
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Metabolic Risk/Epidemiology
- Effect of Different Types of Diagnostic Criteria for Gestational Diabetes Mellitus on Adverse Neonatal Outcomes: A Systematic Review, Meta-Analysis, and Meta-Regression
- Fahimeh Ramezani Tehrani, Marzieh Saei Ghare Naz, Razieh Bidhendi-Yarandi, Samira Behboudi-Gandevani
- Diabetes Metab J. 2022;46(4):605-619. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0178
- 5,124 View
- 298 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Evidence supporting various diagnostic criteria for diagnose gestational diabetes mellitus (GDM) are consensus-based, needs for additional evidence related to outcomes. Therefore, the aim of this systematic-review and meta-analysis was to assess the impact of different GDM diagnostic-criteria on the risk of adverse-neonatal-outcomes.
Methods
Electronic databases including Scopus, PubMed, and Web of Sciences were searched to retrieve English original, population-based studies with the universal GDM screening approach, up to January-2020. GDM diagnostic criteria were classified in seven groups and International Association of the Diabetes and Pregnancy Study Groups (IADPSG) was considered as reference one. We used the Mantel–Haenszel method to calculate the pooled odds of events. The possibility of publication bias was examined by Begg’s test.
Results
A total of 55 population-based studies consisting of 1,604,391 pregnant women with GDM and 7,770,855 non-GDM counterparts were included. Results showed that in all diagnostic-criteria subgroups, the risk of adverse neonatal outcomes including macrosomia, hyperbilirubinemia, respiratory distress syndrome, neonatal hypoglycemia, neonatal intensive care unit admission, preterm birth, and birth-trauma were significantly higher than the non-GDM counterparts were significantly higher than non-GDM counterparts. Meta-regression analysis revealed that the magnitude of neonatal risks in all diagnostic-criteria subgroups are similar.
Conclusion
Our results showed that the risk of adverse-neonatal-outcome increased among women with GDM, but the magnitude of risk was not different among those women who were diagnosed through more or less intensive strategies. These findings may help health-care-providers and policy-makers to select the most cost-effective approach for the screening of GDM among pregnant women. -
Citations
Citations to this article as recorded by- Hyperglycemia in pregnancy did not worsen the short-term outcomes of very preterm infants: a propensity score matching study
Ying Li, Wei Shen, Rong Zhang, Jian Mao, Ling Liu, Yan-Mei Chang, Xiu-Zhen Ye, Yin-Ping Qiu, Li Ma, Rui Cheng, Hui Wu, Dong-Mei Chen, Ling Chen, Ping Xu, Hua Mei, San-Nan Wang, Fa-Lin Xu, Rong Ju, Xiao-Mei Tong, Xin-Zhu Lin, Fan Wu
Frontiers in Pediatrics.2024;[Epub] CrossRef - Diabetesscreening in der Schwangerschaft
Ute Schäfer-Graf
Die Gynäkologie.2023; 56(2): 103. CrossRef - One-step versus two-step screening for diagnosis of gestational diabetes mellitus in Iranian population: A randomized community trial
Fahimeh Ramezani Tehrani, Maryam Rahmati, Farshad Farzadfar, Mehrandokht Abedini, Maryam Farahmand, Farhad Hosseinpanah, Farzad Hadaegh, Farahnaz Torkestani, Majid Valizadeh, Fereidoun Azizi, Samira Behboudi-Gandevani
Frontiers in Endocrinology.2023;[Epub] CrossRef - Predictors of Neonatal Intensive Care Unit Admission and Adverse Outcomes Related to Gestational Diabetes
Abdullah M Al-shahrani
Cureus.2023;[Epub] CrossRef - Positive association between circulating Caveolin-1 and microalbuminuria in overt diabetes mellitus in pregnancy
Y. Shu, Y. Xiong, Y. Song, S. Jin, X. Bai
Journal of Endocrinological Investigation.2023; 47(1): 201. CrossRef - Early-to-mid pregnancy sleep and circadian markers in relation to birth outcomes: An epigenetics pilot study
Erica C. Jansen, Kelvin Pengyuan Zhang, Dana C. Dolinoy, Helen J. Burgess, Louise M. O’Brien, Elizabeth Langen, Naquia Unwala, Jessa Ehlinger, Molly C. Mulcahy, Jaclyn M. Goodrich
Chronobiology International.2023; 40(9): 1224. CrossRef - Various screening and diagnosis approaches for gestational diabetes mellitus and adverse pregnancy outcomes: a secondary analysis of a randomized non-inferiority field trial
Fahimeh Ramezani Tehrani, Ali Sheidaei, Maryam Rahmati, Farshad Farzadfar, Mahsa Noroozzadeh, Farhad Hosseinpanah, Mehrandokht Abedini, Farzad Hadaegh, Majid Valizadeh, Farahnaz Torkestani, Davood Khalili, Faegheh Firouzi, Masoud Solaymani-Dodaran, Afshin
BMJ Open Diabetes Research & Care.2023; 11(6): e003510. CrossRef
- Hyperglycemia in pregnancy did not worsen the short-term outcomes of very preterm infants: a propensity score matching study
- Metabolic Risk/Epidemiology
- Gestational Diabetes Mellitus: Diagnostic Approaches and Maternal-Offspring Complications
- Joon Ho Moon, Hak Chul Jang
- Diabetes Metab J. 2022;46(1):3-14. Published online January 27, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0335

- 14,800 View
- 899 Download
- 54 Web of Science
- 64 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 
- Gestational diabetes mellitus (GDM) is the most common complication during pregnancy and is defined as any degree of glucose intolerance with onset or first recognition during pregnancy. GDM is associated with adverse pregnancy outcomes and long-term offspring and maternal complications. For GDM screening and diagnosis, a two-step approach (1-hour 50 g glucose challenge test followed by 3-hour 100 g oral glucose tolerance test) has been widely used. After the Hyperglycemia and Adverse Pregnancy Outcome study implemented a 75 g oral glucose tolerance test in all pregnant women, a one-step approach was recommended as an option for the diagnosis of GDM after 2010. The one-step approach has more than doubled the incidence of GDM, but its clinical benefit in reducing adverse pregnancy outcomes remains controversial. Long-term complications of mothers with GDM include type 2 diabetes mellitus and cardiovascular disease, and complications of their offspring include childhood obesity and glucose intolerance. The diagnostic criteria of GDM should properly classify women at risk for adverse pregnancy outcomes and long-term complications. The present review summarizes the strengths and weaknesses of the one-step and two-step approaches for the diagnosis of GDM based on recent randomized controlled trials and observational studies. We also describe the long-term maternal and offspring complications of GDM.
-
Citations
Citations to this article as recorded by- Prophylactic administration of metformin reduces gestational diabetes mellitus incidence in the high-risk populations: a meta-analysis
Hui Yu, Jinling Sun, Honglei Hu
Irish Journal of Medical Science (1971 -).2024; 193(1): 199. CrossRef - Association of dietary inflammatory index with risk of gestational diabetes mellitus and preeclampsia: a systematic review and meta-analysis
Li Hong, Liyuan Zhu, Jinru Zhang, Yueqi Fu, Xiaoyan Qi, Mei Zhao
British Journal of Nutrition.2024; 131(1): 54. CrossRef - Ferritin and iron supplements in gestational diabetes mellitus: less or more?
