
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Metabolic Risk/Epidemiology
- Differential Impact of Obesity on the Risk of Diabetes Development in Two Age Groups: Analysis from the National Health Screening Program
- Tae Kyung Yoo, Kyung-Do Han, Yang-Hyun Kim, Ga Eun Nam, Sang Hyun Park, Eun-Jung Rhee, Won-Young Lee
- Diabetes Metab J. 2023;47(6):846-858. Published online August 23, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0242

- 1,200 View
- 143 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The effect of obesity on the development of type 2 diabetes mellitus (DM) in different age groups remains unclear. We assessed the impact of obesity on the development of DM for two age groups (40-year-old, middle age; 66-year-old, older adults) in the Korean population.
Methods
We analyzed Korean National Health Insurance Service data of 4,145,321 Korean adults with 40- and 66-year-old age without DM, between 2009 and 2014. Participants were followed up until 2017 or until the diagnosis of DM. We assessed the risk of DM based on the body mass index and waist circumference of the participants. Multiple confounding factors were adjusted.
Results
The median follow-up duration was 5.6 years. The association of general and abdominal obesity with the risk of DM development was stronger in the 40-year-old group (general obesity: hazard ratio [HR], 3.566, 95% confidence interval [CI], 3.512 to 3.622; abdominal obesity: HR, 3.231; 95% CI, 3.184 to 3.278) than in the 66-year-old group (general obesity: HR, 1.739; 95% CI, 1.719 to 1.759; abdominal obesity: HR, 1.799; 95% CI, 1.778 to 1.820). In the 66-year-old group, abdominal obesity had a stronger association with the development of DM as compared to general obesity. In the 40-year-old group, general obesity had a stronger association with the risk of DM development than abdominal obesity.
Conclusion
The influence of general and abdominal obesity on the development of DM differed according to age. In older adults, abdominal obesity had a stronger association with DM development than general obesity.
- Lifestyle
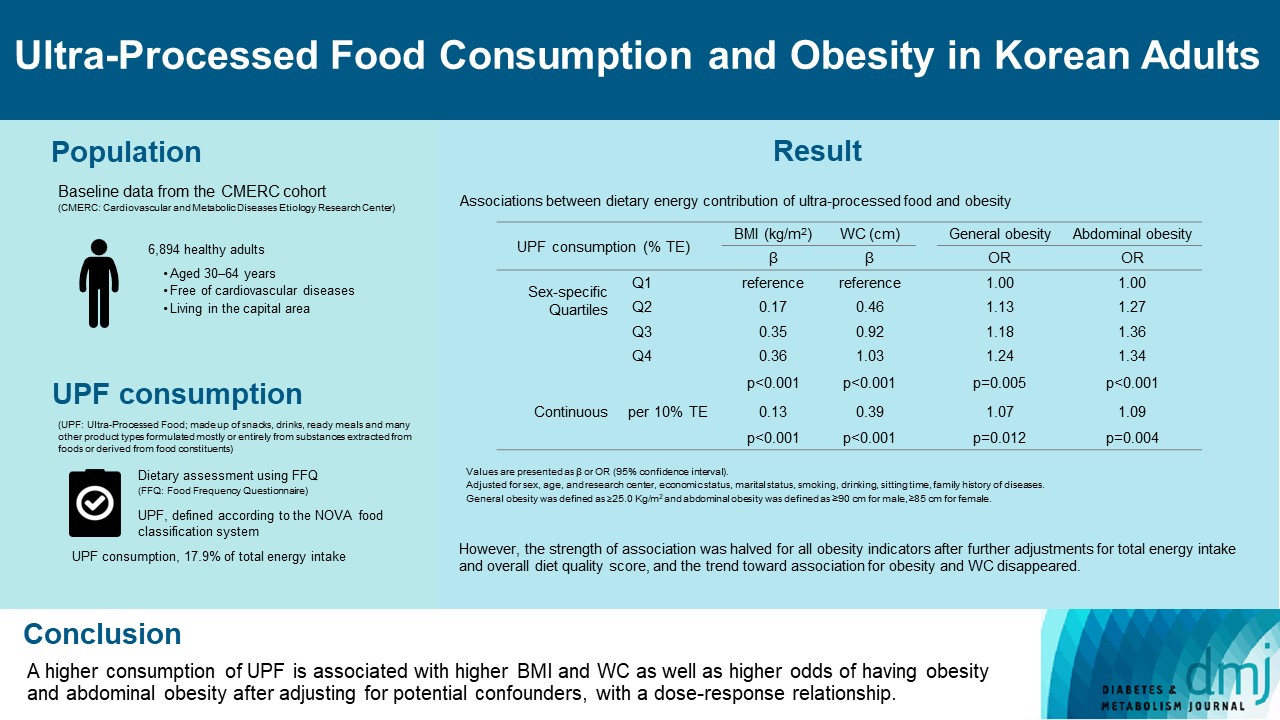
- Ultra-Processed Food Consumption and Obesity in Korean Adults
- Jee-Seon Shim, Kyoung Hwa Ha, Dae Jung Kim, Hyeon Chang Kim
- Diabetes Metab J. 2023;47(4):547-558. Published online April 26, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0026
- 2,876 View
- 139 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
This study aimed to investigate the association between consumption of ultra-processed foods (UPF) and obesity in Korean adults.
Methods
We included the Cardiovascular and Metabolic Diseases Etiology Research Center cohort study baseline data of adults aged 30 to 64 years who completed a validated food frequency questionnaire. UPF was defined using the NOVA food classification. Multivariable linear and logistic regression analyses were performed to assess the association of dietary energy contribution of UPF with obesity indicators (body mass index [BMI], obesity, waist circumference [WC], and abdominal obesity).
Results
Consumption of UPF accounted for 17.9% of total energy intake and obesity and abdominal obesity prevalence was 35.4% and 30.2%, respectively. Compared with those in the lowest quartile of UPF consumption, adults in the highest quartile had greater BMI (β=0.36; 95% confidence interval [CI], 0.15 to 0.56), WC (β=1.03; 95% CI, 0.46 to 1.60), higher odds of having obesity (odds ratio [OR], 1.24; 95% CI, 1.07 to 1.45), and abdominal obesity (OR, 1.34; 95% CI, 1.14 to 1.57), after adjusting for sociodemographic characteristics, health-related behaviors, and family history of diseases. Dose-response associations between UPF consumption and obesity indicators were consistently found (all P trend <0.01). However, the strength of association was halved for all obesity indicators after further adjustments for total energy intake and overall diet quality score, and the trend toward association for obesity and WC disappeared.
