
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Drug/Regimen
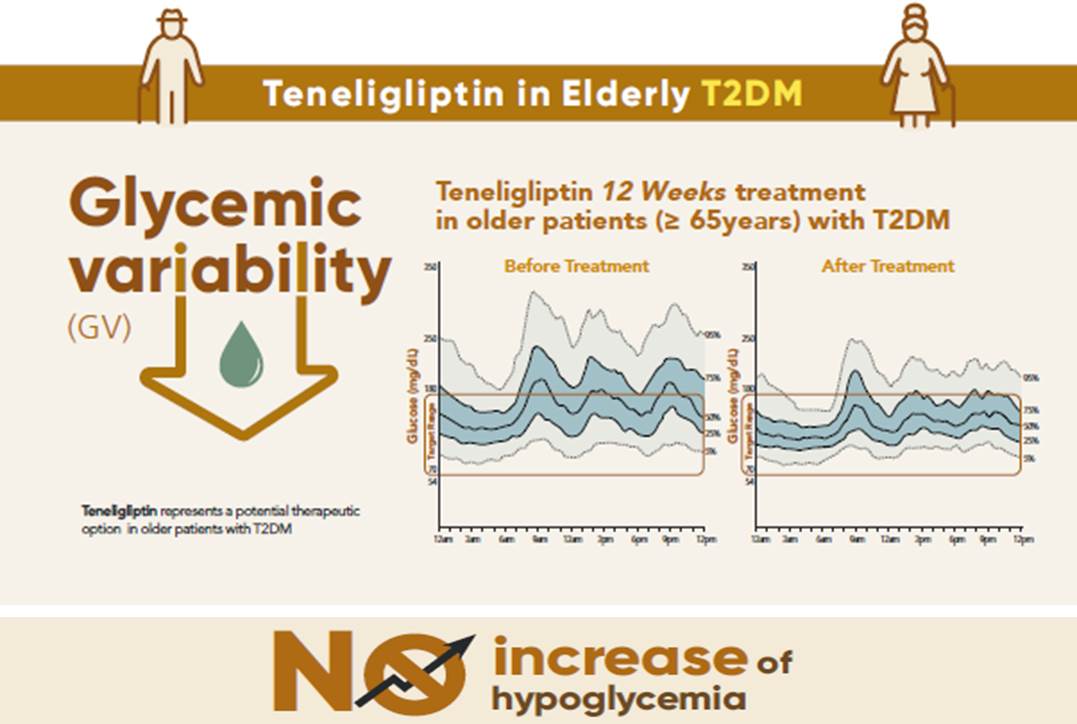
- Effects of Teneligliptin on HbA1c levels, Continuous Glucose Monitoring-Derived Time in Range and Glycemic Variability in Elderly Patients with T2DM (TEDDY Study)
- Ji Cheol Bae, Soo Heon Kwak, Hyun Jin Kim, Sang-Yong Kim, You-Cheol Hwang, Sunghwan Suh, Bok Jin Hyun, Ji Eun Cha, Jong Chul Won, Jae Hyeon Kim
- Diabetes Metab J. 2022;46(1):81-92. Published online June 16, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0016
- 7,595 View
- 431 Download
- 5 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 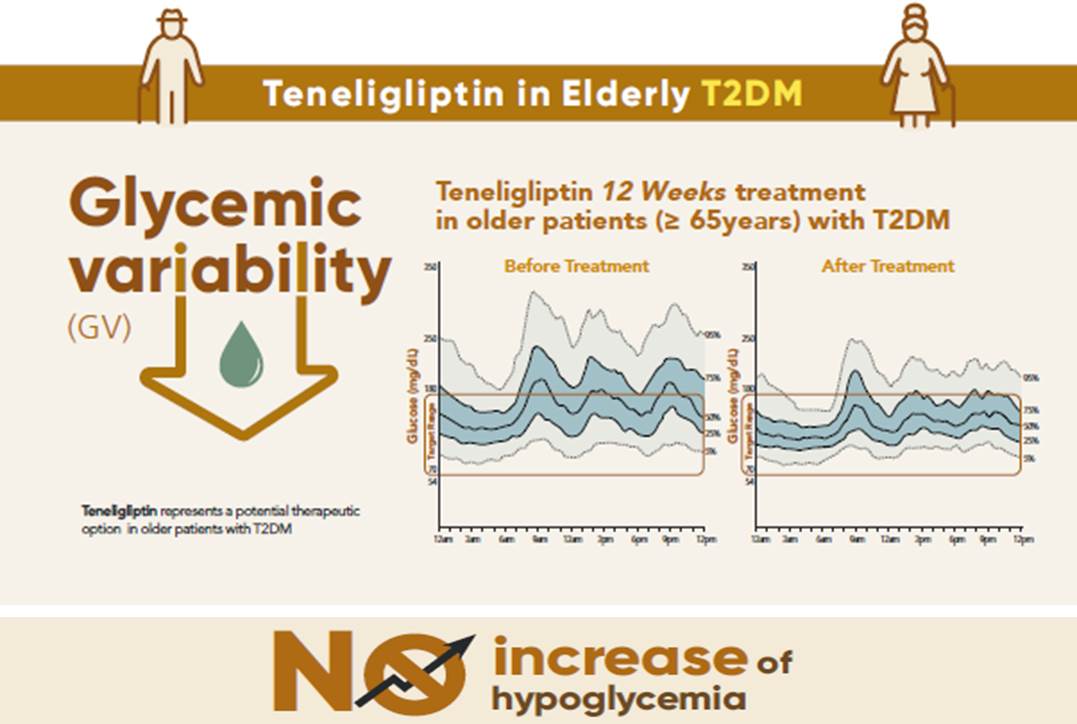
- Background
To evaluate the effects of teneligliptin on glycosylated hemoglobin (HbA1c) levels, continuous glucose monitoring (CGM)-derived time in range, and glycemic variability in elderly type 2 diabetes mellitus patients.
Methods
This randomized, double-blinded, placebo-controlled study was conducted in eight centers in Korea (clinical trial registration number: NCT03508323). Sixty-five participants aged ≥65 years, who were treatment-naïve or had been treated with stable doses of metformin, were randomized at a 1:1 ratio to receive 20 mg of teneligliptin (n=35) or placebo (n=30) for 12 weeks. The main endpoints were the changes in HbA1c levels from baseline to week 12, CGM metrics-derived time in range, and glycemic variability.
Results
After 12 weeks, a significant reduction (by 0.84%) in HbA1c levels was observed in the teneligliptin group compared to that in the placebo group (by 0.08%), with a between-group least squares mean difference of –0.76% (95% confidence interval [CI], –1.08 to –0.44). The coefficient of variation, standard deviation, and mean amplitude of glycemic excursion significantly decreased in participants treated with teneligliptin as compared to those in the placebo group. Teneligliptin treatment significantly decreased the time spent above 180 or 250 mg/dL, respectively, without increasing the time spent below 70 mg/dL. The mean percentage of time for which glucose levels remained in the 70 to 180 mg/dL time in range (TIR70–180) at week 12 was 82.0%±16.0% in the teneligliptin group, and placebo-adjusted change in TIR70–180 from baseline was 13.3% (95% CI, 6.0 to 20.6).
Conclusion
Teneligliptin effectively reduced HbA1c levels, time spent above the target range, and glycemic variability, without increasing hypoglycemia in our study population. -
Citations
Citations to this article as recorded by- Comparison of teneligliptin and other gliptin-based regimens in addressing insulin resistance and glycemic control in type 2 diabetic patients: a cross-sectional study
Harmanjit Singh, Ravi Rohilla, Shivani Jaswal, Mandeep Singla
Expert Review of Endocrinology & Metabolism.2024; 19(1): 81. CrossRef - Potential approaches using teneligliptin for the treatment of type 2 diabetes mellitus: current status and future prospects
Harmanjit Singh, Jasbir Singh, Ravneet Kaur Bhangu, Mandeep Singla, Jagjit Singh, Farideh Javid
Expert Review of Clinical Pharmacology.2023; 16(1): 49. CrossRef - Mechanism of molecular interaction of sitagliptin with human DPP4 enzyme - New Insights
Michelangelo Bauwelz Gonzatti, José Edvar Monteiro Júnior, Antônio José Rocha, Jonathas Sales de Oliveira, Antônio José de Jesus Evangelista, Fátima Morgana Pio Fonseca, Vânia Marilande Ceccatto, Ariclécio Cunha de Oliveira, José Ednésio da Cruz Freire
Advances in Medical Sciences.2023; 68(2): 402. CrossRef - A prospective multicentre open label study to assess effect of Teneligliptin on glycemic control through parameters of time in range (TIR) Metric using continuous glucose monitoring (TOP-TIR study)
Banshi Saboo, Suhas Erande, A.G. Unnikrishnan
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2022; 16(2): 102394. CrossRef - Association between Variability of Metabolic Risk Factors and Cardiometabolic Outcomes
Min Jeong Park, Kyung Mook Choi
Diabetes & Metabolism Journal.2022; 46(1): 49. CrossRef
- Comparison of teneligliptin and other gliptin-based regimens in addressing insulin resistance and glycemic control in type 2 diabetic patients: a cross-sectional study
- COVID-19
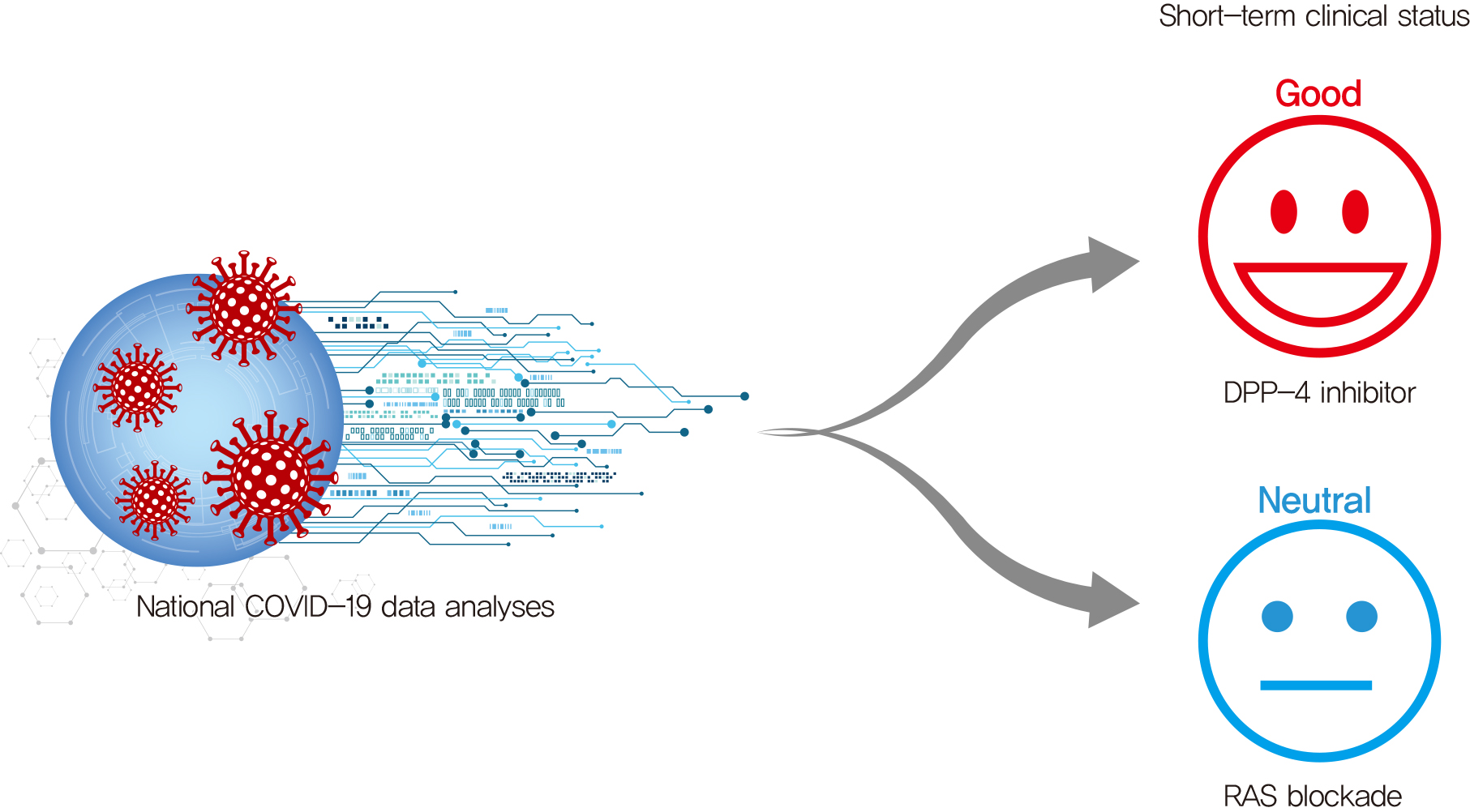
- Effects of a DPP-4 Inhibitor and RAS Blockade on Clinical Outcomes of Patients with Diabetes and COVID-19
- Sang Youl Rhee, Jeongwoo Lee, Hyewon Nam, Dae-Sung Kyoung, Dong Wook Shin, Dae Jung Kim
- Diabetes Metab J. 2021;45(2):251-259. Published online March 5, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0206
- 7,887 View
- 406 Download
- 33 Web of Science
- 34 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 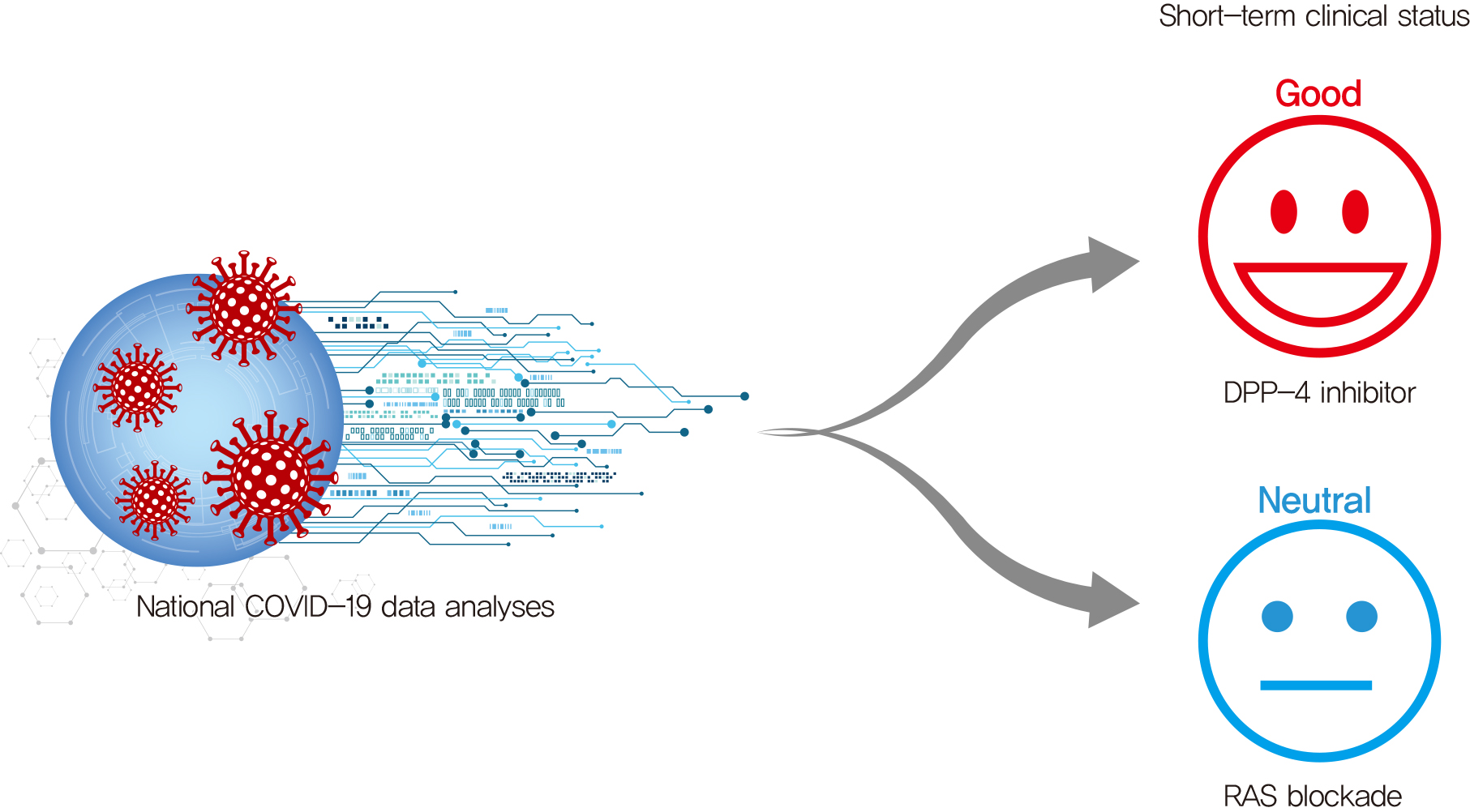
- Background
Dipeptidyl peptidase-4 inhibitor (DPP-4i) and renin-angiotensin system (RAS) blockade are reported to affect the clinical course of coronavirus disease 2019 (COVID-19) in patients with diabetes mellitus (DM).
Methods
As of May 2020, analysis was conducted on all subjects who could confirm their history of claims related to COVID-19 in the National Health Insurance Review and Assessment Service (HIRA) database in Korea. Using this dataset, we compared the short-term prognosis of COVID-19 infection according to the use of DPP-4i and RAS blockade. Additionally, we validated the results using the National Health Insurance Service (NHIS) of Korea dataset.
Results
Totally, data of 67,850 subjects were accessible in the HIRA dataset. Of these, 5,080 were confirmed COVID-19. Among these, 832 subjects with DM were selected for analysis in this study. Among the subjects, 263 (31.6%) and 327 (39.3%) were DPP4i and RAS blockade users, respectively. Thirty-four subjects (4.09%) received intensive care or died. The adjusted odds ratio for severe treatment among DPP-4i users was 0.362 (95% confidence interval [CI], 0.135 to 0.971), and that for RAS blockade users was 0.599 (95% CI, 0.251 to 1.431). These findings were consistent with the analysis based on the NHIS data using 704 final subjects. The adjusted odds ratio for severe treatment among DPP-4i users was 0.303 (95% CI, 0.135 to 0.682), and that for RAS blockade users was 0.811 (95% CI, 0.391 to 1.682).
