
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Others
- Risk Prediction and Management of Chronic Kidney Disease in People Living with Type 2 Diabetes Mellitus
- Ying-Guat Ooi, Tharsini Sarvanandan, Nicholas Ken Yoong Hee, Quan-Hziung Lim, Sharmila S. Paramasivam, Jeyakantha Ratnasingam, Shireene R. Vethakkan, Soo-Kun Lim, Lee-Ling Lim
- Diabetes Metab J. 2024;48(2):196-207. Published online January 26, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0244
- 1,940 View
- 364 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
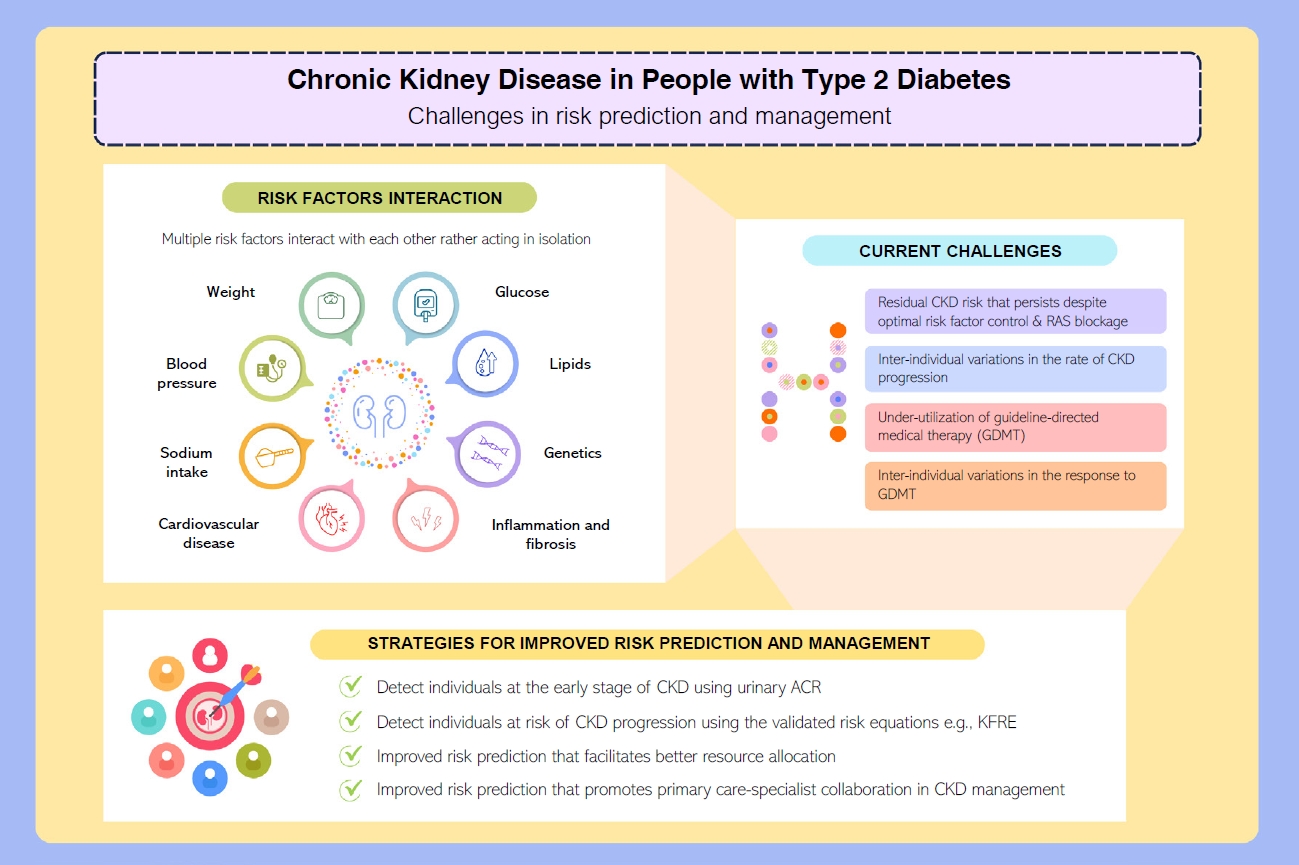
ePub - People with type 2 diabetes mellitus have increased risk of chronic kidney disease and atherosclerotic cardiovascular disease. Improved care delivery and implementation of guideline-directed medical therapy have contributed to the declining incidence of atherosclerotic cardiovascular disease in high-income countries. By contrast, the global incidence of chronic kidney disease and associated mortality is either plateaued or increased, leading to escalating direct and indirect medical costs. Given limited resources, better risk stratification approaches to identify people at risk of rapid progression to end-stage kidney disease can reduce therapeutic inertia, facilitate timely interventions and identify the need for early nephrologist referral. Among people with chronic kidney disease G3a and beyond, the kidney failure risk equations (KFRE) have been externally validated and outperformed other risk prediction models. The KFRE can also guide the timing of preparation for kidney replacement therapy with improved healthcare resources planning and may prevent multiple complications and premature mortality among people with chronic kidney disease with and without type 2 diabetes mellitus. The present review summarizes the evidence of KFRE to date and call for future research to validate and evaluate its impact on cardiovascular and mortality outcomes, as well as healthcare resource utilization in multiethnic populations and different healthcare settings.
- Complications
- Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
- Eugene Han, Mi Kyung Kim, Byoung Kuk Jang, Hye Soon Kim
- Diabetes Metab J. 2021;45(5):698-707. Published online February 2, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0118
- 5,429 View
- 197 Download
- 11 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
This study aimed to investigate the association between hepatic steatosis burden and albuminuria in Korean patients with type 2 diabetes mellitus (T2DM) and nonalcoholic fatty liver disease (NAFLD).
Methods
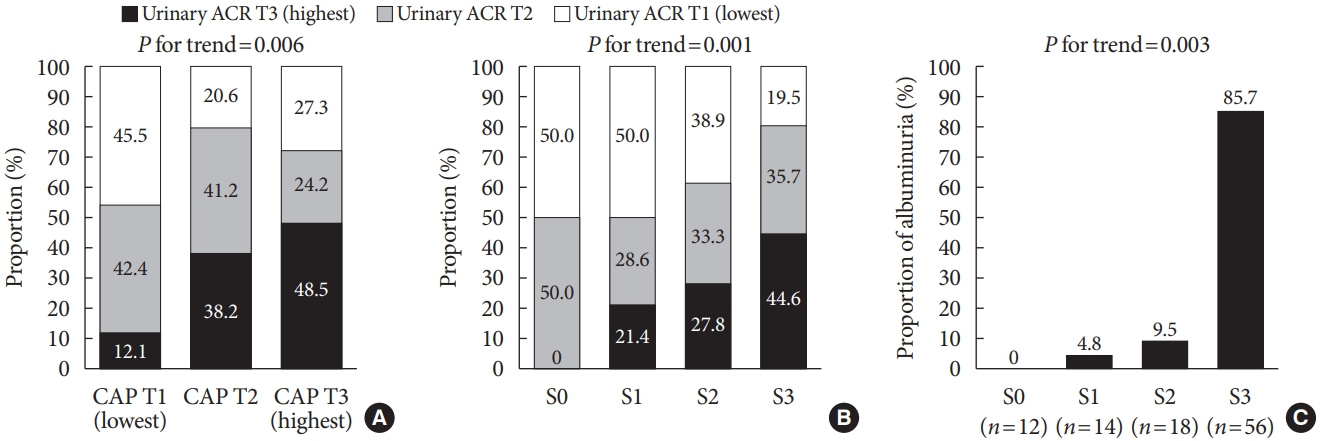
We recruited 100 patients with both T2DM and NAFLD, but without chronic kidney disease. Albuminuria was defined as a spot urinary albumin-to-creatinine ratio (ACR) ≥30 mg/g. Transient elastography was performed, and the steatosis burden was quantified by controlled attenuation parameter (CAP) with significant steatosis defined as CAP >302 dB/m.
Results
The prevalence of significant steatosis and albuminuria was 56.0% and 21.0%, respectively. Subjects with significant steatosis were significantly younger and had a significantly shorter duration of T2DM, greater waist circumference, and higher body mass index, total cholesterol, triglyceride, and low density lipoprotein cholesterol levels, than subjects without severe NAFLD (all P<0.05). Albuminuria was higher in patients with significant steatosis than in patients without significant steatosis (32.1% vs. 6.8%, P=0.002). Urinary ACR showed a correlation with CAP (r=0.331, P=0.001), and multiple linear regression analysis revealed a significant association between a high degree of albuminuria and high CAP value (r=0.321, P=0.001). Additionally, multivariate logistic regression analysis demonstrated the independent association between urinary ACR and significant steatosis after adjustment for confounding factors including age, body mass index, duration of T2DM, low density lipoprotein level, and renin-angiotensin system blocker use (odds ratio, 1.88; 95% confidence interval, 1.31 to 2.71; P=0.001).
Conclusion
T2DM patients with NAFLD had a higher prevalence of albuminuria, which correlated with their steatosis burden. -
Citations
Citations to this article as recorded by- A Novel Anthropometric Parameter, Weight-Adjusted Waist Index Represents Sarcopenic Obesity in Newly Diagnosed Type 2 Diabetes Mellitus
Min Jeong Park, Soon Young Hwang, Nam Hoon Kim, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
Journal of Obesity & Metabolic Syndrome.2023; 32(2): 130. CrossRef - Significance of Diabetic Kidney Disease Biomarkers in Predicting Metabolic-Associated Fatty Liver Disease
Jaehyun Bae, Byung-Wan Lee
Biomedicines.2023; 11(7): 1928. CrossRef - Non-alcoholic fatty liver disease and sarcopenia is associated with the risk of albuminuria independent of insulin resistance, and obesity
Eugene Han, Mi Kyung Kim, Seung-Soon Im, Byoung Kuk Jang, Hye Soon Kim
Journal of Diabetes and its Complications.2022; 36(8): 108253. CrossRef - Development and implementation of patient-level prediction models of end-stage renal disease for type 2 diabetes patients using fast healthcare interoperability resources
San Wang, Jieun Han, Se Young Jung, Tae Jung Oh, Sen Yao, Sanghee Lim, Hee Hwang, Ho-Young Lee, Haeun Lee
Scientific Reports.2022;[Epub] CrossRef - Beyond Liver Disease: Non-Alcoholic Fatty Liver Disease and Advanced Liver Fibrosis in Kidney Disease
Eugene Han
Diabetes & Metabolism Journal.2022; 46(4): 564. CrossRef - Muscle fat contents rather than muscle mass determines nonalcoholic steatohepatitis and liver fibrosis in patients with severe obesity
Eugene Han, Mi Kyung Kim, Hye Won Lee, Seungwan Ryu, Hye Soon Kim, Byoung Kuk Jang, Youngsung Suh
Obesity.2022; 30(12): 2440. CrossRef - Decreased Serum Osteocalcin is an Independent Risk Factor for Metabolic Dysfunction-Associated Fatty Liver Disease in Type 2 Diabetes
Yu-Jie Wang, Chun-Hua Jin, Jiang-Feng Ke, Jun-Wei Wang, Yi-Lin Ma, Jun-Xi Lu, Mei-Fang Li, Lian-Xi Li
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 3717. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2021;45:698-707)
Eugene Han, Hye Soon Kim
Diabetes & Metabolism Journal.2021; 45(6): 972. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2021;45:698-707)
Mi-kyung Kim
Diabetes & Metabolism Journal.2021; 45(6): 968. CrossRef - Liver fibrosis indices are related to diabetic peripheral neuropathy in individuals with type 2 diabetes
Kyuho Kim, Tae Jung Oh, Hyen Chung Cho, Yun Kyung Lee, Chang Ho Ahn, Bo Kyung Koo, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
Scientific Reports.2021;[Epub] CrossRef
- A Novel Anthropometric Parameter, Weight-Adjusted Waist Index Represents Sarcopenic Obesity in Newly Diagnosed Type 2 Diabetes Mellitus
- Epidemiology
- Lower Leg Fat Depots Are Associated with Albuminuria Independently of Obesity, Insulin Resistance, and Metabolic Syndrome (Korea National Health and Nutrition Examination Surveys 2008 to 2011)
- Eugene Han, Nan Hee Cho, Mi Kyung Kim, Hye Soon Kim
- Diabetes Metab J. 2019;43(4):461-473. Published online March 7, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0081
- 5,011 View
- 39 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Although the involvement of obesity in metabolic disorders is well known, leg fat depot influences on albuminuria have not been determined.
