- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 38(4); 2014 > Article
-
ReviewEpidemiology Diabetic Kidney Disease: From Epidemiology to Clinical Perspectives
- Cheol Whee Park
-
Diabetes & Metabolism Journal 2014;38(4):252-260.
DOI: https://doi.org/10.4093/dmj.2014.38.4.252
Published online: August 20, 2014
Division of Nephrology, Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea.
- Corresponding author: Cheol Whee Park. Division of Nephrology, Department of Internal Medicine, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, 222 Banpo-daero, Seocho-gu, Seoul 137-701, Korea. cheolwhee@hanmail.net
Copyright © 2014 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- With worldwide epidemic of diabetes mellitus, diabetic nephropathy which is one of the major causes of microvascular complication has become a serious concern in Korea as well as the rest of the world. In view of its significance, there is an urgent and paramount need for proper managements that could either deter or slow the progression of diabetic nephropathy. Despite advances in care, ever increasing number of patients suffering from diabetic kidney disease and from end-stage renal disease implies that the current management is not adequate in many aspects. The reasons for these inadequacies compromise lack of early diagnosis, failure to intervene with timely and aggressive manner, and lack of understanding on the kind of interventions required. Another issue equally important for the adequate care of patients with diabetic nephropathy is an understanding of past, present and future epidemiology of diabetic nephropathy which serves, especially in Korea, as a material determining standard diagnosis and treatment and a national health-policy decision.
- Chronic kidney disease (CKD) has become a global health care problem. The cost of health services for patients with CKD is 1.8 times higher compared to patients without CKD [1]. The average cost for a dialysis patient is 10.3 times more than that of a non-CKD patient [1]. CKD is one of the widely recognized and notorious indicators for hospitalization, cardiovascular events, cardiovascular and noncardiac mortality, and all-cause of mortality [2,3]. CKD also affects cognitive impairment and quality of life [4,5]. Unfortunately, there is a dispute and it is unclear whether the rates of CKD in Korea are consistently increasing or not. In contrast, there is a clear result that the number of patients with end-stage renal disease (ESRD) undergoing dialysis is on the rise among Koreans which is the main contributor to the increasing prevalence of diabetic kidney disease (DKD) [6]. It is evident that the progression of renal failure continues in DKD despite tight and early glucose control, tight blood pressure control as well as aggressive renin-angiotensin-aldosterone (RAA) blockade. This review summarizes what is known about the epidemiology of CKD and DKD among Korean adults and discusses some of the clinically important challenges associated with the diagnosis of DKD.
INTRODUCTION
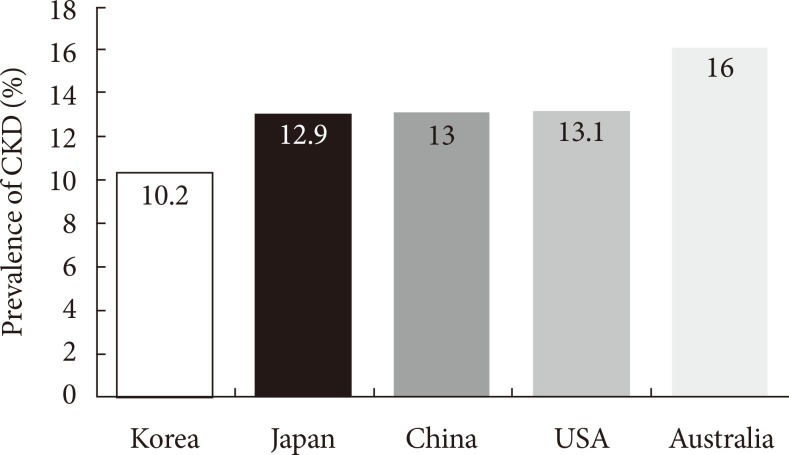
- As CKD patients are identified as a group of patients exposed to high risk for death with high rate of comorbidities, it is justifiable to call for careful study and close attention to the management of risk factor [1]. CKD (estimated glomerular filtration rate [eGFR] <60 mL/min/1.73 m2 or urine albumin-creatinine ratio>30 mg/g) is estimated to affect 13.1% of the United States (US) population, according to the 2012 US Renal Data Systems report [7,8]. Diabetes is the most prevalent cause of ESRD and is also the major cause for 40.4% of newly developed ESRD in the US, followed by hypertension in the cohort in 2005 to 2010 [7,8]. In the Australian Diabetes, Obesity, and Lifestyle Study, 16.0% of the study population had one or more indicators of CKD, such as impaired kidney function, hematuria, or proteinuria [9]. As far as the prevalence of CKD in the Asian population is concerned, it is reported to be 12.9% in Japan [10] and 13.0% in Beijing (Fig. 1) [11]. There were no big differences in the prevalence of CKD among the various countries. Interestingly, the CKD prevalence in the US has increased from 10.0% on National Health and Nutritional Examination Survey (NHANES) III (1988 to 1994) to 13.1% on NHANES 1999 to 2004 [8]. A recent study from Japan also showed that the overall CKD prevalence among the Japanese male has increased from 13.8% in 1974 to 22.1% in 2002 and it was attributed to increase in diabetes, hypercholesterolemia, and obesity over the three decades in males [12].
- In contrast to other countries, the CKD prevalence in the Korean adult population has not been well known. According to Chin [13], the prevalence of CKD in Korean adult population has decreased from 12.4% in 2006 to 10.2% in 2008 (Fig. 1). However, the study was conducted in two tertiary hospitals and it could not explain the reason for the decrease in the prevalence. A recent study also reported that the prevalence of CKD in Korean adults in 2009 to be 4.5% in men and 6.3% in women citing data from the Korea National Health and Nutritional Examination Survey (KNHANES) IV [14]. The authors, however, did not compare the prevalence of CKD by diabetes status, nor did they investigate the determinants of CKD. The KNHANES V, conducted in 2011 has defined albuminuria (a spot urine albumin/creatinine ratio >30 mg/g) and CKD (eGFR <60 mL/min/1.73 m2). The prevalences of microalbuminuria, macroalbuminuria, and CKD among patients without diabetes were 9.4%, 0.8%, and 1.7%, respectively. In contrast, the prevalences of microalbuminuria, macroalbuminuria, and CKD among patients with diabetes were 22.0%, 4.6%, and 8.6%, respectively [15]. In patients without diabetes, the overall prevalence of CKD including albuminuria and decreased eGFR was 11.9% and the prevalence in patients with diabetes was 35.2%. Korean adults with diabetes are exposed to the risk of CKD three times more than the nondiabetic adults, suggesting that diabetes is associated with an approximately 3.0-fold increased risk of CKD [15]. Epidemiological studies based on diabetes as the primary renal disease must be interpreted with caution [16] as renal biopsies are performed in less than 10% to 20% of diabetic patients and thus many of nephropathies are determined by clinical evaluation based on nephrologists' clinical experiences [17].
HOW PREVALENT IS CKD?
- Diabetic nephropathy is associated with an increased risk of CKD, which is characterized by albuminuria or reduced eGFR. Estimates of the prevalence of DKD vary widely. It ranges from 10% to 40% for both type 1 and type 2 diabetes patient groups depending on the definition of the disease used [18,19]. The prevalence of albumiuria varies with ethnicity with higher rates reported in Asians as compared to Caucasians [20,21]. Unfortunately, the prevalence of type 2 diabetes has increased worldwide including Korea [22,23]. Data from the Centers for Disease Control and Prevention (CDC) report that there are approximately 22 million people in the US with diabetes [24]. Moreover, the CDC estimates that one in three adults in the US will have diabetes by 2050 if the current trends continue. According to the numbers from NHANUS III report, 19.3% of diabetes had eGFRs <60 mL/min/1.73 m2, 29.9% had urine albumin-creatinine ratios >30 mg/g, and 8.6% of all patients with diabetes had both [24]. For those with hypertension and without diabetes, the reported prevalence of eGFRs <60 mL/min/1.73 m2, and urine albumin-creatinine ratios >30 mg/g, and both were 12.9%, 24.8%, and 4.1%, respectively [9].