Conclusion
This study suggests that DPP-4i is significantly associated with a better clinical outcome of patients with COVID-19. -
Citations
Citations to this article as recorded by- The Impact of GLP-1 RAs and DPP-4is on Hospitalisation and Mortality in the COVID-19 Era: A Two-Year Observational Study
Salvatore Greco, Vincenzo M. Monda, Giorgia Valpiani, Nicola Napoli, Carlo Crespini, Fabio Pieraccini, Anna Marra, Angelina Passaro
Biomedicines.2023; 11(8): 2292. CrossRef - Efficacy and Safety of Sitagliptin in the Treatment of COVID-19
Ehab Mudher Mikhael, Siew Chin Ong, Siti Maisharah Sheikh Ghadzi
Journal of Pharmacy Practice.2023; 36(4): 980. CrossRef - DPP-4 Inhibitors as a savior for COVID-19 patients with diabetes
Snehasish Nag, Samanwita Mandal, Oindrila Mukherjee, Suprabhat Mukherjee, Rakesh Kundu
Future Virology.2023; 18(5): 321. CrossRef - Risk phenotypes of diabetes and association with COVID-19 severity and death: an update of a living systematic review and meta-analysis
Sabrina Schlesinger, Alexander Lang, Nikoletta Christodoulou, Philipp Linnerz, Kalliopi Pafili, Oliver Kuss, Christian Herder, Manuela Neuenschwander, Janett Barbaresko, Michael Roden
Diabetologia.2023; 66(8): 1395. CrossRef - ACE2, ACE, DPPIV, PREP and CAT L enzymatic activities in COVID-19: imbalance of ACE2/ACE ratio and potential RAAS dysregulation in severe cases
Raquel Leão Neves, Jéssica Branquinho, Júlia Galanakis Arata, Clarissa Azevedo Bittencourt, Caio Perez Gomes, Michelle Riguetti, Gustavo Ferreira da Mata, Danilo Euclides Fernandes, Marcelo Yudi Icimoto, Gianna Mastroianni Kirsztajn, João Bosco Pesquero
Inflammation Research.2023; 72(8): 1719. CrossRef - Association Between Anti-diabetic Agents and Clinical Outcomes of COVID-19 in Patients with Diabetes: A Systematic Review and Meta-Analysis
Tiantian Han, Shaodi Ma, Chenyu Sun, Huimei Zhang, Guangbo Qu, Yue Chen, Ce Cheng, Eric L. Chen, Mubashir Ayaz Ahmed, Keun Young Kim, Raveena Manem, Mengshi Chen, Zhichun Guo, Hongru Yang, Yue Yan, Qin Zhou
Archives of Medical Research.2022; 53(2): 186. CrossRef - Use of DPP4i reduced odds of clinical deterioration and hyperinflammatory syndrome in COVID-19 patients with type 2 diabetes: Propensity score analysis of a territory-wide cohort in Hong Kong
Carlos K.H. Wong, David T.W. Lui, Angel Y.C. Lui, Ashley C.Y. Kwok, Marshall C.H. Low, Kristy T.K. Lau, Ivan C.H. Au, Xi Xiong, Matthew S.H. Chung, Eric H.Y. Lau, Benjamin J. Cowling
Diabetes & Metabolism.2022; 48(1): 101307. CrossRef - Dipeptidyl peptidase-4 (DPP-IV) inhibitor was associated with mortality reduction in COVID-19 — A systematic review and meta-analysis
Ahmad Fariz Malvi Zamzam Zein, Wilson Matthew Raffaello
Primary Care Diabetes.2022; 16(1): 162. CrossRef - Mortality and Severity in COVID-19 Patients on ACEIs and ARBs—A Systematic Review, Meta-Analysis, and Meta-Regression Analysis
Romil Singh, Sawai Singh Rathore, Hira Khan, Abhishek Bhurwal, Mack Sheraton, Prithwish Ghosh, Sohini Anand, Janaki Makadia, Fnu Ayesha, Kiran S. Mahapure, Ishita Mehra, Aysun Tekin, Rahul Kashyap, Vikas Bansal
Frontiers in Medicine.2022;[Epub] CrossRef - Short- and long-term prognosis of glycemic control in COVID-19 patients with type 2 diabetes
K Zhan, X Zhang, B Wang, Z Jiang, X Fang, S Yang, H Jia, L Li, G Cao, K Zhang, X Ma
QJM: An International Journal of Medicine.2022; 115(3): 131. CrossRef - Decreased circulating dipeptidyl peptidase-4 enzyme activity is prognostic for severe outcomes in COVID-19 inpatients
Ákos Nádasdi, György Sinkovits, Ilona Bobek, Botond Lakatos, Zsolt Förhécz, Zita Z Prohászka, Marienn Réti, Miklós Arató, Gellért Cseh, Tamás Masszi, Béla Merkely, Péter Ferdinandy, István Vályi-Nagy, Zoltán Prohászka, Gábor Firneisz
Biomarkers in Medicine.2022; 16(5): 317. CrossRef - Management von Diabetespatienten in der COVID-19-Pandemie
Charlotte Steenblock, Carlotta Hoffmann, Tilman D. Rachner, Florian Guggenbichler, Ermal Tahirukaj, Sacipi Bejtullah, Vsevolod A. Zinserling, Zsuzanna Varga, Stefan R. Bornstein, Nikolaos Perakakis
Diabetes aktuell.2022; 20(01): 43. CrossRef - Letter: Diabesity Associates with Poor COVID-19 Outcomes among Hospitalized Patients (J Obes Metab Syndr 2021;30:149-54)
Tae Jung Oh
Journal of Obesity & Metabolic Syndrome.2022; 31(1): 86. CrossRef - Glucose-Lowering Agents and COVID-19
Ah Reum Khang
The Journal of Korean Diabetes.2022; 23(1): 1. CrossRef - The Association Between Antidiabetic Agents and Clinical Outcomes of COVID-19 Patients With Diabetes: A Bayesian Network Meta-Analysis
Yidan Chen, Xingfei Lv, Sang Lin, Mohammad Arshad, Mengjun Dai
Frontiers in Endocrinology.2022;[Epub] CrossRef - Drug-Disease Severity and Target-Disease Severity Interaction Networks in COVID-19 Patients
Verena Schöning, Felix Hammann
Pharmaceutics.2022; 14(9): 1828. CrossRef - Role of Dipeptidyl Peptidase-4 (DPP4) on COVID-19 Physiopathology
Alba Sebastián-Martín, Belén G. Sánchez, José M. Mora-Rodríguez, Alicia Bort, Inés Díaz-Laviada
Biomedicines.2022; 10(8): 2026. CrossRef - Anti-Diabetic Drugs GLP-1 Agonists and DPP-4 Inhibitors may Represent
Potential Therapeutic Approaches for COVID-19
Aliah Alshanwani, Tarek Kashour, Amira Badr
Endocrine, Metabolic & Immune Disorders - Drug Targets.2022; 22(6): 571. CrossRef - Dipeptidyl peptidase 4 inhibitors in COVID-19: Beyond glycemic control
Niya Narayanan, Dukhabandhu Naik, Jayaprakash Sahoo, Sadishkumar Kamalanathan
World Journal of Virology.2022; 11(6): 399. CrossRef - Associations Between the Use of Renin–Angiotensin System Inhibitors and the Risks of Severe COVID-19 and Mortality in COVID-19 Patients With Hypertension: A Meta-Analysis of Observational Studies
