Insulin Resistance, Non-Alcoholic Fatty Liver Disease and Type 2 Diabetes Mellitus: Clinical and Experimental Perspective
Article information
Abstract
It has been generally accepted that insulin resistance (IR) and reduced insulin secretory capacity are the basic pathogenesis of type 2 diabetes mellitus (T2DM). In addition to genetic factors, the persistence of systemic inflammation caused by obesity and the associated threat of lipotoxicity increase the risk of T2DM. In particular, the main cause of IR is obesity and subjects with T2DM have a higher body mass index (BMI) than normal subjects according to recent studies. The prevalence of T2DM with IR has increased with increasing BMI during the past three decades. According to recent studies, homeostatic model assessment of IR was increased compared to that of the 1990s. Rising prevalence of obesity in Korea have contributed to the development of IR, non-alcoholic fatty liver disease and T2DM and cutting this vicious cycle is important. My colleagues and I have investigated this pathogenic mechanism on this theme through clinical and experimental studies over 20 years and herein, I would like to summarize some of our studies with deep gratitude for receiving the prestigious 2023 Sulwon Award.
Highlights
· Insulin resistance, obesity, and inflammation contribute to type 2 diabetes pathogenesis
· An effective treatment for NASH necessitates a multi-targeted approach
The Sulwon Award for Scientific Achievement is the Korean Diabetes Association’s highest scientific award and honors an individual who has excellently contributed to the progress in the field of diabetes and metabolism. The Sulwon Award is named after an emeritus professor, Eung Jin Kim, who founded Korean Diabetes Association. Prof. Won-Young Lee received the 15th Sulwon Award at the 36th Spring Congress of Korean Diabetes Association, May 11 to 13 in 2023 at Gwangju, Korea.
INTRODUCTION
The process that begins with insulin resistance (IR) due to various causes and eventually leads to a decrease in the insulin secretion capacity is accepted as the basic concept for the development of type 2 diabetes mellitus (T2DM) [1]. Although previous studies were based on data from the 1990s, compared to Western populations, the severity of obesity rate and IR (based on euglycemic clamp studies) in Koreans with T2DM were relatively low [2,3]. However, the overall prevalence of obesity in Koreans continues to rise, and in particular, the prevalence of stage 3 or higher morbid obesity has nearly tripled over the past 10 years [4]. These changes lead to an increase in IR, which may appear in a form similar to the developmental mechanism of Western diabetic patients [5,6]. Furthermore, rising prevalence of obesity in Korea has contributed to the increasing incidence of cardiovascular diseases (CVD), non-alcoholic fatty liver disease (NAFLD) in addition to T2DM [7], and cutting this vicious cycle is important because a large cohort study of Koreans found that the long-term increase in mortality is related to prediabetes as well as T2DM [8]. NAFLD has recently undergone a new definition and change in terminology, called metabolic dysfunction-associated fatty liver disease [9] and is very closely cross-talked with IR [10]. Most importantly, NAFLD is emerging as an independent risk factor for CVD [11,12]. Our hospital has a large cohort called the Kangbuk Samsung Health Study (KSHS), through which retrospective and prospective studies could be conducted. Millions of participants have participated in these cohorts, making that an invaluable tool in longitudinal research to study the nature or associations of disease. Together with my colleagues, I have been studying about this theme through clinical and experimental studies over 20 years and herein, I would like to summarize and introduce some of our works (Fig. 1).