Conclusion
Our finding supports the evidence that consumption of UPF is positively associated with obesity among Korean adults. -
Citations
Citations to this article as recorded by- Ultra-processed food consumption and increased risk of metabolic syndrome in Korean adults: A cross-sectional analysis of the KNHANES 2016–2020
Hansol Park, Youngmi Lee, Jinah Hwang, Yujin Lee
Nutrition.2024; 122: 112374. CrossRef - Diet quality partially mediates the association between ultraprocessed food consumption and adiposity indicators
Jee‐Seon Shim, Kyoung Hwa Ha, Dae Jung Kim, Hyeon Chang Kim
Obesity.2023; 31(9): 2430. CrossRef - Development of a Semi-Quantitative Food-Frequency Questionnaire for Korean Adults with Obesity
Jina Chung, Seoeun Ahn, Hyojee Joung, Sangah Shin
Nutrients.2023; 15(22): 4848. CrossRef
- Ultra-processed food consumption and increased risk of metabolic syndrome in Korean adults: A cross-sectional analysis of the KNHANES 2016–2020
- Cardiovascular Risk/Epidemiology
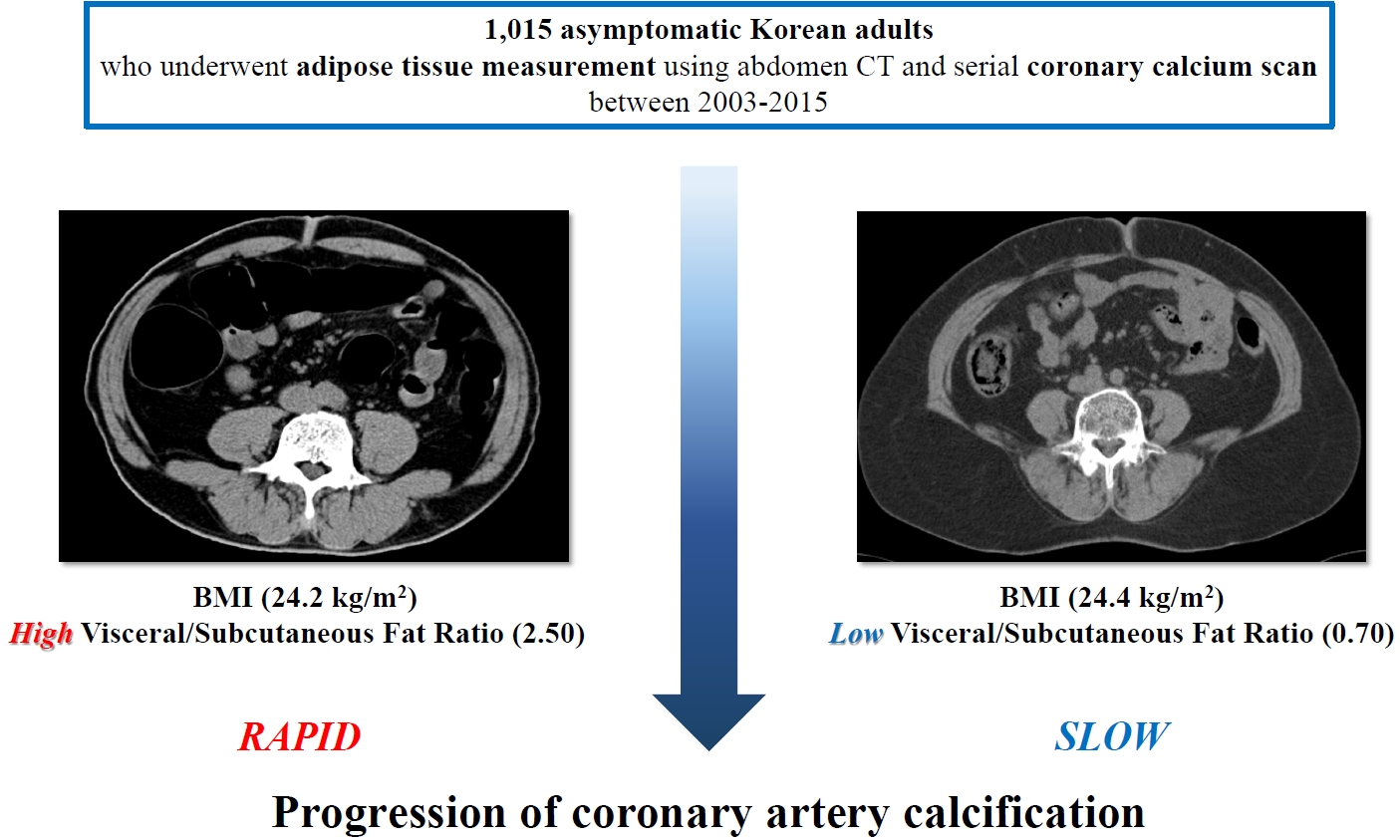
- Clinical Significance of Body Fat Distribution in Coronary Artery Calcification Progression in Korean Population
- Heesun Lee, Hyo Eun Park, Ji Won Yoon, Su-Yeon Choi
- Diabetes Metab J. 2021;45(2):219-230. Published online October 28, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0161
- Correction in: Diabetes Metab J 2021;45(6):974
- 6,515 View
- 257 Download
- 8 Web of Science
- 7 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 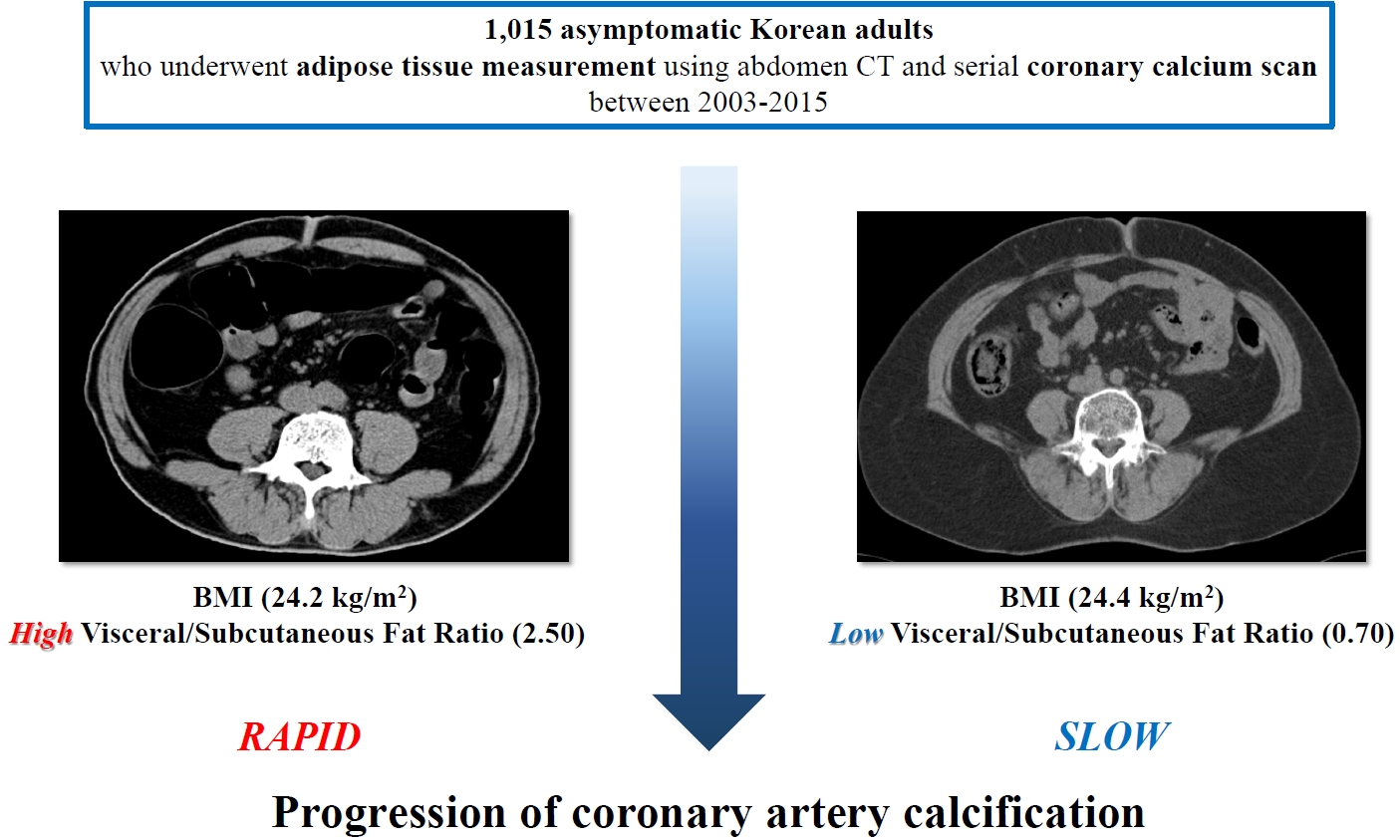
- Background
Although obesity differs according to ethnicity, it is globally established as a solid risk factor for cardiovascular disease. However, it is not fully understood how obesity parameters affect the progression of coronary artery calcification (CAC) in Korean population. We sought to evaluate the association of obesity-related parameters including visceral adipose tissue (VAT) measurement and CAC progression.
Methods
This retrospective observational cohort study investigated 1,015 asymptomatic Korean subjects who underwent serial CAC scoring by computed tomography (CT) with at least 1-year interval and adipose tissue measurement using non-contrast CT at baseline for a routine checkup between 2003 and 2015. CAC progression, the main outcome, was defined as a difference of ≥2.5 between the square roots of the baseline and follow-up CAC scores using Agatston units.
Results
During follow-up (median 39 months), 37.5% of subjects showed CAC progression of a total population (56.4 years, 80.6% male). Body mass index (BMI) ≥25 kg/m2, increasing waist circumferences (WC), and higher VAT/subcutaneous adipose tissue (SAT) area ratio were independently associated with CAC progression. Particularly, predominance of VAT over SAT at ≥30% showed the strongest prediction for CAC progression (adjusted hazard ratio, 2.20; P<0.001) and remained of prognostic value regardless of BMI or WC status. Further, it provided improved risk stratification of CAC progression beyond known prognosticators.
Conclusion
Predominant VAT area on CT is the strongest predictor of CAC progression regardless of BMI or WC in apparently healthy Korean population. Assessment of body fat distribution may be helpful to identify subjects at higher risk. -
Citations
