calculate a sample size of 138 for this study. After considering a dropout rate of 10%, we recruited 160 subjects and attempted to recruit at least 25% of patients who injected insulin. As a result, we enrolled 163 subjects, of which one who lacked sociodemographic data and six who were under the age of 18 were excluded, leaving us with 156 for the study, of which 52 (33.3%) were confirmed to take insulin injections.
- Methods
- BMI calculates the obesity rate by dividing weight (kg) by the square of their height (m2) [1]. This research used a body fat analyzer (InBody 230; Biospace, Seoul, Korea) to measure BMI, which was used to divide the subjects into under-weight (<18.5), normal-weight (18.5 to <23), over-weight (23 to <25), obese (25 to ≤30), and hyperobese (≥30) groups for further analysis [10].
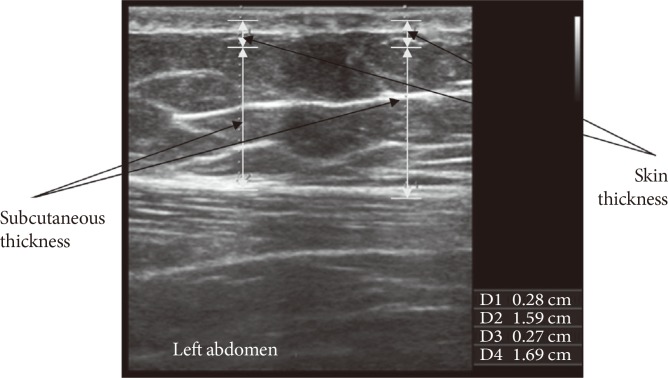
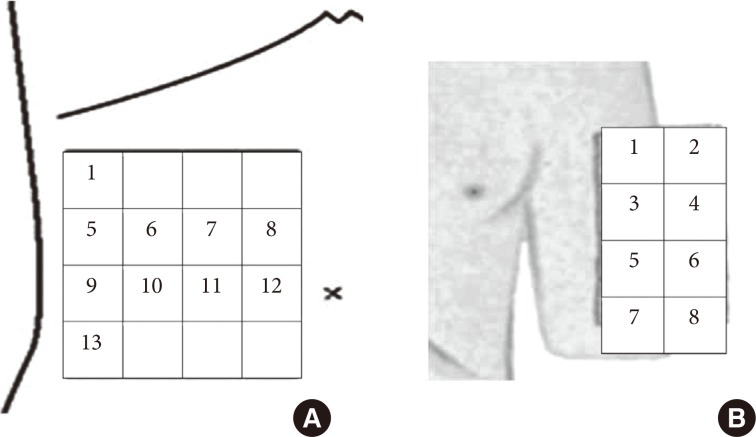
- In this study, the skin thickness was defined as the total thickness of the epidermis and dermis, the subcutaneous fat thickness as the thickness of the subcutaneous tissue, and the total skin and subcutaneous fat thickness as the sum of skin thickness and subcutaneous fat thickness. The skin and subcutaneous fat thicknesses are measured by an ultrasound equipment (Accuvix XG; Samsung Medison, Seoul, Korea) in mm as shown in Fig. 1. The sites where abdominal and brachial skin and subcutaneous fat thicknesses were chosen using an injection site chart created by Sim et al. [19], as shown in Fig. 2. The location of the abdomen is indicated by the total of 10 points which consists of 8 points on the 2nd and 3rd lines and the top and bottom points on the far left side. The location of the upper arm is indicated by the total of 8 points in the 2 columns.
- The measurement sites were chosen based on a previous survey in which diabetic patients answered that insulin was injected from one side to the other, resulting in 2 lines in the abdomen, whereas insulin was injected from top to bottom, resulting in 2 columns in the upper arm. The 2 points on the top and bottom at the far left were added to identify the minimal subcutaneous fat thickness in the abdomen, and preliminary investigations showed that the subcutaneous fat was thinnest in these places.
- Because insulin must be injected into subcutaneous fat, the possibility of intracutaneous insulin injection in the abdomen and upper arm was confirmed by estimating the potential risks of intradermal injection and intramuscular injection. To be more concrete, as for the risk of intradermal injections for different needle lengths, we defined that it was dangerous if the needle length was shorter than the skin thickness, and as for the risk of intramuscular injections, we defined it to be dangerous if the needle length was longer than the total skin and subcutaneous fat thickness on the assumption that insulin was injected at a right angle and that no skinfolds were made.
- Data collection
- This research was approved by the Institutional Ethics Review Board of Samsung Medical Center in November 2012 (IRB number, 2012-09-018-004) and met the guidelines of the Helsinki Declaration and Good Clinical Practice. The data were collected over 4 days from November 2012 to December 2012. Normal and disease related characteristics were investigated by a survey after obtaining written informed consent, and BMI was measured using a body fat analyzer (InBody 230) after the completion of the survey. The skin and subcutaneous fat thicknesses were measured only from one side under the assumption that the left and right sides were symmetrical. In the order of subjects' BMI measurements, we measured the thicknesses of even-number patients from the right side and the odd-number patients from the left side.
- Next, subjects were escorted for ultrasound measurements, and two sonographers measured their skin and subcutaneous thicknesses. The sonographers were certified by the Ministry of Health and Welfare for ultrasound imaging and have had over 3 years of clinical experience. For consistency, measurements were calibrated and the machine was tested for normality in between each subjects, and to reduce the variability from measurement sites, each subjects had a location chart place above their abdomen and upper arm during the measurement. Furthermore, in order to acquire clear and accurate ultrasound images, a gel was applied to the ultrasound probe, it was placed at a right angle above the desired location in the location chart, and the skin and subcutaneous fat thicknesses were measured with 10 MHz as the basic frequency. If the boundary between the skin and subcutaneous fat was not clear, the frequency was altered in the range of 7 to 12 MHz. During the thickness measurement the sonographers applied a transducer on the skin to prevent the tissues from being compressed by the probe. By scanning within the range of the desired location, the thickness was measured by the automated machine after point where each thicknesses were constant was identified.
- Data analysis
- The normal characteristics of subjects were analyzed in percentages in case of categorical variables or by mean±standard deviations (SD) in case of continuous variables. The skin and subcutaneous fat thicknesses and the total skin and subcutaneous fat thickness were measured in mm and were presented in mean±SD, where the total skin and subcutaneous fat thickness was the sum of skin thickness and subcutaneous fat thickness. The differences in the skin and subcutaneous fat thicknesses and the total skin and subcutaneous fat thickness depending on the normal characteristics or BMI were analyzed by analysis of variance and then confirmed by Scheffe test, and the effects of confounding variables (gender, age, and BMI) on the skin and subcutaneous fat thicknesses and the total skin and subcutaneous fat thickness in different injection sites were analyzed by multiple regression analysis. Finally, we defined that there is a risk for intradermal injection if the needle length was shorter than the skin thickness, and we defined that there is a risk of intramuscular injection if the needle length was longer than the total skin and subcutaneous fat thickness, and these were analyzed in frequency and percentage. All significance level was set at 0.05.