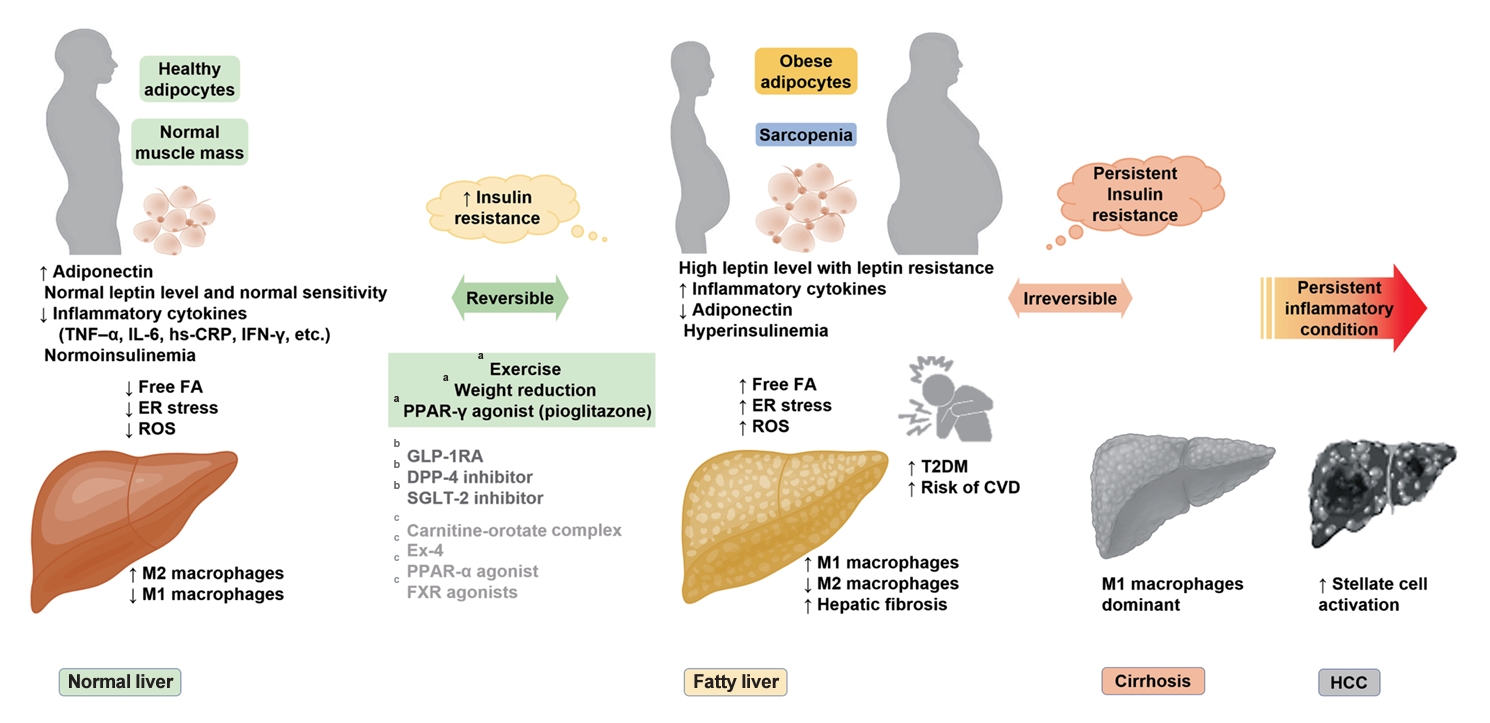
Schematic representation of the pathophysiology in insulin resistance associated with metabolic disorders and progression to non-alcoholic fatty liver disease and type 2 diabetes mellitus (T2DM). TNF-α, tumor necrosis factor-α; IL-6, interleukin-6; hsCRP, high-sensitivity C-reactive protein; IFN-γ, interferon-γ; FA, fatty acids; ER, endoplasmic reticulum; ROS, reactive oxygen species; PPAR, peroxisome proliferator-activated receptor; GLP-1RA, glucagon-like peptide-1 receptor agonist; DPP-4, dipeptidyl peptidase-4; SGLT-2, sodium-glucose cotransporter-2; Ex-4, exendin-4; FXR, farnesoid X receptor; CVD, cardiovascular disease; HCC, hepatocellular carcinoma. aAbsolutely, bProbably, cPossibly.
