
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 38(3); 2014 > Article
-
Original ArticleClinical Care/Education Factors Associated with Health-Related Quality of Life among Saudi Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Survey
- Ayman A. Al Hayek, Asirvatham A. Robert, Abdulghani Al Saeed, Aus A. Alzaid, Fahad S. Al Sabaan
-
Diabetes & Metabolism Journal 2014;38(3):220-229.
DOI: https://doi.org/10.4093/dmj.2014.38.3.220
Published online: June 17, 2014
Department of Endocrinology and Diabetes, Diabetes Treatment Center, Prince Sultan Military Medical City, Riyadh, Saudi Arabia.
- Corresponding author: Ayman A. Al Hayek. Department of Endocrinology and Diabetes, Diabetes Education Unit, Diabetes Treatment Center, Prince Sultan Military Medical City, P.O. Box 7897, Riyadh 11159, Saudi Arabia. ayman.alhayek@yahoo.com
Copyright © 2014 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- Diabetes mellitus (DM) is associated with high mortality, morbidity, poor general health, and loss of health-related quality of life (HRQOL). The objective of the study was to assess the factors associated with HRQOL among patients with type 2 diabetes mellitus (T2DM).
-
Methods
- This was a cross sectional study conducted among 283 T2DM patients during June 2011 and September 2012 at a major tertiary hospital in Riyadh, Saudi Arabia. The respondents were purposively and conveniently selected according to their availability during their routine visit to the outpatient clinics and they were interviewed using the Arabic version of the Short-Form 36-item survey (SF-36) to assess the HRQOL.
-
Results
- The mean age of the participants was 56.4±13.2 years. Around 63% (178) were males and 37% (105) were females. Glycosylated hemoglobin level was found to be significantly higher among female and HRQOL was higher among male. Respondents who were more than 50 years old had poor HRQOL than less than 50 years age group. Poor economic status, reported diabetic complications and longer duration of diabetes were significantly associated with poor HRQOL. The respondents treated with combination of therapies (oral medication plus insulin) indicated better HRQOL than patients with insulin therapy alone. Multivariate analysis indicated that gender, economic status (except subscale energy), and complications of DM (except subscale energy) as independent risk factor for HRQOL.
-
Conclusion
- Gender, economic status, and complication of DM were independent risk factors for majority of the subscales of HRQOL.
- The World Health Organization (WHO) and International Diabetes Federation (IDF) have projected that the number of diabetes cases will increase to 366 million by 2030, an increase of 214% compared to the year 2006 [1]. Diabetes mellitus (DM) is associated with multiple medical complications that decrease the health-related quality of life (HRQOL) and contribute to suboptimal physical and mental functioning and earlier mortality [2,3]. Coronary heart disease, depression, and unhealthy eating habits have significant negative effects on quality of life (QOL) of DM patients [2,4,5].
- The IDF reported that five of the top 10 countries with the highest prevalence rates of diabetes in the world are situated within the Gulf region including Saudi Arabia [6]. There has been a changing pattern of lifestyle among the Saudi population towards urbanization and dietary habits [7]. The chronic consumption of high energy, high fat diets, and low levels of physical activity lead to changes in energy balance with conservation of energy stored as fat. Such excess energy consumption per se promotes insulin resistance even before significant weight gain occurs [7]. The WHO projects a 3-fold increase in the number of people with DM from 890,000 in 2000 to 2,523,000 in 2030 in Saudi Arabia [8].
- HRQOL refers to the physical, psychological, and social domains of health that are influenced by a person's experiences, beliefs, expectations, and perceptions; therefore, health care providers should strive to understand the physical, emotional, and social impacts of chronic disease such as DM [9]. In order to improve the day-to-day functions and HRQOL, patient-centered knowledge can be incorporated into chronic disease treatment strategies that may lead to lesser office visits, hospitalizations and reduced health care costs [10]. Studies have shown that HRQOL among diabetics are much lower than those reported among nondiabetics [4,11].
- There are multifactorial reasons for lower QOL among diabetics. Diabetics are more likely to be older, overweight, less likely to exercise, and more likely to have comorbidities such as hypertension, coronary artery disease, hypercholesterolemia [12]; and are more likely to have complications such as retinopathy, nephropathy, painful polyneuropathy, upper gastrointestinal symptoms, impotence, amputations, symptomatic hyperglycemia, and hypoglycemia [4]. Lower health related QOL scores are associated with all these aspects. In addition, the cost of managing diabetic patients is twice as costly as managing nondiabetic patients, mainly due to the high costs associated with management of diabetic complications [13]. The objective of the present study was to assess the factors associated with HRQOL among patients with type 2 diabetes mellitus (T2DM).
INTRODUCTION
- This was a cross sectional study conducted among 283 type 2 diabetic patients at a major tertiary hospital, Riyadh, Saudi Arabia between June 2011 and September 2012. The respondents were purposively and conveniently selected according to their availability during their routine visit to the outpatient clinics. Inclusion criteria were: age range of 18 to 70 years; diabetes identified as type 2; diabetes diagnosed ≥1 year and Saudi national. Patients who had history of psychopathology, medical instability, visual, hearing, or cognitive impairment, type 1 diabetes, and gestational diabetics were excluded from the study. The demographic and the history of the DM were also collected.
- Definitions of demographic variables and measurements
- The patients were classified as poor if their monthly income was ≤5,000 Saudi Arabian Riyal (SAR), monthly income SAR >5,000 to 10,000 were classified as middle and monthly income SAR >10,000 were considered as high income group.
- Diabetes related complications including diabetic nephropathy, diabetic neuropathy, retinopathy, diabetic cardiomyopathy, coronary artery disease, peripheral vascular disease, and stroke detail were collected. Diabetic nephropathy was diagnosed by the nephrologists (the presence of microalbuminuria which defined as, the presence of microalbuminuria ≥30 to 299 mg/24 hours urine collection sample or the presence of macro albuminuria ≥300 mg/24 hours urine collection sample) was obtained from the patient's record. Diabetic neuropathies are heterogeneous, affecting different parts of the nervous system that present with diverse clinical manifestations. They may be focal or diffuse. Retinopathy was defined according to the American Academy of Ophthalmology. Patients were classified into nonproliferative diabetic retinopathy and proliferative diabetic retinopathy.
- Blood pressure was measured using a standardized sphygmomanometer. A trained nurse performed the procedure while the subject was in a sitting position, with the arm at the level of the heart and after 5 minutes rest. Hypertension was defined as elevated systolic (≥140 mm Hg) or diastolic (≥90 mm Hg) blood pressure. Glycosylated hemoglobin (HbA1c) was analyzed using high-performance liquid chromatography method (Bio-Rad, Hercules, CA, USA).
- The definition of control of lipid profile components used in this study is according to National Cholesterol Educational Program Adult Treatment Panel III and American Diabetes Association recommendations. Family history DM was defined as the presence of DM in first-degree relatives.
- HADS
- The anxiety and depression symptom's measurements were assessed for the patients using hospital anxiety and depression scale (HADS), Arabic version [14]. This scale is very simple and easy to use by most people with no major language problems, and has no cultural or psychological sensitive questions. In addition, it is known to have very high validity and reliability.