- According to the recent study, the prevalence of diabetes and prediabetes in Korea were 10.5% and 19.3%, respectively [25]. In the US, the NHANES III reported that the prevalences of microalbuminuria and macroalbuminuria among adults with type 2 diabetes aged ≥40 years were 35% and 6%, respectively [8]. Based on the study in 930 patients with type 2 diabetes, the Shanghai Diabetic Complications Study reported that the prevalences of microalbuminuria and macroalbuminuria were 22.8% and 3.4%, respectively [26]. According to the KNHANES V in 2011, which conducted survey on measured albuminuria for the first time, the prevalence of microalbuminuria, macroalbuminuria, and CKD were 22.0%, 4.7%, and 8.6%, respectively [15]. Other studies have shown slightly different results. In a single center study conducted in 1995 including 631 Korean patients with type 2 diabetes, the prevalence of albuminuria was 34% (20%, microalbuminuria; 14%, macroalbuminuria) [27] as compared to another study in 2011 on 3,738 patients with type 2 diabetes and hypertension [28], showing 29.4% (23.1%, microalbuminuria; 6.3%, macroalbuminuria) of the prevalence.
- The prevalence of CKD in patients with type 2 diabetes in the KNHANES V was 8.6% which is much lower than that in Western populations as well as in other East Asian populations. In the US, the prevalence of CKD increased from 14.9% in NHANES 1988 to 1994 to 17.7% in NHANES 2005 to 2008 in patients with diabetes [29]. The prevalence of CKD in patients with type 2 diabetes was 10.2% in China [30] and 15.3% in Japan [31]. The reason for the differences among various population groups could be due to their distinct ethnicities and MDRD equation [28].
HOW PREVALENT IS DKD?
- Although there have been significant improvements in the diagnosis of DKD, it is still debatable as to the significance of microalbuminuria as a proper indicator of kidney disease. In addition, the actual proportion of DKD as a cause of CKD is questionable because there often is inaccuracy of documentation of medical diagnosis while some patients labeled with DKD may have another diagnosis such as hypertension or immunoglobulin A nephropathy [32]. In type 1 diabetes, for those with long standing diabetes, retinopathy, microalbuminuria with absence of heavy proteinuria and hematuria and with relatively preserved kidney sizes, the diagnosis of DKD can be made certainly in more than 95% of patients [33,34]. However, renal disease in type 2 diabetes is much more complex. The prevalence of nondiabetic renal disease with or without diabetic nephropathy is reported to be around 27% to 79% in type 2 diabetes with nephropathy [35,36,37,38,39]. Any types of kidney disease can occur in patients with diabetes. Because of the lack of a precise diagnosis and the associated diseases as confounding factors, the clinician should bear in mind that renal disease in patients with type 2 diabetes may not be fully attributable to DKD alone. Usually diabetic patients undergo diagnostic renal biopsies only when the clinical course is not typical for diabetic nephropathy. In terms of eGFR, the equations used to estimate GFR are not accurate reflections of GFR, but rather general estimates [40] and normal aging can result in an eGFR <60 mL/min/1.73 m2. It would be better to select age-appropriate targets for the definition of CKD. Therefore, eGFR <60 mL/min/1.73 m2 is an appropriate indicator for those under 50 years of age, whereas the definition of stage 3 CKD should be eGFR <45 mL/min/1.73 m2 for people above the age of 50 years [32]. In sum, a more accurate reflection of the impact of CKD (and DKD) is seen in ESRD data with no dispute on the number of people with dialysis or transplants [40].
- Since nephrologists do not make the initial diagnosis of DKD, they rely on primary care physicians and endocrinologists to make the diagnosis. Thus, one of the major goals for nephrologists is to provide them with much in-depth education and maintain good liaison with nonnephrology physicians who care for patients with diabetes. The routine evaluation of diabetes for DKD will enable them either to provide appropriate treatment or refer to a nephrologist [32]. Referral to or at least a screening visit to a nephrologist is mandatory if eGFR is declining (<45 mL/min/1.73 m2) and urine albumin-creatinine ratio is >300 mg/g (or urine protein-creatinine ratio is >0.5 g/g) [32]. In fact, 43% of the total patients started dialysis in the US without ever seeing a nephrologist in 2010 [40] and 38.9% of the patients who were known to have diabetes started dialysis therapy without ever being referred to a nephrologist [40]. Late referral to renal specialists is associated with increased morbidity and mortality and may result in poorer patient-related outcomes [41].
HOW DO YOU DIAGNOSE DKD?
- In the US, there were about 35,000 dialysis patients and about 6,000 transplant recipients in 1978 [40]. As of 2010, there were approximately 415,000 dialysis patients and 180,000 transplant recipients. The incidence of ESRD has increased from 86.8 per million to 347 per million cases per year. Of greater importance is the fact that the incidence rates of ESRD had been increasing steadily up to 2002, but have remained almost stable since, although the prevalence continues to rise [40]. The reason for this slowing of incidence rate of ESRD is due to the emergence of diabetes as the major cause of renal disease. Despite an increased incidence of diabetes, many studies have supported that a person with CKD is much more likely to die of a cardiovascular event rather than surviving to receiving dialysis or a transplant for DKD in type 2 diabetes [42,43,44,45]. A recent study demonstrated that patients with diabetes with CKD compared to non-DKD have much higher death rates for the same level of GFR [42]. However, the total number of patients with ESRD continues to increase at a rapid rate with diabetes being the principal cause [44]. Fortunately, this trend might not continue because there is a recent report suggesting that this rapid increase may be slowing down [46].
- In Korea, total number of patients with renal replacement therapy in 2012 was 70,211 and the prevalence of ESRD was 1,353 patients per million population [6], which was 63,341 and 1,224 patients per million population, respectively, in 2011 [6]. As of 2012, the incidence of ESRD was 221 per million cases per year and the number of new ESRD patients was 11,472 (Fig. 2). The most common primary cause of ESRD in 2012 was diabetic nephropathy (50.6%) followed by hypertensive nephrosclerosis (18.5%) and chronic glomerulonephritis (8.1%) (Fig. 3). In contrast to the US, the total number of new patients with ESRD has steadily increased, which occurred along with an increase in the number of patients with diabetes (Fig. 3) [6,25]. Recent KNHANES V study showed that the prevalence of diabetes and prediabetes markedly increased when hemoglobin A1c (HbA1c) is added as a diagnostic criterion [25]. Since the proportion of diabetes and prediabetes has largely increased, the complications of diabetes including DKD will be increasing significantly as well. This trend will be much the same for the prevalence and incidence of ESRD patients. Therefore, new recommendations will be helpful for detection of patients with early diabetic nephropathy with risk of complications. The ESRD registry of Korean Society of Nephrology clearly shows that 46.9% of ESRD patients had died of cardiovascular events [6]. Thus, we should consider novel means as to how we could improve patient care by early diagnosis, aggressive and proper management of patients with diabetes.
HOW PREVALENT IS ESRD?