Methods This population-based, cross-sectional study used a nationally representative sample of 2,076 subjects aged ≥20 years from the Korea National Health and Nutrition Examination Surveys of 2008 to 2011. The ratio of leg fat to total fat (LF/TF ratio) was assessed by dual X-ray absorptiometry, and albuminuria was defined as more than one positive dipstick test or an albumin-to-creatinine ratio of ≥30 mg/g.
Results Individuals whose LF/TF ratio was in the lowest tertile showed a higher proportion of albuminuria than those in the highest tertile (odds ratio [OR], 2.82; 95% confidence interval [CI], 2.01 to 3.96;
P <0.001). This association was observed in both sexes, all age groups, and all subgroups stratified by body mass index, waist circumference, homeostasis model assessments of insulin resistance, and the presence of metabolic syndrome (all,P <0.05). Multiple logistic regression analyses also demonstrated that the lowest LF/TF ratio was independently associated with albuminuria risk (OR, 1.55 to 2.16; all,P <0.05). In addition, the risk of albuminuria was higher in sarcopenic individuals with lower LF/TF ratios than in the highest LF/TF ratio subjects without sarcopenia (OR, 3.73; 95% CI, 2.26 to 6.13).Conclusion A lower LF/TF ratio was associated with an increased risk of albuminuria independent of obesity, insulin resistance, and metabolic syndrome, and when combined with sarcopenia, the albuminuria risk synergistically increased. Hence, our findings may have implications to improve risk stratification and recommendations on body fat distribution in the general population.
-
Citations
Citations to this article as recorded by- Efficacy and safety of evogliptin in patients with type 2 diabetes and non‐alcoholic fatty liver disease: A multicentre, double‐blind, randomized, comparative trial
Eugene Han, Ji Hye Huh, Eun Y. Lee, Ji C. Bae, Sung W. Chun, Sung H. Yu, Soo H. Kwak, Kyong S. Park, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2022; 24(4): 752. CrossRef - Muscle fat contents rather than muscle mass determines nonalcoholic steatohepatitis and liver fibrosis in patients with severe obesity
Eugene Han, Mi Kyung Kim, Hye Won Lee, Seungwan Ryu, Hye Soon Kim, Byoung Kuk Jang, Youngsung Suh
Obesity.2022; 30(12): 2440. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Eugene Han, Mi Kyung Kim, Byoung Kuk Jang, Hye Soon Kim
Diabetes & Metabolism Journal.2021; 45(5): 698. CrossRef
- Efficacy and safety of evogliptin in patients with type 2 diabetes and non‐alcoholic fatty liver disease: A multicentre, double‐blind, randomized, comparative trial
- Complications
- Higher Prevalence and Progression Rate of Chronic Kidney Disease in Elderly Patients with Type 2 Diabetes Mellitus
- Kyung-Soo Kim, Seok Won Park, Yong-Wook Cho, Soo-Kyung Kim
- Diabetes Metab J. 2018;42(3):224-232. Published online May 31, 2018
- DOI: https://doi.org/10.4093/dmj.2017.0065
- 5,268 View
- 73 Download
- 31 Web of Science
- 33 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background To evaluate the prevalence of chronic kidney disease (CKD) and progression rate to CKD in elderly patients with type 2 diabetes mellitus (T2DM).
Methods We investigated the medical records of 190 elderly patients (65 years or older) with T2DM from 2005 to 2011 in 6-month increments. Mean follow-up duration was 64.5 months. CKD was defined as estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2 and/or the presence of albuminuria.
Results The mean age was 70.4 years and mean diabetes duration was 10.6 years. Among all the participants, 113 patients (59.5%) had CKD. The eGFR was significantly decreased between baseline (65.7±15.0 mL/min/1.73 m2) and the end of follow-up (52.7±17.5 mL/min/1.73 m2,
P <0.001). At the end of follow-up, the prevalence of eGFR <60 mL/min/1.73 m2 had increased by 61.6% (at baseline, 44.2%). Furthermore, in patients with eGFR ≥60 mL/min/1.73 m2, the progression rate to more than CKD stage 3 was 39.6% at the end of follow-up; 30.2% of elderly diabetic patients had progressed to albuminuria from normoalbuminuria. Kaplan-Meier analysis showed that the time interval to worsening nephropathy was significantly shorter in elderly patients with diabetes duration ≥10 years than in those with diabetes duration <5 years (P =0.018).Conclusion CKD was commonly observed in older patients with T2DM, and the progression rate to CKD is also high. Consequently, it is important to identify and manage CKD as early as possible in elderly patients with T2DM, especially in those with diabetes duration ≥10 years.
-
Citations
Citations to this article as recorded by- Assessing heatwave effects on disabled persons in South Korea
Yeji Kang, Ingul Baek, Jongchul Park
Scientific Reports.2024;[Epub] CrossRef - Combination of Risks of BMI and Health-Related Lifestyles on Kidney Function in the Prediabetic Japanese Population: A Prospective Cohort Study
Jou-Yin Chen, Shiqi Deng, Yukiko Wagatsuma
International Journal of Environmental Research and Public Health.2023; 20(7): 5338. CrossRef - Hormonal imbalance in patients with chronic renal failure in the pre-dialysis and dialysis periods (part1)
I.P. Katerenchuk, S.T. Rustamyan, V.V. Talash, T.I. Yarmola
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2023; 19(1): 65. CrossRef - The Beneficial Effect of Glycemic Control against Adverse Outcomes in Patients with Type 2 Diabetes Mellitus and Chronic Kidney Disease
Dong-Hwa Lee
Diabetes & Metabolism Journal.2023; 47(4): 484. CrossRef - Association Between Continuous Glucose Monitoring-Derived Glycemia Risk Index and Albuminuria in Type 2 Diabetes
Jee Hee Yoo, Ji Yoon Kim, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2023; 25(10): 726. CrossRef - Global burden and influencing factors of chronic kidney disease due to type 2 diabetes in adults aged 20–59 years, 1990–2019
Dandan Xie, Tianpeng Ma, Haoliang Cui, Jing Li, Aihua Zhang, Zhifeng Sheng, Yiqiang Xie
Scientific Reports.2023;[Epub] CrossRef - Effectiveness of Early Advanced Glycation End Product Accumulation Testing in the Diagnosis of Diabetes: A Health Risk Factor Analysis Using the Body Mass Index as a Moderator
Yi Zhang, Tian Jiang, Chao Liu, Honglin Hu, Fang Dai, Li Xia, Qiu Zhang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Causal association pathways between fetuin-A and kidney function: a mediation analysis
Philip Etabee Bassey, Pawin Numthavaj, Sasivimol Rattanasiri, Piyamitr Sritara, Mark McEvoy, Boonsong Ongphiphadhanakul, Ammarin Thakkinstian
Journal of International Medical Research.2022; 50(4): 030006052210828. CrossRef - Advanced glycation end products and diabetes and other metabolic indicators
Tian Jiang, Yi Zhang, Fang Dai, Chao Liu, Honglin Hu, Qiu Zhang
Diabetology & Metabolic Syndrome.2022;[Epub] CrossRef - Type 2 diabetes management in people aged over seventy-five years: targets and treatment strategies
Theocharis Koufakis, Maria Grammatiki, Kalliopi Kotsa
Maturitas.2021; 143: 118. CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef - Chronic kidney disease progression in aged patients
Murat Tuğcu, Dilek Barutçu Ataş
International Urology and Nephrology.2021; 53(12): 2619. CrossRef - Factors determining the clinical significance of dipeptidyl peptidase-4 inhibitors in the treatment of elderly patients with type 2 diabetes mellitus
I. V. Glinkina, A. V. Balashova, A. S. Shyman, A. V. Oderij, S. A. Khan, G. E. Runova, T. B. Morgunova, V. V. Fadeev
Meditsinskiy sovet = Medical Council.2021; (7): 56. CrossRef - Effect of Oral carnosine supplementation on urinary TGF-β in diabetic nephropathy: a randomized controlled trial
Narongrit Siriwattanasit, Bancha Satirapoj, Ouppatham Supasyndh
BMC Nephrology.2021;[Epub] CrossRef - Estimation of the prevalence of type 2 diabetes in combination with diabetic kidney disease and identification of the associated factors in patients attending primary hospitals in Anhui Province, China
Li Xia, Lanlan Cheng, Tian Jiang, Chao Liu, Shiqi Zhang, Honglin Hu, Fang Dai, Qiu Zhang, Yunxia Lu
Journal of International Medical Research.2021; 49(10): 030006052110512. CrossRef - A STUDY TO EVALUATE THE EFFECT OF ANAEMIA IN TYPE-2 DIABETIC PATIENTS
Radhika Maheshwari, Divya J., J. Sahayaraj, Muthukrishnan R.
