
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Complications
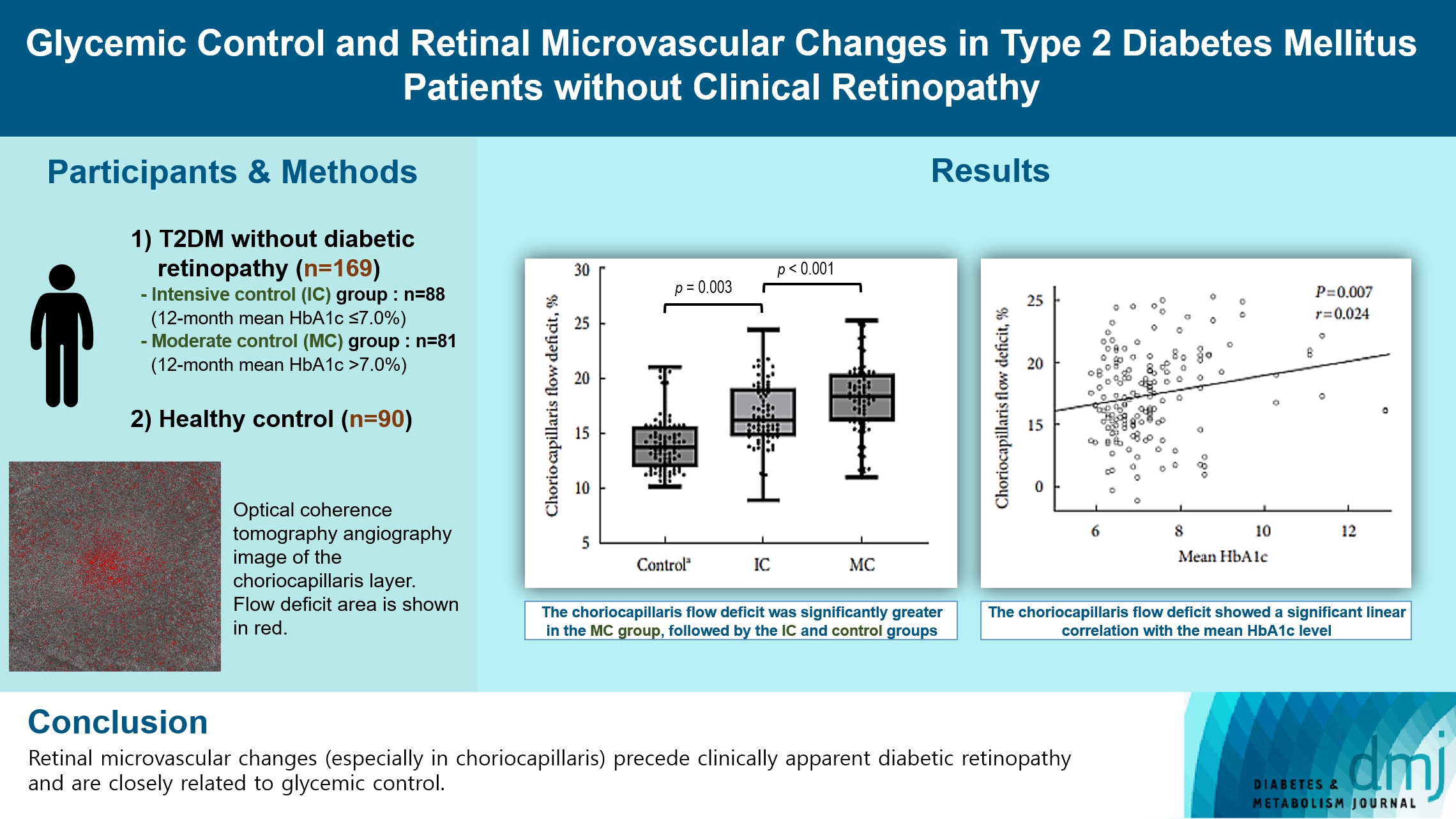
- Glycemic Control and Retinal Microvascular Changes in Type 2 Diabetes Mellitus Patients without Clinical Retinopathy
- Kangmin Lee, Ga Hye Lee, Seung Eun Lee, Jee Myung Yang, Kunho Bae
- Received May 15, 2023 Accepted December 15, 2023 Published online March 13, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0149 [Epub ahead of print]
- 635 View
- 34 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To investigate the association of glycemic control and retinal microvascular changes in patients with type 2 diabetes mellitus (T2DM) without diabetic retinopathy (DR).
Methods
This retrospective, observational, cohort study included patients with T2DM without DR. The patients were categorized into intensive control (IC; mean glycosylated hemoglobin [HbA1c] ≤7.0%) and moderate control (MC; mean HbA1c >7.0%) groups. Optical coherence tomography (OCT) and swept-source OCT angiography (OCTA) image parameters were compared between three groups, including healthy controls.
Results
In total, 259 eyes of 259 participants (88 IC, 81 MC, and 90 controls) were included. The foveal avascular zone area was significantly larger in the MC group than IC and control groups (all P<0.05). The IC group had lower vessel density in the superficial retinal layer and deep retinal layer than the controls (all P<0.05). The choriocapillaris (CC) flow deficit (FD) was significantly greater in the MC group than in the IC and control groups (18.2%, 16.7%, and 14.2%, respectively; all P<0.01). In multivariate regression analysis, CC-FD was associated with the mean HbA1c level (P=0.008). There were no significant differences in OCT parameters among the groups.
Conclusion
OCTA revealed that early CC impairment is associated with HbA1c levels; the CC changes precede clinically apparent DR. The OCTA parameters differed among the groups according to the degree of glycemic control. Our results suggest that microvascular changes precede DR and are closely related to glycemic control.