- To prevent the progression of DKD and subsequent cardiovascular morbidity and mortality entailed in patients with diabetes, it is important to personalize treatment and to set treatment goals for individual patients depending on age, type of diabetes, and its duration [47]. Bearing in mind that longer duration of diabetes, poor glycemic control, presence of albuminuria, and hypertension are the common risk factors for DKD and its progression, a multilateral approach targeting these risk factors could be considered. The Steno-2 trial showed the success of such a multifactorial approach in patients with type 2 diabetes and microalbuminuria [48]. In the Steno-2 trial, all of the patients were treated for a mean period of 7.8 years with either conventional or intensive regimen consisting of tight glucose control (target HbA1c <6.5%), blood pressure control with RAA system (RAAS) blockade (with its use regardless of initial blood pressure level; target blood pressure <130/80 mm Hg), aspirin and lipid-lowering agents (target total cholesterol <175 mg/dL, fasting triglycerides <150 mg/dL). After 13.3 years of follow-up, intensive therapy was associated with a 20% absolute mortality risk reduction. In the intensive group, DKD (20 patients vs. 37 patients) and ESRD (1 patient vs. 6 patients) developed in fewer subjects as compared to the conventional regimen group [48]. These results showed that a multitargeted therapy can slow the progression of DKD. In addition, to potentiate the effects of RAAS blockade, sodium restriction and/or diuretics should be considered [49]. Clinical trials confirming positive effects of aldosterone blockade are also needed [50]. Korean subjects with diabetes showed that high blood pressure was significantly associated with an increased risk of albuminuria while older age, higher serum triglyceride levels, and longer diabetes duration were determinants of CKD [15]. Therefore, a multitargeted therapy might retard and slow the progression of DKD in Korean diabetic patients.
- DKD is characterized by a long period of clinical silence without significant signs or symptoms. Therefore, novel methods for detecting early mediators of renal injury are needed to find out the onset of DKD at the earliest and to prevent its progression. Recently, several new targets are showing promise as markers in the prevention and treatment of early DKD in type 1 diabetes [51]. These are serum uric acid, insulin sensitivity, vasopressin, and sodium-glucose cotransport-2 inhibition which may have same roles in type 2 diabetes as well. However, further studies are required to confirm the roles of these targets in type 2 diabetes. We also try our best to identify novel and modifiable risk factors, including transforming growth factor-β, bone morphogenic growth factor-7 in serum and urine that contribute to the development and progression of early diabetic nephropathy [52].
- Advances in our understanding of the mechanisms of DKD have identified additional risk factors for nephropathy. Subsequently, novel therapeutic options are being explored targeting these factors. The beneficial effects of many of the novel agents on DKD are attributed to their vascular protective factors, antifibrotic, antioxidant, anti-inflammatory, and intracellular metabolic modulatory properties [53,54,55,56,57]. However, many clinical trials with novel agents targeting these effects have not shown dramatic efficacy in preventing or delaying DKD [53]. Thus, continuing research is needed to look for novel therapies for DKD and thereby to reduce the morbidity and mortality associated with it.
HOW TO PREVENT THE PROGRESSION OF DKD TO ESRD
- ESRD is a major public health problem in Korea with diabetes being the leading cause. Significant improvements have been made in the diagnosis, prevention, and treatment of diabetes that have contributed to slow progression of the disease and to prevent the cardiovascular complications. On the contrary, the risk of ESRD in patients with diabetes is not decreasing but it is increasing continually. The principal goals of the health care system should focus on the prevention and slowing of progression of CKD resulting from diabetes and health-care providers including nephrologists and endocrinologists are required to determine the best approach for both diagnosis and management [32].
- It is very important that the nephrology community provides leadership in early diagnosis, best and aggressive management, cost-effective interventions, and education to slow down the DKD epidemic. Furthermore, research into novel therapies to treat diabetic nephropathy is an urgent need aiming at the prevention and management of DKD and this should be preceded by appropriate understanding of the prevalence and the nature of diabetic nephropathy. Clearly, tremendous additional experimental efforts will be needed to uncover the complex pathogenesis of diabetes and its cardiovascular complications.
CONCLUSIONS
-
Acknowledgements
- The author would like to thank Dr. Yaeni Kim for her valuable support in making this manuscript.
ACKNOWLEDGMENTS
- 1. Hunsicker LG. The consequences and costs of chronic kidney disease before ESRD. J Am Soc Nephrol 2004;15:1363-1364. ArticlePubMed
- 2. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 2004;351:1296-1305. ArticlePubMed
- 3. Foley RN, Murray AM, Li S, Herzog CA, McBean AM, Eggers PW, Collins AJ. Chronic kidney disease and the risk for cardiovascular disease, renal replacement, and death in the United States Medicare population, 1998 to 1999. J Am Soc Nephrol 2005;16:489-495. ArticlePubMed
- 4. Madan P, Kalra OP, Agarwal S, Tandon OP. Cognitive impairment in chronic kidney disease. Nephrol Dial Transplant 2007;22:440-444. ArticlePubMed
- 5. Chin HJ, Song YR, Lee JJ, Lee SB, Kim KW, Na KY, Kim S, Chae DW. Moderately decreased renal function negatively affects the health-related quality of life among the elderly Korean population: a population-based study. Nephrol Dial Transplant 2008;23:2810-2817. ArticlePubMed
- 6. Jin DC, Han JS. Renal replacement therapy in Korea, 2012. Kidney Res Clin Pract 2014;33:9-18.ArticlePubMedPMC
- 7. United States Renal Data System: USRDS Annual Data Report. National Institute of Diabetes and Digestive and Kidney Diseases; 2013. updated 2014 May 1. Available from: www.usrds.org.
- 8. Coresh J, Selvin E, Stevens LA, Manzi J, Kusek JW, Eggers P, Van Lente F, Levey AS. Prevalence of chronic kidney disease in the United States. JAMA 2007;298:2038-2047. ArticlePubMed
- 9. Chadban SJ, Briganti EM, Kerr PG, Dunstan DW, Welborn TA, Zimmet PZ, Atkins RC. Prevalence of kidney damage in Australian adults: the AusDiab kidney study. J Am Soc Nephrol 2003;14(7 Suppl 2):S131-S138. PubMed
- 10. Imai E, Horio M, Watanabe T, Iseki K, Yamagata K, Hara S, Ura N, Kiyohara Y, Moriyama T, Ando Y, Fujimoto S, Konta T, Yokoyama H, Makino H, Hishida A, Matsuo S. Prevalence of chronic kidney disease in the Japanese general population. Clin Exp Nephrol 2009;13:621-630. ArticlePubMedPDF
- 11. Zhang L, Zhang P, Wang F, Zuo L, Zhou Y, Shi Y, Li G, Jiao S, Liu Z, Liang W, Wang H. Prevalence and factors associated with CKD: a population study from Beijing. Am J Kidney Dis 2008;51:373-384. ArticlePubMed
- 12. Nagata M, Ninomiya T, Doi Y, Yonemoto K, Kubo M, Hata J, Tsuruya K, Iida M, Kiyohara Y. Trends in the prevalence of chronic kidney disease and its risk factors in a general Japanese population: the Hisayama Study. Nephrol Dial Transplant 2010;25:2557-2564. ArticlePubMed
- 13. Chin HJ, Ahn JM, Na KY, Chae DW, Lee TW, Heo NJ, Kim S. The effect of the World Kidney Day campaign on the awareness of chronic kidney disease and the status of risk factors for cardiovascular disease and renal progression. Nephrol Dial Transplant 2010;25:413-419. ArticlePubMed
- 14. Kang HT, Lee J, Linton JA, Park BJ, Lee YJ. Trends in the prevalence of chronic kidney disease in Korean adults: the Korean National Health and Nutrition Examination Survey from 1998 to 2009. Nephrol Dial Transplant 2013;28:927-936. ArticlePubMed
- 15. Ahn JH, Yu JH, Ko SH, Kwon HS, Kim DJ, Kim JH, Kim CS, Song KH, Won JC, Lim S, Choi SH, Han K, Cha BY, Kim NH. Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Prevalence and determinants of diabetic nephropathy in Korea: Korea national health and nutrition examination survey. Diabetes Metab J 2014;38:109-119. ArticlePubMedPMC
- 16. Chong YB, Keng TC, Tan LP, Ng KP, Kong WY, Wong CM, Cheah PL, Looi LM, Tan SY. Clinical predictors of non-diabetic renal disease and role of renal biopsy in diabetic patients with renal involvement: a single centre review. Ren Fail 2012;34:323-328. ArticlePubMed
- 17. Villar E, Polkinghorne KR, Chang SH, Chadban SJ, McDonald SP. Effect of type 2 diabetes on mortality risk associated with end-stage kidney disease. Diabetologia 2009;52:2536-2541. ArticlePubMedPDF
- 18. Gross JL, de Azevedo MJ, Silveiro SP, Canani LH, Caramori ML, Zelmanovitz T. Diabetic nephropathy: diagnosis, prevention, and treatment. Diabetes Care 2005;28:164-176. ArticlePubMedPDF
- 19. Ritz E, Orth SR. Nephropathy in patients with type 2 diabetes mellitus. N Engl J Med 1999;341:1127-1133. ArticlePubMed
- 20. Young BA, Katon WJ, Von Korff M, Simon GE, Lin EH, Ciechanowski PS, Bush T, Oliver M, Ludman EJ, Boyko EJ. Racial and ethnic differences in microalbuminuria prevalence in a diabetes population: the pathways study. J Am Soc Nephrol 2005;16:219-228. PubMed
- 21. Parving HH, Lewis JB, Ravid M, Remuzzi G, Hunsicker LG. DEMAND investigators. Prevalence and risk factors for microalbuminuria in a referred cohort of type II diabetic patients: a global perspective. Kidney Int 2006;69:2057-2063. ArticlePubMed
- 22. Wild S, Roglic G, Green A, Sicree R, King H. Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 2004;27:1047-1053. ArticlePubMedPDF
- 23. Danaei G, Finucane MM, Lu Y, Singh GM, Cowan MJ, Paciorek CJ, Lin JK, Farzadfar F, Khang YH, Stevens GA, Rao M, Ali MK, Riley LM, Robinson CA, Ezzati M. Global Burden of Metabolic Risk Factors of Chronic Diseases Collaborating Group (Blood Glucose). National, regional, and global trends in fasting plasma glucose and diabetes prevalence since 1980: systematic analysis of health examination surveys and epidemiological studies with 370 country-years and 2.7 million participants. Lancet 2011;378:31-40. ArticlePubMed
- 24. Centers for Disease Control and Prevention: Diabetes report card 2012: national and state profile of diabetes and its complications Updated 2013 Apr 3. Available from: http://www.cdc.gov/diabetes/pubs/reportcard.htm.