Tianlian Li, Jingfan Zhang, Ping Li
European Journal of Nutrition.2024; 63(1): 67. CrossRef - Comparing the screening methods for gestational diabetes mellitus before and during the COVID‐19 pandemic: A systematic review
Xingge Sun, Clare McKeaveney, Helen Noble, Hannah O’Hara, Oliver Perra
Journal of Diabetes Investigation.2024; 15(4): 500. CrossRef - Protective Effects of Paeoniflorin Against Inflammation and Oxidative Stress in Rats with Gestational Diabetes Mellitus via Inhibiting the RhoA/ROCK Signaling Pathway
Cheng kun Yuan, Yan Gao, Jinglu Yu, Limin Peng
Revista Brasileira de Farmacognosia.2024; 34(3): 536. CrossRef - METTL14‐mediated lncRNA XIST silencing alleviates GDM progression by facilitating trophoblast cell proliferation and migration via the miR‐497‐5p/FOXO1 axis
Yanchuan Li, Yanfeng Liu, Xiao Yao, Haili Wang, Ziyun Shi, Meiqing He
Journal of Biochemical and Molecular Toxicology.2024;[Epub] CrossRef - Evaluation of insulin secretion and insulin sensitivity in pregnant women: Application value of simple indices
Shuying Ren, Dan Wu, Ping Li
Clinica Chimica Acta.2024; 554: 117753. CrossRef - ATP5me alleviates high glucose-induced myocardial cell injury
Qingsha Hou, Fang Yan, Xiuling Li, Huanling Liu, Xiang Yang, Xudong Dong
International Immunopharmacology.2024; 129: 111626. CrossRef - Aberrant NK cell profile in gestational diabetes mellitus with fetal growth restriction
Yujing Xiong, Yazhen Wang, Mengqi Wu, Shuqiang Chen, Hui Lei, Hui Mu, Haikun Yu, Yongli Hou, Kang Tang, Xutao Chen, Jie Dong, Xiaohong Wang, Lihua Chen
Frontiers in Immunology.2024;[Epub] CrossRef - Maternal Diabetes and Risk of Hypospadias: A Systemic Review and Meta-Analysis
Zhiyuan Liu, Chengjun Yu, Shuhan Yang, Jin Luo, Jie Zhang, Xiao Wang, Chun Wei, Qinlin Shi, Yi Hua, Xing Liu, Guanghui Wei
Urologia Internationalis.2024; 108(2): 108. CrossRef - Maternal birth weight as an indicator of early and late gestational diabetes mellitus: The Japan Environment and Children's Study
Kazuma Tagami, Noriyuki Iwama, Hirotaka Hamada, Hasumi Tomita, Rie Kudo, Natsumi Kumagai, Hongxin Wang, Seiya Izumi, Zen Watanabe, Mami Ishikuro, Taku Obara, Nozomi Tatsuta, Hirohito Metoki, Chiharu Ota, Takashi Sugiyama, Shinichi Kuriyama, Takahiro Arima
Journal of Diabetes Investigation.2024;[Epub] CrossRef - Perinatal characteristics and pregnancy outcomes of advanced maternal age women with gestational diabetes mellitus: A retrospective cohort study
Chen Jiang, Haiyan Wen, Tingting Hu, Yanfei Liu, Xiaoqing Dai, Yiming Chen
Health Science Reports.2024;[Epub] CrossRef - Phenotypic characterisation of regulatory T cells in patients with gestational diabetes mellitus
Ya-nan Zhang, Qin Wu, Yi-hui Deng
Scientific Reports.2024;[Epub] CrossRef - Healthy behaviors and gestational diabetes mellitus in an Iranian setting: A cross-sectional study
Maryam Zare, Afrouz Mardi, Paria Yeghanenia, Daniel Hackett
Medicine.2024; 103(9): e36431. CrossRef - Post‐load glucose is a stronger predictor of adverse pregnancy outcomes than first‐trimester HbA1c in women without gestational diabetes
Shahin Keshtkar Rajabi, Elham Toghraee, Golnoosh Nejatipour
Journal of Diabetes Investigation.2024;[Epub] CrossRef - Triglyceride-glucose index in early pregnancy predicts the risk of gestational diabetes: a prospective cohort study
Yufeng Guo, Junwen Lu, Mailiman Bahani, Guifeng Ding, Lei Wang, Yuxia Zhang, Huanmei Zhang, Chengyao Liu, Lijun Zhou, Xiaolan Liu, Fangshen Li, Xiaoli Wang, Hong Ding
Lipids in Health and Disease.2024;[Epub] CrossRef - A study on behavior, diet patterns and physical activity among selected GDM and non-GDM women in south India
S Sindhu, S Uma Mageshwari
Journal of Diabetology.2024; 15(1): 86. CrossRef - The Implication of Diabetes-Specialized Nurses in Aiming for the Better Treatment and Management of Patients with Diabetes Mellitus: A Brief Narrative Review
Yefang Zhu, Hongmei Zhang, Ying Xi, Hongli Zhu, Yan Lu, Xue Luo, Zhangui Tang, Hong Lei
Diabetes Therapy.2024; 15(5): 917. CrossRef - Triglyceride-glucose index: A promising biomarker for predicting risks of adverse pregnancy outcomes in Hangzhou, China
Jinghua Zhang, Binbin Yin, Ya Xi, Yongying Bai
Preventive Medicine Reports.2024; 41: 102683. CrossRef - Associations of education attainment with gestational diabetes mellitus and the mediating effects of obesity: A Mendelian randomization study
Xiaoyan Wang, Ying Lan, Na Li, Jinfeng Gao, Dejiao Meng, Shuchuan Miao
Heliyon.2024; 10(7): e29000. CrossRef - Quality assessment of videos on social media platforms related to gestational diabetes mellitus in China: A cross-section study
Qin-Yu Cai, Jing Tang, Si-Zhe Meng, Yi Sun, Xia Lan, Tai-Hang Liu
Heliyon.2024; 10(7): e29020. CrossRef - One abnormal value in oral glucose tolerance test during pregnancy and type 2 diabetes risk: Insights from a 5-Year Follow-Up study
Rawia Hussein-Aro, Esther Maor-Sagie, Yoel Toledano, Mordechai Hallak, Rinat Gabbay-Benziv
Diabetes Research and Clinical Practice.2024; 211: 111659. CrossRef - Assessment of the Level of Knowledge About Risk Factors, Prevention, and Treatment of Gestational Diabetes Mellitus in a Community Sample From Saudi Arabia
Suzan A Morsy, Ayat M Tawfik, Samar Y Badayyan, Lameer K Shaikh, Shaden AzizKhan, AlKhansaa A Zakari
Cureus.2024;[Epub] CrossRef - Genetic Susceptibility, Mendelian Randomization, and Nomogram Model Construction of Gestational Diabetes Mellitus
Qiulian Liang, Ming Li, Gongchen Huang, Ruiqi Li, Linyuan Qin, Ping Zhong, Xuekun Xing, Xiangyuan Yu
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Study on the regulation of trophoblast activity by abnormally expressed hsa_circ_0024838/miR-543/HIF1A in patients with gestational diabetes mellitus
Qian Liu, Faminzi Li, Juan Gui, Lianzhi Wu
Placenta.2024;[Epub] CrossRef - Association between sleep duration during pregnancy and gestational diabetes mellitus: a systematic review and meta-analysis
Yuandong Li, Chao Liang, Cui Wu, Zheng Nan
Frontiers in Medicine.2024;[Epub] CrossRef - Ultrasonographic Diagnosis of Fetal Hemodynamic Parameters in Pregnant Women with Diabetes Mellitus in the Third Trimester of Pregnancy
Dongmei Cai, Su Yan
Heliyon.2024; : e30352. CrossRef - Gestational diabetes mellitus and development of intergenerational non-alcoholic fatty liver disease (NAFLD) after delivery: a systematic review and meta-analysis
Ru Xun Foo, Jenny Junyi Ma, Ruochen Du, George Boon Bee Goh, Yap Seng Chong, Cuilin Zhang, Ling-Jun Li
eClinicalMedicine.2024; 72: 102609. CrossRef - U-shaped Association Between Folic Acid Supplementation and the Risk of Gestational Diabetes Mellitus in Chinese Women