- Metabolic Risk/Epidemiology
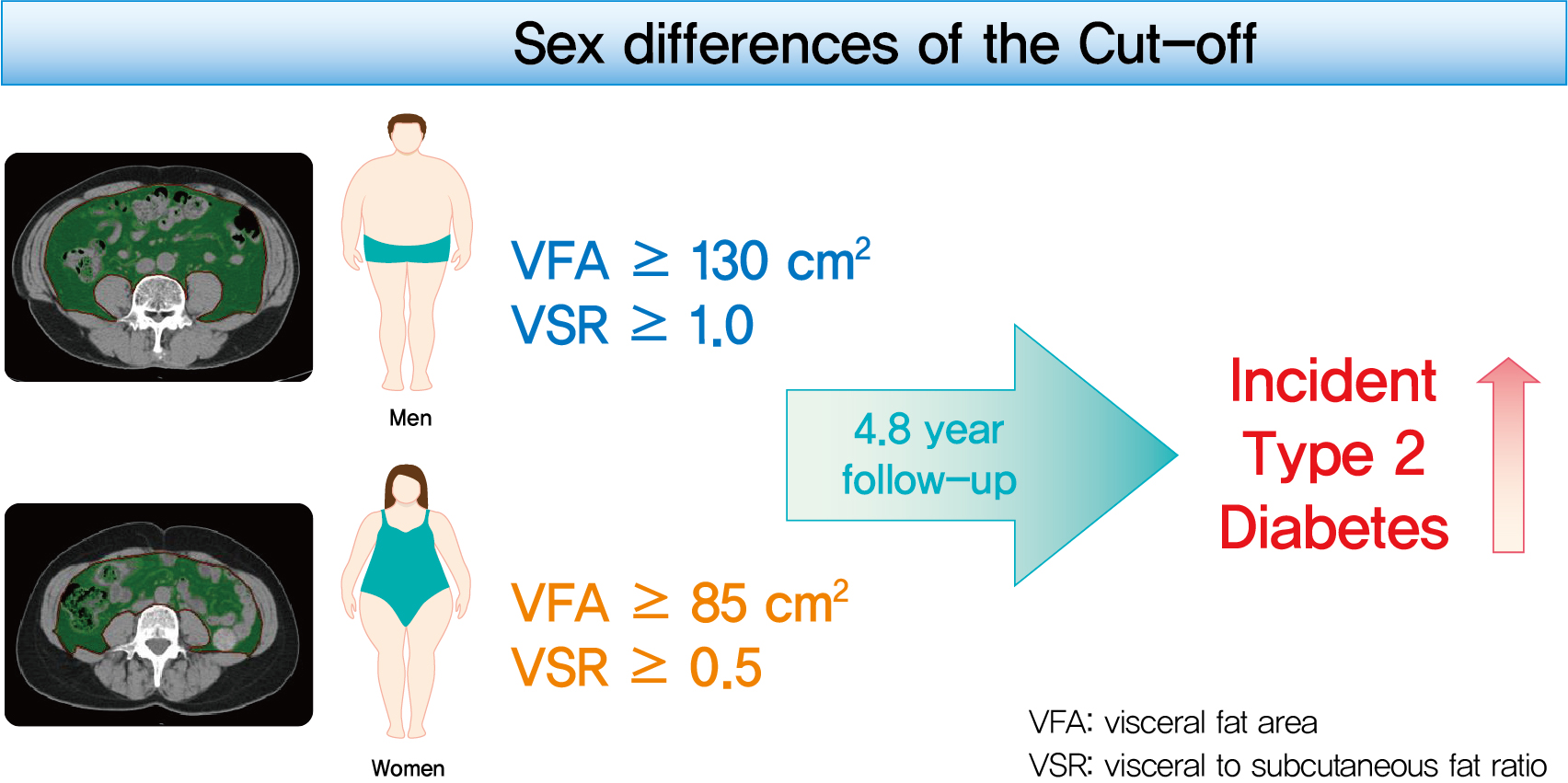
- Sex Differences of Visceral Fat Area and Visceral-to-Subcutaneous Fat Ratio for the Risk of Incident Type 2 Diabetes Mellitus
- Eun Hee Kim, Hong-Kyu Kim, Min Jung Lee, Sung-Jin Bae, Jaewon Choe, Chang Hee Jung, Chul-Hee Kim, Joong-Yeol Park, Woo Je Lee
- Diabetes Metab J. 2022;46(3):486-498. Published online November 18, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0095
- 9,323 View
- 367 Download
- 19 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study aimed to determine the optimal cut-off values of visceral fat area (VFA) and visceral-to-subcutaneous fat ratio (VSR) for predicting incident type 2 diabetes mellitus (T2DM).
Methods
A total of 10,882 individuals (6,835 men; 4,047 women) free of T2DM at baseline aged between 30 and 79 years who underwent abdominal computed tomography scan between 2012 and 2013 as a part of routine health check-ups were included and followed. VFA, subcutaneous fat area, and VSR on L3 vertebral level were measured at baseline.
Results
During a median follow-up of 4.8 years, 730 (8.1% for men; 4.3% for women) incident cases of T2DM were identified. Receiver operating characteristic curve analysis showed that the optimal cut-off values of VFA and VSR for predicting incident T2DM were 130.03 cm2 and 1.08 in men, respectively, and 85.7 cm2 and 0.48 in women, respectively. Regardless of sex, higher VFA and VSR were significantly associated with a higher risk of incident T2DM. Compared with the lowest quartiles of VFA and VSR, the highest quartiles had adjusted odds ratios of 2.62 (95% confidence interval [CI], 1.73 to 3.97) and 1.55 (95% CI, 1.14 to 2.11) in men, respectively, and 32.49 (95% CI, 7.42 to 142.02) and 11.07 (95% CI, 3.89 to 31.50) in women, respectively.
