- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 47(5); 2023 > Article
-
Original ArticleGuideline/Fact Sheet Dyslipidemia Fact Sheet in South Korea, 2022
-
Eun-Sun Jin1*
 , Jee-Seon Shim2*
, Jee-Seon Shim2* , Sung Eun Kim3, Jae Hyun Bae4, Shinae Kang5, Jong Chul Won6, Min-Jeong Shin7, Heung Yong Jin8, Jenny Moon9, Hokyou Lee2, Hyeon Chang Kim2
, Sung Eun Kim3, Jae Hyun Bae4, Shinae Kang5, Jong Chul Won6, Min-Jeong Shin7, Heung Yong Jin8, Jenny Moon9, Hokyou Lee2, Hyeon Chang Kim2 , In-Kyung Jeong10
, In-Kyung Jeong10 , on Behalf of the Committee of Public Relation of the Korean Society of Lipid and Atherosclerosis
, on Behalf of the Committee of Public Relation of the Korean Society of Lipid and Atherosclerosis -
Diabetes & Metabolism Journal 2023;47(5):632-642.
DOI: https://doi.org/10.4093/dmj.2023.0135
Published online: August 2, 2023
1Department of Cardiology, Kyung Hee University Hospital at Gangdong, College of Medicine, Kyung Hee University, Seoul, Korea
10Department of Endocrinology and Metabolism, Kyung Hee University Hospital at Gangdong, College of Medicine, Kyung Hee University, Seoul, Korea
2Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea
3Division of Cardiology, Department of Internal Medicine, Kangdong Sacred Heart Hospital, College of Medicine, Hallym University, Seoul, Korea
4Department of Internal Medicine, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
5Department of Internal Medicine, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
6Department of Internal Medicine, Inje University Sanggye Paik Hospital, College of Medicine, Inje University, Seoul, Korea
7School of Biosystem and Biomedical Science, Korea University, Seoul, Korea
8Division of Endocrinology and Metabolism, Department of Internal Medicine, Jeonbuk National University Medical School, Jeonju, Korea
9Department of Public Health, Yonsei University Graduate School, Seoul, Korea
- In-Kyung Jeong https://orcid.org/0000-0001-7857-546X Department of Endocrinology and Metabolism, Kyung Hee University Hospital at Gangdong, College of Medicine, Kyung Hee University, 892 Dongnam-ro, Gangdong-gu, Seoul 05278, Korea E-mail: jik1016@naver.com
-
Hyeon Chang Kim
 Department of Preventive Medicine, Yonsei University College of Medicine, 50-1 Yonseiro, Seodaemun-gu, Seoul 03722, Korea E-mail: hckim@yuhs.ac
Department of Preventive Medicine, Yonsei University College of Medicine, 50-1 Yonseiro, Seodaemun-gu, Seoul 03722, Korea E-mail: hckim@yuhs.ac - *Eun-Sun Jin and Jee-Seon Shim contributed equally to this study as first authors.
Copyright © 2023 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
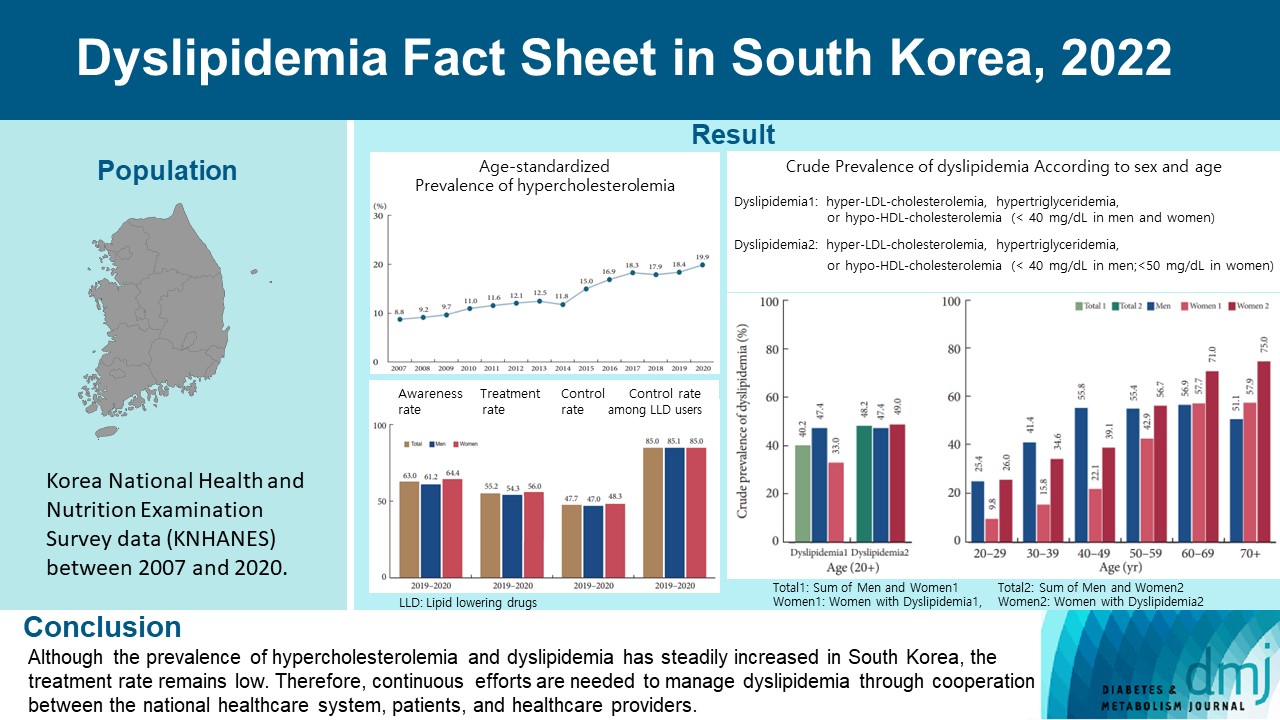
- This study aimed to investigate the prevalence and status of dyslipidemia management among South Korean adults, as performed by the Korean Society of Lipid and Atherosclerosis under the name Dyslipidemia Fact Sheet 2022.
-
Methods
- We analyzed the lipid profiles, age-standardized and crude prevalence, management status of hypercholesterolemia and dyslipidemia, and health behaviors among Korean adults aged ≥20 years, using the Korea National Health and Nutrition Examination Survey data between 2007 and 2020.
