Ubiquitous Diabetes Management System via Interactive Communication Based on Information Technologies: Clinical Effects and Perspectives
Article information
Abstract
New diabetes management systems based on interactive communication have been introduced recently, accompanying rapid advances in information technology; these systems are referred to as "ubiquitous diabetes management systems." In such ubiquitous systems, patients and medical teams can communicate via Internet or telecommunications, with patients uploading their glucose data and personal information, and medical teams sending optimal feedback. Clinical evidence from both long-term and short-term trials has been reported by some researchers. Such systems appear to be effective not only in reducing the levels of HbA1c but also in stabilizing glucose control. However, most notably, evidence for the cost-effectiveness of such a system should be demonstrated before it can be propagated out to the general population in actual clinical practice. To establish a cost-effective model, various types of clinical decision supporting software designed to reduce the labor time of physicians must first be developed. A number of sensors and devices for monitoring patients' data are expected to be available in the near future; thus, methods for automatic interconnections between devices and web charts were also developed. Further investigations to demonstrate the clinical outcomes of such a system should be conducted, hopefully leading to a new paradigm of diabetes management.
INTRODUCTION
Currently, the number of subjects with diabetes mellitus, as well as other chronic diseases, is increasing sharply [1,2]. Fortunately, it has been determined that diabetic complications could be prevented via effective glucose control in long-term large-scale prospective trials [3-5]. However, glucose control status with conventional outpatient management remains insufficient to prevent completely all of the related complications. Actually, the proportion of subjects with the target HbA1c level (< 7%) was approximately 36% in the USA [6], 31% in Europe (target HbA1c < 6.5%) [7] and 21% in Asia (target HbA1c < 7%) [8]. Additionally, the economic burden resulting from diabetic complications is expected to be enormous, with both the rapid increase in the numbers of diabetic patients and the failure of the glucose control status to reach the target range. We currently require a new type of diabetes management with both effective glucose control and cost-effectiveness. Information technology (IT) is a rapidly growing field with the capacity to substantially strengthen the model of care for diabetes, by providing a framework for the monitoring of patient data in real time and providing frequent optimal feedback to patients. Some of the ways in which IT can improve the model for diabetes care include periodic advice and feedback, continuous motivation for glucose control, frequent encouragement, problem assessment, and individualized diet and exercise education, and drug modification [9]. Such IT-based communication systems have generated clinical evidence regarding glucose control over long-term [9] as well as short-term periods [10]. Moreover, more advanced technologies with real-time image and audio contact via equipment such as digital cameras, video phones, and computers can allow for closer interactions between health workers and individual patients. Thus, many people expect such a system may perform a function in improving records in diabetes management for the general population, and eventually may even constitute a wholly new field of industry. However, for actual application to the general population in real practice worldwide, some significant barriers remain to be surmounted. It is crucially important to demonstrate not only evidence of the clinical effectiveness of such management systems, but also their economic impacts. Such systems should be conveniently and readily accessible to the majority of patients, although they are not familiar with Internet usage. Various types of sensors and devices can be developed and applied to management systems for the status monitoring of a variety of patient types. Most importantly, we must build trust with patients regarding both the efficacy and safety of these systems.
Here, we classify the ubiquitous diabetes management systems and summarize their clinical efficacies. We will demonstrate the economic impact of an Internet-based diabetes management system and introduce some advanced clinical decision supporting systems and patients' data monitoring sensors. Finally, we will discuss some various perspectives on ubiquitous diabetes management systems.
