
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Metabolic Risk/Epidemiology
- Temporal Changes in Resting Heart Rate and Risk of Diabetes Mellitus
- Mi Kyoung Son, Kyoungho Lee, Hyun-Young Park
- Received August 29, 2023 Accepted November 13, 2023 Published online February 2, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0305 [Epub ahead of print]

- 671 View
- 47 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To investigate the association between the time-varying resting heart rate (RHR) and change in RHR (∆RHR) over time and the risk of diabetes mellitus (DM) by sex.
Methods
We assessed 8,392 participants without DM or atrial fibrillation/flutter from the Korean Genome and Epidemiology Study, a community-based prospective cohort study that was initiated in 2001 to 2002. The participants were followed up until December 31, 2018. Updating RHR with biennial in-study re-examinations, the time-varying ∆RHR was calculated by assessing the ∆RHR at the next follow-up visit.
Results
Over a median follow-up of 12.3 years, 1,345 participants (16.2%) had DM. As compared with RHR of 60 to 69 bpm, for RHR of ≥80 bpm, the incidence of DM was significantly increased for both male and female. A drop of ≥5 bpm in ∆RHR when compared with the stable ∆RHR group (–5< ∆RHR <5 bpm) was associated significantly with lower risk of DM in both male and female. However, an increase of ≥5 bpm in ∆RHR was significantly associated with higher risk of DM only in female, not in male (hazard ratio for male, 1.057 [95% confidence interval, 0.869 to 1.285]; and for female, 1.218 [95% confidence interval, 1.008 to 1.471]).
Conclusion
In this community-based longitudinal cohort study, a reduction in ∆RHR was associated with a decreased risk of DM, while an increase in ∆RHR was associated with an increased risk of DM only in female.
- Complications
- Effect of the Glucagon-Like Peptide-1 Receptor Agonists on Autonomic Function in Subjects with Diabetes: A Systematic Review and Meta-Analysis
- Carla Greco, Daniele Santi, Giulia Brigante, Chiara Pacchioni, Manuela Simoni
- Diabetes Metab J. 2022;46(6):901-911. Published online April 12, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0314
- 4,581 View
- 267 Download
- 6 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
In addition to the metabolic effects in diabetes, glucagon-like peptide 1 receptor (GLP-1R) agonists lead to a small but substantial increase in heart rate (HR). However, the GLP-1R actions on the autonomic nervous system (ANS) in diabetes remain debated. Therefore, this meta-analysis evaluates the effect of GLP-1R agonist on measures of ANS function in diabetes.
Methods
According to the Cochrane Collaboration and Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement, we conducted a meta-analysis considering clinical trials in which the autonomic function was evaluated in diabetic subjects chronically treated with GLP-1R agonists. The outcomes were the change of ANS function measured by heart rate variability (HRV) and cardiac autonomic reflex tests (CARTs).
Results
In the studies enrolled, HR significantly increased after treatment (P<0.001), whereas low frequency/high frequency ratio did not differ (P=0.410); no changes in other measures of HRV were detected. Considering CARTs, only the 30:15 value derived from lying-to-standing test was significantly lower after treatment (P=0.002), but only two studies reported this measurement. No differences in other CARTs outcome were observed.