- The HADS consists of seven items for anxiety (HADS-A) and seven for depression (HADS-D). The items were scored on a 4-point scale from 0 (not present) to 3 (considerable). The item scores are added, giving subscale scores on the HADS-anxiety and the HADS-depression from 0 to 21 [14].
- SF-36
- Patients were interviewed using the Arabic version of the Short-Form 36-item survey (SF-36) to assess the HRQOL. Interviews were conducted in a separate room in order to maintain privacy and confidentiality. It was revealed that there were no significant mean differences between Arabic and English SF-36 questionnaires in Saudi Cultures [15]. The SF-36 includes eight health concepts: physical functioning, bodily pain, role limitations due to physical health problems, role limitations due to personal or emotional problems, emotional well-being, social functioning, energy/fatigue, and general health perceptions. It also includes a single item that provides an indication of perceived change in health. These 36 items were adapted from longer instruments completed by patients participating in the Medical Outcomes Study, an observational study of variations in physician practice styles and patient outcomes in different systems of health care delivery [16]. Subscale scores are calculated according to standard procedures, yielding score values of 0 to 100, where higher scores indicate better HRQOL. Questionnaires for illiterate subjects were filled in the presence of two witnesses.
- The SF-36 Health Survey items and scales were constructed using the Likert method of summated ratings. Answers to each questions were scored (some items need to be recoded). These scores were then summed to produce raw scale scores for each health concept which were then transformed to a 0 to 100 scale with higher scores indicating better functioning, well-being, and state of health. Reliability and validity of the SF-36 have been demonstrated for both type 1 diabetes patients and type 2 diabetes patients.
- Statistical analysis
- Data analysis was carried out using Microsoft Excel 2002 (Microsoft Corp., Seattle, WA, USA) and SPSS version 16 (SPSS Inc., Chicago, IL, USA). In addition to the descriptive analysis t-test, one way analysis of variance, and Tukey post hoc tests were conducted to look at differences carried out for making comparisons among test groups. Multivariate linear regression analysis was done to understand the variables associated with HRQOL. P value of <0.05 was considered to be statistically significant.
METHODS
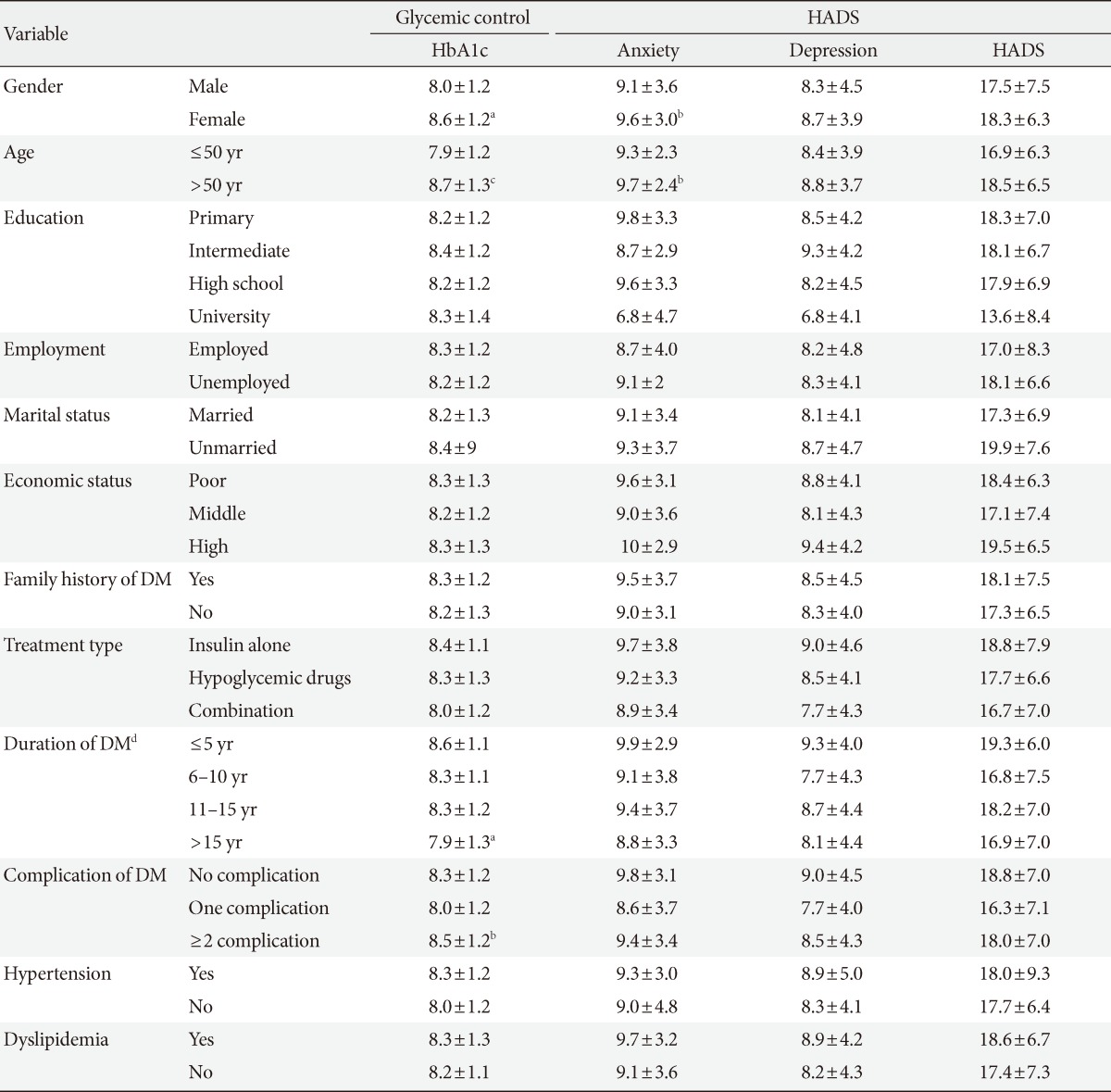
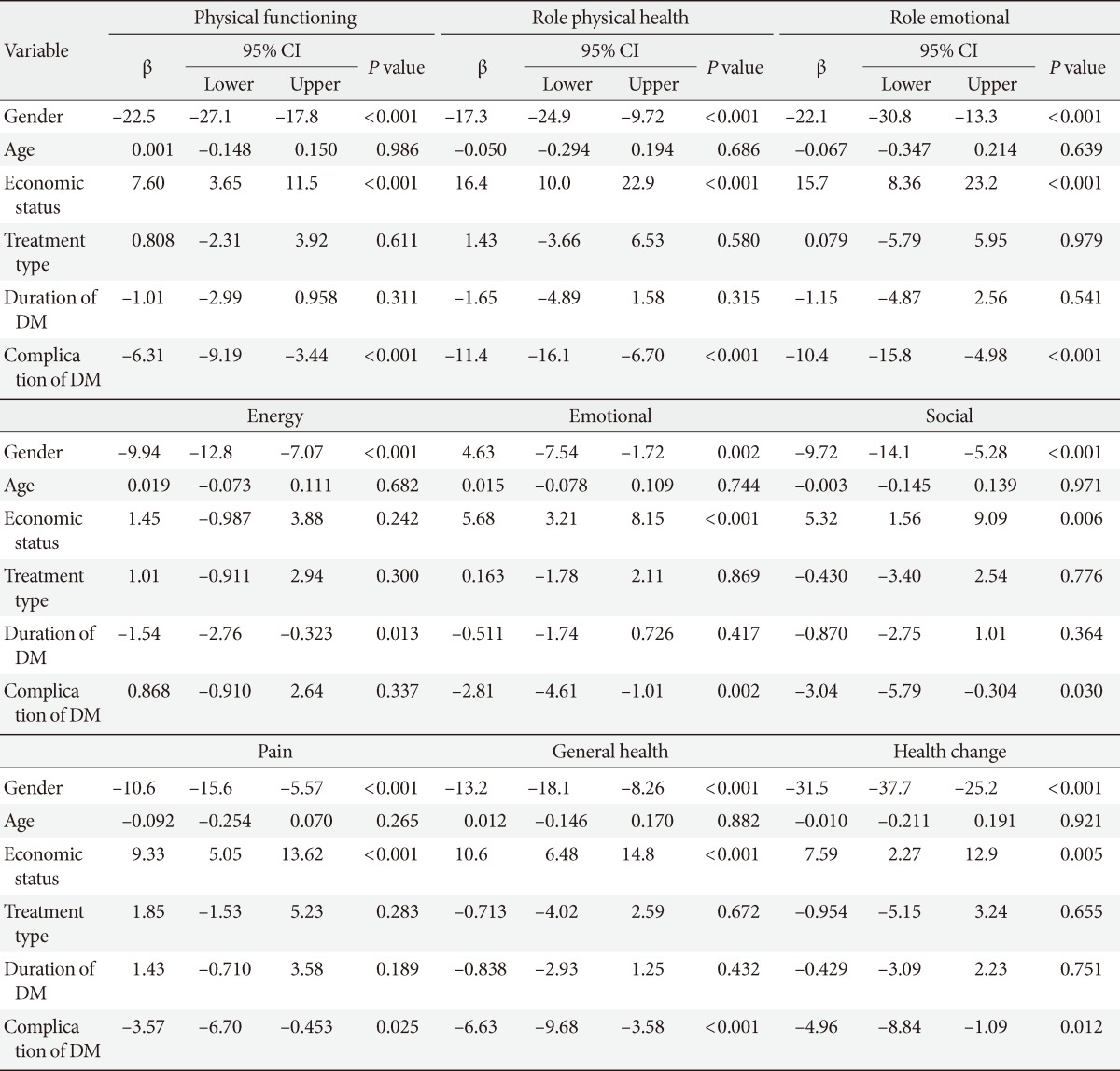
- The demographic data (gender, age, marital status, level of education, income, and employment) are presented in Table 1. The mean age of the study participants was 56.4±13.2 years. One hundred and seventy-eight were males (62.9%) and 105 were females (37.1%). The mean duration of diagnosis of DM was 11.8±8.4 years. Table 2 presents the levels of glycemic control, anxiety, and depression of the study population. Compared to male, female had significantly higher HbA1c (P<0.01) and anxiety level (P<0.05). Likewise, the group with over 50 years of age had significantly higher HbA1c (P<0.001) and anxiety level (P<0.05) than ≤50 years of age group. Also, significant differences were found on HbA1c level of prolonged duration DM patients (P<0.01) and patients with ≥2 complication of DM (P<0.05) compared to ≤5 years duration of DM and DM patients without any complication respectively. Table 3 presents the scores of the SF-36 domains/subscales among the type 2 diabetic subjects. The HRQOL was found to be significantly lower among female on subscale physical functioning, role emotional, energy, emotional, social, and pain than to their counterpart. The group with over 50 years of age also showed significantly lower HRQOL on subscale, physical functioning (P<0.001), role of emotional (P<0.01), and energy (P<0.001) than the group with under 50 years of age. When compared to those with poor economic status, patients with middle and high economic status had