- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Ahead-of print > Article
-
Sulwon Lecture 2023Metabolic Risk/Epidemiology Insulin Resistance, Non-Alcoholic Fatty Liver Disease and Type 2 Diabetes Mellitus: Clinical and Experimental Perspective
-
Inha Jung1
 , Dae-Jeong Koo2, Won-Young Lee3
, Dae-Jeong Koo2, Won-Young Lee3
-
DOI: https://doi.org/10.4093/dmj.2023.0350
Published online: February 2, 2024
- 1,024 Views
- 60 Download
1Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
2Division of Endocrinology and Metabolism, Department of Internal Medicine, Changwon Fatima Hospital, Changwon, Korea
3Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- Corresponding author: Won-Young Lee Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, 29 Saemunan-ro, Jongno-gu, Seoul 03181, Korea E-mail: wonyoung2.lee@samsung.com
Copyright © 2024 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- It has been generally accepted that insulin resistance (IR) and reduced insulin secretory capacity are the basic pathogenesis of type 2 diabetes mellitus (T2DM). In addition to genetic factors, the persistence of systemic inflammation caused by obesity and the associated threat of lipotoxicity increase the risk of T2DM. In particular, the main cause of IR is obesity and subjects with T2DM have a higher body mass index (BMI) than normal subjects according to recent studies. The prevalence of T2DM with IR has increased with increasing BMI during the past three decades. According to recent studies, homeostatic model assessment of IR was increased compared to that of the 1990s. Rising prevalence of obesity in Korea have contributed to the development of IR, non-alcoholic fatty liver disease and T2DM and cutting this vicious cycle is important. My colleagues and I have investigated this pathogenic mechanism on this theme through clinical and experimental studies over 20 years and herein, I would like to summarize some of our studies with deep gratitude for receiving the prestigious 2023 Sulwon Award.
Highlights
- The process that begins with insulin resistance (IR) due to various causes and eventually leads to a decrease in the insulin secretion capacity is accepted as the basic concept for the development of type 2 diabetes mellitus (T2DM) [1]. Although previous studies were based on data from the 1990s, compared to Western populations, the severity of obesity rate and IR (based on euglycemic clamp studies) in Koreans with T2DM were relatively low [2,3]. However, the overall prevalence of obesity in Koreans continues to rise, and in particular, the prevalence of stage 3 or higher morbid obesity has nearly tripled over the past 10 years [4]. These changes lead to an increase in IR, which may appear in a form similar to the developmental mechanism of Western diabetic patients [5,6]. Furthermore, rising prevalence of obesity in Korea has contributed to the increasing incidence of cardiovascular diseases (CVD), non-alcoholic fatty liver disease (NAFLD) in addition to T2DM [7], and cutting this vicious cycle is important because a large cohort study of Koreans found that the long-term increase in mortality is related to prediabetes as well as T2DM [8]. NAFLD has recently undergone a new definition and change in terminology, called metabolic dysfunction-associated fatty liver disease [9] and is very closely cross-talked with IR [10]. Most importantly, NAFLD is emerging as an independent risk factor for CVD [11,12]. Our hospital has a large cohort called the Kangbuk Samsung Health Study (KSHS), through which retrospective and prospective studies could be conducted. Millions of participants have participated in these cohorts, making that an invaluable tool in longitudinal research to study the nature or associations of disease. Together with my colleagues, I have been studying about this theme through clinical and experimental studies over 20 years and herein, I would like to summarize and introduce some of our works (Fig. 1).
INTRODUCTION
- It is agreed that one of the main causes of IR is obesity. Subjects with T2DM have a higher body mass index (BMI) than normal subjects according to numerous studies [6]. The prevalence of T2DM with IR has increased with increasing BMI during the past three decades (Table 1) [5,13-25]. According to a study from the 2000s, homeostatic model assessment of insulin resistance (HOMA-IR) was increased compared to that of the 1990s [13]. However, parameters of insulin secretion (oral disposition index, insulinogenic index) did not change in Korean T2DM [6]. This suggests that the role of IR in the pathogenesis of Korean T2DM has enlarged during past decade. There were two cross-sectional studies that reported that the main pathophysiology in Korean T2DM was IR. Kim et al. [23] performed a short insulin tolerance test and found that the prevalence of IR was 70.6% through a normoglycemic-hyperinsulinemic clamp study. In another study reported by Son et al. [5], the prevalence of IR (HOMA-IR >2.5) was 59.5%.
- Interestingly, we reported a study examining the spectrum of insulin sensitivity in a large sample of Korean adults [26]. The aims were to find the range of values for insulin sensitivity indexes and to determine cutoff levels of HOMA-IR conferring the increased risk for metabolic syndrome. Subjects (n=83,186) were analyzed among apparently healthy person who do not take any medication of T2DM, hypertension or dyslipidemia. By using receiver operating characteristic (ROC) curves, the fasting serum insulin and HOMA levels were compared and the insulin and HOMA values at the point on the ROC curve closest to 100% sensitivity and 100% specificity to detect metabolic syndrome were 9.7 and 2.43 µU/mL, respectively. It was the first try to determine cutoff values for IR indexes above which the risk of metabolic syndrome is increased. This kind of study could be used to assess the IR in epidemiologic studies. It seems undesirable to focus on only one of IR and insulin secretion in the pathogenesis of T2DM. Most patients of T2DM have both IR and insulin secretory defect. If IR appears in people who are genetically susceptible to have low insulin secretory function, and if β-cells can not compensate for IR appropriately, the people will develop T2DM. IR contributes to develop T2DM, and Koreans become T2DM easily with a relatively low BMI status compared to Caucasians. The increased prevalence of obesity and IR could contribute to the increased risk of T2DM during the past three decades in Korea. The preceding evidence shows that although IR is a contributing factor in the development of T2DM in Koreans, defects in insulin secretion are the determining factor.
IR STATUS IN KOREANS
- We investigated whether IR could impact on mortality and inflammation could influence the association of IR and mortality in 165,849 general population in Korea [27]. The study was conducted on 1,417,325.6 person-years over a mean follow-up period of more than 8 years, and IR status was based on HOMA-IR (≥75%) and inflammatory status was based on high-sensitivity C-reactive protein (hs-CRP ≥2.0 mg/L). In this study, we found systemic inflammation can have a role to predict the allcause and cancer-related mortality risks, independent of the IR status. This trend was especially prominent in cancer-related mortality. Although IR could not impact on the mortality in Koreans, observation over the extended period could result in another finding and this needs to be studied. We undertook another longitudinal mortality study in which baseline glycemic status could impact later mortality in over 241,499 Korean adults by analyzing KSHS [8]. IR starts along before the hyperglycemia develops and even the subjects with prediabetes have higher risk for mortality. Baseline glycemic status and 7 years later mortality was assessed, and we found that subjects with T2DM had higher all-cause mortality significantly than normoglycemic subjects after multivariable adjustment. Cancer mortality was also higher in subjects with T2DM. When considering these differences in mortality according to glycemia was prominent in this short observation period, these differences could enlarge over the extended period. Therefore, careful blood glucose management and screening for cancer and cardiovascular complications are important in patients with T2DM.
IR AND MORTALITY IN KOREANS
- The reason why the increasing prevalence of obesity in Korea is of clinical interest is because obesity induces a systemic inflammatory status and is associated with worsening IR [28]. In particular, IR is more affected by fat distribution than simple obesity, and an increase in visceral fat is related to intrahepatic IR as well as peripheral IR [29,30]. Adiponectin, which is secreted from adipocytes and is associated with protective effects against metabolic abnormalities and CVD, is inversely proportional to the amount of fat in the abdomen and liver, and this result is also closely related to peripheral and intrahepatic IR [31,32]. Activation of proinflammatory cytokines such as tumor necrosis factor-α (TNF-α), CRPs, interleukin-6, plasminogen activation factor inhibitor-1, and leptin has been understood as a core pathophysiology in the mechanism by which obesity (including severe subcutaneous fat) causes systemic inflammation [33-36], which ultimately leads to IR and T2DM [37]. In these process, activation of the nuclear factor-κB (NF-κB) pathway and c-Jun NH2-terminal kinase (JNK) pathway due to endoplasmic reticulum (ER) stress, reactive oxygen species, and ceramide was found to play a underlying key role [38-43].
