
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
Original Articles
- COVID-19
- Impact of COVID-19 Lockdown on the Metabolic Control Parameters in Patients with Diabetes Mellitus: A Systematic Review and Meta-Analysis
- Ifan Ali Wafa, Nando Reza Pratama, Nurizzah Farahiyah Sofia, Elsha Stephanie Anastasia, Tiffany Konstantin, Maharani Ayuputeri Wijaya, M. Rifqi Wiyono, Lilik Djuari, Hermina Novida
- Diabetes Metab J. 2022;46(2):260-272. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0125
- 5,925 View
- 272 Download
- 10 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Abrupt implementation of lockdowns during the coronavirus disease 2019 (COVID-19) pandemic affected the management of diabetes mellitus in patients worldwide. Limited access to health facilities and lifestyle changes potentially affected metabolic parameters in patients at risk. We conducted a meta-analysis to determine any differences in the control of metabolic parameters in patients with diabetes, before and during lockdown.
Methods
We performed searches of five databases. Meta-analyses were carried out using random- or fixed-effect approaches to glycaemic control parameters as the primary outcome: glycosylated hemoglobin (HbA1c), random blood glucose (RBG), fasting blood glucose (FBG), time-in-range (TIR), time-above-range (TAR), time-below-range (TBR). Mean difference (MD), confidence interval (CI), and P value were calculated. Lipid profile was a secondary outcome and is presented as a descriptive analysis.
Results
Twenty-one studies enrolling a total of 3,992 patients with type 1 or type 2 diabetes mellitus (T1DM or T2DM) were included in the study. Patients with T1DM showed a significant improvement of TIR and TAR (MD=3.52% [95% CI, 0.29 to 6.74], I2=76%, P=0.03; MD=–3.36% [95% CI, –6.48 to –0.25], I2=75%, P=0.03), while FBG among patients with T2DM significantly worsened (MD=3.47 mg/dL [95% CI, 1.22 to 5.73], I2=0%, P<0.01). No significant difference was found in HbA1c, RBG, and TBR. Use of continuous glucose monitoring in T1DM facilitated good glycaemic control. Significant deterioration of lipid parameters during lockdown, particularly triglyceride, was observed.
Conclusion
Implementation of lockdowns during the COVID-19 pandemic did not worsen glycaemic control in patients with diabetes. Other metabolic parameters improved during lockdown, though lipid parameters, particularly triglyceride, worsened. -
Citations
Citations to this article as recorded by- Disruption of diabetes and hypertension care during the COVID-19 pandemic and recovery approaches in the Latin America and Caribbean region: a scoping review protocol
Samira Barbara Jabakhanji, Oluwabunmi Ogungbe, Sonia Y Angell, Lawrence Appel, David Byrne, Roopa Mehta, John McCaffrey, Lori Rosman, Edward W Gregg, Kunihiro Matsushita
BMJ Open.2024; 14(1): e074443. CrossRef - Influence of the COVID-19 pandemic on the achievement of guideline targets for HbA1c, blood pressure, and LDL cholesterol in people with diabetes in Japan
Shingo Kuwajima, Takahito Itoh, Tatsuya Sato, Shoya Ino, Satoru Shibata, Kouhei Ohno, Hiroyuki Hotta, Tomoaki Matsumoto, Hitoshi Ooiwa, Hirofumi Kubo, Takayuki Miki
