Low Density Lipoprotein Cholesterol Target Goal Attainment Rate and Physician Perceptions about Target Goal Achievement in Korean Patients with Diabetes
Article information
Abstract
Background
This study aims to investigate the discrepancy between clinicians' perceptions and actual achievement rates of low density lipoprotein cholesterol (LDL-C) in Korean patients with diabetes according to updated American Diabetes Association (ADA)/American College of Cardiology Foundation (ACC) recommendations.
Methods
This is a multi-center, retrospective, non-interventional, observational study. Diabetic patients aged 18 years or older were eligible if they had been diagnosed with hypercholesterolemia or were receiving a lipid-lowering therapy between May 2010 and August 2010. The information was obtained by reviewing medical records and using a self-completed questionnaire to examine physician perceptions.
Results
A total of 2,591 subjects who satisfied the inclusion criteria were enrolled. Highest-risk and high-risk patients accounted for 61.9% and 38.1% of the patients, respectively. Although most (96.3%) underwent a statin monotherapy or a statin-based combination therapy, just 47.4% of patients attained the LDL-C target. However, the physicians' perceptions on target achievement rate (70.6%) were different from the actual results (47.4%). Many patients (65.3%) remained on the starting doses of statins, despite evidence of poor achievement of lipid goals.
Conclusion
Only less than half of patients with diabetes attained the LDL-C goal. The surveys showed that poor physician performance might be due to the lack of recognition on ADA/ACC consensus causing a low LDL-C target attainment rate. Therefore, changes in doctor perception are needed to attain target LDL-C level and reduce cardiovascular risk in Korean patients with diabetes.
INTRODUCTION
Cardiovascular disease (CVD) is the major cause of mortality and morbidity in patients with type 2 diabetes [1]. The increased risk of CVD in subjects with type 2 diabetes consists of multiple factors such as hypertension, smoking, albuminuria and hypercholesterolemia [2]. Among them, hypercholesterolemia is one of the key factors that are amenable to intervention.
A large body of research ranging from molecular to population studies indicates that elevated low density lipoprotein cholesterol (LDL-C) is a major predictor of CVD, including in populations with diabetes [3,4]. Treatments for lowering LDL-C below the target level recommended by several guidelines are emphasized in patients with type 2 diabetes due to the increased risk of CVD [5]. Patients with type 2 diabetes without a history of myocardial infarction are regarded to have the same risk of a coronary event as patients without diabetes who have a history of myocardial infarction [6]. This observation was part of the basis for the recommendation by the Adult Treatment Panel III (ATP III) of the National Cholesterol Education Program (NCEP) that diabetes should be considered a "coronary heart disease risk equivalent" and the resulting target for aggressive reduction of risk factors [7]. In line with this, recent guidelines from the American Diabetes Association (ADA) recommended the use of statins for primary prevention of CVD in type 2 diabetes patients [8]. Considering the results of previous study mentioned above [6], recent guidelines will provide good evidence on the quantitative relation between achieving target cholesterol concentration and the probability of cardiovascular events in subjects with diabetes [9].
In 2008, the ADA, in consensus with the American College of Cardiology Foundation (ACC), released guidelines [10] following the NCEP 2003 updated recommendations which included an "optional" LDL-C goal <70 mg/dL for patients who are at the "highest risk" for CVD [11]. Highest-risk patients were defined as 1) patients with CVD or 2) patients with diabetes plus one or more additional major CVD risk factors (smoking, hypertension, and family history of premature CVD). High-risk patients was defined as 1) patients who have diabetes but have no major cardiovascular risk factors and 2) patients who do not have diabetes or CVD but have more than two major cardiovascular risk factors. For these patients, the guidelines recommended a target LDL-C less than 100 mg/dL.