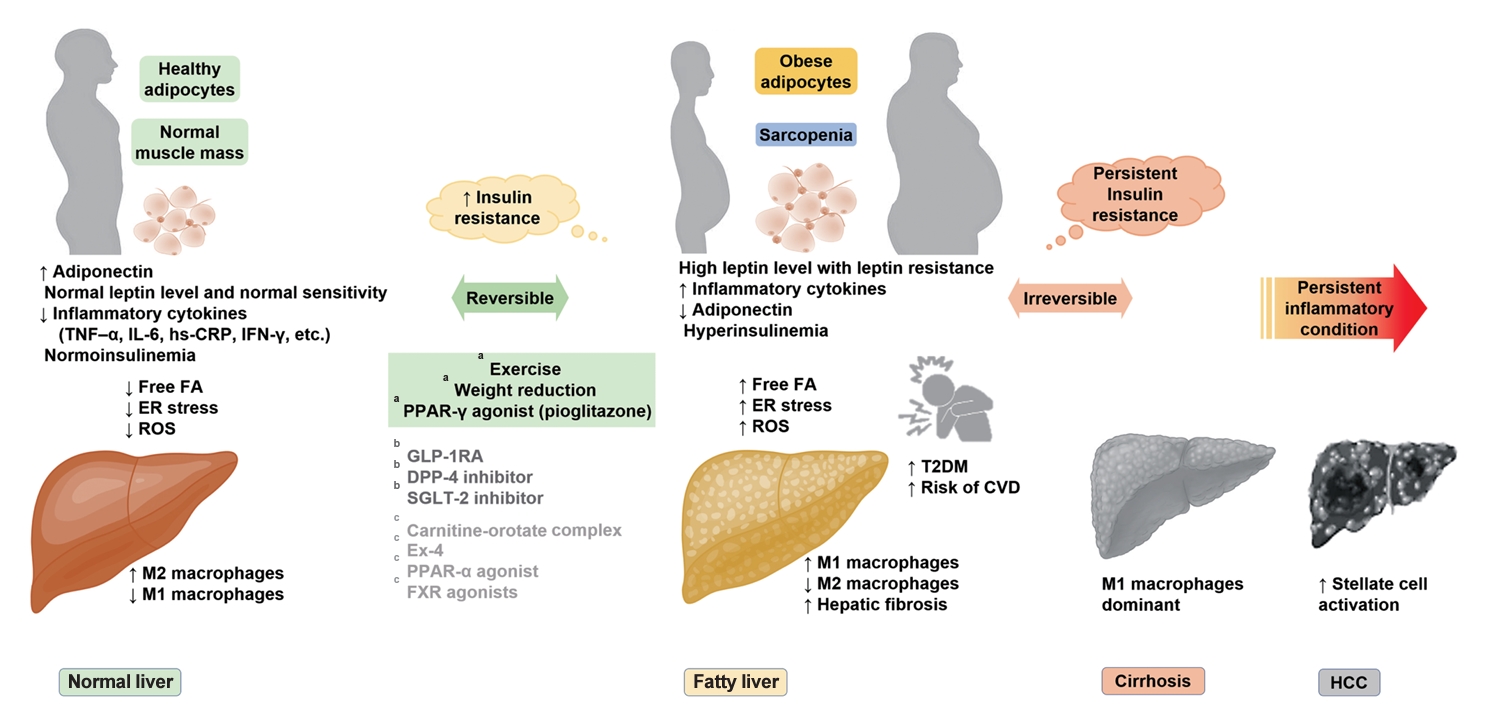
- IR and NAFLD are cross-talked with each other [10], and the relationship may be independent of the severity of obesity [44,45]. IR has been regarded as the culprit behind the development of NAFLD [46-48]. Among the sources of fatty acids for triacylglycerol (TG) synthesis: diet, lipolysis, and hepatic de novo lipogenesis (DNL), the largest source of TG synthesis in NAFLD patients, under dietary control, is free fatty acid (FFA) from lipolysis [49]. When the anti-lipolytic effect of insulin is inhibited under IR condition, FFA is excessively produced [50]. And hyperinsulinemia caused by IR further increases DNL. In this process, activation of sterol receptor binding protein 1c (SREBP-1c) is important, and hyperinsulinemia is a condition that promotes SREBP-1c [51-53]. On the other hand, forkhead box protein A2 (FOXA2), which is activated under low insulin level, promotes lipid metabolism and fatty acid oxidation, but plays the opposite role in hyperinsulinemia [54]. This adaptation process in the early stages of IR promotes steatosis and increases the liver mitochondrial respiration rate during this period [55]. However, if IR persists and progresses to the non-alcoholic steatohepatitis (NASH) stage, such effects disappear. Moreover, when TG synthesis is disrupted, hepatocyte damage occurs due to excessive fatty acid oxidation [56]. On the other hand, some studies show that fatty liver itself, induced by various causes, is a factor that worsens IR [57,58]. FFA excess influx into the liver induces activation of protein kinase C-δ (PKC-δ), which is believed to trigger hepatic IR through insulin receptor phosphorylation [59]. In this process, activation of NF-κB and JNK pathways through PKC-θ and Toll-like receptor (TLR) activation is also involved [60-62]. In animal models, mice with fatty liver induced by SREBP-1c overexpression and inhibition of fatty acid oxidation showed systemic IR [63,64]. Recent studies have shown that lipogenic substrates induce an increase in DNL precursors and enzymes that induce steatosis of liver through carbohydrate response element-binding protein (ChREBP) activation [65]. Furthermore, it has been reported that the composition, structure, and metabolic processes of lipid droplets (LDs) play an important role in the progression of NAFLD [66]. In advanced NAFLD (fibrosis or NASH), hepatic macrophages, especially proinflammatory M1 Kupffer cells stimulated by TLR ligands and interferon-γ, act as key pathological mediators.
- As is well known, prevention of NAFLD and fibrosis progression is clinically very important. We reported the clinical significance of visceral-to-subcutaneous abdominal fat ratio (VSR) in the development of NAFLD as well as fibrosis progression based on a study of 7,465 adults [67]. Liver fibrosis was assessed based on fibrosis-4 (FIB-4) score and aspartate aminotransferase-to-platelet ratio index, and the severity of fibrosis was classified as low, indeterminate, or high. VSR assessed by abdominal computed tomography was significantly related with the prevalence of NAFLD and risk of liver fibrosis. We also reported the association of weight variability and risk of NAFLD in 30,708 Korean adults [68]. Weight gain is closely related with increased IR and some studies suggested that repeated weight gain or loss is related with increased morbidity in various diseases [69]. During 4 years’ observation period, high weight variability was significantly associated with new development of NAFLD regardless of baseline weight status. Targeting to reduce weight variability can be tried to prevent the development of NAFLD. Although many clinical studies dealing with this theme have been reported [70,71], clinical studies to find the role of IR in the development of liver fibrosis is even scarce [72-76]. We reported interesting papers about the association of baseline IR status and new development of liver fibrosis, assessed by biomarkers. One study was about that baseline IR could impact later development of liver fibrosis [77], and another study was that changes in HOMA-IR during the 6-year follow-up period were associated with changes in liver fibrosis indices [78]. Although liver biopsy was not performed in our studies, it is probable that IR in human can be closed related with new development of liver fibrosis and it needs to be validated with liver biopsy studies. Weight gain may be a precipitating factor in the progression of hepatic steatosis to fibrosis. Additionally, changes in IR was associated with later development or progression of NAFLD in our cohort study.