Jiuming Zou, Qiang Fu, Xiaoliu Huang, Zhao Yao, Weiye Wang
Canadian Journal of Diabetes.2023; 47(1): 78. CrossRef - Vitamin D Supplementation for the Outcomes of Patients with Gestational Diabetes Mellitus and Neonates: A Meta-Analysis and Systematic Review
Chunfeng Wu, Yang Song, Xueying Wang, Pier P. Sainaghi
International Journal of Clinical Practice.2023; 2023: 1. CrossRef - Lipolysis and gestational diabetes mellitus onset: a case-cohort genome-wide association study in Chinese
Miao Zhang, Qing Li, Kai-Lin Wang, Yao Dong, Yu-Tong Mu, Yan-Min Cao, Jin Liu, Zi-Heng Li, Hui-Lu Cui, Hai-Yan Liu, An-Qun Hu, Ying-Jie Zheng
Journal of Translational Medicine.2023;[Epub] CrossRef - Interactive effect of prepregnancy overweight/obesity and GDM history on prevalence of GDM in biparous women
Xia Xu, Feipeng Huang, Yanni Guo, Lianghui Zheng, Jianying Yan
Frontiers in Endocrinology.2023;[Epub] CrossRef - Microbiome Changes in Pregnancy Disorders
Luca Giannella, Camilla Grelloni, Dayana Quintili, Alessia Fiorelli, Ramona Montironi, Sonila Alia, Giovanni Delli Carpini, Jacopo Di Giuseppe, Arianna Vignini, Andrea Ciavattini
Antioxidants.2023; 12(2): 463. CrossRef - Effects of early standardized management on the growth trajectory of offspring with gestational diabetes mellitus at 0–5 years old: a preliminary longitudinal study
Bingbing Guo, Jingjing Pei, Yin Xu, Yajie Wang, Xinye Jiang
Scientific Reports.2023;[Epub] CrossRef - Prediction model for gestational diabetes mellitus using the XG Boost machine learning algorithm
Xiaoqi Hu, Xiaolin Hu, Ya Yu, Jia Wang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Prevalence and outcomes of gestational diabetes mellitus in Indian women: Insights from a large real-world study over ten years at tertiary care research institute
Sanjay Gupte, Gayatri Venkataraman, Aarti S. Shah, Shalaka Jamenis, Chandrakant Rao, Shweta M. Jangam, Kaveri M. Adki, Onkar C. Swami
International Journal of Diabetes in Developing Countries.2023; 43(4): 511. CrossRef - Gestational diabetes mellitus: state of art
S. A. Pletneva, E. V. Enkova, O. V. Khoperskaya, S. V. Shamarin, V. V. Enkova
Meditsinskiy sovet = Medical Council.2023; (5): 136. CrossRef - Effect of folic acid supplementation in the association between short sleep duration and gestational diabetes mellitus
Zhen Yang, Sisi Hu, Wei Tong, Zhihao Xu, Xiaoliu Huang, Weiye Wang
Sleep and Breathing.2023; 27(6): 2509. CrossRef - Birth weight and large for gestational age trends in offspring of pregnant women with gestational diabetes mellitus in southern China, 2012-2021
Li-Rong He, Li Yu, Yong Guo
Frontiers in Endocrinology.2023;[Epub] CrossRef - Root causes of long-term complications of gestational diabetes mellitus: Metabolic disturbances of the host and gut microbiota
Mingjin Tao, Gaochen Lu, Sheng Zhang, Pan Li
Clinica Chimica Acta.2023; 548: 117490. CrossRef - Analysis on Related Risk Factors for Gestational Diabetes Mellitus (GDM) in Subsequent Pregnancies in Multiparous Women with No History of GDM
文静 张
Advances in Clinical Medicine.2023; 13(07): 11628. CrossRef - Fetoplacental endothelial dysfunction in gestational diabetes mellitus and maternal obesity: A potential threat for programming cardiovascular disease
Mariana S. Diniz, Ursula Hiden, Inês Falcão-Pires, Paulo J. Oliveira, Luis Sobrevia, Susana P. Pereira
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2023; 1869(8): 166834. CrossRef - Diagnosis and management of gestational diabetes mellitus
Tae Jung Oh
Journal of the Korean Medical Association.2023; 66(7): 414. CrossRef - Hypoglycemia in Children: Major Endocrine-Metabolic Causes and Novel Therapeutic Perspectives
Alessia Quarta, Daniela Iannucci, Miriana Guarino, Annalisa Blasetti, Francesco Chiarelli
Nutrients.2023; 15(16): 3544. CrossRef - Relation between weight gain during pregnancy and postpartum reclassification in gestational diabetes
Sofia Coelho, Marta Canha, Ana Rita Leite, João Sérgio Neves, Ana Isabel Oliveira, Davide Carvalho, Maria do Céu Ameida
Endocrine.2023; 82(2): 296. CrossRef - Nurturing through Nutrition: Exploring the Role of Antioxidants in Maternal Diet during Pregnancy to Mitigate Developmental Programming of Chronic Diseases
Mariana S. Diniz, Carina C. Magalhães, Carolina Tocantins, Luís F. Grilo, José Teixeira, Susana P. Pereira
Nutrients.2023; 15(21): 4623. CrossRef - Blood manganese level and gestational diabetes mellitus: a systematic review and meta-analysis
Yingmei Sun, Yu Zhang
Journal of Obstetrics and Gynaecology.2023;[Epub] CrossRef - Multiparity increases the risk of diabetes by impairing the proliferative capacity of pancreatic β cells
Joon Ho Moon, Joonyub Lee, Kyun Hoo Kim, Hyun Jung Kim, Hyeongseok Kim, Hye-Na Cha, Jungsun Park, Hyeonkyu Lee, So-young Park, Hak Chul Jang, Hail Kim
Experimental & Molecular Medicine.2023; 55(10): 2269. CrossRef - Physiological Mechanisms Inherent to Diabetes Involved in the Development of Dementia: Alzheimer’s Disease
Himan Mohamed-Mohamed, Victoria García-Morales, Encarnación María Sánchez Lara, Anabel González-Acedo, Teresa Pardo-Moreno, María Isabel Tovar-Gálvez, Lucía Melguizo-Rodríguez, Juan José Ramos-Rodríguez
Neurology International.2023; 15(4): 1253. CrossRef - Synergistic effect between pre-pregnancy smoking and assisted reproductive technology on gestational diabetes mellitus in twin pregnancies
Lingyu Zhang, Yan Huang, Mingjin Zhang, Yanqi Jin
Acta Diabetologica.2023; 61(2): 205. CrossRef - A Comprehensive Review of Gestational Diabetes Mellitus: Impacts on Maternal Health, Fetal Development, Childhood Outcomes, and Long-Term Treatment Strategies
Vaishnavi S Nakshine, Sangita D Jogdand
Cureus.2023;[Epub] CrossRef - The role of dietary fiber on preventing gestational diabetes mellitus in an at-risk group of high triglyceride-glucose index women: a randomized controlled trial
Yannan Cao, Jing Sheng, Dongyao Zhang, Li Chen, Ying Jiang, Decui Cheng, Yao Su, Yuexin Yu, Haoyi Jia, Pengyuan He, Li Wang, Xianming Xu
Endocrine.2023; 82(3): 542. CrossRef - Correlation between PAPP-A serum levels in the first trimester of pregnancy with the occurrence of gestational diabetes, a multicenter cohort study
Sedigheh Borna, Masoumeh Ashrafzadeh, Marjan Ghaemi, Nasim Eshraghi, Nafiseh Hivechi, Sedigheh Hantoushzadeh
BMC Pregnancy and Childbirth.2023;[Epub] CrossRef - Impact of COVID-19 lockdown on glycemic levels during pregnancy: A retrospective analysis
Erika Di Zazzo, Sergio Davinelli, Serena Panichella, Giovanni Scapagnini, Mariano Intrieri, Silvio Garofalo