-
Results
- In South Korea, the crude prevalence of hypercholesterolemia (total cholesterol ≥240 mg/dL or use of a lipid-lowering drug) in 2020 was 24%, and the age-standardized prevalence of hypercholesterolemia more than doubled from 2007 to 2020. The crude treatment rate was 55.2%, and the control rate was 47.7%. The crude prevalence of dyslipidemia—more than one out of three conditions (low-density lipoprotein cholesterol ≥160 or the use of a lipid-lowering drug, triglycerides ≥200, or high-density lipoprotein cholesterol [HDL-C] [men and women] <40 mg/dL)—was 40.2% between 2016 and 2020. However, it increased to 48.2% when the definition of hypo-HDL-cholesterolemia in women changed from <40 to <50 mg/dL.
-
Conclusion
- Although the prevalence of hypercholesterolemia and dyslipidemia has steadily increased in South Korea, the treatment rate remains low. Therefore, continuous efforts are needed to manage dyslipidemia through cooperation between the national healthcare system, patients, and healthcare providers.
- Dyslipidemia is defined as elevated plasma concentrations of low-density lipoprotein cholesterol (LDL-C) or triglycerides (TG), a low plasma concentration of high-density lipoprotein cholesterol (HDL-C), or a combination of these features and is a major risk factor for cardiovascular disease, a leading cause of death in most countries [1,2]. Despite constant public education and improvement in awareness of dyslipidemia, management, and control rates have been insufficient [3].
- Hypercholesterolemia is defined as a total cholesterol (TC) level of >240 mg/dL, which is a major risk factor for cardiovascular disease. It can be measured regardless of diet; therefore, it is commonly used to compare the status of cholesterol metabolism diseases among countries. According to a recent World Health Organization report, hypercholesterolemia was approximately 39% in adults aged ≥25 years in 2008, and more than one-third of deaths due to ischemic heart disease or ischemic stroke were attributable to elevated plasma LDL-C levels [3].
- To evaluate national dyslipidemia statistics, including awareness, treatment rate, control rate, and health behaviors, the Korean Society of Lipid and Atherosclerosis has been publishing the Dyslipidemia Fact Sheet (DFS) since 2015. Previous DFS studies have reported a gradually increasing prevalence of hypercholesterolemia and dyslipidemia. It is necessary to update the prevalence trends, management status, and health behaviors of adults with dyslipidemia over time.
- This study (DFS 2022) aimed to investigate the lipid profiles, prevalence, and management of hypercholesterolemia or dyslipidemia, comorbidities, and health behaviors among Korean adults aged ≥20 years, using the Korea National Health and Nutrition Examination Survey (KNHANES) data between 2007 and 2020.
INTRODUCTION
- Data source and study participants
- We analyzed data from the KNHANES between 2007 and 2020. The KNHANES is a nationwide survey that assesses the health and nutritional status of Koreans and monitors trends in healthrelated risk factors and the prevalence and management of major chronic diseases in Korea [4]. The target population comprised non-institutionalized citizens aged ≥1 year residing in Korea, and the survey participants were sampled using a complex survey design. To represent the Korean population, sample weights were assigned to each participant by accounting for the sampling design, survey response, and post-stratification. Diverse information on socioeconomic status, health behaviors, anthropometric measures, health status (measured using biochemical and clinical profiles), and dietary intake was collected. Participants were limited to those aged ≥20 years, with fasting blood lipid measurements, and with information on physician diagnosis and treatment for dyslipidemia. The data was anonymized and provided at the website of the KNHANES of the Korea Centers for Disease Control and Prevention. The study protocol was approved by the Institutional Review Board of Yonsei University Health System, Seoul, Korea (approval 4- 2021-0940). National Health Insurance Service data are provided as personal information has been deleted, and the IRB has approved consent waivers. The Korean and English atlas versions of the “Dyslipidemia fact sheet in Korea 2022” are also available at https://lipid.or.kr/.
- Measurements and definitions
- Serum lipid concentrations such as TC, TG, LDL-C, and HDL-C were measured using blood samples after fasting for at least 8 hours. Since LDL-C measures were available only for some of the participants, the calculated values based on the Friedwald formula were used for those without direct measurement of LDL-C [5]. Non-HDL-C was derived by subtracting HDL-C from TC. Information on physicians’ diagnoses of diseases, medication use, and health behaviors was obtained through a health interview survey. Anthropometric measurements and dietary intake data were obtained through physical examinations and nutritional surveys, respectively.
- Hypercholesterolemia was defined as TC ≥240 mg/dL or the use of a lipid-lowering drug. The awareness rate was defined as the proportion of patients with physician-diagnosed hypercholesterolemia among all patients with hypercholesterolemia. The treatment rate was defined as the proportion of patients using lipid-lowering drugs for ≥20 days per month among those with hypercholesterolemia. The control rate was defined as follows: (1) the proportion of patients with TC <200 mg/dL among all patients with hypercholesterolemia and (2) the proportion of patients with TC <200 mg/dL among those on lipid-lowering medication for hypercholesterolemia.
- Hyper-LDL-cholesterolemia was defined as LDL-C ≥160 mg/dL or the use of a lipid-lowering drug. Hypertriglyceridemia was defined as TG ≥200 mg/dL. Hypo-HDL-cholesterolemia was defined as follows: HDL-C <40 mg/dL in both men and women (hypo-HDL-cholesterolemia 1) and HDL-C <40 mg/dL in men and <50 mg/dL in women (hypo-HDL-cholesterolemia 2).
- Dyslipidemia was defined as having at least one of the following conditions: hyper-LDL-cholesterolemia, hypertriglyceridemia, and hypo-HDL-cholesterolemia. In DFS 2022, we analyzed the prevalence of dyslipidemia in two ways according to two different definitions of hypo-HDL-cholesterolemia: dyslipidemia 1 as dyslipidemia with hypo-HDL-cholesterolemia 1 and dyslipidemia 2 as dyslipidemia with hypo-HDL-cholesterolemia 2.
- To evaluate the magnitude of dyslipidemia and the management status of blood lipids according to the presence of chronic conditions such as diabetes, hypertension, and obesity, we analyzed the KNHANES data from 2016 to 2020. Diabetes was defined as fasting glucose ≥126 mg/dL, glycosylated hemoglobin (HbA1c) ≥6.5%, previously diagnosed, or the use of glucose-lowering drugs or insulin. Prediabetes was defined as fasting glucose 100–125 mg/dL or HbA1c 5.7%–6.4%. Hypertension was defined as systolic blood pressure (SBP) ≥140 mm Hg, diastolic blood pressure (DBP) ≥90 mm Hg, or the use of blood pressure-lowering drugs, whereas prehypertension was defined as SBP 120–139 mm Hg or DBP 80–89 mm Hg. People were divided into four groups according to their body mass index: underweight (<18.5 kg/m2), normal weight (18.5–22.9 kg/m2), overweight (23.0–24.9 kg/m2), and obesity (≥25.0 kg/m2) [6]. Abdominal obesity was defined as a waist circumference ≥90 cm for men and ≥85 cm for women.