OBESITY, IR, AND PROGRESSION OF NAFLD
- NAFLD and CVD are closely related, and we reported the significant relationships between severity of NAFLD and 10-year CVD risk calculated by Framingham risk score and pooled cohort equation (PCE) [79]. This finding suggests that NAFLD severity was an independent factor for ≥7.5% estimated CVD risk and that the PCE calculation may be appropriate when assessing 10-year CVD risk among individuals with NAFLD. We also reported the role of metabolic health in the development of NAFLD in a 4-year longitudinal study and found that metabolic health is more important than obesity in NAFLD [80]. Whether NAFLD might be an independent determinant of metabolic health apart from obesity has not yet been clarified. Therefore, we intended to compare the risk of NAFLD among subjects classified based on metabolic health and obesity status. This study suggests the importance of early and intensive lifestyle modification in metabolically unhealthy subject since a prolonged period of a metabolically unhealthy status could result in NAFLD and metabolic derangements. Another interesting finding was that subjects who were metabolically healthy at baseline but metabolically unhealthy after 4 years had a significantly higher risk of NAFLD compared to subjects who were metabolically unhealthy at baseline but metabolically healthy after 4 years. This result was consistent with previous findings that early intervention in metabolically unhealthy subjects can prevent NAFLD and metabolic abnormalities.
- We further reported the relation of biomarkers and NAFLD in cross-sectional studies and longitudinal studies. Serum adipocyte-specific fatty acid binding protein was significantly associated with fatty liver index [81]. TNF-α was also related with later development of NAFLD in Korean adults [82]. The relationship between autonomic dysfunction and NAFLD was studied by our group because it is unclear although autonomic imbalance is related with an increased risk for metabolic disease [83]. A total of 33,899 participants without NAFLD who underwent health screening programs between 2011 and 2018 were enrolled. With a median follow-up of 5.7 years, low parasympathetic activity, and recently enhanced sympathetic activity might increase the risk of NAFLD. We also reported a study about the simple self-assessment score consists of age, sex, waist circumference, BMI, history of T2DM and dyslipidemia, alcohol intake, physical activity, and menopause status, which are independently associated with NAFLD, and this simple score could be a guide to identify individuals at high-risk of NAFLD [84]. And we studied the association between glomerular hyperfiltration (GHF) and the risk of NAFLD [85]. In a longitudinal study including 147,479 relatively healthy adults, we found that GHF (defined as age- and sex-specific estimated glomerular filtration rate above the 95th percentile) status was associated with future NAFLD development assessed using ultrasonography (US) and progression to fibrosis assessed using NAFLD fibrosis score and FIB-4. A recent study demonstrated the importance of leg-fat to total fat ratio for NAFLD risk in a nationwide survey [86], and another study reported the significance of a noninvasive liver fibrosis score (diabetes fibrosis score) which is more specific for patients with T2DM based on transient elastography [87].
- Recent pharmacological treatments for NASH have been reviewed, and the implications of recent failures about NASH treatment highlight that targeting only one pathway or mechanism is not sufficient to improve NASH [88]. This underscores the need to find the common root of NASH progression and candidates that can modulate multiple pathways or disease cascades in NASH pathophysiology. And above all, we need to strengthen clinical research targeting Koreans.
CHARACTERISTICS OF NAFLD IN KOREANS
- Sarcopenia is reported to be independently related with steatohepatitis and hepatic fibrosis risk in NAFLD patients. Skeletal muscle is a main organ in which glucose metabolism through insulin is proceeded. Many epidemiologic studies and experimental studies show the relation between low muscle mass and increased IR. Thus, we can speculate that sarcopenia can promote IR and thus contribute to development of NAFLD. A recent longitudinal study reported an association between the persistent decline in appendicular muscle mass with aging and the risk of NAFLD [89]. Chronic inflammation also can increase the loss of muscle and inflammation in NAFLD can also promote sarcopenic process, thus activate the vicious cycle between sarcopenia and NAFLD. And the effect of sarcopenia on the liver fibrosis is reported to be higher in non-obese subjects than in obese subjects. NAFLD can be developed in subjects with low visceral adipose tissue, and it is frequently observed in Asian subjects [90]. We reported that regular exercise is associated with reduced risk of NAFLD independent of obesity in Korean adults [91]. Exercise and weight loss is a main strategy and physiologic approach to prevent and treat NAFLD [92]. More research is needed to assess the real relationship between sarcopenia and NAFLD.
ASSOCIATION OF NAFLD AND SARCOPENIA
- NAFLD is regarded as an independent risk factor for T2DM and frequently precede before the development of T2DM. Prospective epidemiologic studies show that alanine transaminase (ALT) or gamma-glutamyl transferase is independently associated with new development of T2DM [93-95] and patients with NAFLD diagnosed by ultrasound have been reported to have a two-fold higher risk of T2DM later in life [96]. 78% of 129 subjects with NAFLD proven with liver biopsy developed glucose intolerance in 14-year prospective study and among them those with liver fibrosis had significantly higher risk for T2DM [97]. NAFLD can be developed from IR and NAFLD itself aggravated IR, thus increase the risk of T2DM [10]. IR can promote the adipose deposit to extra-hepatic organs, such as skeletal muscle and pancreas and it can affect insulin secretory capacity. We reported that hyperinsulinemia at baseline was associated with significantly increased risk for later development of NAFLD [46]. We undertook cross-sectional study among 99,969 subjects and found that NAFLD was significantly related with HOMA-IR and glycosylated hemoglobin in in nondiabetic individuals and this relationship was independent of BMI and other metabolic components [98]. Combined effect of IFG and NAFLD in the development of T2DM was reported in a longitudinal study among 7,849 subjects who underwent annual liver ultrasound for 5 years [99]. That means that NAFLD has an additive and independent effect on the development of T2DM under conditions of impaired insulin secretion. In the same vein, we reported that during the follow-up of 4 years, Korean subjects with the sustained NAFLD had 1.5 higher risk for new development of T2DM compared with those having never NAFLD, whereas the risk was not higher in the intermittent NAFLD group [100]. For this reason, there is a need to pay attention to patients with persistent NAFLD. We also reported the additive effect of NAFLD on new onset of T2DM in subjects with metabolic syndrome [101]. Additionally, we observed that subjects with both NAFLD on US and elevated liver enzymes had higher risk for developing T2DM [102]. Efforts for screening or predicting NAFLD or liver fibrosis in T2DM subjects have been tried. Performance analysis of fibrosis in subjects with NAFLD with or without T2DM was reported [103], and non-laboratory-based screening tool for NAFLD was reported in Koreans with T2DM [104].
- T2DM in subjects with NAFLD is associated with about twofold higher risk of liver fibrosis, liver related death rate [105]. Subjects with T2DM commonly has abnormal liver function or US findings and even with normal liver function test, severity of NAFLD histologically proven is higher. American diabetes association recommends active surveillance for liver fibrosis when NAFLD is suspected in T2DM patients [106]. Hyperinsulinemia and chronic inflammation in T2DM can increase the risk of hepatocellular carcinoma (HCC). In England registry, NAFLD related HCC increased 10-fold for 10 years from 2000 to 2010 and the proportion of patients with metabolic risk factors such as T2DM or obesity was about 66% [107].
- Efforts to improve NAFLD in T2DM with medication was attempted and more trials are needed to test efficacy. There are growing evidence supporting beneficial effects of dipeptidyl peptidase-4 (DPP-4) inhibitor, glucagon-like peptide-1 receptor agonists (GLP-1RAs) and sodium-glucose cotransporter-2 (SGLT-2) inhibitors on NAFLD [108]. While increasing amount of in vivo and in vitro research highlights the potential of DPP-4 inhibitors, GLP-1RAs and SGLT-2 inhibitors in NAFLD treatment, the clinical data demonstrating their efficacy in patients with NAFLD are limited [109,110]. We have proposed that carnitine-orotate complex has the potential to alleviate ALT and computed tomography-identified hepatic steatosis in patients with both T2DM and NAFLD [111].