METHODS
Skin, subcutaneous fat, and the total skin and subcutaneous fat thicknesses
Possibility of intracutaneous insulin injection
- The clinical characteristics of subjects
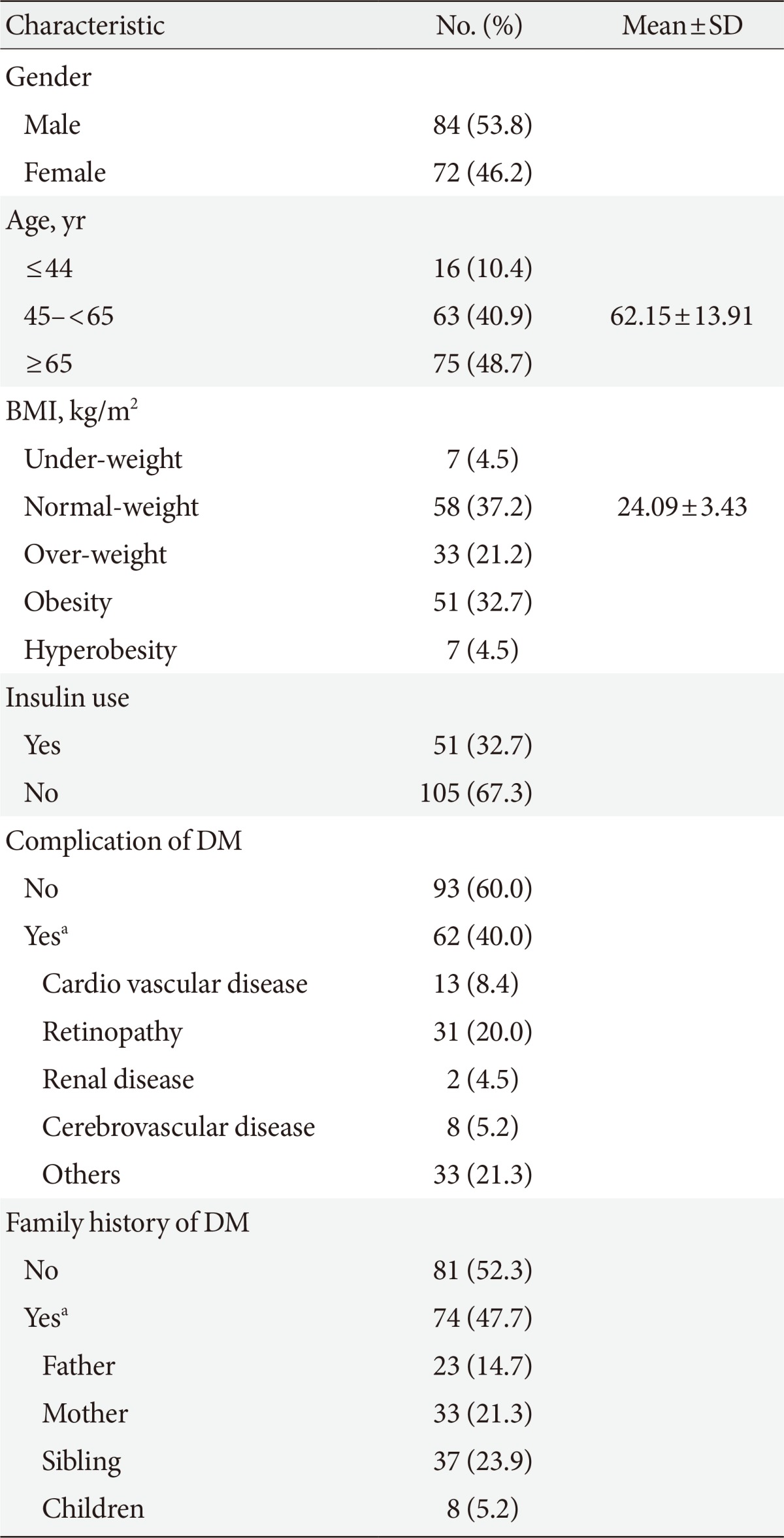
- The clinical characteristics of the subjects are shown in Table 1. The mean age was 62.15±13.91 and 53.8% were male. Their average BMI was 24.09±3.43, with 58.4% of the subjects in the over-weight group. Fifty-one patients (32.7%) used insulin for sugar control, 62 (40.0%) had complications due to diabetes, and 74 (47.7%) had a family history of diabetes.
- The skin and subcutaneous fat thicknesses
- The skin and subcutaneous fat thicknesses and the total skin and subcutaneous fat thickness of the abdomen depending on injection sites are shown in Table 2, with the thickness of the skin of 2.29±0.37 mm (range, 1.34 to 3.29 mm), thickness of subcutaneous fat of 10.15±6.54 mm (range, 0.75 to 36.34 mm), and the total skin and subcutaneous fat thickness of 12.44±6.56 mm (range, 2.24 to 38.24 mm).
- The thickest point of the skin in the abdomen was 7 for males and 8 for females, whereas the thinnest point was 13 for both. The skin thickness range was 1.20 to 3.80 mm and 1.00 to 3.80 mm for males and females, respectively.
- The thickest point of the subcutaneous fat and the total thickness of skin and subcutaneous fat in the abdomen was 12 for both males and females, while the thinnest point was 13 for both. The subcutaneous fat thickness range was 0.40 to 36.30 mm and 0.20 to 39.40 mm for males and females, respectively, and the total thickness of skin and subcutaneous fat range was 1.80 to 38.30 mm and 1.70 to 41.30 mm for males and females, respectively.