- The health behaviors of adults with dyslipidemia were evaluated using the KNHANES data between 2016 and 2018. Dietary intake was assessed using a 24-hour dietary recall. Dietary quality aspects, such as balanced, moderate, and adequate consumption, were evaluated using the components of the Korean Healthy Eating Index [7] provided by the Korea Disease Control and Prevention Agency. We defined balanced total energy intake as 75% to 125% of the energy requirement by sex and age. The recommended proportions of calorie intake were 7%–20% for protein, 56%–65% for carbohydrates, and 15%–30% for fat. Physical activity was measured using the Global Physical Activity Questionnaires and divided into two groups: aerobic physical activity (moderate-intensity activity for ≥2.5 hours, vigorous-intensity activity for ≥1.25 hours, or an equivalent combination of moderate- and vigorous-intensity activity over the past week) and inactivity. The smoking status was classified as current smoking, ex-smoking, or nonsmoking. Drinking was defined as the consumption of alcohol more than once per month in the past year.
- Statistical analysis
- All analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA), accounting for the sample weights assigned to the participants to represent the Korean population. To evaluate the magnitude of the prevalence and management of dyslipidemia, both crude and age-standardized rates were estimated. Age-standardized rates were calculated via the direct standardization method using the 2005 Korean population structure provided by the Population and Housing Census, Statistics Korea.
METHODS
Prevalence and management of hypercholesterolemia
Prevalence of dyslipidemia
Dyslipidemia in a specific population
Health behaviors among adults with dyslipidemia
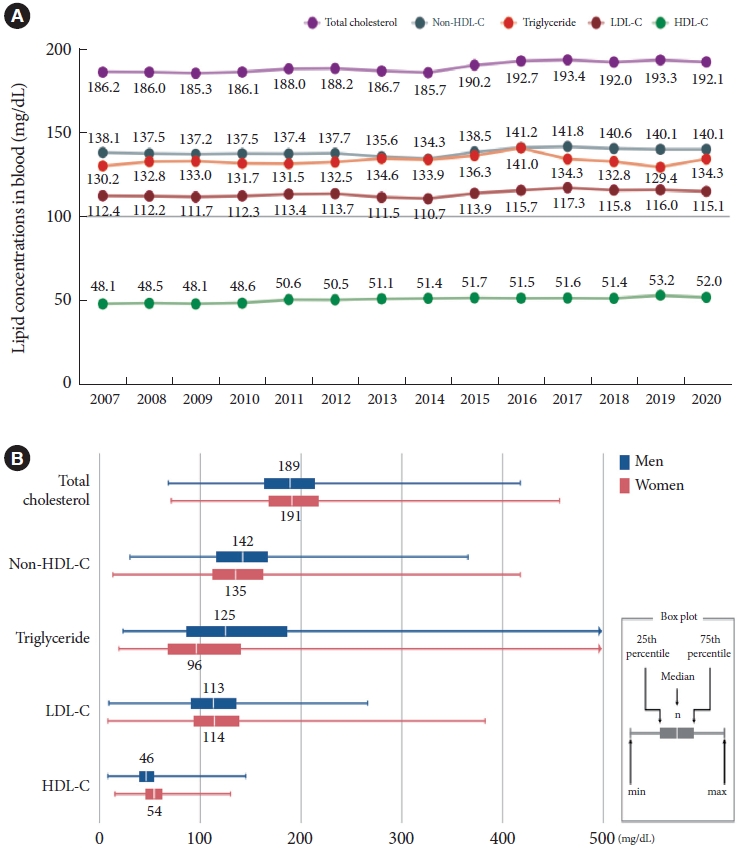
- Lipid profile in Korean adults
- Trends in the age-standardized mean concentrations of blood lipids are shown in Fig. 1A. In 2020, mean concentration of TC was 192.1 mg/dL, non-HDL-C was 140.1 mg/dL, TG was 134.3 mg/dL, LDL-C was 115.1 mg/dL, and HDL-C was 52 mg/dL.
- Blood lipid profiles were slightly different between men and women (Fig. 1B). Men had a higher median concentration of non-HDL-C (142 and 135 mg/dL in men and women, respectively) and TG (125 and 96 mg/dL in men and women, respectively) than women. The median HDL-C level was higher in women than in men (46 and 54 mg/dL in men and women, respectively).
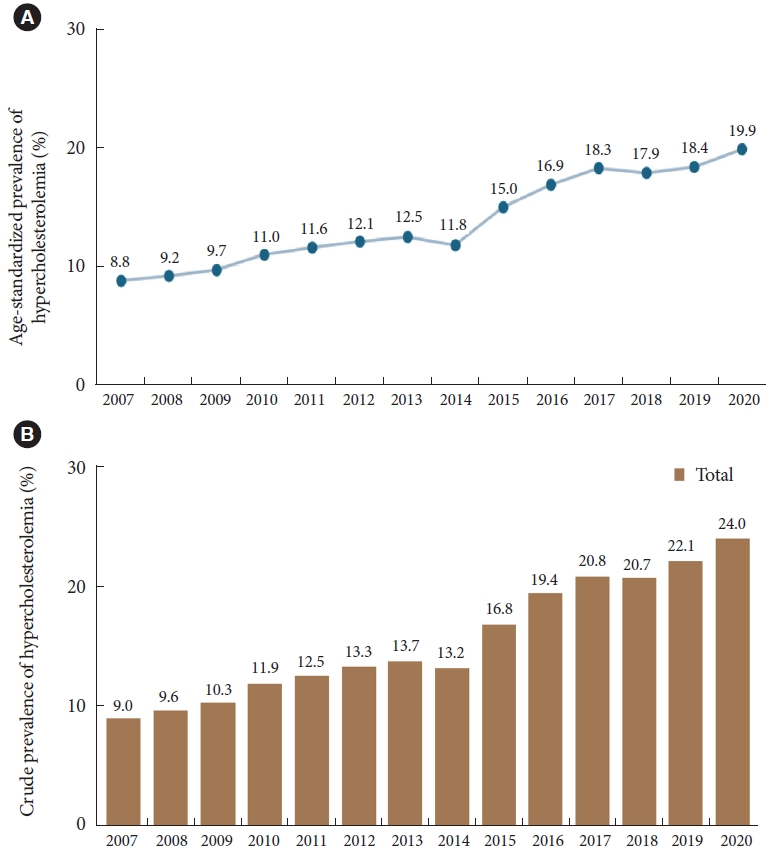
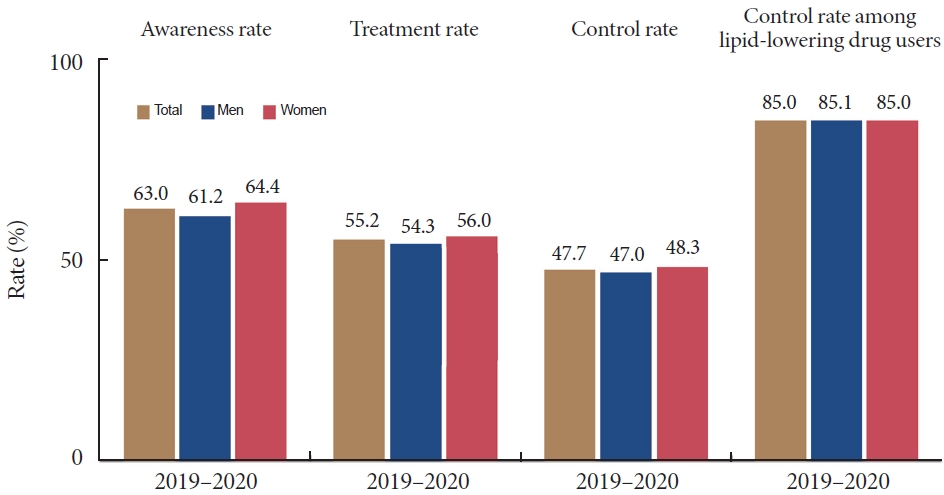
- Hypercholesterolemia
- The prevalence of hypercholesterolemia has steadily increased. The age-standardized prevalence of hypercholesterolemia in 2020 was 19.9%, doubling from 8.8% in 2007 (Fig. 2A). The crude prevalence of hypercholesterolemia in 2020 was 24.0% (Fig. 2B). The awareness, treatment, and control rates during 2019–2020 were 63.0%, 55.2%, and 47.7%, respectively. The control rate among lipid-lowering drug users was 85% (Fig. 3).