Conclusion
Higher VFA and VSR at baseline were independent risk factors for the development of T2DM. Sex-specific reference values for visceral fat obesity (VFA ≥130 cm2 or VSR ≥1.0 in men; VFA ≥85 cm2 or VSR ≥0.5 in women) are proposed for the prediction of incident T2DM. -
Citations
Citations to this article as recorded by- Severity of adipose tissue dysfunction is associated with progression of pre-diabetes to type 2 diabetes: the Tehran Lipid and Glucose Study
Mohammad Jalali, Zahra Bahadoran, Parvin Mirmiran, Fereidoun Azizi, Farhad Hosseinpanah
BMC Public Health.2024;[Epub] CrossRef - Should insulin resistance (HOMA-IR), insulin secretion (HOMA-β), and visceral fat area be considered for improving the performance of diabetes risk prediction models
Huan Hu, Tohru Nakagawa, Toru Honda, Shuichiro Yamamoto, Tetsuya Mizoue
BMJ Open Diabetes Research & Care.2024; 12(1): e003680. CrossRef - Adipose organ dysfunction and type 2 diabetes: Role of nitric oxide
Zahra Bahadoran, Parvin Mirmiran, Asghar Ghasemi
Biochemical Pharmacology.2024; 221: 116043. CrossRef - Prediction of high visceral adipose tissue for sex‐specific community residents in Taiwan
Yu‐Hsuan Chang, Chin‐Sung Chang, Chieh‐Yu Liu, Yin‐Fan Chang, Shiow‐Ching Shun
Nursing & Health Sciences.2024;[Epub] CrossRef - Guidelines for obesity clinic consultations in primary healthcare clinics
Jee-Hyun Kang, Kyoung-Kon Kim
Journal of the Korean Medical Association.2024; 67(4): 240. CrossRef - Correlation between fat-to-muscle mass ratio and cognitive impairment in elderly patients with type 2 diabetes mellitus: a cross-sectional study
Fan Wu, Yanlan Liu, Chenying Lin, Nahal Haghbin, Longfei Xia, Yaoshuang Li, Tong Chen, Huina Qiu, Weiran Jiang, Jingbo Li, Jingna Lin
BMC Geriatrics.2024;[Epub] CrossRef - Body Composition and Metabolic Dysfunction Really Matter for the Achievement of Better Outcomes in High-Grade Serous Ovarian Cancer
Mauricio A. Cuello, Fernán Gómez, Ignacio Wichmann, Felipe Suárez, Sumie Kato, Elisa Orlandini, Jorge Brañes, Carolina Ibañez
Cancers.2023; 15(4): 1156. CrossRef - MEDICINAL BIOMAGNETISM FOR THE TREATMENT OF OBESITY
Ana Vergínia Campagnollo Bueno, Michelli Gonçalves Seneda, Ângela Mara Rambo, Ana Clara Campagnolo Gonçalves Toledo, Caroline Cabral de Azevedo, Adriane Viapiana Bossa
Health and Society.2023; 3(01): 411. CrossRef - Cumulative exposure to metabolic syndrome in a national population-based cohort of young adults and sex-specific risk for type 2 diabetes
Min-Kyung Lee, Jae-Hyuk Lee, Seo Young Sohn, Jiyeon Ahn, Oak-Kee Hong, Mee-Kyoung Kim, Ki-Hyun Baek, Ki-Ho Song, Kyungdo Han, Hyuk-Sang Kwon
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - The correlation between visceral fat/subcutaneous fat area ratio and monocyte/high-density lipoprotein ratio in patients with type 2 diabetes mellitus and albuminuria
Haiyan Lin, Jun Zhu, Chen Zheng, Xiaoming Xu, Shandong Ye
Journal of Diabetes and its Complications.2023; 37(11): 108521. CrossRef - Effects of the abdominal fat distribution on the relationship between exposure to air pollutants and thyroid hormones among Korean adult males
Hyun-Jin Kim, Byungmi Kim, Seyoung Kim, Hyuktae Kwon, Jae Moon Yun, Belong Cho, Jin-Ho Park
European Journal of Medical Research.2023;[Epub] CrossRef - Association of Visceral Fat Obesity, Sarcopenia, and Myosteatosis with Non-Alcoholic Fatty Liver Disease without Obesity
Hong-Kyu Kim, Sung-Jin Bae, Min Jung Lee, Eun Hee Kim, Hana Park, Hwi Seung Kim, Yun Kyung Cho, Chang Hee Jung, Woo Je Lee, Jaewon Choe
Clinical and Molecular Hepatology.2023; 29(4): 987. CrossRef - Visceral adipose tissue reference data computed for GE HealthCare DXA from the National Health and Nutrition Examination Survey data set
Jonathan P. Bennett, Brandon K. Quon, Bo Fan, En Liu, Leila Kazemi, Rosa C. Villegas‐Valle, Raj Ahgun, Xian‐pin Wu, Hou‐De Zhou, Ying Lu, John A. Shepherd
Obesity.2023; 31(12): 2947. CrossRef - Comparison of bioelectrical body and visceral fat indices and anthropometric measures in relation to type 2 diabetes by sex among Chinese adults, a cross-sectional study
Jiangshan He, Binbin Zhang, Yaqi Fan, Yuxue Wang, Mianzhi Zhang, Chunjun Li, Li Zhang, Pei Guo, Minying Zhang
Frontiers in Public Health.2023;[Epub] CrossRef - The predictive significance of lipid accumulation products for future diabetes in a non-diabetic population from a gender perspective: an analysis using time-dependent receiver operating characteristics
Jiajun Qiu, Maobin Kuang, Yang Zou, Ruijuan Yang, Qing Shangguan, Dingyang Liu, Guotai Sheng, Wei Wang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Cellular interplay between cardiomyocytes and non-myocytes in diabetic cardiomyopathy
Ren Jie Phang, Rebecca H. Ritchie, Derek J. Hausenloy, Jarmon G. Lees, Shiang Y. Lim
Cardiovascular Research.2022;[Epub] CrossRef - Implication of Sex Differences in Visceral Fat for the Assessment of Incidence Risk of Type 2 Diabetes Mellitus
Sang Hyeon Ju, Hyon-Seung Yi
Diabetes & Metabolism Journal.2022; 46(3): 414. CrossRef - Visceral fat area and body fat percentage measured by bioelectrical impedance analysis correlate with glycometabolism
Shuying Li, Shaoping Li, Jie Ding, Weihong Zhou
BMC Endocrine Disorders.2022;[Epub] CrossRef - The Demographic Specific Abdominal Fat Composition and Distribution Trends in US Adults from 2011 to 2018
Furong Xu, Jacob E. Earp, Bryan J. Blissmer, Ingrid E. Lofgren, Matthew J. Delmonico, Geoffrey W. Greene
International Journal of Environmental Research and Public Health.2022; 19(19): 12103. CrossRef - Visceral Obesity Is a More Important Factor for Colorectal Adenomas than Skeletal Muscle or Body Fat