Xiao-Ce Dai, Zhuo-Yu An, Zi-Yang Wang, Zi-Zhen Wang, Yi-Ren Wang
Frontiers in Cardiovascular Medicine.2021;[Epub] CrossRef - Risk phenotypes of diabetes and association with COVID-19 severity and death: a living systematic review and meta-analysis
Sabrina Schlesinger, Manuela Neuenschwander, Alexander Lang, Kalliopi Pafili, Oliver Kuss, Christian Herder, Michael Roden
Diabetologia.2021; 64(7): 1480. CrossRef - Protecting older patients with cardiovascular diseases from COVID-19 complications using current medications
Mariana Alves, Marília Andreia Fernandes, Gülistan Bahat, Athanase Benetos, Hugo Clemente, Tomasz Grodzicki, Manuel Martínez-Sellés, Francesco Mattace-Raso, Chakravarthi Rajkumar, Andrea Ungar, Nikos Werner, Timo E. Strandberg, Grodzicki, Strandberg
European Geriatric Medicine.2021; 12(4): 725. CrossRef - Cardiometabolic Therapy and Mortality in Very Old Patients With Diabetes Hospitalized due to COVID-19
Jose Manuel Ramos-Rincón, Luis M Pérez-Belmonte, Francisco Javier Carrasco-Sánchez, Sergio Jansen-Chaparro, Mercedes De-Sousa-Baena, José Bueno-Fonseca, Maria Pérez-Aguilar, Coral Arévalo-Cañas, Marta Bacete Cebrian, Manuel Méndez-Bailón, Isabel Fiteni Me
The Journals of Gerontology: Series A.2021; 76(8): e102. CrossRef - Managing diabetes in diabetic patients with COVID: where do we start from?
Angelo Avogaro, Benedetta Bonora, Gian Paolo Fadini
Acta Diabetologica.2021; 58(11): 1441. CrossRef - The SARS-CoV-2 receptor angiotensin-converting enzyme 2 (ACE2) in myalgic encephalomyelitis/chronic fatigue syndrome: A meta-analysis of public DNA methylation and gene expression data
João Malato, Franziska Sotzny, Sandra Bauer, Helma Freitag, André Fonseca, Anna D. Grabowska, Luís Graça, Clara Cordeiro, Luís Nacul, Eliana M. Lacerda, Jesus Castro-Marrero, Carmen Scheibenbogen, Francisco Westermeier, Nuno Sepúlveda
Heliyon.2021; 7(8): e07665. CrossRef - Effects of a DPP-4 Inhibitor and RAS Blockade on Clinical Outcomes of Patients with Diabetes and COVID-19 (Diabetes Metab J 2021;45:251-9)
Sang Youl Rhee
Diabetes & Metabolism Journal.2021; 45(4): 619. CrossRef - Effects of a DPP-4 Inhibitor and RAS Blockade on Clinical Outcomes of Patients with Diabetes and COVID-19 (Diabetes Metab J 2021;45:251-9)
Guntram Schernthaner
Diabetes & Metabolism Journal.2021; 45(4): 615. CrossRef - COVID-19 and metabolic disease: mechanisms and clinical management
Charlotte Steenblock, Peter E H Schwarz, Barbara Ludwig, Andreas Linkermann, Paul Zimmet, Konstantin Kulebyakin, Vsevolod A Tkachuk, Alexander G Markov, Hendrik Lehnert, Martin Hrabě de Angelis, Hannes Rietzsch, Roman N Rodionov, Kamlesh Khunti, David Hop
The Lancet Diabetes & Endocrinology.2021; 9(11): 786. CrossRef - Diabetes, Obesity, and COVID-19
Sang Youl Rhee
The Journal of Korean Diabetes.2021; 22(3): 174. CrossRef - Sunlight Exposure and Phototherapy: Perspectives for Healthy Aging in an Era of COVID-19
Toshiaki Nakano, Kuei-Chen Chiang, Chien-Chih Chen, Po-Jung Chen, Chia-Yun Lai, Li-Wen Hsu, Naoya Ohmori, Takeshi Goto, Chao-Long Chen, Shigeru Goto
International Journal of Environmental Research and Public Health.2021; 18(20): 10950. CrossRef - Analysis of influence of background therapy for comorbidities in the period before infection on the risk of the lethal COVID outcome. Data from the international ACTIV SARS-CoV-2 registry («Analysis of chronic non-infectious diseases dynamics after COVID-
E. I. Tarlovskaya, A. G. Arutyunov, A. O. Konradi, Yu. M. Lopatin, A. P. Rebrov, S. N. Tereshchenko, A. I. Chesnikova, H. G. Hayrapetyan, A. P. Babin, I. G. Bakulin, N. V. Bakulina, L. A. Balykova, A. S. Blagonravova, M. V. Boldina, A. R. Vaisberg, A. S.
Kardiologiia.2021; 61(9): 20. CrossRef - Association of clinical characteristics, antidiabetic and cardiovascular agents with diabetes mellitus and COVID-19: a 7-month follow-up cohort study
Marzieh Pazoki, Fatemeh Chichagi, Azar Hadadi, Samira Kafan, Mahnaz Montazeri, Sina Kazemian, Arya Aminorroaya, Mehdi Ebrahimi, Haleh Ashraf, Mojgan Mirabdolhagh Hazaveh, Mohammad Reza Khajavi, Reza Shariat Moharari, Seyed Hamidreza Sharifnia, Shahrokh Ka
Journal of Diabetes & Metabolic Disorders.2021; 20(2): 1545. CrossRef - COVID-19 and Diabetes: A Comprehensive Review of Angiotensin Converting Enzyme 2, Mutual Effects and Pharmacotherapy
Lingli Xie, Ziying Zhang, Qian Wang, Yangwen Chen, Dexue Lu, Weihua Wu
Frontiers in Endocrinology.2021;[Epub] CrossRef - The Roles of Dipeptidyl Peptidase 4 (DPP4) and DPP4 Inhibitors in Different Lung Diseases: New Evidence
Tianli Zhang, Xiang Tong, Shijie Zhang, Dongguang Wang, Lian Wang, Qian Wang, Hong Fan
Frontiers in Pharmacology.2021;[Epub] CrossRef
- The Impact of GLP-1 RAs and DPP-4is on Hospitalisation and Mortality in the COVID-19 Era: A Two-Year Observational Study
- Complication
- Soluble Dipeptidyl Peptidase-4 Levels Are Associated with Decreased Renal Function in Patients with Type 2 Diabetes Mellitus
- Eun-Hee Cho, Sang-Wook Kim
- Diabetes Metab J. 2019;43(1):97-104. Published online October 8, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0030
- 4,258 View
- 52 Download
- 13 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Dipeptidyl peptidase-4 (DPP-4) is strongly expressed in the kidney, and soluble levels of this protein are used as a marker in various chronic inflammatory diseases, including diabetes, coronary artery disease, and cancer. This study examined the association between the serum soluble DPP-4 levels and renal function or cardiovascular risk in patients with type 2 diabetes mellitus.
Methods In this retrospective analysis, soluble DPP-4 levels were measured in preserved sera from 140 patients with type 2 diabetes mellitus who had participated in our previous coronary artery calcium (CAC) score study.
