Lipoproteins and β-Cell Functions: From Basic to Clinical Data
Article information
Cholesterol loading to β-cells was shown to increase neuronal nitric oxide synthase (NOS) dimerization, which decreases glucokinase activity [1] and also inhibits glucose-stimulated phosphatidylinositol 4,5-bisphosphate hydrolysis and the closure of KATP channels [2]. Thus, islets exposed to physiologic levels of low density lipoprotein (LDL) show a decrease in glucose-stimulated insulin secretion in a LDL receptor-dependent manner [2,3]. LDL-cholesterol (LDL-C) concentrations as low as 0.8 and 1 mM can inhibit the proliferation of islet cells by 50% to 70% [3]. This inhibition of cultured islets proliferation occurs in β-cells independently of LDL receptor [3]. In addition to the adverse effects on insulin secretion and proliferation, LDL has a negative impact on β-cell survival when it is modified or present at very high concentrations [3,4,5]. Oxidized LDL induces the JNK pathway and the subsequent activation of AP1, thereby leading to impaired insulin synthesis and increased apoptosis [4]. Very low density lipoprotein (VLDL)-mediated apoptosis of β-cells is also associated with an increase in JNK activity [5].
Considering the above-mentioned negative effects of LDL on β-cell functions, cholesterol seems to be very bad for β-cells. However, not only cellular cholesterol content, but also a delicate balance of cholesterol concentrations between different subcellular compartments needs to be finely tuned for optimal β-cell functionality [6]. ATP-binding cassette transporter G1 (ABCG1) plays an important role in the enrichment of insulin secretory granules with cholesterol and the partitioning of cholesterol between different cellular compartments rather than for cholesterol efflux from the β-cells [7,8] while ABCA1 mediates the efflux of cholesterol and phospholipids to an extracellular apolipoprotein acceptor. Mice with ABCA1 deficiency in β-cells have characteristic phenotypes including cholesterol accumulation in islet, normal plasma cholesterol levels, markedly impaired glucose tolerance (IGT), and defective insulin secretion, without influencing insulin sensitivity [9]. On hyperglycemic clamp study, the first phase insulin