
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Drug/Regimen
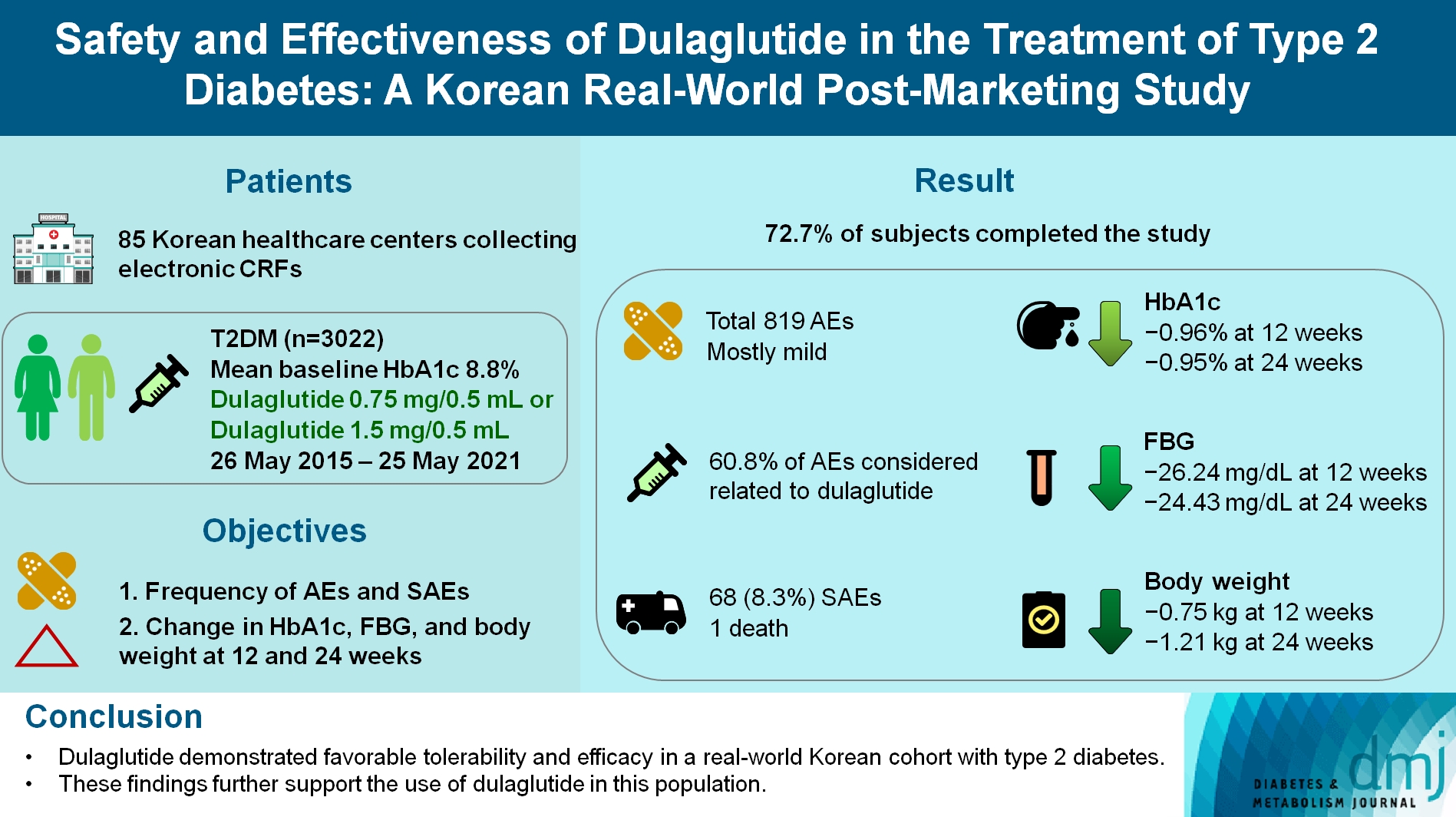
- Safety and Effectiveness of Dulaglutide in the Treatment of Type 2 Diabetes Mellitus: A Korean Real-World Post-Marketing Study
- Jeonghee Han, Woo Je Lee, Kyu Yeon Hur, Jae Hyoung Cho, Byung Wan Lee, Cheol-Young Park
- Received February 3, 2023 Accepted July 10, 2023 Published online February 2, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0030 [Epub ahead of print]
- 667 View
- 56 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader - Background
To investigate the real-world safety and effectiveness of dulaglutide in Korean adults with type 2 diabetes mellitus (T2DM).
