
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Metabolic Risk/Epidemiology
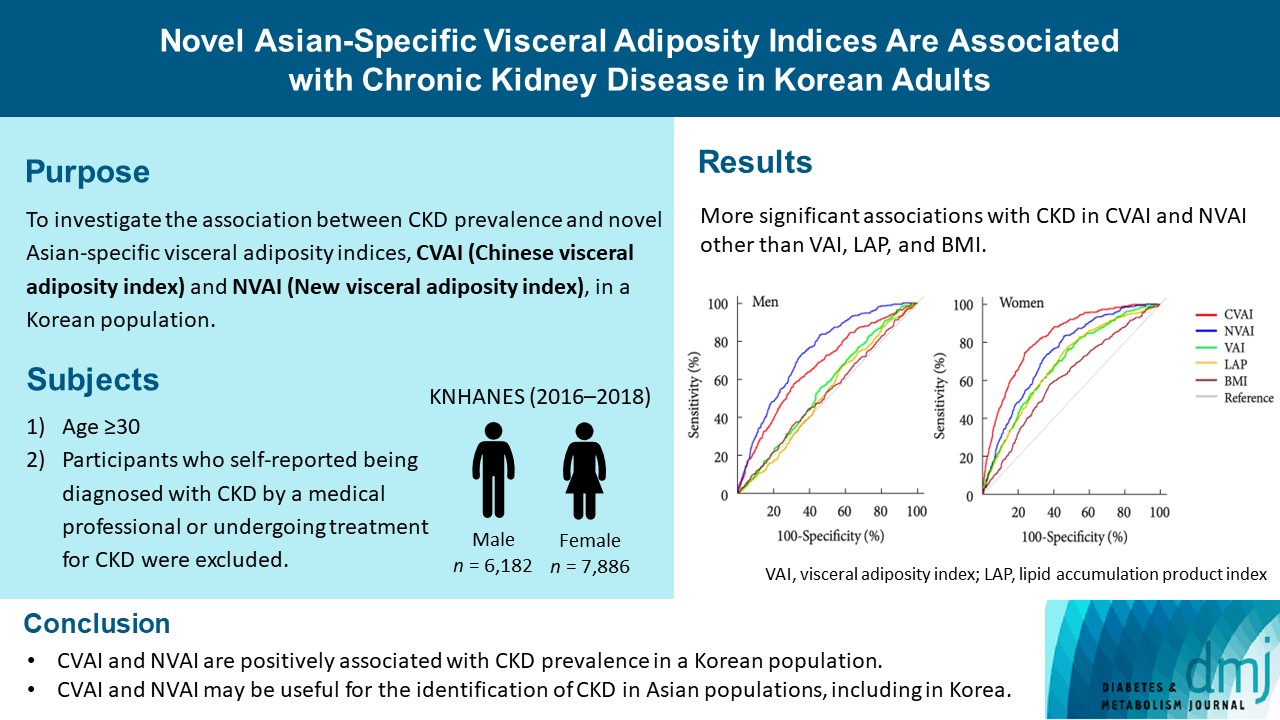
- Novel Asian-Specific Visceral Adiposity Indices Are Associated with Chronic Kidney Disease in Korean Adults
- Jonghwa Jin, Hyein Woo, Youngeun Jang, Won-Ki Lee, Jung-Guk Kim, In-Kyu Lee, Keun-Gyu Park, Yeon-Kyung Choi
- Diabetes Metab J. 2023;47(3):426-436. Published online March 6, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0099
- 2,501 View
- 128 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The Chinese visceral adiposity index (CVAI) and new visceral adiposity index (NVAI) are novel indices of visceral adiposity used to predict metabolic and cardiovascular diseases in Asian populations. However, the relationships of CVAI and NVAI with chronic kidney disease (CKD) have not been investigated. We aimed to characterize the relationships of CVAI and NVAI with the prevalence of CKD in Korean adults.
Methods
A total of 14,068 participants in the 7th Korea National Health and Nutrition Examination Survey (6,182 men and 7,886 women) were included. Receiver operating characteristic (ROC) analyses were employed to compare the associations between indices of adiposity and CKD, and a logistic regression model was used to characterize the relationships of CVAI and NVAI with CKD prevalence.
Results
The areas under the ROC curves for CVAI and NVAI were significantly larger than for the other indices, including the visceral adiposity index and lipid accumulation product, in both men and women (all P<0.001). In addition, high CVAI or NVAI was significantly associated with a high CKD prevalence in both men (odds ratio [OR], 2.14; 95% confidence interval [CI], 1.31 to 3.48 in CVAI and OR, 6.47; 95% CI, 2.91 to 14.38 in NVAI, P<0.05) and women (OR, 4.87; 95% CI, 1.85 to 12.79 in CVAI and OR, 3.03; 95% CI, 1.35 to 6.82 in NVAI, P<0.05); this association remained significant after adjustment for multiple confounding factors in men and women.
Conclusion
CVAI and NVAI are positively associated with CKD prevalence in a Korean population. CVAI and NVAI may be useful for the identification of CKD in Asian populations, including in Korea. -
Citations
Citations to this article as recorded by- Association between Chinese visceral adiposity index and risk of stroke incidence in middle-aged and elderly Chinese population: evidence from a large national cohort study
Zenglei Zhang, Lin Zhao, Yiting Lu, Xu Meng, Xianliang Zhou
Journal of Translational Medicine.2023;[Epub] CrossRef
- Association between Chinese visceral adiposity index and risk of stroke incidence in middle-aged and elderly Chinese population: evidence from a large national cohort study
- Metabolic Risk/Epidemiology
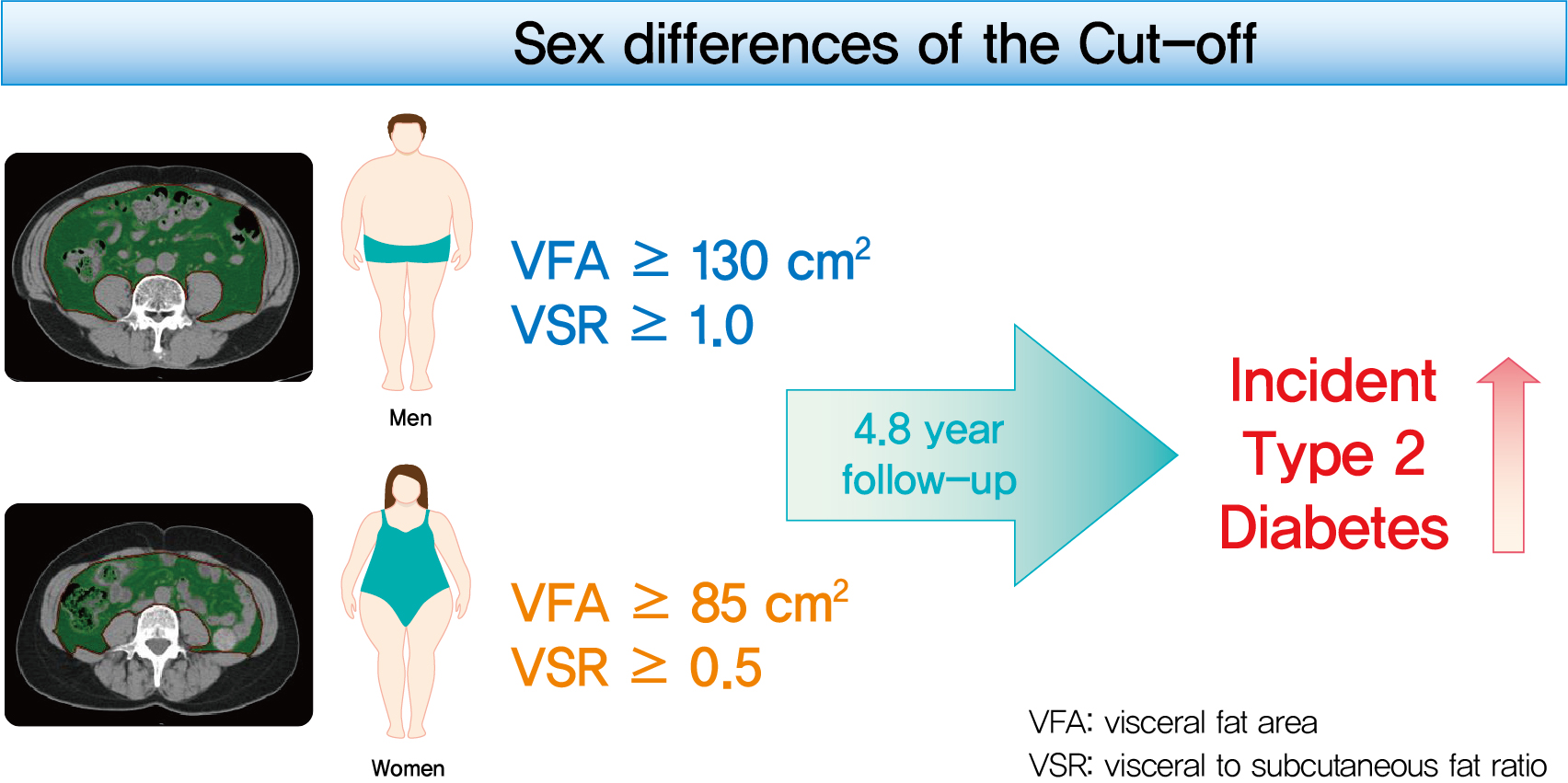
- Sex Differences of Visceral Fat Area and Visceral-to-Subcutaneous Fat Ratio for the Risk of Incident Type 2 Diabetes Mellitus
- Eun Hee Kim, Hong-Kyu Kim, Min Jung Lee, Sung-Jin Bae, Jaewon Choe, Chang Hee Jung, Chul-Hee Kim, Joong-Yeol Park, Woo Je Lee
- Diabetes Metab J. 2022;46(3):486-498. Published online November 18, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0095
- 9,293 View
- 367 Download
- 18 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study aimed to determine the optimal cut-off values of visceral fat area (VFA) and visceral-to-subcutaneous fat ratio (VSR) for predicting incident type 2 diabetes mellitus (T2DM).
Methods
A total of 10,882 individuals (6,835 men; 4,047 women) free of T2DM at baseline aged between 30 and 79 years who underwent abdominal computed tomography scan between 2012 and 2013 as a part of routine health check-ups were included and followed. VFA, subcutaneous fat area, and VSR on L3 vertebral level were measured at baseline.
Results
During a median follow-up of 4.8 years, 730 (8.1% for men; 4.3% for women) incident cases of T2DM were identified. Receiver operating characteristic curve analysis showed that the optimal cut-off values of VFA and VSR for predicting incident T2DM were 130.03 cm2 and 1.08 in men, respectively, and 85.7 cm2 and 0.48 in women, respectively. Regardless of sex, higher VFA and VSR were significantly associated with a higher risk of incident T2DM. Compared with the lowest quartiles of VFA and VSR, the highest quartiles had adjusted odds ratios of 2.62 (95% confidence interval [CI], 1.73 to 3.97) and 1.55 (95% CI, 1.14 to 2.11) in men, respectively, and 32.49 (95% CI, 7.42 to 142.02) and 11.07 (95% CI, 3.89 to 31.50) in women, respectively.
Conclusion
Higher VFA and VSR at baseline were independent risk factors for the development of T2DM. Sex-specific reference values for visceral fat obesity (VFA ≥130 cm2 or VSR ≥1.0 in men; VFA ≥85 cm2 or VSR ≥0.5 in women) are proposed for the prediction of incident T2DM. -
Citations
Citations to this article as recorded by- Severity of adipose tissue dysfunction is associated with progression of pre-diabetes to type 2 diabetes: the Tehran Lipid and Glucose Study
Mohammad Jalali, Zahra Bahadoran, Parvin Mirmiran, Fereidoun Azizi, Farhad Hosseinpanah
BMC Public Health.2024;[Epub] CrossRef - Should insulin resistance (HOMA-IR), insulin secretion (HOMA-β), and visceral fat area be considered for improving the performance of diabetes risk prediction models
Huan Hu, Tohru Nakagawa, Toru Honda, Shuichiro Yamamoto, Tetsuya Mizoue
BMJ Open Diabetes Research & Care.2024; 12(1): e003680. CrossRef - Adipose organ dysfunction and type 2 diabetes: Role of nitric oxide
Zahra Bahadoran, Parvin Mirmiran, Asghar Ghasemi
Biochemical Pharmacology.2024; 221: 116043. CrossRef - Prediction of high visceral adipose tissue for sex‐specific community residents in Taiwan
Yu‐Hsuan Chang, Chin‐Sung Chang, Chieh‐Yu Liu, Yin‐Fan Chang, Shiow‐Ching Shun
Nursing & Health Sciences.2024;[Epub] CrossRef - Guidelines for obesity clinic consultations in primary healthcare clinics
Jee-Hyun Kang, Kyoung-Kon Kim
Journal of the Korean Medical Association.2024; 67(4): 240. CrossRef - Correlation between fat-to-muscle mass ratio and cognitive impairment in elderly patients with type 2 diabetes mellitus: a cross-sectional study
Fan Wu, Yanlan Liu, Chenying Lin, Nahal Haghbin, Longfei Xia, Yaoshuang Li, Tong Chen, Huina Qiu, Weiran Jiang, Jingbo Li, Jingna Lin
BMC Geriatrics.2024;[Epub] CrossRef - Body Composition and Metabolic Dysfunction Really Matter for the Achievement of Better Outcomes in High-Grade Serous Ovarian Cancer
Mauricio A. Cuello, Fernán Gómez, Ignacio Wichmann, Felipe Suárez, Sumie Kato, Elisa Orlandini, Jorge Brañes, Carolina Ibañez
Cancers.2023; 15(4): 1156. CrossRef - MEDICINAL BIOMAGNETISM FOR THE TREATMENT OF OBESITY
Ana Vergínia Campagnollo Bueno, Michelli Gonçalves Seneda, Ângela Mara Rambo, Ana Clara Campagnolo Gonçalves Toledo, Caroline Cabral de Azevedo, Adriane Viapiana Bossa
Health and Society.2023; 3(01): 411. CrossRef - Cumulative exposure to metabolic syndrome in a national population-based cohort of young adults and sex-specific risk for type 2 diabetes
Min-Kyung Lee, Jae-Hyuk Lee, Seo Young Sohn, Jiyeon Ahn, Oak-Kee Hong, Mee-Kyoung Kim, Ki-Hyun Baek, Ki-Ho Song, Kyungdo Han, Hyuk-Sang Kwon
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - The correlation between visceral fat/subcutaneous fat area ratio and monocyte/high-density lipoprotein ratio in patients with type 2 diabetes mellitus and albuminuria
Haiyan Lin, Jun Zhu, Chen Zheng, Xiaoming Xu, Shandong Ye
Journal of Diabetes and its Complications.2023; 37(11): 108521. CrossRef - Effects of the abdominal fat distribution on the relationship between exposure to air pollutants and thyroid hormones among Korean adult males
Hyun-Jin Kim, Byungmi Kim, Seyoung Kim, Hyuktae Kwon, Jae Moon Yun, Belong Cho, Jin-Ho Park
European Journal of Medical Research.2023;[Epub] CrossRef - Association of Visceral Fat Obesity, Sarcopenia, and Myosteatosis with Non-Alcoholic Fatty Liver Disease without Obesity
Hong-Kyu Kim, Sung-Jin Bae, Min Jung Lee, Eun Hee Kim, Hana Park, Hwi Seung Kim, Yun Kyung Cho, Chang Hee Jung, Woo Je Lee, Jaewon Choe
Clinical and Molecular Hepatology.2023; 29(4): 987. CrossRef - Visceral adipose tissue reference data computed for GE HealthCare DXA from the National Health and Nutrition Examination Survey data set
Jonathan P. Bennett, Brandon K. Quon, Bo Fan, En Liu, Leila Kazemi, Rosa C. Villegas‐Valle, Raj Ahgun, Xian‐pin Wu, Hou‐De Zhou, Ying Lu, John A. Shepherd
Obesity.2023; 31(12): 2947. CrossRef - Comparison of bioelectrical body and visceral fat indices and anthropometric measures in relation to type 2 diabetes by sex among Chinese adults, a cross-sectional study
Jiangshan He, Binbin Zhang, Yaqi Fan, Yuxue Wang, Mianzhi Zhang, Chunjun Li, Li Zhang, Pei Guo, Minying Zhang
Frontiers in Public Health.2023;[Epub] CrossRef - The predictive significance of lipid accumulation products for future diabetes in a non-diabetic population from a gender perspective: an analysis using time-dependent receiver operating characteristics
Jiajun Qiu, Maobin Kuang, Yang Zou, Ruijuan Yang, Qing Shangguan, Dingyang Liu, Guotai Sheng, Wei Wang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Cellular interplay between cardiomyocytes and non-myocytes in diabetic cardiomyopathy
Ren Jie Phang, Rebecca H. Ritchie, Derek J. Hausenloy, Jarmon G. Lees, Shiang Y. Lim
Cardiovascular Research.2022;[Epub] CrossRef - Implication of Sex Differences in Visceral Fat for the Assessment of Incidence Risk of Type 2 Diabetes Mellitus
Sang Hyeon Ju, Hyon-Seung Yi
Diabetes & Metabolism Journal.2022; 46(3): 414. CrossRef - Visceral fat area and body fat percentage measured by bioelectrical impedance analysis correlate with glycometabolism