Ji Yeon Seo, Yoo Min Han, Su Jin Chung, Seon Hee Lim, Jung Ho Bae, Goh Eun Chung
Cancers.2022; 14(21): 5256. CrossRef - Recent Advances in Visceral Obesity and Related Diseases
佳佳 魏
Advances in Clinical Medicine.2022; 12(12): 11686. CrossRef - Gender differences in the ideal cutoffs of visceral fat area for predicting MAFLD in China
Pingping Yu, Huachao Yang, Xiaoya Qi, Ruixue Bai, Shouqin Zhang, Jianping Gong, Ying Mei, Peng Hu
Lipids in Health and Disease.2022;[Epub] CrossRef
- Severity of adipose tissue dysfunction is associated with progression of pre-diabetes to type 2 diabetes: the Tehran Lipid and Glucose Study
- Cardiovascular Risk/Epidemiology
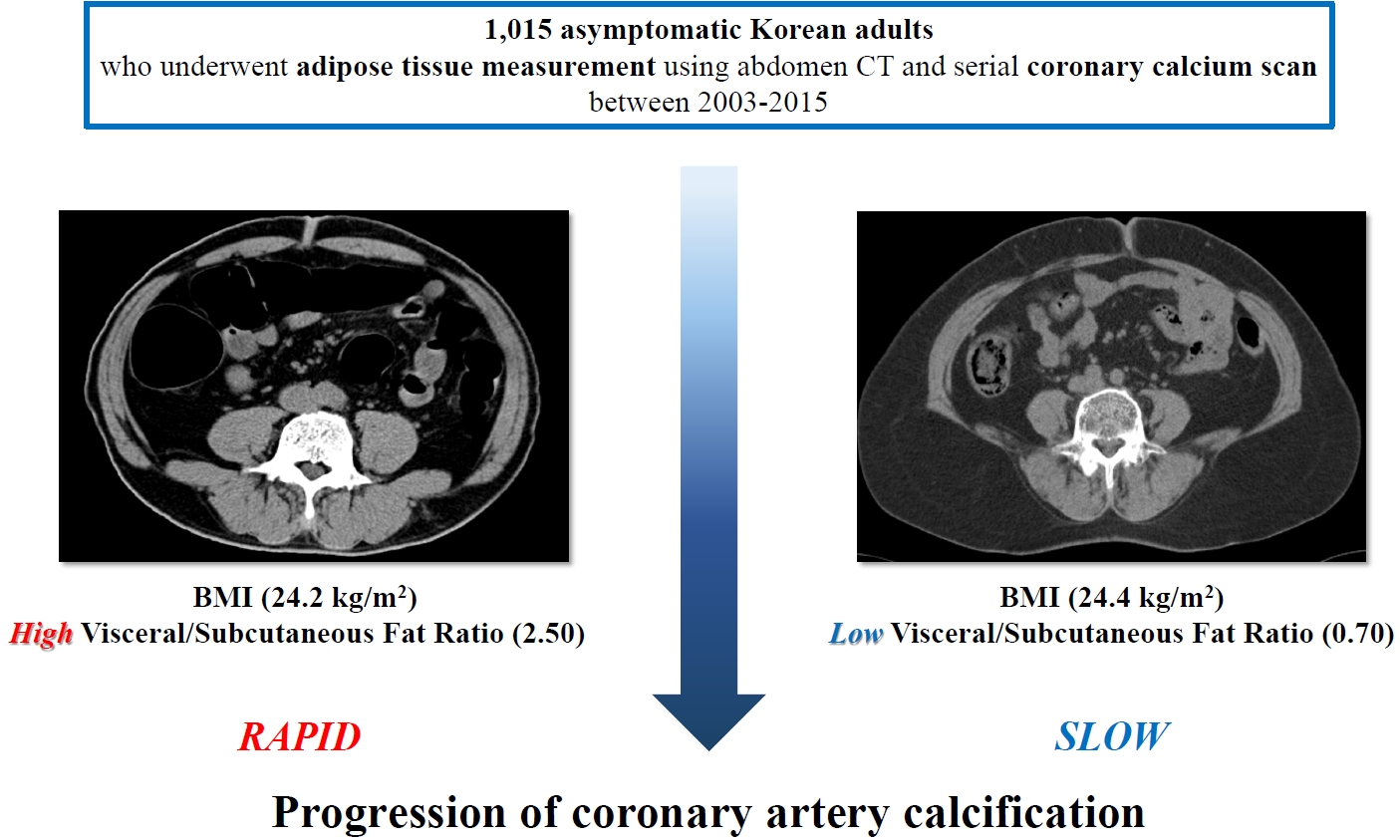
- Clinical Significance of Body Fat Distribution in Coronary Artery Calcification Progression in Korean Population
- Heesun Lee, Hyo Eun Park, Ji Won Yoon, Su-Yeon Choi
- Diabetes Metab J. 2021;45(2):219-230. Published online October 28, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0161
- Correction in: Diabetes Metab J 2021;45(6):974
- 6,518 View
- 257 Download
- 8 Web of Science
- 7 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- Background
Although obesity differs according to ethnicity, it is globally established as a solid risk factor for cardiovascular disease. However, it is not fully understood how obesity parameters affect the progression of coronary artery calcification (CAC) in Korean population. We sought to evaluate the association of obesity-related parameters including visceral adipose tissue (VAT) measurement and CAC progression.
Methods
This retrospective observational cohort study investigated 1,015 asymptomatic Korean subjects who underwent serial CAC scoring by computed tomography (CT) with at least 1-year interval and adipose tissue measurement using non-contrast CT at baseline for a routine checkup between 2003 and 2015. CAC progression, the main outcome, was defined as a difference of ≥2.5 between the square roots of the baseline and follow-up CAC scores using Agatston units.
Results
During follow-up (median 39 months), 37.5% of subjects showed CAC progression of a total population (56.4 years, 80.6% male). Body mass index (BMI) ≥25 kg/m2, increasing waist circumferences (WC), and higher VAT/subcutaneous adipose tissue (SAT) area ratio were independently associated with CAC progression. Particularly, predominance of VAT over SAT at ≥30% showed the strongest prediction for CAC progression (adjusted hazard ratio, 2.20; P<0.001) and remained of prognostic value regardless of BMI or WC status. Further, it provided improved risk stratification of CAC progression beyond known prognosticators.
Conclusion
Predominant VAT area on CT is the strongest predictor of CAC progression regardless of BMI or WC in apparently healthy Korean population. Assessment of body fat distribution may be helpful to identify subjects at higher risk. -
Citations
Citations to this article as recorded by- Gender-specific abdominal fat distribution and insulin resistance associated with organophosphate esters and phthalate metabolites exposure
Xiaoliu Shi, Wanyue Wang, Jiafan Feng, Xiaochun Ma, Mengting Xu, Cui Wang
Environmental Pollution.2024; 349: 123959. CrossRef - The association between C-reactive protein and coronary artery calcification: a systematic review and meta-analysis
Amirhossein Tajani, Masoumeh Sadeghi, Navid Omidkhoda, Amir Hooshang Mohammadpour, Sara Samadi, Vahid Jomehzadeh
BMC Cardiovascular Disorders.2024;[Epub] CrossRef - Visceral adipose tissue is an independent predictor and mediator of the progression of coronary calcification: a prospective sub-analysis of the GEA study
Neftali Eduardo Antonio-Villa, Juan Gabriel Juárez-Rojas, Rosalinda Posadas-Sánchez, Juan Reyes-Barrera, Aida Medina-Urrutia
Cardiovascular Diabetology.2023;[Epub] CrossRef - Deep learning-based prediction for significant coronary artery stenosis on coronary computed tomography angiography in asymptomatic populations
Heesun Lee, Bong Gyun Kang, Jeonghee Jo, Hyo Eun Park, Sungroh Yoon, Su-Yeon Choi, Min Joo Kim
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Relationship between a novel non–insulin-based metabolic score for insulin resistance (METS‐IR) and coronary artery calcification
Zhenwei Wang, Xiaofang Hui, Xu Huang, Jingjie Li, Naifeng Liu
BMC Endocrine Disorders.2022;[Epub] CrossRef - Association Between Abdominal Adipose Tissue Distribution and Risk of Endometrial Cancer: A Case-Control Study
Yuan Cheng, Zhongyu Wang, Xiaoxuan Jia, Rong Zhou, Jianliu Wang
Clinical Medicine Insights: Oncology.2022; 16: 117955492211407. CrossRef - Sex differences in cardiovascular risk may be related to sex differences in diet patterns: a narrative review
A. M. Tindall, V. A. Stallings
Annals of Human Biology.2021; 48(6): 517. CrossRef
- Gender-specific abdominal fat distribution and insulin resistance associated with organophosphate esters and phthalate metabolites exposure
- Metabolic Risk/Epidemiology
- Association between the Thigh Muscle and Insulin Resistance According to Body Mass Index in Middle-Aged Korean Adults
- Ji Eun Heo, Jee-Seon Shim, Hokyou Lee, Hyeon Chang Kim
- Diabetes Metab J. 2020;44(3):446-457. Published online April 16, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0110
- 6,760 View
- 89 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background We examined the associations between thigh muscle area (TMA) and insulin resistance (IR) according to body mass index (BMI) in middle-aged Korean general population.