Methods
This was a real-world, prospective, non-interventional post-marketing safety study conducted from May 26, 2015 to May 25, 2021 at 85 Korean healthcare centers using electronic case data. Data on patients using dulaglutide 0.75 mg/0.5 mL or the dulaglutide 1.5 mg/0.5 mL single-use pens were collected and pooled. The primary objective was to report the frequency and proportion of adverse and serious adverse events that occurred. The secondary objective was to monitor the effectiveness of dulaglutide at 12 and 24 weeks by evaluating changes in glycosylated hemoglobin (HbA1c ), fasting plasma glucose, and body weight.
Results
Data were collected from 3,067 subjects, and 3,022 subjects who received ≥1 dose (of any strength) of dulaglutide were included in the safety analysis set (53% female, mean age 56 years; diabetes duration 11.2 years, mean HbA1c 8.8%). The number of adverse events reported was 819; of these, 68 (8.3%) were serious adverse events. One death was reported. Adverse events were mostly mild in severity; 60.81% of adverse events were considered related to dulaglutide. This study was completed by 72.73% (2,198/3,022) of subjects. At 12/24 weeks there were significant (P<0.0001) reductions from baseline in least-squares mean HbA1c (0.96%/0.95%), fasting blood glucose (26.24/24.43 mg/dL), and body weight (0.75/1.21 kg).
Conclusion
Dulaglutide was generally well tolerated and effective in real-world Korean individuals with T2DM. The results from this study contribute to the body of evidence for dulaglutide use in this population.
- Metabolic Risk/Epidemiology
- Plasma CD36 and Incident Diabetes: A Case-Cohort Study in Danish Men and Women
- Yeli Wang, Jingwen Zhu, Sarah Aroner, Kim Overvad, Tianxi Cai, Ming Yang, Anne Tjønneland, Aase Handberg, Majken K. Jensen
- Diabetes Metab J. 2020;44(1):134-142. Published online October 18, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0273
- 4,346 View
- 70 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Membrane CD36 is a fatty acid transporter implicated in the pathogenesis of metabolic disease. We aimed to evaluate the association between plasma CD36 levels and diabetes risk and to examine if the association was independent of adiposity among Danish population.
Methods We conducted a case-cohort study nested within the Danish Diet, Cancer and Health study among participants free of cardiovascular disease, diabetes and cancer and with blood samples and anthropometric measurements (height, weight, waist circumference, and body fat percentage) at baseline (1993 to 1997). CD36 levels were measured in 647 incident diabetes cases that occurred before December 2011 and a total of 3,515 case-cohort participants (236 cases overlap).
Results Higher plasma CD36 levels were associated with higher diabetes risk after adjusting for age, sex and other lifestyle factors. The hazard ratio (HR) comparing high versus low tertile of plasma CD36 levels was 1.36 (95% confidence interval [CI], 1.00 to 1.86). However, the association lost its significance after further adjustment for different adiposity indices such as body mass index (HR, 1.23; 95% CI, 0.87 to 1.73), waist circumference (HR, 1.21; 95% CI, 0.88 to 1.68) or body fat percentage (HR, 1.20; 95% CI, 0.86 to 1.66). Moreover, raised plasma CD36 levels were moderately associated with diabetes risk among lean participants, but the association was not present among overweight/obese individuals.
Conclusion Higher plasma CD36 levels were associated with higher diabetes risk, but the association was not independent of adiposity. In this Danish population, the association of CD36 with diabetes risk could be either mediated or confounded by adiposity.