Conclusion
The meta-analysis confirms the HR increase but seems to exclude an alteration of the sympatho-vagal balance due to chronic treatment with GLP-1R agonists in diabetes, considering the available measures of ANS function. -
Citations
Citations to this article as recorded by- Liraglutide does not increase heart rate of diabetic patients during acute myocardial infarction
Qianyi Li, Chunxuan Wu, Shiqun Sun, Lingchao Yang, Yanyan Li, Yixin Niu, Li Zhang, Wei Li, Ying Yu
Journal of Diabetes.2024;[Epub] CrossRef - A randomized, double‐blind trial assessing the efficacy and safety of two doses of dulaglutide in Japanese participants with type 2 diabetes (AWARD‐JPN)
Tomoaki Morioka, Masakazu Takeuchi, Akichika Ozeki, Masanori Emoto
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Hormonal Gut–Brain Signaling for the Treatment of Obesity
Eun Roh, Kyung Mook Choi
International Journal of Molecular Sciences.2023; 24(4): 3384. CrossRef - Effects of new hypoglycemic drugs on cardiac remodeling: a systematic review and network meta-analysis
Yi-lin Huang, Xiao-zhuo Xu, Jing Liu, Pin-yao Wang, Xue-li Wang, Hong-lin Feng, Cheng-jiang Liu, Xu Han
BMC Cardiovascular Disorders.2023;[Epub] CrossRef - Obesity and hypertension: Obesity medicine association (OMA) clinical practice statement (CPS) 2023
Tiffany Lowe Clayton, Angela Fitch, Harold Edward Bays
Obesity Pillars.2023; 8: 100083. CrossRef - Incretins and microvascular complications of diabetes: neuropathy, nephropathy, retinopathy and microangiopathy
Jonathan Goldney, Jack A. Sargeant, Melanie J. Davies