significantly higher HRQOL in all subscales (P<0.05). However, there was no significant difference found between middle and high economic status patients (P>0.05). Table 4 shows the scores of SF-36 domains/subscales among type 2 diabetic subjects which are presented based on diabetes complication and associated diseases. Compared to patients who used insulin alone, patient treated with combination of treatments i.e., insulin+hypogly-cemic drug showed significantly higher HRQOL on all the subscales (P<0.05) except pain (P>0.05). However, no significant difference was observed between patients who had hypoglycemic drug and combination of treatments other than physical functioning. The patients who reported having DM for longer duration (>15 years) had significantly higher risk of subscale, physical functioning, role of physical health, role emotional, general health, and health change. When compared to diabetic patients with no complication, patients ≥2 complication had significantly higher risk of subscale, physical functioning, role of physical health, role emotional, energy, emotional, social, pain, general health, and health change. Significant differences were also observed in patients with ≥2 complication on all subscales of HRQOL except energy when compared to patients with one complication. Table 5 demonstrates the results of regression analyses with β-coefficient and 95% confidence interval for SF-36 dimensions adjusted for significant confounders gender, age, economic status, treatment type, duration of DM, and complication of DM. Gender, economic status (except subscale energy) and complications of DM (except subscale energy) were the independent risk factor for HRQOL.
RESULTS
- The prevalence of DM is steadily increasing in Saudi Arabia due to population growth, aging, urbanization, increasing prevalence of obesity and physical inactivity. HRQOL refers to the physical, psychological, and social domains of health that are influenced by a person's experiences, beliefs, expectations, and perceptions [8]. According to the previous study, poor glycemic control is reported among more than half of Saudi populations with T2DM [17].
- Patients with T2DM were generally found to be overweight, obese, sedentary, and frequently found to be hypertensive. It is, therefore, suggested that patients need to pay attention to their weight by participating in weight reduction programmes and improving their physical activity levels to reduce the risk of developing the complications associated with type 2 diabetes [11]. A comprehensive approach that include, diabetes education, life style modification, good glycemic control, minimization of cardiovascular risk, avoidance of drugs that can aggravate glucose or lipid metabolism, and screening for diabetes complications are essential for the management of patients with T2DM. QOL can also be improved by delaying the advancement of diabetes complications through a comprehensive diabetes management [18].
- Over the past decade, differences between men and women with T2DM have been intensively investigated, revealing that the women with diabetes appeared to have worse HRQOL and mental well-being than the men with diabetes [13,19]. The present study also reported that female with diabetes appeared to have worse HRQOL and mental well-being than their counterpart. The multivariate analysis indicated gender as independent risk factor of HRQOL. Therefore, identifying strategies to improve self-rated health and HRQOL among diabetic patients, especially among Saudi women, is of great importance.
- Age has been another parameter which has an effect on the HRQOL of diabetic patients [20]. Hanninen et al. [21] reported that age has no effect on diabetic patient's HRQOL; however, another study reported that patients who are less than 40 years of age have significantly better QOL than other age groups [22]. The present study found a negative correlation between age and HRQOL. In addition, it is understood that men and women with diabetes face different challenges in the management of their condition [23].