ASSOCIATION OF NAFLD AND T2DM
- In our pursuit of understanding the pathogenesis of NAFLD and identifying potential pharmacological interventions, our research encompassed a series of experimental investigations. Initially, we examined the effects of exendin-4 (Ex-4) on sirtuin 1 (SIRT1) expression and its role in ameliorating hepatic steatosis, as described by Lee et al. [112] in this study titled ‘Exendin-4 improves steatohepatitis by increasing Sirt1 expression in high-fat diet-induced obese C57BL/6J mice.’ To elucidate whether Ex-4 modulates SIRT1 expression as a mechanistic basis for improving fatty liver, we conducted a series of experiments in high-fat diet-induced obese C57BL/6J mice and cell culture models. These investigations revealed that the upregulation of SIRT1 induced by Ex-4 treatment provided protection against high-fat diet-induced steatohepatitis, primarily through stimulation of fatty acid oxidation. In another study, we explored Ex-4’s potential to alleviate palmitate-induced ER stress through SIRT1 in HepG2 cells [113]. In this study, palmitate exposure led to an upregulation of ER stress markers (phospho-inositol-requiring transmembrane kinase/endoribonuclease 1α [P-IRE1α], activating transcription factor 6 [ATF6], X-box binding protein 1 [XBP1], CCAAT/enhancer-binding protein homologous protein [CHOP]), but Ex-4 administration effectively downregulated these markers and increased sarco/endoplasmic reticulum calcium ion ATPase 2b (SERCA2b) expression. Additionally, Ex-4 reduced hepatic expression of p53 up-regulated modulator of apoptosis (PUMA), BCL2 associated X (BAX), cytochrome c, and cleaved caspase-3. Importantly, blocking SIRT1 reversed these effects, highlighting the significance of SIRT1 in Ex-4’s protective mechanisms. In our experiments concerning fibroblast growth factor 21 (FGF21), suppressing FGF21 with siRNA in hepatocytes resulted in reduced expression of medium-chain acyl-coenzyme A dehydrogenase (MCAD) and peroxisome proliferator-activated receptor α (PPARα) [114]. Intriguingly, when we treated cells with Ex-4 and inhibited SIRT1 (but not SIRT6) via siRNA, it led to a decrease in FGF21 mRNA expression, while FGF21 inhibition did not impact SIRT1. These findings suggest that Ex-4 may ameliorate hepatic steatosis by enhancing SIRT1-mediated FGF21. Furthermore, the glycoproteins selenoprotein P (SEPP1) and fetuin-A, derived from the liver and circulating in the bloodstream, have emerged as potential biomarkers for IR and NAFLD. However, the influence of Ex-4 on the expression of these hepatokines, SEPP1 and fetuin-A, remains a subject of inquiry. Our experiments with HepG2 cells yielded compelling evidence indicating that Ex-4 significantly reduced the expression of hepatic SEPP1 and fetuin-A [115]. This reduction was attributed to the amelioration of palmitate-induced ER stress, orchestrated by adenosine monophosphate-activated protein kinase. Collectively, these results enhance our overall understanding of NAFLD and potential therapeutic strategies, providing valuable insights into the complex regulatory systems within hepatic physiology.
- We also found that dulaglutide could decrease hepatic lipid accumulation by activating family with sequence similarity 3 member A (FAM3A) signaling pathway [116]. In this study, dulaglutide demonstrated significant reductions in hepatic lipid accumulation and suppression of genes linked to LD binding proteins, DNL, and TG synthesis in palmitic acid treated HepG2 cells. Additionally, Dulaglutide promoted lipolysis, fatty acid oxidation, and FAM3A expression, suggesting its potential therapeutic utility in NAFLD, mediated partly through GLP-1R-dependent upregulation of FAM3A.
- In one study, the loss of farnesoid X receptor (FXR) in mice exacerbated atherosclerosis and hepatic steatosis, with a PPARα agonist partially reversing these conditions by modulating fatty acid metabolism-related gene expression [117]. Another in vitro investigation reveals that succinate acts as a signaling molecule in hepatic stellate cells, contributing to mitochondrial dysfunction [118]. This study also found that gemigliptin, a DPP-4 inhibitor, demonstrated potential in mitigating liver fibrosis by reducing fibrosis markers, abnormal cell proliferation, and improving mitochondrial function. These findings suggest potential therapeutic strategies for liver fibrosis.
EXPERIMENTAL PERSPECTIVE ON NAFLD
- Over recent decades, the world has observed a marked rise in obesity rates, leading to an increase in conditions like T2DM and its consequential complications, notably NAFLD. Contemporary research has illuminated the deep interrelationships between NAFLD and other significant health conditions, such as CVD and sarcopenia, highlighting the pressing need for effective NAFLD treatments. Our investigations into its molecular pathways and the pronounced effects of hepatic lipid accumulation have provided invaluable insights into this complex disease. While promising pharmacological options, including Ex-4, DPP-4 inhibitors, and GLP-1RAs (i.e., dulaglutide) have emerged, a significant gap remains in finding drugs with robust therapeutic effects in human clinical trials. An integrated strategy, combining pharmacological methods with lifestyle interventions, stands out as the most promising approach. As our understanding evolves, a comprehensive, integrative approach to managing not only NAFLD but also interrelated conditions like T2DM becomes increasingly crucial. Continued collaborative efforts in this direction are essential for improving patient outcomes worldwide.
CONCLUSIONS
-
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
They were not involved in the review process of this article. Otherwise, there was no conflict of interest.
-
FUNDING
None
NOTES
-
Acknowledgements
- None

| Year | No. of study subjects | BMI, kg/m2 | T2DM without obesity, % | Criteria for obesity, BMI, kg/m2 | Reference |
|---|---|---|---|---|---|
| 1985 | 87 | NA | 67.8 | 115% of SBW | [14] |
| 1988 | 121 | 23.3±2.7 | NA | NA | [15] |
| 1989 | 2,860 | NA | 55.2 | 24.0 | [16] |
| 1989–1990 | 230 | NA | 63.5 | 25.0 | [17] |
| 1991–1992 | 256 | 23.7 | 76.7 | 27.0 | [18] |
| 1993 | 1,541 | 24.2±3.4 | NA | NA | [19] |
| 1990–1995 | 15,665 | NA | 67.7 | 25.0 | [20] |
| 1996 | 749 | 23.8 for male | 62.0 | 25.0 | [21] |
| 24.8 for female | |||||
| 1997–1999 | 353 | 24.8±0.15 | 57.5 | 25.0 | [13] |
| 1999 | 118 | 25.3±2.8 | NA | 25.0 | [22] |
| 2004–2005 | 1,646 | 24.7±3.2 | 57.5 | 25.0 | [23] |
| 2007–2008 | 349 | 25.6±3.2 | NA | 25.0 | [24] |
| 2009–2010 | 1,314 | 25.2±3.2 | 50.2 | 25.0 | [5] |
| 2007–2011 | 245 | 24.5±0.6 | 55.3 | 25.0 | [13] |
| 2015 | 1,314 | 25.2±3.2 | 50.2 | 25.0 | [5] |
| 2016–2018 | NA | NA | 46.8 | 25.0 | [25] |
Values are presented as mean±standard deviation. Adapted from Kim et al. [6].
BMI, body mass index; T2DM, type 2 diabetes mellitus; NA, not available; SBW, standard body weight.
- 1. Defronzo RA. Banting lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus. Diabetes 2009;58:773-95.PubMedPMC
- 2. Park SW, Yun YS, Song YD, Lee HC, Huh KB. Pathogenetic heterogeneity of type 2 diabetes mellitus in Korea. J Korean Diabetes Assoc 1999;23:62-9.
- 3. Yoon KH. Pathogenesis of type 2 diabetes in Korea. Korean Diabetes J 2000;24:397-403.