Diabetologia.2023; 66(10): 1832. CrossRef - Diabetes-Induced Cardiac Autonomic Neuropathy: Impact on Heart Function and Prognosis
Susumu Z. Sudo, Tadeu L. Montagnoli, Bruna de S. Rocha, Aimeé D. Santos, Mauro P. L. de Sá, Gisele Zapata-Sudo
Biomedicines.2022; 10(12): 3258. CrossRef
- Liraglutide does not increase heart rate of diabetic patients during acute myocardial infarction
- Cardiovascular Risk/Epidemiology
- Association between Variability of Metabolic Risk Factors and Cardiometabolic Outcomes
- Min Jeong Park, Kyung Mook Choi
- Diabetes Metab J. 2022;46(1):49-62. Published online January 27, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0316
- 5,753 View
- 222 Download
- 5 Web of Science
- 7 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 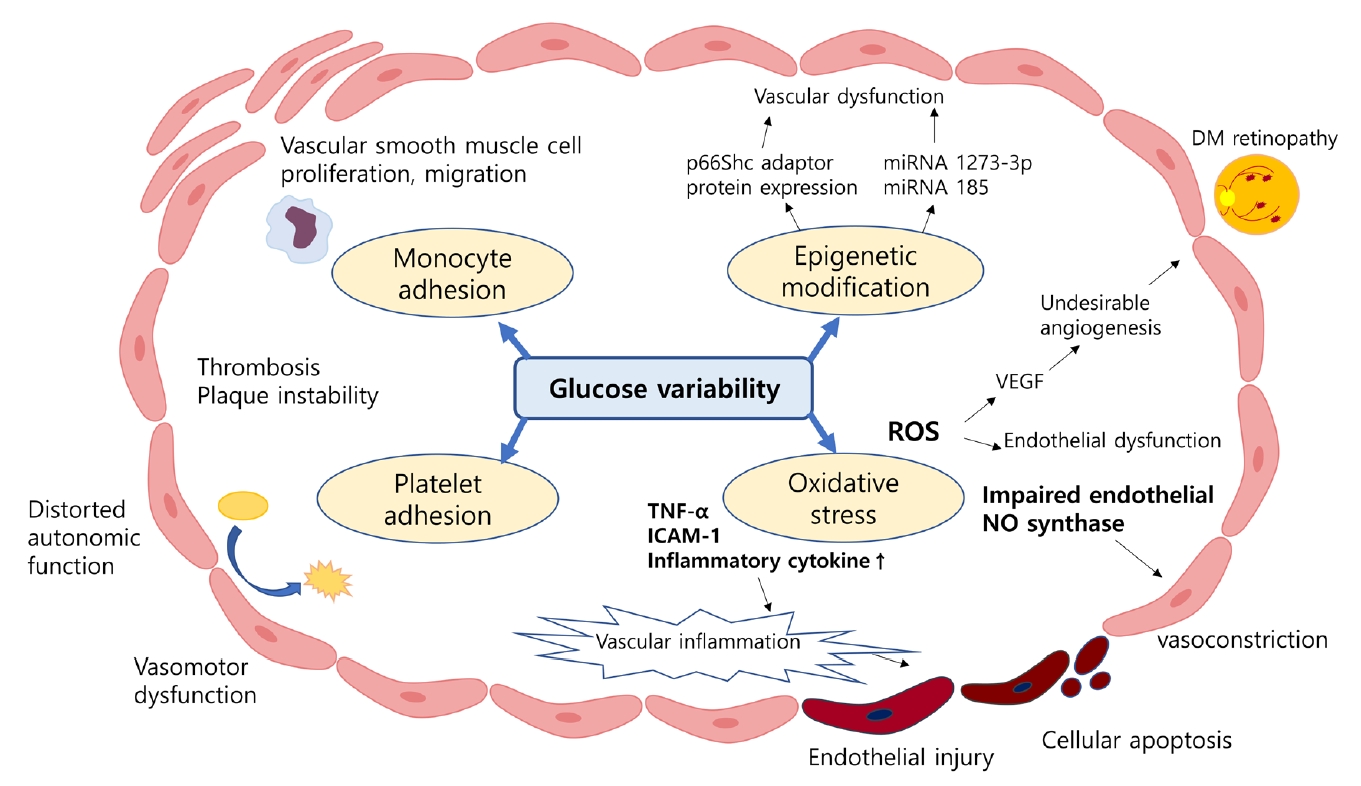
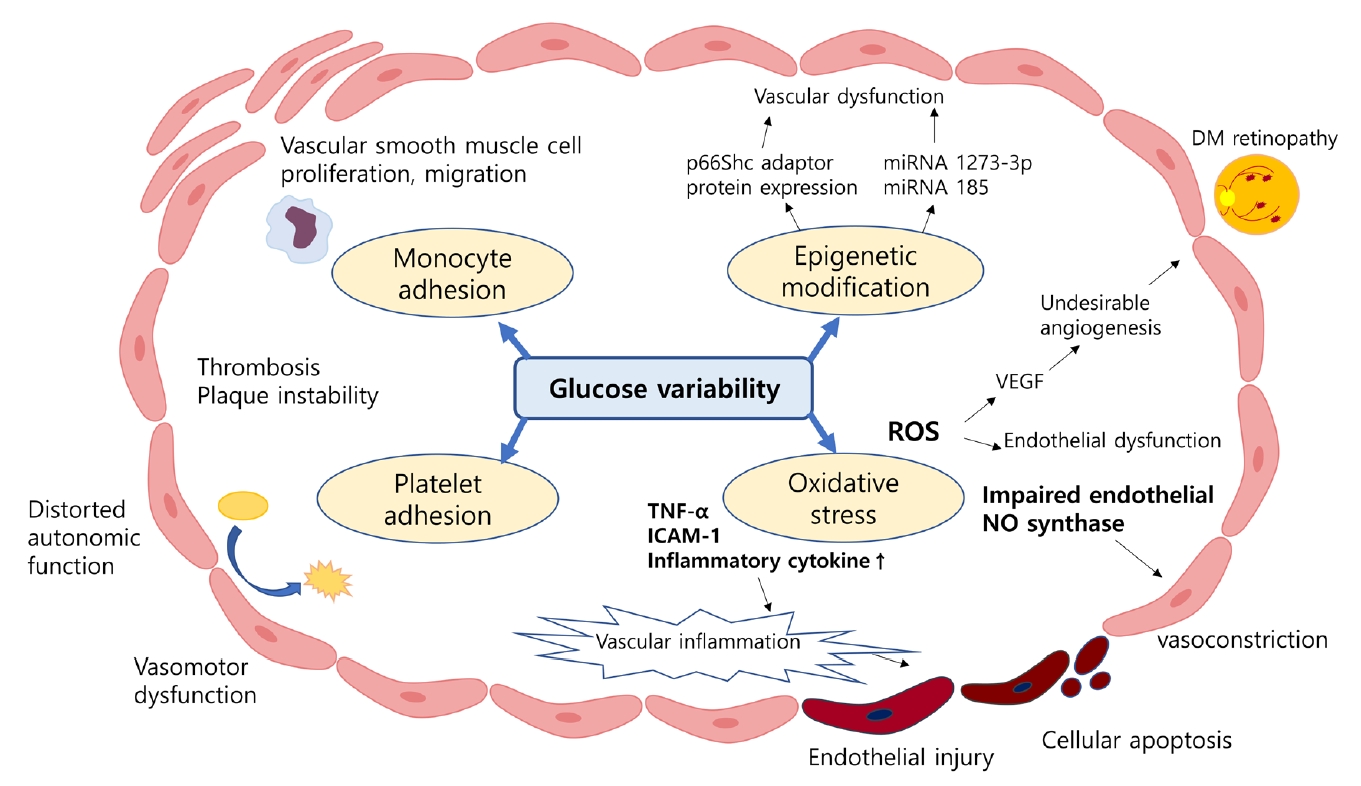
- Despite strenuous efforts to reduce cardiovascular disease (CVD) risk by improving cardiometabolic risk factors, such as glucose and cholesterol levels, and blood pressure, there is still residual risk even in patients reaching treatment targets. Recently, researchers have begun to focus on the variability of metabolic variables to remove residual risks. Several clinical trials and cohort studies have reported a relationship between the variability of metabolic parameters and CVDs. Herein, we review the literature regarding the effect of metabolic factor variability and CVD risk, and describe possible mechanisms and potential treatment perspectives for reducing cardiometabolic risk factor variability.