Shuying Li, Shaoping Li, Jie Ding, Weihong Zhou
BMC Endocrine Disorders.2022;[Epub] CrossRef - The Demographic Specific Abdominal Fat Composition and Distribution Trends in US Adults from 2011 to 2018
Furong Xu, Jacob E. Earp, Bryan J. Blissmer, Ingrid E. Lofgren, Matthew J. Delmonico, Geoffrey W. Greene
International Journal of Environmental Research and Public Health.2022; 19(19): 12103. CrossRef - Visceral Obesity Is a More Important Factor for Colorectal Adenomas than Skeletal Muscle or Body Fat
Ji Yeon Seo, Yoo Min Han, Su Jin Chung, Seon Hee Lim, Jung Ho Bae, Goh Eun Chung
Cancers.2022; 14(21): 5256. CrossRef - Recent Advances in Visceral Obesity and Related Diseases
佳佳 魏
Advances in Clinical Medicine.2022; 12(12): 11686. CrossRef - Gender differences in the ideal cutoffs of visceral fat area for predicting MAFLD in China
Pingping Yu, Huachao Yang, Xiaoya Qi, Ruixue Bai, Shouqin Zhang, Jianping Gong, Ying Mei, Peng Hu
Lipids in Health and Disease.2022;[Epub] CrossRef
- Severity of adipose tissue dysfunction is associated with progression of pre-diabetes to type 2 diabetes: the Tehran Lipid and Glucose Study
- Metabolic Risk/Epidemiology
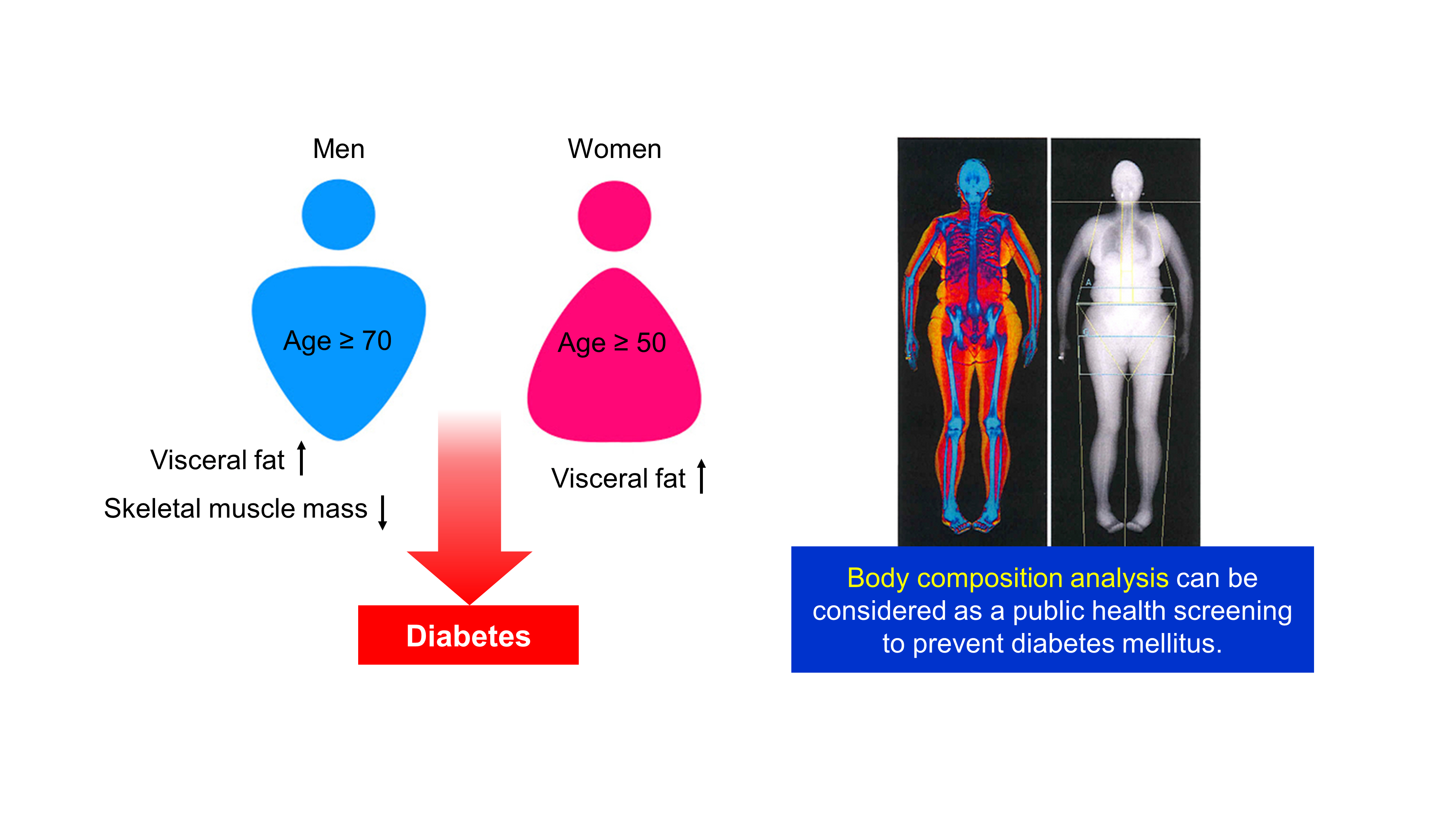
- Age- and Sex-Related Differential Associations between Body Composition and Diabetes Mellitus
- Eun Roh, Soon Young Hwang, Jung A Kim, You-Bin Lee, So-hyeon Hong, Nam Hoon Kim, Ji A Seo, Sin Gon Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
- Diabetes Metab J. 2021;45(2):183-194. Published online June 16, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0171
- 7,444 View
- 236 Download
- 3 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
Background The age- and sex-related differences on the impacts of body composition on diabetes mellitus (DM) remain uncertain.
Methods The fourth and fifth Korea National Health and Nutrition Examination Survey included 15,586 subjects over 30 years of age who completed dual-energy X-ray absorptiometry. We conducted a cross-sectional study to investigate whether muscle mass index (MMI), defined as appendicular skeletal muscle divided by body mass index (BMI), and fat mass index (FMI), defined as trunk fat mass divided by BMI, were differently associated with DM according to age and sex.
Results In multivariate logistic regression, the risk for DM significantly increased across quartiles of FMI in men aged ≥70. Meanwhile, MMI showed a protective association with DM in men of the same age. The odds ratios (ORs) for the highest quartile versus the lowest quartile of FMI and MMI were 3.116 (95% confidence interval [CI], 1.405 to 6.914) and 0.295 (95% CI, 0.157 to 0.554), respectively. In women, the ORs of DM was significantly different across FMI quartiles in those over age 50. The highest quartile of FMI exhibited increased ORs of DM in subjects aged 50 to 69 (OR, 1.891; 95% CI, 1.229 to 2.908) and ≥70 (OR, 2.275; 95% CI, 1.103 to 4.69) compared to lowest quartile. However, MMI was not significantly associated with DM in women of all age groups.
Conclusion Both FMI and MMI were independent risk factors for DM in men aged 70 years or more. In women over 50 years, FMI was independently associated with DM. There was no significant association between MMI and DM in women.
-
Citations
Citations to this article as recorded by- Research Progress on Correlation between Body Composition Changes and Disease Pro-gression of Type 2 Diabetes
敏 张
Advances in Clinical Medicine.2024; 14(03): 936. CrossRef - Low Skeletal Muscle Mass Accompanied by Abdominal Obesity Additively Increases the Risk of Incident Type 2 Diabetes
Ji Eun Jun, Seung-Eun Lee, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Jae Hwan Jee, Jae Hyeon Kim
The Journal of Clinical Endocrinology & Metabolism.2023; 108(5): 1173. CrossRef - Is imaging-based muscle quantity associated with risk of diabetes? A meta-analysis of cohort studies
Shanhu Qiu, Xue Cai, Yang Yuan, Bo Xie, Zilin Sun, Tongzhi Wu
Diabetes Research and Clinical Practice.2022; 189: 109939. CrossRef - Whole and segmental body composition changes during mid-follicular and mid-luteal phases of the menstrual cycle in recreationally active young women
Şükran Nazan Koşar, Yasemin Güzel, Mehmet Gören Köse, Ayşe Kin İşler, Tahir Hazır
Annals of Human Biology.2022; 49(2): 124. CrossRef - Body Composition and Diabetes
Hye Jin Yoo
The Journal of Korean Diabetes.2021; 22(4): 238. CrossRef
- Research Progress on Correlation between Body Composition Changes and Disease Pro-gression of Type 2 Diabetes
- Metabolic Risk/Epidemiology
- Intra-Abdominal Fat and High Density Lipoprotein Cholesterol Are Associated in a Non-Linear Pattern in Japanese-Americans
- Sun Ok Song, You-Cheol Hwang, Steven E. Kahn, Donna L. Leonetti, Wilfred Y. Fujimoto, Edward J. Boyko
- Diabetes Metab J. 2020;44(2):277-285. Published online March 10, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0008
- 4,666 View
- 63 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We describe the association between high density lipoprotein cholesterol (HDL-C) concentration and computed tomography (CT)-measured fat depots.
Methods We examined the cross-sectional associations between HDL-C concentration and intra-abdominal (IAF), abdominal subcutaneous (SCF), and thigh fat (TF) areas in 641 Japanese-American men and women. IAF, SCF, and TF were measured by CT at the level of the umbilicus and mid-thigh. The associations between fat area measurements and HDL-C were examined using multivariate linear regression analysis adjusting for age, sex, diabetes family history, homeostasis model assessment of insulin resistance (HOMA-IR), and body mass index (BMI). Non-linearity was assessed using fractional polynomials.
Results Mean±standard deviation of HDL-C concentration and IAF in men and women were 1.30±0.34 mg/dL, 105±55.3 cm2, and 1.67±0.43 mg/dL, 74.4±46.6 cm2 and differed significantly by gender for both comparisons (
P <0.001). In univariate analysis, HDL-C concentration was significantly associated with CT-measured fat depots. In multivariate analysis, IAF was significantly and non-linearly associated with HDL-C concentration adjusted for age, sex, BMI, HOMA-IR, SCF, and TF (IAF: β=−0.1012, P<0.001; IAF2: β=0.0008,P <0.001). SCF was also negatively and linearly associated with HDL-C (β=−0.4919,P =0.001).Conclusion HDL-C does not linearly decline with increasing IAF in Japanese-Americans. A more complex pattern better fits this association.
-
Citations
Citations to this article as recorded by- Associations of Serum Uric Acid to High-Density Lipoprotein Cholesterol Ratio with Trunk Fat Mass and Visceral Fat Accumulation
Yansu Wang, Yiting Xu, Tingting Hu, Yunfeng Xiao, Yufei Wang, Xiaojing Ma, Haoyong Yu, Yuqian Bao
Diabetes, Metabolic Syndrome and Obesity.2024; Volume 17: 121. CrossRef - Obesity-related parameters in carriers of some BDNF genetic variants may depend on daily dietary macronutrients intake
Urszula Miksza, Edyta Adamska-Patruno, Witold Bauer, Joanna Fiedorczuk, Przemyslaw Czajkowski, Monika Moroz, Krzysztof Drygalski, Andrzej Ustymowicz, Elwira Tomkiewicz, Maria Gorska, Adam Kretowski
Scientific Reports.2023;[Epub] CrossRef - Computed tomography-based investigation of the correlation of abdominal fat areas with metabolic syndrome
Kai-Yuan Cheng, Tsung-Hsien Yen, Jay Wu, Pei-Hsuan Li, Tian-Yu Shih
Journal of Radiological Science.2023; 48(1): 15. CrossRef - Lower High-Density Lipoprotein Cholesterol Concentration Is Independently Associated with Greater Future Accumulation of Intra-Abdominal Fat
Sun Ok Song, You-Cheol Hwang, Han Uk Ryu, Steven E. Kahn, Donna L. Leonetti, Wilfred Y. Fujimoto, Edward J. Boyko
Endocrinology and Metabolism.2021; 36(4): 835. CrossRef
- Associations of Serum Uric Acid to High-Density Lipoprotein Cholesterol Ratio with Trunk Fat Mass and Visceral Fat Accumulation
- Obesity and Metabolic Syndrome
- Association between Blood Mercury Level and Visceral Adiposity in Adults
- Jong Suk Park, Kyoung Hwa Ha, Ka He, Dae Jung Kim
- Diabetes Metab J. 2017;41(2):113-120. Published online December 21, 2016
- DOI: https://doi.org/10.4093/dmj.2017.41.2.113
- 4,852 View
- 46 Download
- 38 Web of Science
- 39 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Few studies have examined the association between mercury exposure and obesity. The aim of this study is to investigate the association between blood mercury concentrations and indices of obesity in adults.
Methods A total of 200 healthy subjects, aged 30 to 64 years, who had no history of cardiovascular or malignant disease, were examined. Anthropometric and various biochemical profiles were measured. Visceral adipose tissue (VAT) was measured using dual-energy X-ray absorptiometry (DXA).
Results All subjects were divided into three groups according to blood mercury concentrations. Compared with the subjects in the lowest tertile of mercury, those in the highest tertile were more likely to be male; were current alcohol drinkers and smokers; had a higher body mass index (BMI), waist circumference (WC), and VAT; had higher levels of blood pressure, fasting glucose, and insulin resistance; and consumed more fish. The blood mercury concentration was significantly associated with anthropometric parameters, showing relationships with BMI, WC, and VAT. After adjusting for multiple risk factors, the odds ratios (ORs) for high mercury concentration was significantly higher in the highest VAT tertile than in the lowest VAT tertile (OR, 2.66; 95% confidence interval, 1.05 to 6.62;
P <0.05).Conclusion The blood mercury concentration was significantly associated with VAT in healthy adults. Further studies are warranted to confirm our findings.