Open Medicine.2023;[Epub] CrossRef - Advancements in Nutritional Strategies for Gestational Diabetes Management: A Systematic Review of Recent Evidence
Juan Carlos Sánchez-García, Ines Saraceno López-Palop, Beatriz Piqueras-Sola, Jonathan Cortés-Martín, Elena Mellado-García, Inmaculada Muñóz Sánchez, Raquel Rodríguez-Blanque
Journal of Clinical Medicine.2023; 13(1): 37. CrossRef - Comparative efficacy and safety of glyburide, metformin, and insulin in treatment of gestational diabetes mellitus
Jing Lin, Rong-zu Tu, Xun-yu Hong
Medicine.2022;[Epub] CrossRef - Stacking Ensemble Method for Gestational Diabetes Mellitus Prediction in Chinese Pregnant Women: A Prospective Cohort Study
Ruiyi Liu, Yongle Zhan, Xuan Liu, Yifang Zhang, Luting Gui, Yimin Qu, Hairong Nan, Yu Jiang, Mehdi Gheisari
Journal of Healthcare Engineering.2022; 2022: 1. CrossRef - Secular increase in the prevalence of gestational diabetes and its associated adverse pregnancy outcomes from 2014 to 2021 in Hebei province, China
Mei-Ling Tian, Li-Yan Du, Guo-Juan Ma, Ting Zhang, Xu-Yuan Ma, Ying-Kui Zhang, Zeng-Jun Tang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Aquaporin-8 overexpression is involved in vascular structure and function changes in placentas of gestational diabetes mellitus patients
Yanxing Shan, Jiawen Cui, Xinyi Kang, Weichun Tang, Yiling Lu, Ying Gao, Liping Chen
Open Life Sciences.2022; 17(1): 1473. CrossRef - Vitamin D status and levels of pro-inflammatory cytokines in newborns born to mothers with endocrine diseases
N. E. Verisokina, L. Ya. Klimov, I. N. Zakharova, A. L. Zaplatnikov, V. V. Zubkov, A. A. Momotova, V. A. Kuryaninova, R. A. Atanesyan, T. V. Zhelezniakova, M. A. Petrosyan, D. V. Bobryshev, D. A. Volkov, Z. A. Magomadova
Meditsinskiy sovet = Medical Council.2022; (19): 9. CrossRef - IL-6 and IL-8: An Overview of Their Roles in Healthy and Pathological Pregnancies
Aleksandra Vilotić, Mirjana Nacka-Aleksić, Andrea Pirković, Žanka Bojić-Trbojević, Dragana Dekanski, Milica Jovanović Krivokuća
International Journal of Molecular Sciences.2022; 23(23): 14574. CrossRef - Higher Muscle Mass Protects Women with Gestational Diabetes Mellitus from Progression to Type 2 Diabetes Mellitus
Yujin Shin, Joon Ho Moon, Tae Jung Oh, Chang Ho Ahn, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
Diabetes & Metabolism Journal.2022; 46(6): 890. CrossRef - Identification of human placenta-derived circular RNAs and autophagy related circRNA-miRNA-mRNA regulatory network in gestational diabetes mellitus
Yindi Bao, Jun Zhang, Yi Liu, Lianzhi Wu, Jing Yang
Frontiers in Genetics.2022;[Epub] CrossRef - The Role of Dietary Polyphenols in Pregnancy and Pregnancy-Related Disorders
Mirjana Nacka-Aleksić, Andrea Pirković, Aleksandra Vilotić, Žanka Bojić-Trbojević, Milica Jovanović Krivokuća, Francesca Giampieri, Maurizio Battino, Dragana Dekanski
Nutrients.2022; 14(24): 5246. CrossRef
- Prophylactic administration of metformin reduces gestational diabetes mellitus incidence in the high-risk populations: a meta-analysis
- Metabolic Risk/Epidemiology
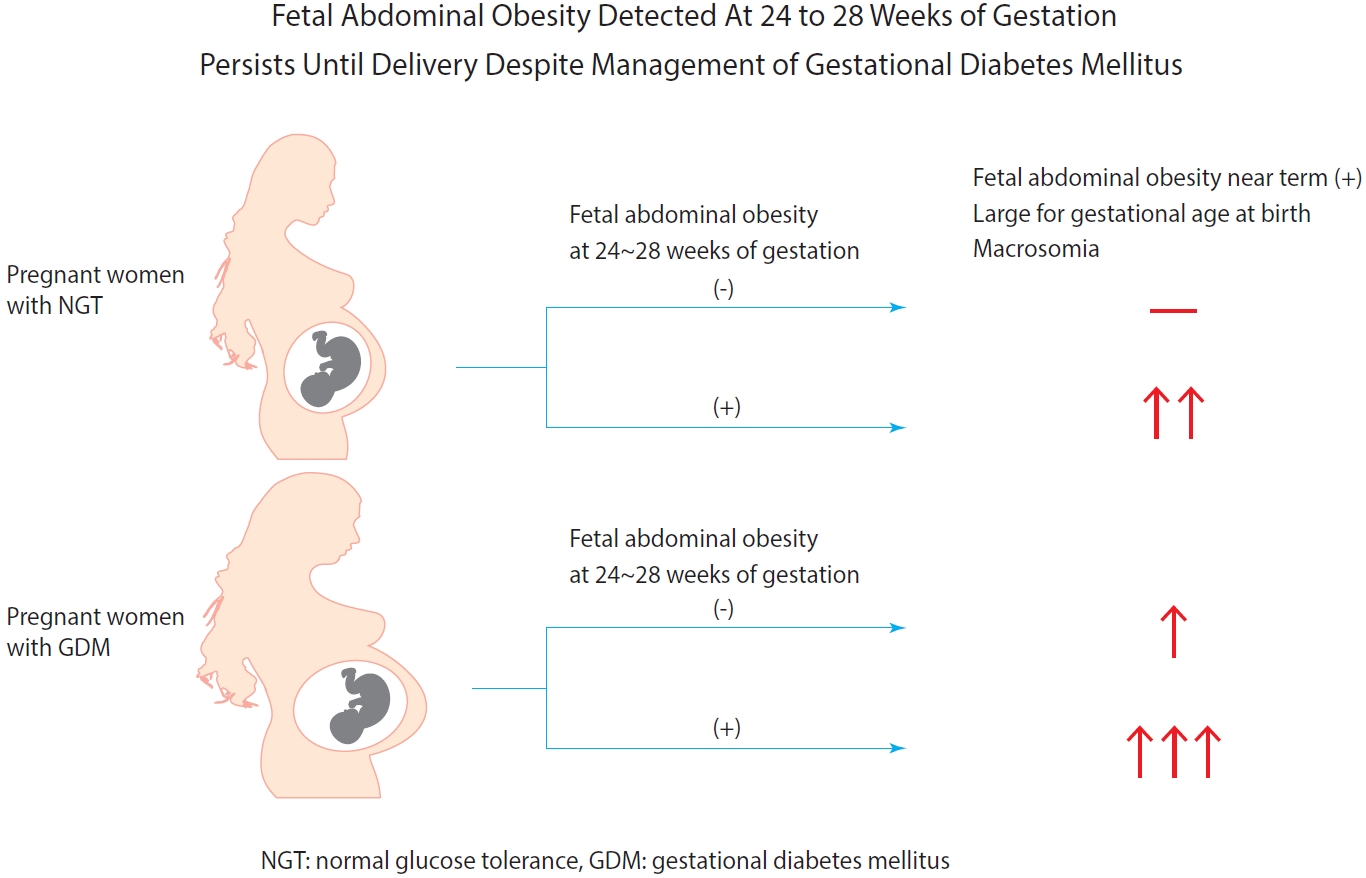
- Fetal Abdominal Obesity Detected At 24 to 28 Weeks of Gestation Persists Until Delivery Despite Management of Gestational Diabetes Mellitus
- Wonjin Kim, Soo Kyung Park, Yoo Lee Kim
- Diabetes Metab J. 2021;45(4):547-557. Published online March 5, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0078
- 5,863 View
- 185 Download
- 7 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 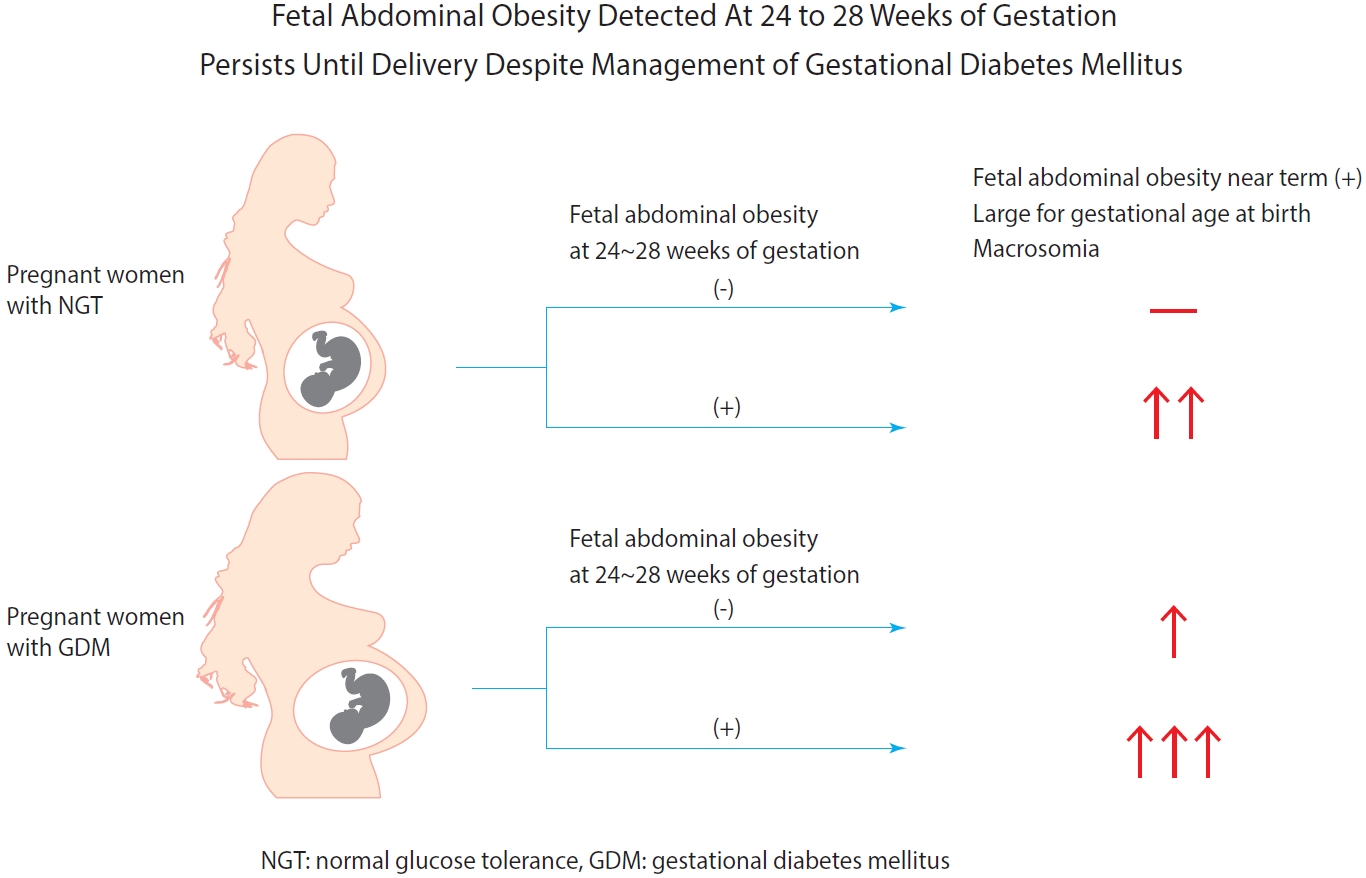
- Background
Fetal abdominal obesity (FAO) has been reported to be affected at gestational diabetes mellitus (GDM) diagnosis at 24 to 28 weeks of gestation in older and/or obese women. This study investigated whether the management of GDM improves FAO in GDM subjects near term.
Methods
Medical records of 7,099 singleton pregnant women delivering at CHA Gangnam Medical Center were reviewed retrospectively. GDM was diagnosed by 100-g oral glucose tolerance test after 50-g glucose challenge test based on Carpenter–Coustan criteria. GDM subjects were divided into four study groups according to maternal age and obesity. FAO was defined as ≥90th percentile of fetal abdominal overgrowth ratios (FAORs) of the ultrasonographically estimated gestational age (GA) of abdominal circumference per actual GA by the last menstruation period, biparietal diameter, or femur length, respectively.
Results
As compared with normal glucose tolerance (NGT) subjects near term, FAORs and odds ratio for FAO were significantly higher in old and/or obese women with GDM but not in young and nonobese women with GDM. For fetuses of GDM subjects with FAO at the time of GDM diagnosis, the odds ratio for exhibiting FAO near term and being large for GA at birth were 7.87 (95% confidence interval [CI], 4.38 to 14.15) and 10.96 (95% CI, 5.58 to 20.53) compared with fetuses of NGT subjects without FAO at GDM diagnosis.
Conclusion
Despite treatment, FAO detected at the time of GDM diagnosis persisted until delivery. Early diagnosis and treatment might be necessary to prevent near term FAO in high-risk older and/or obese women. -
Citations
Citations to this article as recorded by- The effects of gestational diabetes mellitus on fetal growth: is it different for low-risk and medium–high-risk pregnant women?
Jie Wang, Xin Cheng, Zhen-Hua Li, Yi-Cheng Mao, Xin-Qiang Wang, Kang-Di Zhang, Wen-Jie Yu, Ying-Qing Li, Jia-wen Zhao, Mao-Lin Chen, Guo-peng Gao, Cheng-Yang Hu, Xiu-Jun Zhang
Archives of Gynecology and Obstetrics.2023;[Epub] CrossRef - Fetal abdominal obesity and the ensuing adverse perinatal outcomes in older obese pregnant women with or without obesity and with normal glucose tolerance
Wonjin Kim, Soo Kyung Park, Yoo Lee Kim
Scientific Reports.2023;[Epub] CrossRef - Early-life exposure to gestational diabetes mellitus predisposes offspring to pediatric nonalcoholic fatty liver disease
Qian-Ren Zhang, Yan Dong, Jian-Gao Fan
Hepatobiliary & Pancreatic Diseases International.2023;[Epub] CrossRef - Gestational diabetes mellitus and adverse pregnancy outcomes: systematic review and meta-analysis
Wenrui Ye, Cong Luo, Jing Huang, Chenglong Li, Zhixiong Liu, Fangkun Liu
BMJ.2022; : e067946. CrossRef - Fetal abdominal overgrowth is already present at 20–24 gestational weeks prior to diagnosis of gestational diabetes mellitus
Wonjin Kim, Soo Kyung Park, Yoo Lee Kim
Scientific Reports.2021;[Epub] CrossRef
- The effects of gestational diabetes mellitus on fetal growth: is it different for low-risk and medium–high-risk pregnant women?