-
Citations
Citations to this article as recorded by- Long-term variability in physiological measures in relation to mortality and epigenetic aging: prospective studies in the USA and China
Hui Chen, Tianjing Zhou, Shaowei Wu, Yaying Cao, Geng Zong, Changzheng Yuan
BMC Medicine.2023;[Epub] CrossRef - Dose–response relationship between physical activity and cardiometabolic risk in obese children and adolescents: A pre-post quasi-experimental study
Zekai Chen, Lin Zhu
Frontiers in Physiology.2023;[Epub] CrossRef - Association of body weight change with all-cause and cause-specific mortality: A nationwide population-based study
So Yoon Kwon, Gyuri Kim, Jungkuk Lee, Jiyun Park, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Diabetes Research and Clinical Practice.2023; 199: 110666. CrossRef - Association between lipid variability and the risk of mortality in cancer patients not receiving lipid-lowering agents
Seohyun Kim, Gyuri Kim, So Hyun Cho, Rosa Oh, Ji Yoon Kim, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Frontiers in Oncology.2023;[Epub] CrossRef - Association between visit-to-visit lipid variability and risk of ischemic heart disease: a cohort study in China
Yonghao Wu, Peng Shen, Lisha Xu, Zongming Yang, Yexiang Sun, Luhua Yu, Zhanghang Zhu, Tiezheng Li, Dan Luo, Hongbo Lin, Liming Shui, Mengling Tang, Mingjuan Jin, Kun Chen, Jianbing Wang
Endocrine.2023;[Epub] CrossRef - Variability of Metabolic Risk Factors: Causative Factor or Epiphenomenon?
Hye Jin Yoo
Diabetes & Metabolism Journal.2022; 46(2): 257. CrossRef - Long-Term Variability in Physiological Measures in Relation to Mortality and Epigenetic Aging: Prospective Studies in the US and China
Hui Chen, Tianjing Zhou, Shaowei Wu, Yaying Cao, Geng Zong, Changzheng Yuan
SSRN Electronic Journal .2022;[Epub] CrossRef
- Long-term variability in physiological measures in relation to mortality and epigenetic aging: prospective studies in the USA and China
- Clinical Diabetes & Therapeutics
- Effects of High-Dose α-Lipoic Acid on Heart Rate Variability of Type 2 Diabetes Mellitus Patients with Cardiac Autonomic Neuropathy in Korea
- Sol Jae Lee, Su Jin Jeong, Yu Chang Lee, Yong Hoon Lee, Jung Eun Lee, Chong Hwa Kim, Kyung Wan Min, Bong Yun Cha
- Diabetes Metab J. 2017;41(4):275-283. Published online July 6, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.4.275
- 4,967 View
- 69 Download
- 18 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Diabetic cardiac autonomic neuropathy (CAN) is one of the important complications of diabetes. It is characterized by reduced heart rate variability (HRV).