Citations to this article as recorded by- Gender-specific abdominal fat distribution and insulin resistance associated with organophosphate esters and phthalate metabolites exposure
Xiaoliu Shi, Wanyue Wang, Jiafan Feng, Xiaochun Ma, Mengting Xu, Cui Wang
Environmental Pollution.2024; 349: 123959. CrossRef - The association between C-reactive protein and coronary artery calcification: a systematic review and meta-analysis
Amirhossein Tajani, Masoumeh Sadeghi, Navid Omidkhoda, Amir Hooshang Mohammadpour, Sara Samadi, Vahid Jomehzadeh
BMC Cardiovascular Disorders.2024;[Epub] CrossRef - Visceral adipose tissue is an independent predictor and mediator of the progression of coronary calcification: a prospective sub-analysis of the GEA study
Neftali Eduardo Antonio-Villa, Juan Gabriel Juárez-Rojas, Rosalinda Posadas-Sánchez, Juan Reyes-Barrera, Aida Medina-Urrutia
Cardiovascular Diabetology.2023;[Epub] CrossRef - Deep learning-based prediction for significant coronary artery stenosis on coronary computed tomography angiography in asymptomatic populations
Heesun Lee, Bong Gyun Kang, Jeonghee Jo, Hyo Eun Park, Sungroh Yoon, Su-Yeon Choi, Min Joo Kim
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Relationship between a novel non–insulin-based metabolic score for insulin resistance (METS‐IR) and coronary artery calcification
Zhenwei Wang, Xiaofang Hui, Xu Huang, Jingjie Li, Naifeng Liu
BMC Endocrine Disorders.2022;[Epub] CrossRef - Association Between Abdominal Adipose Tissue Distribution and Risk of Endometrial Cancer: A Case-Control Study
Yuan Cheng, Zhongyu Wang, Xiaoxuan Jia, Rong Zhou, Jianliu Wang
Clinical Medicine Insights: Oncology.2022; 16: 117955492211407. CrossRef - Sex differences in cardiovascular risk may be related to sex differences in diet patterns: a narrative review
A. M. Tindall, V. A. Stallings
Annals of Human Biology.2021; 48(6): 517. CrossRef
- Gender-specific abdominal fat distribution and insulin resistance associated with organophosphate esters and phthalate metabolites exposure
- Metabolic Risk/Epidemiology
- Association of Soybean Food Intake and Cardiometabolic Syndrome in Korean Women: Korea National Health and Nutrition Examination Survey (2007 to 2011)
- Sook-Hyun Jun, Woo-Kyoung Shin, Yookyung Kim
- Diabetes Metab J. 2020;44(1):143-157. Published online December 2, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0078
- 5,737 View
- 68 Download
- 6 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Soybean food consumption has been considered as a possible way to lower incidence of cardiometabolic syndrome (CMS) among Asians. However, results from studies investigating its efficacy on CMS in Asians have been inconsistent.
Methods We analyzed the association between soybean intake frequency and prevalence of CMS based on data from the Korea National Health and Nutrition Examination Survey 2007 to 2011. Data of 9,287 women aged 20 to 64 years were analyzed. Food frequency questionnaire was used to assess soybean food consumption frequency. General linear model and multivariable logistic regression model were used to examine the association of soybean intake quintile with CMS and its risk factors. Least square means of metabolic factors mostly showed no significant relevance except liver indexes.