Results The mean±standard deviation soluble DPP-4 levels in our study sample were 645±152 ng/mL. Univariate analyses revealed significant correlations of soluble DPP-4 levels with the total cholesterol (
r =0.214,P =0.019) and serum creatinine levels (r =−0.315,P <0.001) and the estimated glomerular filtration rate (eGFR; estimated using the modification of diet in renal disease equation) (r =0.303,P =0.001). The associations of soluble DPP-4 levels with serum creatinine and GFR remained significant after adjusting for age, body mass index, and duration of diabetes. However, no associations were observed between soluble DPP-4 levels and the body mass index, waist circumference, or CAC score.Conclusion These data suggest the potential use of serum soluble DPP-4 levels as a future biomarker of deteriorated renal function in patients with type 2 diabetes mellitus.
-
Citations
Citations to this article as recorded by- Sitagliptin Mitigates Diabetic Nephropathy in a Rat Model of Streptozotocin-Induced Type 2 Diabetes: Possible Role of PTP1B/JAK-STAT Pathway
Sarah M. AL-Qabbaa, Samaher I. Qaboli, Tahani K. Alshammari, Maha A. Alamin, Haya M. Alrajeh, Lama A. Almuthnabi, Rana R. Alotaibi, Asma S. Alonazi, Anfal F. Bin Dayel, Nawal M. Alrasheed, Nouf M. Alrasheed
International Journal of Molecular Sciences.2023; 24(7): 6532. CrossRef - Evaluation of the efficacy of dipeptidyl peptidase-4 enzyme and selenium element in people with kidney failure in Kirkuk governorate
Ibrahim Abdullah Ali Al-Jubouri, Nadia Ahmed Saleh Al-Jubouri
Materials Today: Proceedings.2022; 60: 795. CrossRef - Cardiovascular Effects of Incretin-Based Therapies: Integrating Mechanisms With Cardiovascular Outcome Trials
John R. Ussher, Amanda A. Greenwell, My-Anh Nguyen, Erin E. Mulvihill
Diabetes.2022; 71(2): 173. CrossRef - Computer-Aided Screening of Phytoconstituents from Ocimum tenuiflorum against Diabetes Mellitus Targeting DPP4 Inhibition: A Combination of Molecular Docking, Molecular Dynamics, and Pharmacokinetics Approaches
Harshit Sajal, Shashank M. Patil, Ranjith Raj, Abdullah M. Shbeer, Mohammed Ageel, Ramith Ramu
Molecules.2022; 27(16): 5133. CrossRef - Association Between DPP4 Inhibitor Use and the Incidence of Cirrhosis, ESRD, and Some Cancers in Patients With Diabetes
Yewon Na, Soo Wan Kim, Ie Byung Park, Soo Jung Choi, Seungyoon Nam, Jaehun Jung, Dae Ho Lee
The Journal of Clinical Endocrinology & Metabolism.2022; 107(11): 3022. CrossRef - An update on the interaction between COVID-19, vaccines, and diabetic kidney disease
Yang Yang, Shubiao Zou, Gaosi Xu
Frontiers in Immunology.2022;[Epub] CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef - Renoprotective Effects of DPP-4 Inhibitors
Daiji Kawanami, Yuichi Takashi, Hiroyuki Takahashi, Ryoko Motonaga, Makito Tanabe
Antioxidants.2021; 10(2): 246. CrossRef - Serum levels of soluble dipeptidyl peptidase-4 in type 2 diabetes are associated with severity of liver fibrosis evaluated by transient elastography (FibroScan) and the FAST (FibroScan-AST) score, a novel index of non-alcoholic steatohepatitis with signif
Masaaki Sagara, Toshie Iijima, Masato Kase, Kanako Kato, Shintaro Sakurai, Takuya Tomaru, Teruo Jojima, Isao Usui, Yoshimasa Aso
Journal of Diabetes and its Complications.2021; 35(5): 107885. CrossRef - Distinctive CD26 Expression on CD4 T-Cell Subsets
Oscar J. Cordero, Carlos Rafael-Vidal, Rubén Varela-Calviño, Cristina Calviño-Sampedro, Beatriz Malvar-Fernández, Samuel García, Juan E. Viñuela, José M. Pego-Reigosa
Biomolecules.2021; 11(10): 1446. CrossRef - The Long-Term Study of Urinary Biomarkers of Renal Injury in Spontaneously Hypertensive Rats
Sebastián Montoro-Molina, Andrés Quesada, Francisco O’Valle, Natividad Martín Morales, María del Carmen de Gracia, Isabel Rodríguez-Gómez, Antonio Osuna, Rosemary Wangensteen, Félix Vargas
Kidney and Blood Pressure Research.2021; 46(4): 502. CrossRef - Serum Dipeptidyl peptidase-4 level is related to adiposity in type 1 diabetic adolescents
Amany Ibrahim, Shaimaa Salah, Mona Attia, Hanan Madani, Samah Ahmad, Noha Arafa, Hend Soliman
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2020; 14(4): 609. CrossRef - Phase I study of YS110, a recombinant humanized monoclonal antibody to CD26, in Japanese patients with advanced malignant pleural mesothelioma
Masayuki Takeda, Yuichiro Ohe, Hidehito Horinouchi, Toyoaki Hida, Junichi Shimizu, Takashi Seto, Kaname Nosaki, Takumi Kishimoto, Itaru Miyashita, Masayuki Yamada, Yutaro Kaneko, Chikao Morimoto, Kazuhiko Nakagawa
Lung Cancer.2019; 137: 64. CrossRef
- Sitagliptin Mitigates Diabetic Nephropathy in a Rat Model of Streptozotocin-Induced Type 2 Diabetes: Possible Role of PTP1B/JAK-STAT Pathway
- Islet Studies and Transplantation
- An Update on the Effect of Incretin-Based Therapies on β-Cell Function and Mass
- Suk Chon, Jean-François Gautier
- Diabetes Metab J. 2016;40(2):99-114. Published online April 25, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.2.99
- 4,978 View
- 111 Download
- 43 Web of Science
- 41 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Type 2 diabetes mellitus (T2DM) is a multifactorial disease with a complex and progressive pathogenesis. The two primary mechanisms of T2DM pathogenesis are pancreatic β-cell dysfunction and insulin resistance. Pancreatic β-cell dysfunction is recognized to be a prerequisite for the development of T2DM. Therapeutic modalities that improve β-cell function are considered critical to T2DM management; however, blood glucose control remains a challenge for many patients due to suboptimal treatment efficacy and the progressive nature of T2DM. Incretin-based therapies are now the most frequently prescribed antidiabetic drugs in Korea. Incretin-based therapies are a favorable class of drugs due to their ability to reduce blood glucose by targeting the incretin hormone system and, most notably, their potential to improve pancreatic β-cell function. This review outlines the current understanding of the incretin hormone system in T2DM and summarizes recent updates on the effect of incretin-based therapies on β-cell function and β-cell mass in animals and humans.
-
Citations
Citations to this article as recorded by- Harnessing gut cells for functional insulin production: Strategies and challenges
Kelvin Baafi, John C. March
Biotechnology Notes.2023; 4: 7. CrossRef - Incretin and Pancreatic β-Cell Function in Patients with Type 2 Diabetes
Chang Ho Ahn, Tae Jung Oh, Se Hee Min, Young Min Cho
Endocrinology and Metabolism.2023; 38(1): 1. CrossRef - Weight loss maintenance with exercise and liraglutide improves glucose tolerance, glucagon response, and beta cell function
Simon B. K. Jensen, Christian R. Juhl, Charlotte Janus, Julie R. Lundgren, Christoffer Martinussen, Christoffer Wiingaard, Cecilie Knudsen, Ruth Frikke‐Schmidt, Bente M. Stallknecht, Jens J. Holst, Sten Madsbad, Signe S. Torekov
Obesity.2023; 31(4): 977. CrossRef - How do parasitic worms prevent diabetes? An exploration of their influence on macrophage and β-cell crosstalk
Inah Camaya, Bronwyn O’Brien, Sheila Donnelly
Frontiers in Endocrinology.2023;[Epub] CrossRef - An Imbalance of Pathophysiologic Factors in Late Postprandial Hypoglycemia Post Bariatric Surgery: A Narrative Review
Marah Alsayed Hasan, Stanley Schwartz, Victoria McKenna, Richard Ing
Obesity Surgery.2023; 33(9): 2927. CrossRef - Therapeutic Dilemma in Personalized Medicine
Ehab S. EL Desoky
Current Reviews in Clinical and Experimental Pharmacology.2022; 17(2): 94. CrossRef - Lessons from neonatal β-cell epigenomic for diabetes prevention and treatment
Amar Abderrahmani, Cécile Jacovetti, Romano Regazzi
Trends in Endocrinology & Metabolism.2022; 33(6): 378. CrossRef - Beneficial metabolic effects of recurrent periods of beta‐cell rest and stimulation using stable neuropeptide Y1 and glucagon‐like peptide‐1 receptor agonists
Neil Tanday, Ryan A. Lafferty, Peter R. Flatt, Nigel Irwin
Diabetes, Obesity and Metabolism.2022; 24(12): 2353. CrossRef - A Randomized Controlled Trial of R-Form Verapamil Added to Ongoing Metformin Therapy in Patients with Type 2 Diabetes
Chih-Yuan Wang, Kuo-Chin Huang, Chia-Wen Lu, Chih-Hsun Chu, Chien-Ning Huang, Harn-Shen Chen, I-Te Lee, Jung-Fu Chen, Ching-Chu Chen, Chung-Sen Chen, Chang-Hsun Hsieh, Kai-Jen Tien, Hung-Yu Chien, Yu-Yao Huang, Jui-Pao Hsu, Guang-Tzuu Shane, Ai-Ching Chan
The Journal of Clinical Endocrinology & Metabolism.2022; 107(10): e4063. CrossRef - Exenatide, Metformin, or Both for Prediabetes in PCOS: A Randomized, Open-label, Parallel-group Controlled Study
Tao Tao, Yi Zhang, Yu-Chen Zhu, Jia-Rong Fu, Yu-Ying Wang, Jie Cai, Jing-Yu Ma, Yu Xu, Yi-Ning Gao, Yun Sun, WuQiang Fan, Wei Liu
The Journal of Clinical Endocrinology & Metabolism.2021; 106(3): e1420. CrossRef - The utility of assessing C-peptide in patients with insulin-treated type 2 diabetes: a cross-sectional study
Tuccinardi Dario, Giorgino Riccardo, Pieralice Silvia, Watanabe Mikiko, Maggi Daria, Palermo Andrea, Defeudis Giuseppe, Fioriti Elvira, Pozzilli Paolo, Manfrini Silvia
Acta Diabetologica.2021; 58(4): 411. CrossRef - Type 2 diabetes: evidence-based medicine approach to glucose-lowering therapy
E. V. Biryukova, I. A. Morozova, S. V. Rodionova
Meditsinskiy sovet = Medical Council.2021; (21): 160. CrossRef - Emerging Role of Caveolin-1 in GLP-1 Action
Alessandra Puddu, Davide Maggi
Frontiers in Endocrinology.2021;[Epub] CrossRef - Improvements in HOMA indices and pancreatic endocrinal tissues in type 2-diabetic rats by DPP-4 inhibition and antioxidant potential of an ethanol fruit extract of Withania coagulans