-
Citations
Citations to this article as recorded by- Exposure to Metal Mixtures and Overweight or Obesity Among Chinese Adults
Gaojie Fan, Qing Liu, Mingyang Wu, Jianing Bi, Xiya Qin, Qing Fang, Zhengce Wan, Yongman Lv, Youjie Wang, Lulu Song
Biological Trace Element Research.2023; 201(8): 3697. CrossRef - Methylmercury drives lipid droplet formation and adipokine expression during the late stages of adipocyte differentiation in 3T3-L1 cells
Yasukazu Takanezawa, Yui Kashiwano, Ryosuke Nakamura, Yuka Ohshiro, Shimpei Uraguchi, Masako Kiyono
Toxicology.2023; 486: 153446. CrossRef - Expression Profiling of Adipogenic and Anti-Adipogenic MicroRNA Sequences following Methylmercury Exposure in Caenorhabditis elegans
Giancarlo Garofalo, Tyson Nielsen, Samuel Caito
Toxics.2023; 11(11): 934. CrossRef - Report of the Scientific Committee of the Spanish Agency for Food Safety and Nutrition (AESAN) on the available evidence in relation to the potential obesogenic activity of certain chemical compounds that may be present in foods
Ana María Rivas Velasco, Irene Bretón Lesmes, Araceli Díaz Perales, Ángel Gil Izquierdo, María José González Muñoz, Victoria Moreno Arribas, María del Puy Portillo Baquedano, Silvia Pichardo Sánchez
Food Risk Assess Europe.2023;[Epub] CrossRef - Lead, mercury, and cadmium exposures are associated with obesity but not with diabetes mellitus: Korean National Environmental Health Survey (KoNEHS) 2015–2017
Min Kyong Moon, Inae Lee, Aram Lee, Hyunwoong Park, Min Joo Kim, Sunmi Kim, Yoon Hee Cho, Sooyeon Hong, Jiyoung Yoo, Gi Jeong Cheon, Kyungho Choi, Young Joo Park, Jeongim Park
Environmental Research.2022; 204: 111888. CrossRef - The Effect of Mixture of Heavy Metals on Obesity in Individuals ≥50 Years of Age
Hai Nguyen Duc, Hojin Oh, Min-Sun Kim
Biological Trace Element Research.2022; 200(8): 3554. CrossRef - MicroRNA Expression Influences Methylmercury-Induced Lipid Accumulation and Mitochondrial Toxicity in Caenorhabditis elegans
Tyson Nielsen, Nicole Crawford, Megan Martell, Belal Khalil, Farooq Imtiaz, Jennifer L. Newell-Caito, Samuel Caito
Chemical Research in Toxicology.2022; 35(1): 77. CrossRef - Relationship Between Serum Levels of Arsenic, Cadmium, and Mercury and Body Mass Index and Fasting Plasma Glucose in a Mexican Adult Population
Héctor Hernández-Mendoza, Héctor Edmundo Álvarez-Loredo, Elizabeth Teresita Romero-Guzmán, Darío Gaytán-Hernández, Consuelo Chang-Rueda, Israel Martínez-Navarro, Bertha Irene Juárez-Flores, María Judith Rios-Lugo
Biological Trace Element Research.2022; 200(12): 4916. CrossRef - Heavy metal-induced lipogenic gene aberration, lipid dysregulation and obesogenic effect: a review
Yang Zhou, Frank Peprah Addai, Xinshuang Zhang, Yuelin Liu, Yinfeng Wang, Feng Lin, Alex Tuffour, Jie Gu, Guangxiang Liu, Haifeng Shi
Environmental Chemistry Letters.2022; 20(3): 1611. CrossRef - Differential fat accumulation in early adulthood according to adolescent‐BMI and heavy metal exposure
Larissa Betanzos‐Robledo, Martha M. Téllez‐Rojo, Hector Lamadrid‐Figueroa, Ernesto Roldan‐Valadez, Karen E. Peterson, Erica C. Jansen, Nil Basu, Alejandra Cantoral
New Directions for Child and Adolescent Development.2022; 2022(181-182): 37. CrossRef - The Association of Mercury and ALT with Obesity in Korean Adults: Using Data from the Korea National Health and Nutrition Examination Survey for 11 Years (KNHANES 2005, 2008~2017)
Sang Shin Pyo
Korean Journal of Clinical Laboratory Science.2022; 54(3): 192. CrossRef - Plasma titanium level is positively associated with metabolic syndrome: A survey in China’s heavy metal polluted regions
Miao Huang, Jingyuan Chen, Guangyu Yan, Yiping Yang, Dan Luo, Xiang Chen, Meian He, Hong Yuan, Zhijun Huang, Yao Lu
Ecotoxicology and Environmental Safety.2021; 208: 111435. CrossRef - Relationship Between Elevated Hair Mercury Levels, Essential Element Status, and Metabolic Profile in Overweight and Obese Adults
Anatoly V. Skalny, Jung-Su Chang, Igor P. Bobrovnitsky, Philippe Yu Kopylov, Margarita G. Skalnaya, Shih-Yi Huang, Monica Maria Bastos Paoliello, Ekaterina S. Ivanova, Weu Wang, Alexey A. Tinkov
Biological Trace Element Research.2021; 199(8): 2874. CrossRef - Associations between metabolic syndrome and four heavy metals: A systematic review and meta-analysis
Ping Xu, Aiping Liu, Fengna Li, Alexey A. Tinkov, Longjian Liu, Ji-Chang Zhou
Environmental Pollution.2021; 273: 116480. CrossRef - Cadmium, lead and mercury in the blood of psoriatic and vitiligo patients and their possible associations with dietary habits
Marta Wacewicz-Muczyńska, Katarzyna Socha, Jolanta Soroczyńska, Marek Niczyporuk, Maria H. Borawska
Science of The Total Environment.2021; 757: 143967. CrossRef - Crude oil and public health issues in Niger Delta, Nigeria: Much ado about the inevitable
Orish Ebere Orisakwe
Environmental Research.2021; 194: 110725. CrossRef - Mercury in the human adrenal medulla could contribute to increased plasma noradrenaline in aging
Roger Pamphlett, Stephen Kum Jew, Philip A. Doble, David P. Bishop
Scientific Reports.2021;[Epub] CrossRef - Multiple metal exposure and obesity: A prospective cohort study of adults living along the Yangtze River, China
Qi Zhong, Qi-rong Qin, Wan-jun Yang, Jia-liu He, Jin-liang Zhu, Zhen-yu Zhu, Fen Huang
Environmental Pollution.2021; 285: 117150. CrossRef - Association between Blood Mercury Levels and Non-Alcoholic Fatty Liver Disease in Non-Obese Populations: The Korean National Environmental Health Survey (KoNEHS) 2012–2014
Yun-Jung Yang, Eun-Jung Yang, Kyongjin Park, Subin Oh, Taehyen Kim, Yeon-Pyo Hong
International Journal of Environmental Research and Public Health.2021; 18(12): 6412. CrossRef - Hair Lead, Aluminum, and Other Toxic Metals in Normal-Weight and Obese Patients with Coronary Heart Disease
Anatoly V. Skalny, Philippe Yu Kopylov, Monica M. B. Paoliello, Jung-Su Chang, Michael Aschner, Igor P. Bobrovnitsky, Jane C.-J. Chao, Jan Aaseth, Sergei N. Chebotarev, Alexey A. Tinkov
International Journal of Environmental Research and Public Health.2021; 18(15): 8195. CrossRef - Methylmercury chronic exposure affects the expression of DNA single-strand break repair genes, induces oxidative stress, and chromosomal abnormalities in young dyslipidemic APOE knockout mice
Cássia R. Roque, Letícia R. Sampaio, Mayumi N. Ito, Daniel V. Pinto, Juan S.R. Caminha, Paulo I.G. Nunes, Ramon S. Raposo, Flávia A. Santos, Cláudia C. Windmöller, Maria Elena Crespo-Lopez, Jacqueline I. Alvarez-Leite, Reinaldo B. Oriá, Ronald F. Pinheiro
Toxicology.2021; 464: 152992. CrossRef - Methylmercury-Induced Metabolic Alterations in Caenorhabditis elegans Are Diet-Dependent
Nicole Crawford, Megan Martell, Tyson Nielsen, Belal Khalil, Farooq Imtiaz, Etienne Nguidjo, Jennifer Newell-Caito, Julia Bornhorst, Tanja Schwerdtle, Samuel Caito
Toxics.2021; 9(11): 287. CrossRef - Antioxidant status in relation to heavy metals induced oxidative stress in patients with polycystic ovarian syndrome (PCOS)
Manal Abudawood, Hajera Tabassum, Atheer H. Alanazi, Fatmah Almusallam, Feda Aljaser, Mir Naiman Ali, Naif D. Alenzi, Samyah T. Alanazi, Manal A. Alghamdi, Ghadah H. Altoum, Manar A. Alzeer, Majed O. Alotaibi, Arwa Abudawood, Hazem K. Ghneim, Lulu Abdulla
Scientific Reports.2021;[Epub] CrossRef - Association of Blood Mercury Levels with the Risks of Overweight and High Waist-to-Height Ratio in Children and Adolescents: Data from the Korean National Health and Nutrition Examination Survey
Ky Young Cho
Children.2021; 8(12): 1087. CrossRef - The sex-specific effects of blood lead, mercury, and cadmium levels on hepatic steatosis and fibrosis: Korean nationwide cross-sectional study
Seung Min Chung, Jun Sung Moon, Ji Sung Yoon, Kyu Chang Won, Hyoung Woo Lee
Journal of Trace Elements in Medicine and Biology.2020; 62: 126601. CrossRef - Elevated blood mercury level has a non-linear association with infertility in U.S. women: Data from the NHANES 2013–2016
Fangfang Zhu, Chi Chen, Yingxuan Zhang, Si Chen, Xian Huang, Jingwei Li, Yanxi Wang, Xiaorong Liu, Gaopi Deng, Jie Gao
Reproductive Toxicology.2020; 91: 53. CrossRef - Methylmercury Induces Metabolic Alterations in Caenorhabditis elegans: Role for C/EBP Transcription Factor
Samuel W Caito, Jennifer Newell-Caito, Megan Martell, Nicole Crawford, Michael Aschner
Toxicological Sciences.2020; 174(1): 112. CrossRef - Association of Fish Consumption and Mercury Exposure During Pregnancy With Metabolic Health and Inflammatory Biomarkers in Children
Nikos Stratakis, David V. Conti, Eva Borras, Eduardo Sabido, Theano Roumeliotaki, Eleni Papadopoulou, Lydiane Agier, Xavier Basagana, Mariona Bustamante, Maribel Casas, Shohreh F. Farzan, Serena Fossati, Juan R. Gonzalez, Regina Grazuleviciene, Barbara He
JAMA Network Open.2020; 3(3): e201007. CrossRef - Elemental Analysis of Aging Human Pituitary Glands Implicates Mercury as a Contributor to the Somatopause
Roger Pamphlett, Stephen Kum Jew, Philip A. Doble, David P. Bishop
Frontiers in Endocrinology.2019;[Epub] CrossRef - Mercury leads to features of polycystic ovary syndrome in rats
Eduardo Merlo, Ingridy R.G. Schereider, Maylla R. Simões, Dalton V. Vassallo, Jones B. Graceli
Toxicology Letters.2019; 312: 45. CrossRef - In utero exposure to mercury and childhood overweight or obesity: counteracting effect of maternal folate status
Guoying Wang, Jessica DiBari, Eric Bind, Andrew M. Steffens, Jhindan Mukherjee, Tami R. Bartell, David C. Bellinger, Xiumei Hong, Yuelong Ji, Mei-Cheng Wang, Marsha Wills-Karp, Tina L. Cheng, Xiaobin Wang
BMC Medicine.2019;[Epub] CrossRef - Mercury Is Taken Up Selectively by Cells Involved in Joint, Bone, and Connective Tissue Disorders
Roger Pamphlett, Stephen Kum Jew
Frontiers in Medicine.2019;[Epub] CrossRef - Cohort Profile: The Cardiovascular and Metabolic Diseases Etiology Research Center Cohort in Korea
Jee-Seon Shim, Bo Mi Song, Jung Hyun Lee, Seung Won Lee, Ji Hye Park, Dong Phil Choi, Myung Ha Lee, Kyoung Hwa Ha, Dae Jung Kim, Sungha Park, Won-Woo Lee, Yoosik Youm, Eui-Cheol Shin, Hyeon Chang Kim
Yonsei Medical Journal.2019; 60(8): 804. CrossRef - Chronic mercury at low doses impairs white adipose tissue plasticity
Danize Aparecida Rizzetti, Patricia Corrales, Janaina Trindade Piagette, José Antonio Uranga-Ocio, Gema Medina-Gomez, Franck Maciel Peçanha, Dalton Valentim Vassallo, Marta Miguel, Giulia Alessandra Wiggers
Toxicology.2019; 418: 41. CrossRef - Associations of cumulative exposure to heavy metal mixtures with obesity and its comorbidities among U.S. adults in NHANES 2003–2014
Xin Wang, Bhramar Mukherjee, Sung Kyun Park
Environment International.2018; 121: 683. CrossRef - Blood mercury concentration in relation to metabolic and weight phenotypes using the KNHANES 2011–2013 data
Kayoung Lee
International Archives of Occupational and Environmental Health.2018; 91(2): 185. CrossRef - The association of total blood mercury levels and overweight among Korean adolescents: analysis of the Korean National Health and Nutrition Examination Survey (KNHANES) 2010–2013
Yi-Yeon Shin, In-Kyung Ryu, Mi-Jung Park, Shin-Hye Kim
Korean Journal of Pediatrics.2018; 61(4): 121. CrossRef - Heavy Metal Exposure and Metabolic Syndrome: Evidence from Human and Model System Studies
Antonio Planchart, Adrian Green, Cathrine Hoyo, Carolyn J. Mattingly
Current Environmental Health Reports.2018; 5(1): 110. CrossRef - Association between Blood Mercury Level and Visceral Adiposity in Adults
Seong-Su Moon
Diabetes & Metabolism Journal.2017; 41(2): 96. CrossRef
- Exposure to Metal Mixtures and Overweight or Obesity Among Chinese Adults
- Arterial Stiffness by Aerobic Exercise Is Related with Aerobic Capacity, Physical Activity Energy Expenditure and Total Fat but not with Insulin Sensitivity in Obese Female Patients with Type 2 Diabetes
- Ji Yeon Jung, Kyung Wan Min, Hee Jung Ahn, Hwi Ryun Kwon, Jae Hyuk Lee, Kang Seo Park, Kyung Ah Han
- Diabetes Metab J. 2014;38(6):439-448. Published online December 15, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.6.439
- 4,677 View
- 32 Download
- 9 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Arterial stiffness is an important factor in atherosclerosis. Thus we examined whether aerobic exercise could reduce arterial stiffness in obese women with type 2 diabetes without diabetic complication.
Methods A total of 35 women with type 2 diabetes (body mass index, 26.6±2.8 kg/m2; age, 56.4±1.9 years; duration of diabetes, 4.7±4.8 years) were assigned to aerobic exercise group (AEG) or control group (CG). AEG completed a 12-week exercise program (3.6 to 5.2 metabolic equivalents, 3 day/week, 60 min/day), with their exercise activities monitored by accelerometers. We measured abdominal total fat area (TFA), visceral fat area (VFA), and subcutaneous fat area (SFA) by computed tomography, insulin sensitivity by insulin tolerance test (KITT), and augmentation index (AIx) by SphygmoCor at baseline and at the end of the 12-week program.
Results The AIx was improved in the AEG compared with the CG (
P <0.001). The percent change of AIx had significant correlation with the improvement of physical activity energy expenditure (PAEE), aerobic capacity, TFA, and SFA (r =-0.416,P =0.013;r =0.560,P <0.001;r =0.489,P =0.003;r =0.531,P =0.001, respectively), but not with insulin sensitivity, energy intake, or VFA.Conclusion Improvement in aortic stiffness by aerobic exercise is related with the improvement of aerobic capacity, PAEE, and total fat but not with insulin sensitivity or energy intake in obese women with type 2 diabetes.
-
Citations
Citations to this article as recorded by- Relationship between objectively measured physical activity and subclinical cardiovascular disease: a systematic review
Aparna Narendrula, Ellen Brinza, Christine Horvat Davey, Chris T Longenecker, Allison R Webel
BMJ Open Sport & Exercise Medicine.2024; 10(1): e001596. CrossRef - Aerobic training reduces pancreatic fat content and improves β‐cell function: A randomized controlled trial using IDEAL‐IQ magnetic resonance imaging
Min Li, Qidong Zheng, Joshua D. Miller, Panpan Zuo, Xiaodan Yuan, Jitao Feng, Chao Liu, Shan Bao, Qingqing Lou
Diabetes/Metabolism Research and Reviews.2022;[Epub] CrossRef - Effect of aerobic exercise on waist circumference in adults with overweight or obesity: A systematic review and meta‐analysis
Alex Armstrong, Klaus Jungbluth Rodriguez, Angelo Sabag, Yorgi Mavros, Helen M. Parker, Shelley E. Keating, Nathan A. Johnson
Obesity Reviews.2022;[Epub] CrossRef - Aortic waveform responses to insulin in late versus early chronotype with metabolic syndrome
Mary‐Margaret E. Remchak, Emily M. Heiston, Anna Ballantyne, Brielle L. Dotson, Steven K. Malin
Physiological Reports.2022;[Epub] CrossRef - Exercise and ectopic fat in type 2 diabetes: A systematic review and meta-analysis
A. Sabag, K.L. Way, S.E. Keating, R.N. Sultana, H.T. O’Connor, M.K. Baker, V.H. Chuter, J. George, N.A. Johnson
Diabetes & Metabolism.2017; 43(3): 195. CrossRef - Arterial Stiffness Measured with the Cuff Oscillometric Method Is Predictive of Exercise Capacity in Patients with Cardiac Diseases
Yasushi Tazawa, Nobuyoshi Mori, Yoshiko Ogawa, Osamu Ito, Masahiro Kohzuki
The Tohoku Journal of Experimental Medicine.2016; 239(2): 127. CrossRef
- Relationship between objectively measured physical activity and subclinical cardiovascular disease: a systematic review
- The Role of Skeletal Muscle in Development of Nonalcoholic Fatty Liver Disease
- Jun Sung Moon, Ji Sung Yoon, Kyu Chang Won, Hyoung Woo Lee
- Diabetes Metab J. 2013;37(4):278-285. Published online August 14, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.4.278
- 4,640 View
- 49 Download
- 58 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Nonalcoholic fatty liver disease (NAFLD) is closely correlated with abnormal accumulation of visceral fat, but the role of skeletal muscle remains unclear. The aim of this study was to elucidate the role of skeletal muscle in development of NAFLD.