GLOBAL JOURNAL FOR RESEARCH ANALYSIS.2021; : 117. CrossRef - Metformin treatment for patients with diabetes and chronic kidney disease: A Korean Diabetes Association and Korean Society of Nephrology consensus statement
Kyu Yeon Hur, Mee Kyoung Kim, Seung Hyun Ko, Miyeun Han, Dong Won Lee, Hyuk-Sang Kwon
Kidney Research and Clinical Practice.2020; 39(1): 32. CrossRef - Metformin Treatment for Patients with Diabetes and Chronic Kidney Disease: A Korean Diabetes Association and Korean Society of Nephrology Consensus Statement
Kyu Yeon Hur, Mee Kyoung Kim, Seung Hyun Ko, Miyeun Han, Dong Won Lee, Hyuk-Sang Kwon
Diabetes & Metabolism Journal.2020; 44(1): 3. CrossRef - The prevalence of diabetic chronic kidney disease in adult Greek subjects with type 2 diabetes mellitus: A series from hospital-based diabetes clinics
Ilias N. Migdalis, Nikolaos Papanas, Athanasios E. Raptis, Ioannis M. Ioannidis, Alexios E. Sotiropoulos, George D. Dimitriadis
Diabetes Research and Clinical Practice.2020; 166: 108243. CrossRef - Proteinuria Is Associated with Carotid Artery Atherosclerosis in Non-Albuminuric Type 2 Diabetes: A Cross-Sectional Study
Jaehyun Bae, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Journal of Clinical Medicine.2020; 9(1): 136. CrossRef - Renal status in elderly patients with type 2 diabetes
Kazunaga Takamatsu
Clinical and Experimental Nephrology.2020; 24(1): 53. CrossRef - The fat mass, estimated glomerular filtration rate, and chronic inflammation in type 2 diabetic patients
Tomáš Šálek, Alena Adamíková, Petr Ponížil
Journal of Clinical Laboratory Analysis.2020;[Epub] CrossRef - Insulin: Trigger and Target of Renal Functions
Ana F. Pina, Diego O. Borges, Maria João Meneses, Patrícia Branco, Rita Birne, Antonio Vilasi, Maria Paula Macedo
Frontiers in Cell and Developmental Biology.2020;[Epub] CrossRef - Rate of kidney function decline and factors predicting progression of kidney disease in type 2 diabetes mellitus patients with reduced kidney function: A nationwide retrospective cohort study
Wisit Kaewput, Charat Thongprayoon, Api Chewcharat, Ram Rangsin, Bancha Satirapoj, Chalermrat Kaewput, Picha Suwannahitatorn, Tarun Bathini, Michael A. Mao, Liam D. Cato, Andrew M. Harrison, Pradeep Vaitla, Wisit Cheungpasitporn
Therapeutic Apheresis and Dialysis.2020; 24(6): 677. CrossRef - Association Between Continuous Glucose Monitoring-Derived Time in Range, Other Core Metrics, and Albuminuria in Type 2 Diabetes
Jee Hee Yoo, Min Sun Choi, Jiyeon Ahn, Sung Woon Park, Yejin Kim, Kyu Yeon Hur, Sang-Man Jin, Gyuri Kim, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2020; 22(10): 768. CrossRef - Comparison of Renal Effects of Ezetimibe–Statin Combination versus Statin Monotherapy: A Propensity-Score-Matched Analysis
Jaehyun Bae, Namki Hong, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Yong-ho Lee
Journal of Clinical Medicine.2020; 9(3): 798. CrossRef - Metformin Use and Risk of All-Cause Mortality and Cardiovascular Events in Patients With Chronic Kidney Disease—A Systematic Review and Meta-Analysis
Yao Hu, Min Lei, Guibao Ke, Xin Huang, Xuan Peng, Lihui Zhong, Ping Fu
Frontiers in Endocrinology.2020;[Epub] CrossRef - Treatment with Cinacalcet in Hemodialysis Patients with Severe Secondary Hyperparathyroidism, Influences Bone Mineral Metabolism and Anemia Parameters
Maria Aktsiali, Theodora Papachrysanthou , Ioannis Griveas, Christos Andriopoulos, Panagiotis Sitaras, Ioannis K. Triantafyllopoulos , George I. Lambrou
Current Drug Therapy.2020; 15(3): 249. CrossRef - Gemigliptin Attenuates Renal Fibrosis Through Down-Regulation of the NLRP3 Inflammasome
Jung Beom Seo, Yeon-Kyung Choi, Hye-In Woo, Yun-A Jung, Sungwoo Lee, Seunghyeong Lee, Mihyang Park, In-Kyu Lee, Gwon-Soo Jung, Keun-Gyu Park
Diabetes & Metabolism Journal.2019; 43(6): 830. CrossRef - Glucometabolic characteristics and higher vascular complication risk in Korean patients with type 2 diabetes with non-albumin proteinuria
Yongin Cho, Yong-ho Lee, Eun Seok Kang, Bong-soo Cha, Byung-wan Lee
Journal of Diabetes and its Complications.2019; 33(8): 585. CrossRef - Assessment of kidney function and associated risk factors among type 2 diabetic patients
Moyad Jamal Shahwan, Nageeb Abdul galil Hassan, Rima Ahd Shaheen
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(4): 2661. CrossRef - Influence of diabetes mellitus on patients with lumbar spinal stenosis: A nationwide population-based study
Chang Kyu Lee, Sun Kyu Choi, Dong Ah Shin, Seong Yi, Yoon Ha, Keung Nyun Kim, Insoo Kim, Gregory W.J. Hawryluk
PLOS ONE.2019; 14(3): e0213858. CrossRef - Predictores de progresión de enfermedad renal en el paciente anciano
Manuel Heras Benito, Mª José Fernández Reyes Luis
Enfermería Nefrológica.2019; 22(1): 19. CrossRef
- Assessing heatwave effects on disabled persons in South Korea
- Prevalence and Determinants of Diabetic Nephropathy in Korea: Korea National Health and Nutrition Examination Survey
- Jae Hee Ahn, Ji Hee Yu, Seung-Hyun Ko, Hyuk-Sang Kwon, Dae Jung Kim, Jae Hyeon Kim, Chul Sik Kim, Kee-Ho Song, Jong Chul Won, Soo Lim, Sung Hee Choi, Kyungdo Han, Bong-Yun Cha, Nan Hee Kim
- Diabetes Metab J. 2014;38(2):109-119. Published online April 18, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.2.109
- 5,354 View
- 99 Download
- 58 Web of Science
- 58 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Diabetic nephropathy is a leading cause of end stage renal disease and is associated with an increased risk of cardiovascular mortality. It manifests as albuminuria or impaired glomerular filtration rate (GFR), and the prevalence of diabetic nephropathy varies with ethnicity. The prevalence of diabetic nephropathy and its determinants in Korean adults have not previously been studied at the national level. This cross-sectional study was undertaken to ascertain the prevalence and determinants of albuminuria and chronic kidney disease (CKD) in Korean patients with diabetes.
Methods The Korea National Health and Nutrition Examination Survey (KNHANES) V, conducted in 2011, was used to define albuminuria (
n =4,652), and the dataset of KNHANES IV-V (2008-2011) was used to define CKD (n =21,521). Selected samples were weighted to represent the entire civilian population in Korea. Albuminuria was defined as a spot urine albumin/creatinine ratio >30 mg/g. CKD was defined as a GFR <60 mL/min/1.73 m2.Results Among subjects with diabetes, 26.7% had albuminuria, and 8.6% had CKD. Diabetes was associated with an approximate 2.5-fold increased risk of albuminuria, with virtually no difference between new-onset and previously diagnosed diabetes. Only systolic blood pressure was significantly associated with albuminuria, and old age, high serum triglyceride levels, and previous cardiovascular disease (CVD) were related with CKD in subjects with diabetes.
Conclusion Korean subjects with diabetes had a higher prevalence of albuminuria and CKD than those without diabetes. Blood pressure was associated with albuminuria, and age, triglyceride level, and previous CVD were independent determinants of CKD in subjects with diabetes.
-
Citations
Citations to this article as recorded by- Associations between dietary patterns and renal impairment in individuals with diabetes: a cross‐sectional study
Ziling Ding, Xingzhe Wu, Chao Liu, Ruixue Ying, Yi Zhang, Shiqi Zhang, Qiu Zhang, Honglin Hu, Fang Dai
Journal of Human Nutrition and Dietetics.2024; 37(1): 193. CrossRef - Determinants of diabetic nephropathy among adult diabetic patients on follow-up at public hospitals in Addis Ababa, Ethiopia: A case-control study
Diriba Etana Tola, Zenebu Begna Bayissa, Tamene Abera Desissa, Lencho Kajela Solbana, Azeb Haile Tesfaye, Bikila Fufa Eba
SAGE Open Medicine.2024;[Epub] CrossRef - Kidney Health Plan 2033 in Korea: bridging the gap between the present and the future
Do Hyoung Kim, Young Youl Hyun, Jin Joo Cha, Sua Lee, Hyun Kyung Lee, Jong Wook Choi, Su-Hyun Kim, Sang Youb Han, Cheol Whee Park, Eun Young Lee, Dae Ryong Cha, Sung Gyun Kim, Chun Soo Lim, Sun-Hee Park
Kidney Research and Clinical Practice.2024; 43(1): 8. CrossRef - Risk Factors of Microalbuminuria among Patients with Type 2 Diabetes Mellitus in Korea: A Cross-Sectional Study Based on 2019–2020 Korea National Health and Nutrition Examination Survey Data
Eun Sook Bae, Jung Yi Hur, Hyung Soon Jang, Jeong Suk Kim, Hye Seung Kang
International Journal of Environmental Research and Public Health.2023; 20(5): 4169. CrossRef - CORRELATION OF VASCULAR ENDOTHELIAL FUNCTION AND INFLAMMATORY FACTORS WITH RENAL FUNCTION IN PATIENTS WITH DIABETIC NEPHROPATHY
A. Y. Mammadzada, Sh. G. Ismayilova, Sh. S. Ibrahimova, N. I. Huseynova, L. A. Huseyn
World of Medicine and Biology.2023; 19(85): 129. CrossRef - Synopsis of the Korean Society of Nephrology 2023 Practical Recommendations for the Management of Diabetic Kidney Disease
Sungjin Chung
The Korean Journal of Medicine.2023; 98(6): 270. CrossRef - 3-Hydroxybutyrate Ameliorates the Progression of Diabetic Nephropathy
Jeeyoun Jung, Woo Yeong Park, Yun Jin Kim, Mikyung Kim, Misun Choe, Kyubok Jin, Ji Hae Seo, Eunyoung Ha
Antioxidants.2022; 11(2): 381. CrossRef - Development and Validation of a Model That Predicts the Risk of Diabetic Nephropathy in Type 2 Diabetes Mellitus Patients: A Cross-Sectional Study
Jing Yang, Sheng Jiang
International Journal of General Medicine.2022; Volume 15: 5089. CrossRef - Renoprotective Mechanism of Sodium-Glucose Cotransporter 2 Inhibitors: Focusing on Renal Hemodynamics
Nam Hoon Kim, Nan Hee Kim
Diabetes & Metabolism Journal.2022; 46(4): 543. CrossRef - Development and assessment of diabetic nephropathy prediction model using hub genes identified by weighted correlation network analysis
Xuelian Zhang, Yao Wang, Zhaojun Yang, Xiaoping Chen, Jinping Zhang, Xin Wang, Xian Jin, Lili Wu, Xiaoyan Xing, Wenying Yang, Bo Zhang
Aging.2022; 14(19): 8095. CrossRef - Neutrophil–lymphocyte ratio as an inflammatory biomarker of diabetic nephropathy among type 2 diabetes mellitus patients: A comparative cross-sectional study
Mesfin Zewude Gurmu, Solomon Genet, Solomon Tebeje Gizaw, Teka Obsa Feyisa, Natesan Gnanasekaran
SAGE Open Medicine.2022; 10: 205031212211402. CrossRef - Did Sejong the Great have ankylosing spondylitis? The oldest documented case of ankylosing spondylitis
JiHwan Lee
International Journal of Rheumatic Diseases.2021; 24(2): 203. CrossRef - Protective effects of klotho on palmitate-induced podocyte injury in diabetic nephropathy
Jeong Suk Kang, Seung Seob Son, Ji-Hye Lee, Seong Woo Lee, Ah Reum Jeong, Eun Soo Lee, Seung-Kuy Cha, Choon Hee Chung, Eun Young Lee, Partha Mukhopadhyay
PLOS ONE.2021; 16(4): e0250666. CrossRef - Nomogram for the prediction of diabetic nephropathy risk among patients with type 2 diabetes mellitus based on a questionnaire and biochemical indicators: a retrospective study
Yuhong Hu, Rong Shi, Ruohui Mo, Fan Hu
Aging.2020; 12(11): 10317. CrossRef - Differential Urinary Proteome Analysis for Predicting Prognosis in Type 2 Diabetes Patients with and without Renal Dysfunction
Hee-Sung Ahn, Jong Ho Kim, Hwangkyo Jeong, Jiyoung Yu, Jeonghun Yeom, Sang Heon Song, Sang Soo Kim, In Joo Kim, Kyunggon Kim
International Journal of Molecular Sciences.2020; 21(12): 4236. CrossRef - Urine E-cadherin: A Marker for Early Detection of Kidney Injury in Diabetic Patients
Michael Koziolek, Gerhard A. Mueller, Gry H. Dihazi, Klaus Jung, Constanze Altubar, Manuel Wallbach, Ivana Markovic, Dirk Raddatz, Olaf Jahn, Hülya Karaköse, Christof Lenz, Henning Urlaub, Abdelhi Dihazi, Abdellatif El El Meziane, Hassan Dihazi