- The awareness, treatment, and control rates in people with hypercholesterolemia and control rates among lipid-lowering drug users consistently increased from 38.3%, 25.8%, 19.1%, and 72.4%, respectively, in 2007–2009 to 63.0%, 55.2%, 47.7%, and 85.0% in 2019–2020 (Supplementary Fig 1). The crude prevalence, awareness, treatment, and control rates have been consistently slightly higher in women than in men throughout the years since 2007 (Supplementary Fig 2). In particular, the control rate among adults treated with lipid-lowering drugs differed according to sex; however, this difference decreased. The previous control rate was higher in men than in women (78.6% and 68.2% in men and women, respectively) between 2007 and 2009. However, currently, the control rate is almost the same in both sexes: 85.1% in men and 85% in women (Supplementary Fig 2D).
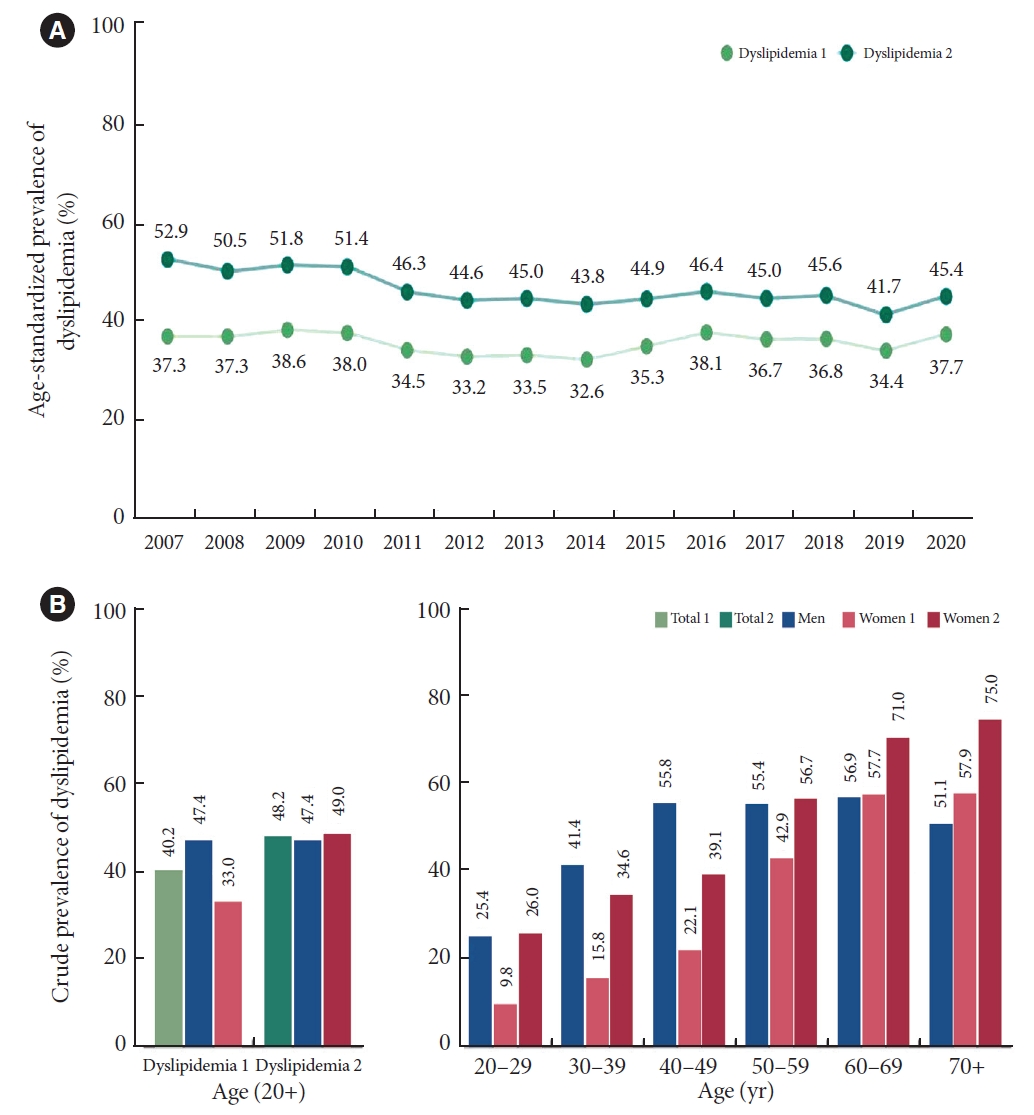
- Dyslipidemia
- The age-standardized prevalence in 2020 was 37.7% for dyslipidemia 1 and 45.4% for dyslipidemia 2 (Fig. 4A). The crude prevalence during 2016–2020 was 40.2% and 48.2% for dyslipidemia 1 and dyslipidemia 2, respectively (Fig. 4B). The prevalence of dyslipidemia 1 in women was lower than that in men (47.4% and 33.0% in men and women, respectively); however, the prevalence of dyslipidemia 2 in women was similar to that in men (47.4% and 49.0% in men and women, respectively) (Fig. 4B).
