
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Cardiovascular risk/Epidemiology
- Risk of Cardiovascular Disease according to Baseline Low-Density Lipoprotein Cholesterol Level in Different Age Groups in Korean Diabetes Population: A Cohort Study
- Tae Kyung Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
- Diabetes Metab J. 2024;48(2):265-278. Published online February 26, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0443
- 855 View
- 171 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
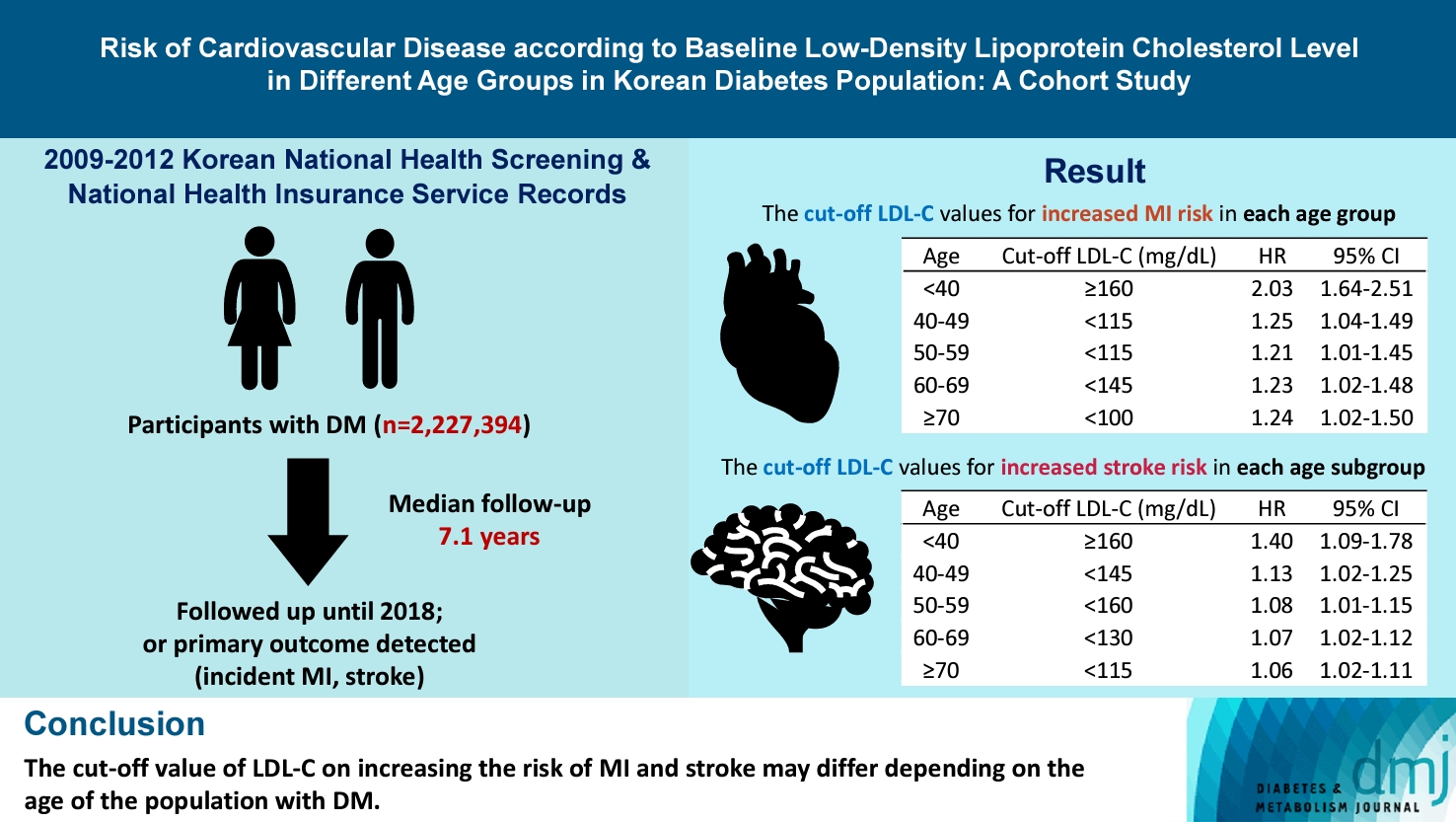
The association between low-density lipoprotein (LDL-C) levels and cardiovascular disease (CVD) risk in different age groups within the diabetes mellitus (DM) population remains unclear. The cohort study was conducted to investigate this relationship.
Methods
We assessed the 2009 to 2012 Korean National Health Screening and National Health Insurance Service records, with follow-up to the primary outcome (myocardial infarction [MI] or stroke) or December 2018. After excluding the participants with a history of MI or stroke, 2,227,394 participants with DM were included and categorized according to baseline LDL-C levels and age. Cox proportional hazards modeling was conducted. The CVD risk of age <40 years and LDL-C <70 mg/dL was set as the reference. In each age group, LDL-C <70 mg/dL was used as a reference for the subgroup analysis.
Results
The cut-off LDL-C value for increased MI risk in each age group varied (<40 years old, LDL-C ≥160 mg/dL: hazard ratios [HR], 2.03; 95% confidence interval [CI], 1.644 to 2.506) (40–49-year-old, LDL-C <115 mg/dL: HR, 1.245; 95% CI, 1.04 to 1.489) (50–59-year-old, LDL-C <115 mg/dL: HR, 1.21; 95% CI, 1.014 to 1.445) (60-69-year-old, LDL-C <145 mg/dL: HR, 1.229; 95% CI, 1.022 to 1.479) (≥70 years old group, LDL-C <100 mg/dL: HR, 1.238; 95% CI, 1.018 to 1.504). The cut-off LDL-C values for increased stroke risk varied in each age subgroup (<40 years old, LDL-C ≥160 mg/dL: HR, 1.395; 95% CI, 1.094 to 1.779) (40–49-year-old, LDL-C <145 mg/dL: HR, 1.13; 95% CI, 1.019 to 1.253) (50–59-year-old, LDL-C <160 mg/dL: HR, 1.079; 95% CI, 1.008 to 1.154) (60–69-year-old, LDL-C <130 mg/dL: HR, 1.07; 95% CI, 1.022 to 1.119) (≥70 years old, LDL-C <115 mg/dL: HR, 1.064; 95% CI, 1.019 to 1.112).
Conclusion
The effect of LDL-C on the risk of CVD differs depending on the age of the population with DM.
- Cardiovascular Risk/Epidemiology
- Comparison of on-Statin Lipid and Lipoprotein Levels for the Prediction of First Cardiovascular Event in Type 2 Diabetes Mellitus
- Ji Yoon Kim, Jimi Choi, Sin Gon Kim, Nam Hoon Kim
- Diabetes Metab J. 2023;47(6):837-845. Published online August 23, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0217
- 1,528 View
- 176 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
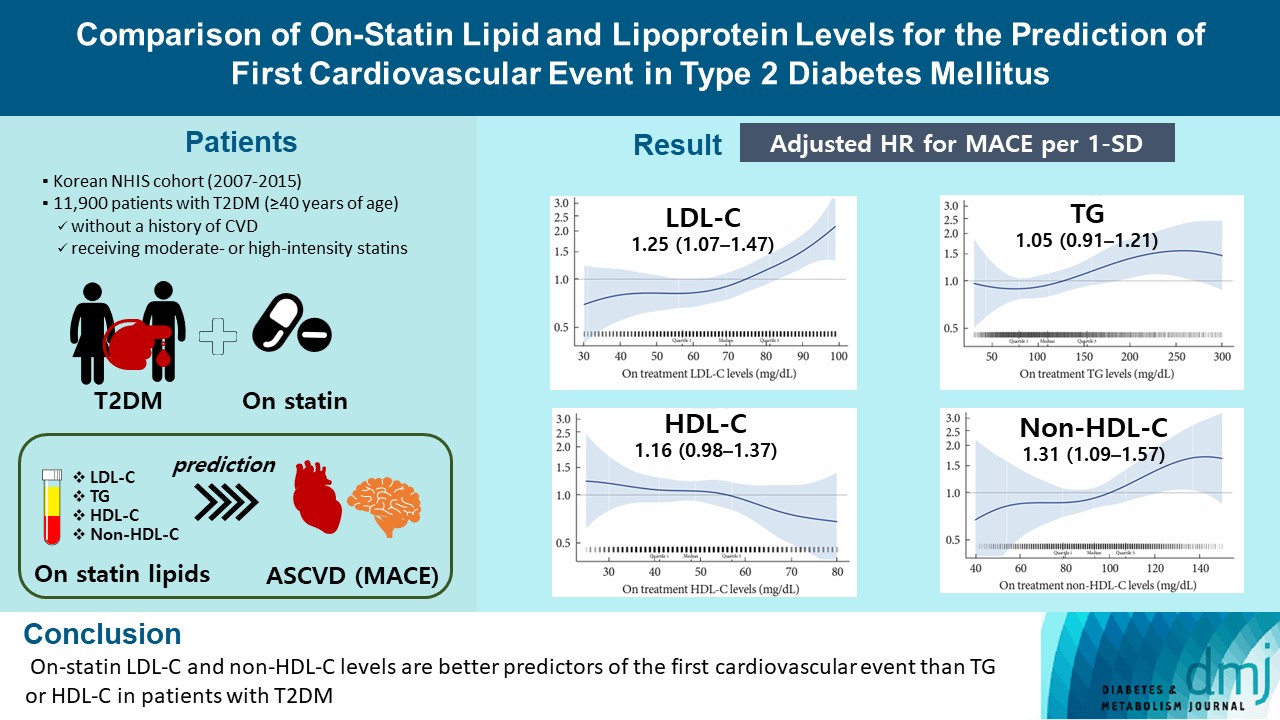
A substantial cardiovascular disease risk remains even after optimal statin therapy. Comparative predictiveness of major lipid and lipoprotein parameters for cardiovascular events in patients with type 2 diabetes mellitus (T2DM) who are treated with statins is not well documented.