Journal of Clinical Medicine.2020; 9(3): 639. CrossRef - Study of serum pentraxin 3 level in patients with diabetic nephropathy
Alaaeldin Abdelsalam Dawood, Mai Ashraf Kamel, Thoria Ahmed Omar, Ahmed Ahmed Mohammed Agaba
The Egyptian Journal of Internal Medicine.2020;[Epub] CrossRef - Limitations of Deep Learning Attention Mechanisms in Clinical Research: Empirical Case Study Based on the Korean Diabetic Disease Setting
Junetae Kim, Sangwon Lee, Eugene Hwang, Kwang Sun Ryu, Hanseok Jeong, Jae Wook Lee, Yul Hwangbo, Kui Son Choi, Hyo Soung Cha
Journal of Medical Internet Research.2020; 22(12): e18418. CrossRef - Long-term effects of various types of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors on changes in glomerular filtration rate in Korea
Seo Yeon Baik, Hyunah Kim, So Jung Yang, Tong Min Kim, Seung-Hwan Lee, Jae Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, Kun-Ho Yoon, Hun-Sung Kim
Frontiers of Medicine.2019; 13(6): 713. CrossRef - Plasma endoglin in Type2 diabetic patients with nephropathy
Ahmed S. Doghish, Atef A. Bassyouni, Mohamed H. Mahfouz, Heba G. Abd El-Aziz, Rania Y. Zakaria
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(1): 764. CrossRef - Cigarette smoking as a risk factor for diabetic nephropathy: A systematic review and meta-analysis of prospective cohort studies
Dan Liao, Liang Ma, Jing Liu, Ping Fu, Noël C. Barengo
PLOS ONE.2019; 14(2): e0210213. CrossRef - Risk factors for diabetic nephropathy complications in community patients with type 2 diabetes mellitus in Shanghai: Logistic regression and classification tree model analysis
Jieqiong Lou, Limei Jing, Hui Yang, Fei Qin, Wen Long, Rong Shi
The International Journal of Health Planning and Management.2019; 34(3): 1013. CrossRef - Predictive Factors for Efficacy of AST-120 Treatment in Diabetic Nephropathy: a Prospective Single-Arm, Open-Label, Multi-Center Study
You-Cheol Hwang, Se Won Kim, Kyu Yeon Hur, Bong-Soo Cha, In Joo Kim, Tae Sun Park, Sei Hyun Baik, Kun Ho Yoon, Kwan Woo Lee, In Kyu Lee, Moon-Kyu Lee
Journal of Korean Medical Science.2019;[Epub] CrossRef - Glycated Albumin Is a More Useful Glycation Index than HbA1c for Reflecting Renal Tubulopathy in Subjects with Early Diabetic Kidney Disease
Ji Hye Huh, Minyoung Lee, So Young Park, Jae Hyeon Kim, Byung-Wan Lee
Diabetes & Metabolism Journal.2018; 42(3): 215. CrossRef - Meta‑analysis of the benefit of sitagliptin treatment in patients with type 2 diabetes complicated with incipient nephropathy
Wei Liu, Jiangyi Yu, Qianhua Yan, Lijuan Wang, Nan Li, Wei Xiong
Experimental and Therapeutic Medicine.2018;[Epub] CrossRef - MicroRNA‐326‐3p ameliorates high glucose and ox‐LDL‐IC‐ induced fibrotic injury in renal mesangial cells by targeting FcγRIII
Yiting Wang, Rui Zhang, Junlin Zhang, Fang Liu
Nephrology.2018; 23(11): 1031. CrossRef - The Global Epidemiology of Diabetes and Kidney Disease
Digsu N. Koye, Dianna J. Magliano, Robert G. Nelson, Meda E. Pavkov
Advances in Chronic Kidney Disease.2018; 25(2): 121. CrossRef - Evaluation of the association between the number of natural teeth and anemia among Korean adults using nationally representative data
Kyungdo Han, Jun‐Beom Park
Journal of Periodontology.2018; 89(10): 1184. CrossRef - Correlation of vascular endothelial function and coagulation factors with renal function and inflammatory factors in patients with diabetic nephropathy
Jie Sun, Caiyan Liu
Experimental and Therapeutic Medicine.2018;[Epub] CrossRef - Cigarette smoking and risk of albuminuria in patients with type 2 diabetes: a systematic review and meta-analysis of observational studies
Haili Xu, Jinliu Suo, Jing Lian
International Urology and Nephrology.2018; 50(5): 911. CrossRef - Diabetes Fact Sheet in Korea, 2016: An Appraisal of Current Status
Jong Chul Won, Jae Hyuk Lee, Jae Hyeon Kim, Eun Seok Kang, Kyu Chang Won, Dae Jung Kim, Moon-Kyu Lee
Diabetes & Metabolism Journal.2018; 42(5): 415. CrossRef - Association between the number of natural teeth and diabetic retinopathy among type 2 diabetes mellitus
Su Jeong Song, Kyungdo Han, Seong-su Lee, Jun-Beom Park
Medicine.2017; 96(47): e8694. CrossRef - Arterial Stiffness Is More Associated with Albuminuria than Decreased Glomerular Filtration Rate in Patients with Type 2 Diabetes Mellitus: The REBOUND Study
Jong Ho Kim, Sang Soo Kim, In Joo Kim, Bo Hyun Kim, Ja Young Park, Chang Won Lee, Ji Hye Suk, Sun Hae Shin, Sung Pyo Son, Min Chul Kim, Jun Hyeob Ahn, Kwang Jae Lee, Min Jung Kwon, Soon Hee Lee, Jeong Hyun Park
Journal of Diabetes Research.2017; 2017: 1. CrossRef - Determinants of diabetic nephropathy in Ayder Referral Hospital, Northern Ethiopia: A case-control study
Solomon Hintsa, Lamessa Dube, Mebrahtu Abay, Teklit Angesom, Abdulhalik Workicho, Petter Bjornstad
PLOS ONE.2017; 12(4): e0173566. CrossRef - Comparison between Atorvastatin and Rosuvastatin in Renal Function Decline among Patients with Diabetes
Eugene Han, Gyuri Kim, Ji-Yeon Lee, Yong-ho Lee, Beom Seok Kim, Byung-Wan Lee, Bong-Soo Cha, Eun Seok Kang
Endocrinology and Metabolism.2017; 32(2): 274. CrossRef - Association between underweight and tooth loss among Korean adults
In-Seok Song, Kyungdo Han, Jae-Jun Ryu, Jun-Beom Park
Scientific Reports.2017;[Epub] CrossRef - Variability in glycated albumin levels predicts the progression of diabetic nephropathy
Su Bin Park, Sang Soo Kim, In Joo Kim, Yoon Jeong Nam, Kang Hee Ahn, Jong Ho Kim, Yun Kyung Jeon, Bo Hyun Kim, Sang Heon Song, Ihm Soo Kwak, Eun Kyung Lee, Yong Ki Kim
Journal of Diabetes and its Complications.2017; 31(6): 1041. CrossRef - Low serum bilirubin level predicts the development of chronic kidney disease in patients with type 2 diabetes mellitus
Kang Hee Ahn, Sang Soo Kim, Won Jin Kim, Jong Ho Kim, Yun Jeong Nam, Su Bin Park, Yun Kyung Jeon, Bo Hyun Kim, In Joo Kim, Yong Ki Kim
The Korean Journal of Internal Medicine.2017; 32(5): 875. CrossRef - Periodontitis is associated with diabetic retinopathy in non-obese adults
Su Jeong Song, Seong-su Lee, Kyungdo Han, Jun-Beom Park
Endocrine.2017; 56(1): 82. CrossRef - Baseline Cardiovascular Characteristics of Adult Patients with Chronic Kidney Disease from the KoreaN Cohort Study for Outcomes in Patients With Chronic Kidney Disease (KNOW-CKD)
Hyoungnae Kim, Tae-Hyun Yoo, Kyu Hun Choi, Kook-Hwan Oh, Joongyub Lee, Soo Wan Kim, Tae Hee Kim, Suah Sung, Seung Hyeok Han
Journal of Korean Medical Science.2017; 32(2): 231. CrossRef - Addition of nonalbumin proteinuria to albuminuria improves prediction of type 2 diabetic nephropathy progression
Jong Ho Kim, Seo Young Oh, Eun Heui Kim, Min Jin Lee, Yun Kyung Jeon, Bo Hyun Kim, Jin Mi Kim, Yong Ki Kim, Sang Soo Kim, In Joo Kim
Diabetology & Metabolic Syndrome.2017;[Epub] CrossRef - Smoking and the risk of diabetic nephropathy in patients with type 1 and type 2 diabetes: a meta-analysis of observational studies
Ning Jiang, Feng Huang, Xiurong Zhang
Oncotarget.2017; 8(54): 93209. CrossRef - Treatment of diabetic kidney disease: current and future targets
Mi-Kyung Kim
The Korean Journal of Internal Medicine.2017; 32(4): 622. CrossRef - Analysis and comparison of the cost-effectiveness of statins according to the baseline low-density lipoprotein cholesterol level in Korea
Y. J. Jeong, H. Kim, S. J. Baik, T. M. Kim, S. J. Yang, S.-H. Lee, J.-H. Cho, H. Lee, H. W. Yim, I. Y. Choi, K.-H. Yoon, H.-S. Kim
Journal of Clinical Pharmacy and Therapeutics.2017; 42(3): 292. CrossRef - Mechanistic Insight and Management of Diabetic Nephropathy: Recent Progress and Future Perspective
Rui Xue, Dingkun Gui, Liyang Zheng, Ruonan Zhai, Feng Wang, Niansong Wang
Journal of Diabetes Research.2017; 2017: 1. CrossRef - Nonalbuminuric Renal Insufficiency: Can It Be a Novel Category of Diabetic Nephropathy?
Masami Tanaka, Hiroshi Itoh
Endocrinology and Metabolism.2016; 31(4): 533. CrossRef - Current Challenges in Diabetic Nephropathy: Early Diagnosis and Ways to Improve Outcomes
Sang Soo Kim, Jong Ho Kim, In Joo Kim
Endocrinology and Metabolism.2016; 31(2): 245. CrossRef - Functional mechanisms for diabetic nephropathy-associated genetic variants
Chengxin Gong, Yonghu Xu, Yongfang Fan, Xingzi Liu, Chaopeng Xiong, Luling He, Changle Liu, Shenqiang Rao, Wen Xiao, Lu Ding, Lan Tang, Fangfang Hu, Mengqi Xiong, Mei Yang, Shangdong Liang, Hong Xu
Genes & Genomics.2016; 38(7): 595. CrossRef - Factors Influencing Intention to Receive Examination of Diabetes Complications
Yi-Lin Hsieh, Fang-Hsin Lee, Chien-Liang Chen, Ming-Fong Chang, Pei-Hsuan Han
Asian Nursing Research.2016; 10(4): 289. CrossRef - Associations between the number of natural teeth and renal dysfunction
Hye Min Choi, Kyungdo Han, Yong Gyu Park, Jun-Beom Park
Medicine.2016; 95(34): e4681. CrossRef - Decreased plasma α-Klotho predict progression of nephropathy with type 2 diabetic patients
Sang Soo Kim, Sang Heon Song, In Joo Kim, Eun Young Lee, Su Mi Lee, Choon Hee Chung, Ihm Soo Kwak, Eun Kyung Lee, Yong Ki Kim
Journal of Diabetes and its Complications.2016; 30(5): 887. CrossRef - The Association Between Smoking Tobacco After a Diagnosis of Diabetes and the Prevalence of Diabetic Nephropathy in the Korean Male Population
Hyungseon Yeom, Jung Hyun Lee, Hyeon Chang Kim, Il Suh
Journal of Preventive Medicine and Public Health.2016; 49(2): 108. CrossRef - Effects of Small Dense LDL in Diabetic Nephropathy in Females with Type 2 Diabetes Mellitus
Seongyul Ryu, Youngwoo Kim, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Hyun Baek, Ki-Ho Song, Kyung-Jin Yun
Journal of Lipid and Atherosclerosis.2016; 5(1): 11. CrossRef - Translational genomics for human diseases: toward a new era of precision medicine
Yoon Shin Cho, Ki Wha Chung, Nam-Soo Kim
Genes & Genomics.2016; 38(7): 573. CrossRef - Lipoprotein(a) predicts a new onset of chronic kidney disease in people with Type 2 diabetes mellitus
J.‐S. Yun, Y.‐B. Ahn, K.‐H. Song, K.‐D. Yoo, Y.‐M. Park, H.‐W. Kim, S.‐H. Ko
Diabetic Medicine.2016; 33(5): 639. CrossRef - The association between abnormal heart rate variability and new onset of chronic kidney disease in patients with type 2 diabetes: A ten-year follow-up study
Jae-Seung Yun, Yu-Bae Ahn, Ki-Ho Song, Ki-Dong Yoo, Hyung-Wook Kim, Yong-Moon Park, Seung-Hyun Ko
Diabetes Research and Clinical Practice.2015; 108(1): 31. CrossRef - Central obesity is an independent risk factor for microalbuminuria in both the general Korean women and nondiabetic nonhypertensive subpopulation: Association of microalbuminuria and metabolic syndrome from the Korea National Health and Nutrition Examinat
John Hoon Rim, Yong-ho Lee, Bong-Soo Cha, Sang-Guk Lee, Jeong-Ho Kim
Clinica Chimica Acta.2015; 448: 74. CrossRef - Diabetic Kidney Disease: From Epidemiology to Clinical Perspectives
Cheol Whee Park
Diabetes & Metabolism Journal.2014; 38(4): 252. CrossRef
- Associations between dietary patterns and renal impairment in individuals with diabetes: a cross‐sectional study
- Subclinical Hypothyroidism Is Independently Associated with Microalbuminuria in a Cohort of Prediabetic Egyptian Adults
- Mervat M. El-Eshmawy, Hala A. Abd El-Hafez, Walaa Othman El Shabrawy, Ibrahim A. Abdel Aal
- Diabetes Metab J. 2013;37(6):450-457. Published online December 12, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.6.450
- 3,280 View
- 36 Download
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Recent evidence has suggested an association between subclinical hypothyroidism (SCH) and microalbuminuria in patients with type 2 diabetes. However, whether SCH is related to microalbuminuria among subjects with prediabetes has not been studied. Thus, we evaluated the association between SCH and microalbuminuria in a cohort of prediabetic Egyptian adults.