Results Compared to participants in the 1st quintile (<2 times/week of soybean food), odds ratios (OR) for CMS and abdominal obesity (AO) in the 4th quintile (8.5 times/week<soybean food≤17 times/week) were 0.73 (95% confidence interval [CI], 0.57 to 0.95) and 0.72 (95% CI, 0.58 to 0.90), respectively. After excluding Tofu products, ORs of CMS, AO, high blood pressure, and hypertriglyceridemia were lower than those without excluding Tofu products. However, results still did not show significant inverse linear trend across frequency quintiles.
Conclusion Our findings suggest that soybean intake of 8.5 to 17 times/week was inversely associated with CMS in Korean women. The relation between soybean intake >17 times/week and CMS varied depending on soybean food items.
-
Citations
Citations to this article as recorded by- Anti-obesogenic effects of plant natural products: A focus on Korean traditional foods
Gitishree Das, Luis Alfonso Jiménez Ortega, Sandra Gonçalves, J. Basilio Heredia, Maria de Lourdes Gomes Pereira, Anabela Romano, Han-Seung Shin, Jayanta Kumar Patra
Trends in Food Science & Technology.2024; : 104470. CrossRef - Sex differences in waist circumference obesity and eating speed: a cross-sectional study of Japanese people with normal body mass index
Yuri Yaguchi, Tsuneo Konta, Nahomi Imaeda, Chiho Goto, Yoshiyuki Ueno, Takamasa Kayama
Frontiers in Nutrition.2024;[Epub] CrossRef - Association of Dietary Patterns with Metabolic Syndrome in Chinese Children and Adolescents Aged 7–17: The China National Nutrition and Health Surveillance of Children and Lactating Mothers in 2016–2017
Jia Shi, Hongyun Fang, Qiya Guo, Dongmei Yu, Lahong Ju, Xue Cheng, Wei Piao, Xiaoli Xu, Zizi Li, Di Mu, Liyun Zhao, Li He
Nutrients.2022; 14(17): 3524. CrossRef - What Is the Relationship between Antioxidant Efficacy, Functional Composition, and Genetic Characteristics in Comparing Soybean Resources by Year?
Han-Na Chu, Suji Lee, Xiaohan Wang, Chi-Do Wee, Hye-Myeong Yoon, Eun-Suk Jung, Mi-Kyung Seo, Yongseok Kwon, Kyeong-A Jang, Haeng-Ran Kim
Antioxidants.2022; 11(11): 2249. CrossRef - Longitudinal changes in adherence to the portfolio and DASH dietary patterns and cardiometabolic risk factors in the PREDIMED-Plus study
Andrea J. Glenn, Pablo Hernández-Alonso, Cyril W.C. Kendall, Miguel Ángel Martínez-González, Dolores Corella, Montserrat Fitó, J.Alfredo Martínez, Ángel M. Alonso-Gómez, Julia Wärnberg, Jesús Vioque, Dora Romaguera, José López-Miranda, Ramon Estruch, Fran
Clinical Nutrition.2021; 40(5): 2825. CrossRef - The Effects of Dietary Pattern on Metabolic Syndrome in Jiangsu Province of China: Based on a Nutrition and Diet Investigation Project in Jiangsu Province
Yuanyuan Wang, Yue Dai, Ting Tian, Jingxian Zhang, Wei Xie, Da Pan, Dengfeng Xu, Yifei Lu, Shaokang Wang, Hui Xia, Guiju Sun
Nutrients.2021; 13(12): 4451. CrossRef - Sex-Specific Energy Intakes and Physical Activity Levels According to the Presence of Metabolic Syndrome in Korean Elderly People: Korean National Health and Nutrition Examination Survey 2016–2018
Won-Sang Jung, Hun-Young Park, Sung-Woo Kim, Kiwon Lim
International Journal of Environmental Research and Public Health.2020; 17(15): 5416. CrossRef
- Anti-obesogenic effects of plant natural products: A focus on Korean traditional foods
- Obesity and Metabolic Syndrome
- Comparison of Competitive Models of Metabolic Syndrome Using Structural Equation Modeling: A Confirmatory Factor Analysis
- Karimollah Hajian-Tilaki
- Diabetes Metab J. 2018;42(5):433-441. Published online October 22, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0010
- 3,232 View
- 41 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The purpose of this study was to apply the structural equation modeling (SEM) to compare the fitness of different competing models (one, two, and three factors) of the metabolic syndrome (MetS) in Iranian adult population.
Methods Data are given on the cardiometabolic risk factors of 841 individuals with nondiabetic adults from a cross-sectional population-based study of glucose, lipids, and MetS in the north of Iran. The three conceptual hypothesized models (single factor, two correlated factors, and three correlated latent factors) were evaluated by using confirmatory factor analysis with the SEM approach. The summary statistics of correlation coefficients and the model summary fitting indexes were calculated.
Results The findings show that a single-factor model and a two-correlated factor model had a poorer summary fitting index compared with a three-correlated factor model. All fitting criteria met the conceptual hypothesized three-correlated factor model for both sexes. However, the correlation structure between the three underlying constructs designating the MetS was higher in women than in men.
Conclusion These results indicate the plausibility of the pathophysiology and etiology of MetS being multifactorial, rather than a single factor, in a nondiabetic Iranian adult population.
-
Citations
Citations to this article as recorded by- Structural Equation Modelling for Predicting the Relative Contribution of Each Component in the Metabolic Syndrome Status Change
José E. Teixeira, José A. Bragada, João P. Bragada, Joana P. Coelho, Isabel G. Pinto, Luís P. Reis, Paula O. Fernandes, Jorge E. Morais, Pedro M. Magalhães
International Journal of Environmental Research and Public Health.2022; 19(6): 3384. CrossRef - New risk score model for identifying individuals at risk for diabetes in southwest China
Liying Li, Ziqiong Wang, Muxin Zhang, Haiyan Ruan, Linxia Zhou, Xin Wei, Ye Zhu, Jiafu Wei, Sen He
Preventive Medicine Reports.2021; 24: 101618. CrossRef - Definition and early diagnosis of metabolic syndrome in children
Gunter Matthias Christian Flemming, Sarah Bussler, Antje Körner, Wieland Kiess
Journal of Pediatric Endocrinology and Metabolism.2020; 33(7): 821. CrossRef - Calcium-Sensing Receptor in Adipose Tissue: Possible Association with Obesity-Related Elevated Autophagy
Pamela Mattar, Sofía Sanhueza, Gabriela Yuri, Lautaro Briones, Claudio Perez-Leighton, Assaf Rudich, Sergio Lavandero, Mariana Cifuentes
International Journal of Molecular Sciences.2020; 21(20): 7617. CrossRef
- Structural Equation Modelling for Predicting the Relative Contribution of Each Component in the Metabolic Syndrome Status Change
- Obesity and Metabolic Syndrome
- Proportion and Characteristics of the Subjects with Low Muscle Mass and Abdominal Obesity among the Newly Diagnosed and Drug-Naïve Type 2 Diabetes Mellitus Patients
- Jung A Kim, Soon Young Hwang, Hye Soo Chung, Nam Hoon Kim, Ji A Seo, Sin Gon Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
- Diabetes Metab J. 2019;43(1):105-113. Published online September 28, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0036
- 4,908 View
- 70 Download
- 12 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Sarcopenic obesity (SO) is a serious public health concern, few studies have examined the clinical implications of SO in newly-diagnosed type 2 diabetes mellitus (T2DM) patients. We evaluated the prevalence of the newly diagnosed, drug-naïve T2DM patients with low muscle mass with abdominal obesity and its association with insulin resistance and other diabetic complications.