Despite available therapies and increased attention to hypercholesterolemia, many patients failed to achieve the LDL-C goals [12]. Data from the third U.S. National Health and Nutrition Examination Survey (NHANES;1988-1994) showed only 42% of patients with diabetes achieved an LDL-C <130 mg/dL [13]. More recent data with the NCEP 2004 updated recommendations demonstrated only 29.4% of very-high-risk patients with both diabetes and CVD reached the LDL-C goal of <70 mg/dL in the United States [14]. There is a need to better understand the reasons why most patients failed to reach these goals despite pharmacological treatment.
Unfortunately, it is uncertain whether target LDL-C level is commonly reached in Korean patients with diabetes. Therefore, we aimed to investigate the lipid target attainment rates according to the ADA and ACC consensus recommendation in Korean patients with diabetes and investigate physician perceptions on lipid target attainment and compared them with actual attainment rates.
METHODS
Subjects
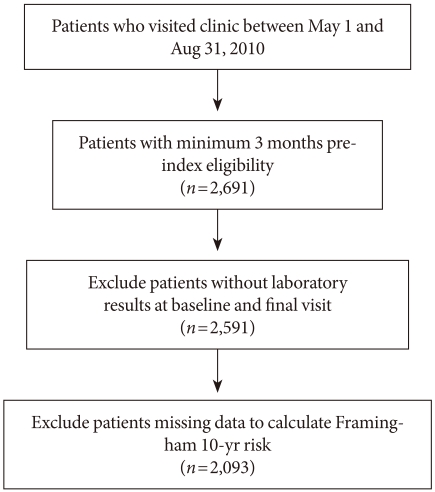
The study population consisted of 2,661 patients who were under the care of diabetic specialists at the 53 secondary and tertiary hospitals in Korea between 1 May 2010 and 31 August 2010 (Fig. 1). Patients were selected from the outpatient clinics of these hospitals with the following selection criteria: 1) type 2 diabetes according to ADA criteria, 2) at least 18 years of age, 3) newly diagnosed with hypercholesterolemia or previously diagnosed with hypercholesterolemia but not on lipid-lowering medication for at least one month prior to the initial visit, 4) on lipid-lowering treatment for at least 3 months. Hypercholesterolemia was defined according to NCEP-ATP III [15]. Patients were eligible for enrollment if they had visited the hospital at least once during the last 3 months. Detailed information on baseline characteristics including age, sex, body mass index (BMI), smoking status, the duration of diabetes, hypertension status, past history of CVD, family history of premature CVD and concomitant medication use was collected by study site personnel through review of medical records. Hypertension was defined as a systolic blood pressure (SBP) ≥140 mm Hg and/or diastolic BP (DBP) ≥90 mm Hg or taking antihypertensive medications. History of CVD was based on each subject's history of angina, myocardial infarction and/or cerebrovascular accidents. Smoking status was classified into non-smoker, ex-smoker and current smoker. The self-completed questionnaire on physicians' perceptions of the achievement rates of LDL-C targets was additively completed through an online survey.
We excluded subjects who met at least one of the following criteria: 1) current enrollment in other clinical studies, 2) participation in any clinical studies within the previous 90 days (except non-interventional and registry studies), 3) unable or unwilling to reveal medical records. After exclusion of ineligible subjects, 2,591 subjects (1,278 men, mean age 56.1±10.8; and 1,313 women, mean age 61.1±10.2) were included in this study.
Study design
This study was a multi-center, non-interventional study using retrospective medial chart reviews. Doctors provided detailed information on patient characteristics and their perception of LDL-C treatment goal achievement. All data were entered and collected in an eCRF, and the eCRF manual was provided separately to the investigator. This study was approved by the Institutional Review Board of the hospitals to which the participating investigators belonged.
Study variables
The values of LDL-C were determined by direct measurement when triglyceride (TG) was higher than 400 mg/dL or patients were on fibrates. Except those conditions, LDL-C was calculated from the Friedwald formula as following: Total cholesterol (TC)-[high density lipoprotein cholesterol (HDL-C)+TG/5]. These values were recorded using the web database. Laboratory records included the date of testing. The Framingham risk score modified by ATP III, which incorporated age, gender, LDL-C, HDL-C, BP, smoking status and TC, was used.