Methods TMA was measured using quantitative computed tomography and corrected by body weight (TMA/Wt) in 1,263 men, 788 premenopausal women, and 1,476 postmenopausal women all aged 30 to 64 years. The tertiles of TMA/Wt were calculated separately for men and for premenopausal and postmenopausal women. Homeostatic model assessment for insulin resistance (HOMA-IR) was performed using fasting blood glucose and insulin levels, and increased IR was defined according to sex-specific, top quartiles of HOMA-IR. Associations between the TMA/Wt tertiles and increased IR according to the BMI categories (<25 and ≥25 kg/m2) were assessed using multivariable logistic regression analysis.
Results In men with higher BMIs, but not in those with lower BMIs, the presence of an increased IR had significantly higher odds ratios in the lower TMA/Wt tertiles, even after adjustment for visceral fat area. However, in premenopausal and postmenopausal women, there was no significant inverse association between TMA/Wt tertiles and increased IR, regardless of BMI category.
Conclusion Our findings suggest that the thigh muscle is inversely associated with IR in men, particularly in those with higher BMIs.
-
Citations
Citations to this article as recorded by- Risk of sleep apnea associated with higher blood pressure among Chinese and Korean Americans
Brittany N. Morey, Yuxi Shi, Soomin Ryu, Susan Redline, Ichiro Kawachi, Hye Won Park, Sunmin Lee
Ethnicity & Health.2024; 29(3): 295. CrossRef - Sex-specific equations to estimate body composition: Derivation and validation of diagnostic prediction models using UK Biobank
Yueqi Lu, Ying Shan, Liang Dai, Xiaosen Jiang, Congying Song, Bangwei Chen, Jingwen Zhang, Jing Li, Yue Zhang, Junjie Xu, Tao Li, Zuying Xiong, Yong Bai, Xiaoyan Huang
Clinical Nutrition.2023; 42(4): 511. CrossRef - Gender Differences in Relation to Body Composition, Insulin Resistance, and Islet Beta Cell Function in Newly Diagnosed Diabetic or Pre-Diabetic Patients
Minglei Ma, Tao Jiang, Zhen Wen, Dongxue Zhang, Lei Xiu
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 723. CrossRef - Non-Alcoholic Fatty Liver Disease with Sarcopenia and Carotid Plaque Progression Risk in Patients with Type 2 Diabetes Mellitus
Yongin Cho, Hye-Sun Park, Byung Wook Huh, Yong-ho Lee, Seong Ha Seo, Da Hea Seo, Seong Hee Ahn, Seongbin Hong, So Hun Kim
Diabetes & Metabolism Journal.2023; 47(2): 232. CrossRef - Prospective External Validation of an Algorithm Predicting Hourly
Basal Insulin Infusion Rates from Characteristics of Patients with Type 1
Diabetes Treated with Insulin Pumps
Jana S. Schmelzer, Melanie Kahle-Stephan, Juris J. Meier, Michael A. Nauck
Experimental and Clinical Endocrinology & Diabetes.2023; 131(10): 539. CrossRef - Establishing reference values for percentage of appendicular skeletal muscle mass and their association with metabolic syndrome in Korean adolescents
Da Hye Lee, Sung-Chan Kang, Seung-Sik Hwang, Yun Jeong Lee, Hwa Young Kim, Seong Yong Lee, Choong Ho Shin, Jaehyun Kim
Annals of Pediatric Endocrinology & Metabolism.2023; 28(4): 237. CrossRef - Evaluating Triglyceride and Glucose Index as a Simple and Easy-to-Calculate Marker for All-Cause and Cardiovascular Mortality
Kyung-Soo Kim, Sangmo Hong, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
Journal of General Internal Medicine.2022; 37(16): 4153. CrossRef - Association between Lower-to-Upper Ratio of Appendicular Skeletal Muscle and Metabolic Syndrome
Hyun Eui Moon, Tae Sic Lee, Tae-Ha Chung
Journal of Clinical Medicine.2022; 11(21): 6309. CrossRef
- Risk of sleep apnea associated with higher blood pressure among Chinese and Korean Americans
- Clinical Diabetes & Therapeutics
- Diabetes and Subclinical Coronary Atherosclerosis
- Chang Hoon Lee, Seung-Whan Lee, Seong-Wook Park
- Diabetes Metab J. 2018;42(5):355-363. Published online October 22, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0041
- 4,732 View
- 58 Download
- 13 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader It is well known that diabetic patients have a high risk of cardiovascular events, and although there has been a tremendous effort to reduce these cardiovascular risks, the incidence of cardiovascular morbidity and mortality in diabetic patients remains high. Therefore, the early detection of coronary artery disease (CAD) is necessary in those diabetic patients who are at risk of cardiovascular events. Significant medical and radiological advancements, including coronary computed tomography angiography (CCTA), mean that it is now possible to investigate the characteristics of plaques, instead of solely evaluating the calcium level of the coronary artery. Recently, several studies reported that the prevalence of subclinical coronary atherosclerosis (SCA) is higher than expected, and this could impact on CAD progression in asymptomatic diabetic patients. In addition, several reports suggest the potential benefit of using CCTA for screening for SCA in asymptomatic diabetic patients, which might dramatically decrease the incidence of cardiovascular events. For these reasons, the medical interest in SCA in diabetic patients is increasing. In this article, we sought to review the results of studies on CAD in asymptomatic diabetic patients and discuss the clinical significance and possibility of using CCTA to screen for SCA.