- 25. Jeon JY, Ko SH, Kwon HS, Kim NH, Kim JH, Kim CS, Song KH, Won JC, Lim S, Choi SH, Jang MJ, Kim Y, Oh K, Kim DJ, Cha BY. Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Prevalence of diabetes and prediabetes according to fasting plasma glucose and HbA1c. Diabetes Metab J 2013;37:349-357. ArticlePubMedPMC
- 26. Jia W, Gao X, Pang C, Hou X, Bao Y, Liu W, Wang W, Zuo Y, Gu H, Xiang K. Prevalence and risk factors of albuminuria and chronic kidney disease in Chinese population with type 2 diabetes and impaired glucose regulation: Shanghai diabetic complications study (SHDCS). Nephrol Dial Transplant 2009;24:3724-3731. ArticlePubMed
- 27. Lee KU, Park JY, Kim SW, Lee MH, Kim GS, Park SK, Park JS. Prevalence and associated features of albuminuria in Koreans with NIDDM. Diabetes Care 1995;18:793-799. ArticlePubMedPDF
- 28. Yang CW, Park JT, Kim YS, Kim YL, Lee YS, Oh YS, Kang SW. Prevalence of diabetic nephropathy in primary care type 2 diabetic patients with hypertension: data from the Korean Epidemiology Study on Hypertension III (KEY III study). Nephrol Dial Transplant 2011;26:3249-3255. ArticlePubMed
- 29. de Boer IH, Rue TC, Hall YN, Heagerty PJ, Weiss NS, Himmelfarb J. Temporal trends in the prevalence of diabetic kidney disease in the United States. JAMA 2011;305:2532-2539. ArticlePubMedPMC
- 30. Chen W, Chen W, Wang H, Dong X, Liu Q, Mao H, Tan J, Lin J, Zhou F, Luo N, He H, Johnson RJ, Zhou SF, Yu X. Prevalence and risk factors associated with chronic kidney disease in an adult population from southern China. Nephrol Dial Transplant 2009;24:1205-1212. ArticlePubMed
- 31. Yokoyama H, Sone H, Oishi M, Kawai K, Fukumoto Y, Kobayashi M. Japan Diabetes Clinical Data Management Study Group. Prevalence of albuminuria and renal insufficiency and associated clinical factors in type 2 diabetes: the Japan Diabetes Clinical Data Management study (JDDM15). Nephrol Dial Transplant 2009;24:1212-1219. ArticlePubMed
- 32. Stanton RC. Clinical challenges in diagnosis and management of diabetic kidney disease. Am J Kidney Dis 2014;63(2 Suppl 2):S3-S21. ArticlePubMed
- 33. Kramer HJ, Nguyen QD, Curhan G, Hsu CY. Renal insufficiency in the absence of albuminuria and retinopathy among adults with type 2 diabetes mellitus. JAMA 2003;289:3273-3277. ArticlePubMed
- 34. Mauer SM, Chavers BM, Steffes MW. Should there be an expanded role for kidney biopsy in the management of patients with type I diabetes? Am J Kidney Dis 1990;16:96-100. ArticlePubMed
- 35. Mak SK, Gwi E, Chan KW, Wong PN, Lo KY, Lee KF, Wong AK. Clinical predictors of non-diabetic renal disease in patients with non-insulin dependent diabetes mellitus. Nephrol Dial Transplant 1997;12:2588-2591. ArticlePubMed
- 36. Tone A, Shikata K, Matsuda M, Usui H, Okada S, Ogawa D, Wada J, Makino H. Clinical features of non-diabetic renal diseases in patients with type 2 diabetes. Diabetes Res Clin Pract 2005;69:237-242. ArticlePubMed
- 37. Caramori ML, Fioretto P, Mauer M. The need for early predictors of diabetic nephropathy risk: is albumin excretion rate sufficient? Diabetes 2000;49:1399-1408. ArticlePubMedPDF
- 38. Lin YL, Peng SJ, Ferng SH, Tzen CY, Yang CS. Clinical indicators which necessitate renal biopsy in type 2 diabetes mellitus patients with renal disease. Int J Clin Pract 2009;63:1167-1176. ArticlePubMed
- 39. Wong TY, Choi PC, Szeto CC, To KF, Tang NL, Chan AW, Li PK, Lai FM. Renal outcome in type 2 diabetic patients with or without coexisting nondiabetic nephropathies. Diabetes Care 2002;25:900-905. ArticlePubMedPDF
- 40. Collins AJ, Foley RN, Herzog C, Chavers B, Gilbertson D, Herzog C, Ishani A, Johansen K, Kasiske B, Kutner N, Liu J, St Peter W, Ding S, Guo H, Kats A, Lamb K, Li S, Li S, Roberts T, Skeans M, Snyder J, Solid C, Thompson B, Weinhandl E, Xiong H, Yusuf A, Zaun D, Arko C, Chen SC, Daniels F, Ebben J, Frazier E, Hanzlik C, Johnson R, Sheets D, Wang X, Forrest B, Constantini E, Everson S, Eggers P, Agodoa L. US renal data system 2012 annual data report. Am J Kidney Dis 2013;61(1 Suppl 1):A7e1-e476. ArticlePubMed
- 41. Navaneethan SD, Nigwekar S, Sengodan M, Anand E, Kadam S, Jeevanantham V, Grieff M, Choudhry W. Referral to nephrologists for chronic kidney disease care: is non-diabetic kidney disease ignored? Nephron Clin Pract 2007;106:c113-c118. ArticlePubMedPDF