Heera Ram, Pramod Kumar, Ashok Purohit, Priya Kashyap, Suresh Kumar, Shivani Kumar, Garima Singh, Abdulaziz A. Alqarawi, Abeer Hashem, Elsayed Fathi Abd-Allah, Al-Bandari Fahad Al-Arjani, Bhim Pratap Singh
Nutrition & Metabolism.2021;[Epub] CrossRef -
Chop
/
Ddit3
depletion in β cells alleviates ER stress and corrects hepatic steatosis in mice
Jing Yong, Vishal S. Parekh, Shannon M. Reilly, Jonamani Nayak, Zhouji Chen, Cynthia Lebeaupin, Insook Jang, Jiangwei Zhang, Thazha P. Prakash, Hong Sun, Sue Murray, Shuling Guo, Julio E. Ayala, Leslie S. Satin, Alan R. Saltiel, Randal J. Kaufman
Science Translational Medicine.2021;[Epub] CrossRef - Assessment of Insulin Secretion and Insulin Resistance in Human
So Young Park, Jean-François Gautier, Suk Chon
Diabetes & Metabolism Journal.2021; 45(5): 641. CrossRef - Targeted pharmacological therapy restores β-cell function for diabetes remission
Stephan Sachs, Aimée Bastidas-Ponce, Sophie Tritschler, Mostafa Bakhti, Anika Böttcher, Miguel A. Sánchez-Garrido, Marta Tarquis-Medina, Maximilian Kleinert, Katrin Fischer, Sigrid Jall, Alexandra Harger, Erik Bader, Sara Roscioni, Siegfried Ussar, Annett
Nature Metabolism.2020; 2(2): 192. CrossRef - The Relationship Between Timing of Initiation on a Glucagon-like Peptide-1 Receptor Agonist and Glycosylated Hemoglobin Values Among Patients With Type 2 Diabetes
Kristina S. Boye, Reema Mody, Maureen J. Lage, Raleigh E. Malik
Clinical Therapeutics.2020; 42(9): 1812. CrossRef - Short-term renal and metabolic effects of low dose vildagliptin treatment added-on insulin therapy in non-proteinuric patients with type 2 diabetes: open-label randomized prospective study
Valentina K. Bayrasheva, Ivan Y. Pchelin, Vladimir A. Dobronravov, Alina Yu. Babenko, Svetlana G. Chefu, Ivan S. Shatalov, Volha N. Vasilkova, Natalia V. Hudiakova, Alexandra N. Ivanova, Pavel A. Andoskin, Elena N. Grineva
Archives of Endocrinology and Metabolism.2020;[Epub] CrossRef - A Phenotypic Screen Identifies Calcium Overload as a Key Mechanism of β-Cell Glucolipotoxicity
Jennifer Vogel, Jianning Yin, Liansheng Su, Sharon X. Wang, Richard Zessis, Sena Fowler, Chun-Hao Chiu, Aaron C. Wilson, Amy Chen, Frederic Zecri, Gordon Turner, Thomas M. Smith, Brian DeChristopher, Heming Xing, Deborah M. Rothman, Xinming Cai, Alina Ber
Diabetes.2020; 69(5): 1032. CrossRef - Neuropeptide 26RFa (QRFP) is a key regulator of glucose homeostasis and its activity is markedly altered in obese/hyperglycemic mice
Gaëtan Prévost, Arnaud Arabo, Marie-Anne Le Solliec, Justine Bons, Marie Picot, Julie Maucotel, Hind Berrahmoune, Mouna El Mehdi, Saloua Cherifi, Alexandre Benani, Emmanuelle Nédélec, Moïse Coëffier, Jérôme Leprince, Anneli Nordqvist, Valéry Brunel, Pierr
American Journal of Physiology-Endocrinology and Metabolism.2019; 317(1): E147. CrossRef - Gastrin analogue administration adds no significant glycaemic benefit to a glucagon‐like peptide‐1 receptor agonist acutely or after washout of both analogues
Krister Bokvist, Ying Ding, William H. Landschulz, Vikram Sinha, Aleksandra Pastrak, Ruth M. Belin
Diabetes, Obesity and Metabolism.2019; 21(7): 1606. CrossRef - Effects of boschnaloside from Boschniakia rossica on dysglycemia and islet dysfunction in severely diabetic mice through modulating the action of glucagon-like peptide-1
Lie-Chwen Lin, Lin-Chien Lee, Cheng Huang, Chiung-Tong Chen, Jen-Shin Song, Young-Ji Shiao, Hui-Kang Liu
Phytomedicine.2019; 62: 152946. CrossRef - The future of new drugs for diabetes management
Clifford J. Bailey, Caroline Day
Diabetes Research and Clinical Practice.2019; 155: 107785. CrossRef - Compact fluidic system for functional assessment of pancreatic islets
Takeshi Hori, Kei Yamane, Takayuki Anazawa, Osamu Kurosawa, Hiroo Iwata
Biomedical Microdevices.2019;[Epub] CrossRef - Pharmacokinetics of Exenatide in nonhuman primates following its administration in the form of sustained-release PT320 and Bydureon
Yazhou Li, Kelli L. Vaughan, David Tweedie, Jin Jung, Hee Kyung Kim, Ho-Il Choi, Dong Seok Kim, Julie A. Mattison, Nigel H. Greig
Scientific Reports.2019;[Epub] CrossRef - Pharmacokinetics and efficacy of PT302, a sustained-release Exenatide formulation, in a murine model of mild traumatic brain injury
Miaad Bader, Yazhou Li, Daniela Lecca, Vardit Rubovitch, David Tweedie, Elliot Glotfelty, Lital Rachmany, Hee Kyung Kim, Ho-Il Choi, Barry J. Hoffer, Chaim G. Pick, Nigel H. Greig, Dong Seok Kim
Neurobiology of Disease.2019; 124: 439. CrossRef - Novel dual incretin agonist peptide with antidiabetic and neuroprotective potential
N.M. Pathak, V. Pathak, V.A. Gault, S. McClean, N. Irwin, P.R. Flatt
Biochemical Pharmacology.2018; 155: 264. CrossRef - Human EndoC-βH1 β-cells form pseudoislets with improved glucose sensitivity and enhanced GLP-1 signaling in the presence of islet-derived endothelial cells
Michael G. Spelios, Lauren A. Afinowicz, Regine C. Tipon, Eitan M. Akirav
American Journal of Physiology-Endocrinology and Metabolism.2018; 314(5): E512. CrossRef - Vildagliptin: ten years in the service for type 2 diabetes mellitus patients. The journey of discovery, innovation and success in clinical practice
Tatiana Yu. Demidova
Problems of Endocrinology.2018; 64(5): 336. CrossRef - Thromboxane-Dependent Platelet Activation in Obese Subjects with Prediabetes or Early Type 2 Diabetes: Effects of Liraglutide- or Lifestyle Changes-Induced Weight Loss
Paola Simeone, Rossella Liani, Romina Tripaldi, Augusto Di Castelnuovo, Maria Guagnano, Armando Tartaro, Riccardo Bonadonna, Virginia Federico, Francesco Cipollone, Agostino Consoli, Francesca Santilli
Nutrients.2018; 10(12): 1872. CrossRef - Nutrient regulation of β-cell function: what do islet cell/animal studies tell us?
R Carlessi, K N Keane, C Mamotte, P Newsholme
European Journal of Clinical Nutrition.2017; 71(7): 890. CrossRef - Effectiveness and safety of exenatide in Korean patients with type 2 diabetes inadequately controlled with oral hypoglycemic agents: an observational study in a real clinical practice
You-Cheol Hwang, Ari Kim, Euna Jo, Yeoree Yang, Jae-Hyoung Cho, Byung-Wan Lee
BMC Endocrine Disorders.2017;[Epub] CrossRef - Efficacy and safety of adding evogliptin versus sitagliptin for metformin‐treated patients with type 2 diabetes: A 24‐week randomized, controlled trial with open label extension
Sang‐Mo Hong, Cheol‐Young Park, Dong‐Min Hwang, Kyung Ah Han, Chang Beom Lee, Choon Hee Chung, Kun‐Ho Yoon, Ji‐Oh Mok, Kyong Soo Park, Sung‐Woo Park
Diabetes, Obesity and Metabolism.2017; 19(5): 654. CrossRef - The effects of vildagliptin compared with metformin on vascular endothelial function and metabolic parameters: a randomized, controlled trial (Sapporo Athero-Incretin Study 3)
Naoyuki Kitao, Hideaki Miyoshi, Tomoo Furumoto, Kota Ono, Hiroshi Nomoto, Aika Miya, Chiho Yamamoto, Atsushi Inoue, Kenichi Tsuchida, Naoki Manda, Yoshio Kurihara, Shin Aoki, Akinobu Nakamura, Tatsuya Atsumi
Cardiovascular Diabetology.2017;[Epub] CrossRef - Recent Advances in Effect‐directed Enzyme Assays based on Thin‐layer Chromatography
Sarah Bräm, Evelyn Wolfram
Phytochemical Analysis.2017; 28(2): 74. CrossRef - Efficacy and safety of gemigliptin, a dipeptidyl peptidase‐4 inhibitor, in patients with type 2 diabetes mellitus inadequately controlled with combination treatment of metformin and sulphonylurea: a 24‐week, multicentre, randomized, double‐blind, placebo‐
Chang Ho Ahn, Kyung Ah Han, Jae Myung Yu, Joo Young Nam, Kyu Jeung Ahn, Tae Keun Oh, Hyoung Woo Lee, Dae Ho Lee, Jaetaek Kim, Choon Hee Chung, Tae Sun Park, Byung Joon Kim, Seok Won Park, Hyeong Kyu Park, Kwang Jae Lee, Sang‐Wook Kim, Jeong Hyun Park, Kwa
Diabetes, Obesity and Metabolism.2017; 19(5): 635. CrossRef - Antihyperglycemic agent therapy for adult patients with type 2 diabetes mellitus 2017: a position statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
The Korean Journal of Internal Medicine.2017; 32(6): 947. CrossRef - Antihyperglycemic Agent Therapy for Adult Patients with Type 2 Diabetes Mellitus 2017: A Position Statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
Diabetes & Metabolism Journal.2017; 41(5): 337. CrossRef - DPP-4 inhibitors in diabetic complications: role of DPP-4 beyond glucose control
Eun Ju Bae
Archives of Pharmacal Research.2016; 39(8): 1114. CrossRef - Liraglutide Enhances the Efficacy of Human Mesenchymal Stem Cells in Preserving Islet ß-cell Function in Severe Non-obese Diabetic Mice
Li-rong Li, Jing Lu, Xiao-lei Jia, Hui Hui, Jie Zhang, Ying Liu, Wei-juan Cui, Qian-yue Xu, Da-long Zhu
Molecular Medicine.2016; 22(1): 800. CrossRef
- Harnessing gut cells for functional insulin production: Strategies and challenges
- Others
- Comparison of Vildagliptin and Pioglitazone in Korean Patients with Type 2 Diabetes Inadequately Controlled with Metformin
- Jong Ho Kim, Sang Soo Kim, Hong Sun Baek, In Kyu Lee, Dong Jin Chung, Ho Sang Sohn, Hak Yeon Bae, Mi Kyung Kim, Jeong Hyun Park, Young Sik Choi, Young Il Kim, Jong Ryeal Hahm, Chang Won Lee, Sung Rae Jo, Mi Kyung Park, Kwang Jae Lee, In Joo Kim
- Diabetes Metab J. 2016;40(3):230-239. Published online April 5, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.3.230
- 5,217 View
- 48 Download
- 13 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background We compared the efficacies of vildagliptin (50 mg twice daily) relative to pioglitazone (15 mg once daily) as an add-on treatment to metformin for reducing glycosylated hemoglobin (HbA1c) levels in Korean patients with type 2 diabetes.