Methods We classified 233 drug-naïve T2DM subjects into four groups according to abdominal obesity (waist circumference ≥90 cm in men and ≥85 cm in women) and low muscle mass status (appendicular skeletal muscle <7.0 kg/m2 for men and <5.4 kg/m2 for women).
Results The proportion of the subjects with low muscle mass and abdominal obesity among the newly diagnosed, drug-naïve T2DM patients was 8.2%. Homeostasis model assessment of insulin resistance (HOMA-IR) increased linearly according to body composition group from normal to abdominal obesity to both low muscle mass and abdominal obesity. The multiple logistic regression analysis indicated that subjects with low muscle mass and abdominal obesity (odds ratio [OR], 9.39; 95% confidence interval [CI], 2.41 to 36.56) showed a higher risk for insulin resistance, defined as HOMA-IR ≥3, than those with abdominal obesity (OR, 5.36; 95% CI, 2.46 to 11.69), even after adjusting for other covariates. However, there were no differences in lipid profiles, microalbuminuria, or various surrogate markers for atherosclerosis among the four groups.
Conclusion Subjects with both low muscle mass and abdominal obesity had a higher risk of insulin resistance than those with low muscle mass or abdominal obesity only.
-
Citations
Citations to this article as recorded by- Clinical observation on acupuncture for 80 patients with abdominal obesity in Germany: based on the theory of unblocking and regulating the Belt Vessel
Yuanyuan Li, Hang Xiong, Shuhui Ma, Jingzhang Dai
Journal of Acupuncture and Tuina Science.2023; 21(2): 137. CrossRef - Waist circumference and end‐stage renal disease based on glycaemic status: National Health Insurance Service data 2009–2018
Yun Kyung Cho, Ji Hye Huh, Shinje Moon, Yoon Jung Kim, Yang‐Hyun Kim, Kyung‐do Han, Jun Goo Kang, Seong Jin Lee, Sung‐Hee Ihm
Journal of Cachexia, Sarcopenia and Muscle.2023; 14(1): 585. CrossRef - Incidence of sarcopenic obesity in older patients with diabetes and association between sarcopenic obesity and higher-level functional capacity: evaluation based on a consensus statement
Satoshi Ida, Ryutaro Kaneko, Kanako Imataka, Kaoru Okubo, Kentaro Azuma, Kazuya Murata
Endocrine Journal.2023; 70(6): 591. CrossRef - A Novel Anthropometric Parameter, Weight-Adjusted Waist Index Represents Sarcopenic Obesity in Newly Diagnosed Type 2 Diabetes Mellitus
Min Jeong Park, Soon Young Hwang, Nam Hoon Kim, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
Journal of Obesity & Metabolic Syndrome.2023; 32(2): 130. CrossRef - Prevalence of sarcopenic obesity in patients with diabetes and adverse outcomes: A systematic review and meta-analysis
Yuan-yuan Zhou, Jin-feng Wang, Qian Yao, Qiu-feng Jian, Zhi-peng Luo
Clinical Nutrition ESPEN.2023; 58: 128. CrossRef - The Correlation Between Leg Muscle Mass Index and Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Mellitus
Menggege Liu, Qing Zhang, Juan Liu, Huiling Bai, Ping Yang, Xinhua Ye, Xiaoqing Yuan
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 4169. CrossRef - Sarcopenic Obesity with Normal Body Size May Have Higher Insulin Resistance in Elderly Patients with Type 2 Diabetes Mellitus
Tingting Han, Ting Yuan, Xinyue Liang, Ningxin Chen, Jia Song, Xin Zhao, Yurong Weng, Yaomin Hu
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 1197. CrossRef - Relationship between Visceral Adipose Index, Lipid Accumulation Product and Type 2 Diabetes Mellitus
停停 陈
Advances in Clinical Medicine.2022; 12(04): 3350. CrossRef - Assessment of the relationship between prediabetes and low skeletal mass based on blood creatinine level
S. I. Ibragimova, G. O. Nuskabayeva, Z. N. Shalkharova, K. Zh. Sadykova, G. A. Junusbekova, M. Oran
Diabetes mellitus.2022; 25(3): 226. CrossRef - Changes in body composition and low blood urea nitrogen level related to an increase in the prevalence of fatty liver over 20 years: A cross‐sectional study
Yasushi Imamura, Seiichi Mawatari, Kohei Oda, Kotaro Kumagai, Yasunari Hiramine, Akiko Saishoji, Atsuko Kakihara, Mai Nakahara, Manei Oku, Kaori Hosoyamada, Shuji Kanmura, Akihiro Moriuchi, Hironori Miyahara, Akio ido
Hepatology Research.2021; 51(5): 570. CrossRef - Body Composition and Diabetes
Hye Jin Yoo
The Journal of Korean Diabetes.2021; 22(4): 238. CrossRef - Reduced Skeletal Muscle Volume and Increased Skeletal Muscle Fat Deposition Characterize Diabetes in Individuals after Pancreatitis: A Magnetic Resonance Imaging Study
Andre E. Modesto, Juyeon Ko, Charlotte E. Stuart, Sakina H. Bharmal, Jaelim Cho, Maxim S. Petrov
Diseases.2020; 8(3): 25. CrossRef - Low alanine aminotransferase levels predict low muscle strength in older patients with diabetes: A nationwide cross‐sectional study in Korea
Seung Min Chung, Jun Sung Moon, Ji Sung Yoon, Kyu Chang Won, Hyoung Woo Lee
Geriatrics & Gerontology International.2020; 20(4): 271. CrossRef - Association between sarcopenic obesity and higher risk of type 2 diabetes in adults: A systematic review and meta-analysis
Dima Khadra, Leila Itani, Hana Tannir, Dima Kreidieh, Dana El Masri, Marwan El Ghoch
World Journal of Diabetes.2019; 10(5): 311. CrossRef
- Clinical observation on acupuncture for 80 patients with abdominal obesity in Germany: based on the theory of unblocking and regulating the Belt Vessel
- Obesity and Metabolic Syndrome
- Serum Calcium and the Risk of Incident Metabolic Syndrome: A 4.3-Year Retrospective Longitudinal Study
- Jong Ha Baek, Sang-Man Jin, Ji Cheol Bae, Jae Hwan Jee, Tae Yang Yu, Soo Kyoung Kim, Kyu Yeon Hur, Moon-Kyu Lee, Jae Hyeon Kim
- Diabetes Metab J. 2017;41(1):60-68. Published online December 26, 2016
- DOI: https://doi.org/10.4093/dmj.2017.41.1.60
- 4,079 View
- 32 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background An association between serum calcium level and risk of metabolic syndrome (MetS) has been suggested in cross-sectional studies. This study aimed to evaluate the association between baseline serum calcium level and risk of incident MetS in a longitudinal study.