Methods
From the Korean Nationwide Cohort, 11,900 patients with T2DM (≥40 years of age) without a history of cardiovascular disease and receiving moderate- or high-intensity statins were included. The primary outcome was the first occurrence of major adverse cardiovascular events (MACE) including ischemic heart disease, ischemic stroke, and cardiovascular death. The risk of MACE was estimated according to on-statin levels of low-density lipoprotein cholesterol (LDL-C), triglyceride (TG), highdensity lipoprotein cholesterol (HDL-C), and non-HDL-C.
Results
MACE occurred in 712 patients during a median follow-up period of 37.9 months (interquartile range, 21.7 to 54.9). Among patients achieving LDL-C levels less than 100 mg/dL, the hazard ratios for MACE per 1-standard deviation change in ontreatment values were 1.25 (95% confidence interval [CI], 1.07 to 1.47) for LDL-C, 1.31 (95% CI, 1.09 to 1.57) for non-HDL-C, 1.05 (95% CI, 0.91 to 1.21) for TG, and 1.16 (95% CI, 0.98 to 1.37) for HDL-C, after adjusting for potential confounders and lipid parameters mutually. The predictive ability of on-statin LDL-C and non-HDL-C for MACE was prominent in patients at high cardiovascular risk or those with LDL-C ≥70 mg/dL.
Conclusion
On-statin LDL-C and non-HDL-C levels are better predictors of the first cardiovascular event than TG or HDL-C in patients with T2DM.
- Cardiovascular Risk/Epidemiology
- Association between Low-Density Lipoprotein Cholesterol Level and Cardiovascular Outcomes in Korean Adults: A Nationwide Cohort Study
- Junghyun Noh, Min Kyong Moon, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong, on Behalf of the Committee of Practice Guideline of Korean Lipid and Atheroscelerosis
- Diabetes Metab J. 2023;47(1):59-71. Published online January 26, 2023
- DOI: https://doi.org/10.4093/dmj.2021.0320

- 2,816 View
- 226 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To validate the treatment target of low-density lipoprotein cholesterol (LDL-C) level according to the cardiovascular disease (CVD) risk which was recommended by Korean dyslipidemia guideline.
Methods
We used the Korean National Health Insurance Service database which included 3,958,048 people aged 20 to 89 years who underwent regular health screening. The primary outcome was incident CVD, defined as a composite of myocardial infarction and stroke during the follow-up period from 2009 to 2018.
Results
The risk of CVD increased from LDL-C level of 70 mg/dL in very high-risk and high-risk groups and from 130 mg/dL in moderate-risk and low-risk groups. Adjusted hazard ratios (HRs) of LDL-C ranges 70–99, 100–129, 130–159, 160–189, and ≥190 mg/dL were 1.20 (95% confidence interval [CI], 1.08–1.33), 1.27 (1.15–1.42), 1.39 (1.23–1.56), 1.69 (1.45–1.96), and 1.84 (1.49– 2.27) in very high-risk group, and 1.07 (1.02–1.13), 1.16 (1.10–1.21), 1.29 (1.22–1.36), 1.45 (1.36–1.55), and 1.73 (1.58–1.90) in high-risk group. Adjusted HRs (95% CI) of LDL-C ranges 130–159, 160–189, and ≥190 mg/dL were 1.15 (1.11–1.20), 1.28 (1.22– 1.34), and 1.45 (1.36–1.54) in moderate-risk group and 1.07 (1.02–1.13), 1.20 (1.13–1.26), and 1.47 (1.37–1.57) in low-risk group.
Conclusion
We confirmed the incidence of CVD was increased in higher LDL-C range. The risk of CVD increased from ≥70 mg/dL of LDL-C in very high-risk and high-risk groups, and from ≥130 mg/dL of LDL-C in moderate-risk and low-risk groups in Korean adults. -
Citations
Citations to this article as recorded by- Efficacy and Safety of a Single-Pill Triple Combination of Olmesartan, Amlodipine, and Rosuvastatin in Hypertensive Patients with Low-to-Moderate Cardiovascular Risk: A Multicenter, Randomized, Open-Label, Active-Control, Phase IV Clinical Trial
Byung Jin Kim, Kwang Soo Cha, Wook Hyun Cho, Eung Ju Kim, Seung-Hyuk Choi, Moo Hyun Kim, Sang-Hyun Kim, Jun-Bean Park, Seong-Mi Park, Il Suk Sohn, Kyu Hyung Ryu, In-Ho Chae
Journal of Cardiovascular Pharmacology and Therapeutics.2023;[Epub] CrossRef
- Efficacy and Safety of a Single-Pill Triple Combination of Olmesartan, Amlodipine, and Rosuvastatin in Hypertensive Patients with Low-to-Moderate Cardiovascular Risk: A Multicenter, Randomized, Open-Label, Active-Control, Phase IV Clinical Trial
- Guideline/Fact Sheet
- Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
- Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon, on Behalf of Committee of Clinical Practice Guideline, Korean Diabetes Association and Clinical Practice Guideline Committee, Korean Society of Lipid and Atherosclerosis
- Diabetes Metab J. 2023;47(1):1-9. Published online January 20, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0448
- 3,682 View
- 382 Download
- 3 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
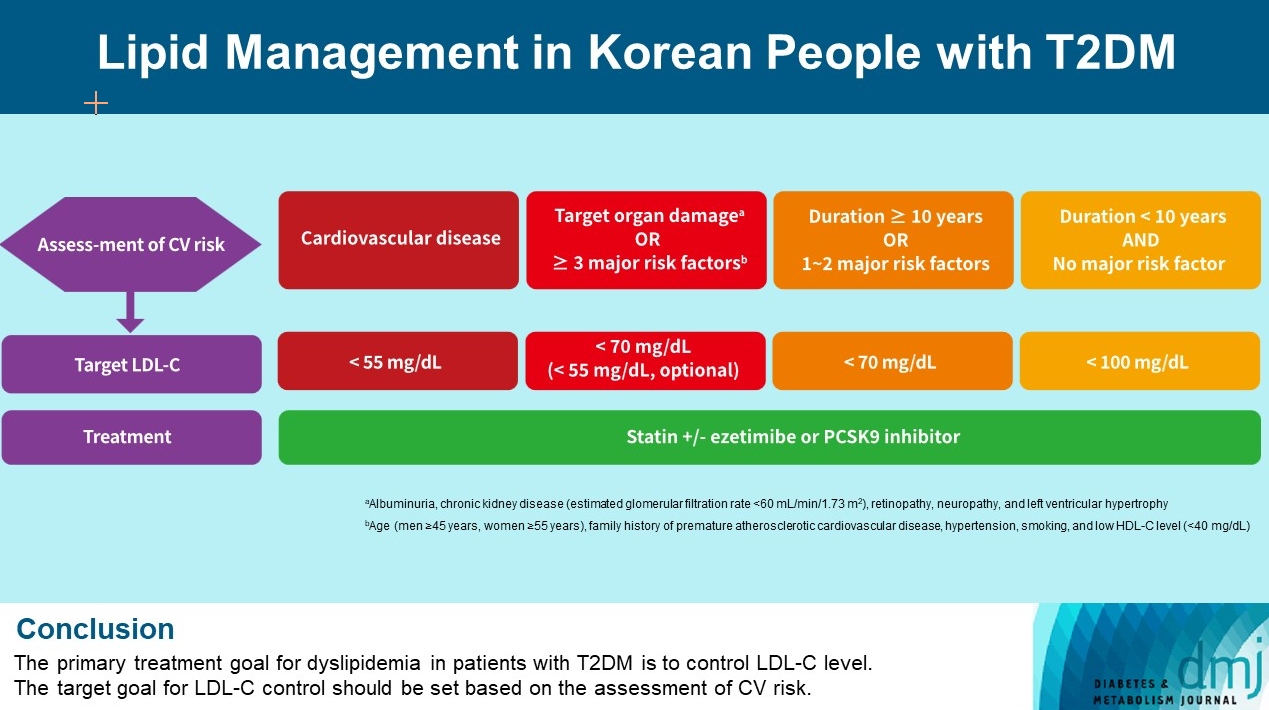
ePub - Dyslipidemia in patients with diabetes is an important treatment target as a modifiable risk factor for cardiovascular disease (CVD). Although the primary treatment goal for dyslipidemia is to control low-density lipoprotein cholesterol (LDL-C), achieving this goal remains suboptimal according to recent studies. It is important to set the target goal for LDL-C control based on an accurate risk assessment for CVD. Here, we summarize the latest evidence on lipid management in patients with diabetes and present a consensus of the Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis on the treatment goals of LDL-C according to the duration of diabetes, presence of CVD, target organ damage, or major cardiovascular risk factors. In patients with type 2 diabetes mellitus (T2DM) and CVD, an LDL-C goal of <55 mg/dL and a reduction in LDL-C level by 50% or more from the baseline is recommended. For the primary prevention of CVD in patients with T2DM with a duration of diabetes ≥10 years, major cardiovascular risk factors, or target organ damage, an LDL-C goal of <70 mg/dL is recommended. In patients with T2DM with a duration of diabetes <10 years and no major cardiovascular risk factors, an LDL-C goal of <100 mg/dL is recommended.