IR STATUS IN KOREANS
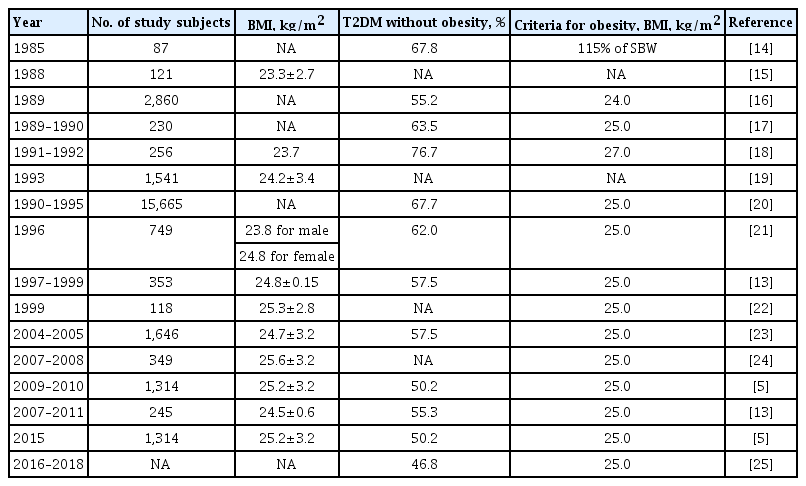
It is agreed that one of the main causes of IR is obesity. Subjects with T2DM have a higher body mass index (BMI) than normal subjects according to numerous studies [6]. The prevalence of T2DM with IR has increased with increasing BMI during the past three decades (Table 1) [5,13-25]. According to a study from the 2000s, homeostatic model assessment of insulin resistance (HOMA-IR) was increased compared to that of the 1990s [13]. However, parameters of insulin secretion (oral disposition index, insulinogenic index) did not change in Korean T2DM [6]. This suggests that the role of IR in the pathogenesis of Korean T2DM has enlarged during past decade. There were two cross-sectional studies that reported that the main pathophysiology in Korean T2DM was IR. Kim et al. [23] performed a short insulin tolerance test and found that the prevalence of IR was 70.6% through a normoglycemic-hyperinsulinemic clamp study. In another study reported by Son et al. [5], the prevalence of IR (HOMA-IR >2.5) was 59.5%.
Interestingly, we reported a study examining the spectrum of insulin sensitivity in a large sample of Korean adults [26]. The aims were to find the range of values for insulin sensitivity indexes and to determine cutoff levels of HOMA-IR conferring the increased risk for metabolic syndrome. Subjects (n=83,186) were analyzed among apparently healthy person who do not take any medication of T2DM, hypertension or dyslipidemia. By using receiver operating characteristic (ROC) curves, the fasting serum insulin and HOMA levels were compared and the insulin and HOMA values at the point on the ROC curve closest to 100% sensitivity and 100% specificity to detect metabolic syndrome were 9.7 and 2.43 µU/mL, respectively. It was the first try to determine cutoff values for IR indexes above which the risk of metabolic syndrome is increased. This kind of study could be used to assess the IR in epidemiologic studies. It seems undesirable to focus on only one of IR and insulin secretion in the pathogenesis of T2DM. Most patients of T2DM have both IR and insulin secretory defect. If IR appears in people who are genetically susceptible to have low insulin secretory function, and if β-cells can not compensate for IR appropriately, the people will develop T2DM. IR contributes to develop T2DM, and Koreans become T2DM easily with a relatively low BMI status compared to Caucasians. The increased prevalence of obesity and IR could contribute to the increased risk of T2DM during the past three decades in Korea. The preceding evidence shows that although IR is a contributing factor in the development of T2DM in Koreans, defects in insulin secretion are the determining factor.