- 4. Yang YS, Han BD, Han K, Jung JH, Son JW; Taskforce Team of the Obesity Fact Sheet of the Korean Society for the Study of Obesity. Obesity fact sheet in Korea, 2021: trends in obesity prevalence and obesity-related comorbidity incidence stratified by age from 2009 to 2019. J Obes Metab Syndr 2022;31:169-77.ArticlePubMedPMC
- 5. Son JW, Park CY, Kim S, Lee HK, Lee YS; Insulin Resistance as Primary Pathogenesis in Newly Diagnosed, Drug Naïve Type 2 Diabetes Patients in Korea (SURPRISE) Study Group. Changing clinical characteristics according to insulin resistance and insulin secretion in newly diagnosed type 2 diabetic patients in Korea. Diabetes Metab J 2015;39:387-94.ArticlePubMedPMC
- 6. Kim JD, Lee WY. Insulin secretory capacity and insulin resistance in Korean type 2 diabetes mellitus patients. Endocrinol Metab (Seoul) 2016;31:354-60.ArticlePubMedPMCPDF
- 7. Han E, Han KD, Lee YH, Kim KS, Hong S, Park JH, et al. Fatty liver & diabetes statistics in Korea: nationwide data 2009 to 2017. Diabetes Metab J 2023;47:347-55.ArticlePubMedPMCPDF
- 8. Rhee EJ, Park SE, Chang Y, Ryu S, Lee WY. Baseline glycemic status and mortality in 241,499 Korean metropolitan subjects: a Kangbuk Samsung Health Study. Metabolism 2016;65:68-77.ArticlePubMed
- 9. Eslam M, Sanyal AJ, George J; International Consensus Panel. MAFLD: a consensus-driven proposed nomenclature for metabolic associated fatty liver disease. Gastroenterology 2020;158:1999-2014.ArticlePubMed
- 10. Koo DJ, Lee WY. The crosstalk between insulin resistance and nonalcoholic fatty liver disease/metabolic dysfunction-associated fatty liver disease: a culprit or a consequence? Cardiovasc Prev Pharmacother 2022;4:132-41.ArticlePDF
- 11. Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med 2010;363:1341-50.ArticlePubMed
- 12. Bhatia LS, Curzen NP, Calder PC, Byrne CD. Non-alcoholic fatty liver disease: a new and important cardiovascular risk factor? Eur Heart J 2012;33:1190-200.ArticlePubMed
- 13. Yang HK, Lee JH, Choi IY, Kwon HS, Shin JA, Jeong SH, et al. The insulin resistance but not the insulin secretion parameters have changed in the Korean population during the last decade. Diabetes Metab J 2015;39:117-25.ArticlePubMedPMC
- 14. Cho JK, Kim HM, Lim SK, Whang Y, Lee HC, Huh KB. A study on change of body weight non-insulin dependent diabetes mellitus. J Korean Diabetes Assoc 1986;10:89-93.
- 15. Park YS, Shin CS, Kim YS, Kim SY, Cho BY, Lee HK, et al. The etiologic heterogenecity of diabetes mellitus in Korean adults. Korean J Intern Med 1991;40:91-103.
- 16. Song TH, Choi BR, Tak SM, Kang JW, Kim CE, Moon FC, et al. A retrospective study on body weight of diabetes in Korea. J Korean Diabetes Assoc 1990;14:229-33.
- 17. Lee KU, Ryu JS, Kim YT, Shong YK, Kim GS, Lee M, et al. Clinical characteristics of Korean diabetic patients classified by fasting plasma C-peptide level and degree of obesity. Korean J Intern Med 1992;42:315-21.
- 18. Park JY, Kim HK, Kim MS, Park KS, Kim SY, Cho BY, et al. Body weight changes of non-insulin dependent diabetic patients in Korea. J Korean Diabetes Assoc 1993;17:51-8.
- 19. Shin CS, Lee HK, Koh CS, Kim YI, Shin YS, Yoo KY, et al. Risk factors for the development of NIDDM in Yonchon County, Korea. Diabetes Care 1997;20:1842-6.ArticlePubMedPDF
- 20. Lee TH. Prevalence of obesity in Korean non-insulin-dependent diabetic patients. Diabetes Res Clin Pract 1996;32:71-80.ArticlePubMed
- 21. Park JY, Lee KU, Kim CH, Kim HK, Hong SK, Park KS, et al. Past and current obesity in Koreans with non-insulin-dependent diabetes mellitus. Diabetes Res Clin Pract 1997;35:49-56.ArticlePubMed
- 22. Kim DJ, Hahm JR, Jeong IK, Yang TY, Oh EY, Choi YH, et al. Insulin secretion and insulin sensitivity in Korean subjects with impaired glucose intolerance. J Korean Diabetes Assoc 2000;24:356-64.
- 23. Kim DJ, Song KE, Park JW, Cho HK, Lee KW, Huh KB. Clinical characteristics of Korean type 2 diabetic patients in 2005. Diabetes Res Clin Pract 2007;77 Suppl 1:S252-7.ArticlePubMed
- 24. Yoon KH, Shin JA, Kwon HS, Lee SH, Min KW, Ahn YB, et al. Comparison of the efficacy of glimepiride, metformin, and rosiglitazone monotherapy in Korean drug-naïve type 2 diabetic patients: the practical evidence of antidiabetic monotherapy study. Diabetes Metab J 2011;35:26-33.ArticlePubMedPMC
- 25. Jung CH, Son JW, Kang S, Kim WJ, Kim HS, Kim HS, et al. Diabetes fact sheets in Korea, 2020: an appraisal of current status. Diabetes Metab J 2021;45:1-10.ArticlePubMedPMCPDF
- 26. Ryu S, Sung KC, Chang Y, Lee WY, Rhee EJ. Spectrum of insulin sensitivity in the Korean population. Metabolism 2005;54:1644-51.ArticlePubMed
- 27. Lee DY, Rhee EJ, Chang Y, Sohn CI, Shin HC, Ryu S, et al. Impact of systemic inflammation on the relationship between insulin resistance and all-cause and cancer-related mortality. Metabolism 2018;81:52-62.ArticlePubMed
- 28. Shoelson SE, Herrero L, Naaz A. Obesity, inflammation, and insulin resistance. Gastroenterology 2007;132:2169-80.ArticlePubMed
- 29. Miyazaki Y, Glass L, Triplitt C, Wajcberg E, Mandarino LJ, DeFronzo RA. Abdominal fat distribution and peripheral and hepatic insulin resistance in type 2 diabetes mellitus. Am J Physiol Endocrinol Metab 2002;283:E1135-43.ArticlePubMed
- 30. Cnop M, Landchild MJ, Vidal J, Havel PJ, Knowles NG, Carr DR, et al. The concurrent accumulation of intra-abdominal and subcutaneous fat explains the association between insulin resistance and plasma leptin concentrations: distinct metabolic effects of two fat compartments. Diabetes 2002;51:1005-15.PubMed
- 31. Cnop M, Havel PJ, Utzschneider KM, Carr DB, Sinha MK, Boyko EJ, et al. Relationship of adiponectin to body fat distribution, insulin sensitivity and plasma lipoproteins: evidence for independent roles of age and sex. Diabetologia 2003;46:459-69.ArticlePubMedPDF
- 32. Bajaj M, Suraamornkul S, Piper P, Hardies LJ, Glass L, Cersosimo E, et al. Decreased plasma adiponectin concentrations are closely related to hepatic fat content and hepatic insulin resistance in pioglitazone-treated type 2 diabetic patients. J Clin Endocrinol Metab 2004;89:200-6.ArticlePubMed
- 33. Dandona P, Aljada A, Bandyopadhyay A. Inflammation: the link between insulin resistance, obesity and diabetes. Trends Immunol 2004;25:4-7.ArticlePubMed
- 34. Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science 1993;259:87-91.ArticlePubMed