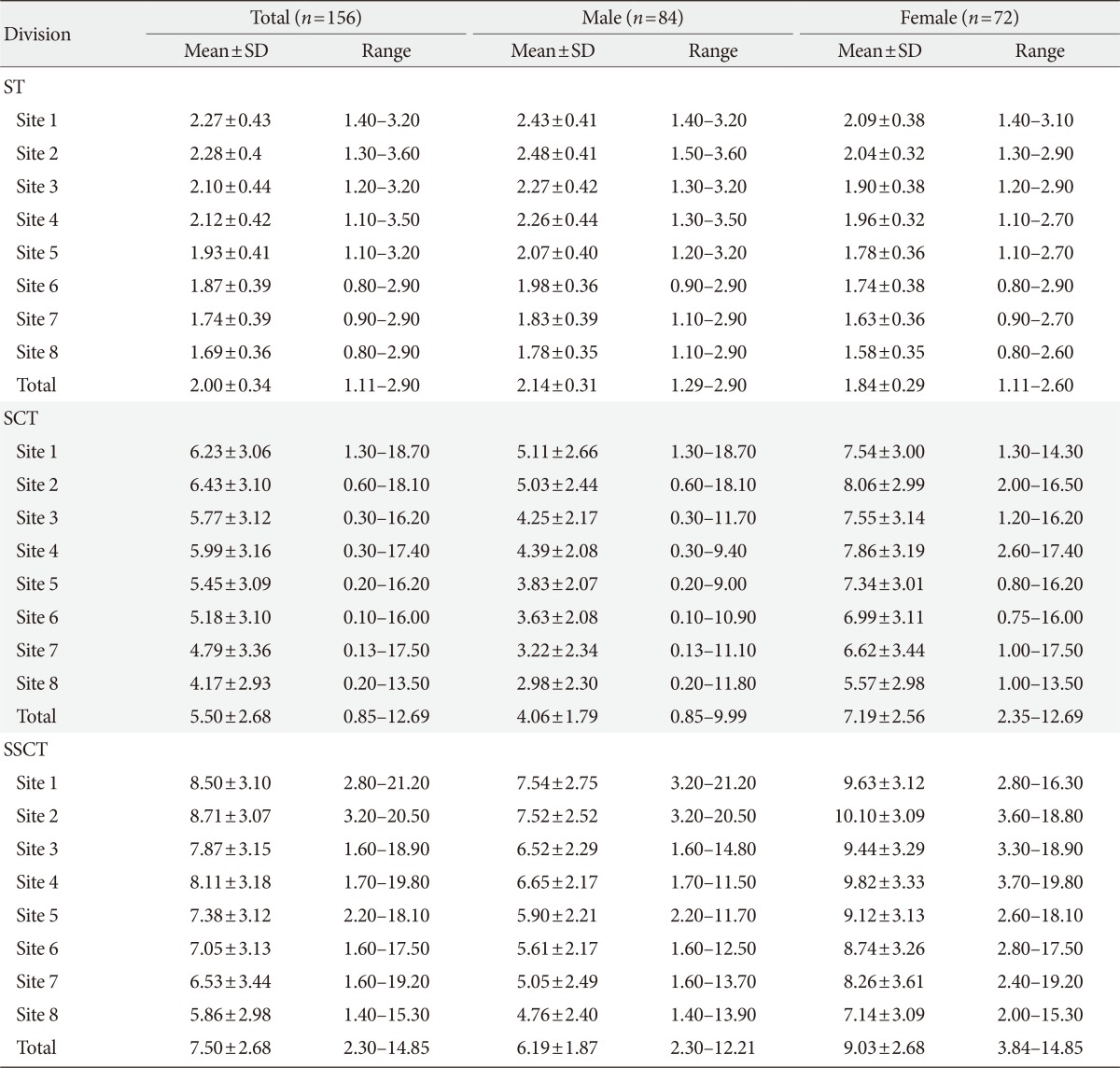
- The skin and subcutaneous fat thicknesses
- The skin and subcutaneous fat thicknesses and the total skin and subcutaneous fat thickness of the upper arm depending on injection sites are shown in Table 3, with the average (range) skin thickness 2.00±0.34 mm (range, 1.11 to 2.90 mm), subcutaneous fat thickness of 5.50±2.68 mm (range, 0.85 to 12.69 mm), and the total skin and subcutaneous fat thickness of 7.50±2.68 mm (range, 2.30 to 14.85 mm).
- The thickest location of the skin in the upper arm was 2 for males and 1 for females, while the thinnest point was 8 for both. The skin thickness range was 0.90 to 3.60 mm and 0.80 to 3.10 mm for males and females, respectively.
- The thickest point of the subcutaneous fat and the total thickness of skin and subcutaneous fat in the upper arm was 1 for males and 2 for females, while the thinnest point was 8 for both. The subcutaneous fat thickness range was 0.10 to 18.70 mm and 0.75 to 17.50 mm for males and females, respectively, and the total thickness of skin and subcutaneous fat range was 1.40 to 21.20 mm and 2.00 to 19.80 mm for males and females, respectively.
- The differences in the skin and subcutaneous fat thicknesses
- The differences in the skin and subcutaneous fat thicknesses and the total skin and subcutaneous fat thickness of the abdomen and upper arm depending on normal characteristics are shown in Table 4. Our analysis indicated that the abdominal and brachial skin, subcutaneous fat and the total of the two were thicker in females compared to male (P<0.05), as well as the thickness increasing with higher BMI (P<0.05), with statistical significance. However, age, use of insulin, family history of diabetes, or complications due to diabetes did not show any significant relevance.
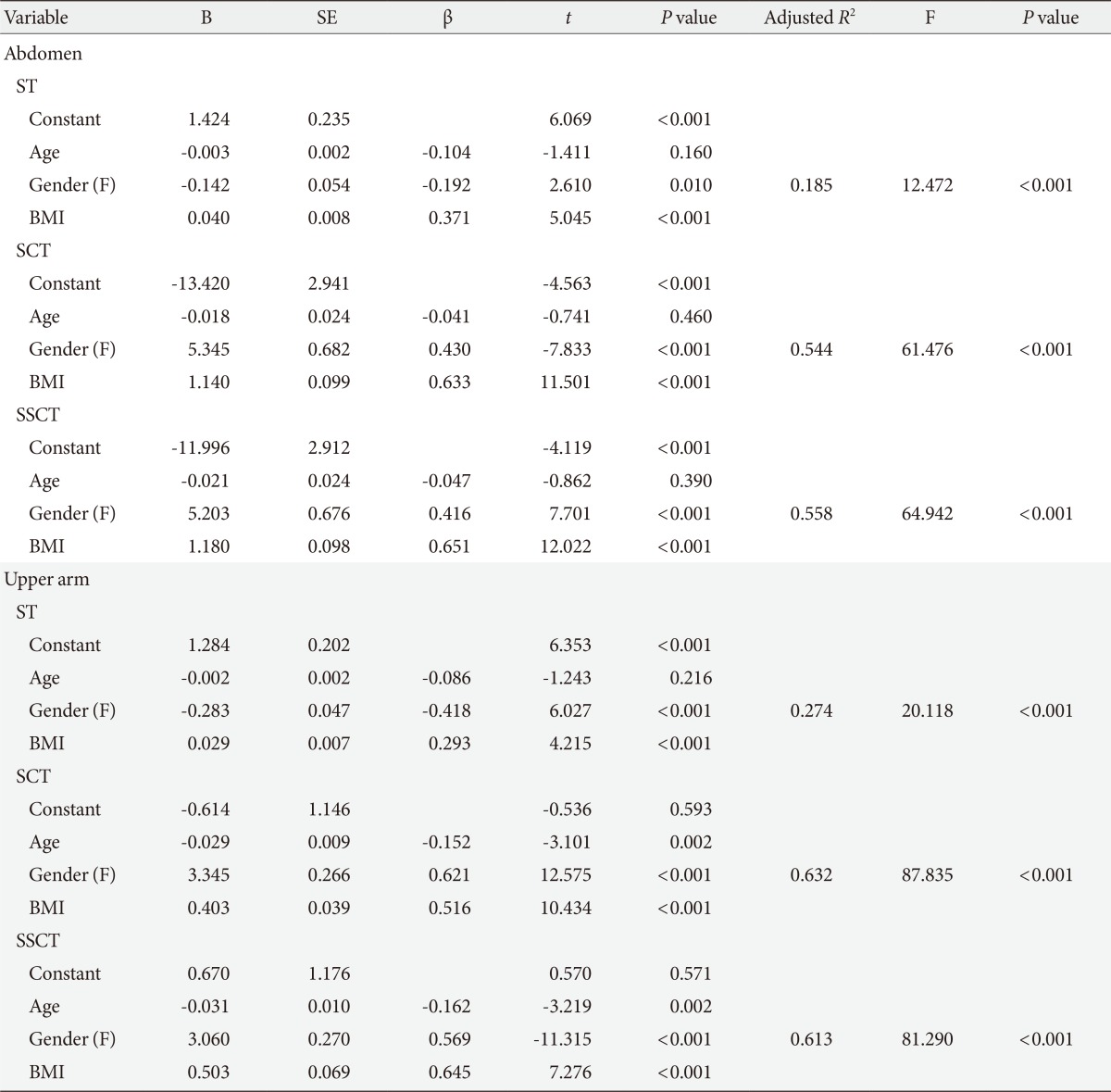
- Factors influencing skin and subcutaneous fat thicknesses of the abdomen and upper arm depending on injection sites
- In order to determine the influential factors for the skin and subcutaneous fat thicknesses and the total skin and subcutaneous fat thickness of the abdomen and upper arm, multiple regression analysis was performed with the identified factors that are related to this such as gender, age, and BMI as independent variables, as shown in Table 5.