Methods Among 11,116 subjects (6,242 males), we examined the effects of skeletal muscle mass and visceral fat area (VFA, by bioelectric impedance analysis) on NAFLD using by the fatty liver index (FLI).
Results Of the total subjects (9,565 total, 5,293 males) included, 1,848 were classified as having NALFD (FLI ≥60). Body mass index, lipid profile, fasting plasma glucose, hemoglobin A1c, prevalence of type 2 diabetes (DM), hypertension (HTN), and metabolic syndrome were higher in males than females, but FLI showed no significant difference. The low FLI group showed the lowest VFA and highest skeletal muscle mass of all the groups. Skeletal muscle to visceral fat ratio (SVR) and skeletal muscle index had inverse correlations with FLI, when adjusted for age and gender. In multivariate regression analysis, SVR was negatively associated with FLI. Among SVR quartiles, the highest quartile showed very low risk of NAFLD when adjusted for age, gender, lipid profile, DM, HTN, and high sensitivity C-reactive protein from the lowest quartiles (odds ratio, 0.037; 95% confidence interval, 0.029 to 0.049).
Conclusion Skeletal muscle mass was inversely associated with visceral fat area, and higher skeletal muscle mass may have a beneficial effect in preventing NAFLD. These results suggest that further studies are needed to ameliorate or slow the progression of sarcopenia.
-
Citations
Citations to this article as recorded by- Effects of nonalcoholic fatty liver disease on sarcopenia: evidence from genetic methods
Jiaqin Yuan, Jinglin Zhang, Qiang Luo, Lipeng Peng
Scientific Reports.2024;[Epub] CrossRef - Influence of Sugar-Sweetened Beverages Intake on Sarcopenic Obesity, Visceral Obesity, and Sarcopenia in Lebanese Patients with MASLD: A Case-Control Study
Maha Hoteit, Myriam Dagher, Nikolaos Tzenios, Najat Al Kaaki, Ghadir Rkein, Abdul Rahman Chahine, Yonna Sacre, Samer Hotayt, Rami Matar, Mahmoud Hallal, Micheal Maitar, Bilal Hotayt
Healthcare.2024; 12(5): 591. CrossRef - Increased visceral fat area to skeletal muscle mass ratio is positively associated with the risk of metabolic dysfunction-associated steatotic liver disease in a Chinese population
Chenbing Liu, Nan Li, Di Sheng, Yahong Shao, Lihong Qiu, Chao Shen, Zhong Liu
Lipids in Health and Disease.2024;[Epub] CrossRef - Using hyperhomocysteinemia and body composition to predict the risk of non-alcoholic fatty liver disease in healthcare workers
Xiaoyan Hao, Honghai He, Liyuan Tao, Peng Wang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Diagnostic Criteria and Prognostic Relevance of Sarcopenia in Patients with Inflammatory Bowel Disease—A Systematic Review
Claudia-Gabriela Potcovaru, Petruța Violeta Filip, Oana-Maria Neagu, Laura Sorina Diaconu, Teodor Salmen, Delia Cinteză, Anca Pantea Stoian, Florin Bobirca, Mihai Berteanu, Corina Pop
Journal of Clinical Medicine.2023; 12(14): 4713. CrossRef - Association between Muscle Mass Deficits and Metabolic Dysfunction-Associated Fatty Liver Disease in Adults with Body Mass Index Less than 23 kg/m2
Mi Young Lee, Hee Jeong Choi, Han Jin Oh
Korean Journal of Family Practice.2023; 13(3): 171. CrossRef - Sex influences the association between appendicular skeletal muscle mass to visceral fat area ratio and non-alcoholic steatohepatitis in patients with biopsy-proven non-alcoholic fatty liver disease
Gang Li, Rafael S. Rios, Xin-Xin Wang, Yue Yu, Kenneth I. Zheng, Ou-Yang Huang, Liang-Jie Tang, Hong-Lei Ma, Yi Jin, Giovanni Targher, Christopher D. Byrne, Xiao-Yan Pan, Ming-Hua Zheng
British Journal of Nutrition.2022; 127(11): 1613. CrossRef - 2019 Global NAFLD Prevalence: A Systematic Review and Meta-analysis
Michael H. Le, Yee Hui Yeo, Xiaohe Li, Jie Li, Biyao Zou, Yuankai Wu, Qing Ye, Daniel Q. Huang, Changqing Zhao, Jie Zhang, Chenxi Liu, Na Chang, Feng Xing, Shiping Yan, Zi Hui Wan, Natasha Sook Yee Tang, Maeda Mayumi, Xinting Liu, Chuanli Liu, Fajuan Rui,
Clinical Gastroenterology and Hepatology.2022; 20(12): 2809. CrossRef - Impact of Sarcopenia and Myosteatosis in Non-Cirrhotic Stages of Liver Diseases: Similarities and Differences across Aetiologies and Possible Therapeutic Strategies
Annalisa Cespiati, Marica Meroni, Rosa Lombardi, Giovanna Oberti, Paola Dongiovanni, Anna Ludovica Fracanzani
Biomedicines.2022; 10(1): 182. CrossRef - Impact of Sarcopenia on the Severity of the Liver Damage in Patients With Non-alcoholic Fatty Liver Disease
Vittoria Zambon Azevedo, Cristina Alina Silaghi, Thomas Maurel, Horatiu Silaghi, Vlad Ratziu, Raluca Pais
Frontiers in Nutrition.2022;[Epub] CrossRef - Fatty Liver Index and Skeletal Muscle Density
Julie A. Pasco, Sophia X. Sui, Emma C. West, Kara B. Anderson, Pamela Rufus-Membere, Monica C. Tembo, Natalie K. Hyde, Lana J. Williams, Zoe S. J. Liu, Mark A. Kotowicz
Calcified Tissue International.2022; 110(6): 649. CrossRef - Skeletal muscle mass to visceral fat area ratio as a predictor of NAFLD in lean and overweight men and women with effect modification by sex
Yoosun Cho, Yoosoo Chang, Seungho Ryu, Hyun‐Suk Jung, Chan‐won Kim, Hyungseok Oh, Mi Kyung Kim, Won Sohn, Hocheol Shin, Sarah H. Wild, Christopher D. Byrne
Hepatology Communications.2022; 6(9): 2238. CrossRef - Association of Low Skeletal Muscle Mass with the Phenotype of Lean Non-Alcoholic Fatty Liver Disease
Jun-Hyeon Byeon, Min-Kyu Kang, Min-Cheol Kim
Healthcare.2022; 10(5): 850. CrossRef - Muscle strength, but not body mass index, is associated with mortality in patients with non‐alcoholic fatty liver disease
Phunchai Charatcharoenwitthaya, Khemajira Karaketklang, Wichai Aekplakorn
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(5): 2393. CrossRef - Effect of progressive resistance training with weight loss compared with weight loss alone on the fatty liver index in older adults with type 2 diabetes: secondary analysis of a 12-month randomized controlled trial
Christine L Freer, Elena S George, Sze-Yen Tan, Gavin Abbott, David W Dunstan, Robin M Daly
BMJ Open Diabetes Research & Care.2022; 10(5): e002950. CrossRef - Muscle Krüppel-like factor 15 regulates lipid flux and systemic metabolic homeostasis
Liyan Fan, David R. Sweet, Domenick A. Prosdocimo, Vinesh Vinayachandran, Ernest R. Chan, Rongli Zhang, Olga Ilkayeva, Yuan Lu, Komal S. Keerthy, Chloe E. Booth, Christopher B. Newgard, Mukesh K. Jain
Journal of Clinical Investigation.2021;[Epub] CrossRef - “Bioelectrical impedance analysis in managing sarcopenic obesity in NAFLD”
David J. Hanna, Scott T. Jamieson, Christine S. Lee, Christopher A. Pluskota, Nicole J. Bressler, Peter N. Benotti, Sandeep Khurana, David D. K. Rolston, Christopher D. Still
Obesity Science & Practice.2021; 7(5): 629. CrossRef - Decreased Muscle-to-Fat Mass Ratio Is Associated with Low Muscular Fitness and High Alanine Aminotransferase in Children and Adolescent Boys in Organized Sports Clubs
Kai Ushio, Yukio Mikami, Hiromune Obayashi, Hironori Fujishita, Kouki Fukuhara, Tetsuhiko Sakamitsu, Kazuhiko Hirata, Yasunari Ikuta, Hiroaki Kimura, Nobuo Adachi
Journal of Clinical Medicine.2021; 10(11): 2272. CrossRef - Association of Skeletal Muscle and Adipose Tissue Distribution with Histologic Severity of Non-Alcoholic Fatty Liver
Min-Kyu Kang, Jung-Hun Baek, Young-Oh Kweon, Won-Young Tak, Se-Young Jang, Yu-Rim Lee, Keun Hur, Gyeonghwa Kim, Hye-Won Lee, Man-Hoon Han, Joon-Hyuk Choi, Soo-Young Park, Jung-Gil Park
Diagnostics.2021; 11(6): 1061. CrossRef - Association of Body Composition and Sarcopenia with NASH in Obese Patients
Sophia Marie-Therese Schmitz, Lena Schooren, Andreas Kroh, Alexander Koch, Christine Stier, Ulf Peter Neumann, Tom Florian Ulmer, Patrick Hamid Alizai
Journal of Clinical Medicine.2021; 10(15): 3445. CrossRef - Patchouli alcohol ameliorates skeletal muscle insulin resistance and NAFLD via AMPK/SIRT1-mediated suppression of inflammation
Do Hyeon Pyun, Tae Jin Kim, Seung Yeon Park, Hyun Jung Lee, A.M. Abd El-Aty, Ji Hoon Jeong, Tae Woo Jung
Molecular and Cellular Endocrinology.2021; 538: 111464. CrossRef - Hepatic Steatosis Contributes to the Development of Muscle Atrophy via Inter-Organ Crosstalk
Kenneth Pasmans, Michiel E. Adriaens, Peter Olinga, Ramon Langen, Sander S. Rensen, Frank G. Schaap, Steven W. M. Olde Damink, Florian Caiment, Luc J. C. van Loon, Ellen E. Blaak, Ruth C. R. Meex
Frontiers in Endocrinology.2021;[Epub] CrossRef - Muscle mass and cellular membrane integrity assessment in patients with nonalcoholic fatty liver disease
Iasmin dos Santos Barreto, Raquel Oliveira dos Santos, Raquel Rocha, Claudineia de Souza, Naiade Almeida, Luiza Valois Vieira, Rafael Leiróz, Manoel Sarno, Carla Daltro, Helma Pinchemel Cotrim
Revista da Associação Médica Brasileira.2021; 67(9): 1233. CrossRef - A significant association of non-obese non-alcoholic fatty liver disease with sarcopenic obesity
Kazuhiro Kashiwagi, Michiyo Takayama, Kayoko Fukuhara, Ryoko Shimizu-Hirota, Po-Sung Chu, Nobuhiro Nakamoto, Nagamu Inoue, Yasushi Iwao, Takanori Kanai
Clinical Nutrition ESPEN.2020; 38: 86. CrossRef - Improvement in Menopause-Associated Hepatic Lipid Metabolic Disorders by Herbal Formula HPC03 on Ovariectomized Rats
BoYoon Chang, Dae Sung Kim, SungYeon Kim
Evidence-Based Complementary and Alternative Medicine.2020; 2020: 1. CrossRef - Sarcopenia is associated with non-alcoholic fatty liver disease in men with type 2 diabetes
D.H. Seo, Y.-h. Lee, S.W. Park, Y.J. Choi, B.W. Huh, E. Lee, K.B. Huh, S.H. Kim, B.-S. Cha
Diabetes & Metabolism.2020; 46(5): 362. CrossRef - Nonalcoholic fatty liver disease and sarcopenia: pathophysiological connections and therapeutic implications
Tiziana Fernández-Mincone, Felipe Contreras-Briceño, Maximiliano Espinosa-Ramírez, Patricio García-Valdés, Antonio López-Fuenzalida, Arnoldo Riquelme, Juan Pablo Arab, Daniel Cabrera, Marco Arrese, Francisco Barrera
Expert Review of Gastroenterology & Hepatology.2020; 14(12): 1141. CrossRef - Association between Atrial Fibrillation and Advanced Liver Fibrosis in Patients with Non-Alcoholic Fatty Liver Disease
Min Kyu Kang, Jung Gil Park, Min Cheol Kim
Yonsei Medical Journal.2020; 61(10): 860. CrossRef - Relative fat mass at baseline and its early change may be a predictor of incident nonalcoholic fatty liver disease
Hwi Young Kim, Su Jung Baik, Hye Ah Lee, Byoung Kwon Lee, Hye Sun Lee, Tae Hun Kim, Kwon Yoo
Scientific Reports.2020;[Epub] CrossRef - Fisetin Alleviates Hepatic and Adipocyte Fibrosis and Insulin Resistance in Diet-Induced Obese Mice
Myung-Sook Choi, Ji-Young Choi, Eun-Young Kwon
Journal of Medicinal Food.2020; 23(10): 1019. CrossRef - Relationship between relative skeletal muscle mass and nonalcoholic fatty liver disease: a systematic review and meta-analysis
Changzhou Cai, Xin Song, Yishu Chen, Xueyang Chen, Chaohui Yu
Hepatology International.2020; 14(1): 115. CrossRef - Sarcopenia Is a New Risk Factor of Nonalcoholic Fatty Liver Disease in Patients with Inflammatory Bowel Disease
Min Kyu Kang, Kyeong Ok Kim, Min Cheol Kim, Jung Gil Park, Byung Ik Jang
Digestive Diseases.2020; 38(6): 507. CrossRef - Relationship between Muscle Mass/Strength and Hepatic Fat Content in Post-Menopausal Women
Yajie Zhang, Dajiang Lu, Renwei Wang, Weijie Fu, Shengnian Zhang
Medicina.2019; 55(10): 629. CrossRef - Lower hand grip strength in older adults with non-alcoholic fatty liver disease: a nationwide population-based study
Beom-Jun Kim, Seong Hee Ahn, Seung Hun Lee, Seongbin Hong, Mark W. Hamrick, Carlos M. Isales, Jung-Min Koh
Aging.2019; 11(13): 4547. CrossRef - Nonalcoholic Fatty Liver Disease in Nonobese Subjects of African Origin Has Atypical Metabolic Characteristics
Debbie S Thompson, Ingrid A Tennant, Deanne P Soares, Clive Osmond, Chris D Byrne, Terrence E Forrester, Michael S Boyne
Journal of the Endocrine Society.2019; 3(11): 2051. CrossRef - Sarcopenia in patients with non‐alcoholic fatty liver disease: is it a clinically significant entity?