secretion rate was shown to be significantly lower in Tangier heterogygotes with loss-of-function mutations in ABCA1 than in control subjects [10]. The lack of β-cell ABCA1 results in impaired depolarization-induced exocytotic fusion of insulin granules, disturbances in membrane microdomain organization, and alteration in Golgi and insulin granule morphology, suggesting that elevated islet cholesterol accumulation directly impairs granule fusion and insulin secretion [6].
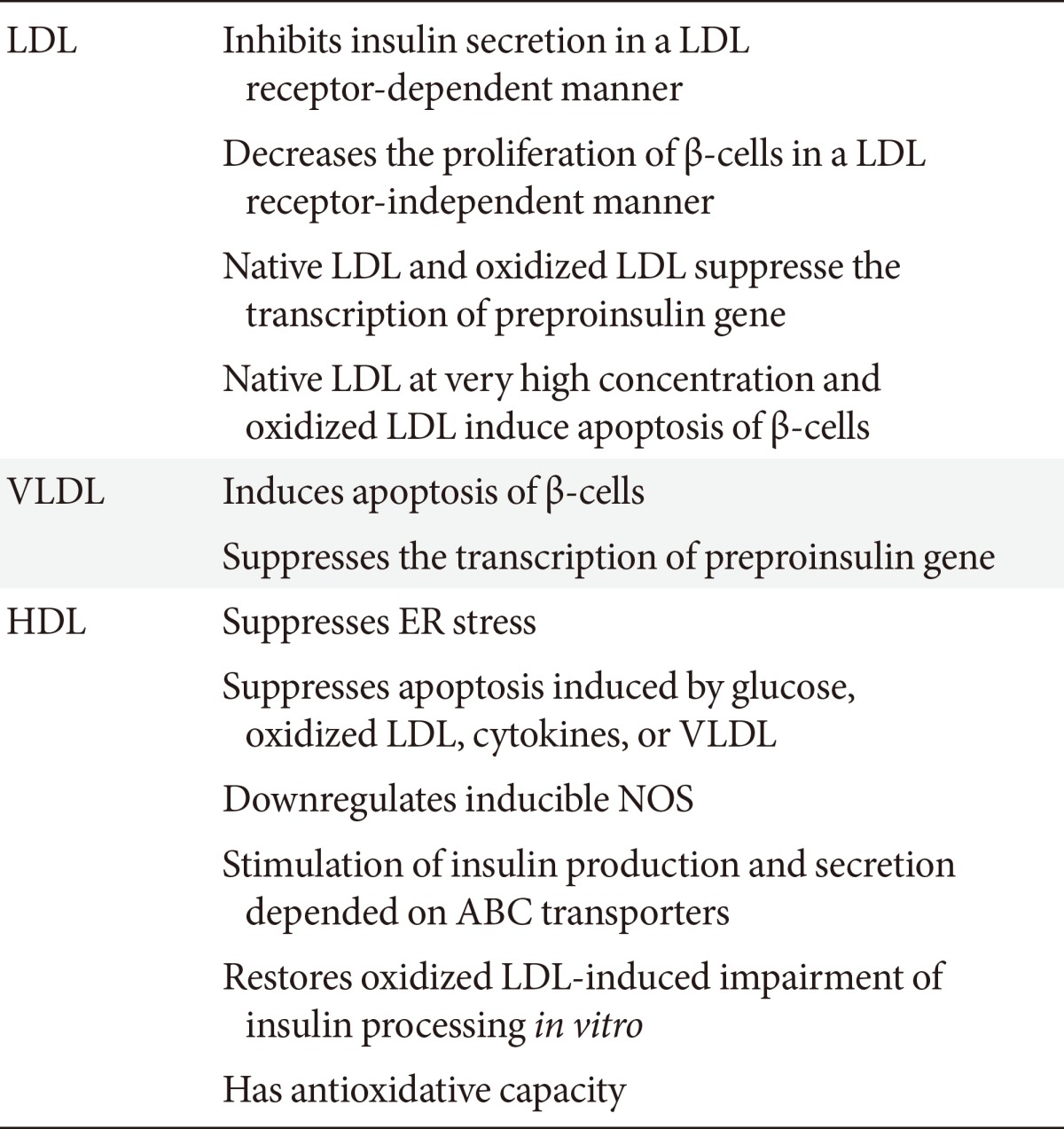
Physiologic levels of high density lipoprotein (HDL) protein may or may not increase basal and glucose-stimulated insulin secretion from β-cells, depending on experimental conditions [3,6]. HDL protects β-cells from endoplasmic reticulum stress, basal apoptosis, and apoptosis induced by various stressful conditions, including glucose, cytokines, VLDL, and oxidized LDL [3,6,11]. Inducible NOS is expressed in β-cells and mediate the proapoptotic effect of glucose and cytokines, but its basal and stimulated expression in islets is suppressed by HDL [3]. Furthermore, the downstream target of activated inducible NOS, namely the death receptor Fas, is downregulated by HDL, whereas antiapoptotic Fas-associated death domain-like interleukin (IL)-1β converting enzyme inhibitory protein is upregulated [3]. Interestingly, in addition to HDL, both apolipoprotein A1 (ApoA1) and sphingsine-1-phosphate, a bioactive sphingolipid carried by HDL, protect β-cells from IL-1β and glucose-induced apoptosis [3]. And, HDL protects β-cells from oxidized LDL-induced loss of insulin expression and death [4]. VLDL also increases the levels of activated cleaved caspase-3 and induces apoptosis in β-cells and the activation of caspase-3 is antagonized by HDL particles (Table 1) [5]. The β-cell protective concentrations of HDL are around 1 mM HDL-cholesterol (HDL-C) in most cases [6]. Whether higher concentrations of HDL and/or ApoA-I than those levels seen in usual clinical situations are required for further protective effects on β-cells is not known, although lipid-free recombinant of ApoA-I, ApoA-II, or discoidal reconstituted HDLs were shown to increase both basal and glucose-stimulated insulin secretion in a dose-dependent manner [12].