IR AND MORTALITY IN KOREANS
We investigated whether IR could impact on mortality and inflammation could influence the association of IR and mortality in 165,849 general population in Korea [27]. The study was conducted on 1,417,325.6 person-years over a mean follow-up period of more than 8 years, and IR status was based on HOMA-IR (≥75%) and inflammatory status was based on high-sensitivity C-reactive protein (hs-CRP ≥2.0 mg/L). In this study, we found systemic inflammation can have a role to predict the allcause and cancer-related mortality risks, independent of the IR status. This trend was especially prominent in cancer-related mortality. Although IR could not impact on the mortality in Koreans, observation over the extended period could result in another finding and this needs to be studied. We undertook another longitudinal mortality study in which baseline glycemic status could impact later mortality in over 241,499 Korean adults by analyzing KSHS [8]. IR starts along before the hyperglycemia develops and even the subjects with prediabetes have higher risk for mortality. Baseline glycemic status and 7 years later mortality was assessed, and we found that subjects with T2DM had higher all-cause mortality significantly than normoglycemic subjects after multivariable adjustment. Cancer mortality was also higher in subjects with T2DM. When considering these differences in mortality according to glycemia was prominent in this short observation period, these differences could enlarge over the extended period. Therefore, careful blood glucose management and screening for cancer and cardiovascular complications are important in patients with T2DM.
OBESITY, IR, AND PROGRESSION OF NAFLD
The reason why the increasing prevalence of obesity in Korea is of clinical interest is because obesity induces a systemic inflammatory status and is associated with worsening IR [28]. In particular, IR is more affected by fat distribution than simple obesity, and an increase in visceral fat is related to intrahepatic IR as well as peripheral IR [29,30]. Adiponectin, which is secreted from adipocytes and is associated with protective effects against metabolic abnormalities and CVD, is inversely proportional to the amount of fat in the abdomen and liver, and this result is also closely related to peripheral and intrahepatic IR [31,32]. Activation of proinflammatory cytokines such as tumor necrosis factor-α (TNF-α), CRPs, interleukin-6, plasminogen activation factor inhibitor-1, and leptin has been understood as a core pathophysiology in the mechanism by which obesity (including severe subcutaneous fat) causes systemic inflammation [33-36], which ultimately leads to IR and T2DM [37]. In these process, activation of the nuclear factor-κB (NF-κB) pathway and c-Jun NH2-terminal kinase (JNK) pathway due to endoplasmic reticulum (ER) stress, reactive oxygen species, and ceramide was found to play a underlying key role [38-43].
IR and NAFLD are cross-talked with each other [10], and the relationship may be independent of the severity of obesity [44,45]. IR has been regarded as the culprit behind the development of NAFLD [46-48]. Among the sources of fatty acids for triacylglycerol (TG) synthesis: diet, lipolysis, and hepatic de novo lipogenesis (DNL), the largest source of TG synthesis in NAFLD patients, under dietary control, is free fatty acid (FFA) from lipolysis [49]. When the anti-lipolytic effect of insulin is inhibited under IR condition, FFA is excessively produced [50]. And hyperinsulinemia caused by IR further increases DNL. In this process, activation of sterol receptor binding protein 1c (SREBP-1c) is important, and hyperinsulinemia is a condition that promotes SREBP-1c [51-53]. On the other hand, forkhead box protein A2 (FOXA2), which is activated under low insulin level, promotes lipid metabolism and fatty acid oxidation, but plays the opposite role in hyperinsulinemia [54]. This adaptation process in the early stages of IR promotes steatosis and increases the liver mitochondrial respiration rate during this period [55]. However, if IR persists and progresses to the non-alcoholic steatohepatitis (NASH) stage, such effects disappear. Moreover, when TG synthesis is disrupted, hepatocyte damage occurs due to excessive fatty acid oxidation [56]. On the other hand, some studies show that fatty liver itself, induced by various causes, is a factor that worsens IR [57,58]. FFA excess influx into the liver induces activation of protein kinase C-δ (PKC-δ), which is believed to trigger hepatic IR through insulin receptor phosphorylation [59]. In this process, activation of NF-κB and JNK pathways through PKC-θ and Toll-like receptor (TLR) activation is also involved [60-62]. In animal models, mice with fatty liver induced by SREBP-1c overexpression and inhibition of fatty acid oxidation showed systemic IR [63,64]. Recent studies have shown that lipogenic substrates induce an increase in DNL precursors and enzymes that induce steatosis of liver through carbohydrate response element-binding protein (ChREBP) activation [65]. Furthermore, it has been reported that the composition, structure, and metabolic processes of lipid droplets (LDs) play an important role in the progression of NAFLD [66]. In advanced NAFLD (fibrosis or NASH), hepatic macrophages, especially proinflammatory M1 Kupffer cells stimulated by TLR ligands and interferon-γ, act as key pathological mediators.