C. H. De Fré, M. A. De Fré, W. J. Kwanten, B. J. Op de Beeck, L. F. Van Gaal, S. M. Francque
Obesity Reviews.2019; 20(2): 353. CrossRef - Nonalcoholic Fatty Liver Disease in The Rotterdam Study: About Muscle Mass, Sarcopenia, Fat Mass, and Fat Distribution
Louise Johanna Maria Alferink, Katerina Trajanoska, Nicole Stephanie Erler, Josje Dorothea Schoufour, Robert Jacobus de Knegt, M. Arfan Ikram, Harry Leonardus Antonius Janssen, Oscar H. Franco, Herold J. Metselaar, Fernando Rivadeneira, Sarwa Darwish Mura
Journal of Bone and Mineral Research.2019; 34(7): 1254. CrossRef - Sarcopenia Is Significantly Associated with Presence and Severity of Nonalcoholic Fatty Liver Disease
Goh Eun Chung, Min Joo Kim, Jeong Yoon Yim, Joo Sung Kim, Ji Won Yoon
Journal of Obesity & Metabolic Syndrome.2019; 28(2): 129. CrossRef - Association of low skeletal muscle mass with advanced liver fibrosis in patients with non‐alcoholic fatty liver disease
Min Kyu Kang, Jung Gil Park, Heon Ju Lee, Min Cheol Kim
Journal of Gastroenterology and Hepatology.2019; 34(9): 1633. CrossRef - Whole‐body vibration for patients with nonalcoholic fatty liver disease: a 6‐month prospective study
Sechang Oh, Natsumi Oshida, Noriko Someya, Tsuyoshi Maruyama, Tomonori Isobe, Yoshikazu Okamoto, Taeho Kim, Bokun Kim, Junichi Shoda
Physiological Reports.2019; 7(9): e14062. CrossRef - L-Lysine Attenuates Hepatic Steatosis in Senescence-Accelerated Mouse Prone 8 Mice
Tomonori SATO, Nao MURAMATSU, Yoshiaki ITO, Yoshio YAMAMOTO, Takashi NAGASAWA
Journal of Nutritional Science and Vitaminology.2018; 64(3): 192. CrossRef - Short-term treatment with metformin reduces hepatic lipid accumulation but induces liver inflammation in obese mice
Alexandre Abilio de Souza Teixeira, Camila O. Souza, Luana A. Biondo, Loreana Sanches Silveira, Edson A. Lima, Helena A. Batatinha, Adriane Pereira Araujo, Michele Joana Alves, Sandro Massao Hirabara, Rui Curi, José Cesar Rosa Neto
Inflammopharmacology.2018; 26(4): 1103. CrossRef - Vitamin D and Related Deficiencies, Sarcopenia and Visceral Obesity in Obese People with NAFLD
Mihaela Petrova
Gastroenterology & Hepatology: Open Access.2018;[Epub] CrossRef - Grip Strength Moderates the Association between Anthropometric and Body Composition Indicators and Liver Fat in Youth with an Excess of Adiposity
Robinson Ramírez-Vélez, Mikel Izquierdo, Jorge Correa-Bautista, Alejandra Tordecilla-Sanders, María Correa-Rodríguez, Jacqueline Schmidt Rio-Valle, Emilio González-Jiménez, Katherine González-Ruíz
Journal of Clinical Medicine.2018; 7(10): 347. CrossRef - Longitudinal Changes in Muscle Mass and Strength, and Bone Mass in Older Adults: Gender-Specific Associations Between Muscle and Bone Losses
Kyoung Min Kim, Soo Lim, Tae Jung Oh, Jae Hoon Moon, Sung Hee Choi, Jae Young Lim, Ki Woong Kim, Kyong Soo Park, Hak Chul Jang
The Journals of Gerontology: Series A.2018; 73(8): 1062. CrossRef - Non-alcoholic fatty liver disease connections with fat-free tissues: A focus on bone and skeletal muscle
Eleonora Poggiogalle, Lorenzo Maria Donini, Andrea Lenzi, Claudio Chiesa, Lucia Pacifico
World Journal of Gastroenterology.2017; 23(10): 1747. CrossRef - Sarcopenia and non-alcoholic fatty liver disease: Is there a relationship? A systematic review
Cristiane V Tovo, Sabrina A Fernandes, Caroline Buss, Angelo A de Mattos
World Journal of Hepatology.2017; 9(6): 326. CrossRef - Multiple molecular targets in the liver, adipose tissue and skeletal muscle in ginger-elicited amelioration of nonalcoholic fatty liver disease
Chunxia Wang, Robert Batey, Johji Yamahara, Yuhao Li
Journal of Functional Foods.2017; 36: 43. CrossRef - Importance of Lean Muscle Maintenance to Improve Insulin Resistance by Body Weight Reduction in Female Patients with Obesity
Yaeko Fukushima, Satoshi Kurose, Hiromi Shinno, Ha Cao Thu, Nana Takao, Hiromi Tsutsumi, Yutaka Kimura
Diabetes & Metabolism Journal.2016; 40(2): 147. CrossRef - Fatty Liver Index Associates with Relative Sarcopenia and GH/ IGF- 1 Status in Obese Subjects
Eleonora Poggiogalle, Carla Lubrano, Lucio Gnessi, Stefania Mariani, Andrea Lenzi, Lorenzo Maria Donini, Rasheed Ahmad
PLOS ONE.2016; 11(1): e0145811. CrossRef - The relationship between hepatic steatosis and skeletal muscle mass index in men with type 2 diabetes
Yoshitaka Hashimoto, Takafumi Osaka, Takuya Fukuda, Muhei Tanaka, Masahiro Yamazaki, Michiaki Fukui
Endocrine Journal.2016; 63(10): 877. CrossRef - Sarcopenia and the cardiometabolic syndrome: A narrative review
G. Bahat, B. İlhan
European Geriatric Medicine.2016; 7(3): 220. CrossRef - Low skeletal muscle mass is associated with non-alcoholic fatty liver disease in Korean adults: the Fifth Korea National Health and Nutrition Examination Survey
Hee Yeon Kim, Chang Wook Kim, Chung-Hwa Park, Jong Young Choi, Kyungdo Han, Anwar T Merchant, Yong-Moon Park
Hepatobiliary & Pancreatic Diseases International.2016; 15(1): 39. CrossRef - Non-alcoholic fatty liver disease and cardiovascular risk: Pathophysiological mechanisms and implications
Sven M. Francque, Denise van der Graaff, Wilhelmus J. Kwanten
Journal of Hepatology.2016; 65(2): 425. CrossRef - Differences among skeletal muscle mass indices derived from height-, weight-, and body mass index-adjusted models in assessing sarcopenia
Kyoung Min Kim, Hak Chul Jang, Soo Lim
The Korean Journal of Internal Medicine.2016; 31(4): 643. CrossRef - Relationship between grip strength and newly diagnosed nonalcoholic fatty liver disease in a large-scale adult population
Ge Meng, Hongmei Wu, Liyun Fang, Chunlei Li, Fei Yu, Qing Zhang, Li Liu, Huanmin Du, Hongbin Shi, Yang Xia, Xiaoyan Guo, Xing Liu, Xue Bao, Qian Su, Yeqing Gu, Huijun Yang, Bin Yu, Yuntang Wu, Zhong Sun, Kaijun Niu
Scientific Reports.2016;[Epub] CrossRef - Volume-dependent effect of supervised exercise training on fatty liver and visceral adiposity index in subjects with type 2 diabetes The Italian Diabetes Exercise Study (IDES)
Stefano Balducci, Patrizia Cardelli, Luca Pugliese, Valeria D’Errico, Jonida Haxhi, Elena Alessi, Carla Iacobini, Stefano Menini, Lucilla Bollanti, Francesco G. Conti, Antonio Nicolucci, Giuseppe Pugliese
Diabetes Research and Clinical Practice.2015; 109(2): 355. CrossRef - Sarcopenia is a risk factor for elevated aminotransferase in men independently of body mass index, dietary habits, and physical activity
Ki Deok Yoo, Dae Won Jun, Kang Nyeong Lee, Hang Lak Lee, Oh Young Lee, Byung Chul Yoon, Ho Soon Choi
Digestive and Liver Disease.2015; 47(4): 303. CrossRef
- Effects of nonalcoholic fatty liver disease on sarcopenia: evidence from genetic methods
- Effects of Exercise Alone on Insulin Sensitivity and Glucose Tolerance in Obese Youth
- SoJung Lee, YoonMyung Kim
- Diabetes Metab J. 2013;37(4):225-232. Published online August 14, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.4.225
- 3,899 View
- 38 Download
- 18 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader As with the dramatic increases in childhood obesity over the past decades, the incidence of type 2 diabetes has increased among children and adolescents in the United States. Insulin resistance is a common feature of childhood obesity and increases the risk of type 2 diabetes, metabolic syndrome, and atherogenic lipoprotein profile in obese youth. Although cross-sectional studies report beneficial effects of physical activity or cardiorespiratory fitness on insulin sensitivity, the role of regular exercise alone (e.g., no calorie restriction) as a strategy to reduce the risk of type 2 diabetes is unclear in obese children and adolescents. In this mini review, we examined the independent effects of various exercise on glucose tolerance and insulin sensitivity in obese youth.
-
Citations
Citations to this article as recorded by- Lifestyle and Pharmacological Interventions and Treatment Indications for the Management of Obesity in Children and Adolescents
Despina Herouvi, George Paltoglou, Alexandra Soldatou, Christina Kalpia, Spyridon Karanasios, Kyriaki Karavanaki
Children.2023; 10(7): 1230. CrossRef - Obesity blunts insulin sensitivity improvements and attenuates strength gains following resistance training in nondiabetic men
Ramzi A. Al-Horani, Khaled M. Alsays, Osama Abo Alrob
European Journal of Applied Physiology.2023;[Epub] CrossRef - Predictors of postprandial glycaemia, insulinaemia and insulin resistance in adolescents
Ryan A. Williams, Karah J. Dring, Simon B. Cooper, John G. Morris, Caroline Sunderland, Mary E. Nevill
British Journal of Nutrition.2021; 125(10): 1101. CrossRef - New insights into the pharmacological treatment of pediatric patients with type 2 diabetes
Tatsuhiko Urakami
Clinical Pediatric Endocrinology.2018; 27(1): 1. CrossRef - Effect of 7 days of exercise on exogenous carbohydrate oxidation and insulin resistance in children with obesity
Lisa Chu, Katherine M. Morrison, Michael C. Riddell, Sandeep Raha, Brian W. Timmons
Applied Physiology, Nutrition, and Metabolism.2018; 43(7): 677. CrossRef - 12-Week aerobic exercise and nutritional program minimized the presence of the 64Arg allele on insulin resistance
Gerusa E. Milano-Gai, Lupe Furtado-Alle, Jorge Mota, Leilane Lazarotto, Gisele E. Milano, Ricardo R. de Souza Lehtonen, Ana C.K. Titski, Íncare C. Jesus, Luciane V. Tureck, Rosana B. Radominski, Manuel João Coelho-e-Silva, Neiva Leite
Journal of Pediatric Endocrinology and Metabolism.2018; 31(9): 1033. CrossRef - ADRB2 Gln27Glu polymorphism influenced changes in leptin but not body composition or metabolic and other inflammatory parameters after twelve weeks of combined training in overweight adolescents
Neiva Leite, Larissa Rosa da Silva, Íncare Correa de Jesus, Wendell Arthur Lopes, Claudia Regina Cavaglieri, Cássio Leandro Consentino, Rosana Bento Radominski, Ricardo Lehtonen Rodrigues de Souza, Luciane Viater Tureck, Lupe Furtado-Alle
Motriz: Revista de Educação Física.2018;[Epub] CrossRef - Patterns of Physical Activity Adherence by Adolescents With Diabetes or Obesity Enrolled in a Personalized Community-Based Intervention
Sara F. Michaliszyn, Melinda Higgins, Melissa Spezia Faulkner
The Diabetes Educator.2018; 44(6): 519. CrossRef - Diet Quality and Mortality Risk in Metabolically Obese Normal-Weight Adults
Yong-Moon Mark Park, Teresa T. Fung, Susan E. Steck, Jiajia Zhang, Linda J. Hazlett, Kyungdo Han, Seung-Hwan Lee, Anwar T. Merchant
Mayo Clinic Proceedings.2016; 91(10): 1372. CrossRef - Mediterranean diet and mortality risk in metabolically healthy obese and metabolically unhealthy obese phenotypes
Y-M Park, S E Steck, T T Fung, J Zhang, L J Hazlett, K Han, A T Merchant
International Journal of Obesity.2016; 40(10): 1541. CrossRef - Efeitos metabólicos do exercício físico na obesidade infantil: uma visão atual
Santiago Tavares Paes, João Carlos Bouzas Marins, Ana Eliza Andreazzi
Revista Paulista de Pediatria.2015; 33(1): 122. CrossRef - Metabolic effects of exercise on childhood obesity: a current view
Santiago Tavares Paes, João Carlos Bouzas Marins, Ana Eliza Andreazzi
Revista Paulista de Pediatria (English Edition).2015; 33(1): 122. CrossRef - Impact of regular physical activity on blood glucose control and cardiovascular risk factors in adolescents with type 2 diabetes mellitus - a multicenter study of 578 patients from 225 centres
A Herbst, T Kapellen, E Schober, C Graf, T Meissner, RW Holl
Pediatric Diabetes.2015; 16(3): 204. CrossRef - Impact of exercise training without caloric restriction on inflammation, insulin resistance and visceral fat mass in obese adolescents
M. Mendelson, A.‐S. Michallet, D. Monneret, C. Perrin, F. Estève, P. R. Lombard, P. Faure, P. Lévy, A. Favre‐Juvin, J.‐L. Pépin, B. Wuyam, P. Flore
Pediatric Obesity.2015; 10(4): 311. CrossRef - Early-life sleep deprivation persistently depresses melatonin production and bio-energetics of the pineal gland: potential implications for the development of metabolic deficiency
Li-You Chen, Cheng Tiong, Chung-Hung Tsai, Wen-Chieh Liao, Shun-Fa Yang, Su-Chung Youn, Fu-Der Mai, Hung-Ming Chang
Brain Structure and Function.2015; 220(2): 663. CrossRef - Whey Protein Improves Exercise Performance and Biochemical Profiles in Trained Mice
WEN-CHYUAN CHEN, WEN-CHING HUANG, CHIEN-CHAO CHIU, YU-KAI CHANG, CHI-CHANG HUANG
Medicine & Science in Sports & Exercise.2014; 46(8): 1517. CrossRef - Type 2 diabetes in the child and adolescent
Phil Zeitler, Junfen Fu, Nikhil Tandon, Kristen Nadeau, Tatsuhiko Urakami, Timothy Barrett, David Maahs
Pediatric Diabetes.2014; 15(S20): 26. CrossRef - ENDOCRINOLOGY AND ADOLESCENCE: Aerobic exercise reduces insulin resistance markers in obese youth: a meta-analysis of randomized controlled trials
Antonio García-Hermoso, Jose M Saavedra, Yolanda Escalante, Mairena Sánchez-López, Vicente Martínez-Vizcaíno
European Journal of Endocrinology.2014; 171(4): R163. CrossRef
- Lifestyle and Pharmacological Interventions and Treatment Indications for the Management of Obesity in Children and Adolescents
- Influence of Visceral Adiposity on Cardiovascular Autonomic Neuropathy in Patients with Type 2 Diabetes Mellitus
- Eun-Hee Jang, Na-Young Kim, Yong-Moon Park, Mee-Kyoung Kim, Ki Hyun Baek, Ki-Ho Song, Kwang Woo Lee, Hyuk-Sang Kwon
- Diabetes Metab J. 2012;36(4):285-292. Published online August 20, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.4.285
- 3,597 View
- 36 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this study was to investigate the influences of visceral adiposity on cardiovascular autonomic neuropathy (CAN) in patients with type 2 diabetes mellitus.
Methods Two hundred eleven patients with type 2 diabetes participated in this study. Anthropometric and metabolic parameters were measured, and the visceral fat area was assessed using computed tomography. CAN was diagnosed using a cardiovascular reflex test. We analyzed the correlation between the visceral fat area and each parameter in this test.
Results The mean age, body mass index (BMI), and duration of diabetes of the study population were 60±14 years (mean±standard deviation), 25.1±4.2 kg/m2, and 12.3±8.9 years, respectively. The visceral fat area showed positive correlations with age, BMI, waist circumference, and subcutaneous fat area. There was no statistically significant difference in the cardiovascular reflex test outcome between genders. Univariate linear regression analysis showed that an increased visceral fat area diminished good heart rate response to a Valsalva maneuver (
R 2=4.9%,P =0.013 in an unadjusted model), but only in women. This statistical association was preserved after adjusting for age and BMI (R 2=9.8%,P =0.0072).Conclusion The results of this study suggest that visceral adiposity contributes to an autonomic imbalance to some degree, as demonstrated by the impaired cardiovascular reflex test among women with type 2 diabetes.
-
Citations
Citations to this article as recorded by- Excessive generalized and visceral adiposity is associated with a higher prevalence of diabetic retinopathy in Caucasian patients with type 2 diabetes
Andrea Tumminia, Agostino Milluzzo, Nunzia Carrubba, Federica Vinciguerra, Roberto Baratta, Lucia Frittitta
Nutrition, Metabolism and Cardiovascular Diseases.2024; 34(3): 763. CrossRef - Obesity, Metabolic Syndrome and the Risk of Microvascular Complications in Patients with Diabetes mellitus
Niki Katsiki, Panagiotis Anagnostis, Kalliopi Kotsa, Dimitrios G. Goulis, Dimitri P. Mikhailidis
Current Pharmaceutical Design.2019; 25(18): 2051. CrossRef - Morphologic Comparison of Peripheral Nerves in Adipocyte Tissue from db/db Diabetic versus Normal Mice
Kyung Ae Lee, Na Young Lee, Tae Sun Park, Heung Yong Jin
Diabetes & Metabolism Journal.2018; 42(2): 169. CrossRef - Gender differences in the perception of difficulty of self-management in patients with diabetes mellitus: a mixed-methods approach
Hideyo Tsutsui, Kyoko Nomura, Masataka Kusunoki, Tetsuya Ishiguro, Takayoshi Ohkubo, Yoshiharu Oshida
Diabetology International.2016; 7(3): 289. CrossRef - Contribution of subcutaneous abdominal fat on ultrasonography to carotid atherosclerosis in patients with type 2 diabetes mellitus
Chan-Hee Jung, Bo-Yeon Kim, Kyu-Jin Kim, Sang-Hee Jung, Chul-Hee Kim, Sung-Koo Kang, Ji-Oh Mok
Cardiovascular Diabetology.2014;[Epub] CrossRef
- Excessive generalized and visceral adiposity is associated with a higher prevalence of diabetic retinopathy in Caucasian patients with type 2 diabetes
- Effects of Aerobic Exercise Intensity on Abdominal and Thigh Adipose Tissue and Skeletal Muscle Attenuation in Overweight Women with Type 2 Diabetes Mellitus
- Ji Yeon Jung, Kyung Ah Han, Hee Jung Ahn, Hwi Ryun Kwon, Jae Hyuk Lee, Kang Seo Park, Kyung Wan Min
- Diabetes Metab J. 2012;36(3):211-221. Published online June 14, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.3.211
- 4,459 View
- 41 Download
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We investigated the effects of exercise intensity on abdominal and mid-thigh adipose tissue, attenuation of skeletal muscle, and insulin sensitivity in overweight women with type 2 diabetes mellitus (T2DM).
