
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
Original Articles
- Cardiovascular Risk/Epidemiology
- Two-Year Changes in Diabetic Kidney Disease Phenotype and the Risk of Heart Failure: A Nationwide Population-Based Study in Korea
- Seung Eun Lee, Juhwan Yoo, Han Seok Choi, Kyungdo Han, Kyoung-Ah Kim
- Diabetes Metab J. 2023;47(4):523-534. Published online April 25, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0096
- 1,785 View
- 100 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
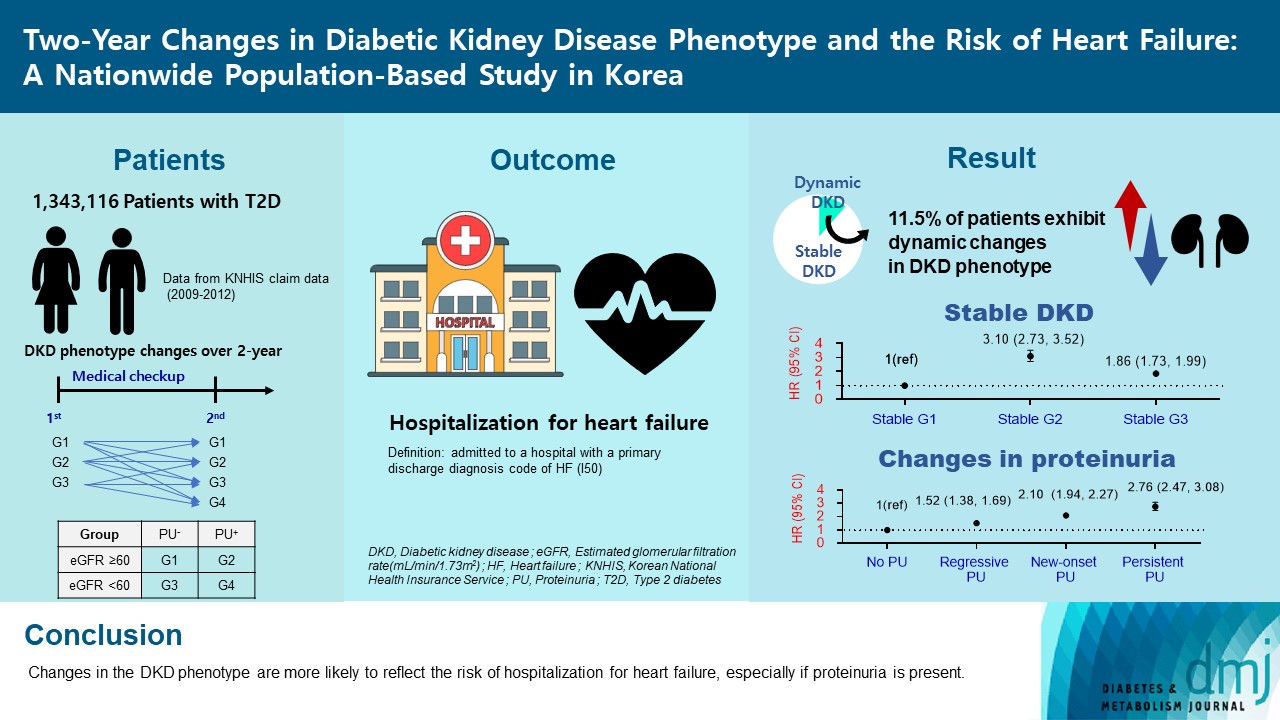
Diabetic kidney disease (DKD) is a risk factor for hospitalization for heart failure (HHF). DKD could be classified into four phenotypes by estimated glomerular filtration rate (eGFR, normal vs. low) and proteinuria (PU, negative vs. positive). Also, the phenotype often changes dynamically. This study examined HHF risk according to the DKD phenotype changes across 2-year assessments.
Methods
The study included 1,343,116 patients with type 2 diabetes mellitus (T2DM) from the Korean National Health Insurance Service database after excluding a very high-risk phenotype (eGFR <30 mL/min/1.73 m2) at baseline, who underwent two cycles of medical checkups between 2009 and 2014. From the baseline and 2-year eGFR and PU results, participants were divided into 10 DKD phenotypic change categories.
Results
During an average of 6.5 years of follow-up, 7,874 subjects developed HHF. The cumulative incidence of HHF from index date was highest in the eGFRlowPU– phenotype, followed by eGFRnorPU+ and eGFRnorPU–. Changes in DKD phenotype differently affect HHF risk. When the persistent eGFRnorPU– category was the reference, hazard ratios for HHF were 3.10 (95% confidence interval [CI], 2.73 to 3.52) in persistent eGFRnorPU+ and 1.86 (95% CI, 1.73 to 1.99) in persistent eGFRlowPU–. Among altered phenotypes, the category converted to eGFRlowPU+ showed the highest risk. In the normal eGFR category at the second examination, those who converted from PU– to PU+ showed a higher risk of HHF than those who converted from PU+ to PU–.
Conclusion
Changes in DKD phenotype, particularly with the presence of PU, are more likely to reflect the risk of HHF, compared with DKD phenotype based on a single time point in patients with T2DM.
- Plasma and urinary Vascular Endothelial Growth Factor and Diabetic Nephropathy in Type 2 Diabetes Mellitus.