EFFECT OF INTERACTIVE COMMUNICATION SYSTEM
Direct communication between patient and medical team
Internet-based communication system
In past iterations of diabetes management systems, medical teams communicated with patients via direct telephone calls. However, this was inappropriate for large populations, owing to prohibitive economic costs. Frequent and close monitoring of patients' glucose data proved impossible to effect simply by telephone. Recently, the Internet has become a communication tool propagated throughout the world. Internet-based interactive communication systems make possible two-way communication between patients and their physicians via the Internet (Fig. 1A). Options range from utilizing e-mail to independently developing a private homepage to share patients' clinical information [11]. In 2004, we reported a short-term reduction in HbA1c through the effects of an Internet-based glucose monitoring system (IBGMS), in which patients and doctors shared a web-chart online (Fig. 2) [10]. Patients uploaded their glucose data as well as their personal histories, hypoglycemic events, and questions to the remote web server, and their doctors provided advice after interpreting the data [10]. However, because this was effective for HbA1c reduction only for a short-term period of 3 months, we wondered whether it could also provide for effective glucose control over a long-term period. Thus, in 2006, we reported the longest prospective study thus far conducted (30 months) regarding the IBGMS on diabetes, where it was effective in reducing HbA1c and maintaining glucose stability (Fig. 3) [9]. We surmised that such a system was unique in its ability not only to provide periodic advice and feedback, but also to provide continuous motivation for glucose control, frequent encouragement, problem assessment, and individualized education regarding diet, exercise, and drug modification, thereby providing a thorough system for the care of diabetic patients. In 2005, McMahon et al. [12] introduced a web-based care management system and reported its effects on patients with poorly controlled diabetes. The web-based management system was effective for HbA1c reduction over 12 months when compared with education and routine care. The two studies mentioned above [9,12] showed similar results, namely that HbA1c levels were reduced in the majority of participants early in the study; however, the levels of HbA1c rebounded in the patients with poor compliance, whereas the patients with good compliance maintained reduced HbA1c levels. This means that compliance for system use may represent an additional important factor for diabetes management. In addition, such Internet-based interactive systems have been applied to lifestyle modification as well as diabetes control. For example, the Internet has been previously employed as a medium for a weight loss program, to prevent diabetes [13], and as part of a walking program for the treatment of type 2 diabetes patients. The latter had a more significant effect on patients' physical activity and reduction of depressive symptoms than did the conventional method of sharing physical activity information [14]. Additionally, an Internet and mobile phone intervention was found to improve cardiovascular risk factors for both type 1 and type 2 diabetes groups [15]. Recently, some commercialized glucose monitoring systems have already been introduced, with clinical evidence of the system in several countries with good IT-infrastructure. For example, MyCare-Team is a diabetes management facilitating solution that uses web-based software, which allows for interactive communication between patients and their physicians or family members (www.mycareteam.com; MyCareTeam Inc., Chelmsford, MA, USA). A similar web-based service system, in which patients could communicate with a diabetes-specialist care team consisting of a nurse, nutritionist, and exercise therapist, was introduced to improve the glycemic control of patients with gestational diabetes mellitus and pregnancy-associated diabetes (www.cared.co.kr; Pyeonghwa Uhealth Co., Seoul, Korea). Growing numbers of healthcare companies are currently employing IT tools for their care solutions rather than traditional telephone-based services in USA. Alere, for example, has developed a diabetes management program that focuses principally on education and ensuring that patients adhere to the physician's directions and clinical guidelines via web-based tools and telephone interactions (www.alere.com; Alere Health, Atlanta, GA, USA). We expect that the IT-based healthcare market can be increased in size in the near future, by establishing evidence of improvements in the quality of disease care, eventual medical cost reductions, and improvements in patient satisfaction.
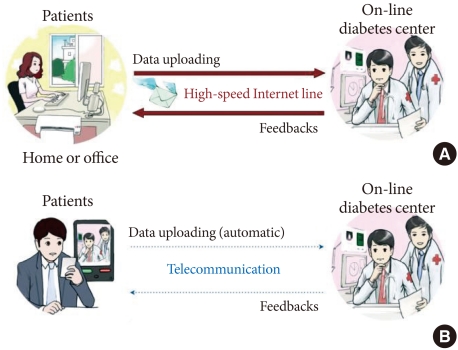
(A) A scheme of the Internet-based glucose monitoring system. Patients logged on to the website from their homes or offices at a time and uploaded their glucose data, together with additional information such as current drug information (the type and dosage of oral hypoglycaemic medications or insulin), lifestyle modifications and hypoglycaemic events. In addition, patients recorded any changes in their blood pressure or weight, and any questions or detailed information that they wished to discuss, such as changes in diet, exercise, hypoglycaemic events, and other factors that might influence their blood glucose level. Medical team of on-line diabetes center reviewed the uploaded information and sent optimal feedbacks to the patients periodically. (B) A scheme of the telecommunication based glucose control system in which mobile devices such as a mobile phone with the capacity to measure blood glucose were adopted. Patients could upload their self-monitoring of blood glucose data through telecommunication automatically and the medical team responded to patients after reviewing the uploaded data. The patient-doctor communication could be achieved practically in real time by the short message service.

The screen viewed by patients and physicians on the website for diabetes management. Basic profile, past history, family history, and laboratory data are shown on the top. Self-monitored blood glucose levels are shown (middle), which are recorded as fasting or postprandial (breakfast, lunch, and dinner). Drug information, notes from the patients, and recommendations from the physicians are shown at the bottom. Weight and blood pressure also can be shown.