-
Citations
Citations to this article as recorded by- The Multifunctionality of CD36 in Diabetes Mellitus and Its Complications—Update in Pathogenesis, Treatment and Monitoring
Kamila Puchałowicz, Monika Ewa Rać
Cells.2020; 9(8): 1877. CrossRef - The Role of CD36 in Type 2 Diabetes Mellitus: β-Cell Dysfunction and Beyond
Jun Sung Moon, Udayakumar Karunakaran, Elumalai Suma, Seung Min Chung, Kyu Chang Won
Diabetes & Metabolism Journal.2020; 44(2): 222. CrossRef
- The Multifunctionality of CD36 in Diabetes Mellitus and Its Complications—Update in Pathogenesis, Treatment and Monitoring
- Obesity and Metabolic Syndrome
- Increased Serum Angiopoietin-Like 6 Ahead of Metabolic Syndrome in a Prospective Cohort Study
- Jun Namkung, Joon Hyung Sohn, Jae Seung Chang, Sang-Wook Park, Jang-Young Kim, Sang-Baek Koh, In Deok Kong, Kyu-Sang Park
- Diabetes Metab J. 2019;43(4):521-529. Published online March 29, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0080
- 4,836 View
- 51 Download
- 15 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Despite being an anti-obesity hepatokine, the levels of serum angiopoietin-like 6 (ANGPTL6) are elevated in various metabolic diseases. Thus, ANGPTL6 expression may reflect metabolic burden and may have compensatory roles. This study investigated the association between serum ANGPTL6 levels and new-onset metabolic syndrome.
Methods In total, 221 participants without metabolic syndrome were randomly selected from a rural cohort in Korea. Baseline serum ANGPTL6 levels were measured using an enzyme-linked immunosorbent assay. Anthropometric and biochemical markers were analyzed before and after follow-up examinations.
Results During an average follow-up period of 2.75 (interquartile range, 0.76) years, 82 participants (37.1%) presented new-onset metabolic syndrome and had higher ANGPTL6 levels before onset than those without metabolic syndrome (48.03±18.84 ng/mL vs. 64.75±43.35 ng/mL,
P =0.001). In the multivariable adjusted models, the odds ratio for the development of metabolic syndrome in the highest quartile of ANGPTL6 levels was 3.61 (95% confidence interval, 1.27 to 10.26). The use of ANGPTL6 levels in addition to the conventional components improved the prediction of new-onset metabolic syndrome (area under the receiver operating characteristic curve: 0.775 vs. 0.807,P =0.036).Conclusion Increased serum ANGPTL6 levels precede the development of metabolic syndrome and its components, including low high density lipoprotein, high triglyceride, and high glucose levels, which have an independent predictive value for metabolic syndrome.