Use of lipid-lowering medication was determined by medical records. Patients were considered to be on a lipid lowering therapy if they had at least one subscription for any lipid-modifying medications during the follow-up period. Statin titration was defined as an increase in the strength of the dispensed statin. A switch was defined as a change of lipid drugs, either statin or non-statin.
Study Objectives
The objective of this study was to investigate the discrepancy between clinicians' perceptions and the actual achievement of LDL-C targets in Korean diabetic patients according to the updated ADA/ACC recommendations.
Statistical methods
Continuous variables are expressed as mean±standard deviation, and categorical variables are expressed as number and proportions (%). Most data are summarized with descriptive statistics. Student's t-tests or paired t-tests were used for continuous variables, and chi-squared tests were used for categorical variables. Multivariate logistic regression analysis was performed to identify the factors contributing to the failure of LDL-C target attainment. Significance was set at 0.05. All statistical analysis was performed using SPSS version 14.0 for Windows (SPSS Inc., Chicago, IL, USA).
RESULTS
Clinical and biochemical characteristics of the subjects
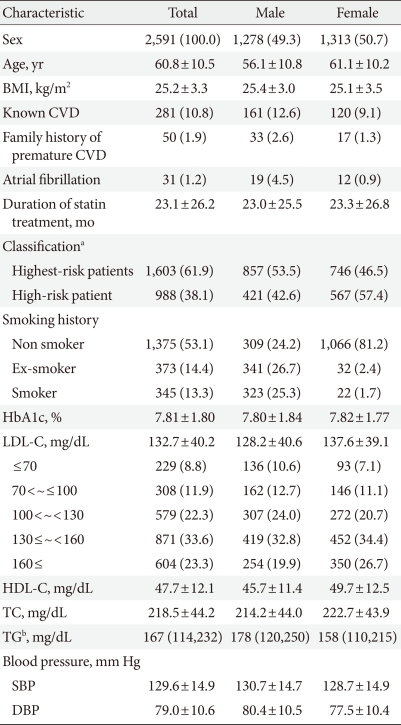
Baseline characteristics of study participants are presented in Table 1. The mean age of patients was 60.8±10.5 years. On average, the patients had a mean BMI of 25.2 kg/m2. Male subjects had a higher proportion of CVD and atrial fibrillation and were younger, more often at highest-risk, and current smokers (P<0.05 for each). Patients with previously diagnosed CVD compromised 10.8% of subjects.
Attainment of target LDL-C level
According to the 2008 ADA/ACC guidelines, 1,603 (61.9%) of the 2,591 patients were highest-risk and 988 (38.1%) were high-risk (Table 1). The mean observed duration of statin use was 23.1±26.2 months. The achievement rate of target LDL-C level (<70 mg/dL in the highest-risk group and <100 mg/dL in the high-risk group, respectively) was 8.8% at baseline. After treatment during the follow-up period, LDL-C target attainment increased up to 47.4% (Fig. 2). Among the high-risk patients (n=988), LDL-C goal attainment increased from 8.2% to 68.6%. For the highest-risk group (n=1,603), target LDL-C attainment increased from 9.2% to 34.2%.

Low density lipoprotein cholesterol target attainment rates according to the 2008 American Diabetes Association (ADA)/American College of Cardiology Foundation (ACC) consensus statement.
Further analyses of the proportion of patients achieving the goal were conducted according to sex. The percentage of patients reaching the LDL-C goal was similar between female (46.2%) and male patients (48.5%).