- Low socioeconomic status and patients with a high school education or less had a strong negative impact on HRQOL of diabetes patients especially in the younger age group [24,25]. The present study also found that patients with a low economic status and high school education or less had at least one poor HRQOL outcome. However, multivariate linear regression analysis indicated only economic status as independent risk factor for HRQOL in diabetes patients.
- Many studies reported an association between increased duration of diabetes and poor HRQOL, in both types of diabetes [26,27]. On the other hand, there are also contradicting findings about the association between duration of diabetes and HRQOL. In this present study we found a negative association between diabetes duration and HRQOL. The longer duration of diabetes is associated with the poor HRQOL.
- Studies reported that insulin treatment was one of the important factors associated with HRQOL. Insulin-treated diabetic patients reported reduced impact on HRQOL than tablets/diet-treated patients [28,29]. This study also observed a significantly better HRQOL among insulin treated patients than oral hypoglycemic drugs treated patients. In addition, the combination of insulin and oral hypoglycemic drugs treated patients had better HRQOL than those treated with insulin alone. However, multivariate analysis indicated no significant association between type of type of treatment and HRQOL.
- Diabetes patients are more susceptible to macro or microangiopathic complications, such as myocardial infarction, stroke, and peripheral arterial occlusive disease than those without T2DM. Literature also suggested a link between diabetic microvascular complications such as retinopathy, nephropathy, and neuropathy, and cardiovascular diseases. There is now extensive evidence that microalbuminuria, a marker of nephropathy, is also a strong predictor of total and cardiovascular mortality in patients with T2DM [11,30]. The American Diabetic Association has estimated that 75% to 80% of adult diabetic patients will ultimately die as a result of macrovascular complications due to their underlying disease [31]. The incidence of diabetic complications has been shown to have a significant impact on QOL in a number of studies [32]. The long-term complications, particularly microvascular disease, have been directly related to poor glycemic control [33]. As many patients are likely to remain undiagnosed for several years before symptoms appear, many will show evidence of diabetic complications at diagnosis [34,35]. The present study indicated a significantly lower HRQOL among patients with diabetes complication than the patients with diabetes alone. Further, multivariate analysis indicated complication of DM as an independent risk factor for all subscales of SF36 except energy.
- In conclusion, the result of this study indicates a significant association between DM and HRQOL. Gender, economic status, diabetes treatment type and complication of DM were independent risk factors for majority of the subscales of HRQOL. Understanding the effect of diabetes on QOL is important for day-to-day clinical management and also for public health policy initiatives in order to improve the QOL and health outcomes of those with diabetes.
DISCUSSION
- 1. Agarwal S, Raman R, Paul PG, Rani PK, Uthra S, Gayathree R, McCarty C, Kumaramanickavel G, Sharma T. Sankara nethralaya-diabetic retinopathy epidemiology and molecular genetic study (SN-DREAMS 1): study design and research methodology. Ophthalmic Epidemiol 2005;12:143-153. ArticlePubMed
- 2. Cong JY, Zhao Y, Xu QY, Zhong CD, Xing QL. Health-related quality of life among Tianjin Chinese patients with type 2 diabetes: a cross-sectional survey. Nurs Health Sci 2012;14:528-534. ArticlePubMed
- 3. Scollan-Koliopoulos M, Bleich D, Rapp KJ, Wong P, Hofmann CJ, Raghuwanshi M. Health-related quality of life, disease severity, and anticipated trajectory of diabetes. Diabetes Educ 2013;39:83-91. ArticlePubMedPDF
- 4. Daniele TM, Bruin VM, Oliveira DS, Pompeu CM, Forti AC. Associations among physical activity, comorbidities, depressive symptoms and health-related quality of life in type 2 diabetes. Arq Bras Endocrinol Metabol 2013;57:44-50. ArticlePubMed
- 5. Egede LE, Hernandez-Tejada MA. Effect of comorbid depression on quality of life in adults with type 2 diabetes. Expert Rev Pharmacoecon Outcomes Res 2013;13:83-91. ArticlePubMed
- 6. Alzaid A. Diabetes: a tale of two cultures. Br J Diabetes Vasc Dis 2012;12:57.ArticlePDF
- 7. Al-Hayek AA, Robert AA, Alzaid AA, Nusair HM, Zbaidi NS, Al-Eithan MH, Sam AE. Association between diabetes self-care, medication adherence, anxiety, depression, and glycemic control in type 2 diabetes. Saudi Med J 2012;33:681-683. PubMed
- 8. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004;27:1047-1053. ArticlePubMedPDF
- 9. Camacho F, Anderson RT, Bell RA, Goff DC Jr, Duren-Winfield V, Doss DD, Balkrishnan R. Investigating correlates of health related quality of life in a low-income sample of patients with diabetes. Qual Life Res 2002;11:783-796. PubMed
- 10. Genovese S, Tedeschi D. Effects of vildagliptin/metformin therapy on patient-reported outcomes: work productivity, patient satisfaction, and resource utilization. Adv Ther 2013;30:152-164. ArticlePubMed
- 11. Oguntibeju OO, Odunaiya N, Oladipo B, Truter EJ. Health behaviour and quality of life of patients with type 2 diabetes attending selected hospitals in south western Nigeria. West Indian Med J 2012;61:619-626. PubMed
- 12. Myers VH, McVay MA, Brashear MM, Johannsen NM, Swift DL, Kramer K, Harris MN, Johnson WD, Earnest CP, Church TS. Exercise training and quality of life in individuals with type 2 diabetes: a randomized controlled trial. Diabetes Care 2013;36:1884-1890. PubMedPMC
- 13. Mikailiukstiene A, Juozulynas A, Narkauskaite L, Zagminas K, Salyga J, Stukas R. Quality of life in relation to social and disease factors in patients with type 2 diabetes in Lithuania. Med Sci Monit 2013;19:165-174. ArticlePubMedPMC
- 14. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-370. ArticlePubMed
- 15. Al Abdulmohsin SA, Coons S, Draugalis JR, Hays RD. Translation of the RAND 36-item health survey 1.0 (aka SF-36) into Arabic. Santa Monica: Rand; 1997.