- When we analyzed the prevalence rate based on dyslipidemia 1, the prevalence in women in their 20s to 50s was lower than that in men, but the prevalence gap between men and women decreased when we analyzed the prevalence rate based on dyslipidemia 2. In the 30 to 49 years age group, the prevalence of dyslipidemia 2 was higher in men; however, in the 60s age group, the sex trend started to reverse. In particular, the prevalence of dyslipidemia in men was steady in their 40s (55.8%) to 60s (56.9%) and then decreased to 51.1% in their 70s. However, in the case of women, it continued to increase with age, with the prevalence of dyslipidemia 2 reaching 75% in their 70s (Fig. 4B).
- The age-standardized prevalence of hyper-LDL-cholesterolemia steadily increased from 8.7% in 2007 to 19.1% in 2020 (Supplementary Fig 3A). Based on the data from 2016 to 2020, nearly one in five Korean adults had hyper-LDL-cholesterolemia (crude prevalence, 20.4%). The prevalence of hyper-LDL-cholesterolemia in both sexes reversed since their 50s (Supplementary Fig 3B). In their 40s, the prevalence of hyper-LDL-cholesterolemia in men was 20.0%, almost twice as high as that in women (11.4%). However, the prevalence in women in their 60s was 45.9%, which was 1.57 times higher than that in men (29.1%) (Supplementary Fig 3B).
- The age-standardized prevalence of hypertriglyceridemia gradually increased from 15.3% in 2007 to 16.8% in 2016, decreased to 13.6% in 2019, and then increased again to 15% in 2020 (Supplementary Fig 4A). The prevalence of hypertriglyceridemia was much higher in men between their 30s and 50s; the most substantial difference being in their 40s (31.6% in men and 7.5% in women), which was nearly four times higher in men than in women. The difference decreased gradually with age and was reversed in their 70s (Supplementary Fig 4B).
- The age-standardized prevalence in 2020 was 15.5% for hypo-HDL-cholesterolemia 1 and 26.8% for hypo-HDL-cholesterolemia 2 (Supplementary Fig 5A). The crude prevalence of hypo-HDL-cholesterolemia 1 was much higher in men throughout all ages than in women (24.3% and 9.1% in men and women, respectively), but the prevalence of hypo-HDL-cholesterolemia 2 in women was higher than that in men (24.3% and 34.6% in men and women, respectively). The difference was maximized in their 70s, with a prevalence of 53.1% in women and 29.3% in men (Supplementary Fig 5B).
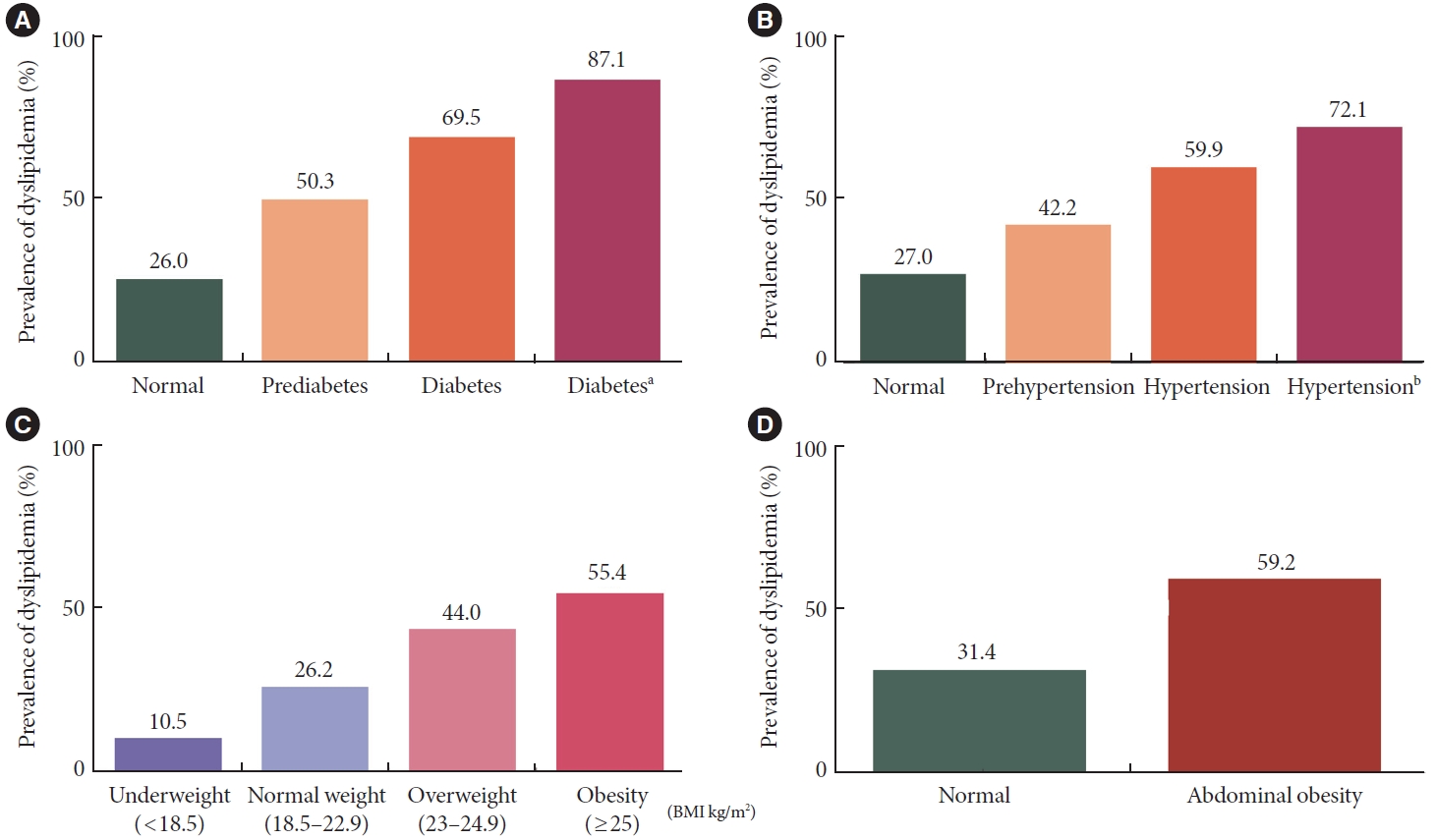
- Dyslipidemia in specific populations
- The prevalence of dyslipidemia differs according to the glucose metabolism status. In individuals with normal glucose levels, the prevalence of dyslipidemia was 26%. However, the prevalence of dyslipidemia increases as the blood glucose levels increase. During the prediabetic status, defined as fasting glucose 100–125 mg/dL or HbA1c is 5.7%–6.4%, the prevalence of dyslipidemia was 50.3%. The prevalence of dyslipidemia increased up to 69.5% in people with diabetes. When we used LDL-C ≥100 mg/dL instead of LDL-C ≥160 mg/dL to define dyslipidemia in people with diabetes, the prevalence increased to 87.1% (Fig. 5A).