- Jeong Heon Oh, Hye Jin Yoo, Soo Yeon Park, Ohk Hyun Ryu, Sang Soo Park, Soon Beom Kwon, Hee Young Kim, Ji A Seo, Kye Won Lee, Sin Gon Kim, Nan Hee Kim, Kyung Mook Choi, Dae Ryong Cha, Sei Hyun Baik, Dong Seop Choi
- Korean Diabetes J. 2004;28(2):111-121. Published online April 1, 2004
- 1,262 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
VEGF(vascular endothelial growth factor) has been implicated in the pathogenesis of neovascularization and endothelial dysfunction in diabetes mellitus. However, its precise role in diabetic nephropathy is still unknown. Our aims were to determine whether alterations of plasma and urinary VEGF levels were related to diabetic microvascular complications, especially nephropathy in type 2 diabetic patients. METHODS: 107 type 2 diabetic patients, without non-diabetic kidney diseases, and 47 healthy control subjects were studied. The urinary albumin excretion was defined as the albumin-to-creatinine ratio(ACR) in 24 hour urine samples. The study subjects were divided into four groups: a nondiabetic healthy control group(n=47), a normoalbuminuric diabetic group(ACR <30mug/mg, n=37), a microalbuminuric diabetic group(ACR 30~299mug/mg, n=37) and an overt proteinuric diabetic group(ACR=300mug/mg, n=33). The plasma and urinary VEGF levels were measured in these subjects by enzyme-linked immunosorbent assays. RESULTS: 1) The urinary VEGF concentrations were significantly higher in the diabetic groups than in the controls, even in the normoalbuminuric stage(log VEGF/Cr, normoalbuminuria; 4.33+/-1.06 vs. control; 3.53+/-0.79, p=0.009). The levels of urinary VEGF excretions increased with advancing diabetic nephropathy stage. 2) The plasma and urinary VEGF levels were higher in the hypertensive diabetic than the normotensive diabetic patients. 3) In the diabetic patients, the level of plasma VEGF was positively correlated with the BUN(r=0.398, p=0.039) and urinary ACR (r=0.251, p=0.044). The level of urinary VEGF was positively correlated with the urinary ACR(r=0.645, p<0.001), and creatinine(r=0.336, p=0.009), but negatively correlated with the level of serum albumin(r=-0.557, p<0.001). Both the levels of urinary VEGF and serum creatinine were independently correlated with the urinary ACR. CONCLUSIONS: The excretion of urinary VEGF increased at a relatively earlier stage in diabetic nephropathy and was significantly correlated with the excretion of urinary albumin. These results suggested the possibility of urinary VEGF as a sensitive marker or the detection of diabetic nephropathy and in predicting disease progression.
- Effect of Glycosaminoglycan on Proteinuria and Urinary N-acetyl- -D-Glucosaminidase Excretion in Otsuka Long-Evans Tokushima Fatty (OLETF) Rats.
- Kyung Mook Choi, Dae Ryong Cha, Sang Youb Han, Dong Rim Kim, Nan Hee Kim, Sei Hyun Baik, Dong Seop Choi
- Korean Diabetes J. 2000;24(5):533-540. Published online January 1, 2001
- 924 View
- 16 Download
-
 Abstract
Abstract
- BACKGROUND
Increased loss of proteoglycan (PG) characterized by an increased loss of anionic charges in the basement membrane has been considered as one of main factors causing urinary loss of albumin. The glycosaminoglycans (GAGs) are linear polymers of repeated disaccharides and the GAG chains are covalently bound to core proteins, forming proteoglycans. It is known that urinary N-acetyl- -D-glucosaminidase (NAG) excretion is a sensitive marker of renal damage and is increased before other renal functional parameters. The aim of this study was to investigate whether GAG treatment is capable of influencing urinary protein and NAG excretion in Otsuka Long-Evans Tokushima Fatty (OLETF) rats which are known as type 2 diabetic animal model. METHODS: Fifteen male OLETF rats and twenty male Long-Evans Tokushima Otsuka (LETO) rats were used for this study. LETO rats are non-diabetic control rats. All OLETF rats were randomly assigned to 2 groups: control group (n=10) given only tap water and GAG group (n=5) feeding with GAG 10 mg/kg from 7 weeks to 55 weeks of age. Measurement of body weight, blood glucose, serum BUN and creatinine was performed periodically. 24-hour urine collection for measurement of urinary protein and NAG excretion was done at 17, 25, 37, 46, 55 weeks of age. RESULTS: 1) OLETF rats showed higher body weight, blood glucose, 24-hour urinary protein and NAG excretion compared with LETO rats. But serum concentration of BUN and creatinine were not different between OLETF and LETO rats. 2) GAG-treated OLETF rats exhibited lower urinary protein/creatinine excretion (17.48+/-0.50 vs 22.49+/-0.11 mg/mg Cr, p< 0.05) and NAG (17.40+/-5.94 vs 43.73+/- 7.44 nmol/h/mg Cr, p< 0.05) excretion compared with non-treated OLETF rats. But body weights, blood glucose, serum concentration of BUN and creatinine were not different between GAG-treated OLETF rats and non-treated OLETF rats. CONCLUSION: 1) The urinary excretion of NAG may be a possible early marker of diabetic nephropathy in OLETF rats. 2) Urinary protein and NAG excretion were decreased in the GAG-treated OLETF rats. GAG seems to have a protective effect against development of diabetic nephropathy.

 KDA
KDA First
First Prev
Prev