Methods The present study was a multicenter, randomized, active-controlled investigation comparing the effects of vildagliptin and pioglitazone in Korean patients receiving a stable dose of metformin but exhibiting inadequate glycemic control. Each patient underwent a 16-week treatment period with either vildagliptin or pioglitazone as an add-on treatment to metformin.
Results The mean changes in HbA1c levels from baseline were –0.94% in the vildagliptin group and –0.6% in the pioglitazone group and the difference between the treatments was below the non-inferiority margin of 0.3%. The mean changes in postprandial plasma glucose (PPG) levels were –60.2 mg/dL in the vildagliptin group and –38.2 mg/dL in the pioglitazone group and these values significantly differed (
P =0.040). There were significant decreases in the levels of total, low density lipoprotein, high density lipoprotein (HDL), and non-HDL cholesterol in the vildagliptin group but increases in the pioglitazone group. The mean change in body weight was –0.07 kg in the vildagliptin group and 0.69 kg in the pioglitazone group, which were also significantly different (P =0.002).Conclusion As an add-on to metformin, the efficacy of vildagliptin for the improvement of glycemic control is not inferior to that of pioglitazone in Korean patients with type 2 diabetes. In addition, add-on treatment with vildagliptin had beneficial effects on PPG levels, lipid profiles, and body weight compared to pioglitazone.
-
Citations
Citations to this article as recorded by- Factors contributing to the adverse drug reactions associated with the dipeptidyl peptidase-4 (DPP-4) inhibitors: A scoping review
Swetha R. Reghunath, Muhammed Rashid, Viji Pulikkel Chandran, Girish Thunga, K.N. Shivashankar, Leelavathi D. Acharya
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(7): 102790. CrossRef - Efficacy and safety of evogliptin in patients with type 2 diabetes and non‐alcoholic fatty liver disease: A multicentre, double‐blind, randomized, comparative trial
Eugene Han, Ji Hye Huh, Eun Y. Lee, Ji C. Bae, Sung W. Chun, Sung H. Yu, Soo H. Kwak, Kyong S. Park, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2022; 24(4): 752. CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - The rs12617336 and rs17574 Dipeptidyl Peptidase-4 Polymorphisms Are Associated With Hypoalphalipoproteinemia and Dipeptidyl Peptidase-4 Serum Levels: A Case-Control Study of the Genetics of Atherosclerotic Disease (GEA) Cohort
Gilberto Vargas-Alarcón, María del Carmen González-Salazar, Christian Vázquez-Vázquez, Adrián Hernández-Díaz Couder, Fausto Sánchez-Muñoz, Juan Reyes-Barrera, Sergio A. Criales-Vera, Marco Sánchez-Guerra, Citlalli Osorio-Yáñez, Rosalinda Posadas-Sánchez
Frontiers in Genetics.2021;[Epub] CrossRef - Reduction in HbA1c with SGLT2 inhibitors vs. DPP-4 inhibitors as add-ons to metformin monotherapy according to baseline HbA1c: A systematic review of randomized controlled trials
A.J. Scheen
Diabetes & Metabolism.2020; 46(3): 186. CrossRef - Combination Therapy of Oral Hypoglycemic Agents in Patients with Type 2 Diabetes Mellitus
Min Kyong Moon
The Journal of Korean Diabetes.2018; 19(1): 23. CrossRef - Comparative Cardiovascular Risks of Dipeptidyl Peptidase-4 Inhibitors: Analyses of Real-world Data in Korea
Kyoung Hwa Ha, Bongseong Kim, Hae Sol Shin, Jinhee Lee, Hansol Choi, Hyeon Chang Kim, Dae Jung Kim
Korean Circulation Journal.2018; 48(5): 395. CrossRef - Safety and efficacy of low dose pioglitazone compared with standard dose pioglitazone in type 2 diabetes with chronic kidney disease: A randomized controlled trial
Bancha Satirapoj, Khanin Watanakijthavonkul, Ouppatham Supasyndh, Stephen L Atkin
PLOS ONE.2018; 13(10): e0206722. CrossRef - Combination therapy of oral hypoglycemic agents in patients with type 2 diabetes mellitus
Min Kyong Moon, Kyu Yeon Hur, Seung-Hyun Ko, Seok-O Park, Byung-Wan Lee, Jin Hwa Kim, Sang Youl Rhee, Hyun Jin Kim, Kyung Mook Choi, Nan-Hee Kim
The Korean Journal of Internal Medicine.2017; 32(6): 974. CrossRef - Combination Therapy of Oral Hypoglycemic Agents in Patients with Type 2 Diabetes Mellitus
Min Kyong Moon, Kyu-Yeon Hur, Seung-Hyun Ko, Seok-O Park, Byung-Wan Lee, Jin Hwa Kim, Sang Youl Rhee, Hyun Jin Kim, Kyung Mook Choi, Nan-Hee Kim
Diabetes & Metabolism Journal.2017; 41(5): 357. CrossRef - Efficacy and safety of adding evogliptin versus sitagliptin for metformin‐treated patients with type 2 diabetes: A 24‐week randomized, controlled trial with open label extension
Sang‐Mo Hong, Cheol‐Young Park, Dong‐Min Hwang, Kyung Ah Han, Chang Beom Lee, Choon Hee Chung, Kun‐Ho Yoon, Ji‐Oh Mok, Kyong Soo Park, Sung‐Woo Park
Diabetes, Obesity and Metabolism.2017; 19(5): 654. CrossRef - Antihyperglycemic agent therapy for adult patients with type 2 diabetes mellitus 2017: a position statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
The Korean Journal of Internal Medicine.2017; 32(6): 947. CrossRef - Antihyperglycemic Agent Therapy for Adult Patients with Type 2 Diabetes Mellitus 2017: A Position Statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
Diabetes & Metabolism Journal.2017; 41(5): 337. CrossRef
- Factors contributing to the adverse drug reactions associated with the dipeptidyl peptidase-4 (DPP-4) inhibitors: A scoping review
- Clinical Care/Education
- Dipeptidyl Peptidase 4 Inhibitors and the Risk of Cardiovascular Disease in Patients with Type 2 Diabetes: A Tale of Three Studies
- Jang Won Son, Sungrae Kim
- Diabetes Metab J. 2015;39(5):373-383. Published online October 22, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.5.373
- 4,621 View
- 55 Download
- 31 Web of Science
- 28 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Dipeptidyl peptidase 4 (DPP4) inhibitors have been touted as promising antihyperglycemic agents due to their beneficial effects on glycemia without inducing hypoglycemia or body weight gain and their good tolerability. Beyond their glucose-lowering effects, numerous clinical trials and experimental studies have suggested that DPP4 inhibitors may exert cardioprotective effects through their pleiotropic actions via glucagon-like peptide 1-dependent mechanisms or involving other substrates. Since 2008, regulatory agencies have required an assessment of cardiovascular disease (CVD) safety for the approval of all new anti-hyperglycemic agents, including incretin-based therapies. Three large prospective DPP4 inhibitor trials with cardiovascular (CV) outcomes have recently been published. According to the Saxagliptin Assessment of Vascular Outcomes Recorded in Patients with Diabetes Mellitus (SAVOR-TIMI 53) and EXamination of cArdiovascular outcoMes with alogliptIN versus standard of carE in patients with type 2 diabetes mellitus and acute coronary syndrome (EXAMINE) trials, DPP4 inhibitors, including saxagliptin and alogliptin, did not appear to increase the risk of CV events in patients with type 2 diabetes and established CVD or high risk factors. Unexpectedly, saxagliptin significantly increased the risk of hospitalization for heart failure by 27%, a finding that has not been explained and that requires further exploration. More recently, the Trial Evaluating Cardiovascular Outcomes with Sitagliptin (TECOS) trial demonstrated the CV safety of sitagliptin, including assessments of the primary composite CV endpoint and hospitalization for heart failure in patients with type 2 diabetes and established CVD. The CV outcomes of an ongoing linagliptin trial are expected to provide new evidence about the CV effects of a DPP4-inhibitor in patients with type 2 diabetes.