Methods Twenty-eight patients were randomly assigned to control (CG,
n =12), moderate intensity exercise (MEG,n =8), or vigorous intensity exercise (VEG,n =8) group. Subjects in both exercise groups completed a 12-week exercise program (MEG, 3.6 to 5.2 METs; VEG, ≥5.2 METs) that was monitored by accelerometers. We assessed body mass index (BMI), total fat area (TFA), visceral fat area (VFA), subcutaneous fat area (SFA), mid-thigh intramuscular adipose tissue (TIMAT), total skeletal muscle (TTM), low density skeletal muscle (TLDM), and normal density skeletal muscle (TNDM) using computed tomography, and measured insulin sensitivity with an insulin tolerance test (KITT), before and after the intervention.Results At baseline, the mean age was 53.8±7.9 years, duration of diabetes was 3.8±2.3 years, and BMI was 26.6±2.6 kg/m2. After 12 weeks, the percent change (%C) in BMI, TIMAT, and TLDM were not different among three groups. However, %C in TFA and VFA were significantly reduced in MEG compared to CG (
P =0.026 andP =0.008, respectively). %C SFA was significantly reduced in VEG compared to CG (P =0.038) and %C TTM, TNDM, and KITT were significantly increased in VEG compared to the CG (P =0.044,P =0.007, andP =0.016, respectively).Conclusion Although there was no difference in the change in BMI among groups, TFA and VFA were more reduced in MEG, and only VEG increased TTM, TNDM, and insulin sensitivity compared to CG.
-
Citations
Citations to this article as recorded by- Intermuscular adipose tissue in metabolic disease
Bret H. Goodpaster, Bryan C. Bergman, Andrea M. Brennan, Lauren M. Sparks
Nature Reviews Endocrinology.2023; 19(5): 285. CrossRef - Dose–response effects of exercise and caloric restriction on visceral adiposity in overweight and obese adults: a systematic review and meta-analysis of randomised controlled trials
Francesco Recchia, Chit K. Leung, Angus P. Yu, Welton Leung, Danny J. Yu, Daniel Y. Fong, David Montero, Chi-Ho Lee, Stephen H.S. Wong, Parco M. Siu
British Journal of Sports Medicine.2023; 57(16): 1035. CrossRef - Muscle quality: the assessment, prognosis, and intervention
翔 畑中, 洋祐 大須賀
Nippon Ronen Igakkai Zasshi. Japanese Journal of Geriatrics.2023; 60(2): 103. CrossRef - Associations of Muscle Density and Area With Coronary Artery Plaque and Physical Function
Kristine M. Erlandson, Triin Umbleja, Michael T. Lu, Jana Taron, Heather J. Ribaudo, Edgar T. Overton, Rachel M. Presti, David W. Haas, Paul E. Sax, Michael T. Yin, Bingxue Kris Zhai, Rochelle Louis, Namrata Upadhyay, Parastou Eslami, Pamela S. Douglas, M
JAIDS Journal of Acquired Immune Deficiency Syndromes.2023; 94(2): 174. CrossRef - Aerobic training reduces pancreatic fat content and improves β‐cell function: A randomized controlled trial using IDEAL‐IQ magnetic resonance imaging
Min Li, Qidong Zheng, Joshua D. Miller, Panpan Zuo, Xiaodan Yuan, Jitao Feng, Chao Liu, Shan Bao, Qingqing Lou
Diabetes/Metabolism Research and Reviews.2022;[Epub] CrossRef - Effect of aerobic exercise on waist circumference in adults with overweight or obesity: A systematic review and meta‐analysis
Alex Armstrong, Klaus Jungbluth Rodriguez, Angelo Sabag, Yorgi Mavros, Helen M. Parker, Shelley E. Keating, Nathan A. Johnson
Obesity Reviews.2022;[Epub] CrossRef - Effect of exercise on myosteatosis in adults: a systematic review and meta-analysis
Robinson Ramírez-Vélez, Yasmin Ezzatvar, Mikel Izquierdo, Antonio García-Hermoso
Journal of Applied Physiology.2021; 130(1): 245. CrossRef - Effect of exercise intervention dosage on reducing visceral adipose tissue: a systematic review and network meta-analysis of randomized controlled trials
Yu-Hsuan Chang, Hui-Ying Yang, Shiow-Ching Shun
International Journal of Obesity.2021; 45(5): 982. CrossRef - Exercise Training to Decrease Ectopic Intermuscular Adipose Tissue in Individuals With Chronic Diseases: A Systematic Review and Meta-Analysis
Mauro Tuñón-Suárez, Alvaro Reyes-Ponce, Rodrigo Godoy-Órdenes, Nicolás Quezada, Marcelo Flores-Opazo
Physical Therapy.2021;[Epub] CrossRef - Low-attenuation muscle is a predictor of diabetes mellitus: A population-based cohort study
Muhei Tanaka, Hiroshi Okada, Yoshitaka Hashimoto, Muneaki Kumagai, Hiromi Nishimura, Michiaki Fukui
Nutrition.2020; 74: 110752. CrossRef - Drop-out ratio between moderate to high-intensity physical exercise treatment by patients with, or at risk of, type 2 diabetes mellitus: A systematic review and meta-analysis
Guillem Jabardo-Camprubí, Rafel Donat-Roca, Mercè Sitjà-Rabert, Raimon Milà-Villarroel, Judit Bort-Roig
Physiology & Behavior.2020; 215: 112786. CrossRef - High-Intensity Interval Training Versus Moderate-Intensity Continuous Training in Middle-Aged and Older Patients with Type 2 Diabetes: A Randomized Controlled Crossover Trial of the Acute Effects of Treadmill Walking on Glycemic Control
Romeu Mendes, Nelson Sousa, José Luís Themudo-Barata, Victor Machado Reis
International Journal of Environmental Research and Public Health.2019; 16(21): 4163. CrossRef - Trunk muscle quality assessed by computed tomography: Association with adiposity indices and glucose tolerance in men
Alexandre Maltais, Natalie Alméras, Isabelle Lemieux, Angelo Tremblay, Jean Bergeron, Paul Poirier, Jean-Pierre Després
Metabolism.2018; 85: 205. CrossRef - Counting Footsteps with a Pedometer to Improve HMW Adiponectin and Metabolic Syndrome among Young Female Adults in the United Arab Emirates
Hayder Hasan, Amita Attlee, Hamid Jan Bin Jan Mohamed, Norliyana Aris, Wan Abdul Manan Bin Wan Muda
Journal of Obesity.2018; 2018: 1. CrossRef - Exercise and ectopic fat in type 2 diabetes: A systematic review and meta-analysis
A. Sabag, K.L. Way, S.E. Keating, R.N. Sultana, H.T. O’Connor, M.K. Baker, V.H. Chuter, J. George, N.A. Johnson
Diabetes & Metabolism.2017; 43(3): 195. CrossRef - Effect of aerobic exercise intensity on glycemic control in type 2 diabetes: a meta-analysis of head-to-head randomized trials
Yilina Liubaoerjijin, Tasuku Terada, Kevin Fletcher, Normand G. Boulé
Acta Diabetologica.2016; 53(5): 769. CrossRef - A systematic review and meta‐analysis on the effects of exercise training versus hypocaloric diet: distinct effects on body weight and visceral adipose tissue
R. J. H. M. Verheggen, M. F. H. Maessen, D. J. Green, A. R. M. M. Hermus, M. T. E. Hopman, D. H. T. Thijssen
Obesity Reviews.2016; 17(8): 664. CrossRef - Muscle wasting and aging: Experimental models, fatty infiltrations, and prevention
Thomas Brioche, Allan F. Pagano, Guillaume Py, Angèle Chopard
Molecular Aspects of Medicine.2016; 50: 56. CrossRef - Arterial Stiffness by Aerobic Exercise Is Related with Aerobic Capacity, Physical Activity Energy Expenditure and Total Fat but not with Insulin Sensitivity in Obese Female Patients with Type 2 Diabetes
Ji Yeon Jung, Kyung Wan Min, Hee Jung Ahn, Hwi Ryun Kwon, Jae Hyuk Lee, Kang Seo Park, Kyung Ah Han
Diabetes & Metabolism Journal.2014; 38(6): 439. CrossRef - Intermuscular Fat: A Review of the Consequences and Causes
Odessa Addison, Robin L. Marcus, Paul C. LaStayo, Alice S. Ryan
International Journal of Endocrinology.2014; 2014: 1. CrossRef - Relative Skeletal Muscle Mass Is Associated with Development of Metabolic Syndrome
Byung Sam Park, Ji Sung Yoon
Diabetes & Metabolism Journal.2013; 37(6): 458. CrossRef
- Intermuscular adipose tissue in metabolic disease
- ATP-Sensitive Potassium Channel-Deficient Mice Show Hyperphagia but Are Resistant to Obesity
- Yeul Bum Park, Yun Jung Choi, So Young Park, Jong Yeon Kim, Seong Ho Kim, Dae Kyu Song, Kyu Chang Won, Yong Woon Kim
- Diabetes Metab J. 2011;35(3):219-225. Published online June 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.3.219
- 3,539 View
- 31 Download
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The hypothalamus, the center for body weight regulation, can sense changes in blood glucose level based on ATP-sensitive potassium (KATP) channels in the hypothalamic neurons. We hypothesized that a lack of glucose sensing in the hypothalamus affects the regulations of appetite and body weight.
Methods To evaluate this hypothesis, the responses to glucose loading and high fat feeding for eight weeks were compared in Kir6.2 knock-out (KO) mice and control C57BL/6 mice, because Kir6.2 is a key component of the KATP channel.
Results The hypothalamic neuropeptide Y (NPY) analyzed one hour after glucose injection was suppressed in C57BL/6 mice, but not in Kir6.2 KO mice, suggesting a blunted hypothalamic response to glucose in Kir6.2 KO mice. The hypothalamic NPY expression at a fed state was elevated in Kir6.2 KO mice and was accompanied with hyperphagia. However, the retroperitoneal fat mass was markedly decreased in Kir6.2 KO mice compared to that in C57BL/6 mice. Moreover, the body weight and visceral fat following eight weeks of high fat feeding in Kir6.2 KO mice were not significantly different from those in control diet-fed Kir6.2 KO mice, while body weight and visceral fat mass were elevated due to high fat feeding in C57BL/6 mice.
Conclusion These results suggested that Kir6.2 KO mice showed a blunted hypothalamic response to glucose loading and elevated hypothalamic NPY expression accompanied with hyperphagia, while visceral fat mass was decreased, suggesting resistance to diet-induced obesity. Further study is needed to explain this phenomenon.
-
Citations
Citations to this article as recorded by- 17β-estradiol promotes acute refeeding in hungry mice via membrane-initiated ERα signaling
Kaifan Yu, Yanlin He, Ilirjana Hyseni, Zhou Pei, Yongjie Yang, Pingwen Xu, Xing Cai, Hesong Liu, Na Qu, Hailan Liu, Yang He, Meng Yu, Chen Liang, Tingting Yang, Julia Wang, Pierre Gourdy, Jean-Francois Arnal, Francoise Lenfant, Yong Xu, Chunmei Wang
Molecular Metabolism.2020; 42: 101053. CrossRef - Brain Glucose-Sensing Mechanism and Energy Homeostasis
A. J. López-Gambero, F. Martínez, K. Salazar, M. Cifuentes, F. Nualart
Molecular Neurobiology.2019; 56(2): 769. CrossRef - The involvement of purinergic signalling in obesity
Geoffrey Burnstock, Daniela Gentile
Purinergic Signalling.2018; 14(2): 97. CrossRef - High‐fat‐diet‐induced remission of diabetes in a subset of KATP‐GOF insulin‐secretory‐deficient mice
Zihan Yan, Zeenat A. Shyr, Manuela Fortunato, Alecia Welscher, Mariana Alisio, Michael Martino, Brian N. Finck, Hannah Conway, Maria S. Remedi
Diabetes, Obesity and Metabolism.2018; 20(11): 2574. CrossRef - Hypothalamic arcuate nucleus glucokinase regulates insulin secretion and glucose homeostasis
Yue Ma, Risheka Ratnasabapathy, Chioma Izzi‐Engbeaya, Marie‐Sophie Nguyen‐Tu, Errol Richardson, Sufyan Hussain, Ivan De Backer, Christopher Holton, Mariana Norton, Gaelle Carrat, Blanche Schwappach, Guy A. Rutter, Waljit S. Dhillo, James Gardiner
Diabetes, Obesity and Metabolism.2018; 20(9): 2246. CrossRef - Overexpression of WNK1 in POMC-expressing neurons reduces weigh gain via WNK4-mediated degradation of Kir6.2
Woo Young Chung, Jung Woo Han, Woon Heo, Min Goo Lee, Joo Young Kim
Molecular and Cellular Biochemistry.2018; 447(1-2): 165. CrossRef - Insights into the role of neuronal glucokinase
Ivan De Backer, Sufyan S. Hussain, Stephen R. Bloom, James V. Gardiner
American Journal of Physiology-Endocrinology and Metabolism.2016; 311(1): E42. CrossRef - Obesogenic and Diabetogenic Effects of High-Calorie Nutrition Require Adipocyte BK Channels
Julia Illison, Lijun Tian, Heather McClafferty, Martin Werno, Luke H. Chamberlain, Veronika Leiss, Antonia Sassmann, Stefan Offermanns, Peter Ruth, Michael J. Shipston, Robert Lukowski
Diabetes.2016; 65(12): 3621. CrossRef -
ABCC8 R1420H Loss-of-Function Variant in a Southwest American Indian Community: Association With Increased Birth Weight and Doubled Risk of Type 2 Diabetes
Leslie J. Baier, Yunhua Li Muller, Maria Sara Remedi, Michael Traurig, Paolo Piaggi, Gregory Wiessner, Ke Huang, Alyssa Stacy, Sayuko Kobes, Jonathan Krakoff, Peter H. Bennett, Robert G. Nelson, William C. Knowler, Robert L. Hanson, Colin G. Nichols, Clif
Diabetes.2015; 64(12): 4322. CrossRef - Glucokinase activity in the arcuate nucleus regulates glucose intake
Syed Hussain, Errol Richardson, Yue Ma, Christopher Holton, Ivan De Backer, Niki Buckley, Waljit Dhillo, Gavin Bewick, Shuai Zhang, David Carling, Steve Bloom, James Gardiner
Journal of Clinical Investigation.2015; 125(1): 337. CrossRef - Dissecting the Etiology of Type 2 Diabetes in the Pima Indian Population
Ewan R. Pearson
Diabetes.2015; 64(12): 3993. CrossRef - Ocular Hypotensive Effects of the ATP-Sensitive Potassium Channel Opener Cromakalim in Human and Murine Experimental Model Systems
Uttio Roy Chowdhury, Cindy K. Bahler, Bradley H. Holman, Peter I. Dosa, Michael P. Fautsch, Ted S Acott
PLOS ONE.2015; 10(11): e0141783. CrossRef - Differential gene expression pattern in hypothalamus of chickens during fasting-induced metabolic reprogramming: Functions of glucose and lipid metabolism in the feed intake of chickens
Xin-Ling Fang, Xiao-Tong Zhu, Sheng-Feng Chen, Zhi-Qi Zhang, Qing-Jie Zeng, Lin Deng, Jian-Long Peng, Jian-Jian Yu, Li-Na Wang, Song-Bo Wang, Ping Gao, Qing-Yan Jiang, Gang Shu
Poultry Science.2014; 93(11): 2841. CrossRef - Combined Treatment of Betulinic Acid, a PTP1B Inhibitor, with Orthosiphon stamineus Extract Decreases Body Weight in High-Fat–Fed Mice
Yoon-Jung Choi, So-Young Park, Jong-Yeon Kim, Kyu-Chang Won, Bo-Ra Kim, Jong-Keun Son, Seung-Ho Lee, Yong-Woon Kim
Journal of Medicinal Food.2013; 16(1): 2. CrossRef
- 17β-estradiol promotes acute refeeding in hungry mice via membrane-initiated ERα signaling
- The Effects of Resistance Training on Muscle and Body Fat Mass and Muscle Strength in Type 2 Diabetic Women
- Hwi Ryun Kwon, Kyung Ah Han, Yun Hyi Ku, Hee Jung Ahn, Bo-Kyung Koo, Ho Chul Kim, Kyung Wan Min
- Korean Diabetes J. 2010;34(2):101-110. Published online April 30, 2010
- DOI: https://doi.org/10.4093/kdj.2010.34.2.101
- 4,951 View
- 73 Download
- 55 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Our goal was to investigate the effects of low intensity resistance training on body fat, muscle mass and strength, cardiovascular fitness, and insulin sensitivity in type 2 diabetes.