Methods In this randomized, double-blind, placebo-controlled, multicenter trial, 75 patients were randomly assigned to one of two groups. One group (
n =41) received α-lipoic acid (ALA) at an oral dose of 600 mg/day for the first 12 weeks and then 1,200 mg/day for the next 12 weeks. The other group (n =34) received placebo treatment for 24 weeks. CAN was assessed by measuring HRVs in people with diabetes.Results Most of the baseline measures for HRVs were similar between the ALA and placebo groups. Although there were no statistically significant HRV changes in the ALA group compared to the placebo group after 24 weeks of trial, we found a positive tendency in some of the HRV parameters of the ALA group. The standard deviations of normal-to-normal RR intervals in the standing position increased by 1.87 ms in the ALA group but decreased by −3.97 ms in the placebo group (
P =0.06). The power spectrum of the low frequency (LF) band in the standing position increased by 15.77 ms2 in the ALA group, whereas it declined by −15.04 ms2 in the placebo group (P =0.08). The high frequency/LF ratio in the upright position increased by 0.35 in the ALA group, whereas it declined by −0.42 in the placebo group (P =0.06). There were no differences between the two groups regarding rates of adverse events.Conclusion Although a slight improvement tendency was seen in HRV in the ALA group, there were no statistically significant HRV changes in the ALA group compared to the placebo group after 24 weeks of trial. However, the high oral dose of ALA was well-tolerated.
-
Citations
Citations to this article as recorded by- Effect of Ramipril on Cardiac Autonomic Neuropathy in Patients With Type II Diabetes Mellitus
Chaitali A Chindhalore, Ganesh N Dakhale, Prathamesh H Kamble, Bharatsing D Rathod, Sunita Kumbhalkar, Mrunal S Phatak
Cureus.2023;[Epub] CrossRef - Evaluating treatment options for cardiovascular autonomic neuropathy in patients with diabetes mellitus: a systematic review
Jasmine KaiLi Goh, Leroy Koh
Diabetology International.2023; 14(3): 224. CrossRef - The effects of alpha lipoic acid (ALA) supplementation on blood pressure in adults: a GRADE-assessed systematic review and dose-response meta-analysis of randomized controlled trials
Mahdi Vajdi, Nooshin Noshadi, Shirin Hassanizadeh, Atefeh Bonyadian, Hooria Seyedhosseini-Ghaheh, Gholamreza Askari
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Combination Therapy of Alpha-Lipoic Acid, Gliclazide and Ramipril Protects Against Development of Diabetic Cardiomyopathy via Inhibition of TGF-β/Smad Pathway
George J. Dugbartey, Quinsker L. Wonje, Karl K. Alornyo, Louis Robertson, Ismaila Adams, Vincent Boima, Samuel D. Mensah
Frontiers in Pharmacology.2022;[Epub] CrossRef - Diabetic Gastroenteropathy: Soothe the Symptoms or Unravel a Cure?
Sondre Meling, Davide Bertoli, Dag A. Sangnes, Christina Brock, Asbjørn Drewes, Niels Ejskjaer, Georg Dimcevski, Eirik Søfteland
Current Diabetes Reviews.2022;[Epub] CrossRef - Efficacy and safety of oral alpha-lipoic acid supplementation for type 2 diabetes management: a systematic review and dose–response meta-analysis of randomized trials
Aliyu Tijani Jibril, Ahmad Jayedi, Sakineh Shab-Bidar
Endocrine Connections.2022;[Epub] CrossRef - Cardiac Autonomic Neuropathy in Type 1 and 2 Diabetes: Epidemiology, Pathophysiology, and Management
Scott Williams, Siddig Abdel Raheim, Muhammad Ilyas Khan, Umme Rubab, Prathap Kanagala, Sizheng Steven Zhao, Anne Marshall, Emily Brown, Uazman Alam
Clinical Therapeutics.2022; 44(10): 1394. CrossRef - An updated systematic review and dose-response meta-analysis of the effects of α-lipoic acid supplementation on glycemic markers in adults
Mahsa Mahmoudi-Nezhad, Mahdi Vajdi, Mahdieh Abbasalizad Farhangi
Nutrition.2021; 82: 111041. CrossRef - Management of diabetic neuropathy