-
Citations
Citations to this article as recorded by- Associations of omega-3 fatty acids vs. fenofibrate with adverse cardiovascular outcomes in people with metabolic syndrome: propensity matched cohort study
Nam Hoon Kim, Ji Yoon Kim, Jimi Choi, Sin Gon Kim
European Heart Journal - Cardiovascular Pharmacotherapy.2024; 10(2): 118. CrossRef - Clinical Characteristics of Patients With Statin Discontinuation in Korea: A Nationwide Population-Based Study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Journal of Lipid and Atherosclerosis.2024; 13(1): 41. CrossRef - Role of Fenofibrate Use in Dyslipidemia and Related Comorbidities in the Asian Population: A Narrative Review
Chaicharn Deerochanawong, Sin Gon Kim, Yu-Cheng Chang
Diabetes & Metabolism Journal.2024; 48(2): 184. CrossRef - Dyslipidemia Fact Sheet in South Korea, 2022
Eun-Sun Jin, Jee-Seon Shim, Sung Eun Kim, Jae Hyun Bae, Shinae Kang, Jong Chul Won, Min-Jeong Shin, Heung Yong Jin, Jenny Moon, Hokyou Lee, Hyeon Chang Kim, In-Kyung Jeong
Diabetes & Metabolism Journal.2023; 47(5): 632. CrossRef - 2023 Clinical Practice Guidelines for Diabetes
Min Kyong Moon
The Journal of Korean Diabetes.2023; 24(3): 120. CrossRef - 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk Factors
Ye Seul Yang
The Journal of Korean Diabetes.2023; 24(3): 135. CrossRef - Dyslipidemia Fact Sheet in South Korea, 2022
Eun-Sun Jin, Jee-Seon Shim, Sung Eun Kim, Jae Hyun Bae, Shinae Kang, Jong Chul Won, Min-Jeong Shin, Heung Yong Jin, Jenny Moon, Hokyou Lee, Hyeon Chang Kim, In-Kyung Jeong
Journal of Lipid and Atherosclerosis.2023; 12(3): 237. CrossRef
- Associations of omega-3 fatty acids vs. fenofibrate with adverse cardiovascular outcomes in people with metabolic syndrome: propensity matched cohort study
- Cardiovascular Risk/Epidemiology
- Myocardial Infarction, Stroke, and All-Cause Mortality according to Low-Density Lipoprotein Cholesterol Level in the Elderly, a Nationwide Study
- You-Bin Lee, Minji Koo, Eunjin Noh, Soon Young Hwang, Jung A Kim, Eun Roh, So-hyeon Hong, Kyung Mook Choi, Sei Hyun Baik, Geum Joon Cho, Hye Jin Yoo
- Diabetes Metab J. 2022;46(5):722-732. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0225
- 7,097 View
- 332 Download
- 6 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We assessed the myocardial infarction (MI), stroke, and all-cause death risks during follow-up according to the low-density lipoprotein cholesterol (LDL-C) levels among older adults.
Methods
The Korean National Health Insurance Service datasets (2002 to 2020) were used for this population-based cohort study. The hazards of MI, stroke, and all-cause mortality during follow-up were analyzed according to LDL-C level in individuals aged ≥65 years without baseline cardiovascular diseases (n=1,391,616).
Results
During a mean 7.55 years, 52,753 MIs developed; 84,224 strokes occurred over a mean 7.47 years. After a mean 8.50 years, 233,963 died. A decrease in LDL-C was associated with lower hazards of MI and stroke. The decreased hazard of stroke in lower LDL-C was more pronounced in statin users, and individuals with diabetes or obesity. The hazard of all-cause death during follow-up showed an inverted J-shaped pattern according to the LDL-C levels. However, the paradoxically increased hazard of mortality during follow-up in lower LDL-C was attenuated in statin users and individuals with diabetes, hypertension, or obesity. In statin users, lower LDL-C was associated with a decreased hazard of mortality during follow-up.
Conclusion
Among the elderly, lower LDL-C was associated with decreased risks of MI and stroke. Lower LDL-C achieved by statins in the elderly was associated with a decreased risk of all-cause death during follow-up, suggesting that LDL-C paradox for the premature death risk in the elderly should not be applied to statin users. Intensive statin therapy should not be hesitated for older adults with cardiovascular risk factors including diabetes. -
Citations
Citations to this article as recorded by- Combination of low- or moderate-intensity statin and ezetimibe vs. high-intensity statin monotherapy on primary prevention of cardiovascular disease and all-cause death: a propensity-matched nationwide cohort study
Ji Eun Jun, In-Kyung Jeong, Kyu Jeong Ahn, Ho Yeon Chung, You-Cheol Hwang
European Journal of Preventive Cardiology.2024;[Epub] CrossRef - Associations of Low-density Lipoprotein Cholesterol With All-cause and Cause-specific Mortality in Older Adults in China
Wenqing Ni, Yuebin Lv, Xueli Yuan, Yan Zhang, Hongmin Zhang, Yijing Zheng, Xiaoming Shi, Jian Xu
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - The relationship of low-density lipoprotein cholesterol and all-cause or cardiovascular mortality in patients with type 2 diabetes: a retrospective study
Chin-Huan Chang, Shu-Tin Yeh, Seng-Wei Ooi, Chung-Yi Li, Hua-Fen Chen
PeerJ.2023; 11: e14609. CrossRef - ERCC1 polymorphism and its expression associated with ischemic stroke in Chinese population
Xiao-Dong Deng, Jian-Lin Ke, Tai-Yu Chen, Qin Gao, Zhuo-Lin Zhao, Wei Zhang, Huan Liu, Ming-Liang Xiang, Li-Zhen Wang, Ying Ma, Yun Liu
Frontiers in Neurology.2023;[Epub] CrossRef - New, Novel Lipid-Lowering Agents for Reducing Cardiovascular Risk: Beyond Statins
Kyuho Kim, Henry N. Ginsberg, Sung Hee Choi
Diabetes & Metabolism Journal.2022; 46(4): 517. CrossRef - Association between the Diabetes Drug Cost and Cardiovascular Events and Death in Korea: A National Health Insurance Service Database Analysis
Seung Min Chung, Ji-In Lee, Eugene Han, Hyun-Ae Seo, Eonju Jeon, Hye Soon Kim, Ji Sung Yoon
Endocrinology and Metabolism.2022; 37(5): 759. CrossRef
- Combination of low- or moderate-intensity statin and ezetimibe vs. high-intensity statin monotherapy on primary prevention of cardiovascular disease and all-cause death: a propensity-matched nationwide cohort study
- Metabolic Risk/Epidemiology
- Current Status of Low-Density Lipoprotein Cholesterol Target Achievement in Patients with Type 2 Diabetes Mellitus in Korea Compared with Recent Guidelines
- Soo Jin Yun, In-Kyung Jeong, Jin-Hye Cha, Juneyoung Lee, Ho Chan Cho, Sung Hee Choi, SungWan Chun, Hyun Jeong Jeon, Ho-Cheol Kang, Sang Soo Kim, Seung-Hyun Ko, Gwanpyo Koh, Su Kyoung Kwon, Jae Hyuk Lee, Min Kyong Moon, Junghyun Noh, Cheol-Young Park, Sungrae Kim
- Diabetes Metab J. 2022;46(3):464-475. Published online March 3, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0088
- 7,061 View
- 347 Download
- 4 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
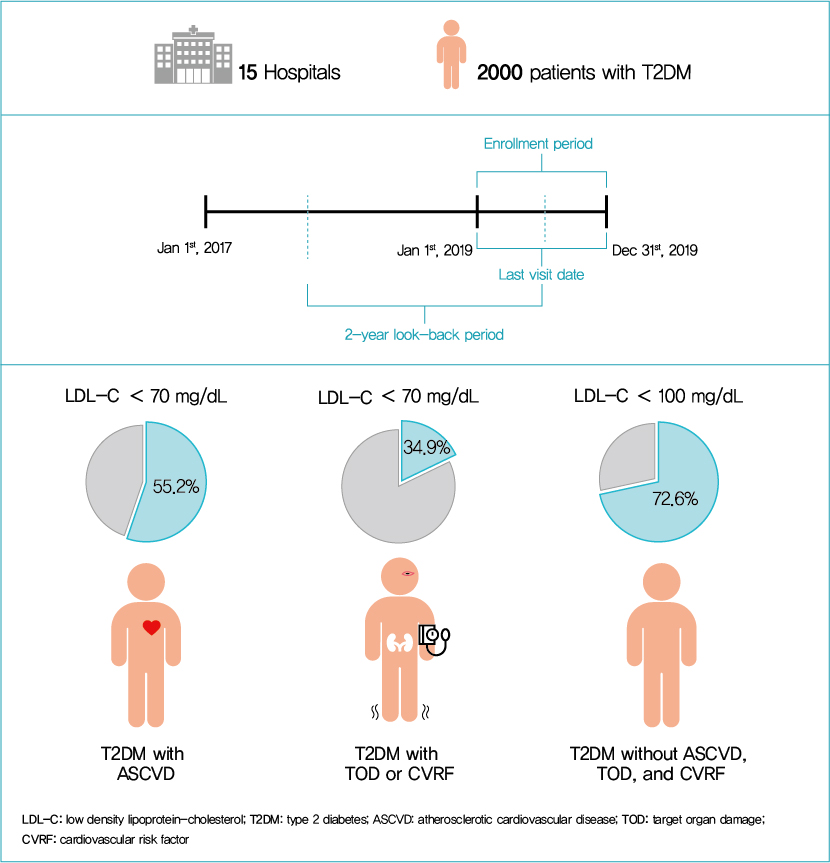
We evaluated the achievement of low-density lipoprotein cholesterol (LDL-C) targets in patients with type 2 diabetes mellitus (T2DM) according to up-to-date Korean Diabetes Association (KDA), European Society of Cardiology (ESC)/European Atherosclerosis Society (EAS), and American Diabetes Association (ADA) guidelines.