- 16. Hays RD, Shapiro MF. An overview of generic health-related quality of life measures for HIV research. Qual Life Res 1992;1:91-97. ArticlePubMedPDF
- 17. Al-Nuaim AR, Mirdad S, Al-Rubeaan K, Al-Mazrou Y, Al-Attas O, Al-Daghari N. Pattern and factors associated with glycemic control of Saudi diabetic patients. Ann Saudi Med 1998;18:109-112. ArticlePubMed
- 18. Imam K. Management and treatment of diabetes mellitus. Adv Exp Med Biol 2012;771:356-380. ArticlePubMed
- 19. Unden AL, Elofsson S, Andreasson A, Hillered E, Eriksson I, Brismar K. Gender differences in self-rated health, quality of life, quality of care, and metabolic control in patients with diabetes. Gend Med 2008;5:162-180. ArticlePubMed
- 20. Song SH. Emerging type 2 diabetes in young adults. Adv Exp Med Biol 2012;771:51-61. ArticlePubMed
- 21. Hanninen J, Takala J, Keinanen-Kiukaanniemi S. Quality of life in NIDDM patients assessed with the SF-20 questionnaire. Diabetes Res Clin Pract 1998;42:17-27. ArticlePubMed
- 22. Al-Maskari MY, Al-Shookri AO, Al-Adawi SH, Lin KG. Assessment of quality of life in patients with type 2 diabetes mellitus in Oman. Saudi Med J 2011;32:1285-1290. PubMed
- 23. Grant JF, Hicks N, Taylor AW, Chittleborough CR, Phillips PJ. North West Adelaide Health Study Team. Gender-specific epidemiology of diabetes: a representative cross-sectional study. Int J Equity Health 2009;8:6ArticlePubMedPMC
- 24. Eljedi A, Mikolajczyk RT, Kraemer A, Laaser U. Health-related quality of life in diabetic patients and controls without diabetes in refugee camps in the Gaza strip: a cross-sectional study. BMC Public Health 2006;6:268ArticlePubMedPMCPDF
- 25. Wubben DP, Porterfield D. Health-related quality of life among North Carolina adults with diabetes mellitus. N C Med J 2005;66:179-185. ArticlePubMed
- 26. Glasgow RE, Ruggiero L, Eakin EG, Dryfoos J, Chobanian L. Quality of life and associated characteristics in a large national sample of adults with diabetes. Diabetes Care 1997;20:562-567. ArticlePubMedPDF
- 27. Redekop WK, Koopmanschap MA, Stolk RP, Rutten GE, Wolffenbuttel BH, Niessen LW. Health-related quality of life and treatment satisfaction in Dutch patients with type 2 diabetes. Diabetes Care 2002;25:458-463. ArticlePubMedPDF
- 28. Bradley C, Todd C, Gorton T, Symonds E, Martin A, Plowright R. The development of an individualized questionnaire measure of perceived impact of diabetes on quality of life: the ADDQoL. Qual Life Res 1999;8:79-91. ArticlePubMed
- 29. Holmanova E, Ziakova K. Audit diabetes-dependent quality of life questionnaire: usefulness in diabetes self-management education in the Slovak population. J Clin Nurs 2009;18:1276-1286. ArticlePubMed
- 30. Dinneen SF, Gerstein HC. The association of microalbuminuria and mortality in non-insulin-dependent diabetes mellitus. A systematic overview of the literature. Arch Intern Med 1997;157:1413-1418. ArticlePubMed
- 31. American Diabetes Association. Detection and management of lipid disorders in diabetes. Diabetes Care 1993;16:828-834. ArticlePubMedPDF
- 32. Lloyd A, Sawyer W, Hopkinson P. Impact of long-term complications on quality of life in patients with type 2 diabetes not using insulin. Value Health 2001;4:392-400. ArticlePubMed
- 33. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837-853. ArticlePubMed
- 34. UK Prospective Diabetes Study 6. Complications in newly diagnosed type 2 diabetic patients and their association with different clinical and biochemical risk factors. Diabetes Res 1990;13:1-11. PubMed
- 35. Harris MI, Klein R, Welborn TA, Knuiman MW. Onset of NIDDM occurs at least 4-7 yr before clinical diagnosis. Diabetes Care 1992;15:815-819. ArticlePubMedPDF
REFERENCES

Values are presented as mean±standard deviation (t-test, one way analysis of variance, and Tukey post hoc test).
DM, diabetes mellitus; HTN, hypertension.
aP<0.05, bP<0.001, cP<0.01, d≤5 years vs. >15 years, eNo complication vs. ≥2 complications, fP<0.001, gP<0.05, hP<0.01, one complication vs. ≥2 complication.
Figure & Data
References
Citations

- Quality of life, stress, anxiety and depression and associated factors among people with type 2 diabetes mellitus in Western region Saudi Arabia
Shahad Abduljalil Abualhamael, Mukhtiar Baig, Waleed Alghamdi, Zohair Jamil Gazzaz, Majid Al-Hayani, Abdulrahman Bazi
Frontiers in Psychiatry.2024;[Epub] CrossRef - Health-Related Quality of Life of Adolescents and Children With Type 1 Diabetes in the Jazan Region of Saudi Arabia
Gassem A Gohal, Aqilah Majhali, Esaam Moafa, Sarah H Talebi, Bushra I Maashi, Amani Mutaen, Walaa J Alhamdan, Ibrahim M Dighriri
Cureus.2024;[Epub] CrossRef - Health-Related Quality of Life Among Type 2 Diabetes Mellitus Patients Using the 36-Item Short Form Health Survey (SF-36) in Central Ethiopia: A Multicenter Study
Habtamu Esubalew, Ayele Belachew, Yimer Seid, Habtamu Wondmagegn, Kidus Temesgen, Tsegazeab Ayele
Diabetes, Metabolic Syndrome and Obesity.2024; Volume 17: 1039. CrossRef - Health-related quality of life and its determinants among patients with diabetes mellitus: a multicentre cross-sectional study in Northwest Ethiopia
Ashenafi Kibret Sendekie, Ephrem Mebratu Dagnew, Bereket Bahiru Tefera, Eyayaw Ashete Belachew
BMJ Open.2023; 13(1): e068518. CrossRef - Illness Perception and Coping Strategies on the Perceived Quality of Life in Adults with Coronary Heart Diseases: A Model Evaluation