Simona Cernea, Itamar Raz
Metabolism.2021; 123: 154867. CrossRef - Effect of alpha-lipoic acid on arterial stiffness parameters in type 2 diabetes mellitus patients with cardiac autonomic neuropathy
Victoria A. Serhiyenko, Ludmila M. Serhiyenko, Volodymyr B. Sehin, Alexandr A. Serhiyenko
Endocrine Regulations.2021; 55(4): 224. CrossRef - The Role of Alpha-lipoic Acid Supplementation in the Prevention of Diabetes Complications: A Comprehensive Review of Clinical Trials
Sarah Jeffrey, Punitha Isaac Samraj, Behin Sundara Raj
Current Diabetes Reviews.2021;[Epub] CrossRef - Safety Evaluation of α-Lipoic Acid Supplementation: A Systematic Review and Meta-Analysis of Randomized Placebo-Controlled Clinical Studies
Federica Fogacci, Manfredi Rizzo, Christoffer Krogager, Cormac Kennedy, Coralie M.G. Georges, Tamara Knežević, Evangelos Liberopoulos, Alexandre Vallée, Pablo Pérez-Martínez, Eliane F.E. Wenstedt, Agnė Šatrauskienė, Michal Vrablík, Arrigo F.G. Cicero
Antioxidants.2020; 9(10): 1011. CrossRef - Update on the Impact, Diagnosis and Management of Cardiovascular Autonomic Neuropathy in Diabetes: What Is Defined, What Is New, and What Is Unmet
Vincenza Spallone
Diabetes & Metabolism Journal.2019; 43(1): 3. CrossRef - Alpha-lipoic acid (ALA) supplementation effect on glycemic and inflammatory biomarkers: A Systematic Review and meta- analysis
Mehran Rahimlou, Maryam Asadi, Nasrin Banaei Jahromi, Anahita Mansoori
Clinical Nutrition ESPEN.2019; 32: 16. CrossRef - Response: Effects of High-Dose α-Lipoic Acid on Heart Rate Variability of Type 2 Diabetes Mellitus Patients with Cardiac Autonomic Neuropathy in Korea (Diabetes Metab J 2017;41:275-83)
Chong Hwa Kim, Sol Jae Lee, Bong Yun Cha
Diabetes & Metabolism Journal.2017; 41(5): 420. CrossRef - Letter: Effects of High-Dose α-Lipoic Acid on Heart Rate Variability of Type 2 Diabetes Mellitus Patients with Cardiac Autonomic Neuropathy in Korea (Diabetes Metab J2017;41:275-83)
Jeongmin Lee, Jae Hyoung Cho
Diabetes & Metabolism Journal.2017; 41(5): 417. CrossRef
- Effect of Ramipril on Cardiac Autonomic Neuropathy in Patients With Type II Diabetes Mellitus
- The Status of Diabetes Mellitus and Effects of Related Factors on Heart Rate Variability in a Community.
- Kyeong Soon Chang, Kwan Lee, Hyun Sul Lim
- Korean Diabetes J. 2009;33(6):537-546. Published online December 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.6.537
- 1,800 View
- 17 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
This study was performed to examine the status of diabetes mellitus (DM) in the community and effects of related factors on heart rate variability (HRV). METHODS: The author conducted HRV testing, a questionnaire survey, and blood chemistry analysis for fasting blood sugar (FBS) and HbA1c levels in 855 patients in a community over a period of 10 days, from August 14 to 25, 2006. The subjects were divided into a DM group and normal group by our study criteria. RESULTS: The proportion of DM was 12.6% and increased with old age. The mean measures of HRV (SDNN, Tp, Vlf, Lf, Hf, Lf/Hf) in the DM group were 22.7 (1.6) msec, 364.9 (2.7) msec2, 174.1 (3.0) msec2, 88.1 (3.2) msec2, 55.3 (3.2) msec2, and 1.6 (2.6), respectively, while those in the normal group were 32.2 (1.6) msec, 676.6 (2.8) msec2, 295.7 (3.1) msec2, 169.2 (3.4) msec2, 117.2 (3.2) msec2, and 1.4 (2.6), respectively. All parameters except for Lf/Hf were significantly lower in the DM group than in the normal group (P < 0.01). The Spearman's correlation coefficients between HRV and FBS or HbA1c were SDNN -0.222/-0.244 (P < 0.01), Tp -0.211/-0.212 (P < 0.01), Vlf -0.149/-0.132 (P < 0.01), Lf -0.188/-0.235 (P < 0.01), Hf -0.207/-0.204 (P < 0.01), and Lf/Hf (P > 0.05), respectively. CONCLUSION: This study shows that the DM group had a reduced HRV and increased pulse rate in comparison with the normal group. According to our results, the HRV test may be used accessorily for the early detection of cardiovascular autonomic neuropathy (CAN) and its related factors, as well as to prevent CAN. -