Methods
This retrospective cohort study collected electronic medical record data from patients with T2DM (≥20 years) managed by endocrinologists from 15 hospitals in Korea (January to December 2019). Patients were categorized according to guidelines to assess LDL-C target achievement. KDA (2019): Very High-I (atherosclerotic cardiovascular disease [ASCVD]) <70 mg/dL; Very High-II (target organ damage [TOD], or cardiovascular risk factors [CVRFs]) <70 mg/dL; high (others) <100 mg/dL. ESC/EAS (2019): Very High-I (ASCVD): <55 mg/dL; Very High-II (TOD or ≥3-CVRF) <55 mg/dL; high (diabetes ≥10 years without TOD plus any CVRF) <70 mg/dL; moderate (diabetes <10 years without CVRF) <100 mg/dL. ADA (2019): Very High-I (ASCVD); Very High-II (age ≥40+ TOD, or any CVRF), for high intensity statin or statin combined with ezetimibe.
Results
Among 2,000 T2DM patients (mean age 62.6 years; male 55.9%; mean glycosylated hemoglobin 7.2%) ASCVD prevalence was 24.7%. Of 1,455 (72.8%) patients treated with statins, 73.9% received monotherapy. According to KDA guidelines, LDL-C target achievement rates were 55.2% in Very High-I and 34.9% in Very High-II patients. With ESC/EAS guidelines, target attainment rates were 26.6% in Very High-I, 15.7% in Very High-II, and 25.9% in high risk patients. Based on ADA guidelines, most patients (78.9%) were very-high risk; however, only 15.5% received high-intensity statin or combination therapy.
Conclusion
According to current dyslipidemia management guidelines, LDL-C goal achievement remains suboptimal in Korean patients with T2DM. -
Citations
Citations to this article as recorded by- Risk factor control and cardiovascular events in patients with type 2 diabetes mellitus
Do Kyeong Song, Young Sun Hong, Yeon-Ah Sung, Hyejin Lee, Hidetaka Hamasaki
PLOS ONE.2024; 19(2): e0299035. CrossRef - Distinct effects of rosuvastatin and rosuvastatin/ezetimibe on senescence markers of CD8+ T cells in patients with type 2 diabetes mellitus: a randomized controlled trial
Sang-Hyeon Ju, Joung Youl Lim, Minchul Song, Ji Min Kim, Yea Eun Kang, Hyon-Seung Yi, Kyong Hye Joung, Ju Hee Lee, Hyun Jin Kim, Bon Jeong Ku
Frontiers in Endocrinology.2024;[Epub] CrossRef - Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - Association between carotid atherosclerosis and presence of intracranial atherosclerosis using three-dimensional high-resolution vessel wall magnetic resonance imaging in asymptomatic patients with type 2 diabetes
Ji Eun Jun, You-Cheol Hwang, Kyu Jeong Ahn, Ho Yeon Chung, Geon-Ho Jahng, Soonchan Park, In-Kyung Jeong, Chang-Woo Ryu
Diabetes Research and Clinical Practice.2022; 191: 110067. CrossRef
- Risk factor control and cardiovascular events in patients with type 2 diabetes mellitus
- Cardiovascular Risk/Epidemiology
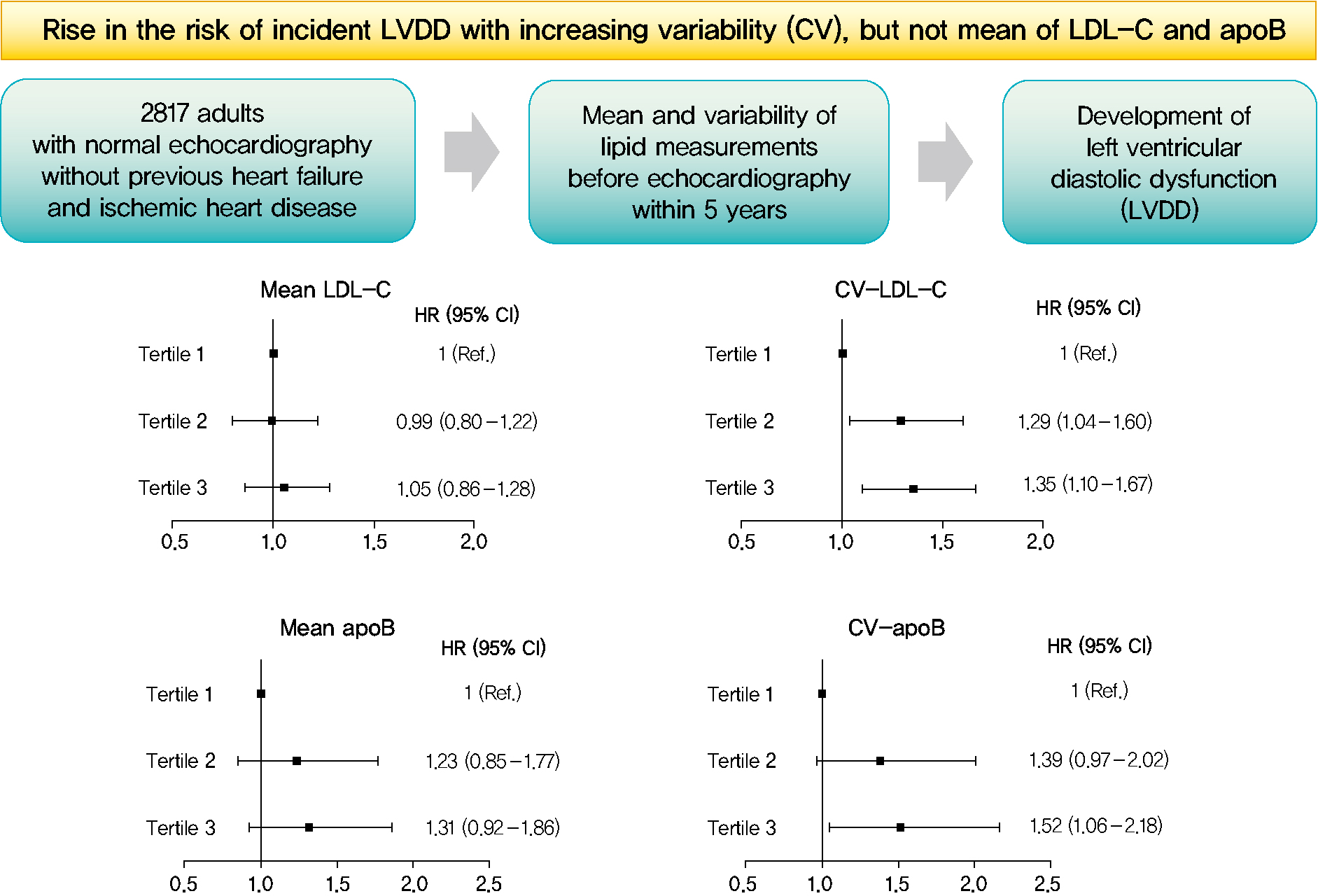
- Mean and Variability of Lipid Measurements and Risk for Development of Subclinical Left Ventricular Diastolic Dysfunction
- Jiyun Park, Mira Kang, Jiyeon Ahn, Min Young Kim, Min Sun Choi, You-Bin Lee, Gyuri Kim, Kyu Yeon Hur, Jae Hyeon Kim, Jeong Hoon Yang, Sang-Man Jin
- Diabetes Metab J. 2022;46(2):286-296. Published online November 22, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0080
- 5,716 View
- 196 Download
- 1 Web of Science
- 2 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 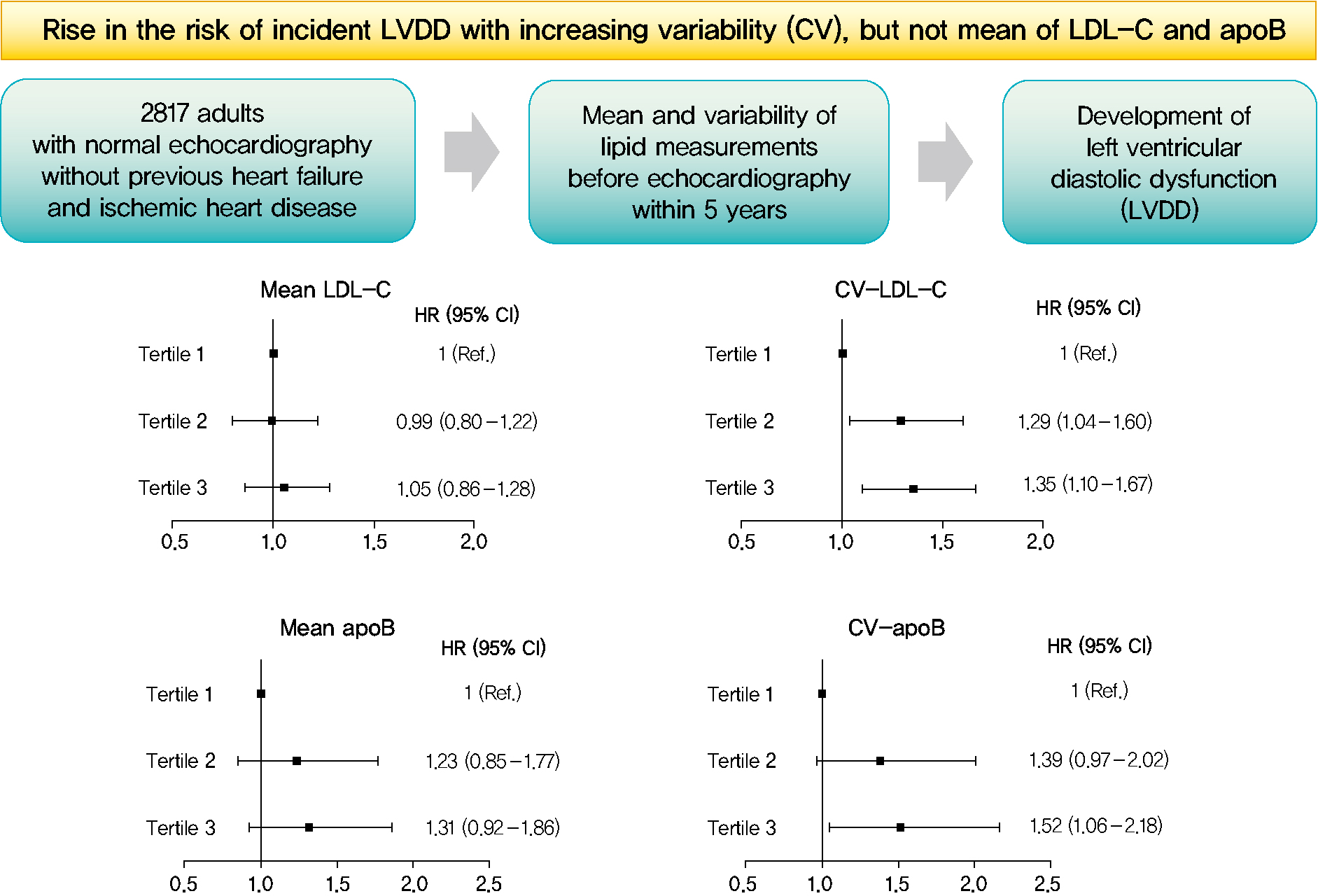
- Background
Subclinical left ventricular diastolic dysfunction (LVDD) is an emerging consequence of increased insulin resistance, and dyslipidemia is one of the few correctable risk factors of LVDD. This study evaluated the role of mean and visit-to-visit variability of lipid measurements in risk of LVDD in a healthy population.
Methods