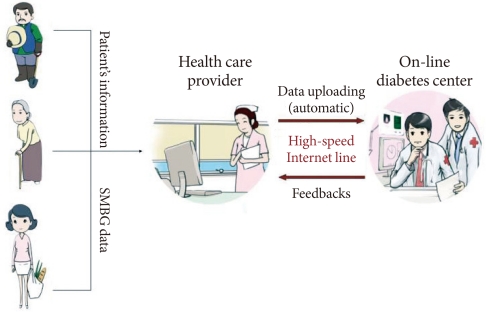
Scheme of the Internet-based diabetes management system using a PDA-type blood glucometer. First, a nurse checked the self-monitoring of blood glucose (SMBG) data of patients with PDA-type glucometer and sent the patients' data, including SMBG data, to the medical team of the on-line diabetes center. The medical team reviewed the patients' uploaded information and sent optimal messages to the nurse. The nurse educated and managed the patients according to the recommendations sent by medical team.
Cell phone-based communication system
A real-time telemedicine transmission system has also been previously developed and tested. Farmer et al. [16] demonstrated that real-time telemedicine was both feasible and realistic in a randomized controlled trial. Further, the notion of measuring the blood glucose level directly via a mobile phone has also been conceived of and introduced (Fig. 1B). In the Republic of Korea, a mobile phone with a glucometer, called a "diabetes phone" has been developed, with which patients could measure glucose levels and send the data directly to the web server of an online diabetes center. We conducted a randomized controlled trial to compare a new telecommunication-based interactive system using the "diabetes phone" coupled with the previous Internet-based glucose monitoring system. In 2009, we reported that the effect of the mobile communication system using the "diabetes phone" was not inferior to that of the Internet-based glucose monitoring system in terms of patient's supervision, care, and patient's satisfaction [17]. In the same year, Yoo et al. [18] reported a ubiquitous chronic disease care system using cellular phones and the Internet for overweight patients with both type 2 diabetes and hypertension. Using this system, they could induce significant improvements in HbA1c and blood pressure. Total cholesterol, low density lipoprotein cholesterol, and triglyceride levels were also improved. Interest in telecommunication-based interactive systems has increased, especially because mobile phones, among all the currently available patient-directed technologies, are likely to have the greatest potential use even in countries with low IT-resource settings as well as in countries with good IT-resource settings, such as the Internet. Additionally, a mobile diabetes education and care system for a rural area exerted beneficial effects in children and young people suffering from type 1 diabetes [19]. However, when employing mobile phones and text messages, the potential length of the messages is quite limited, for example within 80 bytes. The fact that text messaging on mobile phones is a very limited means of communication represents a possible disadvantage for utilizing real-time telemedicine in providing various kinds of information with regard to patients' blood glucose status. Thus, we will require other types of real-time mobile communication devices, such as smartphones, which could provide both convenience and a sufficient quantity of information. Additionally, we anticipate that various medical apparatus integrated with such mobile communications devices will be developed within the not-too-distant future.
Indirect communication system mediated by health care provider
Above, we described the clinical effects of the direct interactive communication system on diabetes. However, we must consider that there are more patients, for example, people living in rural areas, who cannot readily access diabetes centers or meet nurses or doctors who specialize in diabetes. For these individuals, such interactive communications might prove an effective tool for diabetes management. Thus, we have attempted to develop a new healthcare delivery system, which could link endocrinologists at diabetes centers in urban areas and people living in rural areas via ITs. We allowed nurses working in public healthcare posts in rural areas to send information regarding specific patients' glucose readings to an endocrinologist using PDA-type glucometers. The specialist could review the uploaded data and could send advice regarding patient management to the nurses. The nurses then educated the patients in accordance with the advice sent from the specialist (Fig. 3) [20]. This indirect communication system might eventually be applied to health workers living in low-resource settings, thereby contributing to the improvement of universal IT-based diabetes management systems and improvements in diabetes management.
JOURNEY TO IMPROVING COST EFFECTIVENESS
In above, we have introduced clinical evidence of an interactive communication system using IT. However, increases in medical costs are also certain to facilitate the maintenance of interactive services. Therefore, efforts must be made to demonstrate the economic impacts of such services and to reduce the costs associated with maintenance of the service. We reported a simulation study in which it was shown that the Internet-based glucose monitoring system could significantly reduce the development of most diabetic complications relative to conventional out-patient management systems [21]. Additionally, the willingness-to-pay threshold might save $27,666 of costs per person for 35 years compared to conventional face-to-face interview systems in outpatient clinics [22]. Johnson et al. [23] reported previously that individuals were willing to pay $1,500 over 3 years to participate in a lifestyle intervention program similar to the Diabetes Prevention program. This means that individuals at high risk of diabetes are willing to pay more than individuals with lower levels of perceived risk. An IT-based patient care system could be more effective and seems rather tempting; once again, though, the key to the feasibility of such a system lies in the cost-effectiveness of such IT-based interactive systems [24] even in high-resource settings, and the amount that an individual is willing to pay may well depend on their perception of risk.