- Similar to diabetes, the prevalence of dyslipidemia increases with blood pressure. In normotensive individuals, the prevalence of dyslipidemia was 27%, and in individuals with prehypertension, the prevalence was 42.2%. In people with hypertension, the prevalence was high (59.9%). When we applied the criteria of LDL-C ≥130 mg/dL instead of LDL-C ≥160 mg/dL in patients with hypertension, the prevalence of dyslipidemia increased to 72.1% (Fig. 5B).
- The prevalence of dyslipidemia was 10.5%, 26.2%, 44%, and 55.4% in the underweight, normal weight, overweight, and obesity groups, respectively (Fig. 5C). Abdominal obesity was strongly associated with dyslipidemia. Among people with normal-ranged abdominal circumference, 31.4% had dyslipidemia, but among those with abdominal obesity, 59.2% had dyslipidemia (Fig. 5D).
- Health behaviors
- Among adults with dyslipidemia, 49.7% of men and 48.7% of women had a balanced total energy intake. Protein intake was balanced in 85.5% of men and 91% of women, whereas carbohydrate intake was balanced only in 29.2% of men and 22.8% of women. Balanced fat intake was observed in 53.6% of men and 44.7% of women (Supplementary Fig 6A).
- Only 26.8% of men and 20.4% of women with dyslipidemia ate vegetables more than 8 servings/day (for women aged ≥65 years, more than 6 servings/day). Approximately 62.2% of men and 72.5% of women with dyslipidemia consumed an adequate amount of saturated fat (<7% of the total energy). Approximately 40% of men and 30% of women with dyslipidemia consumed more saturated fat than was recommended (Supplementary Fig 6B).
- Among individuals with dyslipidemia, 54.3% of men and 61.9% of women did not meet the recommendations for physical activity. Moreover, 39.5% of men and 5.5% of women smoked cigarettes, and 71.6% of men and 32.1% of women consumed alcohol (Supplementary Fig 6C).
- In Korean adults, the total energy intake increased until the mid-2010s and decreased again to 2,281 kcal for men and 1,615 kcal for women in 2020. Carbohydrate intake decreased gradually, whereas fat intake increased in both sexes (Supplementary Fig 7A). Cigarette smoking decreased gradually, with age-standardized prevalence peaking at 48.3 in 2010 and then decreasing to 34.0 in 2020, which was attributable to the decreased prevalence in men (Supplementary Fig 7B).
RESULTS
Hyper-LDL-cholesterolemia
Hypertriglyceridemia
Hypo-HDL-cholesterolemia
Diabetes mellitus
Hypertension
Obesity
- In the DFS reported in 2015, the prevalence of dyslipidemia among adults aged ≥30 years was 47.8%. In the DFS reported in 2018, the prevalence of hypercholesterolemia and dyslipidemia in adults aged ≥30 years was 19.9% and 40.5%, respectively, in 2016. In the DFS reported in 2020, the prevalence of dyslipidemia among adults aged ≥20 years was 38.4%.
- The most recent DFS (2022) revealed an increasing prevalence of hypercholesterolemia. Almost one-fourth of adults were diagnosed with hypercholesterolemia in Korea in 2020: 22.9% and 25% in men and women, respectively. When hypo-HDL-cholesterolemia was defined as <50 mg/dL in women, the prevalence of dyslipidemia in women increased, which was similar to that in men (47.4% and 49% in men and women, respectively).
- The leading cause is the increase in hypercholesterolemia due to the westernization of nutrition and lifestyle. However, the increase in the intake of cholesterol-lowering drugs is also a cause of the increase in the prevalence of hypercholesterolemia because the definition of hypercholesterolemia contains the concept of ‘taking lipid-lowering drugs.’ Because of this, the LDL-C level did not increase significantly, although the prevalence of hypercholesterolemia increased.
- Notably, awareness of hypercholesterolemia is also increasing. There were notable sex differences in the earlier periods (2013–2015 and 2016–2018), and awareness and treatment rates showed a relatively steeper increase in men than in women during 2019 to 2020. The control rate of hypercholesterolemia has significantly increased from 19.1% to 47.7% over the past 10 years. However, there are still limitations to the control rates, with more than half of the adults with hypercholesterolemia without adequate control.
- Considering that the ideal goals for hypercholesterolemia have been increasingly changing (Korean guidelines for the management of dyslipidemia 5th), there are two things to note [8,9]. First, as treatment targets become stricter, the control rate of dyslipidemia is expected to decrease gradually. Second, owing to the current standstill of those reaching the target blood cholesterol level, the community should be educated regarding aggressive drug treatment strategies, including the combinatorial use of drugs with different mechanisms.
- The prevalence of dyslipidemia differed from that of hypercholesterolemia. The age-standardized prevalence of dyslipidemia 1 and dyslipidemia 2 slightly decreased from 2007 to 2019 and then increased in 2020 (Fig. 4A). This trend is probably attributable to the decrease in physical activity and increase in obesity due to social distancing owing to SARS-CoV-2 pandemic [10]. This trend shows a similar pattern for hypo-HDL-cholesterolemia and hypertriglyceridemia. Both hypo-HDL-cholesterolemia and hypertriglyceridemia are atherogenic dyslipidemias caused by insulin resistance, which can increase the incidence of metabolic syndrome and the risk of cardiovascular diseases.
- In DFS 2022, unlike the previous DFS editions, the epidemiologic characteristics of dyslipidemia were additionally analyzed by defining hypo-HDL-cholesterolemia as <50 mg/dL in women, unlike in men. The definition of hypo-HDL-cholesterolemia differs according to sex. It has been proven in many countries, besides Korea, that HDL-C levels are approximately 10 mg/dL higher in women than in men. When defining metabolic syndrome, the criteria for hypo-HDL-cholesterolemia are also defined differently in men and women [11].
- Thus, when the hypo-HDL-cholesterolemia criteria were equally applied to men and women at <40 mg/dL, the prevalence of dyslipidemia in women was underestimated (Supplementary Fig 5). Therefore, in DFS 2022, the prevalence of dyslipidemia was further analyzed according to the two different criteria for hypo-HDL-cholesterolemia (dyslipidemia 1 vs. dyslipidemia 2). The difference in the prevalence of dyslipidemia between men and women was significantly reduced when dyslipidemia 2 was applied compared with when dyslipidemia 1 was applied (Fig. 4). The prevalence of dyslipidemia was higher in men than in women in their 30s to 40s, but this was reversed after their 50s. Remarkably, hypo-HDL-cholesterolemia and growing hyper-LDL-cholesterolemia and hypertriglyceridemia as women age are the main factors contributing to this trend.