Methods A total of 147 prediabetic subjects and 150 healthy controls matched for age and sex were enrolled in this study. Anthropometric measurements, plasma glucose, lipid profile, homeostasis model assessment of insulin resistance (HOMA-IR), thyroid stimulating hormone (TSH), free thyroxine, triiodothyronine levels, and urinary albumin-creatinine ratio (UACR) were assessed.
Results The prevalence of SCH and microalbuminuria in the prediabetic subjects was higher than that in the healthy controls (16.3% vs. 4%,
P <0.001; and 12.9% vs. 5.3%,P =0.02, respectively). Prediabetic subjects with SCH were characterized by significantly higher HOMA-IR, TSH levels, UACR, and prevalence of microalbuminuria than those with euthyroidism. TSH level was associated with total cholesterol (P =0.05), fasting insulin (P =0.01), HOMA-IR (P =0.01), and UACR (P =0.005). UACR was associated with waist circumference (P =0.01), fasting insulin (P =0.05), and HOMA-IR (P =0.02). With multiple logistic regression analysis, SCH was associated with microalbuminuria independent of confounding variables (β=2.59;P =0.01).Conclusion Our findings suggest that prediabetic subjects with SCH demonstrate higher prevalence of microalbuminuria than their non-SCH counterparts. SCH is also independently associated with microalbuminuria in prediabetic subjects. Screening and treatment for SCH may be warranted in those patients.
-
Citations
Citations to this article as recorded by- The prevalence of subclinical hypothyroidism in a pre-diabetes population and an analysis of related factors
Xingyu Chang, Yaqi Wang, Yi Liu, Yanyu Shen, Jiaqing Feng, Qianqian Liu, Chenjun Jiang, Jing Yu, Xulei Tang, Gaojing Jing, Qianglong Niu, Songbo Fu
Annals of Medicine.2023; 55(1): 643. CrossRef - High Thyroid-Stimulating Hormone and Low Free Triiodothyronine Levels Are Associated with Chronic Kidney Disease in Three Population-Based Studies from Germany
Till Ittermann, Sabrina von Rheinbaben, Marcello R. P. Markus, Marcus Dörr, Antje Steveling, Matthias Nauck, Alexander Teumer, Maik Gollasch, Dominik Spira, Maximilian König, Ilja Demuth, Elisabeth Steinhagen-Thiessen, Henry Völzke, Sylvia Stracke
Journal of Clinical Medicine.2023; 12(17): 5763. CrossRef - Free triiodothyronine predicts the risk of developing diabetic kidney disease
Weihong Li, Zhi Yang, Shengjian Li, Shanshan Jiang, Wan Hu, Zhenying Wan, Ping Tu, Peng Duan
BMC Nephrology.2023;[Epub] CrossRef - The Correlation between Thyroid Hormone Levels and the Kidney Disease Progression Risk in Patients with Type 2 Diabetes
Zhi Yang, Peng Duan, Weihong Li, Ronghui Nie, Xiaoyang Lou, Lina Wang, Kexia Wu, Jiang Liu, Ping Tu, Xiaoyang Lai
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 59. CrossRef - Thyroid hormone status in patients with impaired kidney function
Juliane Peters, Stefanos Roumeliotis, Peter R. Mertens, Vassilios Liakopoulos
International Urology and Nephrology.2021; 53(11): 2349. CrossRef - Subclinical hypothyroidism is associated with albuminuria in Japanese nondiabetic subjects
Akiko Toda, Shigeko Hara, Hiroshi Tsuji, Yasuji Arase
Endocrine.2020; 68(3): 592. CrossRef - Hypothyroidism and Kidney Function: A Mendelian Randomization Study
Christina Ellervik, Samia Mora, Paul M. Ridker, Daniel I. Chasman
Thyroid.2020; 30(3): 365. CrossRef - Relationship between serum thyrotropin and urine albumin excretion in euthyroid subjects with diabetes
Gautam Das, Peter N Taylor, Hussam Abusahmin, Amer Ali, Brian P Tennant, John Geen, Onyebuchi Okosieme
Annals of Clinical Biochemistry: International Journal of Laboratory Medicine.2019; 56(1): 155. CrossRef - The longitudinal effect of subclinical hypothyroidism on urine microalbumin-to-urine creatinine ratio in patients with type 2 diabetes mellitus
Juan Xie, Xiaoqing Wang, Yiyuan Zhang, Hailun Li, Yong Xu, Donghui Zheng
BMC Endocrine Disorders.2019;[Epub] CrossRef - The effect of l-thyroxine substitution on oxidative stress in early-stage diabetic nephropathy patients with subclinical hypothyroidism: a randomized double-blind and placebo-controlled study
Yong Chen, Ganlin Wu, Meirong Xu
International Urology and Nephrology.2018; 50(1): 97. CrossRef - Association between subclinical hypothyroidism and diabetic nephropathy in type 2 diabetes
Ayman Abd-Elrahman Mohamed Nsr-Allah, Azza H. Abd-El Fatah, Mahmoud Azab, Maggie M. Fawzi
The Egyptian Journal of Internal Medicine.2018; 30(3): 160. CrossRef - Role of Microalbuminuria in Predicting Cardiovascular Mortality in Individuals With Subclinical Hypothyroidism
Tushar A. Tuliani, Maithili Shenoy, Kevin Belgrave, Abhishek Deshmukh, Sadip Pant, Anthony Hilliard, Luis Afonso
The American Journal of the Medical Sciences.2017; 354(3): 285. CrossRef - Inositol(s) in thyroid function, growth and autoimmunity
Salvatore Benvenga, Alessandro Antonelli
Reviews in Endocrine and Metabolic Disorders.2016; 17(4): 471. CrossRef - Hypothyroïdie infra-clinique et risque d’évènements cardiovasculaires chez la femme diabétique de type 2
M. Gourine, K. Bentadj, S. Mostefa-Kara, A. Cherrak, S. Halimi, M. Belhadj
Médecine des Maladies Métaboliques.2016; 10(5): 466. CrossRef - Can levothyroxine treatment reduce urinary albumin excretion rate in patients with early type 2 diabetic nephropathy and subclinical hypothyroidism? A randomized double-blind and placebo-controlled study
Peng Liu, Ruidong Liu, Xia Chen, Yingying Chen, Debao Wang, Fengmei Zhang, Yangang Wang
Current Medical Research and Opinion.2015; 31(12): 2233. CrossRef - Free Triiodothyronine Levels Are Associated with Diabetic Nephropathy in Euthyroid Patients with Type 2 Diabetes
Jingcheng Wu, Xiaohua Li, Yang Tao, Yufei Wang, Yongde Peng
International Journal of Endocrinology.2015; 2015: 1. CrossRef - Letter: Subclinical Hypothyroidism Is Independently Associated with Microalbuminuria in a Cohort of Prediabetic Egyptian Adults (Diabetes Metab J2013;37:450-7)
In-Kyung Jeong
Diabetes & Metabolism Journal.2014; 38(1): 83. CrossRef - Free Triiodothyronine Concentrations Are Inversely Associated with Microalbuminuria
Yulin Zhou, Lei Ye, Tiange Wang, Jie Hong, Yufang Bi, Jie Zhang, Baihui Xu, Jichao Sun, Xiaolin Huang, Min Xu
International Journal of Endocrinology.2014; 2014: 1. CrossRef - Thyroid hormone and heart failure: from myocardial protection to systemic regulation
Laura Sabatino, Giorgio Iervasi, Alessandro Pingitore
Expert Review of Cardiovascular Therapy.2014; 12(10): 1227. CrossRef
- The prevalence of subclinical hypothyroidism in a pre-diabetes population and an analysis of related factors
- Chronic Kidney Disease and Associated Cardiovascular Risk Factors in Chinese with Type 2 Diabetes
- Qing-Lin Lou, Xiao-Jun Ouyang, Liu-Bao Gu, Yong-Zhen Mo, Ronald Ma, Jennifer Nan, Alice Kong, Wing-Yee So, Gary Ko, Juliana Chan, Chun-Chung Chow, Rong-Wen Bian
- Diabetes Metab J. 2012;36(6):433-442. Published online December 12, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.6.433
- 3,772 View
- 42 Download
- 25 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background To determine the frequency of chronic kidney disease (CKD) and its associated risk factors in Chinese type 2 diabetic patients, we conducted a cross-sectional study in Nanjing, China, in the period between January 2008 and December 2009.
Methods Patients with type 2 diabetes under the care by Jiangsu Province Official Hospital, Nanjing, China were invited for assessment. CKD was defined as the presence of albuminuria or estimated glomerular filtration rate <60 mL/min/1.73 m2. Albuminuria was defined as urinary albumin-to-creatinine ratio ≥30 mg/g.
Results We recruited 1,521 urban Chinese patients with type 2 diabetes (mean age, 63.9±12.0 years). The frequency of CKD and albuminuria was 31.0% and 28.9%, respectively. After adjusted by age and sex, hypertension, anemia and duration of diabetes were significantly associated with CKD with odds ratio (95% confidence interval) being 1.93 (1.28 to 2.93), 1.70 (1.09 to 2.64), and 1.03 (1.00 to 1.06), respectively.
Conclusion In conclusion, CKD was common in the urban Nanjing Chinese with type 2 diabetes. Strategies to prevent or delay progression of kidney disease in diabetes should be carried out at the early disease course of type 2 diabetes.