As is well known, prevention of NAFLD and fibrosis progression is clinically very important. We reported the clinical significance of visceral-to-subcutaneous abdominal fat ratio (VSR) in the development of NAFLD as well as fibrosis progression based on a study of 7,465 adults [67]. Liver fibrosis was assessed based on fibrosis-4 (FIB-4) score and aspartate aminotransferase-to-platelet ratio index, and the severity of fibrosis was classified as low, indeterminate, or high. VSR assessed by abdominal computed tomography was significantly related with the prevalence of NAFLD and risk of liver fibrosis. We also reported the association of weight variability and risk of NAFLD in 30,708 Korean adults [68]. Weight gain is closely related with increased IR and some studies suggested that repeated weight gain or loss is related with increased morbidity in various diseases [69]. During 4 years’ observation period, high weight variability was significantly associated with new development of NAFLD regardless of baseline weight status. Targeting to reduce weight variability can be tried to prevent the development of NAFLD. Although many clinical studies dealing with this theme have been reported [70,71], clinical studies to find the role of IR in the development of liver fibrosis is even scarce [72-76]. We reported interesting papers about the association of baseline IR status and new development of liver fibrosis, assessed by biomarkers. One study was about that baseline IR could impact later development of liver fibrosis [77], and another study was that changes in HOMA-IR during the 6-year follow-up period were associated with changes in liver fibrosis indices [78]. Although liver biopsy was not performed in our studies, it is probable that IR in human can be closed related with new development of liver fibrosis and it needs to be validated with liver biopsy studies. Weight gain may be a precipitating factor in the progression of hepatic steatosis to fibrosis. Additionally, changes in IR was associated with later development or progression of NAFLD in our cohort study.
CHARACTERISTICS OF NAFLD IN KOREANS
NAFLD and CVD are closely related, and we reported the significant relationships between severity of NAFLD and 10-year CVD risk calculated by Framingham risk score and pooled cohort equation (PCE) [79]. This finding suggests that NAFLD severity was an independent factor for ≥7.5% estimated CVD risk and that the PCE calculation may be appropriate when assessing 10-year CVD risk among individuals with NAFLD. We also reported the role of metabolic health in the development of NAFLD in a 4-year longitudinal study and found that metabolic health is more important than obesity in NAFLD [80]. Whether NAFLD might be an independent determinant of metabolic health apart from obesity has not yet been clarified. Therefore, we intended to compare the risk of NAFLD among subjects classified based on metabolic health and obesity status. This study suggests the importance of early and intensive lifestyle modification in metabolically unhealthy subject since a prolonged period of a metabolically unhealthy status could result in NAFLD and metabolic derangements. Another interesting finding was that subjects who were metabolically healthy at baseline but metabolically unhealthy after 4 years had a significantly higher risk of NAFLD compared to subjects who were metabolically unhealthy at baseline but metabolically healthy after 4 years. This result was consistent with previous findings that early intervention in metabolically unhealthy subjects can prevent NAFLD and metabolic abnormalities.