- Metabolic Risk/Epidemiology
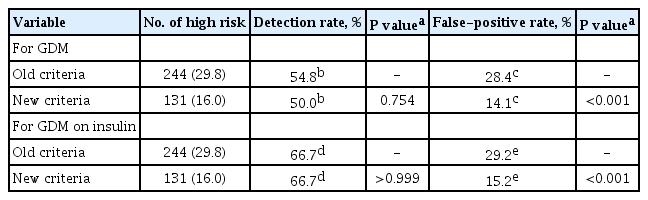
- A Comparison of Predictive Performances between Old versus New Criteria in a Risk-Based Screening Strategy for Gestational Diabetes Mellitus
- Subeen Hong, Seung Mi Lee, Soo Heon Kwak, Byoung Jae Kim, Ja Nam Koo, Ig Hwan Oh, Sohee Oh, Sun Min Kim, Sue Shin, Won Kim, Sae Kyung Joo, Errol R. Norwitz, Souphaphone Louangsenlath, Chan-Wook Park, Jong Kwan Jun, Joong Shin Park
- Diabetes Metab J. 2020;44(5):726-736. Published online April 13, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0126
- 6,629 View
- 123 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background The definition of the high-risk group for gestational diabetes mellitus (GDM) defined by the American College of Obstetricians and Gynecologists was changed from the criteria composed of five historic/demographic factors (old criteria) to the criteria consisting of 11 factors (new criteria) in 2017. To compare the predictive performances between these two sets of criteria.
Methods This is a secondary analysis of a large prospective cohort study of non-diabetic Korean women with singleton pregnancies designed to examine the risk of GDM in women with nonalcoholic fatty liver disease. Maternal fasting blood was taken at 10 to 14 weeks of gestation and measured for glucose and lipid parameters. GDM was diagnosed by the two-step approach.
Results Among 820 women, 42 (5.1%) were diagnosed with GDM. Using the old criteria, 29.8% (
n =244) of women would have been identified as high risk versus 16.0% (n =131) using the new criteria. Of the 42 women who developed GDM, 45.2% (n =19) would have been mislabeled as not high risk by the old criteria versus 50.0% (n =21) using the new criteria (1-sensitivity, 45.2% vs. 50.0%,P >0.05). Among the 778 patients who did not develop GDM, 28.4% (n =221) would have been identified as high risk using the old criteria versus 14.1% (n =110) using the new criteria (1-specificity, 28.4% vs. 14.1%,P <0.001).Conclusion Compared with the old criteria, use of the new criteria would have decreased the number of patients identified as high risk and thus requiring early GDM screening by half (from 244 [29.8%] to 131 [16.0%]).
-
Citations
Citations to this article as recorded by- Predicting the Risk of Insulin-Requiring Gestational Diabetes before Pregnancy: A Model Generated from a Nationwide Population-Based Cohort Study in Korea
Seung-Hwan Lee, Jin Yu, Kyungdo Han, Seung Woo Lee, Sang Youn You, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim
Endocrinology and Metabolism.2023; 38(1): 129. CrossRef - Metabolic Dysfunction-Associated Fatty Liver Disease and Subsequent Development of Adverse Pregnancy Outcomes
Seung Mi Lee, Young Mi Jung, Eun Saem Choi, Soo Heon Kwak, Ja Nam Koo, Ig Hwan Oh, Byoung Jae Kim, Sun Min Kim, Sang Youn Kim, Gyoung Min Kim, Sae Kyung Joo, Bo Kyung Koo, Sue Shin, Errol R. Norwitz, Chan-Wook Park, Jong Kwan Jun, Won Kim, Joong Shin Park
Clinical Gastroenterology and Hepatology.2022; 20(11): 2542. CrossRef - Nonalcoholic fatty liver disease and early prediction of gestational diabetes mellitus using machine learning methods
Seung Mi Lee, Suhyun Hwangbo, Errol R. Norwitz, Ja Nam Koo, Ig Hwan Oh, Eun Saem Choi, Young Mi Jung, Sun Min Kim, Byoung Jae Kim, Sang Youn Kim, Gyoung Min Kim, Won Kim, Sae Kyung Joo, Sue Shin, Chan-Wook Park, Taesung Park, Joong Shin Park
Clinical and Molecular Hepatology.2022; 28(1): 105. CrossRef - Nonalcoholic fatty liver disease-based risk prediction of adverse pregnancy outcomes: Ready for prime time?
Seung Mi Lee, Won Kim
Clinical and Molecular Hepatology.2022; 28(1): 47. CrossRef - Postprandial Free Fatty Acids at Mid-Pregnancy Increase the Risk of Large-for-Gestational-Age Newborns in Women with Gestational Diabetes Mellitus
So-Yeon Kim, Young Shin Song, Soo-Kyung Kim, Yong-Wook Cho, Kyung-Soo Kim
Diabetes & Metabolism Journal.2022; 46(1): 140. CrossRef - Effect of Different Types of Diagnostic Criteria for Gestational Diabetes Mellitus on Adverse Neonatal Outcomes: A Systematic Review, Meta-Analysis, and Meta-Regression
Fahimeh Ramezani Tehrani, Marzieh Saei Ghare Naz, Razieh Bidhendi-Yarandi, Samira Behboudi-Gandevani
Diabetes & Metabolism Journal.2022; 46(4): 605. CrossRef - Development of early prediction model for pregnancy-associated hypertension with graph-based semi-supervised learning
Seung Mi Lee, Yonghyun Nam, Eun Saem Choi, Young Mi Jung, Vivek Sriram, Jacob S. Leiby, Ja Nam Koo, Ig Hwan Oh, Byoung Jae Kim, Sun Min Kim, Sang Youn Kim, Gyoung Min Kim, Sae Kyung Joo, Sue Shin, Errol R. Norwitz, Chan-Wook Park, Jong Kwan Jun, Won Kim,
Scientific Reports.2022;[Epub] CrossRef - The Clinical Characteristics of Gestational Diabetes Mellitus in Korea: A National Health Information Database Study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Endocrinology and Metabolism.2021; 36(3): 628. CrossRef - The risk of pregnancy‐associated hypertension in women with nonalcoholic fatty liver disease
Young Mi Jung, Seung Mi Lee, Subeen Hong, Ja Nam Koo, Ig Hwan Oh, Byoung Jae Kim, Sun Min Kim, Sang Youn Kim, Gyoung Min Kim, Sae Kyung Joo, Sue Shin, Errol R. Norwitz, Chan‐Wook Park, Jong Kwan Jun, Won Kim, Joong Shin Park
Liver International.2020; 40(10): 2417. CrossRef
- Predicting the Risk of Insulin-Requiring Gestational Diabetes before Pregnancy: A Model Generated from a Nationwide Population-Based Cohort Study in Korea
- Clinical Care/Education
- Pregnancy Outcomes of Women Additionally Diagnosed as Gestational Diabetes by the International Association of the Diabetes and Pregnancy Study Groups Criteria
- Min Hyoung Kim, Soo Heon Kwak, Sung-Hoon Kim, Joon Seok Hong, Hye Rim Chung, Sung Hee Choi, Moon Young Kim, Hak C. Jang
- Diabetes Metab J. 2019;43(6):766-775. Published online February 28, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0192
- 5,994 View
- 89 Download
- 26 Web of Science
- 28 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background We investigated the pregnancy outcomes in women who were diagnosed with gestational diabetes mellitus (GDM) by the International Association of the Diabetes and Pregnancy Study Groups (IADPSG) criteria but not by the Carpenter-Coustan (CC) criteria.
Methods A total of 8,735 Korean pregnant women were identified at two hospitals between 2014 and 2016. Among them, 2,038 women participated in the prospective cohort to investigate pregnancy outcomes. Diagnosis of GDM was made via two-step approach with 50-g glucose challenge test for screening followed by diagnostic 2-hour 75-g oral glucose tolerance test. Women were divided into three groups: non-GDM, GDM diagnosed exclusively by the IADPSG criteria, and GDM diagnosed by the CC criteria.
Results The incidence of GDM was 2.1% according to the CC criteria, and 4.1% by the IADPSG criteria. Women diagnosed with GDM by the IADPSG criteria had a higher body mass index (22.0±3.1 kg/m2 vs. 21.0±2.8 kg/m2,
P <0.001) and an increased risk of preeclampsia (odds ratio [OR], 6.90; 95% confidence interval [CI], 1.84 to 25.87;P =0.004) compared to non-GDM women. Compared to neonates of the non-GDM group, those of the IADPSG GDM group had an increased risk of being large for gestational age (OR, 2.39; 95% CI, 1.50 to 3.81;P <0.001), macrosomia (OR, 2.53; 95% CI, 1.26 to 5.10;P =0.009), and neonatal hypoglycemia (OR, 3.84; 95% CI, 1.01 to 14.74;P =0.049); they were also at an increased risk of requiring phototherapy (OR, 1.57; 95% CI, 1.07 to 2.31;P =0.022) compared to the non-GDM group.Conclusion The IADPSG criteria increased the incidence of GDM by nearly three-fold, and women diagnosed with GDM by the IADPSG criteria had an increased risk of adverse pregnancy outcomes in Korea.