Maedeh Bagheri, Mohammadnaghi Farahani, Hamidreza Hasanabadi, Balal Izanloo
Journal of Kermanshah University of Medical Sciences.2023;[Epub] CrossRef - Chlorella improves inflammatory profiles and quality of life of prediabetes and diabetes patients
Fernanda Martins, Tamara C. Lopes de Castro, Sara T. Olalla Saad, Rose C. G. Trevisane, Ricardo P. Moreira, Edite Taninaga, Mary L. S. Queiroz, Cristiane Okuda Torello
Fundamental Toxicological Sciences.2023; 10(2): 31. CrossRef - Health-related Quality of Life among Type 2 Diabetes Patients in Southern
Province of Saudi Arabia using WHOQOL-BREF: A Cross-section Study
Areej Homady, Osama Albasheer, Amenah Bajawi, Shatha Hamdi, Aisha Awaf, Tahani Madkhali, Abdallah Sabai, Mohammad R. Zaino, Mohammed Somaili
Current Diabetes Reviews.2023;[Epub] CrossRef - Predicting Factors of Health-Related Quality of Life Among Adults With Type 2 Diabetes: A Systematic Review
Margareta Teli, Ratsiri Thato, Yohanes Andy Rias
SAGE Open Nursing.2023;[Epub] CrossRef - The Impact of Diabetic Disease on Health-Related Quality of Life in
Type 2 Diabetic Patients Karbala. Iraq: Across sectional study
Sammar Jassim Mahan, Mohammed Mahmood Mahammad, Hassan Mutrtadha Hassan
Bionatura.2023; 8(CSS 1): 1. CrossRef - Evaluation of General Health Status in Diabetic Patients Using Short
Form Health Survey (SF-36)
Ali Shlash Al-Ibrahimy, Ihsan Salah Rabea
Current Diabetes Reviews.2023;[Epub] CrossRef - Knowledge and Attitudes About Type 2 Diabetes Among Female Nursing Students in Saudi Arabia
Hafsa A. Abdirahman, Tasneem Hassan, Nada A. AbuAlUla, Kathryn H. Jacobsen
World Medical & Health Policy.2022; 14(1): 47. CrossRef - Toward Personalized Hemoglobin A1c Estimation for Type 2 Diabetes
Namho Kim, Da Young Lee, Wonju Seo, Nan Hee Kim, Sung-Min Park
IEEE Sensors Journal.2022; 22(23): 23023. CrossRef - Health-related quality of life of patients with type 2 diabetes mellitus at a tertiary care hospital in Ethiopia
Girma Tekle Gebremariam, Selam Biratu, Metasebia Alemayehu, Abraham Gebregziabiher Welie, Kebede Beyene, Beate Sander, Gebremedhin Beedemariam Gebretekle, Vijayaprakash Suppiah
PLOS ONE.2022; 17(2): e0264199. CrossRef - The contribution of gastrointestinal microbiota in the existence of type 2 diabetes in Saudi Arabia: Current information and perspectives
Nesreen Aljahdali
Saudi Journal of Biological Sciences.2022; 29(6): 103286. CrossRef - The Health-Related Quality of Life of Patients with Type 2 Diabetes in Saudi Arabia
Amal Khaleel AbuAlhommos, Amjad Heji Alturaifi, Amnah Mohammed Al-Bin Hamdhah, Hawra Hassan Al-Ramadhan, Zahra Abdullah Al Ali, Hawra Jumah Al Nasser
Patient Preference and Adherence.2022; Volume 16: 1233. CrossRef - Quality of life and factors associated with a good quality of life among diabetes mellitus patients in northern Thailand
Ratipark Tamornpark, Suphaphorn Utsaha, Tawatchai Apidechkul, Dunlayaphap Panklang, Fartima Yeemard, Peeradone Srichan
Health and Quality of Life Outcomes.2022;[Epub] CrossRef - Glycaemic control and its associated factors in patients with type 2 diabetes in the Middle East and North Africa: An updated systematic review and meta‐analysis
Odai Hamed Al‐ma'aitah, Daniel Demant, Samantha Jakimowicz, Lin Perry
Journal of Advanced Nursing.2022; 78(8): 2257. CrossRef - Health‐related quality of life of people with type 2 diabetes and its associated factors at a tertiary care clinic in Ningbo, China: A cross‐sectional study
Naomi Carter, Jialin Li, Miao Xu, Li Li, Xuelan Fan, Shuyan Zhu, Pritpal Chahal, Kaushik Chattopadhyay
Endocrinology, Diabetes & Metabolism.2022;[Epub] CrossRef - Health-related quality of life and associated factors among type 2 diabetic adult patients in Debre Markos Referral Hospital, Northwest Ethiopia
Tewodros Eshete Wonde, Tessema Reta Ayene, Nurilign Abebe Moges, Yibelu Bazezew
Heliyon.2022; : e10182. CrossRef - Quality of life among patients with the common chronic disease during COVID-19 pandemic in Northwest Ethiopia: A structural equation modelling
Tadesse Awoke Ayele, Habtewold Shibru Fanta, Malede Mequanent Sisay, Tesfahun Melese Yilma, Melkitu Fentie, Telake Azale, Tariku Belachew, Kegnie Shitu, Tesfa Sewunet Alamneh, Filipe Prazeres
PLOS ONE.2022; 17(12): e0278557. CrossRef - Diabetic foot ulcers: Classification, risk factors and management
Xuan Wang, Chong-Xi Yuan, Bin Xu, Zhi Yu
World Journal of Diabetes.2022; 13(12): 1049. CrossRef - Health‐related quality of life and its predictors among the type 2 diabetes population of Bangladesh: A nation‐wide cross‐sectional study
Lingkan Barua, Mithila Faruque, Hasina Akhter Chowdhury, Palash Chandra Banik, Liaquat Ali
Journal of Diabetes Investigation.2021; 12(2): 277. CrossRef - Assessment of nutritional status and quality of life in individuals with and without diabetes over 65 years of age
Gulseren Pamuk, Gulsah Kaner, Esra Meltem Koc, Tuncay Toşur, Sumeyra Dasdelen, Saliha Aksun, Baris Önder Pamuk
International Journal of Diabetes in Developing Countries.2021; 41(1): 141. CrossRef - Function of family of origin and current quality of life: exploring the mediator role of resilience in Chinese patients with type 2 diabetes
Guizhi Jia, Xin Li, Yuying Chu, Hongliang Dai
International Journal of Diabetes in Developing Countries.2021; 41(2): 346. CrossRef - Self-care activities, glycaemic control and health-related quality of life of patients with type 2 diabetes in a tertiary hospital in Nigeria