-
Citations
Citations to this article as recorded by- Associations between dietary patterns and renal impairment in individuals with diabetes: a cross‐sectional study
Ziling Ding, Xingzhe Wu, Chao Liu, Ruixue Ying, Yi Zhang, Shiqi Zhang, Qiu Zhang, Honglin Hu, Fang Dai
Journal of Human Nutrition and Dietetics.2024; 37(1): 193. CrossRef - A Randomised Controlled Study of Can Ling Bai Shu San Combined with Guizhi Fuling Pills and Dagliflozin in the Treatment of Proteinuria in Type 2 Diabetic Nephropathy Stage IV
杰 张
Advances in Clinical Medicine.2024; 14(01): 1829. CrossRef - Evaluation of Renal Impairment in Patients with Diabetic Kidney Disease by Integrated Chinese and Western Medicine
Yi-lun Qu, Zhe-yi Dong, Hai-mei Cheng, Qian Liu, Qian Wang, Hong-tao Yang, Yong-hui Mao, Ji-jun Li, Hong-fang Liu, Yan-qiu Geng, Wen Huang, Wen-hu Liu, Hui-di Xie, Fei Peng, Shuang Li, Shuang-shuang Jiang, Wei-zhen Li, Shu-wei Duan, Zhe Feng, Wei-guang Zh
Chinese Journal of Integrative Medicine.2023; 29(4): 308. CrossRef - Extracellular status of thrombospondin-2 in type 2 diabetes mellitus and utility as a biomarker in the determination of early diabetic kidney disease
Zhenzhen Lin, Didong Zhang, Xinxin Zhang, Wanxie Guo, Wenjun Wang, Yingchao Zhang, Zhen Liu, Yanxue Bi, Maolan Wu, Zhuofeng Lin, Xuemian Lu
BMC Nephrology.2023;[Epub] CrossRef - Serum Lipocalin-2 Levels Are Increased and Independently Associated With Early-Stage Renal Damage and Carotid Atherosclerotic Plaque in Patients With T2DM
Jing Gan, Yu Zheng, Qiongli Yu, Yingchao Zhang, Wei Xie, Yaru Shi, Ning Yu, Yu Yan, Zhuofeng Lin, Hong Yang
Frontiers in Endocrinology.2022;[Epub] CrossRef - The Prevalence, Progress and Risk Factor Control of Chronic Kidney Disease in Chinese Adults With Type 2 Diabetes Mellitus in Primary Care
Lingwang An, Qiuzhi Yu, Hong Tang, Xianglan Li, Dandan Wang, Qi Tang, Haiyang Xing, Yali He, Xiaona Zhao, Shuhui Zhao, Yaujiunn Lee, Juming Lu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Hydration status according to impedance vectors and its association with clinical and biochemical outcomes and mortality in patients with chronic kidney disease
Paola Vanessa Miranda Alatriste, Eloísa Colin Ramírez, Ximena Atilano Carsi, Cristino Cruz-Rivera, Ángeles Espinosa-Cuevas
Nutrición Hospitalaria.2022;[Epub] CrossRef - The Prevalence of Diabetic Microvascular Complications in China and the USA
Yu Kuei Lin, Bixia Gao, Lili Liu, Lynn Ang, Kara Mizokami-Stout, Rodica Pop-Busui, Luxia Zhang
Current Diabetes Reports.2021;[Epub] CrossRef - Reno-protective potential of sodium glucose cotransporter-2 (SGLT2) inhibitors: Summary evidence from clinical and real-world data
Niti Mittal, Vikas Sehray, Rakesh Mittal, Surjit Singh
European Journal of Pharmacology.2021; 907: 174320. CrossRef - Association between Renal Podocalyxin Expression and Renal Dysfunction in Patients with Diabetic Nephropathy: A Single-Center, Retrospective Case-Control Study
Rongzhen Wang, Can Yao, Feng Liu
BioMed Research International.2020; 2020: 1. CrossRef - Renoprotection with SGLT2 inhibitors in type 2 diabetes over a spectrum of cardiovascular and renal risk
Francesco Giorgino, Jiten Vora, Peter Fenici, Anna Solini
Cardiovascular Diabetology.2020;[Epub] CrossRef - Prevalence of diabetic nephropathy among Chinese patients with type 2 diabetes mellitus and different categories of their estimated glomerular filtration rate based on the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation in primary car
Ka Yee Mok, Pang Fai Chan, Loretta K. P. Lai, Kai Lim Chow, David V. K. Chao
Journal of Diabetes & Metabolic Disorders.2019; 18(2): 281. CrossRef - The association between serum uric acid to creatinine ratio and renal disease progression in type 2 diabetic patients in Chinese communities
Yao Chunlei, Gu Liubao, Wang Tao, Xing Changying
Journal of Diabetes and its Complications.2019; 33(7): 473. CrossRef - Risk factors of chronic kidney diseases in Chinese adults with type 2 diabetes
Lin Yang, Tsun Kit Chu, Jinxiao Lian, Cheuk Wai Lo, Pak Ki Lau, Hairong Nan, Jun Liang
Scientific Reports.2018;[Epub] CrossRef - Any grade of relative overhydration is associated with long-term mortality in patients with Stages 4 and 5 non-dialysis chronic kidney disease
Almudena Vega, Soraya Abad, Nicolás Macías, Inés Aragoncillo, Ana García-Prieto, Tania Linares, Esther Torres, Andrés Hernández, José Luño
Clinical Kidney Journal.2018; 11(3): 372. CrossRef - The impact of the quality of care and other factors on progression of chronic kidney disease in Thai patients with Type 2 Diabetes Mellitus: A nationwide cohort study
Paithoon Sonthon, Supannee Promthet, Siribha Changsirikulchai, Ram Rangsin, Bandit Thinkhamrop, Suthee Rattanamongkolgul, Cameron P. Hurst, Cheng Hu
PLOS ONE.2017; 12(7): e0180977. CrossRef - Association of Chronic Kidney Disease with Coronary Heart Disease and Stroke Risks in Patients with Type 2 Diabetes Mellitus
Xue Sun, Jie He, Xiao-Li Ji, Yi-Ming Zhao, Han-Yu Lou, Xiao-Xiao Song, Li-Zhen Shan, Ying-Xiu Kang, Wen-Heng Zeng, Xiao-Hong Pang, Song-Zhao Zhang, Yue Ding, Yue-Zhong Ren, Peng-Fei Shan
Chinese Medical Journal.2017; 130(1): 57. CrossRef - Prevalence of chronic kidney disease and associated factors in Chinese individuals with type 2 diabetes: Cross-sectional study
Kaifeng Guo, Lei Zhang, Fangya Zhao, Junxi Lu, Pan Pan, Haoyong Yu, Yuqian Bao, Haibing Chen, Weiping Jia
Journal of Diabetes and its Complications.2016; 30(5): 803. CrossRef - The association between abnormal heart rate variability and new onset of chronic kidney disease in patients with type 2 diabetes: A ten-year follow-up study
Jae-Seung Yun, Yu-Bae Ahn, Ki-Ho Song, Ki-Dong Yoo, Hyung-Wook Kim, Yong-Moon Park, Seung-Hyun Ko
Diabetes Research and Clinical Practice.2015; 108(1): 31. CrossRef - Association of elevated glycosylated hemoglobin A1c with hyperfiltration in a middle-aged and elderly Chinese population with prediabetes or newly diagnosed diabetes: a cross-sectional study
Wen Hu, Hairong Hao, Weinan Yu, Xiaojuan Wu, Hongwen Zhou
BMC Endocrine Disorders.2015;[Epub] CrossRef - Prevalence of Chronic Kidney Disease in Adults with Type 2 Diabetes Mellitus
Serena KM Low, Chee Fang Sum, Lee Ying Yeoh, Subramaniam Tavintharan, Xiao Wei Ng, Simon BM Lee, Wern Ee Tang, Su Chi Lim
Annals of the Academy of Medicine, Singapore.2015; 44(5): 164. CrossRef - Low Ankle-Brachial Index Is Associated with Early-Stage Chronic Kidney Disease in Type 2 Diabetic Patients Independent of Albuminuria
Xuehong Dong, Dingting Wu, Chengfang Jia, Yu Ruan, Xiaocheng Feng, Guoxing Wang, Jun Liu, Yi Shen, Hong Li, Lianxi Li, Karin Jandeleit-Dahm
PLoS ONE.2014; 9(10): e109641. CrossRef - Health Behaviors and Risk Factors Associated with Chronic Kidney Disease in Korean Patients with Diabetes: The Fourth Korean National Health and Nutritional Examination Survey
Suk Jeong Lee, Chae Weon Chung
Asian Nursing Research.2014; 8(1): 8. CrossRef - Urinary miR-29 Correlates with Albuminuria and Carotid Intima-Media Thickness in Type 2 Diabetes Patients
Hui Peng, Meirong Zhong, Wenbo Zhao, Cheng Wang, Jun Zhang, Xun Liu, Yuanqing Li, Sujay Dutta Paudel, Qianqian Wang, Tanqi Lou, Emmanuel A. Burdmann
PLoS ONE.2013; 8(12): e82607. CrossRef - Diabetes and its comorbidities—where East meets West
Alice P. S. Kong, Gang Xu, Nicola Brown, Wing-Yee So, Ronald C. W. Ma, Juliana C. N. Chan
Nature Reviews Endocrinology.2013; 9(9): 537. CrossRef
- Associations between dietary patterns and renal impairment in individuals with diabetes: a cross‐sectional study
- Serum Cystatin C Reflects the Progress of Albuminuria
- Jeong Seon Yoo, Young Mi Lee, Eun Hae Lee, Ji Woon Kim, Shin Young Lee, Ki-Cheon Jeong, Shin Ae Kang, Jong Suk Park, Joo Young Nam, Chul Woo Ahn, Young Duk Song, Kyung Rae Kim
- Diabetes Metab J. 2011;35(6):602-609. Published online December 26, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.6.602
- 4,538 View
- 38 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Research on the relationship between urinary albumin excretion and serum cystatin C in diabetes is restricted to cross-sectional studies. In this study, we investigated how well serial measurements of serum cystatin C level reflect changes in the urinary albumin excretion rate.
Methods We enrolled and retrospectively collected data on 1,058 participants with type 2 diabetes who were older than 18 years and who had more than 3 years of follow-up with serial measurements of albuminuria and serum cystatin C at an outpatient clinic.
Results With the use of a linear mixed model, we found that the albuminuria level for each patient over time corresponded with the annual change in serum cystatin C-based estimated glomerular filtration rate (cysC-eGFR) but did not correspond with the creatinine-based eGFR calculated by the modification of diet in renal disease formula (MDRD-eGFR). The discrepancy in the direction of the trend was smaller with cysC-eGFR than with MDRD-eGFR.
Conclusion Serum cystatin C level reflects the trend in albuminuria level more accurately than serum creatinine level in Korean type 2 diabetes mellitus patients.
-
Citations
Citations to this article as recorded by- Assessment of Cystatin C and Microalbumin as Biomarkers for Nephropathy in Patients with Type 2 Diabetes Mellitus
Bhuneshwar Yadav, Shashidhar K.N, Raveesha A, Muninarayana C.