This was a 3.7-year (interquartile range, 2.1 to 4.9) longitudinal cohort study including 2,817 adults (median age 55 years) with left ventricular ejection fraction >50% who underwent an annual or biannual health screening between January 2008 and July 2016. The mean, standard deviation (SD), coefficient of variation (CV), variability independent of the mean (VIM), and average real variability of total cholesterol, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), apolipoprotein B (apoB), non-HDL-C, and triglycerides were obtained from three to six measurements during the 5 years preceding the first echocardiogram.
Results
Among the 2,817 patients, 560 (19.9%) developed LVDD. The mean of no component of lipid measurements was associated with risk of LVDD. CV (hazard ratio [HR], 1.35; 95% confidence interval [CI], 1.10 to 1.67), SD (HR, 1.27; 95% CI, 1.03 to 1.57), and VIM (HR, 1.26; 95% CI, 1.03 to 1.55) of LDL-C and all the variability parameters of apoB were significantly associated with development of LVDD. The association between CV-LDL and risk of LVDD did not have significant interaction with sex, increasing/decreasing trend at baseline, or use of stain and/or lipid-modifying agents.
Conclusion
The variability of LDL-C and apoB, rather than their mean, was associated with risk for LVDD. -
Citations
Citations to this article as recorded by- Separate and Joint Associations of Remnant Cholesterol Accumulation and Variability With Carotid Atherosclerosis: A Prospective Cohort Study
Jinqi Wang, Rui Jin, Xiaohan Jin, Zhiyuan Wu, Haiping Zhang, Ze Han, Zongkai Xu, Yueruijing Liu, Xiaoyu Zhao, Xiuhua Guo, Lixin Tao
Journal of the American Heart Association.2023;[Epub] CrossRef - Variability of Metabolic Risk Factors: Causative Factor or Epiphenomenon?
Hye Jin Yoo
Diabetes & Metabolism Journal.2022; 46(2): 257. CrossRef
- Separate and Joint Associations of Remnant Cholesterol Accumulation and Variability With Carotid Atherosclerosis: A Prospective Cohort Study
- Statin Discontinuation after Achieving a Target Low Density Lipoprotein Cholesterol Level in Type 2 Diabetic Patients without Cardiovascular Disease: A Randomized Controlled Study
- Seung-Hwan Lee, Hyuk-Sang Kwon, Yong-Moon Park, Seung-Hyun Ko, Yoon-Hee Choi, Kun-Ho Yoon, Yu-Bae Ahn
- Diabetes Metab J. 2014;38(1):64-73. Published online February 19, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.1.64
- 3,955 View
- 48 Download
- 16 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background This study investigated the rate of relapse of dyslipidemia and the factors which could predict relapse following a short-term statin discontinuation after achieving a target low density lipoprotein cholesterol (LDL-C) level in type 2 diabetic patients without cardiovascular disease (CVD).
Methods Ninety-nine subjects on rosuvastatin treatment and whose LDL-C level was lower than 100 mg/dL were randomly assigned to discontinue or maintain statin treatment at a 2:1 ratio. The subjects were followed-up after 10 weeks. A relapse of dyslipidemia was defined as a reascent of LDL-C level to greater than 100 mg/dL.
Results The statin discontinuation group had a significant rate of relapse compared to the maintenance group (79% vs. 3%, respectively). Pretreatment and baseline lipid levels, their ratios, and hemoglobin A1c level were significantly different between the relapse and nonrelapse groups. The pretreatment and baseline lipid profiles and their ratios were independently associated with relapse. The pretreatment LDL-C level was the most useful parameter for predicting a relapse, with a cutoff of 123 mg/dL. During the follow-up period, no CVD event was noted.
Conclusion The relapse rate of dyslipidemia was high when statins were discontinued in type 2 diabetic patients without CVD. Statin discontinuation should be considered carefully based on the pretreatment lipid profiles of patients.