- 35. Dandona P, Weinstock R, Thusu K, Abdel-Rahman E, Aljada A, Wadden T. Tumor necrosis factor-alpha in sera of obese patients: fall with weight loss. J Clin Endocrinol Metab 1998;83:2907-10.PubMed
- 36. Mohamed-Ali V, Goodrick S, Rawesh A, Katz DR, Miles JM, Yudkin JS, et al. Subcutaneous adipose tissue releases interleukin-6, but not tumor necrosis factor-alpha, in vivo. J Clin Endocrinol Metab 1997;82:4196-200.PubMed
- 37. Kubaszek A, Pihlajamaki J, Komarovski V, Lindi V, Lindstrom J, Eriksson J, et al. Promoter polymorphisms of the TNF-alpha (G-308A) and IL-6 (C-174G) genes predict the conversion from impaired glucose tolerance to type 2 diabetes: the Finnish Diabetes Prevention Study. Diabetes 2003;52:1872-6.PubMed
- 38. Ozcan U, Cao Q, Yilmaz E, Lee AH, Iwakoshi NN, Ozdelen E, et al. Endoplasmic reticulum stress links obesity, insulin action, and type 2 diabetes. Science 2004;306:457-61.ArticlePubMed
- 39. Furukawa S, Fujita T, Shimabukuro M, Iwaki M, Yamada Y, Nakajima Y, et al. Increased oxidative stress in obesity and its impact on metabolic syndrome. J Clin Invest 2004;114:1752-61.ArticlePubMedPMC
- 40. Summers SA. Ceramides in insulin resistance and lipotoxicity. Prog Lipid Res 2006;45:42-72.ArticlePubMed
- 41. Shoelson SE, Lee J, Goldfine AB. Inflammation and insulin resistance. J Clin Invest 2006;116:1793-801.ArticlePubMedPMC
- 42. Hirosumi J, Tuncman G, Chang L, Gorgun CZ, Uysal KT, Maeda K, et al. A central role for JNK in obesity and insulin resistance. Nature 2002;420:333-6.ArticlePubMedPDF
- 43. Barnes PJ, Karin M. Nuclear factor-kappaB: a pivotal transcription factor in chronic inflammatory diseases. N Engl J Med 1997;336:1066-71.ArticlePubMed
- 44. Seppala-Lindroos A, Vehkavaara S, Hakkinen AM, Goto T, Westerbacka J, Sovijarvi A, et al. Fat accumulation in the liver is associated with defects in insulin suppression of glucose production and serum free fatty acids independent of obesity in normal men. J Clin Endocrinol Metab 2002;87:3023-8.ArticlePubMed
- 45. Kelley DE, McKolanis TM, Hegazi RA, Kuller LH, Kalhan SC. Fatty liver in type 2 diabetes mellitus: relation to regional adiposity, fatty acids, and insulin resistance. Am J Physiol Endocrinol Metab 2003;285:E906-16.ArticlePubMed
- 46. Rhee EJ, Lee WY, Cho YK, Kim BI, Sung KC. Hyperinsulinemia and the development of nonalcoholic fatty liver disease in nondiabetic adults. Am J Med 2011;124:69-76.ArticlePubMed
- 47. Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol 2013;10:330-44.ArticlePubMedPDF
- 48. Birkenfeld AL, Shulman GI. Nonalcoholic fatty liver disease, hepatic insulin resistance, and type 2 diabetes. Hepatology 2014;59:713-23.ArticlePubMed
- 49. Donnelly KL, Smith CI, Schwarzenberg SJ, Jessurun J, Boldt MD, Parks EJ. Sources of fatty acids stored in liver and secreted via lipoproteins in patients with nonalcoholic fatty liver disease. J Clin Invest 2005;115:1343-51.ArticlePubMedPMC
- 50. Roden M. Mechanisms of disease: hepatic steatosis in type 2 diabetes. Pathogenesis and clinical relevance. Nat Clin Pract Endocrinol Metab 2006;2:335-48.ArticlePubMedPDF
- 51. Shimano H, Horton JD, Shimomura I, Hammer RE, Brown MS, Goldstein JL. Isoform 1c of sterol regulatory element binding protein is less active than isoform 1a in livers of transgenic mice and in cultured cells. J Clin Invest 1997;99:846-54.ArticlePubMedPMC
- 52. Yahagi N, Shimano H, Hasty AH, Matsuzaka T, Ide T, Yoshikawa T, et al. Absence of sterol regulatory element-binding protein-1 (SREBP-1) ameliorates fatty livers but not obesity or insulin resistance in Lep(ob)/Lep(ob) mice. J Biol Chem 2002;277:19353-7.PubMed
- 53. Tamura S, Shimomura I. Contribution of adipose tissue and de novo lipogenesis to nonalcoholic fatty liver disease. J Clin Invest 2005;115:1139-42.ArticlePubMedPMC
- 54. Wolfrum C, Asilmaz E, Luca E, Friedman JM, Stoffel M. Foxa2 regulates lipid metabolism and ketogenesis in the liver during fasting and in diabetes. Nature 2004;432:1027-32.ArticlePubMedPDF
- 55. Koliaki C, Szendroedi J, Kaul K, Jelenik T, Nowotny P, Jankowiak F, et al. Adaptation of hepatic mitochondrial function in humans with non-alcoholic fatty liver is lost in steatohepatitis. Cell Metab 2015;21:739-46.ArticlePubMed
- 56. Yamaguchi K, Yang L, McCall S, Huang J, Yu XX, Pandey SK, et al. Inhibiting triglyceride synthesis improves hepatic steatosis but exacerbates liver damage and fibrosis in obese mice with nonalcoholic steatohepatitis. Hepatology 2007;45:1366-74.ArticlePubMed
- 57. Hebbard L, George J. Animal models of nonalcoholic fatty liver disease. Nat Rev Gastroenterol Hepatol 2011;8:35-44.ArticlePubMedPDF
- 58. Gruben N, Shiri-Sverdlov R, Koonen DP, Hofker MH. Nonalcoholic fatty liver disease: a main driver of insulin resistance or a dangerous liaison? Biochim Biophys Acta 2014;1842:2329-43.ArticlePubMed
- 59. Lam TK, Carpentier A, Lewis GF, van de Werve G, Fantus IG, Giacca A. Mechanisms of the free fatty acid-induced increase in hepatic glucose production. Am J Physiol Endocrinol Metab 2003;284:E863-73.ArticlePubMed
- 60. Gao Z, Zhang X, Zuberi A, Hwang D, Quon MJ, Lefevre M, et al. Inhibition of insulin sensitivity by free fatty acids requires activation of multiple serine kinases in 3T3-L1 adipocytes. Mol Endocrinol 2004;18:2024-34.ArticlePubMed
- 61. Lee JY, Sohn KH, Rhee SH, Hwang D. Saturated fatty acids, but not unsaturated fatty acids, induce the expression of cyclooxygenase-2 mediated through Toll-like receptor 4. J Biol Chem 2001;276:16683-9.ArticlePubMed
- 62. Shi H, Kokoeva MV, Inouye K, Tzameli I, Yin H, Flier JS. TLR4 links innate immunity and fatty acid-induced insulin resistance. J Clin Invest 2006;116:3015-25.ArticlePubMedPMC
- 63. Knebel B, Haas J, Hartwig S, Jacob S, Kollmer C, Nitzgen U, et al. Liver-specific expression of transcriptionally active SREBP-1c is associated with fatty liver and increased visceral fat mass. PLoS One 2012;7:e31812.ArticlePubMedPMC
- 64. Ibdah JA, Perlegas P, Zhao Y, Angdisen J, Borgerink H, Shadoan MK, et al. Mice heterozygous for a defect in mitochondrial trifunctional protein develop hepatic steatosis and insulin resistance. Gastroenterology 2005;128:1381-90.ArticlePubMed
- 65. Palma R, Pronio A, Romeo M, Scognamiglio F, Ventriglia L, Ormando VM, et al. The role of insulin resistance in fueling NAFLD pathogenesis: from molecular mechanisms to clinical implications. J Clin Med 2022;11:3649.ArticlePubMedPMC
- 66. Scorletti E, Carr RM. A new perspective on NAFLD: focusing on lipid droplets. J Hepatol 2022;76:934-45.ArticlePubMed