- We found that the skin thickness of the abdomen and upper arm was higher in male and those with high BMI, with the explanatory power of adjusted R2 of 18.5% and 27.4% in the abdomen and upper arm, respectively. As for the subcutaneous fat thickness and the total skin and subcutaneous fat thickness, the thickness was positively correlated with gender (female) and high BMI in the abdomen, whereas it was positively correlated with gender (female), younger age, and high BMI in the upper arm. The explanatory power of adjusted R2 was 54.4% and 63.2% for the subcutaneous fat thickness of the abdomen and upper arm, respectively, and 55.8% and 61.3% for the total skin and subcutaneous fat thickness of the abdomen and upper arm, respectively.
- Our analysis showed that the regression models related to the skin and subcutaneous fat thicknesses and skin-subcutaneous thickness of the abdomen and upper arm were statistically significant (P<0.001). Furthermore, factors that influence these variables such as gender, age, and BMI did not have autocorrelation, with Dubin-Watson statistics of 1.791 to 2.058, and the variation inflation factor was 1.005 to 1.010 which is lower than 10 and therefore suggest no issues with the multicollinearity of these variables. Thus we may conclude that the results of regression analyses are reliable.
- The needle length-dependent possibility for the injection of insulin to the abdomen and upper arm
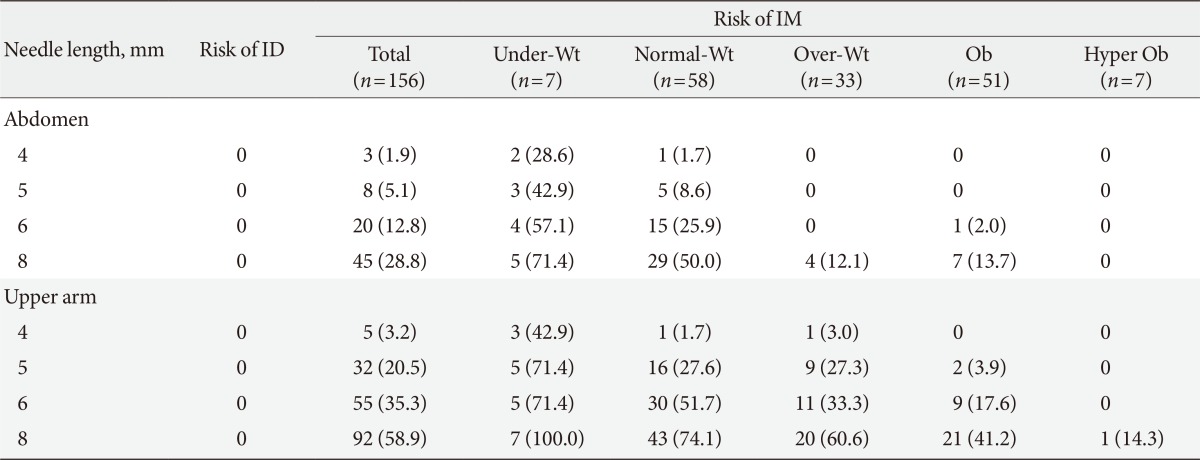
- The possibility of insulin injection to the abdomen and upper arm depending on the needle length was determined by analyzing the intradermal and intramuscular risks, as shown in Table 6.
- Investigations revealed that there were no cases of intradermal injection of insulin either to the abdomen or to the upper arm for all needle lengths. Differently, of the 156 patients, 3 (1.9%), 8 (5.1%), 20 (12.8%), and 45 (28.8%) cases were reported to have injected insulin into the muscles for the 4-, 5-, 6-, and 8-needles, respectively, where the frequency of intramuscular injection using 8-mm needles were more than 10-fold higher than when using 4-mm needles in the abdomen. Furthermore, 5 (3.2%), 32 (20.5%), 55 (35.3%), and 92 (58.9%) cases were reported for the same problem when using 4-, 5-, 6-, and 8-mm needles, respectively, in the upper arm, which denotes much higher risks than injecting into the abdomen. Nonetheless, these results plainly show that the risk of intramuscular injection increases with longer needles in both the abdomen and upper arm.
RESULTS
- The pain and complexities of an injection for insulin treatment notably reduces its compliance. Therefore, in an attempt to reduce pain and simplify the injection technique, short 4- or 5-mm needles were developed and applied to practical use, but domestic patients and nurses still tend to use the 8-mm needles. During an injection, insulin is injected into the dermis if the needle is shorter than the skin thickness, while it is injected into the muscles if the needle is longer than the total skin and subcutaneous fat thickness, which subsequently leads to problems in sugar control. For these reasons, the thicknesses of the skin and subcutaneous fat are important variables to consider when choosing the needle length and injection method. Therefore the purpose of this study stands to have great importance, which was to check the skin and subcutaneous fat thicknesses in the injection site and hence confirm the suitability of the newly developed short needles with Korean patients. However, this study failed to recruit a sufficient number of under-weight patients. Moreover we neglected the possibility of the variation in the skin and subcutaneous fat thicknesses depending on the right or left-handedness of our subjects and randomized the patients, measuring the thicknesses either on the right or left arm without putting this possibility into consideration. Still, bearing these limitations in mind, we may discuss some important facts about the results of this research.
- The average thickness of the skin in the was 2.29 mm (2.37 mm for males and 2.20 mm for females) and 2.00 mm (2.14 mm in males and 1.84 mm in females) in the abdomen and upper arm, respectively. Our results are consistent to the research by Gibney et al. [3] who reported an average skin thickness of 2.20 mm, and although the age group is different, it was also similar to the study conducted by Lo Presti et al. [13] who reported average skin thicknesses of 2.18 and 1.92 mm in the abdomen and upper arm of 14 to 17 years old teenagers, respectively. Despite these similarities, our results were strangely dissimilar to other studies conducted with Korean subjects, where Choi et al. [15] reported that the thicknesses of the skin were 1.57 mm and 1.53 to 1.57 mm in the abdomen and upper arm, respectively, and Park et al. [20] showed 1.31 mm (1.28 mm in males and 1.37 mm in females) in the abdomen, whose results are both thinner compared to ours. On the contrary, a study by Jung et al. [14] that was conducted with subjects more than 60 years old showed that the skin thicknesses were 2.97 and 2.16 mm in the abdomen and upper arm, respectively, which are thicker than our results.