-
Citations
Citations to this article as recorded by- Cardiovascular Outcomes and Mortality Associated With Discontinuing Statins in Older Patients Receiving Polypharmacy
Federico Rea, Annalisa Biffi, Raffaella Ronco, Matteo Franchi, Simona Cammarota, Anna Citarella, Valeria Conti, Amelia Filippelli, Carmine Sellitto, Giovanni Corrao
JAMA Network Open.2021; 4(6): e2113186. CrossRef - Visit-to-visit variability of lipid measurements and the risk of myocardial infarction and all-cause mortality: A prospective cohort study
Xiaoxue Liu, Shouling Wu, Qiaofeng Song, Xizhu Wang
Atherosclerosis.2020; 312: 110. CrossRef - 2018 Guidelines for the management of dyslipidemia
Eun-Jung Rhee, Hyeon Chang Kim, Jae Hyeon Kim, Eun Young Lee, Byung Jin Kim, Eun Mi Kim, YoonJu Song, Jeong Hyun Lim, Hae Jin Kim, Seonghoon Choi, Min Kyong Moon, Jin Oh Na, Kwang-Yeol Park, Mi Sun Oh, Sang Youb Han, Junghyun Noh, Kyung Hee Yi, Sang-Hak L
The Korean Journal of Internal Medicine.2019; 34(4): 723. CrossRef - 2018 Guidelines for the Management of Dyslipidemia in Korea
Eun-Jung Rhee, Hyeon Chang Kim, Jae Hyeon Kim, Eun Young Lee, Byung Jin Kim, Eun Mi Kim, YoonJu Song, Jeong Hyun Lim, Hae Jin Kim, Seonghoon Choi, Min Kyong Moon, Jin Oh Na, Kwang-Yeol Park, Mi Sun Oh, Sang Youb Han, Junghyun Noh, Kyung Hee Yi, Sang-Hak L
Journal of Lipid and Atherosclerosis.2019; 8(2): 78. CrossRef - Patterns of statin use and long‐term adherence and persistence among older adults with diabetes
Richard Ofori‐Asenso, Jenni Ilomäki, Mark Tacey, Ella Zomer, Andrea J. Curtis, J. Simon Bell, Sophia Zoungas, Danny Liew
Journal of Diabetes.2018; 10(9): 699. CrossRef - Effect of visit-to-visit LDL-, HDL-, and non-HDL-cholesterol variability on mortality and cardiovascular outcomes after percutaneous coronary intervention
Eun Young Lee, Yeoree Yang, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Wook Sung Chung, Seung-Hwan Lee, Kiyuk Chang
Atherosclerosis.2018; 279: 1. CrossRef - Change in ALT levels after administration of HMG‐CoA reductase inhibitors to subjects with pretreatment levels three times the upper normal limit in clinical practice
Hyunah Kim, Hyeseon Lee, Tong Min Kim, So Jung Yang, Seo Yeon Baik, Seung‐Hwan Lee, Jae‐Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, In Young Choi, Kun‐Ho Yoon, Hun‐Sung Kim
Cardiovascular Therapeutics.2018;[Epub] CrossRef - Orthodox religious fasting as a medical nutrition therapy for dyslipidemia: where do we stand and how far can we go?
Theocharis Koufakis, Spyridon N Karras, Pantelis Zebekakis, Kalliopi Kotsa
European Journal of Clinical Nutrition.2018; 72(4): 474. CrossRef - Phenotyping of Korean patients with better-than-expected efficacy of moderate-intensity statins using tensor factorization
Jingyun Choi, Yejin Kim, Hun-Sung Kim, In Young Choi, Hwanjo Yu, Katriina Aalto-Setala
PLOS ONE.2018; 13(6): e0197518. CrossRef - Impact of educational outreach intervention on enhancing health care providers' knowledge about statin therapy prescribing in Malaysian patients with type 2 diabetes mellitus
Mohamed Hassan Elnaem, Mohamad Haniki Nik Mohamed, Hasniza Zaman Huri, Shah M Azarisman
Journal of Evaluation in Clinical Practice.2018; 24(3): 521. CrossRef - Use of Moderate‐Intensity Statins for Low‐Density Lipoprotein Cholesterol Level above 190 mg/dL at Baseline in Koreans
Hun‐Sung Kim, Hyeseon Lee, Sue Hyun Lee, Yoo Jin Jeong, Tong Min Kim, So Jung Yang, Sun Jung Baik, Hyunah Kim, Seung‐Hwan Lee, Jae Hyoung Cho, In‐Young Choi, Kun‐Ho Yoon, Ju Han Kim
Basic & Clinical Pharmacology & Toxicology.2017; 121(4): 272. CrossRef - Cholesterol variability and the risk of mortality, myocardial infarction, and stroke: a nationwide population-based study
Mee Kyoung Kim, Kyungdo Han, Hun-Sung Kim, Yong-Moon Park, Hyuk-Sang Kwon, Kun-Ho Yoon, Seung-Hwan Lee
European Heart Journal.2017; 38(48): 3560. CrossRef - Analysis and comparison of the cost-effectiveness of statins according to the baseline low-density lipoprotein cholesterol level in Korea
Y. J. Jeong, H. Kim, S. J. Baik, T. M. Kim, S. J. Yang, S.-H. Lee, J.-H. Cho, H. Lee, H. W. Yim, I. Y. Choi, K.-H. Yoon, H.-S. Kim
Journal of Clinical Pharmacy and Therapeutics.2017; 42(3): 292. CrossRef - The differences in the incidence of diabetes mellitus and prediabetes according to the type of HMG-CoA reductase inhibitors prescribed in Korean patients
Tong Min Kim, Hyunah Kim, Yoo Jin Jeong, Sun Jung Baik, So Jung Yang, Seung-Hwan Lee, Jae-Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, In Young Choi, Kun-Ho Yoon, Hun-Sung Kim
Pharmacoepidemiology and Drug Safety.2017; 26(10): 1156. CrossRef - Statin for the Primary Prevention of Cardiovascular Disease in Patients with Diabetes Mellitus
Bo Kyung Koo
Diabetes & Metabolism Journal.2014; 38(1): 32. CrossRef
- Cardiovascular Outcomes and Mortality Associated With Discontinuing Statins in Older Patients Receiving Polypharmacy
- Smaller Mean LDL Particle Size and Higher Proportion of Small Dense LDL in Korean Type 2 Diabetic Patients
- Sunghwan Suh, Hyung-Doo Park, Se Won Kim, Ji Cheol Bae, Alice Hyun-Kyung Tan, Hye Soo Chung, Kyu Yeon Hur, Jae Hyeon Kim, Kwang-Won Kim, Moon-Kyu Lee
- Diabetes Metab J. 2011;35(5):536-542. Published online October 31, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.5.536
- 4,715 View
- 39 Download
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Small dense low density lipoprotein (sdLDL) has recently emerged as an important risk factor of coronary heart disease.
Methods The mean LDL particle size was measured in 203 patients with type 2 diabetes mellitus (T2DM) and 212 matched subjects without diabetes using polyacrylamide tube gel electrophoresis. Major vascular complications were defined as stroke, angiographically-documented coronary artery disease or a myocardial infarction. Peripheral vascular stenosis, carotid artery stenosis (≥50% in diameter) or carotid artery plaque were considered minor vascular complications. Overall vascular complications included both major and minor vascular complications.
Results Diabetic patients had significantly smaller mean-LDL particle size (26.32 nm vs. 26.49 nm) and a higher percentage of sdLDL to total LDL compared to those of subjects without diabetes (21.39% vs. 6.34%). The independent predictors of sdLDL in this study were serum triglyceride level and body mass index (odds ratio [OR], 1.020 with
P <0.001 and OR 1.152 withP <0.027, respectively). However, no significant correlations were found between sdLDL and major vascular complications (P =0.342), minor vascular complications (P =0.573) or overall vascular complications (P =0.262) in diabetic subjects.Conclusion Diabetic patients had a smaller mean-LDL particle size and higher proportion of sdLDL compared to those of subjects without diabetes. Obese diabetic patients with hypertriglyceridemia have an increased risk for atherogenic small dense LDL. However, we could not verify an association between LDL particle size and vascular complications in this study.