- The crude prevalence of dyslipidemia in men was similar to that in men in their 40s to 60, decreasing slightly in their 70s. However, in women, the prevalence of dyslipidemia 2 in their 70s is particularly high, reaching 75%. This was mainly due to the high incidence of hyper-LDL-cholesterolemia (40.7%) and hypo-HDL-cholesterolemia (53.1%) among older women. The prevalence of hyper-LDL-cholesterolemia in women was almost half as low as that in men before their 50s, but it increased sharply from 11.4% in their 40s, 31.2% in their 50s, and up to 45.9% in their 60s, while the prevalence in men was 29.1% in their 60s.
- Menopause significantly impacts cholesterol metabolism, contributing considerably to the increase in cardiovascular risk in postmenopausal women [12]. In the case of hypercholesterolemia, although we did not confirm the control rate in older individuals in this study, the overall control rate in women was 48.3%, which is less than half; therefore, it is necessary to encourage diagnosis and treatment of dyslipidemia in postmenopausal women. In men, the frequency of hyper-LDL-cholesterolemia and hypertriglyceridemia is high among relatively young people in their 40s and 50s, which is a sex hormone-dependent characteristic that and also likely related to unhealthy eating and drinking habits.
- The prevalence of dyslipidemia among adults with comorbidities, including diabetes, hypertension, and obesity, remained stable when the analysis was extended from 2007–2018 to 2007–2020 [3]. The proportions of adults with dyslipidemia increased across the spectrum of normoglycemia to diabetes, normal blood pressure to hypertension, and underweight to obesity. Diabetes mellitus, hypertension, and obesity are important cardiovascular risk factors, and the risk increases when accompanied by dyslipidemia. To lower this risk, the target level of LDL-C control is lower than that of the general population, which is why more patients with those conditions are taking cholesterol-lowering drugs resulting in the diagnosis of hypercholesterolemia.
- Adults with diabetes had a better distribution of LDL-C levels than those without diabetes, suggesting that many adults with diabetes were taking lipid-lowering agents. However, only 51.8% of adults with diabetes achieved lipid control of LDL-C <100 mg/dL for those without cardiovascular disease, based on the Korean guidelines for the management of dyslipidemia [1,13]. In contrast, a comparable distribution of LDL-C levels was observed between adults with and without hypertension. Approximately 60% of adults with dyslipidemia had hypertension and thus were at least at moderate risk of cardiovascular disease. The achievement of LDL-C <130 mg/dL was slightly higher in adults with hypertension (71.0%) than in those without hypertension (66.7%). Obesity and abdominal obesity are important risk factors for dyslipidemia. In Korea, the prevalence of obesity and abdominal obesity has steadily increased over the last decade [10]. Given the pathophysiological mechanisms, the increasing trend in obesity and abdominal obesity may affect the prevalence and control rate of dyslipidemia in the future [14]. Therefore, comprehensive management of dyslipidemia and its comorbidities is needed to reduce the risk of metabolic and cardiovascular complications.
- In this DFS, we could not directly compare the eating and exercise patterns of people with and without dyslipidemia. Since this was a cross-sectional study, the survey may have been conducted in a state in which people diagnosed with dyslipidemia thoroughly improved their diet and exercise habits after the diagnosis. In this study, the lifestyles of people with dyslipidemia were analyzed and compared with the recommended lifestyles. Protein intake was appropriate; however, the intake of carbohydrates, vegetables, and saturated fatty acids required correction. Both men and women lacked physical activity, and smoking and drinking remained major health problems in men.
- In conclusion, DFS 2022 showed that the prevalence of hypercholesterolemia has steadily increased in Korea, and the treatment rate remains low. Moreover, when hypo-HDL-cholesterolemia was defined as <50 mg/dL in women, the prevalence of dyslipidemia was high (up to 48.2%). Prevalence of dyslipidemia places a heavy burden on the affected individuals and society. Therefore, continuous efforts are needed to manage dyslipidemia through cooperation between the national healthcare system, patients, and healthcare providers. We hope that DFS 2022 will provide a better understanding of the characteristics of dyslipidemia, help enhance public awareness, and encourage adequate treatment.
DISCUSSION
SUPPLEMENTARY MATERIALS
Supplementary Fig. 1.
Supplementary Fig. 2.
Supplementary Fig. 3.
Supplementary Fig. 4.
Supplementary Fig. 5.
Supplementary Fig. 6.
Supplementary Fig. 7.
-
CONFLICTS OF INTEREST
Hyeon Chang Kim has been statistical advisor of the Diabetes & Metabolism Journal since 2022. He was not involved in the review process of this article. Otherwise, there was no conflict of interest.
-
AUTHOR CONTRIBUTIONS
Conception or design: E.S.J., J.S.S., H.C.K., I.K.J.
Acquisition, analysis, or interpretation of data: E.S.J., J.S.S., S.E.K., J.H.B., S.K., J.C.W., M.J.S., H.Y.J., J.M., H.L.,H.C.K., I.K.J.
Drafting the work or revising: E.S.J., J.S.S., S.E.K., J.H.B., S.K.
Final approval of the manuscript: H.C.K., I.K.J.K.
-
FUNDING
None
NOTES
-
Acknowledgements
- This paper is published in duplicate in the Diabetes & Metabolism Journal and the Journal of Lipid and Atherosclerosis. We thank the Korean Society of Lipid and Atherosclerosis for supporting this study.
- This study received support from the Korean Society of Lipids and Atherosclerosis, with contributions from the following members of the Board of Directors in 2022: Myung-A Kim, Jae Bum Kim, Donghoon Choi, Chul Sik Kim, Soon Jun Hong, Dae Jung Kim, Sang-Hak Lee, Jaetaek Kim, In-Kyung Jeong, Sung Hee Choi, Hyun-Jae Kang, Byung Jin Kim, Sungha Park, Young Mi Park, Sang-Hyun Kim, Min-Jeong Shin, Kee-Ho Song, Seong-Hoon Choi, Ung Kim, and Young Joon Hong.


- 1. Rhee EJ, Kim HC, Kim JH, Lee EY, Kim BJ, Kim EM, et al. 2018 Guidelines for the management of dyslipidemia in Korea. J Lipid Atheroscler 2019;8:78-131.ArticlePubMedPMCPDF
- 2. World Health Organization. Fact sheets: cardiovascular diseases (CVDs). Available from: https://www.who.int/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (cited 2023 Jul 10).