Data analysis system and clinical decision-supporting system
In order to develop a more cost-efficient system, the labor time required of healthcare providers should be minimized, while preserving some communication between patients and medical team and not affecting their influences on diabetes. Recently, we piloted a system, referred to as a semi-automatic response system (SARS), which responds automatically to patients when the glucose levels are acceptable, but which will report to the medical team for further evaluation when the results are abnormal or difficult to determine. We also reported the effects of the SARS for glucose control on labor savings. This system, which featured an algorithm-based glucose decision tree, reduced physicians' labor time by nearly 50% without affecting glucose control while preserving interactive communications when necessary [25]. Simple algorithm-based programs might prove inadequate to meet the complexity of clinical decision-making however, and in the future artificial intelligence-based programs may be developed to handle complex patient data, detect the relevant patterns, and suggest a new treatment strategy. Various types of clinical decision supporting systems (CDSS) have been developed, which can provide diagnostic services and therapeutic services to both clinicians and patients by using electronically-recorded health data. In 2010, Rossi et al. [26], introduced a new telemedicine system based on an interactive diabetes diary, which helped patients to follow a flexible diet and insulin therapy using a carbohydrate program. The interactive diabetes diary was at least as effective as traditional carbohydrate counting education, allowing dietary freedom for patients with type 1 diabetes. This reduced the time required for education and was associated with lower levels of weight gain. Most of all, "Diabetes Interactive Diary" significantly improved treatment satisfaction and quality-of-life dimensions. In the future, more types of CDSS should be developed and we anticipate that such CDSS could improve the accuracy of diagnosis and the efficacy of treatment.
SENSORS, DEVICES, AND INTERCONNECTION
Many people expect various types of sensors or devices for patients' data monitoring to be developed in the near future. Nowadays, some new sensors or devices have already been introduced. For example, a physical activity monitor (Lifecoder, Suzuken, Japan; Actical, Philips, Andover, MA, USA) is currently in use for the monitoring of actual home physical activity. Then, measured patient data needs to be sent automatically to improve convenience. Recently, we introduced an automatic data uploading system for this purpose. This system allows for self-monitored glucose data measured with a home glucometer (OneTouch Ultra; Lifescan, Milipitas, CA, USA) to be sent to a patient's web chart via the Internet, simply by connecting it to a personal computer. Physicians can view the automatically uploaded glucose data on the web chart and send messages to the patients, along with suggestions. Other patient data, including data regarding physical activity in the home, also needs to be fed into a communication system. Moreover, the idea of integrating web-based communication with the hospital's own electronic medical record charting system was previously introduced [27]. Electronic Health Records (EHR) will be generated according to patient demographics, progress notes, problems, medications, vital signs, past medical history, immunization, laboratory data, and radiology reports, and data were monitored by different sensors or devices. The EHR data automates the clinician's workflow, generating a complete record of a clinical patient encounter.
CONCLUSION
In this study, interactive communication systems using ITs such as the Internet or telecommunications devices were shown to be effective in diabetes management. Thus, it is generally believed that the dramatic development of IT and its application to health management systems will play a crucial role in medicine. Simple IT management models for the control of blood glucose levels for diabetic patients will definitely evolve into far more complex models, in which various types of communication technologies or patients' data sensing technologies are integrated in order to effect the complex management functions required. Thus, a data analysis system or a clinical decision supporting system that can meet the complex patients' data efficiently should be developed in the future. Most of all, cost effectiveness must be demonstrated, and efforts to minimize the labor time of medical team should be followed. As the numbers of patients with diabetes is increasing sharply in recent years, the novel system introduced herein can be expanded to achieve more effective diabetes management in the near future. However, there is little evidence thus far regarding the clinical outcomes of the system. We require further investigations to demonstrate the clinical outcomes of the system, including the incidence of diabetic complications and mortality rates. In addition, various types of ubiquitous management models for other chronic diseases aside from diabetes should be developed according to advances in bio-technology and IT.