Journal of Evolution of Medical and Dental Sciences.2021; 10(25): 1866. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Eugene Han, Mi Kyung Kim, Byoung Kuk Jang, Hye Soon Kim
Diabetes & Metabolism Journal.2021; 45(5): 698. CrossRef - Increase of BACE1, Brain-Renal Risk Factor, Contributes to Kidney Damage in an Alzheimer’s Disease Mouse Model
Yan Shi, Feng Gao, Xiaoli Yang, Dongwei Liu, Qiuxia Han, Zhangsuo Liu, Hanyu Zhu, Yong Shen
Journal of Alzheimer's Disease.2020; 76(1): 237. CrossRef - Lower Leg Fat Depots Are Associated with Albuminuria Independently of Obesity, Insulin Resistance, and Metabolic Syndrome (Korea National Health and Nutrition Examination Surveys 2008 to 2011)
Eugene Han, Nan Hee Cho, Mi Kyung Kim, Hye Soon Kim
Diabetes & Metabolism Journal.2019; 43(4): 461. CrossRef - Evaluation of creatinine-based and cystatin C-based equations for estimation of glomerular filtration rate in type 1 diabetic patients
Caroline Pereira Domingueti, Rodrigo Bastos Fóscolo, Ana Cristina Simões e Silva, Luci Maria S. Dusse, Janice Sepúlveda Reis, Maria das Graças Carvalho, Ana Paula Fernandes, Karina Braga Gomes
Archives of Endocrinology and Metabolism.2016; 60(2): 108. CrossRef
- Assessment of Cystatin C and Microalbumin as Biomarkers for Nephropathy in Patients with Type 2 Diabetes Mellitus
- Serum Visfatin and Fetuin-A Levels and Glycemic Control in Patients with Obese Type 2 Diabetes Mellitus
- Fethiye Oztop Gunduz, Sembol Turkmen Yildirmak, Mustafa Temizel, Yilmaz Faki, Mustafa Cakmak, Mustafa Durmuscan, Funda Sezgin
- Diabetes Metab J. 2011;35(5):523-528. Published online October 31, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.5.523
- 65,535 View
- 29 Download
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Visfatin is an adipokine produced by visceral adipose tissue and has insulin-mimicking effects. Fetuin-A is a hepatic secretory protein that binds the insulin receptor and inhibits insulin action both
in vivo andin vitro . The authors of the present study aimed to investigate the levels of serum visfatin and fetuin-A and their correlation with hemoglobin A1c (HbA1c) and urine albumin levels in patients with type 2 diabetes mellitus (T2DM).Methods A total of 40 obese patients with T2DM (11 males and 29 females; age, 54.47±10.83 years and 23 obese nondiabetic controls (8 males and 15 females; age, 53.04±11.33 years) were included in the study. Age, sex, and body mass index were similar in the 2 groups. Serum visfatin and fetuin-A levels were measured by enzyme-linked immunosorbent assay. HbA1c and urine albumin levels were measured by high performance liquid chromatography and nephelometric method, respectively.
Results Serum levels of visfatin in patients with T2DM (4.03±2.44 ng/mL) were similar to the control group (3.65±3.02 ng/mL). Serum fetuin-A levels were significantly lower in patients with T2DM than the controls (298.75±78.86 and 430.73±94.46 µg/mL, respectively). HbA1c levels were significantly higher in the T2DM group compared with controls (7.33±1.32 and 5.44±0.84%, respectively). Correlations between visfatin, fetuin-A and HbA1c levels were not observed.
Conclusion The present study suggests fetuin-A may play a role in the pathogenesis of T2DM.
-
Citations
Citations to this article as recorded by- Assessment of serum and salivary visfatin levels in newly diagnosed patients of type-II DM
Faith R. Jerusha, Vandana Raghunath
Journal of Oral and Maxillofacial Pathology.2023; 27(4): 663. CrossRef - Evaluation of the serum visfatin eotaxin and fetuin-A levels of patients with type 2 diabetes mellitus
Hacer KAYHAN KAYA, Abdurrahman ŞERMET, Zafer PEKKOLAY, Ezel TAŞDEMİR, Dilek AYGÜN KEŞİM
Anatolian Current Medical Journal.2022; 4(1): 113. CrossRef - The Association Between Three Adipocytokines (Adiponectin, Resistin and Visfatin) And Thyroid Status in Patients With Type 2 Diabetes Mellitus and Autoimmune Thyroiditis
Š. Sotak, Z. Schroner, I. Lazúrová, M. Felšőci, I. Jochmanová, D. Petrášová, I. Bertková, M. Mitníková, B. Nováková, H. Wagnerová, O. Bobelová
Physiological Research.2021; (6): 865. CrossRef - Prediction of gestational diabetes mellitus in the first trimester: comparison of maternal fetuin-A, N-terminal proatrial natriuretic peptide, high-sensitivity C-reactive protein, and fasting glucose levels
Hatice Kansu-Celik, A. Seval Ozgu-Erdinc, Burcu Kisa, Rahime Bedir Findik, Canan Yilmaz, Yasemin Tasci
Archives of Endocrinology and Metabolism.2019;[Epub] CrossRef - The association between circulating fetuin-A levels and type 2 diabetes mellitus risk: systematic review and meta-analysis of observational studies
F. Roshanzamir, M. Miraghajani, M. H. Rouhani, M. Mansourian, R. Ghiasvand, S. M. Safavi
Journal of Endocrinological Investigation.2018; 41(1): 33. CrossRef - Fetuin-A level in type 2 diabetic patients: relation to microvascular complications
Nehal H. Al-Said, Fatma M. Taha, Ghada M. Abdel-Aziz, Marwa S. Abdel-Tawab
The Egyptian Journal of Internal Medicine.2018; 30(3): 121. CrossRef - Serum levels of fetuin A are increased in women with gestational diabetes mellitus
Ozlem Turhan Iyidir, Ceyla Konca Degertekin, Banu Aktas Yilmaz, Alev E. Altinova, Fusun B. Toruner, Nuray Bozkurt, Goksun Ayvaz, Mujde Akturk
Archives of Gynecology and Obstetrics.2015; 291(4): 933. CrossRef - Lower Fetuin-A, Retinol Binding Protein 4 and Several Metabolites after Gastric Bypass Compared to Sleeve Gastrectomy in Patients with Type 2 Diabetes
Mia Jüllig, Shelley Yip, Aimin Xu, Greg Smith, Martin Middleditch, Michael Booth, Richard Babor, Grant Beban, Rinki Murphy, Pankaj K. Singh
PLoS ONE.2014; 9(5): e96489. CrossRef - Preventive roles of swimming exercise and pioglitazone treatment on hepatic dysfunction in a rat model of metabolic syndrome
Hussein F. Sakr, Fahaid H. Al-Hashem, Waffaa M. Hassab El-Naby, Mahmoud A. Alkhateeb, Mohamed Samir A. Zaki, Hesham M. El Refaey, Mohamed D. Morsy
Canadian Journal of Physiology and Pharmacology.2014; 92(2): 162. CrossRef - Relationship between circulating visfatin/NAMPT, nutritional status and insulin resistance in an elderly population – results from the PolSenior substudy
Magdalena Olszanecka-Glinianowicz, Aleksander Owczarek, Maria Bożentowicz-Wikarek, Aniceta Brzozowska, Małgorzata Mossakowska, Tomasz Zdrojewski, Tomasz Grodzicki, Andrzej Więcek, Jerzy Chudek
Metabolism.2014; 63(11): 1409. CrossRef
- Assessment of serum and salivary visfatin levels in newly diagnosed patients of type-II DM
- Homocysteine as a Risk Factor for Development of Microalbuminuria in Type 2 Diabetes
- Eun-Hee Cho, Eun Hee Kim, Won Gu Kim, Eun Hui Jeong, Eun Hee Koh, Woo-Je Lee, Min-Seon Kim, Joong-Yeol Park, Ki-Up Lee
- Korean Diabetes J. 2010;34(3):200-206. Published online June 30, 2010
- DOI: https://doi.org/10.4093/kdj.2010.34.3.200
- 3,579 View
- 26 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Kidney function is critical in homocysteine clearance, and plasma homocysteine level is frequently increased in patients with renal failure. On the other hand, recent studies in animals have shown that hyperhomocysteinemia induces renal injury. In this study, we determined whether hyperhomocysteinemia can be a risk factor for the development of microalbuminuria in patients with type 2 diabetes.
Methods A nested case-control study. Of 887 patients with type 2 diabetes who did not have microalbuminuria at baseline, 76 developed microalbuminuria during follow-up (mean, 36.0 ± 11.7 months; range, 18 to 76 months). The control group consisted of 152 age- and sex-matched subjects who did not develop microalbuminuria. Baseline plasma homocysteine concentrations were measured in stored samples.
Results Baseline plasma homocysteine concentrations and mean HbA1C levels during follow-up were significantly higher in patients who developed microalbuminuria than in those who remained normoalbuminuric. Multivariate logistic regression analysis showed that baseline plasma homocysteine level and mean HbA1C were independent predictors of microalbuminuria in type 2 diabetes.
Conclusion Hyperhomocysteinemia was associated with increased risk of microalbuminuria in patients with type 2 diabetes supporting the concept that hyperhomocysteinemia has an etiologic role in the pathogenesis of diabetic nephropathy.
-
Citations
Citations to this article as recorded by- Homocysteine and diabetes: Role in macrovascular and microvascular complications
Emir Muzurović, Ivana Kraljević, Mirsala Solak, Siniša Dragnić, Dimitri P. Mikhailidis
Journal of Diabetes and its Complications.2021; 35(3): 107834. CrossRef - Associations of Homocysteine with B Vitamins and Zinc in Serum Levels of Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Study
Sadako MATSUI, Chika HIRAISHI, Ryo SATO, Takai KOJIMA, Kiyotaka ANDO, Kei FUJIMOTO, Hiroshi YOSHIDA
Journal of Nutritional Science and Vitaminology.2021; 67(6): 417. CrossRef - A risk scoring system for the decreased glomerular filtration rate in Chinese general population
Yan Gu, Min Chen, Bei Zhu, Xiaohua Pei, Zhenzhu Yong, Xiaona Li, Qun Zhang, Weihong Zhao
Journal of Clinical Laboratory Analysis.2020;[Epub] CrossRef - Relationship between plasma total homocysteine and the severity of renal function in Chinese patients with type 2 diabetes mellitus aged ≥75 years
Ning Ma, Ning Xu, Dong Yin, Weiwei Liu, Mengping Wu, Xingbo Cheng
Medicine.2020; 99(27): e20737. CrossRef - Correlation between serum homocysteine level and ulcerative colitis: A meta-analysis
Yifang Zhong, Feng Yan, Weixia Jie, Ying Zhou, Fang Fang
Pteridines.2019; 30(1): 114. CrossRef - The role of molecular genetic alterations in genes involved in folate and homocysteine metabolism in multifactorial diseases pathogenesis
A. M. Burdennyy, V. I. Loginov, T. M. Zavarykina, E. A. Braga, A. A. Kubatiev
Russian Journal of Genetics.2017; 53(5): 528. CrossRef - МОЛЕКУЛЯРНО-ГЕНЕТИЧЕСКИЕ НАРУШЕНИЯ ГЕНОВ ФОЛАТНОГО И ГОМОЦИСТЕИНОВОГО ОБМЕНА В ПАТОГЕНЕЗЕ РЯДА МНОГОФАКТОРНЫХ ЗАБОЛЕВАНИЙ, "Генетика"
А. М. Бурдённый, В.И. Логинов, Т.М. Заварыкина, Э.А. Брага, А.А. Кубатиев
Генетика.2017; (5): 526. CrossRef - Association Between Plasma Homocysteine and Microalbuminuria in Untreated Patients with Essential Hypertension: a Case-Control Study
Ze-min Kuang, Ying Wang, Shu-jun Feng, Long Jiang, Wen-li Cheng
Kidney and Blood Pressure Research.2017; 42(6): 1303. CrossRef - NMDA Receptors as Potential Therapeutic Targets in Diabetic Nephropathy: Increased Renal NMDA Receptor Subunit Expression in Akita Mice and Reduced Nephropathy Following Sustained Treatment With Memantine or MK-801
Hila Roshanravan, Eun Young Kim, Stuart E. Dryer
Diabetes.2016; 65(10): 3139. CrossRef - Association between homocysteine status and the risk of nephropathy in type 2 diabetes mellitus
Song Mao, Wei Xiang, Songming Huang, Aihua Zhang
Clinica Chimica Acta.2014; 431: 206. CrossRef - Prevalence and Determinants of Diabetic Nephropathy in Korea: Korea National Health and Nutrition Examination Survey
Jae Hee Ahn, Ji Hee Yu, Seung-Hyun Ko, Hyuk-Sang Kwon, Dae Jung Kim, Jae Hyeon Kim, Chul Sik Kim, Kee-Ho Song, Jong Chul Won, Soo Lim, Sung Hee Choi, Kyungdo Han, Bong-Yun Cha, Nan Hee Kim
Diabetes & Metabolism Journal.2014; 38(2): 109. CrossRef - Plasma Homocysteine level and its clinical correlation with type 2 diabetes mellitus and its complications
Satyendra Kumar Sonkar, Gyanendra Kumar Sonkar, Deepika Soni, Dheeraj Soni, Kauser Usman
International Journal of Diabetes in Developing Countries.2014; 34(1): 3. CrossRef - Genetic Predisposition for Development of Nephropathy in Type 2 Diabetes Mellitus
Ravindra Kumar, Raj Kumar Sharma, Sarita Agarwal
Biochemical Genetics.2013; 51(11-12): 865. CrossRef - Is C677T Polymorphism in Methylenetetrahydrofolate Reductase Gene a Risk Factor for Diabetic Nephropathy or Diabetes Mellitus in a Chinese Population?