-
Citations
Citations to this article as recorded by- Gestational diabetes mellitus and adverse maternal and perinatal outcomes in twin and singleton pregnancies: a systematic review and meta-analysis
Elena Greco, Maria Calanducci, Kypros H. Nicolaides, Eleanor V.H. Barry, Mohammed S.B. Huda, Stamatina Iliodromiti
American Journal of Obstetrics and Gynecology.2024; 230(2): 213. CrossRef - Neonatal outcomes according to different glucose threshold values in gestational diabetes: a register-based study
Kaisa Kariniemi, Marja Vääräsmäki, Tuija Männistö, Sanna Mustaniemi, Eero Kajantie, Sanna Eteläinen, Elina Keikkala, Anneli Pouta, Risto Kaaja, Johan G Eriksson, Hannele Laivuori, Mika Gissler
BMC Pregnancy and Childbirth.2024;[Epub] CrossRef - Pregnancy complications in women with pregestational and gestational diabetes mellitus
Lukas Reitzle, Christin Heidemann, Jens Baumert, Matthias Kaltheuner, Heinke Adamczewski, Andrea Icks, Christa Scheidt-Nave
Deutsches Ärzteblatt international.2023;[Epub] CrossRef - Predicting the Risk of Insulin-Requiring Gestational Diabetes before Pregnancy: A Model Generated from a Nationwide Population-Based Cohort Study in Korea
Seung-Hwan Lee, Jin Yu, Kyungdo Han, Seung Woo Lee, Sang Youn You, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim
Endocrinology and Metabolism.2023; 38(1): 129. CrossRef - Treatment of women with mild gestational diabetes mellitus decreases the risk of adverse perinatal outcomes
Fanny Goyette, Bi Lan Wo, Marie-Hélène Iglesias, Evelyne Rey, Ariane Godbout
Diabetes & Metabolism.2023; 49(4): 101458. CrossRef - Maternal and fetal outcomes of pregnancies associated with single versus double abnormal values in 100 gr glucose tolerance test
Mohammadali Shahriari, Ali Shahriari, Maryam Khooshideh, Anahita Dehghaninezhad, Arezoo Maleki-Hajiagha, Rana Karimi
Journal of Diabetes & Metabolic Disorders.2023; 22(2): 1347. CrossRef - Diagnosis and management of gestational diabetes mellitus
Tae Jung Oh
Journal of the Korean Medical Association.2023; 66(7): 414. CrossRef - Update on gestational diabetes and adverse pregnancy outcomes
Bryan Ugwudike, ManHo Kwok
Current Opinion in Obstetrics & Gynecology.2023; 35(5): 453. CrossRef - Effects of early standardized management on the growth trajectory of offspring with gestational diabetes mellitus at 0–5 years old: a preliminary longitudinal study
Bingbing Guo, Jingjing Pei, Yin Xu, Yajie Wang, Xinye Jiang
Scientific Reports.2023;[Epub] CrossRef - Can Triglyceride/Glucose Index (TyG) and Triglyceride/HDL-Cholesterol Ratio (TG/HDL-c) Predict Gestational Diabetes Mellitus?
Seval YILMAZ ERGANİ, Tolgay Tuyan İLHAN, Betül TOKGÖZ, Burak BAYRAKTAR, Mevlüt BUCAK, Müjde Can İBANOĞLU, Kadriye YAKUT YÜCEL, Kadriye ERDOĞAN, Cantekin İSKENDER, Yaprak ÜSTÜN
Ankara Eğitim ve Araştırma Hastanesi Tıp Dergisi.2023; 56(2): 117. CrossRef - Risk factors for postpartum urinary incontinence: The impact of early-onset and late-onset Gestational Diabetes Mellitus in a nested case-control study
Carlos I. Sartorão Filho, Fabiane A. Pinheiro, Luiz Takano, Caroline B. Prudêncio, Sthefanie K. Nunes, Hallur RLS, Iracema M.P. Calderon, Angélica M.P. Barbosa, Marilza V.C. Rudge
European Journal of Obstetrics & Gynecology and Reproductive Biology.2023; 290: 5. CrossRef - Review of the Screening Guidelines for Gestational Diabetes Mellitus: How to Choose Wisely
Ravleen Kaur Bakshi, Akshay Kumar, Vandana Gupta, A.G. Radhika, Puneet Misra, Pankaj Bhardwaj
Indian Journal of Community Medicine.2023; 48(6): 828. CrossRef - Postprandial Free Fatty Acids at Mid-Pregnancy Increase the Risk of Large-for-Gestational-Age Newborns in Women with Gestational Diabetes Mellitus
So-Yeon Kim, Young Shin Song, Soo-Kyung Kim, Yong-Wook Cho, Kyung-Soo Kim
Diabetes & Metabolism Journal.2022; 46(1): 140. CrossRef - Gestational Diabetes Mellitus: Diagnostic Approaches and Maternal-Offspring Complications
Joon Ho Moon, Hak Chul Jang
Diabetes & Metabolism Journal.2022; 46(1): 3. CrossRef - Risk and Risk Factors for Postpartum Type 2 Diabetes Mellitus in Women with Gestational Diabetes: A Korean Nationwide Cohort Study
Mi Jin Choi, Jimi Choi, Chae Weon Chung
Endocrinology and Metabolism.2022; 37(1): 112. CrossRef - Gestational diabetes mellitus: current screening problems
N. I. Volkova, S. O. Panenko
Diabetes mellitus.2022; 25(1): 72. CrossRef - Gestational diabetes mellitus and adverse pregnancy outcomes: systematic review and meta-analysis
Wenrui Ye, Cong Luo, Jing Huang, Chenglong Li, Zhixiong Liu, Fangkun Liu
BMJ.2022; : e067946. CrossRef - Effect of Different Types of Diagnostic Criteria for Gestational Diabetes Mellitus on Adverse Neonatal Outcomes: A Systematic Review, Meta-Analysis, and Meta-Regression
Fahimeh Ramezani Tehrani, Marzieh Saei Ghare Naz, Razieh Bidhendi-Yarandi, Samira Behboudi-Gandevani
Diabetes & Metabolism Journal.2022; 46(4): 605. CrossRef - Triglyceride and glucose index and the risk of gestational diabetes mellitus: A nationwide population-based cohort study
Jung A Kim, Jinsil Kim, Eun Roh, So-hyeon Hong, You-Bin Lee, Sei Hyun Baik, Kyung Mook Choi, Eunjin Noh, Soon Young Hwang, Geum Joon Cho, Hye Jin Yoo
Diabetes Research and Clinical Practice.2021; 171: 108533. CrossRef - Effect of the IADPSG screening strategy for gestational diabetes on perinatal outcomes in Switzerland
Evelyne M. Aubry, Luigi Raio, Stephan Oelhafen
Diabetes Research and Clinical Practice.2021; 175: 108830. CrossRef - Estimated impact of introduction of new diagnostic criteria for gestational diabetes mellitus
Leon de Wit, Anna B Zijlmans, Doortje Rademaker, Christiana A Naaktgeboren, J Hans DeVries, Arie Franx, Rebecca C Painter, Bas B van Rijn
World Journal of Diabetes.2021; 12(6): 868. CrossRef - The Clinical Characteristics of Gestational Diabetes Mellitus in Korea: A National Health Information Database Study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Endocrinology and Metabolism.2021; 36(3): 628. CrossRef - Fetal Abdominal Obesity Detected At 24 to 28 Weeks of Gestation Persists Until Delivery Despite Management of Gestational Diabetes Mellitus
Wonjin Kim, Soo Kyung Park, Yoo Lee Kim
Diabetes & Metabolism Journal.2021; 45(4): 547. CrossRef - Nonalcoholic fatty liver disease and the risk of insulin-requiring gestational diabetes
Sang Youn You, Kyungdo Han, Seung-Hawn Lee, Mee Kyoung Kim
Diabetology & Metabolic Syndrome.2021;[Epub] CrossRef - Maternal Hyperglycemia during Pregnancy Increases Adiposity of Offspring
Hye Rim Chung, Joon Ho Moon, Jung Sub Lim, Young Ah Lee, Choong Ho Shin, Joon-Seok Hong, Soo Heon Kwak, Sung Hee Choi, Hak Chul Jang
Diabetes & Metabolism Journal.2021; 45(5): 730. CrossRef - Prepregnancy smoking and the risk of gestational diabetes requiring insulin therapy
Mee Kyoung Kim, Kyungdo Han, Sang Youn You, Hyuk-Sang Kwon, Kun-Ho Yoon, Seung-Hwan Lee
Scientific Reports.2020;[Epub] CrossRef - Gestational Diabetes Mellitus: Diagnosis and Glycemic Control
Tae Jung Oh, Hak Chul Jang
The Journal of Korean Diabetes.2020; 21(2): 69. CrossRef - New Diagnostic Criteria for Gestational Diabetes Mellitus and Pregnancy Outcomes in Korea
Kyu Yeon Hur
Diabetes & Metabolism Journal.2019; 43(6): 763. CrossRef
- Gestational diabetes mellitus and adverse maternal and perinatal outcomes in twin and singleton pregnancies: a systematic review and meta-analysis
- Clinical Diabetes & Therapeutics
- Progression to Gestational Diabetes Mellitus in Pregnant Women with One Abnormal Value in Repeated Oral Glucose Tolerance Tests
- Sunyoung Kang, Min Hyoung Kim, Moon Young Kim, Joon-Seok Hong, Soo Heon Kwak, Sung Hee Choi, Soo Lim, Kyong Soo Park, Hak C. Jang
- Diabetes Metab J. 2019;43(5):607-614. Published online February 28, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0159
- 5,899 View
- 103 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Women with one abnormal value (OAV) in a 100 g oral glucose tolerance test (OGTT) during pregnancy are reported to have an increased risk of adverse pregnancy outcomes. However, there is limited data about whether women with OAV will progress to gestational diabetes mellitus (GDM) when the OGTT is repeated.