-
Citations
Citations to this article as recorded by- Evaluation of measured and calculated small dense low-density lipoprotein in capillary blood and association with the metabolic syndrome
Sara Deza, Inmaculada Colina, Oscar Beloqui, José Ignacio Monreal, Estéfani Martínez-Chávez, Julia Maroto-García, Carmen Mugueta, Alvaro González, Nerea Varo
Clinica Chimica Acta.2024; 557: 117897. CrossRef - Association between measured or calculated small dense low‐density lipoprotein cholesterol and oxidized low‐density lipoprotein in subjects with or without type 2 diabetes mellitus
Hyun‐Ki Kim, Jinyoung Hong, Sunyoung Ahn, Woochang Lee, Sail Chun, Won‐Ki Min
Journal of Clinical Laboratory Analysis.2023;[Epub] CrossRef - The association of apolipoprotein in the risk of ST-elevation myocardial infarction in patients with documented coronary artery disease
Astuti Giantini, Nur Gifarani Pratiwi, Renan Sukmawan, Joedo Prihartono, Suzanna Immanuel, Merci Monica Pasaribu, Sri Suryo Adiyanti, Yusuf Bahasoan
International Journal of Cardiology Cardiovascular Risk and Prevention.2023; 18: 200194. CrossRef - Atherogenic Index of Plasma and Its Association with Risk Factors of Coronary Artery Disease and Nutrient Intake in Korean Adult Men: The 2013–2014 KNHANES
Hye Ran Shin, SuJin Song, Jin Ah Cho, Sun Yung Ly
Nutrients.2022; 14(5): 1071. CrossRef - The Atherogenic Index of Plasma: A Powerful and Reliable Predictor for Coronary Artery Disease in Patients With Type 2 Diabetes
Kuo Zhou, Zheng Qin, Jinfan Tian, Kongyong Cui, Yunfeng Yan, Shuzheng Lyu
Angiology.2021; 72(10): 934. CrossRef - Direct bilirubin is associated with low-density lipoprotein subfractions and particle size in overweight and centrally obese women
Y.-J. Kwon, H.-S. Lee, J.-W. Lee
Nutrition, Metabolism and Cardiovascular Diseases.2018; 28(10): 1021. CrossRef - Correlation between Cholesterol, Triglycerides, Calculated, and Measured Lipoproteins: Whether Calculated Small Density Lipoprotein Fraction Predicts Cardiovascular Risks
Sikandar Hayat Khan, Nadeem Fazal, Athar Abbas Gilani Shah, Syed Mohsin Manzoor, Naveed Asif, Aamir Ijaz, Najmusaqib Khan Niazi, Muhammad Yasir
Journal of Lipids.2017; 2017: 1. CrossRef - Effects of Small Dense LDL in Diabetic Nephropathy in Females with Type 2 Diabetes Mellitus
Seongyul Ryu, Youngwoo Kim, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Hyun Baek, Ki-Ho Song, Kyung-Jin Yun
Journal of Lipid and Atherosclerosis.2016; 5(1): 11. CrossRef - Prepregnancy Adverse Lipid Profile and Subsequent Risk of Gestational Diabetes
Emily S. Han, Ronald M. Krauss, Fei Xu, Sneha B. Sridhar, Assiamira Ferrara, Charles P. Quesenberry, Monique M. Hedderson
The Journal of Clinical Endocrinology & Metabolism.2016; 101(7): 2721. CrossRef - Meta-analysis of Atherogenic Index of Plasma and other lipid parameters in relation to risk of type 2 diabetes mellitus
Xiao-Wei Zhu, Fei-Yan Deng, Shu-Feng Lei
Primary Care Diabetes.2015; 9(1): 60. CrossRef - Higher levels of small dense low‐density lipoprotein (LDL) are associated with cardiac autonomic neuropathy in patients with Type 2 diabetes
E.‐H. Jang, Y.‐M. Park, J. Hur, M.‐K. Kim, S.‐H. Ko, K.‐H. Baek, K.‐H. Song, K.‐W. Lee, H.‐S. Kwon
Diabetic Medicine.2013; 30(6): 694. CrossRef - Sleep Status and Low-Density Lipoprotein Particle Size in a General Japanese Female Population: The Mima Study
Kazuhiko Kotani, Kokoro Tsuzaki, Shinji Fujiwara, Naoki Sakane
Medical Principles and Practice.2013; 22(5): 510. CrossRef - Serum small-dense LDL abnormalities in chronic renal disease patients
M. Chu, A. Y. M. Wang, I. H. S. Chan, S. H. Chui, C. W. K. Lam
British Journal of Biomedical Science.2012; 69(3): 99. CrossRef - Small Dense Low-density Lipoprotein and Cardiovascular Disease
Sunghwan Suh, Moon-Kyu Lee
Journal of Lipid and Atherosclerosis.2012; 1(1): 1. CrossRef
- Evaluation of measured and calculated small dense low-density lipoprotein in capillary blood and association with the metabolic syndrome
- Efficacy Evaluation of Atorvastatin in Korean Hyperlipidemic Patients with Type 2 Diabetes Mellitus.
- Dong Seop Choi, Duk Kyu Kim, Doo Man Kim, Seong Yeon Kim, Moon Suk Nam, Yong Soo Park, Ho Sang Shon, Chul Woo Ahn, Kwan Woo Lee, Ki Up Lee, Moon Kyu Lee, Choon Hee Chung, Bong Yeon Cha
- Korean Diabetes J. 2006;30(4):292-302. Published online July 1, 2006
- DOI: https://doi.org/10.4093/jkda.2006.30.4.292
- 2,090 View
- 20 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
NCEP ATP III Guideline recommends aggressive treatments of diabetic dyslipidemia, recognizing diabetes mellitus as CHD risk equivalents. This study was conducted to evaluate the effectiveness and safety of atorvastatin in hyperlipidemic patients with Type 2 diabetes mellitus through post-marketing drug use investigation of atorvastatin. METHODS: An open, multi-center, non-comparison, titrated dosage study was conducted in hyperlipidemic patients, who were treated with atorvastatin at first visiting hospitals from Mar. 2004 to Sep. 2004. 96 endocrinologists participated from 66 centers in this study. Total 2,182 hyperlipidemic patients were enrolled and 1,514 patients among them were accompanied by diabetes mellitus. Efficacy was evaluated at later than 4-week treatment by % change of total cholesterol, triglycerides, HDL-cholesterol and LDL-cholesterol from baseline. Percent of patients reaching LDL-cholesterol level less than 100 mg/dL was also analyzed. The adverse events incidence and abnormalities of clinical laboratory values were evaluated for safety monitoring. RESULTS: Total cholesterol, triglycerides, and LDL-cholesterol level were reduced by 26.6%, 12.0%, and 34.8%, respectively, in diabetic hyperlipidemic patients after atorvastatin treatment. The patients with LDL-cholesterol level of less than 100 mg/dL were increased from 2.8% to 52.6%. Atorvastatin was considered to be safe because adverse drug reactions were reported in 32 patients (1.5%) of total 2,182 patients. CONCLUSION: Atorvastatin was effective and safe in hyperlipidemic patients with type 2 diabetes mellitus. -
Citations
Citations to this article as recorded by- Response: A Retrospective Study on the Efficacy of a Ten-Milligram Dosage of Atorvastatin for Treatment of Hypercholesterolemia in Type 2 Diabetes Mellitus Patients (Korean Diabetes J 2010;34:359-67)
Dong Kyun Kim, Sa Rah Lee, Min Sik Kim, Suk Hyang Bae, Jin Yeon Hwang, Jung-Min Kim, Sung Hwan Suh, Hye-Jeong Lee, Mi Kyoung Park, Duk Kyu Kim
Diabetes & Metabolism Journal.2011; 35(1): 88. CrossRef - A Retrospective Study on the Efficacy of a Ten-Milligram Dosage of Atorvastatin for Treatment of Hypercholesterolemia in Type 2 Diabetes Mellitus Patients
Dong Kyun Kim, Sa Rah Lee, Min Sik Kim, Suk Hyang Bae, Jin Yeon Hwang, Jung-Min Kim, Sung Hwan Suh, Hye-Jeong Lee, Mi Kyoung Park, Duk Kyu Kim
Korean Diabetes Journal.2010; 34(6): 359. CrossRef - The Association of Plasma HDL-Cholesterol Level with Cardiovascular Disease Related Factors in Korean Type 2 Diabetic Patients
Hye Sook Hong, Jong Suk Park, Han Kyoung Ryu, Wha Young Kim
Korean Diabetes Journal.2008; 32(3): 215. CrossRef
- Response: A Retrospective Study on the Efficacy of a Ten-Milligram Dosage of Atorvastatin for Treatment of Hypercholesterolemia in Type 2 Diabetes Mellitus Patients (Korean Diabetes J 2010;34:359-67)
- The Relationship between Visceral & Subcutaneous Fat and Small Dense Low Density Lipoprotein Cholesterol Concentration in Type 2 Diabetic Patients.
- Wan Sub Shim, Soo Kyung Kim, Hae Jin Kim, Eun Seok Kang, Chul Woo Ahn, Sung Kil Lim, Hyun Chul Lee, Bong Soo Cha
- Korean Diabetes J. 2006;30(3):207-216. Published online May 1, 2006
- DOI: https://doi.org/10.4093/jkda.2006.30.3.207
- 2,109 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Visceral obesity is closely associated with cardiovascular disease (CVD). Small dense (sd) LDL is closely associated with CVD. The aim of this study was to evaluate the relationship between visceral and subcutaneous fat accumulation and sd LDL-C concentration. METHODS: 264 type 2 diabetic patients underwent ultrasonography to estimate visceral & subcutaneous fat accumulation and sd LDL-C concentrations were measured. RESULTS: BMI, total cholesterol, sd LDL-C concentration and percentage of sd LDL-C were higher in highest tertile of visceral fat length in male than those in lowest tertile. BMI, total cholesterol, triglyceride, LDL-C, sd LDL-C concentration and percentage of sd LDL-C were higher in highest tertile of visceral fat length in female than those in lowest tertile. But sd LDL-C concentration and percentage of sd LDL-C were not different among three groups based on the tertile of subcutaneous fat length in male and female. Visceral fat length was correlated with sd LDL-C concentration and percentage of sd LDL-C, total cholesterol, triglyceride, LDL-C, but negatively with percentage of large buoyant LDL-C and HDL-C after adjustment of age, sex and BMI. Subcutaneous fat length was not correlated with sd LDL-C and percentage of sd LDL-C, total cholesterol, triglyceride, HDL-C and LDL-C. CONCLUSION: The association between visceral fat length and sd LDL-C could be a factor that explains the association between visceral obesity and CVD.