We further reported the relation of biomarkers and NAFLD in cross-sectional studies and longitudinal studies. Serum adipocyte-specific fatty acid binding protein was significantly associated with fatty liver index [81]. TNF-α was also related with later development of NAFLD in Korean adults [82]. The relationship between autonomic dysfunction and NAFLD was studied by our group because it is unclear although autonomic imbalance is related with an increased risk for metabolic disease [83]. A total of 33,899 participants without NAFLD who underwent health screening programs between 2011 and 2018 were enrolled. With a median follow-up of 5.7 years, low parasympathetic activity, and recently enhanced sympathetic activity might increase the risk of NAFLD. We also reported a study about the simple self-assessment score consists of age, sex, waist circumference, BMI, history of T2DM and dyslipidemia, alcohol intake, physical activity, and menopause status, which are independently associated with NAFLD, and this simple score could be a guide to identify individuals at high-risk of NAFLD [84]. And we studied the association between glomerular hyperfiltration (GHF) and the risk of NAFLD [85]. In a longitudinal study including 147,479 relatively healthy adults, we found that GHF (defined as age- and sex-specific estimated glomerular filtration rate above the 95th percentile) status was associated with future NAFLD development assessed using ultrasonography (US) and progression to fibrosis assessed using NAFLD fibrosis score and FIB-4. A recent study demonstrated the importance of leg-fat to total fat ratio for NAFLD risk in a nationwide survey [86], and another study reported the significance of a noninvasive liver fibrosis score (diabetes fibrosis score) which is more specific for patients with T2DM based on transient elastography [87].
Recent pharmacological treatments for NASH have been reviewed, and the implications of recent failures about NASH treatment highlight that targeting only one pathway or mechanism is not sufficient to improve NASH [88]. This underscores the need to find the common root of NASH progression and candidates that can modulate multiple pathways or disease cascades in NASH pathophysiology. And above all, we need to strengthen clinical research targeting Koreans.
ASSOCIATION OF NAFLD AND SARCOPENIA
Sarcopenia is reported to be independently related with steatohepatitis and hepatic fibrosis risk in NAFLD patients. Skeletal muscle is a main organ in which glucose metabolism through insulin is proceeded. Many epidemiologic studies and experimental studies show the relation between low muscle mass and increased IR. Thus, we can speculate that sarcopenia can promote IR and thus contribute to development of NAFLD. A recent longitudinal study reported an association between the persistent decline in appendicular muscle mass with aging and the risk of NAFLD [89]. Chronic inflammation also can increase the loss of muscle and inflammation in NAFLD can also promote sarcopenic process, thus activate the vicious cycle between sarcopenia and NAFLD. And the effect of sarcopenia on the liver fibrosis is reported to be higher in non-obese subjects than in obese subjects. NAFLD can be developed in subjects with low visceral adipose tissue, and it is frequently observed in Asian subjects [90]. We reported that regular exercise is associated with reduced risk of NAFLD independent of obesity in Korean adults [91]. Exercise and weight loss is a main strategy and physiologic approach to prevent and treat NAFLD [92]. More research is needed to assess the real relationship between sarcopenia and NAFLD.
ASSOCIATION OF NAFLD AND T2DM
NAFLD is regarded as an independent risk factor for T2DM and frequently precede before the development of T2DM. Prospective epidemiologic studies show that alanine transaminase (ALT) or gamma-glutamyl transferase is independently associated with new development of T2DM [93-95] and patients with NAFLD diagnosed by ultrasound have been reported to have a two-fold higher risk of T2DM later in life [96]. 78% of 129 subjects with NAFLD proven with liver biopsy developed glucose intolerance in 14-year prospective study and among them those with liver fibrosis had significantly higher risk for T2DM [97]. NAFLD can be developed from IR and NAFLD itself aggravated IR, thus increase the risk of T2DM [10]. IR can promote the adipose deposit to extra-hepatic organs, such as skeletal muscle and pancreas and it can affect insulin secretory capacity. We reported that hyperinsulinemia at baseline was associated with significantly increased risk for later development of NAFLD [46]. We undertook cross-sectional study among 99,969 subjects and found that NAFLD was significantly related with HOMA-IR and glycosylated hemoglobin in in nondiabetic individuals and this relationship was independent of BMI and other metabolic components [98]. Combined effect of IFG and NAFLD in the development of T2DM was reported in a longitudinal study among 7,849 subjects who underwent annual liver ultrasound for 5 years [99]. That means that NAFLD has an additive and independent effect on the development of T2DM under conditions of impaired insulin secretion. In the same vein, we reported that during the follow-up of 4 years, Korean subjects with the sustained NAFLD had 1.5 higher risk for new development of T2DM compared with those having never NAFLD, whereas the risk was not higher in the intermittent NAFLD group [100]. For this reason, there is a need to pay attention to patients with persistent NAFLD. We also reported the additive effect of NAFLD on new onset of T2DM in subjects with metabolic syndrome [101]. Additionally, we observed that subjects with both NAFLD on US and elevated liver enzymes had higher risk for developing T2DM [102]. Efforts for screening or predicting NAFLD or liver fibrosis in T2DM subjects have been tried. Performance analysis of fibrosis in subjects with NAFLD with or without T2DM was reported [103], and non-laboratory-based screening tool for NAFLD was reported in Koreans with T2DM [104].