- There are various methods to estimate the skin thickness, such as histopathologic analysis, computed tomography, ultrasound imaging, and so forth. However, there are several downsides for each method. When creating tissue sections for histopathologic analysis, the spaces between collagen proteins expand, making the section look thicker than it actually is. Furthermore, low-frequency ultrasound imaging does not provide a clear image that the investigators fail to definitely identify the boundary between epidermis and dermis and therefore lead to inaccurate estimation of the skin thickness, and computed tomography imaging has the tendency of compressing the skin, hence leading to underestimated skin thickness. Considering these possible biases, the skin thickness measured by Park et al. [20] using computed tomography were thinner, and those measured by Jung et al. [14] using low-frequency ultrasound were thicker than our results. Yet, those measured by Choi et al. using high-frequency ultrasound were thinner, while the results of Gibney et al. were similar to ours. Collectively, we believe that by using 10 MHz ultrasound and altering the frequency in the range of 7 to 12 MHz depending on the clarity of epidermal-dermal boundary, our results nicely reflect the actual thickness. In addition, the thicknesses measured by Jung et al. [14] varied from 1.99 to 4.59 mm depending on where it was measured, despite measuring the same abdomen. Our study also showed a variance of skin thickness depending on the measurement location, from 1.99 to 2.47 mm for the abdomen and from 1.69 to 2.28 mm for the upper arm. Unlike other studies that presented their data based on a single measurement, we measured the skin thickness from 10 different points for the abdomen and 8 different points for the upper arm and calculated the average. Thus we are confident that our results are accurate and have significant impact.
- Here the skin thicknesses of both the abdomen and upper arm differed depending on gender and BMI, and although the skin of males were thicker than females and their thickness also increased with increasing BMI value within a certain range, their explanatory power was 18.5% and 27.4% for the abdomen and upper arm, respectively, which is not a very high value. Gibney et al. [3] reported injection site, gender, BMI, and ethnicity as influential variables, considering that this study was conducted with a single ethnic group, this study supports the results of the present work. In detail, female skin was thicker than those of males, which is consistent to many other previous studies [3,15,20]. As for age, we recognized it to be a non-important factor for skin thickness, but the conclusion for this variable differed among many other research. Park et al. [20] reported that skin becomes thicker until when at a certain point it starts to thin down, but Jung et al. [14] reports a reversed result where they suggest that old age group has thicker skin compared to young and middle age groups. Nevertheless many other research have reported in favor of the opinion that age was irrelevant to skin thickness [3,15,21], and Shuster et al. [21] have suggested that the collagen and substrates in dermis are lost with progressing age, but the rearrangement of dermal collagen maintains the skin thickness. Together, it is necessary to rethink the hypothesis regarding the correlation of age and skin thickness, and repeated experiments to confirm this is required.
- BMI was identified as a factor affecting skin thickness in this research, where skin thickens with increasing BMI. Although this agrees with the results of Gibney et al. [3], it also somewhat disagrees with the results of Choi et al. [15] that suggests there is no significant relationship between the weight, one of the important variables for the calculation of BMI, and skin thickness. As weight increases, the cells that constitute the dermis becomes larger, and because the thickness of dermis is included in the calculation for the skin thickness, we speculate that skin thickness to be positively correlated to BMI. Further study to elucidate the underlying mechanisms behind the relationship between these two variables is necessary.
- The average subcutaneous fat thickness was 10.15 mm (7.75 mm for male and 13.07 for female) and 5.50 mm (4.06 mm for male and 7.19 mm for female) for the abdomen and upper arm, respectively, denoting that female had thicker subcutaneous fat layer and that abdomen was thicker than upper arm. Although this is fairly consistent with the research conducted on American diabetic patients by Gibney et al. [3] who reported that the subcutaneous fat thickness was 13.92 mm (12.3 mm for male and 15.9 mm for female) and 10.77 mm (8.4 mm for male and 13.7 mm for female) for the abdomen and upper arm, respectively, as well as being consistent with another research conducted with Korean diabetic patients by Jeong et al. [18] who reported thicknesses of 16.8 mm (16.3 mm for male and 17.3 mm for female) for the abdomen, the thicknesses measured in this study are generally thinner.
- The study by Gibney et al. [3] was conducted in a different country to the present study, for which reason we speculate that dietary patterns and ethnic factors may have some effects on the end result. On the other hand, the study by Jeong et al. [18] that was conducted in the same country was performed with patients residing in the province, which is very different to the current study that was performed with diabetic patients residing in Seoul and visiting a higher class general hospital. Hence we carefully suspect that, although the population-social factors and the extent of diabetes control was not thoroughly investigated, the quality of life and diabetes control quality may have affected the patients' weight, causing a decrease in subcutaneous fat thickness. Altogether, we encourage further study evaluating the effect of population-social factors and the extent of diabetes control on BMI or perhaps even on the actual subcutaneous fat thickness, and utilize those results, together with the results of this study, in the education for diabetes.
- Our results revealed gender and BMI (explanatory power 54.4%) for abdomen, and age, gender, and BMI (explanatory power 63.2%) for upper arm as the influential factors for subcutaneous fat thickness. Here, we showed that, within a certain range, the subcutaneous fat thickness increased by 0.63 and 0.52 mm in the abdomen and upper arm, respectively, per 1 kg/m2 increase in BMI, which is consistent to the data from Gibney et al. [3] who showed that the thickness increased by 0.4 mm per 1 kg/m2 increase in BMI, as well as the data from Joo and Sohng [4] who reported that the thickness increased by 0.71 and 0.62 mm in males and females, respectively, per 1 kg/m2 increase in BMI. As expected, the immediate relevance of BMI and subcutaneous fat thickness was very high like the many other domestically conducted studies [16,17]. Since obesity is highly associated with various metabolic diseases, especially diabetes, the importance of maintaining standard body weight to control blood glucose level as a diabetic patient must be emphasized.
- Subcutaneous fat thickness is also easily affected by gender, where females had thicker subcutaneous fat layer compared to males, and this is highly consistent throughout many other research [3,22]. The reason why females have thicker subcutaneous fat layers compared to males is because surplus fat is generally stored as visceral fat for males, while it is generally stored in the subcutaneous fat layer or the limbs for females [9], consequently giving rise to thicker subcutaneous fat layer in females compared to males. This implies that gender and BMI are crucial factors to be considered when selecting the appropriate needle length for subcutaneous and intramuscular injections.
- Insulin must be injected into subcutaneous fat. Thus, it is essential for short needles to fully penetrate the skin to avoid intradermal injections of insulin. All subjects of this study were confirmed to have skins less than 4 mm thick, and another study that was also conducted in Korea by Choi et al. [15] had the thickest skin yet to be reported, ranging from 2.77 to 3.87 mm for the abdomen. Therefore, including the commercially available 4-mm needle, all insulin syringe needles with different lengths are free of any risk of intradermal injections.