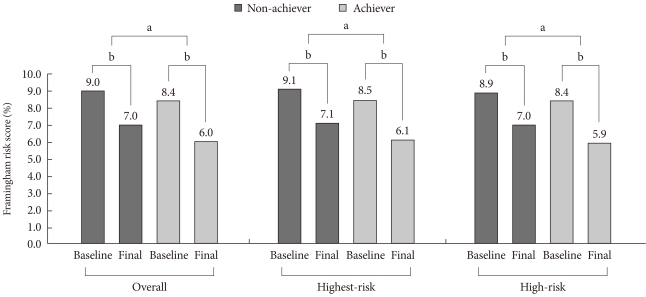
Regarding the reduction of risk for future CVD by decreased LDL-C level, Framingham risk score was significantly lower after using lipid-lowering drug at final visit compared to the baseline Framingham risk score, as shown in Fig. 3 (P<0.0001). When we compared the scores by stratifying the subjects who achieved the LDL-C target into high- and highest-risk groups, a significant difference was observed in the both group at the initial visit and the final visit (8.5±3.3 vs. 6.1±3.2, P<0.0001 in the highest risk patients; 8.4±3.2 vs. 5.9±3.2, P<0.001 in the high risk patients). Furthermore, goal-achievers at final visit had significant reduction of Framingham risk score at the final visit compared to non-achievers (P<0.05).
Physician treatment strategies and factors affecting LDL-C goal attainment
In general, 65.3% of patients did not switch drugs between baseline and the final visit (Fig. 4A). Increased titration was prescribed in only 3.2% of patients, while 4.0% were prescribed decreased titration. Among 3-hydroxy-3-methyl-CoA reductase (HMG-CoA reductase) inhibitors, rosuvastatin was the most frequently used one (48.8%). Fibrates were being taken by 6.9% of patients at the initial visit and were newly subscribed to 3.4% of patients during the follow-up period.
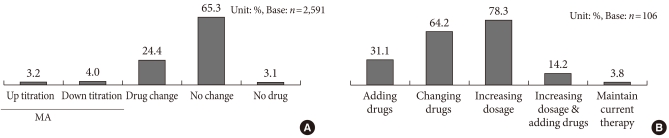
Physician treatment strategies to achieve target goals analyzed (A) by chart review, (B) by physicians' answers to a survey. MA, multiple answers.
To identify the factors affecting LDL-C goal attainment, we compared the baseline characteristics between target LDL-C achievers and non-achievers regarding to sex, age, BMI, HbA1c, LDL-C, HDL-C, TC, smoking history and blood pressure. The results showed that patients who did not attain the LDL-C goal were more likely to be current smokers, have a family history of premature CVD, hypertension, lower HDL-C level, and higher LDL-C level (P<0.05 each). A logistic regression analysis was performed with these variables, which showed that subjects with older patients, patients with higher baseline LDL-C and current smokers tended to fail to achieve target LDL-C level. When we analyzed the factors in high-risk and highest-risk group separately, age, smoking, and higher baseline LDL-C level were the significant factors affecting LDL-C target attainment in the high-risk group, while age and smoking history were those in the highest-risk group (P<0.05, respectively). The effects of non-statins, statin titration, and switching between lipid-lowering drugs on goal achievement were not analyzed. The average treatment doses were not statistically different between groups.
Physician perceptions of LDL-C goal achievement
To analyze the possible factors contributing to the low target goal attainment rate (47.4% overall, Fig. 2), physicians completed a self-reporting survey. As shown in Fig. 5, we found that physician perceptions of target LDL-C achievement differed from the guidelines. Of those who were initially tested for LDL-C after diagnosis of diabetes, a majority (83.2%) were classified as high-risk by the physicians, while only 14.8% were classified as highest-risk. After treatment, while 70.6% were perceived to have achieved the target LDL-C by physicians, only 47.4% achieved the goal according to the ADA/ACC guidelines.