Methods We conducted a retrospective longitudinal study of 12,706 participants without MetS who participated in a health screening program, had normal range serum calcium level at baseline (mean age, 51 years), and were followed up for 4.3 years (18,925 person-years). The risk of developing MetS was analyzed according to the baseline serum calcium levels.
Results A total of 3,448 incident cases (27.1%) of MetS developed during the follow-up period. The hazard ratio (HR) for incident MetS did not increase with increasing tertile of serum calcium level in an age- and sex-matched model (
P for trend=0.915). The HRs (95% confidence interval [CI]) for incident MetS comparing the second and the third tertiles to the first tertile of baseline serum calcium level were 0.91 (95% CI, 0.84 to 0.99) and 0.85 (95% CI, 0.78 to 0.92) in a fully adjusted model, respectively (P for trend=0.001). A decreased risk of incident MetS in higher tertiles of serum calcium level was observed in subjects with central obesity and/or a metabolically unhealthy state at baseline.Conclusion There was no positive correlation between baseline serum calcium levels and incident risk of MetS in this longitudinal study. There was an association between higher serum calcium levels and decreased incident MetS in individuals with central obesity or two components of MetS at baseline.
-
Citations
Citations to this article as recorded by- Independent associations of serum calcium with or without albumin adjustment and serum phosphorus with nonalcoholic fatty liver disease: results from NHANES 1999-2018
Haolong Qi, Bin Wang, Lei Zhu
Frontiers in Endocrinology.2024;[Epub] CrossRef - Association of the serum calcium level with metabolic syndrome and its components among adults in Taiwan
Jer-min Chen, Tai-yin Wu, Yi-fan Wu, Kuan-liang Kuo
Archives of Endocrinology and Metabolism.2023;[Epub] CrossRef - Elevated Chinese visceral adiposity index increases the risk of stroke in Chinese patients with metabolic syndrome
Zeyu Liu, Qin Huang, Bi Deng, Minping Wei, Xianjing Feng, Fang Yu, Jie Feng, Yang Du, Jian Xia
Frontiers in Endocrinology.2023;[Epub] CrossRef - Metformin: Expanding the Scope of Application—Starting Earlier than Yesterday, Canceling Later
Yulia A. Kononova, Nikolai P. Likhonosov, Alina Yu. Babenko
International Journal of Molecular Sciences.2022; 23(4): 2363. CrossRef - Metformin in prediabetes: key mechanisms for the prevention of diabetes and cardiometabolic risks
A. Yu. Babenko
Meditsinskiy sovet = Medical Council.2022; (10): 96. CrossRef Calcium and Phosphate Levels are Among Other Factors Associated with Metabolic Syndrome in Patients with Normal Weight
Kamila Osadnik, Tadeusz Osadnik, Marcin Delijewski, Mateusz Lejawa, Martyna Fronczek, Rafał Reguła, Mariusz Gąsior, Natalia Pawlas
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 1281. CrossRef- Association between selected trace elements and body mass index and waist circumference: A cross sectional study
Mahnaz Zohal, Saeedeh Jam-Ashkezari, Nasim Namiranian, Amin Moosavi, Akram Ghadiri-Anari
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(2): 1293. CrossRef - Letter: Increased Serum Angiopoietin-Like 6 Ahead of Metabolic Syndrome in a Prospective Cohort Study (Diabetes Metab J 2019;43:521-9)
Jin Hwa Kim
Diabetes & Metabolism Journal.2019; 43(5): 727. CrossRef - Genotype effects of glucokinase regulator on lipid profiles and glycemic status are modified by circulating calcium levels: results from the Korean Genome and Epidemiology Study
Oh Yoen Kim, So-Young Kwak, Hyunjung Lim, Min-Jeong Shin
Nutrition Research.2018; 60: 96. CrossRef
- Independent associations of serum calcium with or without albumin adjustment and serum phosphorus with nonalcoholic fatty liver disease: results from NHANES 1999-2018
- Optimal Waist Circumference Cutoff Value Based on Insulin Resistance and Visceral Obesity in Koreans with Type 2 Diabetes
- Jung Soo Lim, Young Ju Choi, Soo-Kyung Kim, Byoung Wook Huh, Eun Jig Lee, Kap Bum Huh
- Diabetes Metab J. 2015;39(3):253-263. Published online April 24, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.3.253
- 4,294 View
- 28 Download
- 10 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Visceral obesity is the most powerful contributor to the development of metabolic syndrome (MetS) and cardiovascular diseases. In light of visceral obesity, however, there is a paucity of data on the appropriate cutoff point of waist circumference (WC) in subjects with type 2 diabetes. The aim of this study was to investigate the optimal cutoff value for WC that signals insulin resistance (IR) and visceral obesity in Koreans with type 2 diabetes.
Methods We evaluated 4,252 patients with type 2 diabetes (male 2,220, female 2,032, mean age 57.24 years) who visited our clinic between January 2003 and June 2009. WC was measured at the midpoint between the lower rib and the iliac crest, and insulin sensitivity was assessed by the rate constant of plasma glucose disappearance (
Kitt %/min) using an insulin tolerance test. Visceral fat thickness was measured using ultrasonography. Statistical analysis was performed using receiver operating characteristic curve.Results The optimal cutoff points for WC for identifying the presence of IR and visceral obesity, as well as two or more metabolic components, were 87 cm for men and 81 cm for women. Moreover, these cutoff points had the highest predictive powers for the presence of visceral obesity. The MetS defined by new criteria correlated with the increased carotid intima-media thickness in female subjects.
Conclusion Our results suggest that the optimal cutoff values for WC in Koreans with type 2 diabetes should be reestablished based on IR and visceral obesity.