- 42. Afkarian M, Sachs MC, Kestenbaum B, Hirsch IB, Tuttle KR, Himmelfarb J, de Boer IH. Kidney disease and increased mortality risk in type 2 diabetes. J Am Soc Nephrol 2013;24:302-308. ArticlePubMedPMC
- 43. Jude EB, Anderson SG, Cruickshank JK, Srivatsa A, Tentolouris N, Chandrasekaran R, Gokal R, Boulton AJ. Natural history and prognostic factors of diabetic nephropathy in type 2 diabetes. QJM 2002;95:371-377. ArticlePubMed
- 44. Muntner P, Bowling CB, Gao L, Rizk D, Judd S, Tanner RM, McClellan W, Warnock DG. Age-specific association of reduced estimated glomerular filtration rate and albuminuria with all-cause mortality. Clin J Am Soc Nephrol 2011;6:2200-2207. ArticlePubMedPMC
- 45. Ninomiya T, Perkovic V, de Galan BE, Zoungas S, Pillai A, Jardine M, Patel A, Cass A, Neal B, Poulter N, Mogensen CE, Cooper M, Marre M, Williams B, Hamet P, Mancia G, Woodward M, Macmahon S, Chalmers J. ADVANCE Collaborative Group. Albuminuria and kidney function independently predict cardiovascular and renal outcomes in diabetes. J Am Soc Nephrol 2009;20:1813-1821. ArticlePubMedPMC
- 46. Couchoud C, Villar E. End-stage renal disease epidemic in diabetics: is there light at the end of the tunnel? Nephrol Dial Transplant 2013;28:1073-1076. ArticlePubMed
- 47. Waanders F, Visser FW, Gans RO. Current concepts in the management of diabetic nephropathy. Neth J Med 2013;71:448-458. PubMed
- 48. Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med 2008;358:580-591. ArticlePubMed
- 49. Esnault VL, Ekhlas A, Delcroix C, Moutel MG, Nguyen JM. Diuretic and enhanced sodium restriction results in improved antiproteinuric response to RAS blocking agents. J Am Soc Nephrol 2005;16:474-481. ArticlePubMed
- 50. Sato A, Hayashi K, Naruse M, Saruta T. Effectiveness of aldosterone blockade in patients with diabetic nephropathy. Hypertension 2003;41:64-68. ArticlePubMed
- 51. Bjornstad P, Cherney D, Maahs DM. Early diabetic nephropathy in type 1 diabetes: new insights. Curr Opin Endocrinol Diabetes Obes 2014;21:279-286. PubMedPMC
- 52. de Zeeuw D, Akizawa T, Audhya P, Bakris GL, Chin M, Christ-Schmidt H, Goldsberry A, Houser M, Krauth M, Lambers Heerspink HJ, McMurray JJ, Meyer CJ, Parving HH, Remuzzi G, Toto RD, Vaziri ND, Wanner C, Wittes J, Wrolstad D, Chertow GM. BEACON Trial Investigators. Bardoxolone methyl in type 2 diabetes and stage 4 chronic kidney disease. N Engl J Med 2013;369:2492-2503. ArticlePubMedPMC
- 53. Mima A, Qi W, King GL. Implications of treatment that target protective mechanisms against diabetic nephropathy. Semin Nephrol 2012;32:471-478. ArticlePubMedPMC
- 54. Chung S, Park CW. Role of peroxisome proliferator-activated receptor alpha in diabetic nephropathy. Diabetes Metab J 2011;35:327-336. ArticlePubMedPMC
- 55. Fineberg D, Jandeleit-Dahm KA, Cooper ME. Diabetic nephropathy: diagnosis and treatment. Nat Rev Endocrinol 2013;9:713-723. ArticlePubMedPDF
- 56. Higgins GC, Coughlan MT. Mitochondrial dysfunction and mitophagy: the beginning and end to diabetic nephropathy? Br J Pharmacol 2014;171:1917-1942. ArticlePubMedPMC
- 57. Mima A. Inflammation and oxidative stress in diabetic nephropathy: new insights on its inhibition as new therapeutic targets. J Diabetes Res 2013;2013:248563ArticlePubMedPMCPDF
REFERENCES
Fig. 1The prevalence of chronic kidney disease (CKD) in Korea, Japan, China, USA, and Australia in 2008.


Fig. 2The prevalence (A) and incidence (B) of end-stage renal disease (ESRD) from 1986 to 2012 among Korean adults from Insan Memorial Dialysis Registry, 2012 [6]. (C) The prevalence of ESRD in various countries including Korea, Japan, China, USA, and Australia. p.m.p., per million people.
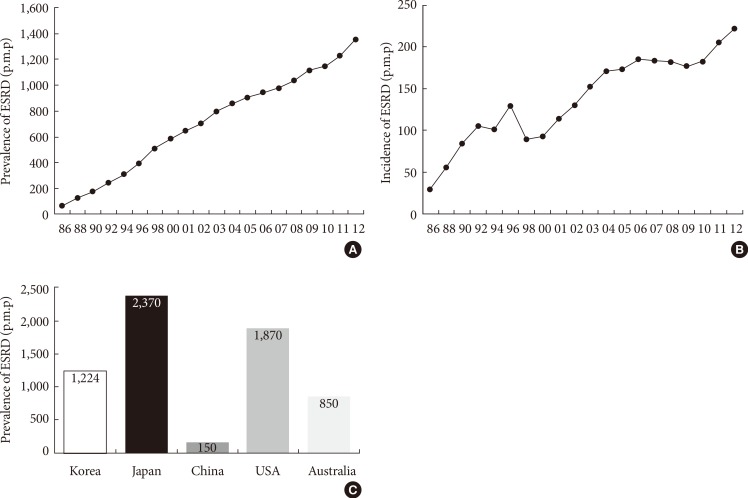
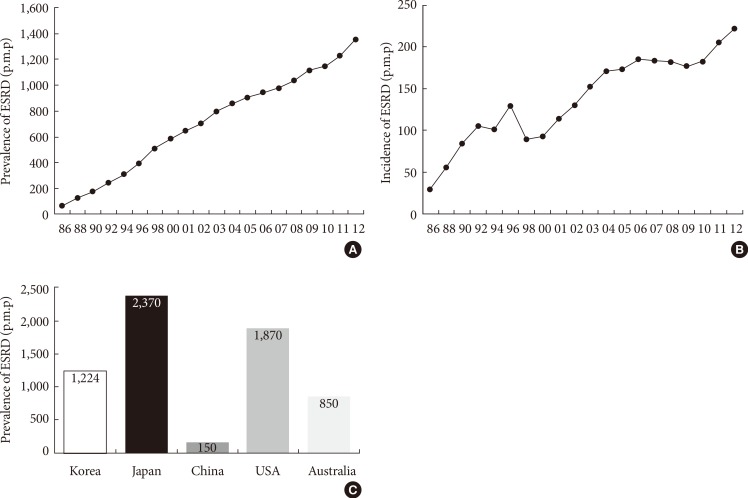
Fig. 3(A) Four major causes of end-stage renal disease (ESRD) in Korean adult patients who initiated renal replacement therapy each year among Korean adults from Insan Memorial Dialysis Registry, 2012 [6]. (B) The incidence of diabetic nephropathy (DN) as a cause of ESRD in various countries including Korea, Japan, China, USA, and Australia in 2011. HBP, hypertensive nephropathy; CGN, chronic glomerulonephritis; CD, cystic disease.