- Assuming that insulin was injected at a right angle to the skin, the risk for intramuscular injections was evaluated for needles of different lengths, deeming a needle length longer than the total skin and subcutaneous fat thickness to be dangerous. As a result, the risks of intramuscular injections were 1.9%, 5.1%, 12.8%, and 28.8% for 4-, 5-, 6-, and 8-mm needles, respectively, for the abdomen, while they were 3.2%, 20.5%, 35.3%, and 58.9% for 4-, 5-, 6-, and 8-mm needles, respectively, for the upper arm, indicating that longer needles had higher risks of intramuscular injections. These results are also consistent to the study by Gibney et al. [3] who also suggested that longer needles are tend to be at more risks of intramuscular injections, as well as the study by Lo Presti et al. [13] which was conducted with teenagers. In particular, the total skin and subcutaneous fat thickness of different groups divided according to BMI were 5.80, 9.42, 13.07, 15.07, and 15.07 mm for the abdomen, and 4.61, 6.70, 7.20, 8.41, and 11.85 mm for the upper arm for under-weight, normal-weight, over-weight, obese, and extremely obese groups, respectively. Therefore, together with our analysis of maximum skin thickness, we can conclude that 4- and 5-mm needles for the abdomen and 4-mm needle for the upper arm are appropriate for injection at a right angle to the skin, free of intradermal or intramuscular injection risks, without having to inject at a 45-degree angle or making skinfolds. One drawback is that the subcutaneous fat thickness of the abdomen and upper arm varied depending on the injection site. In this study, the outer section of the abdomen had thinner subcutaneous fat than the middle section, whereas the upper part was thinner than the lower part of the upper arm. Of special note, for some patients in the under-weight group, even the 4-mm needle which is the shortest had a risk for intramuscular injections. Therefore, when treating the under-weight group, some injection skills may still be necessary such as injecting at a 45-degree angle or making skinfolds, despite using the shortest needle.
- Pregnant patients diagnosed with gestational diabetes avoid injections to the abdomen and prefer to have insulin injections either to the upper arm or to the thigh in concern of their baby. In case of injecting insulin to the upper arm where the subcutaneous fat in relatively thin, special injection techniques such as injecting at a 45-degree angle or making skinfolds are necessary, but this is extremely difficult for the patients to perform by themselves. However, the results of this study indicated that the skin thickness of women in the upper arm was thinner than 4 mm while the total skin and subcutaneous fat thickness was thicker than 4 mm, pointing out that self-injections at a right angle to the skin is possible with short needles. Therefore we think that it is advisable to encourage pregnant patients with gestational diabetes to use short needled insulin syringes to make them more submissive to insulin treatment.
- The number of old aged diabetic patients has been increasing recently [7], along with the increase in the number of elderly living alone. The elderly also have issues with injecting at an angle or making skinfolds, so it is necessary to simplify the injection technique. In this regard, it is unnecessary to inject at an angle or make skinfolds when using short needles, so we hope that encouraging the usage of such short needles will make the elderly more compliant to insulin treatment.
- In another aspect, Hauner et al. [23] reported that 60% patients who do not change the injection site and 22% who do change the injection site but do so irregularly have lipodystrophy. Changing the injection site does not simply mean that the injection site must be changed, but the 'same time, same place' principle must be kept [1]. According to a recent investigation, although the medical doctors instruct diabetic patients to take part in the education for diabetes, most patients do not follow [24]. Even in the preliminary investigation of the present study, patients did not use the whole abdominal area to inject insulin, but mainly used the points 7, 8, 11, and 12 to inject insulin, and have explained that they did not use the whole abdominal area because it was inconvenient to inject on the outer area and also because they were in fear of injecting too deeply. We believe that our study which investigated the skin and subcutaneous fat thicknesses for each different injection sites on the abdomen and upper arm will be a strong supportive material in persuading patients to fully use the injection sites available and to do so in a consistently changing manner. Still, our study was conducted in only one hospital, and the number of patients less than 45 years old was 10.4%. For the generalization of our work, we propose further studies which repeat our study with expanded number of patients less than 45 years old as well as the number of hospitals. It would also be preferable to measure the skin and subcutaneous fat thicknesses of type 1 DM patients and children.
- In conclusion, we presented our measurements of skin thickness and skin-subcutaneous thickness as a diagram so that it can be used as a basis for subcutaneous insulin injection. Furthermore, we investigated the risks of intradermal and intramuscular injections for needles of different lengths to evaluate the suitability and also the necessary or unnecessary techniques to be used with those needles. Our evaluations pinpoint the commercially available 4-mm long needles for usage by Korean diabetic patients. Overall this study will contribute immensely to the evidence-based decisions of appropriate needle length and injection sites for different diabetic patients.
DISCUSSION
-
Acknowledgements
- The authors thank all the Becton Dickinson and Company, Korea employees who helped in this study, especially Hyunjoo Dan.
ACKNOWLEDGMENTS
-
This work was partially supported by the Becton Dickinson and Company, but no potential conflict of interest relevant to this article was reported.
NOTES
- 1. Korean Association of Diabetes Nursing Education. Guideline for education of insulin. 1st ed. Seoul: LeadersMD; 2010. p. 61-86.
- 2. Choi DW, Sohng KY, Kim BS. Prediction of optimal gluteal intramuscular needle length by skinfold thickness measurements in Korean adults. J Korean Acad Nurs 2010;40:844-851. ArticlePubMed
- 3. Gibney MA, Arce CH, Byron KJ, Hirsch LJ. Skin and subcutaneous adipose layer thickness in adults with diabetes at sites used for insulin injections: implications for needle length recommendations. Curr Med Res Opin 2010;26:1519-1530. ArticlePubMed
- 4. Joo G, Sohng KY. Gluteal subcutaneous fat thickness measured by computed tomography as an estimate of proper gluteal intramuscular injections in Korean adults. J Korean Acad Nurs 2010;40:247-254. ArticlePubMed
- 5. Lippert WC, Wall EJ. Optimal intramuscular needle-penetration depth. Pediatrics 2008;122:e556-e563. ArticlePubMedPDF
- 6. King L. Subcutaneous insulin injection technique. Nurs Stand 2003;17:45-52. Article
- 7. Kim KS, Kim SK, Sung KM, Cho YW, Park SW. Management of type 2 diabetes mellitus in older adults. Diabetes Metab J 2012;36:336-344. ArticlePubMedPMC
- 8. Hirsch LJ, Gibney MA, Albanese J, Qu S, Kassler-Taub K, Klaff LJ, Bailey TS. Comparative glycemic control, safety and patient ratings for a new 4 mm x 32G insulin pen needle in adults with diabetes. Curr Med Res Opin 2010;26:1531-1541. PubMed
- 9. Kreugel G, Keers JC, Kerstens MN, Wolffenbuttel BH. Randomized trial on the influence of the length of two insulin pen needles on glycemic control and patient preference in obese patients with diabetes. Diabetes Technol Ther 2011;13:737-741. ArticlePubMedPMC
- 10. Kim MJ, Park HS, Choi SH, Sohng KY, Kim HS, Nam JJ, Park GH, Paek SH, Lee KI, Lee KE, Chung SK, Han SJ, Hong YH. Fundamentals of nursing. Seoul: Hyunmoonsa; 2005.
- 11. Yoo JW, Suh MJ. Analysis of insulin injection focused self-care and related factors in diabetics. J Korean Diabetes Assoc 2003;27:153-164.
- 12. Zaybak A, Gunes UY, Tamsel S, Khorshid L, Eser I. Does obesity prevent the needle from reaching muscle in intramuscular injections? J Adv Nurs 2007;58:552-556. ArticlePubMed
- 13. Lo Presti D, Ingegnosi C, Strauss K. Skin and subcutaneous thickness at injecting sites in children with diabetes: ultrasound findings and recommendations for giving injection. Pediatr Diabetes 2012;13:525-533. ArticlePubMed
- 14. Jung HJ, Kim DW, Chung SL, Kim TH. A study on the skin thickness of Koreans by ultrasound. Korean J Dermatol 1990;28:121-129.