-
Citations
Citations to this article as recorded by- Angiopoietin-Like Proteins: Cardiovascular Biology and Therapeutic Targeting for the Prevention of Cardiovascular Diseases
Eric Thorin, Pauline Labbé, Mélanie Lambert, Pauline Mury, Olina Dagher, Géraldine Miquel, Nathalie Thorin-Trescases
Canadian Journal of Cardiology.2023; 39(12): 1736. CrossRef - Hyperlipidemia and hypothyroidism
Xin Su, Hua Peng, Xiang Chen, Xijie Wu, Bin Wang
Clinica Chimica Acta.2022; 527: 61. CrossRef - Multidimensional Biomarker Analysis Including Mitochondrial Stress Indicators for Nonalcoholic Fatty Liver Disease
Eunha Chang, Jae Seung Chang, In Deok Kong, Soon Koo Baik, Moon Young Kim, Kyu-Sang Park
Gut and Liver.2022; 16(2): 171. CrossRef - Triglyceride and Triglyceride-Rich Lipoproteins in Atherosclerosis
Bai-Hui Zhang, Fan Yin, Ya-Nan Qiao, Shou-Dong Guo
Frontiers in Molecular Biosciences.2022;[Epub] CrossRef - Relationship of ANGPTL6 With Neonatal Glucose Homeostasis and Fat Mass Is Disrupted in Gestational Diabetic Pregnancies
Abel Valencia-Martínez, Ute Schaefer-Graf, Encarnación Amusquivar, Emilio Herrera, Henar Ortega-Senovilla
The Journal of Clinical Endocrinology & Metabolism.2022; 107(10): e4078. CrossRef - Update on dyslipidemia in hypothyroidism: the mechanism of dyslipidemia in hypothyroidism
Huixing Liu, Daoquan Peng
Endocrine Connections.2022;[Epub] CrossRef - RETRACTED ARTICLE: Relationship between the development of hyperlipidemia in hypothyroidism patients
Xin Su, Xiang Chen, Bin Wang
Molecular Biology Reports.2022; 49(11): 11025. CrossRef - Effects of Exercise Intervention on Mitochondrial Stress Biomarkers in Metabolic Syndrome Patients: A Randomized Controlled Trial
Jae Seung Chang, Jun Namkung
International Journal of Environmental Research and Public Health.2021; 18(5): 2242. CrossRef - Angiopoietin-like proteins in atherosclerosis
Yi-Zhang Liu, Chi Zhang, Jie-Feng Jiang, Zhe-Bin Cheng, Zheng-Yang Zhou, Mu-Yao Tang, Jia-Xiang Sun, Liang Huang
Clinica Chimica Acta.2021; 521: 19. CrossRef - Effects of Bariatric Surgeries on Fetuin-A, Selenoprotein P, Angiopoietin-Like Protein 6, and Fibroblast Growth Factor 21 Concentration
Jakub Poloczek, Wojciech Kazura, Ewa Kwaśnicka, Janusz Gumprecht, Jerzy Jochem, Dominika Stygar, Munmun Chattopadhyay
Journal of Diabetes Research.2021; 2021: 1. CrossRef - Hepatokines and Non-Alcoholic Fatty Liver Disease: Linking Liver Pathophysiology to Metabolism
Tae Hyun Kim, Dong-Gyun Hong, Yoon Mee Yang
Biomedicines.2021; 9(12): 1903. CrossRef - Serum levels of angiopoietin-related growth factor in diabetes mellitus and chronic hemodialysis
Semra ÖZKAN ÖZTÜRK, Hilmi ATASEVEN
Cumhuriyet Medical Journal.2021;[Epub] CrossRef - ANGPTL6 Level in Patient with Coronary Heart Disease and Its Relationship with the Severity of Coronary Artery Lesions
蕾 任
Advances in Clinical Medicine.2020; 10(05): 714. CrossRef - Investigating the Role of Myeloperoxidase and Angiopoietin-like Protein 6 in Obesity and Diabetes
Mohammad G. Qaddoumi, Muath Alanbaei, Maha M. Hammad, Irina Al Khairi, Preethi Cherian, Arshad Channanath, Thangavel Alphonse Thanaraj, Fahd Al-Mulla, Mohamed Abu-Farha, Jehad Abubaker
Scientific Reports.2020;[Epub] CrossRef - Letter: Increased Serum Angiopoietin-Like 6 Ahead of Metabolic Syndrome in a Prospective Cohort Study (Diabetes Metab J 2019;43:521-9)
Jin Hwa Kim
Diabetes & Metabolism Journal.2019; 43(5): 727. CrossRef - Response: Increased Serum Angiopoietin-Like 6 Ahead of Metabolic Syndrome in a Prospective Cohort Study (Diabetes Metab J 2019;43:521-9)
Jun Namkung, Kyu-Sang Park
Diabetes & Metabolism Journal.2019; 43(5): 729. CrossRef
- Angiopoietin-Like Proteins: Cardiovascular Biology and Therapeutic Targeting for the Prevention of Cardiovascular Diseases

 KDA
KDA
 First
First Prev
Prev