-
Citations
Citations to this article as recorded by- Coronary Artery Calcium Score directed risk stratification of patients with Type-2 diabetes mellitus
Mahmoud Nassar, Nso Nso, Kelechi Emmanuel, Mohsen Alshamam, Most Sirajum Munira, Anoop Misra
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2022; 16(6): 102503. CrossRef - Association between carotid atherosclerosis and presence of intracranial atherosclerosis using three-dimensional high-resolution vessel wall magnetic resonance imaging in asymptomatic patients with type 2 diabetes
Ji Eun Jun, You-Cheol Hwang, Kyu Jeong Ahn, Ho Yeon Chung, Geon-Ho Jahng, Soonchan Park, In-Kyung Jeong, Chang-Woo Ryu
Diabetes Research and Clinical Practice.2022; 191: 110067. CrossRef - Serum metabolic signatures of subclinical atherosclerosis in patients with type 2 diabetes mellitus: a preliminary study
Jiaorong Su, Qing Zhao, Aihua Zhao, Wei Jia, Wei Zhu, Jingyi Lu, Xiaojing Ma
Acta Diabetologica.2021; 58(9): 1217. CrossRef - Atherogenic Index of Plasma, Triglyceride-Glucose Index and Monocyte-to-Lymphocyte Ratio for Predicting Subclinical Coronary Artery Disease
Yueqiao Si, Wenjun Fan, Chao Han, Jingyi Liu, Lixian Sun
The American Journal of the Medical Sciences.2021; 362(3): 285. CrossRef - Cardiologist's approach to the diabetic patient: No further delay for a paradigm shift
Francesco Maranta, Lorenzo Cianfanelli, Carlo Gaspardone, Vincenzo Rizza, Rocco Grippo, Marco Ambrosetti, Domenico Cianflone
International Journal of Cardiology.2021; 338: 248. CrossRef - Co‐expression of glycosylated aquaporin‐1 and transcription factor NFAT5 contributes to aortic stiffness in diabetic and atherosclerosis‐prone mice
Rosalinda Madonna, Vanessa Doria, Anikó Görbe, Nino Cocco, Péter Ferdinandy, Yong‐Jian Geng, Sante Donato Pierdomenico, Raffaele De Caterina
Journal of Cellular and Molecular Medicine.2020; 24(5): 2857. CrossRef - Recent Updates on Vascular Complications in Patients with Type 2 Diabetes Mellitus
Chan-Hee Jung, Ji-Oh Mok
Endocrinology and Metabolism.2020; 35(2): 260. CrossRef - Quantitative measure of asymptomatic cardiovascular disease risk in Type 2 diabetes: Evidence from Indian outpatient setting
Samit Ghosal, Binayak Sinha, Jignesh Ved, Mansij Biswas
Indian Heart Journal.2020; 72(2): 119. CrossRef - Role of pregnancy hormones and hormonal interaction on the maternal cardiovascular system: a literature review
Vitaris Kodogo, Feriel Azibani, Karen Sliwa
Clinical Research in Cardiology.2019; 108(8): 831. CrossRef - Letter: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2019;43:582–9)
Tae Seo Sohn
Diabetes & Metabolism Journal.2019; 43(6): 909. CrossRef - Effects of Diabetes on Motor Recovery After Cerebral Infarct: A Diffusion Tensor Imaging Study
Jun Sung Moon, Seung Min Chung, Sung Ho Jang, Kyu Chang Won, Min Cheol Chang
The Journal of Clinical Endocrinology & Metabolism.2019; 104(9): 3851. CrossRef
- Coronary Artery Calcium Score directed risk stratification of patients with Type-2 diabetes mellitus
- Complications
- Serum Total Bilirubin Levels Provide Additive Risk Information over the Framingham Risk Score for Identifying Asymptomatic Diabetic Patients at Higher Risk for Coronary Artery Stenosis
- Jaechan Leem, Eun Hee Koh, Jung Eun Jang, Chang-Yun Woo, Jin Sun Oh, Min Jung Lee, Joon-Won Kang, Tae-Hwan Lim, Chang Hee Jung, Woo Je Lee, Joong-Yeol Park, Ki-Up Lee
- Diabetes Metab J. 2015;39(5):414-423. Published online October 22, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.5.414
- 4,247 View
- 30 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The diagnosis of coronary artery disease (CAD) is often delayed in patients with type 2 diabetes. Serum total bilirubin levels are inversely associated with CAD. However, no studies have examined whether this can be used as a biochemical marker for identifying asymptomatic diabetic patients at higher risk for having obstructive CAD.
Methods We performed a cross-sectional study of 460 consecutive asymptomatic patients with type 2 diabetes. All patients underwent coronary computed tomographic angiography, and their serum total bilirubin levels were measured. Obstructive CAD was defined as ≥50% diameter stenosis in at least one coronary artery.
Results Serum total bilirubin tertiles showed an inverse association with the prevalence of obstructive CAD. In multivariate logistic regression analysis, the odds ratio for the highest versus the lowest tertile of total bilirubin was 0.227 (95% confidence interval [CI], 0.130 to 0.398), and an increment of 1 µmol/L in serum total bilirubin level was associated with a 14.6% decrease in obstructive CAD after adjustment for confounding variables. Receiver operating characteristic curve analysis showed that the area under the curve for the Framingham Risk Score (FRS) plus serum total bilirubin level was 0.712 (95% CI, 0.668 to 0.753), which is significantly greater than that of the FRS alone (
P =0.0028).Conclusion Serum total bilirubin level is inversely associated with obstructive CAD and provides additive risk information over the FRS. Serum total bilirubin may be helpful for identifying asymptomatic patients with type 2 diabetes who are at higher risk for obstructive CAD.
-
Citations
Citations to this article as recorded by- DECREASE IN SERUM BILIRUBIN AS AN UNFAVORABLE MARKER OF CARDIOVASCULAR DISORDERS
L. M. Strilchuk, O. O. Zimba, I. B. Zhakun
Eastern Ukrainian Medical Journal.2020; 8(3): 268. CrossRef - Contemporary diagnostic algorithm for coronary artery disease: achievements and prospects
A. S. Akselrod, D. Yu. Shchekochikhin, E. S. Tebenkova, A. V. Zhelankin, D. A. Stonogina, E. A. Syrkina, S. K. Ternovoy
Kardiologiya i serdechno-sosudistaya khirurgiya.2019; 12(5): 418. CrossRef - Pharmacological actions and therapeutic potentials of bilirubin in islet transplantation for the treatment of diabetes
Qing Yao, Xue Jiang, Longfa Kou, Adelaide T. Samuriwo, He-Lin Xu, Ying-Zheng Zhao
Pharmacological Research.2019; 145: 104256. CrossRef - Evaluation of genetic effect of NOS3 and G×E interaction on the variability of serum bilirubin in a Han Chinese population
Yingshui Yao, Zhengmei Fang, Song Yang, Hailong Zhao, Yanchun Chen, Yuelong Jin, Xianghai Zhao, Lijun Zhu, Yuanrui Tian, Chong Shen
Nitric Oxide.2017; 70: 25. CrossRef - Supplementation with Phycocyanobilin, Citrulline, Taurine, and Supranutritional Doses of Folic Acid and Biotin—Potential for Preventing or Slowing the Progression of Diabetic Complications
Mark McCarty
Healthcare.2017; 5(1): 15. CrossRef - Effect of bilirubin concentration on the risk of diabetic complications: A meta-analysis of epidemiologic studies
Bo Zhu, Xiaomei Wu, Yifei Bi, Yang Yang
Scientific Reports.2017;[Epub] CrossRef - Role of Bilirubin in Diabetic Vascular Complications: Can Bilirubin Predict More than Just Liver Disease?