- 3. Cho SMJ, Lee H, Lee HH, Baek J, Heo JE, Joo HJ, et al. Dyslipidemia fact sheets in Korea 2020: an analysis of nationwide population-based data. J Lipid Atheroscler 2021;10:202-9.ArticlePubMedPMCPDF
- 4. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol 2014;43:69-77.ArticlePubMedPMC
- 5. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972;18:499-502.ArticlePubMedPDF
- 6. Seo MH, Lee WY, Kim SS, Kang JH, Kang JH, Kim KK, et al. 2018 Korean Society for the Study of Obesity guideline for the management of obesity in Korea. J Obes Metab Syndr 2019;28:40-5.ArticlePubMedPMC
- 7. Yun S, Park S, Yook SM, Kim K, Shim JE, Hwang JY, et al. Development of the Korean Healthy Eating Index for adults, based on the Korea National Health and Nutrition Examination Survey. Nutr Res Pract 2022;16:233-47.ArticlePubMedPMCPDF
- 8. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 2020;41:111-88.ArticlePubMedPDF
- 9. Yang YS, Kim HL, Kim SH, Moon MK. Lipid management in Korean people with type 2 diabetes mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement. Diabetes Metab J 2023;47:1-9.ArticlePubMedPMCPDF
- 10. Yang YS, Han BD, Han K, Jung JH, Son JW; Taskforce Team of the Obesity Fact Sheet of the Korean Society for the Study of Obesity. Obesity fact sheet in Korea, 2021: trends in obesity prevalence and obesity-related comorbidity incidence stratified by age from 2009 to 2019. J Obes Metab Syndr 2022;31:169-77.ArticlePubMedPMC
- 11. Wilson PW, Grundy SM. The metabolic syndrome: a practical guide to origins and treatment: Part II. Circulation 2003;108:1537-40.ArticlePubMed
- 12. Williams CM. Lipid metabolism in women. Proc Nutr Soc 2004;63:153-60.ArticlePubMed
- 13. Hur KY, Moon MK, Park JS, Kim SK, Lee SH, Yun JS, et al. 2021 Clinical practice guidelines for diabetes mellitus of the Korean Diabetes Association. Diabetes Metab J 2021;45:461-81.ArticlePubMedPMCPDF
- 14. Lingvay I, Sumithran P, Cohen RV, le Roux CW. Obesity management as a primary treatment goal for type 2 diabetes: time to reframe the conversation. Lancet 2022;399:394-405.ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Oxidative Balance Score and New-Onset Type 2 Diabetes Mellitus in Korean Adults without Non-Alcoholic Fatty Liver Disease: Korean Genome and Epidemiology Study-Health Examinees (KoGES-HEXA) Cohort
Mid-Eum Moon, Dong Hyuk Jung, Seok-Jae Heo, Byoungjin Park, Yong Jae Lee
Antioxidants.2024; 13(1): 107. CrossRef - Comparison of metabolic and neurological comorbidities in Asian patients with psoriasis and atopic dermatitis
Hee Joo Yang, Mi Young Lee, Jeong Hyeon Lee, Chang Jin Jung, Woo Jin Lee, Chong Hyun Won, Mi Woo Lee, Joon Min Jung, Sung Eun Chang
Scientific Reports.2024;[Epub] CrossRef - Effect of Adding Apolipoprotein B Testing on the Prevalence of Dyslipidemia and Risk of Cardiovascular Disease in the Korean Adult Population
Rihwa Choi, Sang Gon Lee, Eun Hee Lee
Metabolites.2024; 14(3): 169. CrossRef - Exploring Utilization and Establishing Reference Intervals for the Apolipoprotein B Test in the Korean Population
Rihwa Choi, Sang Gon Lee, Eun Hee Lee
Diagnostics.2023; 13(20): 3194. CrossRef

 KDA
KDA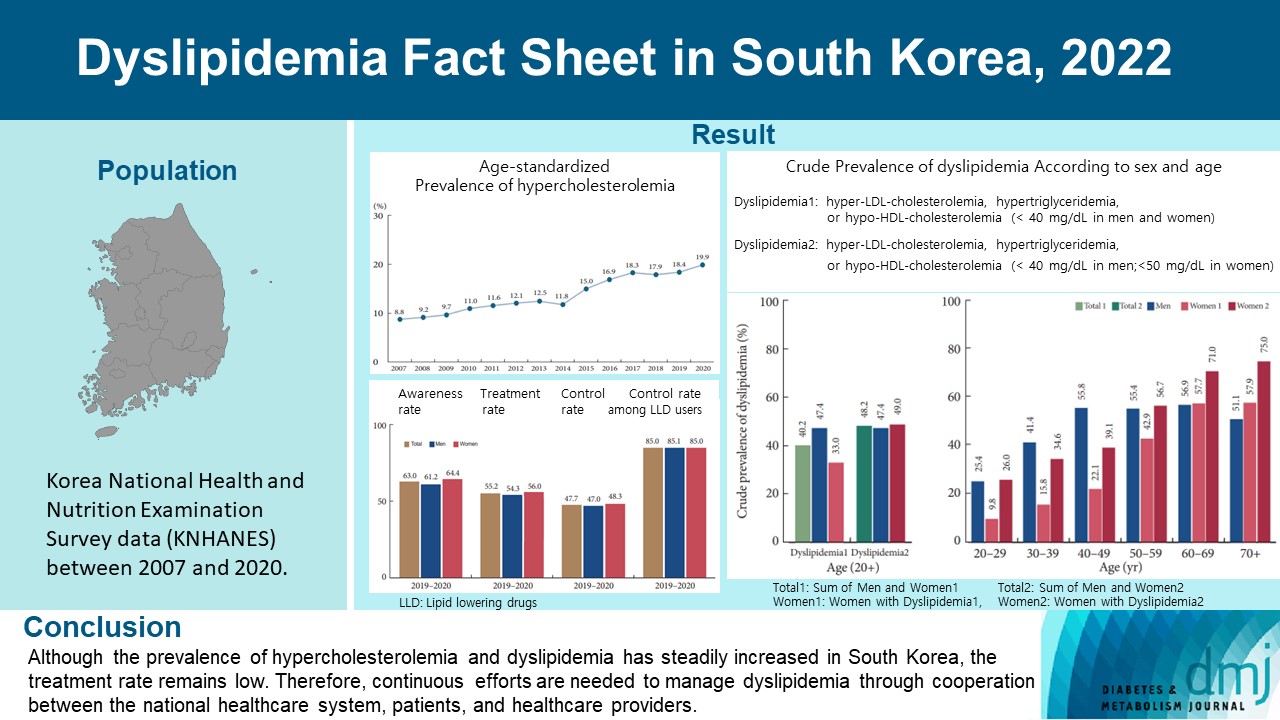
 PubReader
PubReader ePub Link
ePub Link Cite
Cite