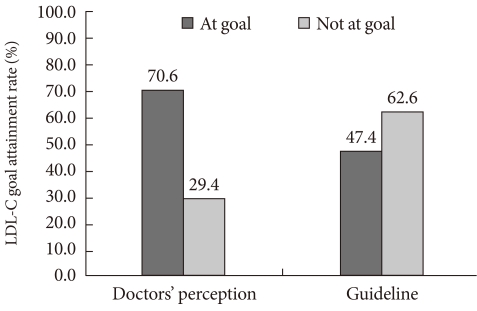
The discrepancy between physicians' perception of low density lipoprotein cholesterol (LDL-C) goal attainment and actual results according to the 2008 American Diabetes Association (ADA)/American College of Cardiology Foundation (ACC) guidelines.
For the diagnosis of hypercholesterolemia, physicians considered the following lipid levels most important (in descending order): LDL-C (92.5%), TG (46.2%), HDL-C (38.7%), and TC (57.5%). From the survey, doctors reported that 96.2% used guidelines for setting target cholesterol level. The guidelines commonly used are shown in Fig. 6, with the NCEP ATP III guidelines being the most frequent.
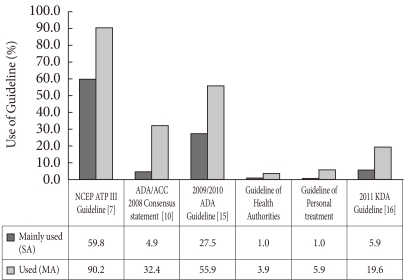
Patterns of physicians' adherence to guideline. NCEP, National Cholesterol Education Program; ATP III, Adult Treatment Panel III; ADA, American Diabetes Association; ACC, American College of Cardiology Foundation; KDA, Korean Diabetes Association; MA, multiple answers; SA, single answers.
Ninety-eight percent of physicians reported that they informed patients of their cholesterol value, and most (86.8%) also informed patients of their LDL-C level. Regular follow-ups on cholesterol level were completed every 6 months in 56.6% of cases, every 3 months in 25.5%, and once a year in 13.2%. When the target goal was not achieved, physicians replied that they would increase dosage (78.3%) or change medication (64.2%) (Fig. 4B). However, increased titration was carried out in only 3.2% of patients (Fig. 4A).
DISCUSSION
In this study, the ADA/ACC recommended LDL-C goal was achieved in approximately 47.4% of Korean patients with diabetes, which was significantly lower than physicians' perceptions (70.6%). Compared to those who did not reach the target LDL-C level, the risk of future coronary heart disease (CHD) was substantially lower among those who did achieve the goal, as shown in the reduction of the Framingham risk score.
This study also demonstrated that there was a large gap between physicians' perceptions and guidelines in categorizing the severity of hypercholesterolemia. Although most physicians answered that they would increase the dosage of lipid-lowering medications if the target LDL-C goal was not reached, only 3.2% prescribed increased titration (Fig. 4A). Although factors affecting physicians' recognition were not analyzed, inferring by the fact that most patients were considered high-risk but not highest-risk to physicians, the updated guidelines might not be fully recognized.
During the treatment period, 65.3% of patients did not have any drug adjustment, including up-titration, add-on, or drug switching (Fig. 4A). Factors such as old age, multi-drug usage, and adverse effects of up-titration or combination therapy might have affected physician decisions. Also, the guidelines used by the physicians may have affected LDL-C level. From the survey, NCEP APT III guidelines [7] (59.8%) were the most frequently used. The 2009/2010 ADA guidelines [8] (27.5%), ADA/ACC consensus statement (4.9%), and Korean Diabetes Association (KDA) guidelines [16] (5.9%) were applied less frequently.
A few studies have evaluated the attainability of the more aggressive LDL-C treatment goal recommended by the NCEP ATPIII or ADA guidelines [14,17]. Kennedy et al. [14] reported that it would be extremely difficult to reach an LDL-C goal of <70 mg/dL in patients with diabetes and CVD in the United States. They estimated that 25% of patients would require more than two lipid-lowering drugs at maximal doses to attain this goal [14]. In a recent survey of 4,888 patients treated with statins, only 38% reached the recommended LDL-C level according to the NCEP guidelines [12]. Although our study was conducted ten years later and used the ADA/ACC guidelines, our findings were consistent with the results of above studies.