-
Citations
Citations to this article as recorded by- Association between Muscle Mass, Body Fat Mass, and Abdominal Circumstances with Insulin Resistance among Young Adult Population with Prediabetes Risk
Anindya Putri Adhisti, Siti Fatimah-Muis, Amalia Sukmadianti, Darmono S.S., Febe Christianto
The Indian Journal of Nutrition and Dietetics.2023; : 176. CrossRef - Brazil nut prevents oxidative DNA damage in type 2 diabetes patients
Tamires Pavei Macan, Thais Aquino de Amorim, Adriani Paganini Damiani, Ângela Caroline da Luz Beretta, Marina Lummertz Magenis, Thais Ceresér Vilela, João Paulo Teixeira, Vanessa Moraes de Andrade
Drug and Chemical Toxicology.2022; 45(3): 1066. CrossRef - Metabolic Syndrome and Breast Cancer Molecular Subtypes: An Observational Patient Study
Dafina Ademi-Islami, Suzana Manxhuka-Kerliu, Dhurata Tarifa-Koroveshi, Rozafa Koliqi, Blerim Mujaj
Breast Cancer: Basic and Clinical Research.2022; 16: 117822342210805. CrossRef - Performance of Two Novel Obesity Indicators for the Management of Metabolic Syndrome in Young Adults
Xiaoli Liu, Chunpeng Ma, Fuzai Yin, Rui Wang, Qiang Lu, Na Lu, Chunming Ma
Frontiers in Endocrinology.2021;[Epub] CrossRef - Differential effect of subcutaneous abdominal and visceral adipose tissue on cardiometabolic risk
Susan Sam
Hormone Molecular Biology and Clinical Investigation.2018;[Epub] CrossRef - Three novel obese indicators perform better in monitoring management of metabolic syndrome in type 2 diabetes
Chun-Ming Ma, Na Lu, Rui Wang, Xiao-Li Liu, Qiang Lu, Fu-Zai Yin
Scientific Reports.2017;[Epub] CrossRef - Association between Body Weight Changes and Menstrual Irregularity: The Korea National Health and Nutrition Examination Survey 2010 to 2012
Kyung Min Ko, Kyungdo Han, Youn Jee Chung, Kun-Ho Yoon, Yong Gyu Park, Seung-Hwan Lee
Endocrinology and Metabolism.2017; 32(2): 248. CrossRef - The renal tubular damage marker urinary N-acetyl-β-d-glucosaminidase may be more closely associated with early detection of atherosclerosis than the glomerular damage marker albuminuria in patients with type 2 diabetes
So Ra Kim, Yong-ho Lee, Sang-Guk Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Cardiovascular Diabetology.2017;[Epub] CrossRef - The association between metabolic health, obesity phenotype and the risk of breast cancer
Yong‐Moon Mark Park, Alexandra J. White, Hazel B. Nichols, Katie M. O'Brien, Clarice R. Weinberg, Dale P. Sandler
International Journal of Cancer.2017; 140(12): 2657. CrossRef - Reappraisal of waist circumference cutoff value according to general obesity
Kyung-Soo Kim, Hyun-Ju Oh, Young Ju Choi, Byung Wook Huh, Soo-Kyung Kim, Seok Won Park, Eun Jig Lee, Yong-Wook Cho, Kap-Bum Huh
Nutrition & Metabolism.2016;[Epub] CrossRef
- Association between Muscle Mass, Body Fat Mass, and Abdominal Circumstances with Insulin Resistance among Young Adult Population with Prediabetes Risk
- A Cross-Sectional Study of the Phenotypes of Obesity and Insulin Resistance in Adults with Down Syndrome
- Diego Real de Asua, Pedro Parra, Ramón Costa, Fernando Moldenhauer, Carmen Suarez
- Diabetes Metab J. 2014;38(6):464-471. Published online December 15, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.6.464
- 3,555 View
- 47 Download
- 24 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Despite the confluence of multiple cardiovascular risk factors, subclinical atherosclerotic damage and cardiovascular events remain extremely rare in adults with Down syndrome (DS). We aim to determine the prevalence of obesity and metabolic disorders in an adult cohort with DS and to compare our findings with adults without DS.
Methods Cross-sectional study of 51 consecutively selected adults with DS living in the community and 51 healthy controls in an outpatient clinic of a tertiary care hospital in Madrid, Spain. Epidemiological data (age and gender), anthropometric data (body mass index and waist-to-height ratio), coexisting clinical conditions, and laboratory data (fasting glucose, insulin, glycated hemoglobin, creatinine, thyroid hormones, vitamins, and lipid profile) were measured and compared between the groups.
Results Adults with DS were significantly younger and more often men with a higher prevalence of overweight and obesity than controls. Their waist-to-height ratio was higher, and they more frequently had abdominal obesity. The results of an analysis adjusted for age and gender revealed no differences in fasting insulin levels, homeostatic model assessment indexes, or lipid profile between adults with DS and controls.
Conclusion Adults with DS presented a high prevalence of overweight and obesity. However, we found no differences in lipid profile, prevalence of insulin resistance, or metabolic syndrome between adults with DS and controls.
-
Citations
Citations to this article as recorded by- Obesity, diabetes and their metabolic correlates in middle‐aged adults with Down syndrome
J. A. Luchsinger, D. Pang, S. J. Krinsky‐McHale, N. Schupf, J. H. Lee, W. Silverman, W. B. Zigman
Journal of Intellectual Disability Research.2024; 68(3): 212. CrossRef - Differentiation of the body build and posture in the population of people with intellectual disabilities and Down Syndrome: a systematic review
Eliza Gaweł, Diana Celebańska, Anna Zwierzchowska
BMC Public Health.2024;[Epub] CrossRef - Cardiometabolic profiles in children and adults with overweight and obesity and down syndrome
Nicolas M. Oreskovic, Nicole T. Baumer, Chiara Di Camillo, Michelle Cornachia, Catherine Franklin, Sarah J. Hart, Priya S. Kishnani, Andrew McCormick, Anna L. Milliken, Vasiliki Patsiogiannis, Katherine G. Pawlowski, Stephanie L. Santoro, Sabrina Sargado,
American Journal of Medical Genetics Part A.2023; 191(3): 813. CrossRef - Long-Term Effects of SARS-CoV-2 in the Brain: Clinical Consequences and Molecular Mechanisms
Ann-Charlotte Granholm
Journal of Clinical Medicine.2023; 12(9): 3190. CrossRef - Cut‐off points for isometric handgrip and low limb explosive strength in relation to indicators of overweight/obesity in people with intellectual disabilities: analysis by age groups
P. Ferrero‐Hernández, C. Farías‐Valenzuela, G. Ferrari, S. Espoz‐Lazo, S. Álvarez‐Arangua, P. Valdivia‐Moral
Journal of Intellectual Disability Research.2023; 67(11): 1124. CrossRef - Metabolic Diseases and Down Syndrome: How Are They Linked Together?