Methods To identify clinical and metabolic predictors for GDM in women with OAV, we conducted a retrospective study and identified women with OAV in the OGTT done at 24 to 30 weeks gestational age (GA) and repeated the second OGTT between 32 and 34 weeks of GA.
Results Among 137 women with OAV in the initial OGTT, 58 (42.3%) had normal, 40 (29.2%) had OAV and 39 (28.5%) had GDM in the second OGTT. Maternal age, prepregnancy body mass index, weight gain from prepregnancy to the second OGTT, GA at the time of the OGTT, and parity were similar among normal, OAV, and GDM groups. Plasma glucose levels in screening tests were different (151.8±15.7, 155.8±14.6, 162.5±20.3 mg/dL,
P <0.05), but fasting, 1-, 2-, and 3-hour glucose levels in the initial OGTT were not. Compared to women with screen negative, women with untreated OAV had a higher frequency of macrosomia.Conclusion We demonstrated that women with OAV in the initial OGTT significantly progressed to GDM in the second OGTT. Clinical parameters predicting progression to GDM were not found. Repeating the OGTT in women with OAV in the initial test may be helpful to detect GDM progression.
-
Citations
Citations to this article as recorded by- Maternal and fetal outcomes of pregnancies associated with single versus double abnormal values in 100 gr glucose tolerance test
Mohammadali Shahriari, Ali Shahriari, Maryam Khooshideh, Anahita Dehghaninezhad, Arezoo Maleki-Hajiagha, Rana Karimi
Journal of Diabetes & Metabolic Disorders.2023; 22(2): 1347. CrossRef - One abnormal value or vomiting after oral glucose tolerance test in pregnancy: incidence and impact on maternal-fetal outcomes
Humberto Navarro-Martinez, Juana-Antonia Flores-Le Roux, Gemma Llauradó, Lucia Gortazar, Antonio Payà, Laura Mañé, Juan Pedro-Botet, David Benaiges
Gynecological Endocrinology.2023;[Epub] CrossRef - Analysis of the gut microflora in women with gestational diabetes mellitus
Xuping Wang, Bingfeng Bian, Fuman Du, Chaofeng Xiang, Yu Liu, Na Li, Binhong Duan
International Journal of Diabetes in Developing Countries.2023;[Epub] CrossRef - The association between gestational impaired glucose tolerance and hyperglycemic markers: A prospective study
Ohad Gluck, Hadas Ganer Herman, Nataly Fainstein, Neri Katz, Jacob Bar, Michal Kovo
International Journal of Gynecology & Obstetrics.2022; 156(1): 82. CrossRef - Association of abnormal-glucose tolerance during pregnancy with exposure to PM2.5 components and sources
Dejian Mai, Chengfang Xu, Weiwei Lin, Dingli Yue, Shaojie Fu, Jianqing Lin, Luan Yuan, Yan Zhao, Yuhong Zhai, Huiying Mai, Xiaoling Zeng, Tingwu Jiang, Xuejiao Li, Jiajia Dai, Boning You, Qin Xiao, Qing Wei, Qiansheng Hu
Environmental Pollution.2022; 292: 118468. CrossRef - Postprandial Free Fatty Acids at Mid-Pregnancy Increase the Risk of Large-for-Gestational-Age Newborns in Women with Gestational Diabetes Mellitus
So-Yeon Kim, Young Shin Song, Soo-Kyung Kim, Yong-Wook Cho, Kyung-Soo Kim
Diabetes & Metabolism Journal.2022; 46(1): 140. CrossRef - The Clinical Characteristics of Gestational Diabetes Mellitus in Korea: A National Health Information Database Study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Endocrinology and Metabolism.2021; 36(3): 628. CrossRef - Gestational Diabetes Mellitus: Diagnosis and Glycemic Control
Tae Jung Oh, Hak Chul Jang
The Journal of Korean Diabetes.2020; 21(2): 69. CrossRef - Health literacy and diabetes control in pregnant women
Azar Pirdehghan, Mohammad Eslahchi, Farzaneh Esna-Ashari, Shiva Borzouei
Journal of Family Medicine and Primary Care.2020; 9(2): 1048. CrossRef
- Maternal and fetal outcomes of pregnancies associated with single versus double abnormal values in 100 gr glucose tolerance test
- Maternal and Neonatal Outcomes in Korean Women with Type 1 and Type 2 Diabetes
- Hee-Sook Kim, Hye-Jung Jang, Jeong-Eun Park, Moon-Young Kim, Sun-Young Ko, Sung-Hoon Kim
- Diabetes Metab J. 2015;39(4):316-320. Published online August 17, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.4.316
- 3,350 View
- 35 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The purpose of this study was to evaluate maternal and neonatal outcomes in Korean women with type 1 diabetes and type 2 diabetes.
Methods We performed a retrospective survey of 163 pregnancies in women with type 1 diabetes (
n =13) and type 2 diabetes (n =150) treated from 2003 to 2010 at Cheil General Hospital & Women's Healthcare Center, Korea. We compared maternal characteristics as well as maternal and neonatal outcomes between groups.Results Differences in glycosylated hemoglobin between type 1 and type 2 diabetes were not significant. Birth weight (3,501±689.6 g vs. 3,366±531.4 g) and rate of major congenital malformations (7.7% vs. 5.6%) were not significantly different. However, women with type 1 diabetes had higher rates of preeclampsia (38.5% vs. 8.2%,
P =0.006), large for gestational age (LGA; 46.2% vs. 20.4%,P =0.004), macrosomia (38.5% vs. 13.4%,P =0.032), and admission for neonatal care (41.7% vs. 14.8%,P =0.03) than women with type 2 diabetes.Conclusion Maternal and neonatal outcomes for women with type 1 diabetes were poorer than for women with type 2 diabetes, especially preeclampsia, LGA, macrosomia and admission to the neonatal intensive care unit.
-
Citations
Citations to this article as recorded by- The Impact of Type 2 Diabetes on Women’s Health and Well-being During Their Reproductive Years: A Mixed-methods Systematic Review
Aycan Celik, Rita Forde, Simona Racaru, Angus Forbes, Jackie Sturt
Current Diabetes Reviews.2022;[Epub] CrossRef - Application of the electronic nose in predicting preeclampsia in high-risk pregnancies. Pilot study
Karen Beatriz Méndez Rodríguez, Luis Manuel Ramírez Gómez, Leticia Carrizales Yáñez, Rogelio Flores Ramírez, Omar Ornelas-Rebolledo, Jaime Antonio Borjas-García, Francisco Pérez-Vázquez, Maribel Rodríguez Aguilar
Archives of Medical Research.2021;[Epub] CrossRef - Obstetric and neonatal complications among women with autoimmune disease
Andrew Williams, Katherine Grantz, Indulaxmi Seeni, Candace Robledo, Shanshan Li, Marion Ouidir, Carrie Nobles, Pauline Mendola
Journal of Autoimmunity.2019; 103: 102287. CrossRef - Effects of maternal age, parity and pre-pregnancy body mass index on the glucose challenge test and gestational diabetes mellitus
Adel T. Abu-Heija, Majeda R. Al-Bash, Moza A. Al-Kalbani
Journal of Taibah University Medical Sciences.2017; 12(4): 338. CrossRef - Deficient Vitamin E Uptake During Development Impairs Neural Tube Closure in Mice Lacking Lipoprotein Receptor SR-BI
Nicolás Santander, Carlos Lizama, María José Parga, Alonso Quiroz, Druso Pérez, Guadalupe Echeverría, Lorena Ulloa, Verónica Palma, Attilio Rigotti, Dolores Busso
Scientific Reports.2017;[Epub] CrossRef
- The Impact of Type 2 Diabetes on Women’s Health and Well-being During Their Reproductive Years: A Mixed-methods Systematic Review
- Gestational Diabetes Mellitus in Korean Women: Similarities and Differences from Other Racial/Ethnic Groups
- Catherine Kim
- Diabetes Metab J. 2014;38(1):1-12. Published online February 19, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.1.1
- 3,509 View
- 33 Download
- 20 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Gestational diabetes mellitus (GDM) reflects defects in insulin secretion in response to the metabolic demands of pregnancy. While GDM is increasingly common worldwide due in large part to the obesity epidemic, its frequency is relatively low in Korean women. In this report, the prevalence and risk factors for GDM, perinatal outcomes, and postpartum course are compared in non-Korean and Korean women. While Koreans and non-Koreans with GDM share pathophysiology and complications, there may be differences in the role of obesity and thus the effectiveness of interventions targeting obesity in GDM women. Further investigations of the effectiveness of weight loss interventions and pharmacotherapy specifically among Korean women are needed. Dietary and other lifestyle data from Korean populations could inform prevention and treatment strategies in other countries which suffer from significantly higher prevalences of GDM.