- The Relationship between Metabolic Syndrome and Small Dense Low Density Lipoprotein-Cholesterol.
- Wan Sub Shim, Hae Jin Kim, Eun Seok Kang, Yu Mie Rhee, Chul Woo Ahn, Sung Kil Lim, Hyun Chul Lee, Bong Soo Cha
- Korean Diabetes J. 2005;29(6):548-556. Published online November 1, 2005
- 1,050 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Type 2 diabetes mellitus and metabolic syndrome (MS) are associated with the increased risk of cardiovascular disease and with characteristic dyslipidemia which is composed of high level of triglyceride, low level of HDL-C and increased small dense LDL (sd-LDL). Recently a simple method was established for the quantification of sd-LDL-C using heparin-magnesium precipitation. The aim of this study was to evaluate the relationship between the sd-LDL-C and the number of components of MS in type 2 diabetic patients. METHODS: 287 type 2 diabetic patients, who did not use the medication which can affect the concentration of lipid such as statin, fibrate, thiazolidinediones and corticosteroid, were enrolled. The NCEP-ATP III criteria of MS were used except obesity. RESULTS: Although LDL-C concentrations were not changed according to the number of components of MS, absolute level and percentage of sd-LDL-C were increased. Although LDL-C concentrations were not different between presence and absence of MS, in the case of MS, absolute level and percentage of sd-LDL-C were higher than not in the case of MS. Sd-LDL-C concentration was positively correlated with fasting plasma glucose, HbA1c, total cholesterol, triglyceride, LDL-C and percentage of sd-LDL-C, and negatively with HDL-C. The percentage of sd-LDL-C was positively correlated with total cholesterol, triglyceride and sd-LDL-C, and negatively with HDL-C. CONCLUSION: The sd-LDL-C may a factor that explains the higher risk of CVD in diabetic patients with the MS.
- Relationship of LDL Particle Size to IMT and Insulin Resistance in Non-Diabetic Adult.
- Jina Park, Chul Sik Kim, Jong Suk Park, Dol Mi Kim, Min Ho Cho, Jee Hyun Kong, Hai Jin Kim, Jeong Ho Kim, Chul Woo Ahn, Kyung Rae Kim, Bong Soo Cha, Sung Kil Lim, Hyun Chul Lee
- Korean Diabetes J. 2005;29(4):333-343. Published online July 1, 2005
- 1,028 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The aims of this study were to investigate the predictor of the low density lipoprotein(LDL) particle size and the relationship of the LDL particle size to the levels of insulin resistance and the carotid intima-media thickness (IMT) in healthy Koreans. METHODS: The subjects were 47 and 89 clinically healthy males and females, aged between 32 and 70years, without medications that could potentially alter glucose and lipid metabolisms. The mean LDL particle size was determined by polyacrylamide tube gel electrophoresis(Lipoprint(r) LDL, Quantimetrix), the insulin resistance using a short insulin tolerance test kit, and the subclinical atherosclerosis from the carotid intima-media thickness. RESULTS: The LDL particle size was found to be significantly correlated with insulin resistance using a simple Pearson's correlation(r=0.233, P<0.01), but the independent predictors of the LDL particle size, as determined by a multiple stepwise regression analysis, were serum triglyceride(TG), high density lipoprotein(HDL) cholesterol level and age(beta=-0.403, P=< 0.001; beta=0.309, P=0.003; beta=-0.219, P=0.016, respectively). Significant relationships were found between an increasing IMT and the traditional risk factors of atherosclerosis: age, LDL cholesterol, HDL cholesterol, systolic and diastolic blood pressure(r=0.490, P<0.001; r=-0.251, P<0.01; r=0.211, P<0.05; r=0.298, P<0.01; r=0.263, P<0.01, respectively). However, no significant correlation was found between an increasing IMT and the LDL particle size (r=-0.172, P=0.075). CONCLUSION: The best predictors for the LDL particle size were the serum TG level, HDL cholesterol level and age. Insulin resistance was not found to be an independent predictor of the LDL particle size. Small dense LDL was not found to be a predictor of the IMT in healthy Koreans.
- Effect of Oxidized LDL on the Amount of Insulin Receptor and Gi-proteins in the Caveolae of Bovine Aortic Endothelial Cells (BAEC).
- Sung Yoon Jeon, Hyun Shik Son, Jung Min Lee, Sung Dae Moon, Kun Ho Yoon, Bong Yun Cha, Kwang Woo Lee, Ho Young Son, Sung Koo Kang
- Korean Diabetes J. 2001;25(1):71-82. Published online February 1, 2001
- 1,143 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
AND AIMS: Oxidized LDL (ox-LDL) may induce endothelial cell dysfunction and suggested to have an association with atherosclerosis or insulin resistance. Several studies have shown that ox-LDL inhibits signaling pathways mediated by inhibitory GTP-binding proteins (Gi-proteins). G-protein coupled receptors (GPCRs) can be internalized via caveolae. Caveolae are small flask-shaped invaginations of the plasma membrane, characterized by high levels of cholesterol and glycosphingolipids and also by the presence of caveolin, a 20-24 kDa integral membrane protein. G-proteins are enriched within caveolae membranes, where caveolin-1 directly interacts with the -subunits of G-proteins. It is reported that functional changes of G-proteins such as mutational or pharmacological activation of G-proteins affect direct interaction between G-proteins and caveolin-1. Thus, we investigated the effect of ox-LDL on the change of the amount of insulin receptor and Gi proteins in the caveolae. MATERIALS AND METHODS: ox-LDL was prepared by exposing samples of native LDL (n-LDL) to CuSO4 for 24 hours. Caveolae were extracted after treating BAECs at several concentrations of ox-LDL (10, 50, 100 g/mL) for various durations (0-48 hr), and we investigated the changes of the amount of caveolin-1, Gi -proteins and insulin receptor using immunoblot. RESULTS: While the amount of caveolin-1 was decreased, the amount of insulin receptor, Gi 2 and Gi 3 proteins in caveolae were also decreased after treatment of ox-LDL on the BAECs (insulin receptor: 66%; Gi 2 protein: 33%; Gi 3 protein: 66%, p<0.05). The amount of caveolin-1 was increased for the first 6 hours and then decreased, however, the amount of Gi -proteins and insulin receptor were vice versa during 48 hours incubation. CONCLUSION: These results indicate that ox-LDL can affect the change of the amount of insulin receptor and Gi-proteins in caveolae and it may induce endothelial cell dysfunction.
- The Effect of Micronized Fenofibrate on the Plasma Levels of Glycated LDL-C, Lp(a) and Insulin Resistance in Patients with Type 2 Diabetes Mellitus.
- Mi Kyoung Park, Duk Kyu Kim
- Korean Diabetes J. 2000;24(6):678-688. Published online January 1, 2001
- 839 View
- 21 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
It has been indicated that micronized fenofibrate therapy changes the atherogenic lipid profile into more favorable lipid profile in patients with type 2 diabetes and dyslipidemia. The aim of this study is to evaluate the effect of micronized fenofibrate on the plasma levels of glycated LDL-C, Lp(a), FFA and insulin resistance in patients with type 2 diabetes and dyslipidemia. METHODS: Forty-seven patients with type 2 diabetes (M/F=23/24, mean age 57 +/- 7 yrs) were studied who had relatively good glycemic index (HbA1c < 8.0%) but dyslipidemia (i.e., dyslipidemia : TG >2.25 mmol/L or HDL-C < 0.90 mmol/L or LDL-C >3.36 mmol/L). All the patients were maintained by the previous method of glucose control without change during entire period of the study. The patients were randomized to drug group (Lipidil ) or placebo group for 12 weeks and measured for fasting plasma levels of lipid, glycated LDL-C, Lp(a), insulin, C-peptide, glucose. The results were compared before and after the administration. RESULTS: Micronized fenofibrate therapy significantly reduced the plasma levels of triglyceride, total cholesterol, LDL-C, TC/HDL-C (p<0.0001), FFA (p<0.05) and ele vated the level of HDL-C (p<0.0001) after 12 weeks administration. However, no significant(-3.6%) changes were observed in the level of Lp(a) . In both groups, the plasma levels of glycated LDL-C were elevated even though the glycemic controls were good (drug group: 0.09+/-0.05 mmol/L, placebo group: 0.10+/-0.03 mmol/L), but no significant changes were noticed after administration for 12 weeks (-13.5%, +4.8%, respectively). HOMA-IR index was significantly decreased in the drug group after administration (p<0.01). The change of plasma insulin level was significantly different when compared to that of the placebo group (p<0.05). The plasma level of C-peptide and glycemic indexes (FBS and HbA1c) were not changed significant. CONCLUSION: Micronized fenofibrate therapy for 12 weeks was very effective for control of diabetic dyslipidemia. It significantly reduced FFA to improve the insulin resistance, but it didn't improve the elevated plasma level of glycated LDL-C and Lp(a).

 KDA
KDA
 First
First Prev
Prev