Diabetology International.2024;[Epub] CrossRef - Glycemic Control in Type 1 Diabetes Mellitus and COVID-19: What We Learned From the Lockdown Experience
Catarina Almeida, André Ferreira, Daniela Duarte, Ana Filipa Viegas, André Santos, Alexandra Vaz, Edite Nascimento
Cureus.2023;[Epub] CrossRef - Changes in body weight and glycemic control in association with COVID-19 Shutdown among 23,000 adults with type 2 diabetes
Emily Panza, Kevin E. Kip, Kripa Venkatakrishnan, Oscar C. Marroquin, Rena R. Wing
Acta Diabetologica.2023; 60(6): 787. CrossRef - The Impact of a Lockdown for the COVID-19 Pandemic on Seasonal HbA1c Variation in Patients with Type 2 Diabetes
Yu-Cheng Cheng, Yu-Hsuan Li, Hsiu-Chen Liu, Chiann-Yi Hsu, Wan-Jen Chang, I-Te Lee, Chin-Li Lu
Life.2023; 13(3): 763. CrossRef - The Impact of Partial Lockdown During COVID-19 Pandemic on Metabolic Control in People with Type 2 Diabetes Mellitus
Ayşe Zülal TOKAÇ, Tuğde Buse UĞUR, Buse Ecem KURUGÖL, Sevilay ALİGÜLÜ, Osman HAYRAN
Journal of Biotechnology and Strategic Health Research.2023; 7(1): 67. CrossRef - Retrospective Study on the Impact of COVID-19 Lockdown on Patients with Type 2 Diabetes in Northern Taiwan
Hsuan Huang, Hsiao-Ling Su, Chih-Hsung Huang, Yi-Hsin Lin
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 2539. CrossRef - RIPK1 and RIPK3 inhibitors: potential weapons against inflammation to treat diabetic complications
Dan Ke, Zhen Zhang, Jieting Liu, Peijian Chen, Yucen Dai, Xinhai Sun, Yanhui Chu, Luxin Li
Frontiers in Immunology.2023;[Epub] CrossRef - “Does Physical Exercise Promote Health Benefits for Diabetic Patients during the COVID-19 Pandemic?”: A Systematic Review
Erivaldo de Souza, Daniela Meneses-Santos, Josué Cruz Santos, Felipe J. Aidar, Carla Roberta de Oliveira Carvalho, Jymmys Lopes dos Santos, Anderson Carlos Marçal
Sports.2023; 11(10): 192. CrossRef - Impact of National Lockdown From COVID-19 Pandemic in Patients With Type 2 Diabetes: An Observational Study
Nuntakorn Thongtang, Niracha Chanwimol, Lukana Preechasuk, Varisara Boonyuang, Pinyo Rattanaumpawan, Supawadee Likitmaskul, Apiradee Sriwijitkamol
Asia Pacific Journal of Public Health.2022; 34(6-7): 708. CrossRef
- Disruption of diabetes and hypertension care during the COVID-19 pandemic and recovery approaches in the Latin America and Caribbean region: a scoping review protocol
- Cardiovascular Risk/Epidemiology
- Appraisal of Guidelines for the Management of Blood Pressure in Patients with Diabetes Mellitus: The Consensuses, Controversies and Gaps
- Menghui Liu, Shaozhao Zhang, Xiaohong Chen, Yue Guo, Xiangbin Zhong, Zhenyu Xiong, Yifen Lin, Huimin Zhou, Yiquan Huang, Zhengzhipeng Zhang, Lichun Wang, Xiaodong Zhuang, Xinxue Liao
- Diabetes Metab J. 2021;45(5):753-764. Published online April 23, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0134
- 4,866 View
- 143 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Currently available guidelines contain conflicting recommendations on the management of blood pressure (BP) in patients with diabetes mellitus (DM). Therefore, it is necessary to appraise the guidelines and summarize the agreements and differences among recommendations.