Figure & Data
References
Citations
Citations to this article as recorded by 

- N6-methyladenosine RNA methylation in diabetic kidney disease
Jiaan Huang, Fan Yang, Yan Liu, Yuehua Wang
Biomedicine & Pharmacotherapy.2024; 171: 116185. CrossRef - Association of advanced chronic kidney disease with diabetic retinopathy severity in older patients with diabetes: a retrospective cross-sectional study
Geun Woo Lee, Chul Ho Lee, Seong Gyu Kim
Journal of Yeungnam Medical Science.2023; 40(2): 146. CrossRef - Age at Mortality in Patients with Type 2 Diabetes Who Underwent Kidney Transplantation: An Analysis of Data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
Sun Ok Song, Eugene Han, Kang Ju Son, Bong-Soo Cha, Byung-Wan Lee
Journal of Clinical Medicine.2023; 12(9): 3160. CrossRef - Single‐cell RNA‐seq with spatial transcriptomics to create an atlas of human diabetic kidney disease
Duo Chen, Mingwei Shao, Yi Song, Gaofei Ren, Feng Guo, Xunjie Fan, Yanyan Wang, Wei Zhang, Guijun Qin
The FASEB Journal.2023;[Epub] CrossRef - Metabolomic profiling of amino acids study reveals a distinct diagnostic model for diabetic kidney disease
Jiao Wang, Chunyu Zhou, Qing Zhang, Zhangsuo Liu
Amino Acids.2023; 55(11): 1563. CrossRef - New insights into the mechanisms of diabetic kidney disease: Role of circadian rhythm and Bmal1
Zhimei Peng, Yanting Liang, Xueying Liu, Jie Shao, Nan Hu, Xinzhou Zhang
Biomedicine & Pharmacotherapy.2023; 166: 115422. CrossRef - Physical exercise as a friend not a foe in acute kidney diseases through immune system modulation
Ana Carolina Costanti-Nascimento, Leonilia Brelaz-Abreu, Elayne Bragança-Jardim, Welbert de Oliveira Pereira, Niels Olsen Saraiva Camara, Mariane Tami Amano
Frontiers in Immunology.2023;[Epub] CrossRef - Sodium-dependent glucose transporter 2 inhibitor alleviates renal lipid deposition and improves renal oxygenation levels in newly diagnosed type 2 diabetes mellitus patients: a randomized controlled trial
Li Zhang, Tongdan Wang, Yan Kong, Haizhen Sun, Yuling Zhang, Junmei Wang, Zhida Wang, Shan Lu, Pei Yu, Saijun Zhou
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Neutrophil lymphocyte ratio: a reliable biomarker for diabetic nephropathy?
Ashutosh Singh, Anshu Kumar Jha, Bipul Chandra Kalita, Dharmendra Kumar Jha, Yash Alok
International Journal of Diabetes in Developing Countries.2022; 42(3): 523. CrossRef - miR-193a as a potential mediator of WT-1/synaptopodin in the renoprotective effect of Losartan on diabetic kidney
Dan Gao, Pei Yu, Sanhui Jing, Chengcheng Yan, Dandan Ding, Yingjin Qiao, Ge Wu
Canadian Journal of Physiology and Pharmacology.2022; 100(1): 26. CrossRef - 3-Hydroxybutyrate Ameliorates the Progression of Diabetic Nephropathy
Jeeyoun Jung, Woo Yeong Park, Yun Jin Kim, Mikyung Kim, Misun Choe, Kyubok Jin, Ji Hae Seo, Eunyoung Ha
Antioxidants.2022; 11(2): 381. CrossRef - Emerging Role of Epitranscriptomics in Diabetes Mellitus and Its Complications
Xinqian Geng, Zheng Li, Ying Yang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Analysis of serum circulating MicroRNAs level in Malaysian patients with gestational diabetes mellitus
Sajad Jamalpour, Shamsul Mohd Zain, Reza Vazifehmand, Zahurin Mohamed, Yuh Fen Pung, Hesam Kamyab, Siti Zawiah Omar
Scientific Reports.2022;[Epub] CrossRef - Combined Single-Cell RNA-Seq and Spatial Transcriptomics Reveal an Atlas of Human Diabetic Kidney Disease
Duo Chen, Mingwei Shao, Yi Song, Gaofei Ren, Feng Guo, Xunjie Fan, Yanyan Wang, Wei Zhang, Guijun Qin
SSRN Electronic Journal .2022;[Epub] CrossRef - How to inhibit transforming growth factor beta safely in diabetic kidney disease
Yuxin Yang, Kexin Shi, Devang M. Patel, Fang Liu, Tieqiao Wu, Zhonglin Chai
Current Opinion in Nephrology & Hypertension.2021; 30(1): 115. CrossRef - Plasma miR-193a-3p can be a potential biomarker for the diagnosis of diabetic nephropathy
Yan Hong, Jidong Wang, Lai Zhang, Wenjuan Sun, Xuefang Xu, Kaiyue Zhang
Annals of Clinical Biochemistry: International Journal of Laboratory Medicine.2021; 58(2): 141. CrossRef - Severe hypoglycemia and the risk of end stage renal disease in type 2 diabetes
Jae-Seung Yun, Yong-Moon Park, Kyungdo Han, Hyung-Wook Kim, Seon-Ah Cha, Yu-Bae Ahn, Seung-Hyun Ko
Scientific Reports.2021;[Epub] CrossRef - Integrin β3 overexpression contributes to podocyte injury through inhibiting RhoA/YAP signaling pathway
Zhuo Li, Zhiwen Lian, Jianchao Ma, Li Zhang, Xingji Lian, Shuangxin Liu, Jianteng Xie, Zhonglin Feng, Ting Lin, Hong Zhang, Xinling Liang
Bioengineered.2021; 12(1): 1138. CrossRef - A Nonlinear Relationship Between Serum 25-Hydroxyvitamin D and Urine Albumin to Creatinine Ratio in Type 2 Diabetes: A Cross-Sectional Study in China
Qian Liang, Haofei Hu, Han Wu, Xuan Chen, Wei Wang, Ying Le, Shufen Yang, Lijing Jia
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 2581. CrossRef - Proteinuria as a significant predictive factor for the progression of carotid artery atherosclerosis in non-albuminuric type 2 diabetes
Young-eun Kim, Minyoung Lee, Yong-ho Lee, Eun Seok Kang, Bong-soo Cha, Byung-Wan Lee
Diabetes Research and Clinical Practice.2021; 181: 109082. CrossRef - USP9X prevents AGEs-induced upregulation of FN and TGF-β1 through activating Nrf2-ARE pathway in rat glomerular mesangial cells
Kaipeng Huang, Xilin Zhao
Experimental Cell Research.2020; 393(2): 112100. CrossRef - D-dimer Levels in Chronic Kidney Illness: A Comprehensive and Systematic Literature Review
Sahar Vahdat, Shahrzad Shahidi
Proceedings of the National Academy of Sciences, India Section B: Biological Sciences.2020; 90(5): 911. CrossRef - Circulating Expression Level of LncRNA Malat1 in Diabetic Kidney Disease Patients and Its Clinical Significance
Lian-ji Zhou, Da-wei Yang, Li-Na Ou, Xing-Rong Guo, Biao-liang Wu
Journal of Diabetes Research.2020; 2020: 1. CrossRef - Impact of chronic kidney disease definition on assessment of its incidence and risk factors in patients with newly diagnosed type 1 and type 2 diabetes in the UK: A cohort study using primary care data from the United Kingdom
Antonio González-Pérez, Maria E. Saéz, David Vizcaya, Marcus Lind, Luis A. García Rodríguez