Idongesit L. Jackson, Samuel I. Onung, Emmanuel P. Oiwoh
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2021; 15(1): 137. CrossRef - Quality of life among adult patients living with diabetes in Rwanda: a cross-sectional study in outpatient clinics
Charilaos Lygidakis, Jean Paul Uwizihiwe, Michela Bia, Francois Uwinkindi, Per Kallestrup, Claus Vögele
BMJ Open.2021; 11(2): e043997. CrossRef - Health-related quality of life and associated factors among patients with type II diabetes mellitus: A study in the family medicine center (FMC) of Agricultural General Hospital in Hanoi, Vietnam
Nguyen Tran Kien, Nguyen Phuong Hoa, Duong Minh Duc, Johan Wens
Health Psychology Open.2021; 8(1): 205510292199617. CrossRef - Quality of life and adherence to mediterranean diet among type 2 diabetes mellitus patients of a primary health care clinic in Hebron city, Palestine
Manal Badrasawi, May Hamdan, Mohammad Al Tamimi
Mediterranean Journal of Nutrition and Metabolism.2021; 14(3): 255. CrossRef - The TELE-DD project on treatment nonadherence in the population with type 2 diabetes and comorbid depression
Juan Francisco Roy, María Luisa Lozano del Hoyo, Fernando Urcola-Pardo, Alicia Monreal-Bartolomé, Diana Cecilia Gracia Ruiz, María Mercedes Gómez Borao, Ana Belén Artigas Alcázar, José Pedro Martínez Casbas, Alexandra Aceituno Casas, María Teresa Andaluz
Scientific Reports.2021;[Epub] CrossRef - Quality of life among type II diabetic patients attending the primary health centers of King Saud Medical City in Riyadh, Saudi Arabia
Saleh Alsuwayt, Mohammed Almesned, Shahad Alhajri, Naif Alomari, Razan Alhadlaq, Abdullah Alotaibi
Journal of Family Medicine and Primary Care.2021; 10(8): 3040. CrossRef - Influence of Diabetes complications and limitations on health-related quality of life: a study in a southeastern Brazilian city
Cecilia Correa Avila, Margareth Guimarães Lima, Marilisa Berti de Azevedo Barros
Quality of Life Research.2020; 29(2): 473. CrossRef - The impact of diabetes mellitus on health-related quality of life in Saudi Arabia
Diena M. Almasri, Ahmad O. Noor, Ragia H. Ghoneim, Alaa A. Bagalagel, Mansour Almetwazi, Nujud A. Baghlaf, Esraa A. Hamdi
Saudi Pharmaceutical Journal.2020; 28(12): 1514. CrossRef - Predictors of health-related quality of life among patients with diabetes on follow-up at Nekemte specialised Hospital, Western Ethiopia: a cross-sectional study
Bikila Regassa Feyisa, Mekdes Tigistu Yilma, Belachew Etana Tolessa
BMJ Open.2020; 10(7): e036106. CrossRef - Health-related quality of life among patients with type 2 diabetes mellitus in Eastern Province, Saudi Arabia: A cross-sectional study
Dhfer Alshayban, Royes Joseph, Manal S. Fawzy
PLOS ONE.2020; 15(1): e0227573. CrossRef - Factors Associated With Health-Related Quality of Life in Patients With Diabetic Foot Ulcer: A Cross-Sectional Study From Saudi Arabia
Mousab Al Ayed, Mutasem Ababneh, Asirvatham Alwin Robert, Nasser Al Misfer, Maria Cruz, Hesiel C Austria, Mohamed Al Dawish
Cureus.2020;[Epub] CrossRef - Study of Health-Related Quality of Life and Healthcare Utilization among Type 2 Diabetic Population in an Urban Area of Eastern Nepal
Sangita Shah, Nilambar Jha, Deepak Kumar Yadav, Prajjwal Pyakurel, Sanjib Kumar Sharma, Suman Bahadur Singh, Alexander Schreiber
International Journal of Endocrinology.2020; 2020: 1. CrossRef - Oral Health-related Knowledge and Assessment of Oral Health Status of Diabetic Patients Attending Dental Clinic at College of Dentistry, Hail, Kingdom of Saudi Arabia
Rashid I Mian, Fawzeyah FH Rashidi, Tahani M Alshammary, Saad Al Zubaidi, Freah Al Shammary, Junaid Amin, Rabia S Khan
The Journal of Contemporary Dental Practice.2020; 21(1): 78. CrossRef - Prevalence and predictors of depression, anxiety, and stress symptoms among patients with type II diabetes attending primary healthcare centers in the western region of Saudi Arabia: a cross-sectional study
Alhussain Alzahrani, Abdulrahman Alghamdi, Turki Alqarni, Reem Alshareef, Abdullah Alzahrani
International Journal of Mental Health Systems.2019;[Epub] CrossRef - Health-related quality of life among people living with type 2 diabetes: a community based cross-sectional study in rural Nepal
Sailendra Thapa, Prajjwal Pyakurel, Dharani Dhar Baral, Nilambar Jha
BMC Public Health.2019;[Epub] CrossRef - Demographic and clinical predictors of health-related quality of life among people with type 2 diabetes mellitus living in northern Thailand: A cross-sectional study
Saneh Khunkaew, Ritin Fernandez, Jenny Sim
Health and Quality of Life Outcomes.2019;[Epub] CrossRef - Health related quality of life (HRQOL) among low socioeconomic population in Malaysia
Sharifa Ezat Wan Puteh, Chamhuri Siwar, Mohd Azlan Shah Zaidi, Hazila Abdul Kadir
BMC Public Health.2019;[Epub] CrossRef - Exploring variables associated with poor health‐related quality of life in patients with type 2 diabetes in Jordan
Anan S. Jarab, Eman Alefishat, Tareq L. Mukattash, Abdel Qader Albawab, Rana K. Abu‐Farha, James C. McElnay
Journal of Pharmaceutical Health Services Research.2019; 10(2): 211. CrossRef - Health-related quality of life among adults living with diabetic foot ulcers: a meta-analysis
Saneh Khunkaew, Ritin Fernandez, Jenny Sim