Jun Sung Moon
Diabetes & Metabolism Journal.2015; 39(5): 384. CrossRef
- DECREASE IN SERUM BILIRUBIN AS AN UNFAVORABLE MARKER OF CARDIOVASCULAR DISORDERS
- Diagnostic Accuracy of 64-Slice MDCT Coronary Angiography for the Assessment of Coronary Artery Disease in Korean Patients with Type 2 Diabetes
- Jun Sung Moon, Ji Sung Yoon, Kyu Chang Won, Ihn-Ho Cho, Hyoung Woo Lee
- Diabetes Metab J. 2013;37(1):54-62. Published online February 15, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.1.54
- 3,674 View
- 29 Download
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background A 64-slice multidetector computed tomography (MDCT) is well known to be a useful noninvasive form of angiography for the general population, but not for certain patients with diabetes. The aim of this study was to investigate the diagnostic accuracy and usefulness of 64-slice MDCT coronary angiography for detecting coronary artery disease in Korean patients with type 2 diabetes mellitus (T2DM).
Methods A total of 240 patients were included, 74 of whom had type 2 diabetes (M:F=40:33; 41.8±9.5 years). We compared significant coronary stenosis (>50% luminal narrowing) in MDCT with invasive coronary angiography (ICA) by segment, artery, and patient. We also evaluated the influence of obesity and coronary calcium score on MDCT accuracy.
Results Of the 4,064 coronary segments studied, 4,062 segments (T2DM=1,109) were assessed quantitatively by both MDCT and ICA, and 706 segments (T2DM=226) were detected as a significant lesion by ICA in all patients. Sensitivity, specificity, as well as positive and negative predictive values for the presence of significant stenosis in T2DM were: by segment, 89.4%, 96.4%, 85.8%, and 97.4%, respectively; by artery (
n =222), 95.1%, 92.9%, 94.4%, and 93.8%, respectively; by patients (n =74), 98.4%, 100.0%, 98.4%, and 90.0%, respectively. Regardless of presence of diabetes, there was no significant difference in diagnostic accuracy. Obesity (≥25 kg/m2) and coronary calcium score did not also affect the diagnostic accuracy of MDCT.Conclusion The 64-slice MDCT coronary angiography was found to have similar diagnostic accuracy with ICA, regardless of diabetes. These results suggest MDCT may be helpful to reduce unnecessary invasive studies for patients with diabetes.
-
Citations
Citations to this article as recorded by- Can Radiation Dose Burden of CT Angiography be Reduced While Still Accurately Diagnosing Etiology of Acute Chest Pain?
Sherine M. Sharara, Scott R. Monnin, Manolo Rubio, Rami N. Khouzam, Samar R. Ragheb
Current Problems in Cardiology.2021; 46(4): 100766. CrossRef - Assessment of high sensitivity C-reactive protein and coronary plaque characteristics by computed tomography in patients with and without diabetes mellitus
Hai-Ting Zhou, De-Li Zhao, Guo-Kun Wang, Tian-Zuo Wang, Hong-Wei Liang, Jin-Ling Zhang
BMC Cardiovascular Disorders.2020;[Epub] CrossRef - Triglyceride Glucose-Waist Circumference Better Predicts Coronary Calcium Progression Compared with Other Indices of Insulin Resistance: A Longitudinal Observational Study
Yun Kyung Cho, Jiwoo Lee, Hwi Seung Kim, Eun Hee Kim, Min Jung Lee, Dong Hyun Yang, Joon-Won Kang, Chang Hee Jung, Joong-Yeol Park, Hong-Kyu Kim, Woo Je Lee
Journal of Clinical Medicine.2020; 10(1): 92. CrossRef - The impact of non-alcoholic fatty liver disease and metabolic syndrome on the progression of coronary artery calcification
Yun Kyung Cho, Yu Mi Kang, Jee Hee Yoo, Jiwoo Lee, Seung Eun Lee, Dong Hyun Yang, Joon-Won Kang, Joong-Yeol Park, Chang Hee Jung, Hong-Kyu Kim, Woo Je Lee
Scientific Reports.2018;[Epub] CrossRef - Effects of Low-density Lipoprotein Cholesterol on Coronary Artery Calcification Progression According to High-density Lipoprotein Cholesterol Levels
Da Young Lee, Ji Hyun Kim, Se Eun Park, Cheol-young Park, Ki-won Oh, Sung-woo Park, Eun-Jung Rhee, Won-young Lee
Archives of Medical Research.2017; 48(3): 284. CrossRef - 2013 ACC/AHA Cholesterol Guideline Versus 2004 NCEP ATP III Guideline in the Prediction of Coronary Artery Calcification Progression in a Korean Population
Yun Kyung Cho, Chang Hee Jung, Yu Mi Kang, Jenie Yoonoo Hwang, Eun Hee Kim, Dong Hyun Yang, Joon‐Won Kang, Joong‐Yeol Park, Hong‐Kyu Kim, Woo Je Lee
Journal of the American Heart Association.2016;[Epub] CrossRef - Imaging Quality Evaluation of Low Tube Voltage Coronary CT Angiography Using Low Concentration Contrast Medium
Chengzhong Zhang, Yuejun Yu, Zaixian Zhang, Qingguo Wang, Linfeng Zheng, Yan Feng, Zhiguo Zhou, Guixiang Zhang, Kangan Li, Zhuoli Zhang
PLOS ONE.2015; 10(3): e0120539. CrossRef - 2013 ACC/AHA versus 2004 NECP ATP III Guidelines in the Assignment of Statin Treatment in a Korean Population with Subclinical Coronary Atherosclerosis
Chang Hee Jung, Min Jung Lee, Yu Mi Kang, Dong Hyun Yang, Joon-Won Kang, Eun Hee Kim, Duk-Woo Park, Joong-Yeol Park, Hong-Kyu Kim, Woo Je Lee, Yingmei Feng
PLOS ONE.2015; 10(9): e0137478. CrossRef - Serum Total Bilirubin Levels Provide Additive Risk Information over the Framingham Risk Score for Identifying Asymptomatic Diabetic Patients at Higher Risk for Coronary Artery Stenosis
Jaechan Leem, Eun Hee Koh, Jung Eun Jang, Chang-Yun Woo, Jin Sun Oh, Min Jung Lee, Joon-Won Kang, Tae-Hwan Lim, Chang Hee Jung, Woo Je Lee, Joong-Yeol Park, Ki-Up Lee
Diabetes & Metabolism Journal.2015; 39(5): 414. CrossRef - Association between serum gamma-glutamyltransferase and the progression of coronary artery calcification
Yun Kyung Cho, Yu Mi Kang, Jenie Yoonoo Hwang, Eun Hee Kim, Dong Hyun Yang, Joon-Won Kang, Joong-Yeol Park, Woo Je Lee, Hong-Kyu Kim, Chang Hee Jung
Atherosclerosis.2015; 243(1): 300. CrossRef - Role of Bilirubin in Diabetic Vascular Complications: Can Bilirubin Predict More than Just Liver Disease?