-
Citations
Citations to this article as recorded by- Sodium-Glucose Cotransporter-2 Inhibitor Use is Associated with a Reduced Risk of Heart Failure Hospitalization in Patients with Heart Failure with Preserved Ejection Fraction and Type 2 Diabetes Mellitus: A Real-World Study on a Diverse Urban Population
Weijia Li, Adarsh Katamreddy, Rachna Kataria, Merle L. Myerson, Cynthia C. Taub
Drugs - Real World Outcomes.2022; 9(1): 53. CrossRef - Comparative Cardiovascular Outcomes of SGLT2 Inhibitors in Type 2 Diabetes Mellitus: A Network Meta-Analysis of Randomized Controlled Trials
Yu Jiang, Pingping Yang, Linghua Fu, Lizhe Sun, Wen Shen, Qinghua Wu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Association of Baseline HbA1c With Cardiovascular and Renal Outcomes: Analyses From DECLARE-TIMI 58
Avivit Cahn, Stephen D. Wiviott, Ofri Mosenzon, Erica L. Goodrich, Sabina A. Murphy, Ilan Yanuv, Aliza Rozenberg, Deepak L. Bhatt, Lawrence A. Leiter, Darren K. McGuire, John P.H. Wilding, Ingrid A.M. Gause-Nilsson, Anna Maria Langkilde, Marc S. Sabatine,
Diabetes Care.2022; 45(4): 938. CrossRef Effect of Switching from Linagliptin to Teneligliptin Dipeptidyl Peptidase-4 Inhibitors in Older Patients with Type 2 Diabetes Mellitus
Eugene Han, Minyoung Lee, Yong-ho Lee, Hye Soon Kim, Byung-wan Lee, Bong-Soo Cha, Eun Seok Kang
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 4113. CrossRef- Effects of Teneligliptin on the Progressive Left Ventricular Diastolic Dysfunction in Patients with Type 2 Diabetes Mellitus in Open-Label, Marker-Stratified Randomized, Parallel-Group Comparison, Standard Treatment-Controlled Multicenter Trial (TOPLEVEL
Miki Imazu, Atsushi Nakano, Shin Ito, Toshimitsu Hamasaki, Masafumi Kitakaze
Cardiovascular Drugs and Therapy.2019; 33(3): 363. CrossRef - Dipeptidyl peptidase-4 inhibitor use and risk of diabetic retinopathy: A population-based study
N.H. Kim, J. Choi, N.H. Kim, K.M. Choi, S.H. Baik, J. Lee, S.G. Kim
Diabetes & Metabolism.2018; 44(4): 361. CrossRef - Glucagon secretion determined by the RIA method is lower in patients with low left ventricular ejection fraction: The new glass study
Makoto Murata, Hitoshi Adachi, Taishuke Nakade, Shigeru Oshima
Diabetes Research and Clinical Practice.2018; 144: 260. CrossRef - Coadministration of DPP-4 inhibitor and insulin therapy does not further reduce the risk of cardiovascular events compared with DPP-4 inhibitor therapy in diabetic foot patients: a nationwide population-based study
Yi-Hsuan Lin, Yu-Yao Huang, Yi-Ling Wu, Cheng-Wei Lin, Pei-Chun Chen, Chee Jen Chang, Sheng-Hwu Hsieh, Jui-Hung Sun, Szu-Tah Chen, Chia-Hung Lin
Diabetology & Metabolic Syndrome.2018;[Epub] CrossRef - Postmeal increment in intact glucagon-like peptide 1 level, but not intact glucose-dependent insulinotropic polypeptide levels, is inversely associated with metabolic syndrome in patients with type 2 diabetes
Soyeon Yoo, Eun-Jin Yang, Sang Ah Lee, Gwanpyo Koh
Endocrine Research.2018; 43(1): 47. CrossRef - Dipeptidyl Peptidase‐4 Inhibitors and Heart Failure Exacerbation in the Veteran Population: An Observational Study
Michael R. Cobretti, Benjamin Bowman, Ted Grabarczyk, Emily Potter
Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy.2018; 38(3): 334. CrossRef - Effects of a Dipeptidyl Peptidase 4 Inhibitor Sitagliptin on Glycemic Control and Lipoprotein Metabolism in Patients with Type 2 Diabetes Mellitus (GLORIA Trial)
Daisaku Masuda, Takuya Kobayashi, Masami Sairyou, Hiroyuki Hanada, Tohru Ohama, Masahiro Koseki, Makoto Nishida, Norikazu Maeda, Shinji Kihara, Tatsuya Minami, Koji Yanagi, Yasushi Sakata, Shizuya Yamashita
Journal of Atherosclerosis and Thrombosis.2018; 25(6): 512. CrossRef - Management of diabetes in older adults
G. Sesti, R. Antonelli Incalzi, E. Bonora, A. Consoli, A. Giaccari, S. Maggi, G. Paolisso, F. Purrello, G. Vendemiale, N. Ferrara
Nutrition, Metabolism and Cardiovascular Diseases.2018; 28(3): 206. CrossRef - DPP4 inhibitors and cardiovascular outcomes: safety on heart failure
Chang Xia, Aditya Goud, Jason D’Souza, CHanukya Dahagam, Xiaoquan Rao, Sanjay Rajagopalan, Jixin Zhong
Heart Failure Reviews.2017; 22(3): 299. CrossRef - Sodium Glucose Cotransporter-2 Inhibition in Heart Failure
Yuliya Lytvyn, Petter Bjornstad, Jacob A. Udell, Julie A. Lovshin, David Z.I. Cherney
Circulation.2017; 136(17): 1643. CrossRef - Antidiabetic medications use trends in an Andalusian region from 2001 to 2014
Rocío López-Sepúlveda, María Ángeles García Lirola, Esther Espínola García, Jose María Jurado Martínez, Salvadora Martín Sances, Sonia Anaya Ordóñez, José Cabeza Barrera
Primary Care Diabetes.2017; 11(3): 254. CrossRef - The regulatory role of DPP4 in atherosclerotic disease
Lihua Duan, Xiaoquan Rao, Chang Xia, Sanjay Rajagopalan, Jixin Zhong
Cardiovascular Diabetology.2017;[Epub] CrossRef - Guidelines on the management of arterial hypertension and related comorbidities in Latin America
Journal of Hypertension.2017; 35(8): 1529. CrossRef - Sodium Glucose Cotransporter 2 and Dipeptidyl Peptidase-4 Inhibition: Promise of a Dynamic Duo
Ildiko Lingvay
Endocrine Practice.2017; 23(7): 831. CrossRef - Assessment of the Risk of Hospitalization for Heart Failure With Dipeptidyl Peptidase-4 Inhibitors, Saxagliptin, Alogliptin, and Sitagliptin in Patients With Type 2 Diabetes, Using an Alternative Measure to the Hazard Ratio
Masayuki Kaneko, Mamoru Narukawa
Annals of Pharmacotherapy.2017; 51(7): 570. CrossRef - Dipeptidyl peptidase-4 inhibitors and cancer risk in patients with type 2 diabetes: a meta-analysis of randomized clinical trials
Ming Zhao, Jiayi Chen, Yanyan Yuan, Zuquan Zou, Xiaolong Lai, Daud M Rahmani, Fuyan Wang, Yang Xi, Qin Huang, Shizhong Bu
Scientific Reports.2017;[Epub] CrossRef - High circulating plasma dipeptidyl peptidase- 4 levels in non-obese Asian Indians with type 2 diabetes correlate with fasting insulin and LDL-C levels, triceps skinfolds, total intra-abdominal adipose tissue volume and presence of diabetes: a case–control
Shajith Anoop, Anoop Misra, Surya Prakash Bhatt, Seema Gulati, Ravindra Mohan Pandey, Harsh Mahajan
BMJ Open Diabetes Research & Care.2017; 5(1): bmjdrc-2017-000393. CrossRef - Vildagliptin reduces plasma stromal cell‐derived factor‐1α in patients with type 2 diabetes compared with glimepiride
Kyeong Seon Park, SooHeon Kwak, Young Min Cho, Kyong Soo Park, Hak C Jang, Seong Yeon Kim, Hye Seung Jung
Journal of Diabetes Investigation.2017; 8(2): 218. CrossRef - New peroral antidiabetic drugs and heart failure
Jana Jiráčková, Alena Šmahelová
Interní medicína pro praxi.2016; 18(2): 78. CrossRef - Plasma DPP4 activity is associated with no-reflow and major bleeding events in Chinese PCI-treated STEMI patients
Jing Wei Li, Yun Dai Chen, Wei Ren Chen, Jing Jing, Jie Liu, Yong Qiang Yang
Scientific Reports.2016;[Epub] CrossRef - Sitagliptin and risk of heart failure hospitalization in patients with type 2 diabetes on dialysis: A population-based cohort study
Yi-Chih Hung, Che-Chen Lin, Wei-Lun Huang, Man-Ping Chang, Ching-Chu Chen
Scientific Reports.2016;[Epub] CrossRef - Cardiovascular efficacy of sitagliptin in patients with diabetes at high risk of cardiovascular disease: a 12-month follow-up
Takashi Nakamura, Yoshitaka Iwanaga, Yuki Miyaji, Ryuji Nohara, Takao Ishimura, Shunichi Miyazaki
Cardiovascular Diabetology.2016;[Epub] CrossRef - Treating Diabetes in Patients with Heart Failure: Moving from Risk to Benefit
Ersilia M. DeFilippis, Michael M. Givertz
Current Heart Failure Reports.2016; 13(3): 111. CrossRef - Transcriptomic alterations in the heart of non-obese type 2 diabetic Goto-Kakizaki rats
Márta Sárközy, Gergő Szűcs, Veronika Fekete, Márton Pipicz, Katalin Éder, Renáta Gáspár, Andrea Sója, Judit Pipis, Péter Ferdinandy, Csaba Csonka, Tamás Csont
Cardiovascular Diabetology.2016;[Epub] CrossRef
- Sodium-Glucose Cotransporter-2 Inhibitor Use is Associated with a Reduced Risk of Heart Failure Hospitalization in Patients with Heart Failure with Preserved Ejection Fraction and Type 2 Diabetes Mellitus: A Real-World Study on a Diverse Urban Population
- Predictive Clinical Parameters and Glycemic Efficacy of Vildagliptin Treatment in Korean Subjects with Type 2 Diabetes
- Jin-Sun Chang, Juyoung Shin, Hun-Sung Kim, Kyung-Hee Kim, Jeong-Ah Shin, Kun-Ho Yoon, Bong-Yun Cha, Ho-Young Son, Jae-Hyoung Cho
- Diabetes Metab J. 2013;37(1):72-80. Published online February 15, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.1.72
- 3,755 View
- 32 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aims of this study are to investigate the glycemic efficacy and predictive parameters of vildagliptin therapy in Korean subjects with type 2 diabetes.
Methods In this retrospective study, we retrieved data for subjects who were on twice-daily 50 mg vildagliptin for at least 6 months, and classified the subjects into five treatment groups. In three of the groups, we added vildagliptin to their existing medication regimen; in the other two groups, we replaced one of their existing medications with vildagliptin. We then analyzed the changes in glucose parameters and clinical characteristics.
Results Ultimately, 327 subjects were analyzed in this study. Vildagliptin significantly improved hemoglobin A1c (HbA1c) levels over 6 months. The changes in HbA1c levels (ΔHbA1c) at month 6 were -2.24% (
P =0.000), -0.77% (P =0.000), -0.80% (P =0.001), -0.61% (P =0.000), and -0.34% (P =0.025) for groups 1, 2, 3, 4, and 5, respectively, with significance. We also found significant decrements in fasting plasma glucose levels in groups 1, 2, 3, and 4 (P <0.05). Of the variables, initial HbA1c levels (P =0.032) and history of sulfonylurea use (P =0.026) were independently associated with responsiveness to vildagliptin treatment.Conclusion Vildagliptin was effective when it was used in subjects with poor glycemic control. It controlled fasting plasma glucose levels as well as sulfonylurea treatment in Korean type 2 diabetic subjects.
-
Citations
Citations to this article as recorded by- Predictive clinical parameters for the hemoglobin A1c-lowering effect of vildagliptin in Japanese patients with type 2 diabetes
Yukihiro Bando, Masayuki Yamada, Keiko Aoki, Hideo Kanehara, Azusa Hisada, Kazuhiro Okafuji, Daisyu Toya, Nobuyoshi Tanaka
Diabetology International.2014; 5(4): 229. CrossRef - The Efficacy of Vildagliptin in Korean Patients with Type 2 Diabetes
Jun Sung Moon, Kyu Chang Won
Diabetes & Metabolism Journal.2013; 37(1): 36. CrossRef
- Predictive clinical parameters for the hemoglobin A1c-lowering effect of vildagliptin in Japanese patients with type 2 diabetes
- Changes in Adenosine Deaminase Activity in Patients with Type 2 Diabetes Mellitus and Effect of DPP-4 Inhibitor Treatment on ADA Activity
- Jae-Geun Lee, Dong Gu Kang, Jung Re Yu, Youngree Kim, Jinsoek Kim, Gwanpyo Koh, Daeho Lee
- Diabetes Metab J. 2011;35(2):149-158. Published online April 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.2.149
- 4,227 View
- 33 Download
- 28 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Dipeptidyl peptidase 4 (DPP-4, also known as CD26) binds with adenosine deaminase (ADA) to activate T lymphocytes. Here, we investigated whether ADA activity is specifically affected by treatment with DPP-4 inhibitor (DPP4I) compared with other anti-diabetic agents.
Methods Fasting ADA activity, in addition to various metabolic and biochemical parameters, were measured in 262 type 2 diabetes mellitus (T2DM) patients taking various anti-diabetic agents and in 46 non-diabetic control subjects.