Manon Moreau, Soukaina Benhaddou, Rodolphe Dard, Stefania Tolu, Rim Hamzé, François Vialard, Jamileh Movassat, Nathalie Janel
Biomedicines.2021; 9(2): 221. CrossRef - Effects of Motor-Games-Based Concurrent Training Program on Body Composition Indicators of Chilean Adults with Down Syndrome
Claudio Farías-Valenzuela, Cristian Cofré-Bolados, Gerson Ferrari, Sebastián Espoz-Lazo, Giovanny Arenas-Sánchez, Sebastián Álvarez-Arangua, Alexis Espinoza-Salinas, Pedro Valdivia-Moral
Sustainability.2021; 13(10): 5737. CrossRef - PNPLA3 gene polymorphism is associated with liver steatosis in children with Down syndrome
Diletta Valentini, Antonella Mosca, Chiara Di Camillo, Annalisa Crudele, Maria Rita Sartorelli, Vittorio Scoppola, Luigi Tarani, Alberto Villani, Massimiliano Raponi, Antonio Novelli, Anna Alisi
Nutrition, Metabolism and Cardiovascular Diseases.2020; 30(9): 1564. CrossRef - Co‐occurring medical conditions in adults with Down syndrome: A systematic review toward the development of health care guidelines. Part II
George Capone, Mary Stephens, Stephanie Santoro, Brian Chicoine, Peter Bulova, Moya Peterson, Joan Jasien, Anna Jo Smith
American Journal of Medical Genetics Part A.2020; 182(7): 1832. CrossRef - Adults with Down syndrome challenge another paradigm: When aging no longer entails arterial hypertension
Emilia Roy‐Vallejo, José María Galván‐Román, Fernando Moldenhauer, Diego Real de Asúa
The Journal of Clinical Hypertension.2020; 22(7): 1127. CrossRef - Metabolic syndrome and its components in people with intellectual disability: a meta‐analysis
D. Vancampfort, F. Schuch, T. Van Damme, J. Firth, S. Suetani, B. Stubbs, D. Van Biesen
Journal of Intellectual Disability Research.2020; 64(10): 804. CrossRef - Evaluation of biochemical and hematological parameters in adults with Down syndrome
David de Gonzalo-Calvo, Isabel Barroeta, Madalina Nicoleta Nan, José Rives, Diana Garzón, María Carmona-Iragui, Bessy Benejam, Laura Videla, Susana Fernández, Miren Altuna, Sílvia Valldeneu, Rafael Blesa, Alberto Lleó, Francisco Blanco-Vaca, Juan Fortea,
Scientific Reports.2020;[Epub] CrossRef - Meta-analysis of metabolites involved in bioenergetic pathways reveals a pseudohypoxic state in Down syndrome
Laszlo Pecze, Elisa B. Randi, Csaba Szabo
Molecular Medicine.2020;[Epub] CrossRef - Diurnal cortisol and obesity in adolescents with and without Down syndrome
E. A. Pitchford, R. E. Hasson, J. E. Hornyak, J. C. Lumeng, K. E. Peterson, D. A. Ulrich
Journal of Intellectual Disability Research.2019; 63(12): 1401. CrossRef - Cardiometabolic Risk and Body Composition in Youth With Down Syndrome
Sheela N. Magge, Babette S. Zemel, Mary E. Pipan, Samuel S. Gidding, Andrea Kelly
Pediatrics.2019;[Epub] CrossRef - Acanthosis nigricans and the metabolic syndrome
Ayse Serap Karadağ, Yi You, Retno Danarti, Safaa Al-Khuzaei, WenChieh Chen
Clinics in Dermatology.2018; 36(1): 48. CrossRef - Co‐occurring medical conditions in adults with Down syndrome: A systematic review toward the development of health care guidelines
George T. Capone, Brian Chicoine, Peter Bulova, Mary Stephens, Sarah Hart, Blythe Crissman, Andrea Videlefsky, Katherine Myers, Nancy Roizen, Anna Esbensen, Moya Peterson, Stephanie Santoro, Jason Woodward, Barry Martin, David Smith
American Journal of Medical Genetics Part A.2018; 176(1): 116. CrossRef - Recomendaciones para la atención a los adultos con síndrome de Down. Revisión de la literatura
M. González-Cerrajero, M. Quero-Escalada, F. Moldenhauer, C. Suárez Fernández
Medicina de Familia. SEMERGEN.2018; 44(5): 342. CrossRef - Systematic review and meta-analysis shows a specific micronutrient profile in people with Down Syndrome: Lower blood calcium, selenium and zinc, higher red blood cell copper and zinc, and higher salivary calcium and sodium
Amene Saghazadeh, Maryam Mahmoudi, Atefeh Dehghani Ashkezari, Nooshin Oliaie Rezaie, Nima Rezaei, Jacobus P. van Wouwe
PLOS ONE.2017; 12(4): e0175437. CrossRef - Cardiovascular and general health status of adults with Trisomy 21
Samuel A. Hayes, Shelby Kutty, Joshua Thomas, Joyce T. Johnson, Anji T. Yetman
International Journal of Cardiology.2017; 241: 173. CrossRef - Feasibility of Assessing Diet with a Mobile Food Record for Adolescents and Young Adults with Down Syndrome
Katherine Bathgate, Jill Sherriff, Helen Leonard, Satvinder Dhaliwal, Edward Delp, Carol Boushey, Deborah Kerr
Nutrients.2017; 9(3): 273. CrossRef - Coenzyme Q10 and pro-inflammatory markers in children with Down syndrome: clinical and biochemical aspects
Moushira E. Zaki, Hala T. El-Bassyouni, Angie M.S. Tosson, Eman Youness, Jihan Hussein
Jornal de Pediatria (Versão em Português).2017; 93(1): 100. CrossRef - Coenzyme Q10 and pro-inflammatory markers in children with Down syndrome: clinical and biochemical aspects
Moushira E. Zaki, Hala T. El-Bassyouni, Angie M.S. Tosson, Eman Youness, Jihan Hussein
Jornal de Pediatria.2017; 93(1): 100. CrossRef - Retrospective Study of Obesity in Children with Down Syndrome
Janet S. Basil, Stephanie L. Santoro, Lisa J. Martin, Katherine Wusik Healy, Barbara A. Chini, Howard M. Saal
The Journal of Pediatrics.2016; 173: 143. CrossRef
- Obesity, diabetes and their metabolic correlates in middle‐aged adults with Down syndrome

 KDA
KDA
 First
First Prev
Prev