Jun Sung Moon
Diabetes & Metabolism Journal.2015; 39(5): 384. CrossRef - The Association of Rate of Weight Gain During Early Adulthood With the Prevalence of Subclinical Coronary Artery Disease in Recently Diagnosed Type 2 Diabetes: The MAXWEL-CAD Study
Soo Lim, Sung Hee Choi, Kyoung Min Kim, Sang Il Choi, Eun Ju Chun, Min Joo Kim, Kyong Soo Park, Hak Chul Jang, Naveed Sattar
Diabetes Care.2014; 37(9): 2491. CrossRef - Retraction: Diagnostic Accuracy of 64-Slice MDCT Coronary Angiography for the Assessment of Coronary Artery Disease in Korean Patients with Type 2 Diabetes
Jun Sung Moon, Ji Sung Yoon, Kyu Chang Won, Ihn-Ho Cho, Hyoung Woo Lee
Diabetes & Metabolism Journal.2013; 37(3): 217. CrossRef
- Can Radiation Dose Burden of CT Angiography be Reduced While Still Accurately Diagnosing Etiology of Acute Chest Pain?
- The Correlation Between Visceral Fat Distance Measured by Ultrasonography and Visceral Fat Amount by Computed Tomography in Type 2 Diabetes.
- Eui Dal Jung, Duck Soo Chung, Ji Yun Lee
- Korean Diabetes J. 2008;32(5):418-427. Published online October 1, 2008
- DOI: https://doi.org/10.4093/kdj.2008.32.5.418
- 2,058 View
- 20 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Visceral adipose tissue accumulation highly correlates with metabolic abnormalities and cardiovascular disease. Computed tomography (CT) is considered to be the standard method for visceral fat evaluation, but it is not used as a routine procedure. Ultrasonography (US) is a safe method, fairly inexpensive and widely available modality for measuring abdominal fat thickness. The aim of this study was to investigate the correlation between the intra-abdominal fat distance by US measurement and the visceral fat amount by CT and cardiovascular risk factors and to evaluate whether the intra-abdominal fat distance is better correlate with visceral fat amount by CT than other anthropometric parameters and to assess the cut-off value of intra-abdominal fat distance for visceral obesity in type 2 diabetic patients. METHODS: We obtained abdominal subcutaneous and intra-abdominal fat distance by using a high-resolution US (HDI 5000, ATL, Phillps, USA) at 1 cm above umbilical level in one hundred twenty-eight type 2 diabetic patients. CT scan (Light Speed plus, GE, USA) for the measurement of subcutaneous and intra-abdominal visceral fat area was also performed in the supine position at the L4-5 level. Lean body mass and % body fat were measured in a bioimpedance using DSM (Direct Segmental Measurement by 8-point electrode) method (InBody 3.0, Biospace, Seoul, Korea). We measured patient's height, weight, BMI (Body mass index), waist circumference, WHR(Waist-hip ratio) and blood pressure and also measured fasting blood glucose, HbA1c and lipid profiles. RESULTS: Abdominal subcutaneous and visceral fat distance measured by US is 2.05 +/- 0.52 cm, 4.43 +/- 1.54 cm, respectively. In pearson's correlations, visceral fat distance were correlated with BMI (r = 0.681, P < 0.001), waist circumference (r = 0.661, P < 0.001), WHR (r = 0.571, P < 0.001), triglyceride (r = 0.316, P < 0.001), HDL-cholesterol (r = -0.207, P < 0.004). US-determined visceral fat distance was also correlated with visceral fat amount by CT (r = 0.674, P < 0.001) and BMI (r = 0.610, P < 0.001), waist circumference (r = 0.626, P < 0.001), WHR (r = 0.557, P < 0.001). When we used waist circumference (men: 90 cm, women: 85 cm) as parameters for visceral obesity, the cutoff value of visceral fat distance, obtained by the receiver operating characteristic curve analysis, were 4.670 cm in men, 3.695 cm in women diabetic patients. CONCLUSION: Intra-abdominal fat distance measured by US reveals strongly correlated with visceral fat area, which is determined by CT and also well correlated with anthropometric parameters and lipid profiles. We suggest that US provided a better index compared to anthropometry for the prediction of visceral obesity and could be an alternative method for CT for visceral fat determination in diabetic patients. -
Citations
Citations to this article as recorded by- Aspects of transthoracic echocardiography protocol in obese patients
O. N. Dzhioeva, O. A. Maksimova, E. A. Rogozhkina, O. M. Drapkina
Russian Journal of Cardiology.2023; 27(12): 5243. CrossRef - Ultrasound-assisted assessment of visceral and subcutaneous adipose tissue thickness. Methodological guidelines
O. M. Drapkina, R. K. Angarsky, E. A. Rogozhkina, O. A. Maksimova, A. A. Ivanova, E. V. Zyatenkova, O. N. Dzhioeva
Cardiovascular Therapy and Prevention.2023; 22(3): 3552. CrossRef - The Correlations between Extremity Circumferences with Total and Regional Amounts of Skeletal Muscle and Muscle Strength in Obese Women with Type 2 Diabetes
Hwi Ryun Kwon, Kyung Ah Han, Hee Jung Ahn, Jae Hyuk Lee, Gang Seo Park, Kyung Wan Min
Diabetes & Metabolism Journal.2011; 35(4): 374. CrossRef - Small Rice Bowl-Based Meal Plan versus Food Exchange-Based Meal Plan for Weight, Glucose and Lipid Control in Obese Type 2 Diabetic Patients
Hee-Jung Ahn, Kyung-Ah Han, Hwi-Ryun Kwon, Bo-Kyung Koo, Hyun-Jin Kim, Kang-Seo Park, Kyung-Wan Min
Korean Diabetes Journal.2010; 34(2): 86. CrossRef
- Aspects of transthoracic echocardiography protocol in obese patients

 KDA
KDA
 First
First Prev
Prev