Results ADA activity was increased in T2DM patients compared with that in non-diabetic control subjects (mean±standard error, 23.1±0.6 U/L vs. 18.6±0.8 U/L;
P <0.05). ADA activity was correlated with fasting plasma glucose (r =0.258,P <0.05), HbA1c (r =0.208,P <0.05), aspartate aminotransferase (r =0.325,P <0.05), and alanine aminotransferase (r =0.248,P <0.05). Compared with the well-controlled T2DM patients (HbA1c<7%), the poorly controlled group (HbA1c>9%) showed significantly increased ADA activity (21.1±0.8 U/L vs. 25.4±1.6 U/L;P <0.05). The effect of DPP4I on ADA activity in T2DM patients did not differ from those of other oral anti-diabetic agents or insulin. T2DM patients on metformin monotherapy showed a lower ADA activity (20.9±1.0 U/L vs. 28.1±2.8 U/L;P <0.05) compared with that of those on sulfonylurea monotherapy.Conclusion Our results show that ADA activity is increased in T2DM patients compared to that in non-diabetic patients, is positively correlated with blood glucose level, and that DPP4I has no additional specific effect on ADA activity, except for a glycemic control- or HbA1c-dependent effect.
-
Citations
Citations to this article as recorded by- Influence of BMI on adenosine deaminase and stroke outcomes in mechanical thrombectomy subjects
Benton Maglinger, Christopher J. McLouth, Jacqueline A. Frank, Chintan Rupareliya, Madison Sands, Lila Sheikhi, Shivani Pahwa, David Dornbos, Jordan P. Harp, Amanda L. Trout, Jadwiga Turchan-Cholewo, Ann M. Stowe, Justin F. Fraser, Keith R. Pennypacker
Brain, Behavior, & Immunity - Health.2022; 20: 100422. CrossRef - Glutamine restores testicular glutathione-dependent antioxidant defense and upregulates NO/cGMP signaling in sleep deprivation-induced reproductive dysfunction in rats
M.A. Hamed, T.M. Akhigbe, R.E. Akhigbe, A.O. Aremu, P.A. Oyedokun, J.A. Gbadamosi, P.E. Anifowose, M.A. Adewole, O.O. Aboyeji, H.O. Yisau, G.O. Tajudeen, M.M. Titiloye, N.F. Ayinla, A.F. Ajayi
Biomedicine & Pharmacotherapy.2022; 148: 112765. CrossRef - Effects of quercetin and metabolites on uric acid biosynthesis and consequences for gene expression in the endothelium
Sarka Tumova, Yuanlu Shi, Ian M. Carr, Gary Williamson
Free Radical Biology and Medicine.2021; 162: 191. CrossRef - The value of adenosine deaminase activity in latent autoimmune diabetes in adults and type 2 diabetes patients
Yu Zhou, Wei-Dong Jin, Zhen-Zhen Pang, Jun Xia, Su-Feng Chen
International Journal of Diabetes in Developing Countries.2021; 41(1): 48. CrossRef - Purinergic signaling in diabetes and metabolism
Shanu Jain, Kenneth A. Jacobson
Biochemical Pharmacology.2021; 187: 114393. CrossRef - Berberine modulates crucial erectogenic biomolecules and alters histological architecture in penile tissues of diabetic rats
Stephen Adeniyi Adefegha, Ganiyu Oboh, Felix Abayomi Dada, Sunday Idowu Oyeleye, Bathlomew Maduka Okeke
Andrologia.2021;[Epub] CrossRef - Suppression of uric acid and lactate production by sodium acetate ameliorates hepatic triglyceride accumulation in fructose-insulin resistant pregnant rats
Adewumi O. Oyabambi, Kehinde S. Olaniyi, Ayodele O. Soladoye, Lawrence A. Olatunji
Environmental Toxicology and Pharmacology.2020; 80: 103452. CrossRef - Therapeutic Perspectives of Adenosine Deaminase Inhibition in Cardiovascular Diseases
Barbara Kutryb-Zajac, Paulina Mierzejewska, Ewa M. Slominska, Ryszard T. Smolenski
Molecules.2020; 25(20): 4652. CrossRef - Adenosine as a Marker and Mediator of Cardiovascular Homeostasis: A Translational Perspective
Trevor Simard, Richard Jung, Alisha Labinaz, Mohammad Ali Faraz, F. Daniel Ramirez, Pietro Di Santo, Ian Pitcher, Pouya Motazedian, Chantal Gaudet, Rebecca Rochman, Jeffrey Marbach, Paul Boland, Kiran Sarathy, Saleh Alghofaili, Juan J. Russo, Etienne Cout
Cardiovascular & Hematological Disorders-Drug Targets.2019; 19(2): 109. CrossRef - Mineralocorticoid receptor blockade attenuates disrupted glutathione-dependent antioxidant defense and elevated endoglin in the hearts of pregnant rats exposed to testosterone
Taofeek O. Usman, Olufunto O. Badmus, InKyeom Kim, Lawrence A. Olatunji
Naunyn-Schmiedeberg's Archives of Pharmacology.2019; 392(7): 773. CrossRef - Serum activities of dipeptidyl peptidase-4 and adenosine deaminase in polycystic ovary syndrome: association with obesity
Seda Kahraman, Alev Eroglu Altinova, Serenay Elgun, Mehmet Muhittin Yalcin, Banu Aktas Yilmaz, Cigdem Ozkan, Mujde Akturk, Fusun Balos Toruner
Gynecological Endocrinology.2019; 35(8): 714. CrossRef - Serum adenosine deaminase activity and coronary artery disease: a retrospective case-control study based on 9929 participants
Chao Xuan, Qing-Wu Tian, Shao-Yan Zhang, Hui Li, Ting-Ting Tian, Peng Zhao, Kang Yue, Yan-Yan Ling, Guo-Wei He, Li-Min Lun
Therapeutic Advances in Chronic Disease.2019; 10: 204062231989153. CrossRef - Metabolites related to purine catabolism and risk of type 2 diabetes incidence; modifying effects of the TCF7L2-rs7903146 polymorphism
Christopher Papandreou, Jun Li, Liming Liang, Mònica Bulló, Yan Zheng, Miguel Ruiz-Canela, Edward Yu, Marta Guasch-Ferré, Cristina Razquin, Clary Clish, Dolores Corella, Ramon Estruch, Emilio Ros, Montserrat Fitó, Fernando Arós, Lluís Serra-Majem, Nuria R
Scientific Reports.2019;[Epub] CrossRef - Current status of G-protein coupled receptors as potential targets against type 2 diabetes mellitus
Mehboob Hoque, Safdar Ali, Muddasarul Hoda
International Journal of Biological Macromolecules.2018; 118: 2237. CrossRef - Endoglin inhibition by sodium acetate and flutamide ameliorates cardiac defective G6PD-dependent antioxidant defense in gestational testosterone-exposed rats
Lawrence A. Olatunji, Emmanuel D. Areola, Olufunto O. Badmus
Biomedicine & Pharmacotherapy.2018; 107: 1641. CrossRef - Sodium acetate and androgen receptor blockade improve gestational androgen excess-induced deteriorated glucose homeostasis and antioxidant defenses in rats: roles of adenosine deaminase and xanthine oxidase activities
Taofeek O. Usman, Emmanuel D. Areola, Olufunto O. Badmus, InKyeom Kim, Lawrence A. Olatunji
The Journal of Nutritional Biochemistry.2018; 62: 65. CrossRef - ADENOSINE DEAMINASE ACTIVITY IN TYPE 2 DIABETES MELLITUS
Farija Peruvankuzhiyil, Lavanya Madhavan, Manaloor George Joseraj
Journal of Evidence Based Medicine and Healthcare.2017; 4(5): 238. CrossRef - Adenosine signaling in diabetes mellitus and associated cardiovascular and renal complications
Maria Peleli, Mattias Carlstrom
Molecular Aspects of Medicine.2017; 55: 62. CrossRef - The Adenosinergic System in Diabetic Retinopathy
J. Vindeirinho, A. R. Santiago, C. Cavadas, A. F. Ambrósio, P. F. Santos
Journal of Diabetes Research.2016; 2016: 1. CrossRef - Upregulation of inducible NO synthase by exogenous adenosine in vascular smooth muscle cells activated by inflammatory stimuli in experimental diabetes
Alberto Nassi, Francesca Malorgio, Serena Tedesco, Andrea Cignarella, Rosa Maria Gaion
Cardiovascular Diabetology.2016;[Epub] CrossRef - Reduced adenosine A2a receptor–mediated efferent arteriolar vasodilation contributes to diabetes-induced glomerular hyperfiltration
Patrik Persson, Peter Hansell, Fredrik Palm
Kidney International.2015; 87(1): 109. CrossRef - CD26/DPP4 Levels in Peripheral Blood and T Cells in Patients With Type 2 Diabetes Mellitus
Sang Ah Lee, Young Ree Kim, Eun Jin Yang, Eun-Jeong Kwon, Sun Hyung Kim, Sung Ha Kang, Doek Bae Park, Byung-Chul Oh, Jinseok Kim, Sang Taek Heo, Gwanpyo Koh, Dae Ho Lee
The Journal of Clinical Endocrinology & Metabolism.2013; 98(6): 2553. CrossRef - Raised Serum Adenosine Deaminase Level in Nonobese Type 2 Diabetes Mellitus
Vineet Kumar Khemka, Debajit Bagchi, Arindam Ghosh, Oishimaya Sen, Aritri Bir, Sasanka Chakrabarti, Anindita Banerjee
The Scientific World Journal.2013; 2013: 1. CrossRef - Phosphodiesterase III Inhibition Increases cAMP Levels and Augments the Infarct Size Limiting Effect of a DPP-4 Inhibitor in Mice with Type-2 Diabetes Mellitus
Yochai Birnbaum, Alexander C. Castillo, Jinqiao Qian, Shukuan Ling, Hongmei Ye, Jose R. Perez-Polo, Mandeep Bajaj, Yumei Ye
Cardiovascular Drugs and Therapy.2012; 26(6): 445. CrossRef - Serum Adenosine deaminase activity in type 2 Diabetes Mellitus patients
M. N. Vanitha Gowda, K. C. Vasudha, S. Reshma, K. J. Sujatha
International Journal of Diabetes in Developing Countries.2012; 32(3): 176. CrossRef - Cyclic AMP and PKA: How can a Lot of Good Come from the Potentially Bad?
Barbara Huisamen
Cardiovascular Drugs and Therapy.2012; 26(6): 435. CrossRef - Gadd45α: A Novel Diabetes-Associated Gene Potentially Linking Diabetic Cardiomyopathy and Baroreflex Dysfunction
Ning Wang, Chao Yang, Fang Xie, Lihua Sun, Xiaolin Su, Ying Wang, Ran Wei, Rong Zhang, Xia Li, Baofeng Yang, Jing Ai, Rajesh Gopalrao Katare
PLoS ONE.2012; 7(12): e49077. CrossRef - The CD39-Adenosinergic Axis in the Pathogenesis of Immune and Nonimmune Diabetes
Joanne S. J. Chia, Jennifer L. McRae, Peter J. Cowan, Karen M. Dwyer
Journal of Biomedicine and Biotechnology.2012; 2012: 1. CrossRef
- Influence of BMI on adenosine deaminase and stroke outcomes in mechanical thrombectomy subjects

 KDA
KDA
 First
First Prev
Prev