Primary Care Diabetes.2020; 14(4): 381. CrossRef Resveratrol Inhibits Lipopolysaccharide-Induced Extracellular Matrix Accumulation and Inflammation in Rat Glomerular Mesangial Cells by SphK1/S1P2/NF-κB Pathway
Wenyan Gong, Jie Li, Wenying Chen, Fuzhen Feng, Yanhui Deng
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 4495. CrossRef- Effects of dietary iron restriction on kidney mitochondria function and oxidative stress in streptozotocin-diabetic rats
Donovan J. Peña-Montes, Maribel Huerta-Cervantes, Mónica Ríos-Silva, Xóchitl Trujillo, Christian Cortés-Rojo, Miguel Huerta, Alfredo Saavedra-Molina
Mitochondrion.2020; 54: 41. CrossRef - Significance of glycated LDL in different stages of diabetic nephropathy
Khalid Siddiqui, Teena P. George, Shaik Sarfaraz Nawaz, Maram Yaslam, Ebtehal Almogbel, Khalid Al-Rubeaan
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(1): 548. CrossRef - Prognostic value of visit-to-visit systolic blood pressure variability related to diabetic kidney disease among patients with type 2 diabetes
Zhe-Bin Yu, Jian-Bing Wang, Die Li, Xue-Yu Chen, Hong-Bo Lin, Kun Chen
Journal of Hypertension.2019; 37(7): 1411. CrossRef - Epigenetics and epigenomics in diabetic kidney disease and metabolic memory
Mitsuo Kato, Rama Natarajan
Nature Reviews Nephrology.2019; 15(6): 327. CrossRef - Resveratrol inhibits high glucose-induced activation of AP-1 and NF-κB via SphK1/S1P2 pathway to attenuate mesangial cells proliferation and inflammation
Yanhui Deng, Wenyan Gong, Qiang Li, Xian Wu, Liyao Wu, Xiaoxia Zheng, Wenying Chen, Heqing Huang
Journal of Functional Foods.2019; 55: 86. CrossRef - Predictive Factors for Efficacy of AST-120 Treatment in Diabetic Nephropathy: a Prospective Single-Arm, Open-Label, Multi-Center Study
You-Cheol Hwang, Se Won Kim, Kyu Yeon Hur, Bong-Soo Cha, In Joo Kim, Tae Sun Park, Sei Hyun Baik, Kun Ho Yoon, Kwan Woo Lee, In Kyu Lee, Moon-Kyu Lee
Journal of Korean Medical Science.2019;[Epub] CrossRef - Potential Diagnostic Hemorheological Indexes for Chronic Kidney Disease in Patients With Type 2 Diabetes
Hoyoon Lee, Wonwhi Na, Sang Bae Lee, Chul Woo Ahn, Jun Sung Moon, Kyu Chang Won, Sehyun Shin
Frontiers in Physiology.2019;[Epub] CrossRef - Comparing the Effect of Dipeptidyl-Peptidase 4 Inhibitors and Sulfonylureas on Albuminuria in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A Prospective Open-Label Study
Po-Chung Cheng, Shang-Ren Hsu, Jeng-Fu Kuo, Yun-Chung Cheng, Yu-Hsiu Liu, Shih-Te Tu
Journal of Clinical Medicine.2019; 8(10): 1715. CrossRef - Mechanisms of Adiponectin Action: Implication of Adiponectin Receptor Agonism in Diabetic Kidney Disease
Yaeni Kim, Cheol Whee Park
International Journal of Molecular Sciences.2019; 20(7): 1782. CrossRef - Regulatory T cells in acute and chronic kidney diseases
Rahul Sharma, Gilbert R. Kinsey
American Journal of Physiology-Renal Physiology.2018; 314(5): F679. CrossRef - Herba Artemisiae Capillaris Extract Prevents the Development of Streptozotocin-Induced Diabetic Nephropathy of Rat
Jianan Geng, Xiaoyan Yu, Chunyu Liu, Chengbo Sun, Menghuan Guo, Zhen Li, Yingli Jin, Yinggang Zou, Jinghua Yu
Evidence-Based Complementary and Alternative Medicine.2018; 2018: 1. CrossRef - Overview of the burden of illness and the role of once-weekly glucagon-like peptide-1 receptor agonist therapy in type 2 diabetes
Deborah Hinnen
Journal of the American Association of Nurse Practitioners.2018; 30(1): S4. CrossRef - Previous Exercise Training Reduces Markers of Renal Oxidative Stress and Inflammation in Streptozotocin-Induced Diabetic Female Rats
Liliany Souza de Brito Amaral, Cláudia Silva Souza, Rildo Aparecido Volpini, Maria Heloisa Massola Shimizu, Ana Carolina de Bragança, Daniele Canale, Antonio Carlos Seguro, Terezila Machado Coimbra, Amélia Cristina Mendes de Magalhães, Telma de Jesus Soar
Journal of Diabetes Research.2018; 2018: 1. CrossRef - Critical Shear Stress is Associated with Diabetic Kidney Disease in Patients with Type 2 Diabetes
Seung Min Chung, Jung Hyun Oh, Jun Sung Moon, Yu Kyung Kim, Ji Sung Yoon, Kyu Chang Won, Hyoung Woo Lee
Scientific Reports.2018;[Epub] CrossRef - Losartan Alleviates Renal Fibrosis and Inhibits Endothelial-to-Mesenchymal Transition (EMT) Under High-Fat Diet-Induced Hyperglycemia
Yufeng Yao, Yong Li, Xiaofei Zeng, Zheng Ye, Xia Li, Lu Zhang
Frontiers in Pharmacology.2018;[Epub] CrossRef - Association between poor psychosocial conditions and diabetic nephropathy in Japanese type 2 diabetes patients: A cross‐sectional study
Hiroyo Ninomiya, Naoto Katakami, Taka‐aki Matsuoka, Mitsuyoshi Takahara, Hitoshi Nishizawa, Norikazu Maeda, Michio Otsuki, Akihisa Imagawa, Hiroyasu Iso, Tetsuya Ohira, Iichiro Shimomura
Journal of Diabetes Investigation.2018; 9(1): 162. CrossRef - Urinary Microvesicle-Bound Uromodulin: A Potential Molecular Biomarker in Diabetic Kidney Disease
Neng-jun Lou, Yi-hong Ni, Hong-ying Jia, Jing-ti Deng, Lu Jiang, Feng-jie Zheng, Ai-li Sun
Journal of Diabetes Research.2017; 2017: 1. CrossRef - Renoprotective effect of fucoidan from Acaudina molpadioides in streptozotocin/high fat diet-induced type 2 diabetic mice
Shiwei Hu, Jinhui Wang, Jingfeng Wang, Shijie Li, Wei Jiang, Yu Liu
Journal of Functional Foods.2017; 31: 123. CrossRef - Analysis and comparison of the cost-effectiveness of statins according to the baseline low-density lipoprotein cholesterol level in Korea
Y. J. Jeong, H. Kim, S. J. Baik, T. M. Kim, S. J. Yang, S.-H. Lee, J.-H. Cho, H. Lee, H. W. Yim, I. Y. Choi, K.-H. Yoon, H.-S. Kim
Journal of Clinical Pharmacy and Therapeutics.2017; 42(3): 292. CrossRef - Visualization of kidney fibrosis in diabetic nephropathy by long diffusion tensor imaging MRI with spin-echo sequence
Jun-Ya Kaimori, Yoshitaka Isaka, Masaki Hatanaka, Satoko Yamamoto, Naotsugu Ichimaru, Akihiko Fujikawa, Hiroshi Shibata, Akira Fujimori, Sosuke Miyoshi, Takashi Yokawa, Kagayaki Kuroda, Toshiki Moriyama, Hiromi Rakugi, Shiro Takahara
Scientific Reports.2017;[Epub] CrossRef - Rutin suppresses high glucose-induced ACTA2 and p38 protein expression in diabetic nephropathy
Chun-Shan Han, Kai Liu, Ning Zhang, Shi-Wen Li, Hai-Cheng Gao
Experimental and Therapeutic Medicine.2017; 14(1): 181. CrossRef - Emodin self-emulsifying platform ameliorates the expression of FN, ICAM-1 and TGF-β1 in AGEs-induced glomerular mesangial cells by promoting absorption