- 67. Jung CH, Rhee EJ, Kwon H, Chang Y, Ryu S, Lee WY. Visceral-to-subcutaneous abdominal fat ratio is associated with nonalcoholic fatty liver disease and liver fibrosis. Endocrinol Metab (Seoul) 2020;35:165-76.ArticlePubMedPMCPDF
- 68. Jung I, Koo DJ, Lee MY, Moon SJ, Kwon H, Park SE, et al. Increased risk of nonalcoholic fatty liver disease in individuals with high weight variability. Endocrinol Metab (Seoul) 2021;36:845-54.ArticlePubMedPMCPDF
- 69. Xu L, Li D. Body-weight fluctuations and outcomes in coronary disease. N Engl J Med 2017;377:94.Article
- 70. Gaggini M, Morelli M, Buzzigoli E, DeFronzo RA, Bugianesi E, Gastaldelli A. Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease. Nutrients 2013;5:1544-60.ArticlePubMedPMC
- 71. Bedogni G, Miglioli L, Masutti F, Tiribelli C, Marchesini G, Bellentani S. Prevalence of and risk factors for nonalcoholic fatty liver disease: the Dionysos nutrition and liver study. Hepatology 2005;42:44-52.ArticlePubMed
- 72. Sorrentino P, Terracciano L, D’Angelo S, Ferbo U, Bracigliano A, Vecchione R. Predicting fibrosis worsening in obese patients with NASH through parenchymal fibronectin, HOMA-IR, and hypertension. Am J Gastroenterol 2010;105:336-44.ArticlePubMedPDF
- 73. Pais R, Charlotte F, Fedchuk L, Bedossa P, Lebray P, Poynard T, et al. A systematic review of follow-up biopsies reveals disease progression in patients with non-alcoholic fatty liver. J Hepatol 2013;59:550-6.ArticlePubMed
- 74. Gomez de la Cuesta S, Aller de la Fuente R, Tafur Sanchez C, Izaola O, Garcia Sanchez C, Mora N, et al. Analytical, anthropometric and dietary factors associated with the development of fibrosis in patients with nonalcoholic fatty liver disease. Rev Esp Enferm Dig 2018;110:292-8.PubMed
- 75. McPherson S, Hardy T, Henderson E, Burt AD, Day CP, Anstee QM. Evidence of NAFLD progression from steatosis to fibrosing-steatohepatitis using paired biopsies: implications for prognosis and clinical management. J Hepatol 2015;62:1148-55.ArticlePubMed
- 76. Bae JC, Beste LA, Utzschneider KM. The impact of insulin resistance on hepatic fibrosis among United States adults with non-alcoholic fatty liver disease: NHANES 2017 to 2018. Endocrinol Metab (Seoul) 2022;37:455-65.ArticlePubMedPMCPDF
- 77. Koo DJ, Lee MY, Jung I, Moon SJ, Kwon H, Park SE, et al. Baseline homeostasis model assessment of insulin resistance associated with fibrosis progression in patients with nonalcoholic fatty liver disease without diabetes: a cohort study. PLoS One 2021;16:e0255535.ArticlePubMedPMC
- 78. Koo DJ, Lee MY, Jung I, Moon SJ, Kwon H, Park SE, et al. Changes in insulin resistance index and the risk of liver fibrosis in patients with nonalcoholic fatty liver disease without diabetes: Kangbuk Samsung Health Study. Endocrinol Metab (Seoul) 2021;36:1016-28.ArticlePubMedPMCPDF
- 79. Lee JI, Kim MC, Moon BS, Song YS, Han EN, Lee HS, et al. The relationship between 10-year cardiovascular risk calculated using the pooled cohort equation and the severity of nonalcoholic fatty liver disease. Endocrinol Metab (Seoul) 2016;31:86-92.ArticlePubMedPMCPDF
- 80. Lee MK, Rhee EJ, Kim MC, Moon BS, Lee JI, Song YS, et al. Metabolic health is more important than obesity in the development of nonalcoholic fatty liver disease: a 4-year retrospective study. Endocrinol Metab (Seoul) 2015;30:522-30.ArticlePubMedPMC
- 81. Jeon WS, Park SE, Rhee EJ, Park CY, Oh KW, Park SW, et al. Association of serum adipocyte-specific fatty acid binding protein with fatty liver index as a predictive indicator of nonalcoholic fatty liver disease. Endocrinol Metab (Seoul) 2013;28:283-7.ArticlePubMedPMC
- 82. Seo YY, Cho YK, Bae JC, Seo MH, Park SE, Rhee EJ, et al. Tumor necrosis factor-α as a predictor for the development of nonalcoholic fatty liver disease: a 4-year follow-up study. Endocrinol Metab (Seoul) 2013;28:41-5.ArticlePubMedPMC
- 83. Jung I, Lee DY, Lee MY, Kwon H, Rhee EJ, Park CY, et al. Autonomic imbalance increases the risk for non-alcoholic fatty liver disease. Front Endocrinol (Lausanne) 2021;12:752944.ArticlePubMedPMC
- 84. Lee YH, Bang H, Park YM, Bae JC, Lee BW, Kang ES, et al. Non-laboratory-based self-assessment screening score for non-alcoholic fatty liver disease: development, validation and comparison with other scores. PLoS One 2014;9:e107584.ArticlePubMedPMC
- 85. Koo DJ, Lee MY, Jung I, Moon SJ, Kwon H, Rhee EJ, et al. Increased risk of NAFLD in adults with glomerular hyperfiltration: an 8-year cohort study based on 147,162 Koreans. J Pers Med 2022;12:1142.ArticlePubMedPMC
- 86. Kim HM, Lee YH. The leg fat to total fat ratio is associated with lower risks of non-alcoholic fatty liver disease and less severe hepatic fibrosis: results from nationwide surveys (KNHANES 2008-2011). Endocrinol Metab (Seoul) 2021;36:1232-42.ArticlePubMedPMCPDF
- 87. Lee CH, Seto WK, Ieong K, Lui DT, Fong CH, Wan HY, et al. Development of a non-invasive liver fibrosis score based on transient elastography for risk stratification in patients with type 2 diabetes. Endocrinol Metab (Seoul) 2021;36:134-45.ArticlePubMedPMCPDF
- 88. Cho Y, Lee YH. State-of-the-art overview of the pharmacological treatment of non-alcoholic steatohepatitis. Endocrinol Metab (Seoul) 2022;37:38-52.ArticlePubMedPMCPDF
- 89. Lee MJ, Kim EH, Bae SJ, Kim GA, Park SW, Choe J, et al. Age-related decrease in skeletal muscle mass is an independent risk factor for incident nonalcoholic fatty liver disease: a 10-year retrospective cohort study. Gut Liver 2019;13:67-76.ArticlePubMed
- 90. Eslam M, Sarin SK, Wong VW, Fan JG, Kawaguchi T, Ahn SH, et al. The Asian Pacific Association for the Study of the Liver clinical practice guidelines for the diagnosis and management of metabolic associated fatty liver disease. Hepatol Int 2020;14:889-919.ArticlePubMedPDF
- 91. Bae JC, Suh S, Park SE, Rhee EJ, Park CY, Oh KW, et al. Regular exercise is associated with a reduction in the risk of NAFLD and decreased liver enzymes in individuals with NAFLD independent of obesity in Korean adults. PLoS One 2012;7:e46819.ArticlePubMedPMC
- 92. Lee BW, Lee YH, Park CY, Rhee EJ, Lee WY, Kim NH, et al. Non-alcoholic fatty liver disease in patients with type 2 diabetes mellitus: a position statement of the Fatty Liver Research Group of the Korean Diabetes Association. Diabetes Metab J 2020;44:382-401.ArticlePubMedPMCPDF