It has been suggested that if LDL-C goals are not met, it is necessary to take patient opinions about their illness into account. A prospective survey in Australia using prescription renewals as a surrogate for drug discontinuation found that 60% of patients stopped their medication after 1 year, and half of them discontinued within 3 months of therapy initiation. A major reason for discontinuation was lack of self-perception regarding the need for further treatment [18]. However, when patients were compliant, there were many possible pitfalls underlying patient non-achievement with current treatment goals such as inappropriate drug or dose selection, limited drug efficacy. Failure to achieve target LDL-C level was in large part due to inadequate doses or titration by physicians. Most patients who began treatment with a statin remained at the initial dose [19,20].
In other studies [19,21], patients with diabetes had the lowest success rate in the treatment with lipid lowering drugs. However, subjects with diabetes are known to be at a substantially higher risk for stroke [22], CHD, and death [5]. Moreover, diabetics with [23] or without [24] established CHD benefit from statin treatment in a manner equal to or greater than that of nondiabetic subjects [20,21]. A subgroup analysis of the Greek Atorvastatin and Coronary Heart Disease Evaluation (GREACE) study which compared structured care and usual care in clinical practice in Greece [23] found that diabetic patients showed early reductions of more than 50% in total mortality, coronary mortality, coronary morbidity, and stroke in the structured care arm. The Collaborative Atorvastatin Diabetes Study (CARDS) showed that, over a 3-year period, a daily 10 mg dose of atorvastatin reduced the risk of a major cardiovascular event in patients with type 2 diabetes mellitus without incident CHD by 37% and that of stroke by almost half (48%) [24]. In our study population, 10.8% of subjects had previous CVD, and a majority (61.9%) was classified as at highest-risk. Although the current treatment gap in LDL-C targets is comparable with published international data, this gap is unacceptable, and undoubtedly leads to an excess number of cardiovascular deaths, infarcts, strokes and need for revascularization. To improve the management of hypercholesterolemia, physicians should be aware of and focus on patients with diabetes. A recent randomized controlled trial demonstrated the incremental impact of team-based care approach to cholesterol management in patients with diabetes [25]. Although primary study outcome was set as achieving LDL-C level of 100 mg/dL regardless of CVD risk, it showed that physician-paramedical staff approach can be considered to improve LDL-C goal attainment.
A major strength of this study was the large sample size; nearly 2,600 patients were included in the main analysis. Another advantage is the inclusion of a survey concerning physician perceptions in the diagnosis of hypercholesteroelemia and treatment strategy. However, this study had several limitations. The diagnosis of CVD used to classify patients into high-risk and highest-risk categories was based on a chart review. Thus, misclassification of LDL-C severity and outcome may have occurred. Also, we did not have detailed dietary information for the patients and therefore could not estimate the effects of dietary intervention on LDL-C level [26]. Another limitation was that the study population did not reflect patients with diabetes who were receiving primary care. Finally, the sex-specific Framingham CHD predictions have not been validated in Koreans. The Framingham prediction was first demonstrated in Caucasians and was later applied to Japanese-Americans and other ethnic groups after recalibration for differing prevalence of risk factors [27]. However, no validation or recalibration has been carried out in Koreans. Furthermore, our study was able to measure the effect of statins over only a short-term period. In many instances, statin treatment had been ongoing for a long period of time. Additionally, patient compliance with the lipid-modifying drugs was not monitored.
In conclusion, this study showed that actual LDL-C target attainment rates according to the ADA/ACC consensus statement were low in Korean patients with diabetes. However, more than 70% of physicians perceived their patients to have achieved these goals. Thus, our results suggested that changes in clinical practices and physician perceptions might be needed to reach cholesterol target goals recommended by updated guidelines.
ACKNOWLEDGMENTS
This study was funded by AstraZeneca Korea.
Notes
No potential conflict of interest relevant to this article was reported.