Jiani Huang, Wenyan Gong, Zhiquan Chen, Junying Huang, Qiuhong Chen, Heqing Huang, Chunshun Zhao
European Journal of Pharmaceutical Sciences.2017; 99: 128. CrossRef - New therapeutic agents in diabetic nephropathy
Yaeni Kim, Cheol Whee Park
The Korean Journal of Internal Medicine.2017; 32(1): 11. CrossRef - Urine clusterin/apolipoprotein J is linked to tubular damage and renal outcomes in patients with type 2 diabetes mellitus
Sang Soo Kim, Sang Heon Song, Jong Ho Kim, Yun Kyung Jeon, Bo Hyun Kim, Min‐Cheol Kang, Sung Wan Chun, Soo Hyun Hong, Michelle Chung, Yong Ki Kim, In Joo Kim, Young‐Bum Kim
Clinical Endocrinology.2017; 87(2): 156. CrossRef - Treatment of diabetic kidney disease: current and future targets
Mi-Kyung Kim
The Korean Journal of Internal Medicine.2017; 32(4): 622. CrossRef - Sphingosine kinase 1 mediates AGEs-induced fibronectin upregulation in diabetic nephropathy
Cheng Chen, Wenyan Gong, Changzheng Li, Fengxiao Xiong, Shaogui Wang, Junying Huang, Yu Wang, Zhiquan Chen, Qiuhong Chen, Peiqing Liu, Tian Lan, Heqing Huang
Oncotarget.2017; 8(45): 78660. CrossRef - Comparison between Atorvastatin and Rosuvastatin in Renal Function Decline among Patients with Diabetes
Eugene Han, Gyuri Kim, Ji-Yeon Lee, Yong-ho Lee, Beom Seok Kim, Byung-Wan Lee, Bong-Soo Cha, Eun Seok Kang
Endocrinology and Metabolism.2017; 32(2): 274. CrossRef - Glycemic Management of Patients Undergoing Dialysis
Mi-Kyung Kim
The Journal of Korean Diabetes.2016; 17(3): 164. CrossRef - Probucol in Albuminuric Type 2 Diabetes Mellitus Patients on Renin–Angiotensin System Blockade
Sang-Man Jin, Kyung Ah Han, Jae Myung Yu, Tae Seo Sohn, Sung Hee Choi, Choon Hee Chung, Ie Byung Park, Eun Jung Rhee, Sei Hyun Baik, Tae Sun Park, In-Kyu Lee, Seung-Hyun Ko, You-Cheol Hwang, Bong Soo Cha, Hyoung Woo Lee, Moon-Suk Nam, Moon-Kyu Lee
Arteriosclerosis, Thrombosis, and Vascular Biology.2016; 36(10): 2108. CrossRef - MicroRNA-27a promotes renal tubulointerstitial fibrosis via suppressing PPARγ pathway in diabetic nephropathy
Xiaoyan Hou, Jianwei Tian, Jian Geng, Xiao Li, Xun Tang, Jun Zhang, Xiaoyan Bai
Oncotarget.2016; 7(30): 47760. CrossRef - Lipoprotein(a) predicts a new onset of chronic kidney disease in people with Type 2 diabetes mellitus
J.‐S. Yun, Y.‐B. Ahn, K.‐H. Song, K.‐D. Yoo, Y.‐M. Park, H.‐W. Kim, S.‐H. Ko
Diabetic Medicine.2016; 33(5): 639. CrossRef - Metabolic biomarkers for chronic kidney disease
Marc Breit, Klaus M. Weinberger
Archives of Biochemistry and Biophysics.2016; 589: 62. CrossRef - Effect of Sodium-Glucose Co-Transporter 2 Inhibitor, Dapagliflozin, on Renal Renin-Angiotensin System in an Animal Model of Type 2 Diabetes
Seok Joon Shin, Sungjin Chung, Soo Jung Kim, Eun-Mi Lee, Young-Hye Yoo, Ji-Won Kim, Yu-Bae Ahn, Eun-Sook Kim, Sung-Dae Moon, Myung-Jun Kim, Seung-Hyun Ko, Kwang-Hyun Baek
PLOS ONE.2016; 11(11): e0165703. CrossRef - Renoprotective Effect of Gemigliptin, a Dipeptidyl Peptidase-4 Inhibitor, in Streptozotocin-Induced Type 1 Diabetic Mice
Gwon-Soo Jung, Jae-Han Jeon, Mi Sun Choe, Sung-Woo Kim, In-Kyu Lee, Mi-Kyung Kim, Keun-Gyu Park
Diabetes & Metabolism Journal.2016; 40(3): 211. CrossRef - Beneficial effects of previous exercise training on renal changes in streptozotocin-induced diabetic female rats
Liliany S de Brito Amaral, Fernanda A Silva, Vicente B Correia, Clara EF Andrade, Bárbara A Dutra, Márcio V Oliveira, Amélia CM de Magalhães, Rildo A Volpini, Antonio C Seguro, Terezila M Coimbra, Telma de J Soares
Experimental Biology and Medicine.2016; 241(4): 437. CrossRef - Adenosine monophosphate–activated protein kinase in diabetic nephropathy
Yaeni Kim, Cheol Whee Park
Kidney Research and Clinical Practice.2016; 35(2): 69. CrossRef - Estimated Glucose Disposal Rate (eGDR) – A Marker for the Assessment of Insulin Resistance in Type 1 Diabetes Mellitus
Mihaela L. Bîcu, Daniel Bîcu, Sigina Gârgavu, Magdalena Sandu, Mihaela I. Vladu, Diana Clenciu, Eugen Moţa, Maria Moţa
Romanian Journal of Diabetes Nutrition and Metabolic Diseases.2016; 23(2): 177. CrossRef - Polydatin attenuates AGEs-induced upregulation of fibronectin and ICAM-1 in rat glomerular mesangial cells and db/db diabetic mice kidneys by inhibiting the activation of the SphK1-S1P signaling pathway
Cheng Chen, Kaipeng Huang, Jie Hao, Junying Huang, Zhiying Yang, Fengxiao Xiong, Peiqing Liu, Heqing Huang
Molecular and Cellular Endocrinology.2016; 427: 45. CrossRef - Glycated albumin and the risk of micro- and macrovascular complications in subjects with Type 1 Diabetes
Hye-jin Yoon, Yong-ho Lee, So Ra Kim, Tyler Hyungtaek Rim, Eun Young Lee, Eun Seok Kang, Bong-Soo Cha, Hyun Chul Lee, Byung-Wan Lee
Cardiovascular Diabetology.2015;[Epub] CrossRef - Tripterygium Glycosides Tablet Ameliorates Renal Tubulointerstitial Fibrosis via the Toll-Like Receptor 4/Nuclear Factor Kappa B Signaling Pathway in High-Fat Diet Fed and Streptozotocin-Induced Diabetic Rats
Ze-jun Ma, Xiao-na Zhang, Li Li, Wei Yang, Shan-shan Wang, Xin Guo, Pei Sun, Li-ming Chen
Journal of Diabetes Research.2015; 2015: 1. CrossRef - The association between abnormal heart rate variability and new onset of chronic kidney disease in patients with type 2 diabetes: A ten-year follow-up study
Jae-Seung Yun, Yu-Bae Ahn, Ki-Ho Song, Ki-Dong Yoo, Hyung-Wook Kim, Yong-Moon Park, Seung-Hyun Ko
Diabetes Research and Clinical Practice.2015; 108(1): 31. CrossRef - Finerenone: third-generation mineralocorticoid receptor antagonist for the treatment of heart failure and diabetic kidney disease
Licette CY Liu, Elise Schutte, Ron T Gansevoort, Peter van der Meer, Adriaan A Voors
Expert Opinion on Investigational Drugs.2015; 24(8): 1123. CrossRef - Effects of pentoxifylline on proteinuria and glucose control in patients with type 2 diabetes: a prospective randomized double-blind multicenter study
Seung Jin Han, Hae Jin Kim, Dae Jung Kim, Seung Soo Sheen, Choon Hee Chung, Chul Woo Ahn, Se Hwa Kim, Yong-Wook Cho, Seok Won Park, Soo-Kyung Kim, Chul Sik Kim, Kyung Wook Kim, Kwan Woo Lee
Diabetology & Metabolic Syndrome.2015;[Epub] CrossRef - Proteomic Profile in Glomeruli of Type-2 Diabetic KKAy Mice using 2-Dimensional Differential Gel Electrophoresis
Lining Wang
Medical Science Monitor.2014; 20: 2705. CrossRef

 KDA
KDA PubReader
PubReader Cite
Cite