Quality of Life Research.2019; 28(6): 1413. CrossRef - Health-related quality of life and its associated factors among adult patients with type II diabetes attending Mizan Tepi University Teaching Hospital, Southwest Ethiopia
Tadesse Gebremedhin, Abdulhalik Workicho, Dessie Abebaw Angaw
BMJ Open Diabetes Research & Care.2019; 7(1): e000577. CrossRef - Quality of life of people with diabetes mellitus
Isabela Fernandes de Aguiar Tonetto, Marcelo Henrique Barbosa Baptista, Danielle dos Santos Gomides, Ana Emilia Pace
Revista da Escola de Enfermagem da USP.2019;[Epub] CrossRef - Evaluating the Direct and Indirect Effects of SF-36 Domains Score on Two Main Factors in Diabetic Patients with Path Analysis: Health-Related Quality of Life Study
Paria Dehesh, Tania Dehesh, Mohammad Hossein Gozashti
Romanian Journal of Diabetes Nutrition and Metabolic Diseases.2019; 26(1): 21. CrossRef - General health status in Iranian diabetic patients assessed by short-form-36 questionnaire: a systematic review and meta-analysis
Masoud Behzadifar, Rahim Sohrabi, Roghayeh Mohammadibakhsh, Morteza Salemi, Sharare Taheri Moghadam, Masood Taheri Mirghaedm, Meysam Behzadifar, Hamid Reza Baradaran, Nicola Luigi Bragazzi
BMC Endocrine Disorders.2018;[Epub] CrossRef - Influencing Pathways to Quality of Life and HbA1c in Patients With Diabetes: A Longitudinal Study That Inform Evidence‐Based Practice
Hui‐Chun Hsu, Yau‐Jiunn Lee, Ruey‐Hsia Wang
Worldviews on Evidence-Based Nursing.2018; 15(2): 104. CrossRef - Effects of a Psychoeducational Program on Hemoglobin A1c Level and Health-Related Quality of Life in Patients with Type 2 Diabetes Mellitus, Jazan, Saudi Arabia
Samy Shaban Mahmoud, Mona Husein EL Mahdy, Mohamed Salih Mahfouz, Ibrahim Saad Nada, Abdulwahab Abdoh Aqeeli, Mohammed Ahmed AL Darbi, Anas Elias Ahmed
BioMed Research International.2018; 2018: 1. CrossRef - The effects of periodontal treatment on diabetic patients: The DIAPERIO randomized controlled trial
Jean‐Noel Vergnes, Thibault Canceill, Alexia Vinel, Sara Laurencin‐Dalicieux, Françoise Maupas‐Schwalm, Vincent Blasco‐Baqué, Hélène Hanaire, Elise Arrivé, Vincent Rigalleau, Cathy Nabet, Michel Sixou, Pierre Gourdy, Paul Monsarrat
Journal of Clinical Periodontology.2018; 45(10): 1150. CrossRef - Health-related quality of life and associated factors among patients with diabetes mellitus in Botswana
Godfrey Mutashambara Rwegerera, Thato Moshomo, Marea Gaenamong, Taibat Aderonke Oyewo, Sivasomnath Gollakota, Yordanka Piña Rivera, Anthony Masaka, Brian Godman, Meshack Shimwela, Dereje Habte
Alexandria Journal of Medicine.2018; 54(2): 111. CrossRef - Related factors of quality of life of type 2 diabetes patients: a systematic review and meta-analysis
Xiyue Jing, Jiageng Chen, Yanan Dong, Duolan Han, Haozuo Zhao, Xuying Wang, Fei Gao, Changping Li, Zhuang Cui, Yuanyuan Liu, Jun Ma
Health and Quality of Life Outcomes.2018;[Epub] CrossRef - Minimally important difference and predictors of change in quality of life in type 2 diabetes: A community‐based survey in China
Xuejing Jin, Gordon G. Liu, Hertzel C. Gerstein, Mitchell A.H. Levine, Haijing Guan, Hongchao Li, Feng Xie
Diabetes/Metabolism Research and Reviews.2018;[Epub] CrossRef - Effects of long-term multicomponent exercise on health-related quality of life in older adults with type 2 diabetes: evidence from a cohort study
Liliana C. Baptista, Gonçalo Dias, Nelba R. Souza, Manuel T. Veríssimo, Raul A. Martins
Quality of Life Research.2017; 26(8): 2117. CrossRef - Health benefits of Quran memorization for older men
Nazmus Saquib, Juliann Saquib, Abdulrahman Alhadlag, Mohamad Anas Albakour, Bader Aljumah, Mohammed Sughayyir, Ziad Alhomidan, Omar Alminderej, Mohamed Aljaser, Ahmed Mohammed Al-Dhlawiy, Abdulrahman Al-Mazrou
SAGE Open Medicine.2017; 5: 205031211774099. CrossRef - Prevalence of overactive bladder and its impact on quality of life in 1025 patients with type 2 diabetes in mainland China
Dongjuan Xu, Jie Gao, Xiaojuan Wang, Liqun Huang, Kefang Wang
Journal of Diabetes and its Complications.2017; 31(8): 1254. CrossRef - Testing whether patients with diabetes and healthy people perceive the meaning of the items in the Persian version of the SF-36 questionnaire similarly: a differential item functioning analysis
Zahra Bagheri, Peyman Jafari, Marzieh Mahmoodi, Mohammad Hossein Dabbaghmanesh
Quality of Life Research.2017; 26(4): 835. CrossRef - Negative effects of diabetes–related distress on health-related quality of life: an evaluation among the adult patients with type 2 diabetes mellitus in three primary healthcare clinics in Malaysia
Boon-How Chew, Sherina Mohd-Sidik, Sazlina Shariff-Ghazali
Health and Quality of Life Outcomes.2015;[Epub] CrossRef
- Related articles
-
- Clinical Effects of a Home Care Pilot Program for Patients with Type 1 Diabetes Mellitus: A Retrospective Cohort Study
- Low Household Income Status and Death from Pneumonia in People with Type 2 Diabetes Mellitus: A Nationwide Study
- Safety of COVID-19 Vaccines among Patients with Type 2 Diabetes Mellitus: Real-World Data Analysis
- Advanced Liver Fibrosis Is Associated with Chronic Kidney Disease in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
- Serum Retinol-Binding Protein Levels Are Associated with Nonalcoholic Fatty Liver Disease in Chinese Patients with Type 2 Diabetes Mellitus: A Real-World Study

 KDA
KDA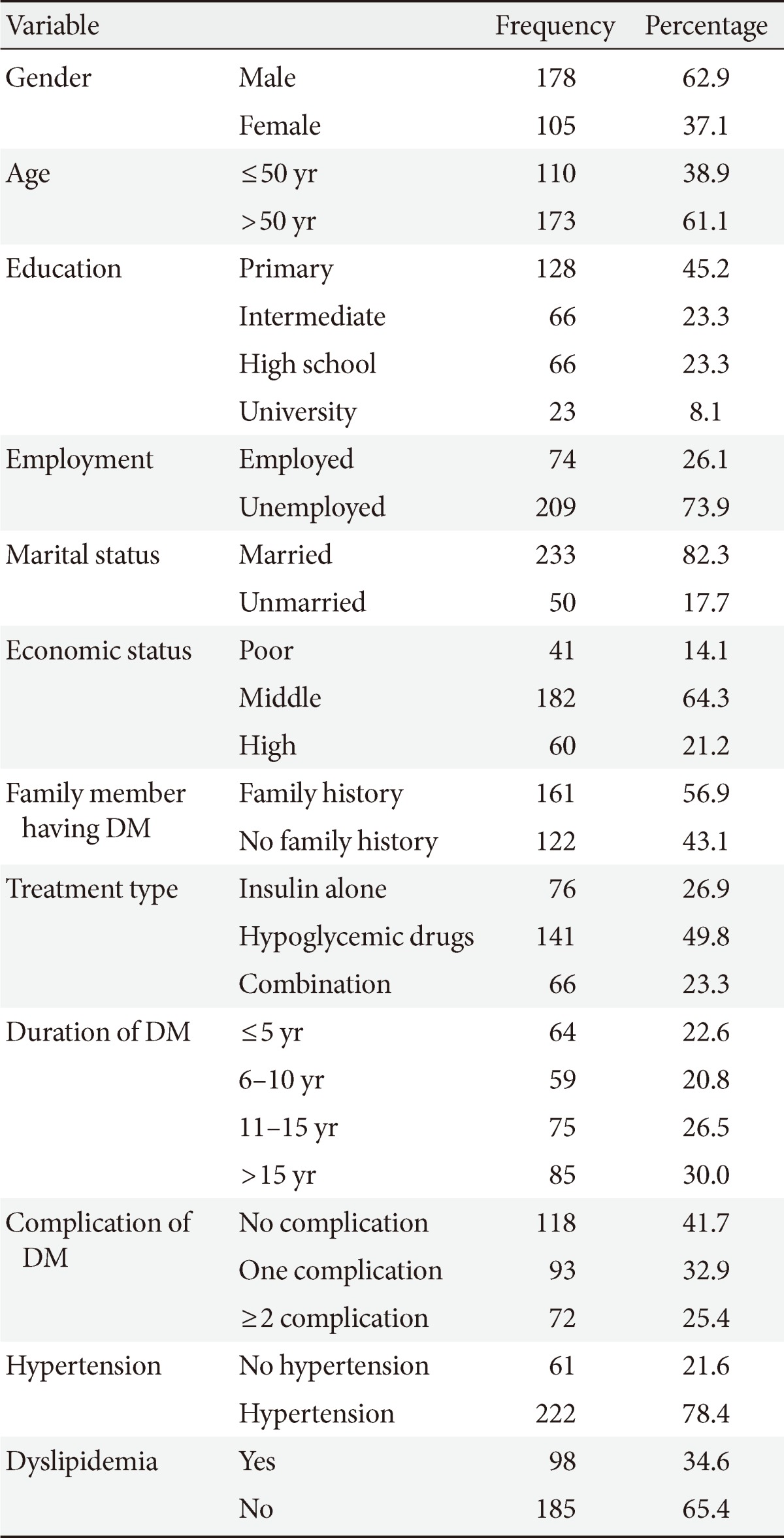

 PubReader
PubReader Cite
Cite