- 15. Choi SW, Lee JH, Kim HO, Kim JI, Lee HK. A comparative study on skin thickness between an old-aged group and a young aged group by 20 MHz-high frequency ultrasonography. Korean J Dermatol 1999;37:719-725.
- 16. Sung SK, Jang SJ. Body composition and measurement of subcutaneous fat thickness by ultrasonic method. J Ergon Soc Korea 1994;13:47-58.
- 17. Shin D, Son D, Park M, Kim J, Han K. Characteristics of fat tissue according to the anatomical regions of the body: computed tomographic and histological findings. J Korean Soc Plast Reconstr Surg 2010;37:535-546.
- 18. Jeong GH, Kim SK, Chung JO, Cho DH, Chung DJ, Chung MY. Association between ultrasonographic visceral fat indices and cardiovascular risk factors in type 2 diabetic patients. Korean J Med 2007;73:618-630.
- 19. Sim KH, Kim KW, Lee MK. Rotation table for insulin injection cited 2013 Mar 4. Available from: http://www.kipi.or.kr.
- 20. Park JS, Cho BK, Park SH. A study on the skin thickness in Koreans by computed tomography. Korean J Dermatol 1995;33:303-313.
- 21. Shuster S, Black MM, McVitie E. The influence of age and sex on skin thickness, skin collagen and density. Br J Dermatol 1975;93:639-643. ArticlePubMed
- 22. Ko JH, Park JS, Kim KJ. The relationship between abdominal visceral fat area and regional subcutaneous skinfold thickness in Korean adults. Korean J Obes 2008;17:45-52.
- 23. Hauner H, Stockamp B, Haastert B. Prevalence of lipohypertrophy in insulin-treated diabetic patients and predisposing factors. Exp Clin Endocrinol Diabetes 1996;104:106-110. ArticlePubMed
- 24. Kim MY, Suh S, Jin SM, Kim SW, Bae JC, Hur KY, Kim SH, Rha MY, Cho YY, Lee MS, Lee MK, Kim KW, Kim JH. Education as prescription for patients with type 2 diabetes mellitus: compliance and efficacy in clinical practice. Diabetes Metab J 2012;36:452-459. ArticlePubMedPMC
REFERENCES
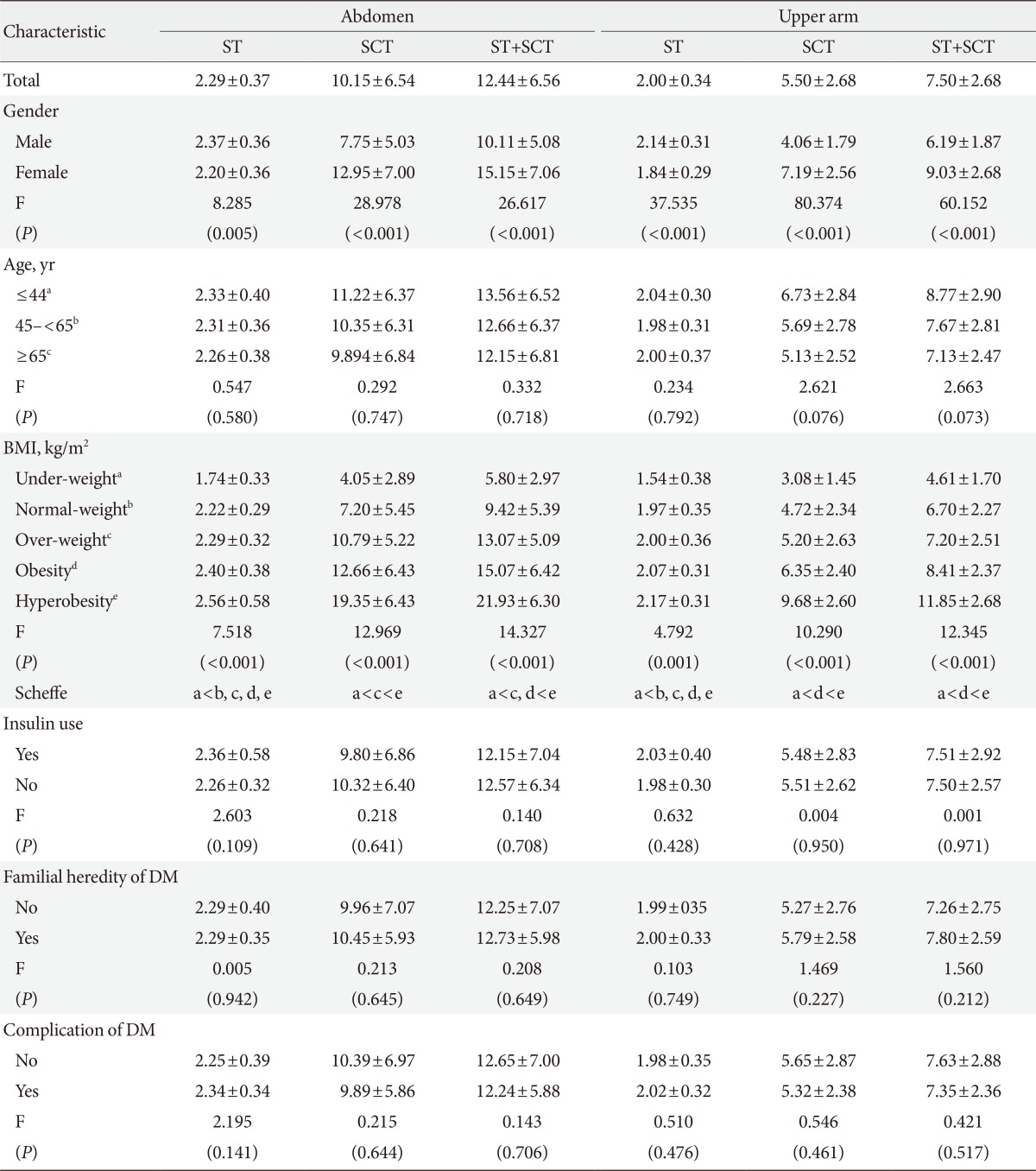
Figure & Data
References
Citations

- Inadvertent intramuscular injection risk with subcutaneous insulin injections and risk predictors in adults: a cross-sectional sonographic study
U. A. Liyanage, Y. Mathangasinghe, C. K. Liyanage, E. S. Wijewickrama, D. Mahathanthila, A. J. Dharmawansa, S. Jeyerajesingham, D. S. Warapitiya, M. D. M. S. Wijayabandara, B. C. T. A. N. W. M. R. C. S. Kempitiya, A. Aravinthan, L. M. D. T. Jayasekara, N.