T2DM in subjects with NAFLD is associated with about twofold higher risk of liver fibrosis, liver related death rate [105]. Subjects with T2DM commonly has abnormal liver function or US findings and even with normal liver function test, severity of NAFLD histologically proven is higher. American diabetes association recommends active surveillance for liver fibrosis when NAFLD is suspected in T2DM patients [106]. Hyperinsulinemia and chronic inflammation in T2DM can increase the risk of hepatocellular carcinoma (HCC). In England registry, NAFLD related HCC increased 10-fold for 10 years from 2000 to 2010 and the proportion of patients with metabolic risk factors such as T2DM or obesity was about 66% [107].
Efforts to improve NAFLD in T2DM with medication was attempted and more trials are needed to test efficacy. There are growing evidence supporting beneficial effects of dipeptidyl peptidase-4 (DPP-4) inhibitor, glucagon-like peptide-1 receptor agonists (GLP-1RAs) and sodium-glucose cotransporter-2 (SGLT-2) inhibitors on NAFLD [108]. While increasing amount of in vivo and in vitro research highlights the potential of DPP-4 inhibitors, GLP-1RAs and SGLT-2 inhibitors in NAFLD treatment, the clinical data demonstrating their efficacy in patients with NAFLD are limited [109,110]. We have proposed that carnitine-orotate complex has the potential to alleviate ALT and computed tomography-identified hepatic steatosis in patients with both T2DM and NAFLD [111].
EXPERIMENTAL PERSPECTIVE ON NAFLD
In our pursuit of understanding the pathogenesis of NAFLD and identifying potential pharmacological interventions, our research encompassed a series of experimental investigations. Initially, we examined the effects of exendin-4 (Ex-4) on sirtuin 1 (SIRT1) expression and its role in ameliorating hepatic steatosis, as described by Lee et al. [112] in this study titled ‘Exendin-4 improves steatohepatitis by increasing Sirt1 expression in high-fat diet-induced obese C57BL/6J mice.’ To elucidate whether Ex-4 modulates SIRT1 expression as a mechanistic basis for improving fatty liver, we conducted a series of experiments in high-fat diet-induced obese C57BL/6J mice and cell culture models. These investigations revealed that the upregulation of SIRT1 induced by Ex-4 treatment provided protection against high-fat diet-induced steatohepatitis, primarily through stimulation of fatty acid oxidation. In another study, we explored Ex-4’s potential to alleviate palmitate-induced ER stress through SIRT1 in HepG2 cells [113]. In this study, palmitate exposure led to an upregulation of ER stress markers (phospho-inositol-requiring transmembrane kinase/endoribonuclease 1α [P-IRE1α], activating transcription factor 6 [ATF6], X-box binding protein 1 [XBP1], CCAAT/enhancer-binding protein homologous protein [CHOP]), but Ex-4 administration effectively downregulated these markers and increased sarco/endoplasmic reticulum calcium ion ATPase 2b (SERCA2b) expression. Additionally, Ex-4 reduced hepatic expression of p53 up-regulated modulator of apoptosis (PUMA), BCL2 associated X (BAX), cytochrome c, and cleaved caspase-3. Importantly, blocking SIRT1 reversed these effects, highlighting the significance of SIRT1 in Ex-4’s protective mechanisms. In our experiments concerning fibroblast growth factor 21 (FGF21), suppressing FGF21 with siRNA in hepatocytes resulted in reduced expression of medium-chain acyl-coenzyme A dehydrogenase (MCAD) and peroxisome proliferator-activated receptor α (PPARα) [114]. Intriguingly, when we treated cells with Ex-4 and inhibited SIRT1 (but not SIRT6) via siRNA, it led to a decrease