Methods
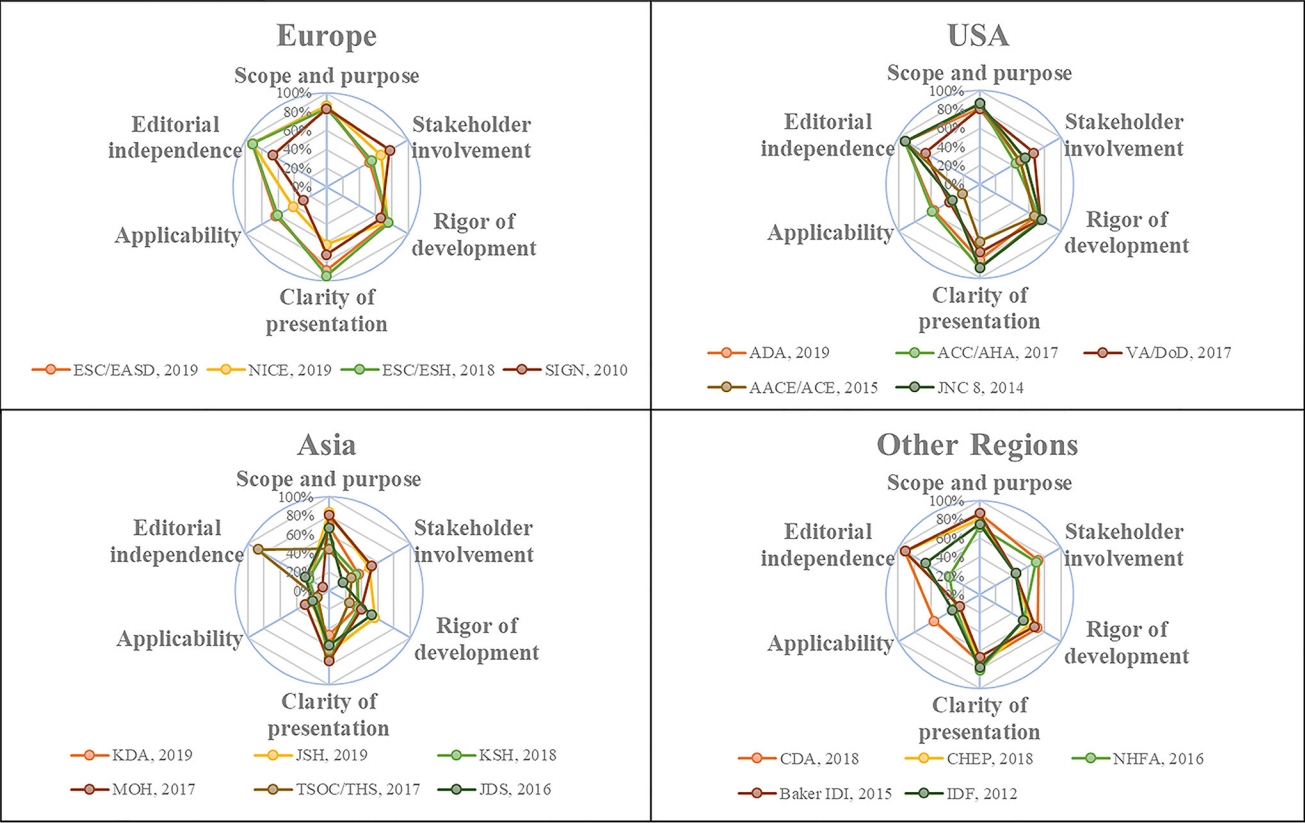
Four databases and the websites of guideline organizations were searched for guidelines regarding BP targets and thresholds for pharmacologic therapy in DM patients, and the included guidelines were appraised with the Appraisal of Guidelines for Research and Evaluation (AGREE) II instrument.
Results
In 6,498 records identified, 20 guidelines met our inclusion criteria with 64.0% AGREE II scores (interquartile range, 48.5% to 72.0%). The scores of the European and American guidelines were superior to those of the Asian guidelines (both adjusted P<0.001). Most of the guidelines advocated systolic BP targets <130 mm Hg (12 guidelines, 60%) and diastolic BP targets <80 mm Hg (14 guidelines, 70%) in DM patients. Approximately half of the guidelines supported systolic BP thresholds >140 mm Hg (10 guidelines, 50%) and diastolic BP thresholds >90 mm Hg (nine guidelines, 45%). The tiny minority of the guidelines provided the relevant recommendations regarding the lower limit of official BP targets and the ambulatory BP monitoring (ABPM)/home BP monitoring (HBPM) targets and thresholds in DM patients.
Conclusion
The lower official BP targets (<130/80 mm Hg) in patients with DM are advocated by most of the guidelines, but they contain conflicting recommendations on the official BP thresholds. Moreover, the gaps regarding the lower limit of official BP targets and the ABPM/HBPM targets and thresholds need to be considered by future study.

 KDA
KDA
 First
First Prev
Prev