International Journal of Diabetes in Developing Countries.2023; 43(5): 731. CrossRef - COVID-19 vaccination and the skin to deltoid muscle distance in adults with diabetes
Marjan Doppen, Ali Mirjalili, Matire Harwood, Allie Eathorne, Irene Braithwaite, Jonathan Bong, Louis Kirton, Ruth Semprini, Mark Weatherall, Alex Semprini, Ciléin Kearns, Melissa Black, Stacey Kung, Michaela Walton, Richard Beasley, Thomas Hills
Vaccine: X.2023; 13: 100248. CrossRef - Integration of capillaric strain sensors toward recognition of human movements
Hudson Gasvoda, Nick Cmager, Rana Altay, Ju Young Lee, I. Emre Araci
Sensors & Diagnostics.2023; 2(1): 212. CrossRef - What variables should inform needle length choice for deltoid intramuscular injection? A systematic review
Ciléin Kearns, Claire Houghton, Emily Dickinson, Lee Hatter, Pepa Bruce, Srinidhi Krishnamoorthy, Mark Weatherall, Thomas Hills, Marjan Doppen, Seyed Ali Mirjalili, Richard Beasley
BMJ Open.2023; 13(1): e063530. CrossRef - Investigation of appropriate needle length considering skin thickness with the real injection posture for insulin injections in diabetic patients
Aya Torii-Goto, Kana Hirai, Yuri Inukai, Yoshimi Hoshina, Kazumi Shiomi, Junko Ito, Masae Yoshikawa
Journal of Pharmaceutical Health Care and Sciences.2023;[Epub] CrossRef - Machine Learning-Based Prediction of Abdominal Subcutaneous Fat Thickness During Pregnancy
Moon Sook Hwang, Eunjeong Song, Jeonghee Ahn, Seungmi Park
Metabolic Syndrome and Related Disorders.2023; 21(9): 479. CrossRef - Human continuous glucose monitors for measurement of glucose in dairy cows
M.K.H. Byrd, A.G. Arneson, D.R. Soffa, J.W. Stewart, M.L. Rhoads
JDS Communications.2022; 3(1): 78. CrossRef - A finite element model of abdominal human tissue for improving the accuracy in insulin absorption assessment: A feasibility study
Pasquale Arpaia, Davide Cuneo, Sabrina Grassini, Francesca Mancino, Simone Minucci, Nicola Moccaldi, Isabella Sannino
Measurement: Sensors.2021; 18: 100218. CrossRef - Abdominal skin subcutaneous fat thickness over the gestational period in Korean pregnant women: a descriptive observational study
Moon Sook Hwang
Korean Journal of Women Health Nursing.2021; 27(4): 318. CrossRef - User experience for manual injection of 2 mL viscous solutions is enhanced by a new prefillable syringe with a staked 8 mm ultra-thin wall needle
Aurélie Pager, Anne Combedazou, Karen Guerrero, Tzvetelina Tzvetkova-Chevolleau, Didier Morel, Cécile Frolet, Stanislav Glezer
Expert Opinion on Drug Delivery.2020; 17(10): 1485. CrossRef - Evaluating the Impact of Human Factors and Pen Needle Design on Insulin Pen Injection
Christopher Rini, Bruce C. Roberts, Didier Morel, Rick Klug, Benjamin Selvage, Ronald J. Pettis
Journal of Diabetes Science and Technology.2019; 13(3): 533. CrossRef - Subcutaneous Injection of Drugs: Literature Review of Factors Influencing Pain Sensation at the Injection Site
Iris Usach, Rafael Martinez, Teodora Festini, José-Esteban Peris
Advances in Therapy.2019; 36(11): 2986. CrossRef - The Injection Technique Factor: What You Don’t Know or Teach Can Make a Difference
Laurence J. Hirsch, Kenneth W. Strauss
Clinical Diabetes.2019; 37(3): 227. CrossRef - Factors associated with removal difficulties of etonogestrel-containing contraceptive implants (Nexplanon ® )
Julien Chevreau, David Krief, Osama Abou Arab, Mickaël Zitoun, Arthur Foulon, Fabrice Sergent, Jean Gondry
European Journal of Obstetrics & Gynecology and Reproductive Biology.2018; 224: 81. CrossRef - Insulin Injection Technique in China Compared with the Rest of the World
Zhenqiang Song, Xiaohui Guo, Linong Ji, Xiao Huang, Laurence J. Hirsch, Kenneth W. Strauss
Diabetes Therapy.2018; 9(6): 2357. CrossRef - Ultrasound-guided measurement of skin and subcutaneous tissue thickness in children with diabetes and recommendations for giving insulin injections
Soo Ting Joyce Lim, Yuen Ching Angela Hui, Pei Kwee Lim, Chin Choo Evelyn Lim, Yen Yen Chia, Rashida Farhad Vasanwala
Journal of Clinical & Translational Endocrinology.2018; 12: 26. CrossRef - Comment on the New Indian Injection Technique Recommendations: Critical Appraisal of the Real-World Implementation of the Current Guidelines
Felice Strollo, Sandro Gentile
Diabetes Therapy.2017; 8(3): 507. CrossRef - Worldwide Injection Technique Questionnaire Study
Anders H. Frid, Laurence J. Hirsch, Astrid R. Menchior, Didier R. Morel, Kenneth W. Strauss
Mayo Clinic Proceedings.2016; 91(9): 1212. CrossRef - Skin and subcutaneous tissue thickness at insulin injection sites in Chinese diabetes patients: Clinical implications
W. Wang, X. Guo, G. Shen, G. Bai, Z. Wei, J. Liu, L. Hirsch, K. Strauss
Diabetes & Metabolism.2016; 42(5): 374. CrossRef - New Insulin Delivery Recommendations
Anders H. Frid, Gillian Kreugel, Giorgio Grassi, Serge Halimi, Debbie Hicks, Laurence J. Hirsch, Mike J. Smith, Regine Wellhoener, Bruce W. Bode, Irl B. Hirsch, Sanjay Kalra, Linong Ji, Kenneth W. Strauss
Mayo Clinic Proceedings.2016; 91(9): 1231. CrossRef - Le tissu sous-cutané et l’insuline : Une cohabitation délicate Revue de la littérature
K. Strauss, S. Halimi
Médecine des Maladies Métaboliques.2015; 9(5): 504. CrossRef - Subcutaneous Injection Depth Does Not Affect the Pharmacokinetics or Glucodynamics of Insulin Lispro in Normal Weight or Healthy Obese Subjects
Amparo de la Peña, Kwee P. Yeo, Helle Linnebjerg, Edward Catton, Shobha Reddy, Patricia Brown-Augsburger, Linda Morrow, Debra A. Ignaut
Journal of Diabetes Science and Technology.2015; 9(4): 824. CrossRef

 KDA
KDA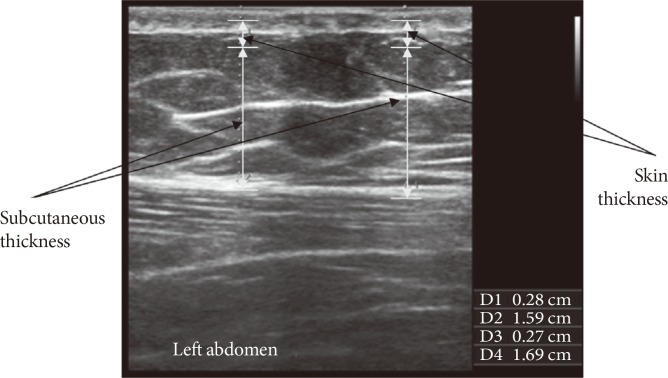

 PubReader
PubReader Cite
Cite