- 93. Andre P, Balkau B, Born C, Charles MA, Eschwege E; D.E.S.I.R. study group. Three-year increase of gamma-glutamyltransferase level and development of type 2 diabetes in middle-aged men and women: the D.E.S.I.R. cohort. Diabetologia 2006;49:2599-603.ArticlePubMedPMCPDF
- 94. Kim CH, Park JY, Lee KU, Kim JH, Kim HK. Association of serum gamma-glutamyltransferase and alanine aminotransferase activities with risk of type 2 diabetes mellitus independent of fatty liver. Diabetes Metab Res Rev 2009;25:64-9.PubMed
- 95. Ko SH, Baeg MK, Han KD, Ko SH, Ahn YB. Increased liver markers are associated with higher risk of type 2 diabetes. World J Gastroenterol 2015;21:7478-87.ArticlePubMedPMC
- 96. Ballestri S, Zona S, Targher G, Romagnoli D, Baldelli E, Nascimbeni F, et al. Nonalcoholic fatty liver disease is associated with an almost twofold increased risk of incident type 2 diabetes and metabolic syndrome. Evidence from a systematic review and meta-analysis. J Gastroenterol Hepatol 2016;31:936-44.ArticlePubMedPDF
- 97. Ekstedt M, Franzen LE, Mathiesen UL, Thorelius L, Holmqvist M, Bodemar G, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology 2006;44:865-73.ArticlePubMed
- 98. Bae JC, Cho YK, Lee WY, Seo HI, Rhee EJ, Park SE, et al. Impact of nonalcoholic fatty liver disease on insulin resistance in relation to HbA1c levels in nondiabetic subjects. Am J Gastroenterol 2010;105:2389-95.ArticlePubMedPDF
- 99. Bae JC, Rhee EJ, Lee WY, Park SE, Park CY, Oh KW, et al. Combined effect of nonalcoholic fatty liver disease and impaired fasting glucose on the development of type 2 diabetes: a 4-year retrospective longitudinal study. Diabetes Care 2011;34:727-9.PubMedPMC
- 100. Bae JC, Han JM, Cho JH, Kwon H, Park SE, Park CY, et al. The persistence of fatty liver has a differential impact on the development of diabetes: the Kangbuk Samsung Health Study. Diabetes Res Clin Pract 2018;135:1-6.ArticlePubMed
- 101. Bae JC, Kim SK, Han JM, Kwon S, Lee DY, Kim J, et al. Additive effect of non-alcoholic fatty liver disease on the development of diabetes in individuals with metabolic syndrome. Diabetes Res Clin Pract 2017;129:136-43.ArticlePubMed
- 102. Choi JH, Rhee EJ, Bae JC, Park SE, Park CY, Cho YK, et al. Increased risk of type 2 diabetes in subjects with both elevated liver enzymes and ultrasonographically diagnosed nonalcoholic fatty liver disease: a 4-year longitudinal study. Arch Med Res 2013;44:115-20.ArticlePubMed
- 103. Chung SM, Kang MK, Moon JS, Park JG. Performance of simple fibrosis score in non-alcoholic fatty liver disease with and without type 2 diabetes. Endocrinol Metab (Seoul) 2023;38:277-81.ArticlePubMedPMCPDF
- 104. Kim J, Lee M, Kim SY, Kim JH, Nam JS, Chun SW, et al. Nonlaboratory-based simple screening model for nonalcoholic fatty liver disease in patients with type 2 diabetes developed using multi-center cohorts. Endocrinol Metab (Seoul) 2021;36:823-34.ArticlePubMedPMCPDF
- 105. Barb D, Repetto EM, Stokes ME, Shankar SS, Cusi K. Type 2 diabetes mellitus increases the risk of hepatic fibrosis in individuals with obesity and nonalcoholic fatty liver disease. Obesity (Silver Spring) 2021;29:1950-60.ArticlePubMedPMCPDF
- 106. ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 4. Comprehensive medical evaluation and assessment of comorbidities: standards of care in diabetes: 2023. Diabetes Care 2023;46(Suppl 1):S49-67.PubMed
- 107. Dyson J, Jaques B, Chattopadyhay D, Lochan R, Graham J, Das D, et al. Hepatocellular cancer: the impact of obesity, type 2 diabetes and a multidisciplinary team. J Hepatol 2014;60:110-7.ArticlePubMed
- 108. Ranjbar G, Mikhailidis DP, Sahebkar A. Effects of newer antidiabetic drugs on nonalcoholic fatty liver and steatohepatitis: think out of the box! Metabolism 2019;101:154001.ArticlePubMed
- 109. Dougherty JA, Guirguis E, Thornby KA. A systematic review of newer antidiabetic agents in the treatment of nonalcoholic fatty liver disease. Ann Pharmacother 2021;55:65-79.ArticlePubMedPDF
- 110. Bae JC. DPP-4 inhibitor in type 2 diabetes mellitus patient with non-alcoholic fatty liver disease: achieving two goals at once? Endocrinol Metab (Seoul) 2022;37:858-60.ArticlePubMedPMCPDF
- 111. Bae JC, Lee WY, Yoon KH, Park JY, Son HS, Han KA, et al. Improvement of nonalcoholic fatty liver disease with carnitineorotate complex in type 2 diabetes (CORONA): a randomized controlled trial. Diabetes Care 2015;38:1245-52.ArticlePubMedPDF
- 112. Lee J, Hong SW, Chae SW, Kim DH, Choi JH, Bae JC, et al. Exendin-4 improves steatohepatitis by increasing Sirt1 expression in high-fat diet-induced obese C57BL/6J mice. PLoS One 2012;7:e31394.ArticlePubMedPMC
- 113. Lee J, Hong SW, Park SE, Rhee EJ, Park CY, Oh KW, et al. Exendin-4 attenuates endoplasmic reticulum stress through a SIRT1-dependent mechanism. Cell Stress Chaperones 2014;19:649-56.ArticlePubMedPMCPDF
- 114. Lee J, Hong SW, Park SE, Rhee EJ, Park CY, Oh KW, et al. Exendin-4 regulates lipid metabolism and fibroblast growth factor 21 in hepatic steatosis. Metabolism 2014;63:1041-8.ArticlePubMed
- 115. Lee J, Hong SW, Park SE, Rhee EJ, Park CY, Oh KW, et al. Exendin-4 inhibits the expression of SEPP1 and fetuin-A via improvement of palmitic acid-induced endoplasmic reticulum stress by AMPK. Endocrinol Metab (Seoul) 2015;30:177-84.ArticlePubMedPMC
- 116. Lee J, Hong SW, Kim MJ, Moon SJ, Kwon H, Park SE, et al. Dulaglutide ameliorates palmitic acid-induced hepatic steatosis by activating FAM3A signaling pathway. Endocrinol Metab (Seoul) 2022;37:74-83.ArticlePubMedPMCPDF
- 117. Lee Y, Kim BR, Kang GH, Lee GJ, Park YJ, Kim H, et al. The effects of PPAR agonists on atherosclerosis and nonalcoholic fatty liver disease in ApoE-/-FXR-/- mice. Endocrinol Metab (Seoul) 2021;36:1243-53.ArticlePubMedPMCPDF
- 118. Nguyen G, Park SY, Do DV, Choi DH, Cho EH. Gemigliptin alleviates succinate-induced hepatic stellate cell activation by ameliorating mitochondrial dysfunction. Endocrinol Metab (Seoul) 2022;37:918-28.ArticlePubMedPMCPDF
REFERENCES
Figure & Data
References
Citations

- Figure
- Related articles
-
- Comparison of Insulin-Treated Patients with Ambiguous Diabetes Type with Definite Type 1 and Type 2 Diabetes Mellitus Subjects: A Clinical Perspective
- Serum Retinol-Binding Protein Levels Are Associated with Nonalcoholic Fatty Liver Disease in Chinese Patients with Type 2 Diabetes Mellitus: A Real-World Study

 KDA
KDA
 PubReader
PubReader ePub Link
ePub Link Cite
Cite