Wen-peng Cui, Bing Du, Ye Jia, Wen-hua Zhou, Sheng-mao Liu, Ying-chun Cui, Fu-zhe Ma, Ping Luo, Li-ning Miao
Archives of Medical Research.2012; 43(1): 42. CrossRef - The role of coagulation and inflammation in the development of diabetic nephropathy in patients withdiabetes mellitus type 2
Yulia Valer'evna Khasanova, Alsu Asatovna Nelaeva, Anna Borisovna Galkina, Irina Vasil'evna Medvedeva
Diabetes mellitus.2012; 15(1): 31. CrossRef
- Homocysteine and diabetes: Role in macrovascular and microvascular complications
- Association of Spot Urine Albumin-to-Creatinine Ratio and 24 Hour-Collected Urine Albumin Excretion Rate in Patients with Type 2 Diabetes Mellitus.
- Jee In Lee, Hyuk Sang Kwon, Su Jin Oh, Jung Min Lee, Sang Ah Chang, Bong Yun Cha, Hyun Shik Son, Tae Seo Sohn
- Korean Diabetes J. 2009;33(4):299-305. Published online August 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.4.299
- 2,678 View
- 29 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Measuring urine albumin in diabetic patients is an important screening test to identify those individuals at high risk for cardiovascular disease and the progression of kidney disease. Recently, spot urine albumin-to-creatinine ratio (ACR) has replaced 24 hour-collected urine albumin excretion rate (AER) as a screening test for microalbuminuria given its comparative simplicity. The purpose of the current study was to evaluate the degree of correlation between AER and ACR in the normal, microalbuminuric and macroalbuminuric ranges, and to identify the lower limits of ACR for both genders. METHODS: A total of 310 type 2 diabetics admitted to one center were enrolled in the present study. Following the collection of a spot urine sample, urine was collected for 24 hours and albumin content was measured in both specimens. RESULTS: Mean patient age was 60.2 years. A total of 25.4% had microalbuminuria and 15.8% had macroalbuminuria. The data revealed a strongly positive correlation between AER and ACR across all ranges of albuminuria (R = 0.8). The cut-off value of ACR for 30 mg/day of AER by the regression equation was 24 microgram/mg for men, 42 microgram/mg for women and 31.2 microgram/mg for all patients. The diagnostic performance expressed as the area under the curve (AUC) was 0.938 (95% CI, 0.911-0.965) for ACR. ACR revealed a sensitivity of 84% and specificity of 84%, when a cut-off value of 31.2 microgram/mg was employed. CONCLUSION: ACR was highly correlated with AER, particularly in the range of microalbuminuria. The gender combined cut-off value of ACR in type 2 diabetic patients was determined to be 31.2 microg/mg However, additional studies of large outpatient populations, as opposed to the inpatient population used in the present study, are required to confirm the utility of this value.
- The Association Between Urinary Albumin to Creatinine Ratio and Coronary Artery Calcification in Type 2 Diabetic Patients.
- Ju Young Lee, Yeon Kyung Choi, Hyun Ae Seo, Jae Han Jeon, Jung Eun Lee, Seong Su Moon, Jung Guk Kim, Bo Wan Kim, In Kyu Lee
- Korean Diabetes J. 2009;33(4):289-298. Published online August 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.4.289
- 2,186 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Atherosclerosis, the most common cause of death in type 2 diabetic patients, is closely associated with coronary artery calcium deposition. The coronary calcifications can be easily measured using coronary calcium scoring computed tomography (CT). And microalbuminuria is known as an independent risk factor of cardiovascular disease. So, we examined the association of urinary albumin to creatinine ratio (UACR) and coronary calcification score (CCS) in type 2 diabetic patients. METHODS: Among type 2 diabetic patients who underwent the multidetector CT scanning for the evaluation of CCS at Kyungpook National University Hospital between December 2007 and May 2008, 155 subjects were included. CCS, demographic and laboratory data were assessed. RESULTS: Coronary artery calcifications were identified in 90 patients (51%) and mean, median CCS was 205.8 +/- 476.9, 8.74 (0, 132.0). 60 subjects revealed UACR greater than 30 ug/mg. With the UACR increment, CCS revealed a significant increase (P < 0.001). Age, duration of diabetes, serum Apo A1 level, serum high sensitivity C-reactive protein (hs-CRP) level were also associated with CCS. However, after adjusting for age, UACR and CCS exhibited a significant positive relationship (P = 0.002). CONCLUSION: Increased UACR is associated with coronary artery calcification in type 2 diabetic patients and these results will be useful in early evaluating the presence of macrovascular complications in these patients.
- Frequency of Silent Myocardial Ischemia Detected by Thallium-201 SPECT in Patients with Type 2 Diabetes.
- Dong Woo Kim, Eun Hee Jung, Eun Hee Koh, Min Seon Kim, Joong Yeol Park, Seung Whan Lee, Seong Wook Park, Jin Sook Ryu, Ki Up Lee
- Korean Diabetes J. 2009;33(3):225-231. Published online June 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.3.225
- 1,785 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Silent myocardial ischemia (SMI) is more common in diabetic patients than among the general population. It is not yet established whether a routine screening test for SMI is necessary, and which screening test would be most useful. The purpose of this study was to estimate the prevalence of SMI detected by Thallium-201 perfusion single photon emission computed tomography (SPECT) in type 2 diabetic patients. METHODS: A total of 173 asymptomatic type 2 diabetic patients were included in the study. Thallium-201 perfusion SPECT was performed to screen for SMI. RESULTS: Among the 173 patients, abnormal perfusion patterns were found in 11 patients. Coronary angiography was carried out for these patients, and significant coronary artery stenosis was found in ten of them (positive predictive value; 90.9%). There was a significant association between SMI and overt albuminuria (OR = 7.33, 95% CI, 1.825-29.437). CONCLUSION: Thallium-201 perfusion SPECT is not sensitive enough to identify SMI, but is accurate in detecting decreased myocardial perfusion. This may be a useful screening tool for detecting SMI in type 2 diabetic patients with impaired renal function.
- Clinical Significance of Decreased Glomerular Filtration Rate (GFR) without Albuminuria among Type 2 Diabetics.
- Ji Eun Lee, Kyu Chang Won, Hyoung Woo Lee, Ji Sung Yoon
- Korean Diabetes J. 2008;32(3):252-258. Published online June 1, 2008
- DOI: https://doi.org/10.4093/kdj.2008.32.3.252
- 2,334 View
- 22 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Microalbuminuria in type 2 diabetes is a predictor of development of clinical nephropathy and cardiovascular disease. But, it has been reported that reduced glomerular filtration rate (GFR) may occur in some normoalbuminuric diabetic patients. The aim of this study was to identify whether decreased GFR without microalbuminuria is to predict diabetic vascular complications. METHODS: Between January 1998 and February 2001, 73 patients with type 2 diabetes who visited Yeungnam university medical center were divided into 5 groups according to initial GFR ranges: group 1 (GFR < 30 mL/min), group 2 (30 < or = GFR < 60 mL/min), group 3 (60 < or = GFR < 90 mL/min), group 4 (90 < or = GFR < 125 mL/min), group 5 (125 mL/min < or = GFR). They were examined for microvascular and macrovascular complications initially and after 4 years. RESULTS: Decreased GFR had a negative correlation with age (r = -0.472, P = 0.001). Decreased GFR without microalbuminuria had a significant correlation with development of diabetic nephropathy (P = 0.016) after 4 years. There were no significant correlation with the prevalence of diabetic retinopathy, peripheral neuropathy, and macrovacular disease. But, our study showed that coronary artery disease had an increasing tendency with decreased GFR without statistical significance (P = 0.085). CONCLUSIONS: Our data suggest that reduced GFR, independent of albuminuria, may be an important predictor of diabetic nephropathy and coronary artery disease to some extent. So we recommend that not only the microalbuminuria, but also the decrease in GFR should be evaluated at the follow-up of patients with type 2 diabetes. -
Citations
Citations to this article as recorded by- Screening and Management of Diabetic Nephropathy
Ji Sung Yoon
The Journal of Korean Diabetes.2013; 14(1): 19. CrossRef
- Screening and Management of Diabetic Nephropathy
- The Role of Glomerular Podocytes in Diabetic Nephropathy.
- Eun Young Lee, Choon Hee Chung
- Korean Diabetes J. 2007;31(6):451-454. Published online November 1, 2007
- DOI: https://doi.org/10.4093/jkda.2007.31.6.451
- 2,150 View
- 19 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Diabetic nephropathy is the most common cause of end-stage renal disease and accounts for significant morbidity and mortality among individuals with diabetes mellitus. Therefore, the clarification of the pathogenesis of diabetic nephropathy is an urgent issue. Podocytes cover the outer layer of the glomerulus and maintain its integrity so that fluid and toxins exit in urine, but cells and important proteins are kept in the blood stream. Diabetes mellitus alters this structure, it becomes scarred and then the ability of the kidney to clear toxins is lost. Recent evidence shows that early in diabetes the podocyte number is reduced, areas of the glomerular basement membrane are denuded, and podocyte number predicts long-term urinary albumin excretion in the patients with diabetes and microalbuminuria. These results suggest that podocytes play a critical role in the early stage of diabetic nephropathy. It is the purpose of this article to review the pathogenetic role of podocytes in diabetic nephropathy.
-
Citations
Citations to this article as recorded by- Inhibition of dipeptidyl peptidase-4 (DPP4), antioxidant, antiglycation and anti-inflammatory effect of Ferulic acid against streptozotocin toxicity mediate nephropathy in diabetic rats
Maryam A. AL-Ghamdi, Said S. Moselhy
Environmental Science and Pollution Research.2022; 30(12): 33942. CrossRef - Study of Antiglycation, Hypoglycemic, and Nephroprotective Activities of the Green Dwarf Variety Coconut Water (Cocos nucifera L.) in Alloxan-Induced Diabetic Rats
Isabella F.D. Pinto, Railmara P. Silva, Adriano de B. Chaves Filho, Lucas S. Dantas, Vanderson S. Bispo, Isaac A. Matos, Felipe A.M. Otsuka, Aline C. Santos, Humberto Reis Matos
Journal of Medicinal Food.2015; 18(7): 802. CrossRef - Effects of ferulic acid on diabetic nephropathy in a rat model of type 2 diabetes
Ran Choi, Bo Hwan Kim, Jarinyaporn Naowaboot, Mi Young Lee, Mi Ri Hyun, Eun Ju Cho, Eun Soo Lee, Eun Young Lee, Young Chul Yang, Choon Hee Chung
Experimental and Molecular Medicine.2011; 43(12): 676. CrossRef
- Inhibition of dipeptidyl peptidase-4 (DPP4), antioxidant, antiglycation and anti-inflammatory effect of Ferulic acid against streptozotocin toxicity mediate nephropathy in diabetic rats

 KDA
KDA
 First
First Prev
Prev