Citations
Citations to this article as recorded by- Psychophysiological Responses of Adults According to Cognitive Demand Levels for Horticultural Activities
Seon-Ok Kim, Yun-Jin Kim, Sin-Ae Park
Sustainability.2022; 14(14): 8252. CrossRef - Physiological and psychological responses of humans to the index of greenness of an interior space
Ji-Young Choi, Sin-Ae Park, Soo-Jin Jung, Ji-Young Lee, Ki-Cheol Son, Youn-Joo An, Sang-Woo Lee
Complementary Therapies in Medicine.2016; 28: 37. CrossRef
- Psychophysiological Responses of Adults According to Cognitive Demand Levels for Horticultural Activities
- Detection of Diabetic Autonomic Neuropathy by 24-Hour Heart Rate Variability Analysis in Type 2 Diabetes Mellitus Patients.
- Young Hee Rho, Nan Hee Kim, Dong Lim Kim, Dong Hyun Shin, Sin Gon Kim, Kyung Mook Choi, Woo Hyuk Song, Sei Hyun Baik, Woo Keun Seo, Min Kyu Park, Dong Seop Choi
- Korean Diabetes J. 2002;26(3):208-219. Published online June 1, 2002
- 1,265 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Diabetic autonomic neuropathy is a relatively common diabetic complication, associated with high long-term mortality. Ewing's test is known as the 'gold standard' for evaluating and diagnosing this disease, yet is not widely used due to the inconvenient procedures of the test. 24-hour Holter EKG monitoring, and the analytical product, heart rate variability, is being introduced as a relatively simple and reliable procedure for the evaluation of diabetic autonomic neuropathy. We explored whether such heart rate variability products derived from Holter monitoring, correlated with the presence, absence, or severity of diabetes mellitus, and whether it correlated well with conventional autonomic tests. METHODS: We compared 59 type 2 diabetic patients with 71 normal subjects. All underwent 24-hr Holter EKG monitoring and basic autonomic evaluations, such as the head-up tilting, hand grip, and deep breathing-heart rate variability tests. Those who had diabetes also underwent evaluation for basic blood chemistry, and complication studies, for things such as: 24-hour urine albumin excretion, fundoscopy and nerve conduction. RESULTS: Variables for heart rate variability were expressed as SDDN, rMSSD, LF, HF, and LF/HF, where SDDN is the Standard Deviation of all RR intervals, rMSSD the square root of the mean of the sum of the squares of differences between adjacent RR intervals, LF the power in the Low Frequency range and HF the power in the High Frequency range, with LF/HF being the ratio between LF and HF. Heart rate variability was significantly lower in terms of rMSSD, LF, HF, but not in terms of the LF/HF ratio, for the diabetic patients compared to the normal subjects. These three variables also correlated with the conventional autonomic tests of systolic blood pressure changes during standing up (negatively), and heart rate variability during deep breathing (positively). SDDN, rMSSD, LF, and HF also correlated negatively with the duration of diabetes. SDDN, LF and HF were significantly lower among patients who had complications such as: retinopathy, nephropathy or peripheral neuropathy, than in those who did not. CONCLUSION: Heart rate variability was lower in type 2 diabetic patients than the control subjects, which correlated well with the duration of diabetes mellitus, diabetic chronic complications and the conventional autonomic nervous function tests, so could be an useful adjunct or even a replacement, for conventional autonomic nervous system testing procedures. More research is needed in this field.

 KDA
KDA
 First
First Prev
Prev