Methods Twenty-eight overweight women with type 2 diabetes were randomly assigned to a resistance training group (RG,
n = 13) or a control group (CG,n = 15). RG performed resistance training using elastic bands, of which strength was equal to 40 to 50% of one repetition maximum (1RM), for three days per week. Each exercise consisted of three sets for 60 minutes. We assessed abdominal fat using computed tomography, muscle mass using dual-energy X-ray absorptiometry, and muscle strength using Keiser's chest and leg press. Insulin sensitivity was measured using the insulin tolerance test, and aerobic capacity was expressed as oxygen uptake at the anaerobic threshold (AT-VO2) before and after the 12-week exercise program.Results The age of participants was 56.4 ± 7.1 years, duration of diabetes was 5.9 ± 5.5 years, and BMI was 27.4 ± 2.5 kg/m2, without significant differences between two groups. During intervention, a greater increase in muscle mass and greater decreases in both total fat mass and abdominal fat were observed in RG compared to those of CG (
P = 0.015,P = 0.011,P = 0.010, respectively). Increase in 1RM of upper and lower extremities was observed in the RG (P = 0.004,P = 0.040, respectively), without changes in AT-VO2 and insulin resistance in either group.Conclusion In conclusion, the low intensity resistance training was effective in increasing muscle mass and strength and reducing total fat mass without change of insulin sensitivity in type 2 diabetic patients.
-
Citations
Citations to this article as recorded by- The Impact of Resistance Exercise Training on Glycemic Control Among Adults with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Yuwen Wan, Zhanguo Su
Biological Research For Nursing.2024;[Epub] CrossRef - Current trends in the development of soy-based foods containing probiotics and paving the path for soy-synbiotics
Minnu Sasi, Sandeep Kumar, Muzaffar Hasan, Arpitha S. R., Enriqueta Garcia-Gutierrez, Sweta Kumari, Om Prakash, Lata Nain, Archana Sachdev, Anil Dahuja
Critical Reviews in Food Science and Nutrition.2023; 63(29): 9995. CrossRef - Communication Strategies and Resources for Health and Fitness Professionals to Minimize Diabetes-Related Social Stigma
Lindsay J. Della, Annika Reitenga, Kristi M. King
ACSM'S Health & Fitness Journal.2023; 27(2): 54. CrossRef - IMPACTS OF MUSCLE TRAINING LOADS ON COLLEGE STUDENTS' PHYSICAL FITNESS
Wang Lu, Zheng Hua, Wang Tailin, Wei Xuanxi
Revista Brasileira de Medicina do Esporte.2023;[Epub] CrossRef - Effect of resistance training on HbA1c in adults with type 2 diabetes mellitus and the moderating effect of changes in muscular strength: a systematic review and meta-analysis
Anna K Jansson, Li X Chan, David R Lubans, Mitch J Duncan, Ronald C Plotnikoff
BMJ Open Diabetes Research & Care.2022; 10(2): e002595. CrossRef - Role of genetic factors (biology of telomeres) in cardiac rehabilitation
D. M. Aronov, O. M. Drapkina, M. G. Bubnova
Cardiovascular Therapy and Prevention.2022; 21(6): 3272. CrossRef - Effects of 12-Week Progressive Sandbag Exercise Training on Glycemic Control and Muscle Strength in Patients with Type 2 Diabetes Mellitus Combined with Possible Sarcopenia
Yu-Hsuan Chien, Chia-Jen Tsai, Dean-Chuan Wang, Pin-Hung Chuang, Hwai-Ting Lin
International Journal of Environmental Research and Public Health.2022; 19(22): 15009. CrossRef - Effects of Online Live Pilates Training during the COVID-19 Pandemic on Body Composition, Cardiovascular Function, and Physical Fitness in Sedentary Middle-aged Obese Women
Jung-Heon Choi, Ko-Eun Choi, Man-Gyoon Lee
Korean Journal of Sport Science.2022; 33(4): 521. CrossRef - Muscular Strength, Functional Fitness, Body Composition, and Quality of Life after 12 Weeks of Detraining in Older Females
Matúš Krčmár, Nora Halmová, Jaroslav Krajčovič, Bohumila Krčmárová
Physical & Occupational Therapy In Geriatrics.2021; 39(2): 129. CrossRef - Comparison between different types of exercise training in patients with type 2 diabetes mellitus: A systematic review and network metanalysis of randomized controlled trials
Edoardo Mannucci, Allegra Bonifazi, Matteo Monami
Nutrition, Metabolism and Cardiovascular Diseases.2021; 31(7): 1985. CrossRef - DETERMINING NEW ANTHROPOMETRIC MARKERS FOR SCREENING TYPE 2 DM IN A CARIBBEAN REGION.
Amruta Rajput, Upendra K Gupta, Guri Tzivion, Ravindrasingh Rajput
INTERNATIONAL JOURNAL OF SCIENTIFIC RESEARCH.2021; : 58. CrossRef - Effect of elastic band resistance training with green coffee extract supplementation on adiposity indices and TyG-related Indicators in Obese Women
Zahra Rashidi, Rezvan Beigi, Majid Mardaniyan Ghahfarrokhi, Mohammad Faramarzi, Ebrahim Banitalebi, Tina Jafari, Conrad P. Earnest, Julien S. Baker
Obesity Medicine.2021; 24: 100351. CrossRef - Effect of resistance training with and without caloric restriction on visceral fat: A systemic review and meta‐analysis
Mousa Khalafi, Abbas Malandish, Sara K. Rosenkranz, Ali A. Ravasi
Obesity Reviews.2021;[Epub] CrossRef - The Effect of Elastic Resistance Band Training on Postural Control and Body Composition in Sedentary Women
Yağmur KOCAOĞLU, Nurtekin ERKMEN
Spor Bilimleri Araştırmaları Dergisi.2021; 6(1): 233. CrossRef - Strength Training and Insulin Resistance: The Mediating Role of Body Composition
McKayla J. Niemann, Larry A. Tucker, Bruce W. Bailey, Lance E. Davidson
Journal of Diabetes Research.2020; 2020: 1. CrossRef - Beyond general resistance training. Hypertrophy versus muscular endurance training as therapeutic interventions in adults with type 2 diabetes mellitus: A systematic review and meta‐analysis
Pedro Acosta‐Manzano, María Rodriguez‐Ayllon, Francisco M. Acosta, David Niederseer, Josef Niebauer
Obesity Reviews.2020;[Epub] CrossRef - Resistance Exercise Intensity is Correlated with Attenuation of HbA1c and Insulin in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis
Yubo Liu, Weibing Ye, Qian Chen, Yong Zhang, Chia-Hua Kuo, Mallikarjuna Korivi
International Journal of Environmental Research and Public Health.2019; 16(1): 140. CrossRef - Effectiveness of Exercise Intervention in Reducing Body Weight and Glycosylated Hemoglobin Levels in Patients with Type 2 Diabetes Mellitus in Korea: A Systematic Review and Meta-Analysis
Ji-Eun Jang, Yongin Cho, Byung Wan Lee, Ein-Soon Shin, Sun Hee Lee
Diabetes & Metabolism Journal.2019; 43(3): 302. CrossRef - Effects of a moderate-to-high intensity resistance circuit training on fat mass, functional capacity, muscular strength, and quality of life in elderly: A randomized controlled trial
Pablo Jorge Marcos-Pardo, Francisco Javier Orquin-Castrillón, Gemma María Gea-García, Ruperto Menayo-Antúnez, Noelia González-Gálvez, Rodrigo Gomes de Souza Vale, Alejandro Martínez-Rodríguez
Scientific Reports.2019;[Epub] CrossRef - Effects of Resistance Exercise on Glycated Hemoglobin and Functional Performance in Older Patients with Comorbid Diabetes Mellitus and Knee Osteoarthritis: A Randomized Trial
Shu-Mei Chen, Feng-Chih Shen, Jung-Fu Chen, Wen-Dien Chang, Nai-Jen Chang
International Journal of Environmental Research and Public Health.2019; 17(1): 224. CrossRef - Effects of low‐intensity resistance training on muscular function and glycemic control in older adults with type 2 diabetes
Eri Takenami, ShinMin Iwamoto, Noriko Shiraishi, Akiko Kato, Yuichi Watanabe, Yoshifumi Yamada, Satoru Yamada, Naokata Ishii
Journal of Diabetes Investigation.2019; 10(2): 331. CrossRef - Effect of 12-Month Resistance Training on Changes in Abdominal Adipose Tissue and Metabolic Variables in Patients with Prediabetes: A Randomized Controlled Trial
Juan Yan, Xia Dai, Jitao Feng, Xiaodan Yuan, Jianing Li, Lihong Yang, Panpan Zuo, Zhaohui Fang, Chao Liu, Cunyi Hsue, Junya Zhu, Joshua D. Miller, Qingqing Lou
Journal of Diabetes Research.2019; 2019: 1. CrossRef - Positive Effects of a Short-Term Intense Elastic Resistance Training Program on Body Composition and Physical Functioning in Overweight Older Women
Nicole B. Fritz, Álvaro Juesas, Pedro Gargallo, Joaquín Calatayud, Julio Fernández-Garrido, Michael E. Rogers, Juan C. Colado
Biological Research For Nursing.2018; 20(3): 321. CrossRef - Protein timing during the day and its relevance for muscle strength and lean mass
Samuel L. Buckner, Jeremy P. Loenneke, Paul D. Loprinzi
Clinical Physiology and Functional Imaging.2018; 38(2): 332. CrossRef - Exercise training modalities in patients with type 2 diabetes mellitus: a systematic review and network meta-analysis
Bei Pan, Long Ge, Yang-qin Xun, Ya-jing Chen, Cai-yun Gao, Xue Han, Li-qian Zuo, Hou-qian Shan, Ke-hu Yang, Guo-wu Ding, Jin-hui Tian
International Journal of Behavioral Nutrition and Physical Activity.2018;[Epub] CrossRef - Resistance training reduces metabolic syndrome and inflammatory markers in older women: A randomized controlled trial
Crisieli M. Tomeleri, Mariana F. Souza, Roberto C. Burini, Cláudia R. Cavaglieri, Alex S. Ribeiro, Melissa Antunes, João P. Nunes, Danielle Venturini, Décio S. Barbosa, Luís B. Sardinha, Edilson S. Cyrino
Journal of Diabetes.2018; 10(4): 328. CrossRef - Effect of Resistance Training with Blood Flow Restriction on Follistatin to Myostatin Ratio, Body Composition and Anaerobic Power of Trained-Volleyball Players
Reza Bagheri, Amir Rashidlamir, Seyyed Reza Attarzadeh Hosseini
Medical Laboratory Journal.2018; 12(6): 28. CrossRef - Effects of 8-week kettlebell training on body composition, muscle strength, pulmonary function, and chronic low-grade inflammation in elderly women with sarcopenia
Hung-Ting Chen, Huey-June Wu, Yu-Jen Chen, Sung-Yen Ho, Yu-Chun Chung
Experimental Gerontology.2018; 112: 112. CrossRef - F inding the O ptimal volume and intensity of R esistance T raining E xercise for Type 2 Diabetes: The FORTE Study, a Randomized Trial
Pearl Yang, Walter Swardfager, Daniel Fernandes, Sheila Laredo, George Tomlinson, Paul I. Oh, Scott Thomas
Diabetes Research and Clinical Practice.2017; 130: 98. CrossRef - Exercise and ectopic fat in type 2 diabetes: A systematic review and meta-analysis
A. Sabag, K.L. Way, S.E. Keating, R.N. Sultana, H.T. O’Connor, M.K. Baker, V.H. Chuter, J. George, N.A. Johnson
Diabetes & Metabolism.2017; 43(3): 195. CrossRef - Resistance training to improve type 2 diabetes: working toward a prescription for the future
Dominik H. Pesta, Renata L. S. Goncalves, Anila K. Madiraju, Barbara Strasser, Lauren M. Sparks
Nutrition & Metabolism.2017;[Epub] CrossRef - Improvement of obesity-linked skeletal muscle insulin resistance by strength and endurance training
Sergio Di Meo, Susanna Iossa, Paola Venditti
Journal of Endocrinology.2017; 234(3): R159. CrossRef - Leisure time sedentary behavior, physical activity and frequency of protein consumption on lower extremity strength and lean mass
P D Loprinzi, J P Loenneke, D L Hamilton
European Journal of Clinical Nutrition.2017; 71(12): 1399. CrossRef - Strength Training Prevents Hyperinsulinemia, Insulin Resistance, and Inflammation Independent of Weight Loss in Fructose-Fed Animals
José D. Botezelli, Andressa Coope, Ana C. Ghezzi, Lucieli T. Cambri, Leandro P. Moura, Pedro P. M. Scariot, Rodrigo Stellzer Gaspar, Rania A. Mekary, Eduardo Rochete Ropelle, José Rodrigo Pauli
Scientific Reports.2016;[Epub] CrossRef - Effects of Elastic Band Resistance Training on Glucose Control, Body Composition, and Physical Function in Women With Short- vs. Long-Duration Type-2 Diabetes
Bong-Sup Park, Andy V. Khamoui, Lee E. Brown, Do-Youn Kim, Kyung-Ah Han, Kyung-Wan Min, Geun-Hee An
Journal of Strength and Conditioning Research.2016; 30(6): 1688. CrossRef - Neuromuscular dysfunction in type 2 diabetes: underlying mechanisms and effect of resistance training
Giorgio Orlando, Stefano Balducci, Ilenia Bazzucchi, Giuseppe Pugliese, Massimo Sacchetti
Diabetes/Metabolism Research and Reviews.2016; 32(1): 40. CrossRef - Physical exercises with free weights and elastic bands can improve body composition parameters in postmenopausal women
Simoni T. Bittar, Sergio S. Maeda, Marília M.S. Marone, Cláudio Santili
Menopause.2016; 23(4): 383. CrossRef - Effects of exercise training using resistance bands on glycaemic control and strength in type 2 diabetes mellitus: a meta-analysis of randomised controlled trials
Samantha K. McGinley, Marni J. Armstrong, Normand G. Boulé, Ronald J. Sigal
Acta Diabetologica.2015; 52(2): 221. CrossRef - Effect of exercise training on neuromuscular function of elbow flexors and knee extensors of type 2 diabetic patients
I. Bazzucchi, G. De Vito, F. Felici, S. Dewhurst, A. Sgadari, M. Sacchetti
Journal of Electromyography and Kinesiology.2015; 25(5): 815. CrossRef - Effects of short term elastic resistance training on muscle mass and strength in untrained older adults: a randomized clinical trial
Wagner Rodrigues Martins, Marisete Peralta Safons, Martim Bottaro, Juscelino Castro Blasczyk, Leonardo Rios Diniz, Romulo Maia Carlos Fonseca, Ana Clara Bonini-Rocha, Ricardo Jacó de Oliveira
BMC Geriatrics.2015;[Epub] CrossRef - Brain-derived neurotrophic factor correlated with muscle strength in subjects undergoing stationary bicycle exercise training
Sen-Wei Tsai, Yin-Ching Chan, Francois Liang, Chiann-Yi Hsu, I-Te Lee
Journal of Diabetes and its Complications.2015; 29(3): 367. CrossRef - Implementation of Resources to Support Patient Physical Activity through Diabetes Centres in Nova Scotia: The Effectiveness of Enhanced Support for Exercise Participation
Jonathon R. Fowles, Chris Shields, Lisette d’Entremont, Stephanie McQuaid, Brittany Barron, Peggy Dunbar
Canadian Journal of Diabetes.2014; 38(6): 423. CrossRef - Changes in insulin sensitivity in response to different modalities of exercise: a review of the evidence
S. Mann, C. Beedie, S. Balducci, S. Zanuso, J. Allgrove, F. Bertiato, A. Jimenez
Diabetes/Metabolism Research and Reviews.2014; 30(4): 257. CrossRef - The surprising influence of family history to type 2 diabetes on anaerobic performance of young male élite athletes
Antonino Bianco, Francesco Pomara, Antonino Patti, Ewan Thomas, Marco Petrucci, Marianna Bellafiore, Giuseppe Battaglia, Antonio Paoli, Antonio Palma