in FGF21 mRNA expression, while FGF21 inhibition did not impact SIRT1. These findings suggest that Ex-4 may ameliorate hepatic steatosis by enhancing SIRT1-mediated FGF21. Furthermore, the glycoproteins selenoprotein P (SEPP1) and fetuin-A, derived from the liver and circulating in the bloodstream, have emerged as potential biomarkers for IR and NAFLD. However, the influence of Ex-4 on the expression of these hepatokines, SEPP1 and fetuin-A, remains a subject of inquiry. Our experiments with HepG2 cells yielded compelling evidence indicating that Ex-4 significantly reduced the expression of hepatic SEPP1 and fetuin-A [115]. This reduction was attributed to the amelioration of palmitate-induced ER stress, orchestrated by adenosine monophosphate-activated protein kinase. Collectively, these results enhance our overall understanding of NAFLD and potential therapeutic strategies, providing valuable insights into the complex regulatory systems within hepatic physiology.
We also found that dulaglutide could decrease hepatic lipid accumulation by activating family with sequence similarity 3 member A (FAM3A) signaling pathway [116]. In this study, dulaglutide demonstrated significant reductions in hepatic lipid accumulation and suppression of genes linked to LD binding proteins, DNL, and TG synthesis in palmitic acid treated HepG2 cells. Additionally, Dulaglutide promoted lipolysis, fatty acid oxidation, and FAM3A expression, suggesting its potential therapeutic utility in NAFLD, mediated partly through GLP-1R-dependent upregulation of FAM3A.
In one study, the loss of farnesoid X receptor (FXR) in mice exacerbated atherosclerosis and hepatic steatosis, with a PPARα agonist partially reversing these conditions by modulating fatty acid metabolism-related gene expression [117]. Another in vitro investigation reveals that succinate acts as a signaling molecule in hepatic stellate cells, contributing to mitochondrial dysfunction [118]. This study also found that gemigliptin, a DPP-4 inhibitor, demonstrated potential in mitigating liver fibrosis by reducing fibrosis markers, abnormal cell proliferation, and improving mitochondrial function. These findings suggest potential therapeutic strategies for liver fibrosis.
CONCLUSIONS
Over recent decades, the world has observed a marked rise in obesity rates, leading to an increase in conditions like T2DM and its consequential complications, notably NAFLD. Contemporary research has illuminated the deep interrelationships between NAFLD and other significant health conditions, such as CVD and sarcopenia, highlighting the pressing need for effective NAFLD treatments. Our investigations into its molecular pathways and the pronounced effects of hepatic lipid accumulation have provided invaluable insights into this complex disease. While promising pharmacological options, including Ex-4, DPP-4 inhibitors, and GLP-1RAs (i.e., dulaglutide) have emerged, a significant gap remains in finding drugs with robust therapeutic effects in human clinical trials. An integrated strategy, combining pharmacological methods with lifestyle interventions, stands out as the most promising approach. As our understanding evolves, a comprehensive, integrative approach to managing not only NAFLD but also interrelated conditions like T2DM becomes increasingly crucial. Continued collaborative efforts in this direction are essential for improving patient outcomes worldwide.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
They were not involved in the review process of this article. Otherwise, there was no conflict of interest.
FUNDING
None
Acknowledgements
None