A low level of HDL-C is not only a well-known cardiovascular risk factor [13], but it is also known to be an independent risk factor for the development of type 2 diabetes [14,15]. In line with the relationship between HDL and diabetes, Drew et al. [16] reported that the infusion of reconstituted HDL consisting of ApoA-I and phosphatidylcholine into diabetic patients caused a significant increase in plasma insulin level as well as a decrease in plasma glucose levels without a significant change of insulin sensitivity.
In an analysis of the participants in the Fenofibrate Intervention and Event Lowering in Diabetes trial, lower levels of HDL-C and HDL-C/apoA-I ratio at baseline could predict the progression to pharmacologic glucose control among those initially treated with lifestyle measures alone [17]. The effect of HDL-C/apoA-I on the progression persisted after adjustment for multiple metabolic and lifestyle factors, including homeostatic model assessment of insulin resistance (HOMA-IR) and triglycerides (TGs) [17]. Recently, the Prevention of Renal and Cardiovascular End-Stage Disease study, a population-based prospective cohort study, showed that both HDL-C and HDL-C/apoA-I were inversely associated with the development of type 2 diabetes independent of TG levels or HOMA-IR [14].
Elevations in plasma TG concentrations are frequently associated with diabetes [18]. However, lipoprotein lipase (LPL)-deficient subjects with hypertriglyceridemia were reported to display an enhanced glucose-stimulated insulin response as well as lower blood glucose levels [19]. In addition, in the same study, a long-term follow-up over 17 years of a patient with a homozygous LPL-deficiency revealed that this patient's glucose and plasma insulin levels did not change, despite the fact that she continued to have high levels of free fatty acid and TG [19]. This study suggests that hypertriglyceridemia alone may not be detrimental to β-cells.
In this issue, Shimodaira et al. [20] investigated the association between serum TG and HDL-C levels, and TG/HDL-C ratio and early-phase insulin secretion in normoglycemic and prediabetic subjects in Japan, and showed that early insulin secretion responses to oral glucose challenge were correlated with HDL-C levels in subjects with prediabetes, but not in subjects with normal glucose tolerance. When early insulin secretory responses were normalized by accounting for insulin sensitivity, these correlations remained significant even after adjusting for multiple confounding factors. However, the negative correlations between the log-transformed TG and TG/HDL-C levels and early insulinogenic indices were maintained consistently only in a specific group of subjects with prediabetes (in those with IGT, but neither in those with impaired fasting glucose [IFG] nor in those with both IGT and IFG). These findings strongly suggest that HDL does not prevent the impairment of glucose homeostasis, but protects β-cells from further damage mediated by the pathophysiologic stresses of impaired glucose homeostasis. Although the study did not account for cytokines and inflammatory markers, and some subgroups with prediabetes were not large enough, considering the consistent positive correlations between HDL-C and early insulin secretion in subjects with prediabetes, clinical implications from these results is that the metabolically beneficial roles of HDL may be very delicate and may not be easily discernible in some clinical situations, including prediabetes and metabolic syndrome. HDL has been shown to be a very heterogeneous class of lipoproteins that contains more than 80 bioactive proteins and even more lipid species [6].
Thus, the metabolic roles of HDL are still mysterious. Further studies are required for the elucidation of the roles of lipoproteins in the modulations of β-cell functions. Also, the questions of which levels of HDL-C and/or ApoA-I must be achieved with what treatment modality need to be addressed in future studies. Such studies will give us a clue to overcome the challenges to the current lipid therapies, including diabetogenic effects of statin, implication of fibrate therapy, recent failure of niacin clinical trials, and the development of cholesteryl ester transfer protein inhibitor and ApoA-I mimetics.
Notes
No potential conflict of interest relevant to this article was reported.