SpringerPlus.2014;[Epub] CrossRef - Skeletal muscle and organ masses differ in overweight adults with type 2 diabetes
Lance E. Davidson, David E. Kelley, Stanley Heshka, John Thornton, F. Xavier Pi-Sunyer, Lawrence Boxt, Ashok Balasubramanyam, Dympna Gallagher
Journal of Applied Physiology.2014; 117(4): 377. CrossRef - The effects of elastic band resistance training combined with blood flow restriction on strength, total bone‐free lean body mass and muscle thickness in postmenopausal women
Robert S. Thiebaud, Jeremy P. Loenneke, Christopher A. Fahs, Lindy M. Rossow, Daeyeol Kim, Takashi Abe, Mark A. Anderson, Kaelin C. Young, Debra A. Bemben, Michael G. Bemben
Clinical Physiology and Functional Imaging.2013; 33(5): 344. CrossRef - Predicting Aerobic Fitness Improvements after Participation in a Hybrid Supervised and Home-Based Exercise Program in People with Type 2 Diabetes
Pearl Yang, Paul Oh
Canadian Journal of Diabetes.2013; 37(6): 388. CrossRef - Impacto do treinamento resistido na força e hipertrofia muscular em HIV-soropositivos
Ciro José Brito, Edmar Lacerda Mendes, Aparecido Pimentel Ferreira, Sérgio Oliveira De Paula, Otávio de Tolêdo Nóbrega, Cláudio Córdova
Motriz: Revista de Educação Física.2013; 19(2): 313. CrossRef - Resistance Training for Diabetes Prevention and Therapy: Experimental Findings and Molecular Mechanisms
Barbara Strasser, Dominik Pesta
BioMed Research International.2013; 2013: 1. CrossRef - Resistance training, visceral obesity and inflammatory response: a review of the evidence
B. Strasser, M. Arvandi, U. Siebert
Obesity Reviews.2012; 13(7): 578. CrossRef - The effects of resistance training on ApoB/ApoA-I ratio, Lp(a) and inflammatory markers in patients with type 2 diabetes
Nikolaos P. E. Kadoglou, Grigorios Fotiadis, Zoi Athanasiadou, Ioulia Vitta, Stylianos Lampropoulos, Ioannis S. Vrabas
Endocrine.2012; 42(3): 561. CrossRef - A systematic review and meta‐analysis of the effect of aerobic vs. resistance exercise training on visceral fat
I. Ismail, S. E. Keating, M. K. Baker, N. A. Johnson
Obesity Reviews.2012; 13(1): 68. CrossRef - Aging, Resistance Training, and Diabetes Prevention
Kyle D. Flack, Kevin P. Davy, Matthew W. Hulver, Richard A. Winett, Madlyn I. Frisard, Brenda M. Davy
Journal of Aging Research.2011; 2011: 1. CrossRef - The Effects of Aerobic/Resistance Exercise on Body Fat Mass, Muscle Strength and Endothelial Function in Korean Type 2 Diabetes mellitus Patients
Kyung Wan Min
Journal of Korean Diabetes.2011; 12(1): 6. CrossRef - Exercise and Type 2 Diabetes
Sheri R. Colberg, Ronald J. Sigal, Bo Fernhall, Judith G. Regensteiner, Bryan J. Blissmer, Richard R. Rubin, Lisa Chasan-Taber, Ann L. Albright, Barry Braun
Diabetes Care.2010; 33(12): e147. CrossRef
- The Impact of Resistance Exercise Training on Glycemic Control Among Adults with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
- Effects of Aerobic Exercise on Abdominal Fat, Thigh Muscle Mass and Muscle Strength in Type 2 Diabetic Subject
- Hwi Ryun Kwon, Kyung Wan Min, Hee Jung Ahn, Hee Geum Seok, Bo Kyung Koo, Ho Chul Kim, Kyung Ah Han
- Korean Diabetes J. 2010;34(1):23-31. Published online February 28, 2010
- DOI: https://doi.org/10.4093/kdj.2010.34.1.23
- 3,647 View
- 43 Download
- 18 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Aerobic exercise can effectively reduce visceral fat. However, few studies have examined the effect of daily physical activity on obesity and cardiopulmonary function in the subjects with diabetes. We examined the effect of moderate intensity of walking in obese diabetes patients by monitoring of daily activity and measuring the change in abdominal fat area, muscle are and maximal muscle strength.
Methods We randomly assigned 27 obese women with type 2 diabetes to an aerobic exercise group (AG, n = 13) and control group (CG, n = 14). The AG performed moderate intensity walking for 60 minutes per exercise, 5 times per week, and for 12 weeks. The activity energy expenditure was monitored by a multi-record accelerometer. The CG maintained routine daily activities. At the time of the initiation of the study and after 12 weeks of exercise, the aerobic exercise capacity was assessed using oxygen consumption rate at anaerobic threshold (VO2-AT). The abdominal fat area and the quadriceps muscle area were measured by computed tomography, and the maximum muscle strength of the upper and lower limbs was measured by a chest press and a leg press, respectively.
Results The mean age of the study subjects was 56.6 ± 8.0 years, the mean duration of diabetes was 6.3 ± 6.0 years, and the body weight index (BMI) was 27.3 ± 2.7 kg/m2. The BMI of the AG was significantly decreased (
P = 0.003). In the AG, the visceral fat area and subcutaneous fat area were also significantly decreased (P = 0.018 andP < 0.001, respectively) but not in CG. VO2-AT of the AG was significantly improved, while that of the CG did not change (P = 0.009 andP = 0.115, respectively). The quadriceps muscle mass and the maximal muscle strength of the AG did not change, however, the CG showed a significant decrease. Duration of moderate intensity exercise was correlated with the decrease in total abdominal fat area (r = -0.484;P = 0.011) and that of high intensity exercise was correlated with improvement of cardiopulmonary function (r = 0.414;P = 0.032).Conclusion Daily moderate intensity aerobic exercise is effective at reducing abdominal fat mass, while high intensity exercise improves cardiopulmonary function.
-
Citations
Citations to this article as recorded by- Relationship Between Visceral Fat Tissue and Exercise
Ebru Ceviz
Türk Spor Bilimleri Dergisi.2024;[Epub] CrossRef - Walking for subjects with type 2 diabetes: a systematic review and joint AMD/SID/SISMES evidence-based practical guideline
P. Moghetti, S. Balducci, L. Guidetti, P. Mazzuca, E. Rossi, F. Schena, P. Moghetti, S. Balducci, L. Guidetti, F. Schena, P. Mazzuca, E. Rossi
Sport Sciences for Health.2021; 17(1): 1. CrossRef - Effect of exercise intervention dosage on reducing visceral adipose tissue: a systematic review and network meta-analysis of randomized controlled trials
Yu-Hsuan Chang, Hui-Ying Yang, Shiow-Ching Shun
International Journal of Obesity.2021; 45(5): 982. CrossRef - Comparison between different types of exercise training in patients with type 2 diabetes mellitus: A systematic review and network metanalysis of randomized controlled trials
Edoardo Mannucci, Allegra Bonifazi, Matteo Monami
Nutrition, Metabolism and Cardiovascular Diseases.2021; 31(7): 1985. CrossRef - The Therapeutic Effects of Mild to Moderate Intensity Aerobic Exercise on Glycemic Control in Patients with Type 2 Diabetes Mellitus: A Meta-Analysis of Randomized Trials
Siyao Gao, Jialing Tang, Guozhong Yi, Zhong Li, Zhenyin Chen, Ling Yu, Feng Zheng, Yajing Hu, Zhangui Tang
Diabetes Therapy.2021; 12(10): 2767. CrossRef - Walking for subjects with type 2 diabetes: A systematic review and joint AMD/SID/SISMES evidence-based practical guideline
P. Moghetti, S. Balducci, L. Guidetti, P. Mazzuca, E. Rossi, F. Schena
Nutrition, Metabolism and Cardiovascular Diseases.2020; 30(11): 1882. CrossRef - Effect of Coordinative Locomotor Training Program on Body Fat and Muscle mass of Male University students
Hyung chun Nam, Nam jeong Cho, Jae yong Choi
Archives of Orthopedic and Sports Physical Therapy.2019; 15(2): 109. CrossRef - Exercise training modalities in patients with type 2 diabetes mellitus: a systematic review and network meta-analysis
Bei Pan, Long Ge, Yang-qin Xun, Ya-jing Chen, Cai-yun Gao, Xue Han, Li-qian Zuo, Hou-qian Shan, Ke-hu Yang, Guo-wu Ding, Jin-hui Tian
International Journal of Behavioral Nutrition and Physical Activity.2018;[Epub] CrossRef - Exercise and ectopic fat in type 2 diabetes: A systematic review and meta-analysis
A. Sabag, K.L. Way, S.E. Keating, R.N. Sultana, H.T. O’Connor, M.K. Baker, V.H. Chuter, J. George, N.A. Johnson
Diabetes & Metabolism.2017; 43(3): 195. CrossRef - A systematic review and meta‐analysis on the effects of exercise training versus hypocaloric diet: distinct effects on body weight and visceral adipose tissue
R. J. H. M. Verheggen, M. F. H. Maessen, D. J. Green, A. R. M. M. Hermus, M. T. E. Hopman, D. H. T. Thijssen
Obesity Reviews.2016; 17(8): 664. CrossRef - Effects of Aerobic Exercise Associated with Abdominal Microcurrent: A Preliminary Study
Andreia Noites, Rita Nunes, Ana Isabel Gouveia, Alexandra Mota, Cristina Melo, Ágata Viera, Nuno Adubeiro, José Mesquita Bastos
The Journal of Alternative and Complementary Medicine.2015; 21(4): 229. CrossRef - Brain-derived neurotrophic factor correlated with muscle strength in subjects undergoing stationary bicycle exercise training
Sen-Wei Tsai, Yin-Ching Chan, Francois Liang, Chiann-Yi Hsu, I-Te Lee
Journal of Diabetes and its Complications.2015; 29(3): 367. CrossRef - Impact of Walking on Glycemic Control and Other Cardiovascular Risk Factors in Type 2 Diabetes: A Meta-Analysis
Shanhu Qiu, Xue Cai, Uwe Schumann, Martina Velders, Zilin Sun, Jürgen Michael Steinacker, Lamberto Manzoli
PLoS ONE.2014; 9(10): e109767. CrossRef - A systematic review and meta‐analysis of the effect of aerobic vs. resistance exercise training on visceral fat
I. Ismail, S. E. Keating, M. K. Baker, N. A. Johnson
Obesity Reviews.2012; 13(1): 68. CrossRef - The Effects of Regular Pilates Exercise on Blood pressure and Pulmonary Variables
Gyu-Chang Lee, Dong-Yeop Lee, Jae-Ho Yu
Journal of the Korea Academia-Industrial cooperation Society.2011; 12(7): 3088. CrossRef - The Effects of Aerobic/Resistance Exercise on Body Fat Mass, Muscle Strength and Endothelial Function in Korean Type 2 Diabetes mellitus Patients
Kyung Wan Min
Journal of Korean Diabetes.2011; 12(1): 6. CrossRef - The Evaluation of Workplace Obesity Intervention Program using Six Sigma Methodology
Ji Yeon Kang, Ill Keun Park, Yun Kyun Chang, Sook Hee Sung, Yoo Kyoung Park, Sang Woon Cho, Yun Mi Paek, Tae In Choi
The Korean Journal of Obesity.2011; 20(4): 193. CrossRef - How Can We Measure the Effects of Exercise in Daily Life?
Sang Yong Kim
Korean Diabetes Journal.2010; 34(1): 21. CrossRef
- Relationship Between Visceral Fat Tissue and Exercise
- The Effects of Low-Calorie Diets on Abdominal Visceral Fat, Muscle Mass, and Dietary Quality in Obese Type 2 Diabetic Subjects.
- Hee Jung Ahn, Youn Ok Cho, Hwi Ryun Kwon, Yun Hyi Ku, Bo Kyung Koo, Kyung Ah Han, Kyung Wan Min
- Korean Diabetes J. 2009;33(6):526-536. Published online December 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.6.526
- 2,397 View
- 36 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Weight loss through low-calorie diets (LCDs) decreases visceral fat (VF). However, the effects on muscle mass, changes of dietary quality, and insulin sensitivity are unknown for Korean obese type 2 diabetic subjects. Therefore, this study examined such effects of LCDs. METHODS: A total of 30 obese type 2 diabetic subjects (body mass index, 27.0 +/- 2.2 kg/m2) were randomly assigned to an LCD or control group. Subjects on LCDs took 500~1,000 kcal fewer energy than their usual dietary intake (1,000~1,500 kcal/day) over the course of 12 weeks. The abdominal VF and femoral muscle mass were evaluated by computed tomography, and insulin sensitivity was assessed using an insulin tolerance test (Kitt; rate constant for plasma glucose disappearance, %/min). Dietary nutrient intake consumed by subjects was assessed by 3-day food records. RESULTS: The percent VF reduction was -23.4 +/- 17.2% in the LCD group and -9.8 +/- 11.8% in the control group after 12 weeks (P < 0.001, P = 0.002). However, significant decrease in femoral mass or proportional change of marcronutrient intake and mean adequacy ratio were not found in the LCD group, as compared to the control group. Insulin sensitivity improved in the LCD group, as compared to the control group (P = 0.040). CONCLUSION: LCD effectively improved insulin sensitivity and reduced abdominal VF without reduction of femoral muscle and dietary quality in obese type 2 diabetic subjects. -
Citations
Citations to this article as recorded by- The association between measurement sites of visceral adipose tissue and cardiovascular risk factors after caloric restriction in obese Korean women
Hye-Ok Lee, Jung-Eun Yim, Jeong-Sook Lee, Young-Seol Kim, Ryowon Choue
Nutrition Research and Practice.2013; 7(1): 43. CrossRef - Effects of age on changes of body composition through caloric restriction in overweight and obese women
Jung-Eun Yim, Young-Seol Kim, Ryowon Choue
Journal of Nutrition and Health.2013; 46(5): 410. CrossRef - The effects of weight loss by a low-calorie diet and a low-calorie plus exercise in overweight undergraduate students
Gun-Ae Yoon, Hyun-Ho Ahn, Bo-Hae Park, Danbi Yoo, Sunmin Park
Korean Journal of Nutrition.2012; 45(4): 315. CrossRef - Effect of an abdominal obesity management program on dietary intake, stress index, and waist to hip ratio in abdominally obese women - Focus on comparison of the WHR decrease and WHR increase groups -
Ji Won Lee, Sook Young Yoo, So Young Yang, Hyesook Kim, Seong Kyung Cho
Korean Journal of Nutrition.2012; 45(2): 127. CrossRef - The Evaluation of Workplace Obesity Intervention Program using Six Sigma Methodology
Ji Yeon Kang, Ill Keun Park, Yun Kyun Chang, Sook Hee Sung, Yoo Kyoung Park, Sang Woon Cho, Yun Mi Paek, Tae In Choi
The Korean Journal of Obesity.2011; 20(4): 193. CrossRef - The Usefulness of an Accelerometer for Monitoring Total Energy Expenditure and Its Clinical Application for Predicting Body Weight Changes in Type 2 Diabetic Korean Women
Ji Yeon Jung, Kyung Ah Han, Hwi Ryun Kwon, Hee Jung Ahn, Jae Hyuk Lee, Kang Seo Park, Kyung Wan Min
Korean Diabetes Journal.2010; 34(6): 374. CrossRef - The Effects of Low-Calorie Diets on Abdominal Visceral Fat, Muscle Mass, and Dietary Quality in Obese Type 2 Diabetic Subjects (Korean Diabetes J 2009;33:526-36)
Won-Young Lee
Korean Diabetes Journal.2010; 34(1): 66. CrossRef
- The association between measurement sites of visceral adipose tissue and cardiovascular risk factors after caloric restriction in obese Korean women

 KDA
KDA
 First
First Prev
Prev