-
Citations
Citations to this article as recorded by- More Physical Exercise is Required for Overweight or Obese Women with Gestational Diabetes Mellitus to Achieve Good Plasma Glucose Control During Pregnancy: Finding from a Prospective Cohort in Shanghai
Xiangjin Gao, Xiuqi Zhang, Le Kuai, Qing Yang, Huan Li, Rui Zhang, Bin Li, Ruiping Wang
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 3925. CrossRef - The role of plasminogen activator inhibitor-1 in gynecological and obstetrical diseases: An update review
Jiaqi Zhai, Zijian Li, Yue Zhou, Xiuhua Yang
Journal of Reproductive Immunology.2022; 150: 103490. CrossRef - Gestational diabetes in Korea: Temporal trends in prevalence, treatment, and short-term consequences from a national health insurance claims database between 2012 and 2016
Chan-Hee Jung, Sang-Hee Jung, Dughyun Choi, Bo-Yeon Kim, Chul-Hee Kim, Ji-Oh Mok
Diabetes Research and Clinical Practice.2021; 171: 108586. CrossRef - Maternal Nutrition Status Associated with Pregnancy-Related Adverse Outcomes
Maria J Miele, Renato T Souza, Iracema M Calderon, Francisco E Feitosa, Debora F Leite, Edilberto A Rocha Filho, Janete Vettorazzi, Jussara Mayrink, Karayna G Fernandes, Matias C Vieira, Rodolfo C Pacagnella, José G. Cecatti
Nutrients.2021; 13(7): 2398. CrossRef - Pregnancy Outcomes of Women Additionally Diagnosed as Gestational Diabetes by the International Association of the Diabetes and Pregnancy Study Groups Criteria
Min Hyoung Kim, Soo Heon Kwak, Sung-Hoon Kim, Joon Seok Hong, Hye Rim Chung, Sung Hee Choi, Moon Young Kim, Hak C. Jang
Diabetes & Metabolism Journal.2019; 43(6): 766. CrossRef - Environmental neglect: endocrine disruptors as underappreciated but potentially modifiable diabetes risk factors
Robert M. Sargis, Rebecca A. Simmons
Diabetologia.2019; 62(10): 1811. CrossRef - Prediction of gestational diabetes mellitus in the Born in Guangzhou Cohort Study, China
Kimberly K. Schaefer, Wanqing Xiao, Qiaozhu Chen, Jianrong He, Jinhua Lu, Fanfan Chan, Niannian Chen, Mingyang Yuan, Huimin Xia, Kin Bong Hubert Lam, Jane E. Hirst, Xiu Qiu
International Journal of Gynecology & Obstetrics.2018; 143(2): 164. CrossRef - Effects of the interaction between glycated haemoglobin genetic risk score and postpartum weight reduction on glycaemic changes: A gene–weight interaction analysis
Liyuan Han, Donghui Duan, Shuang Zhang, Weiqin Li, Leishen Wang, Huikun Liu, Junhong Leng, Nan Li, Xiaoyun Shang, Gang Hu, Lu Qi
Diabetes, Obesity and Metabolism.2018; 20(12): 2733. CrossRef - Adipokines and Insulin Resistance According to Characteristics of Pregnant Women with Gestational Diabetes Mellitus
Eon Ju Jeon, Seong Yeon Hong, Ji Hyun Lee
Diabetes & Metabolism Journal.2017; 41(6): 457. CrossRef - The MC4R genotype is associated with postpartum weight reduction and glycemic changes among women with prior gestational diabetes: longitudinal analysis
Aline Martins de Carvalho, Ping Shao, Huikun Liu, Han-Ling Cheng, Yan Zheng, Junhong Leng, Weiqin Li, Tao Huang, Tiange Wang, Leishen Wang, Shuang Zhang, Gang Hu, Lu Qi
Scientific Reports.2017;[Epub] CrossRef - Simple Screening Using Ultrasonography for Prediction of Gestational Diabetes Mellitus
Seung Min Chung, Jun Sung Moon
Diabetes & Metabolism Journal.2017; 41(6): 438. CrossRef - Prevention of type 2 diabetes mellitus in women with previous gestational diabetes mellitus
Joon Ho Moon, Soo Heon Kwak, Hak C. Jang
The Korean Journal of Internal Medicine.2017; 32(1): 26. CrossRef - Expression of intercellular adhesion molecule-1 in umbilical vascular of pregnant women with gestational diabetes mellitus and the clinical significance
Fei Teng, Jinfang Wu, Min Wei, Yongxiu Yang
Experimental and Therapeutic Medicine.2017;[Epub] CrossRef - Diagnostic value of haemoglobin A1c in post‐partum screening of women with gestational diabetes mellitus
K.‐S. Kim, S.‐K. Kim, Y.‐W. Cho, S. W. Park
Diabetic Medicine.2016; 33(12): 1668. CrossRef - Comparison of the performance of screening test for gestational diabetes in singleton versus twin pregnancies
Yun Ji Jung, Ja Young Kwon, Hee Young Cho, Yong-Won Park, Young-Han Kim
Obstetrics & Gynecology Science.2015; 58(6): 439. CrossRef - Circulating retinol-binding protein 4 levels in gestational diabetes mellitus: a meta-analysis of observational studies
Qi-Tao Huang, Qiong Huang, Wei Luo, Fei Li, Li-Lin Hang, Yan-Hong Yu, Mei Zhong
Gynecological Endocrinology.2015; 31(5): 337. CrossRef - Transition of maternal and child nutrition in Asia
Pattanee Winichagoon
Current Opinion in Clinical Nutrition and Metabolic Care.2015; 18(3): 312. CrossRef - Diabetes in Asians
Eun-Jung Rhee
Endocrinology and Metabolism.2015; 30(3): 263. CrossRef - The rs2237892 Polymorphism in KCNQ1 Influences Gestational Diabetes Mellitus and Glucose Levels: A Case-Control Study and Meta-Analysis
Deng Ao, Hai-jun Wang, Li-fang Wang, Jie-yun Song, Hui-xia Yang, Yan Wang, Marta Letizia Hribal
PLOS ONE.2015; 10(6): e0128901. CrossRef - Late Preterm Infants' Outcome Born from Mothers with Positive Screening but Negative Diagnostic Test for Gestational Diabetes
Jeong Min Lee, Bo Seon Seo, Eun Sun Kim
Korean Journal of Perinatology.2015; 26(3): 200. CrossRef
- More Physical Exercise is Required for Overweight or Obese Women with Gestational Diabetes Mellitus to Achieve Good Plasma Glucose Control During Pregnancy: Finding from a Prospective Cohort in Shanghai
- Insulin Resistance During Pregnancy.
- Kyu Jeung Ahn
- Korean Diabetes J. 2009;33(2):77-82. Published online April 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.2.77
- 1,795 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - Pregnancy is a complex metabolic state involving dramatic alterations in the hormonal or cytokine environments (increases in estrogen, progesterone, prolactin, cortisol, human chorionic gonadotropin, placental growth hormone and human placental lactogen, TNF-alpha, resistin, leptin, and a decrease in adiponectin) as well as an increasing burden of fuel utilization by the conceptus. Metabolically, the first trimester is characterized by increased insulin sensitivity and lipogenesis. The second and third trimesters, in contrast, are characterized by insulin resistance and increased lipolysis.
- A Case of Diabetic Ketoacidosis in Gestational Diabetes Mellitus.
- Myung Hwan Kim, Eui Dal Jung, Seung Pyo Hong, Gyu Hwan Bae, Sun Young Ahn, Eon Ju Jeon, Seong Yeon Hong, Ji Hyun Lee, Ho Sang Son
- Korean Diabetes J. 2007;31(4):368-371. Published online July 1, 2007
- DOI: https://doi.org/10.4093/jkda.2007.31.4.368
- 2,052 View
- 27 Download
-
 Abstract
Abstract
 PDF
PDF - Gestational diabetes mellitus (GDM) is defined as glucose intolerance of variant severity with onset or first recognition during present pregnancy. Recently the prevalence of GDM in Korean has reported as 1.7~4.0%. Diabetic ketoacidosis is a serious metabolic complication of diabetes with high mortality if undetected. Its occurrence is very rare in gestational diabetes patients, but is harmful to fetal and maternal health. A 26 years-old pregnant woman was admitted at 37 weeks gestation because of progressive generalized weakness, anorexia and weight loss. Initial physical examination reveals that she had been dehydrated, and blood pressure 130/80 mmHg, pulse rate 100/min, respiratory rate 20/min, and body temperature was 36.9 degrees C. Serum glucose was 545 mg/dL, pH 7.282, HCO3- 10.5 mmol/L, urine ketone 3+, urine glucose 2+ when initial laboratory work was done. She was treated with intravenous fluid and insulin under the impression of diabetic ketoacidosis. Her delivery was performed after 24 hours from admission because of suggestive fetal distress. After recovery, she is being treated with insulin at outpatient department. We experienced a appropriately treated case of diabetic ketoacidosis in pregnant woman with GDM, and report it with a literature review.
- Pregnancy Outcome in Korean Women with Gestational Diabetes Mellitus Diagnosed by the Carpenter-Coustan Criteria.
- Hak Chul Jang, Young Min Cho, Kyong Soo Park, Seong Yeon Kim, Hong Kyu Lee, Moon Young Kim, Jae Hyug Yang, Son Moon Shin
- Korean Diabetes J. 2004;28(2):122-130. Published online April 1, 2004
- 1,164 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The American Diabetes Association recently proposed the Carpenter-Coustan criteria for the diagnosis of gestational diabetes mellitus(GDM) based on the results of the Toronto Tri-Hospital Study. The prevalence of GDM in Korean women increased, on average, by 60% when the Carpenter-Coustan criteria were applied. However, the pregnancy outcome of Korean women with GDM with regard to the Carpenter-Coustan criteria tremains to be reported. The pregnancy outcomes of those Korean women with GDM by the Carpenter- Coustan criteria, but not by the NDDG criteria were assessed. METHODS: In this study, a total of 2776 pregnant women underwent universal screening for GDM, between January 1993 and December 1994, as recommended by the Third International Workshop-Conference on Gestational Diabetes Mellitus with minor modifications. The primary pregnancy outcomes were preeclampsia, premature delivery, delivery by C-section, birth weight and LGA infants. RESULTS: Of the 2776 women, 656 screened-positive for GDM. Of these, 37 and 74 had GDM by the Carpenter-Coustan and NDDG criteria, respectively. With increasing glucose intolerance, there was a stepwise increase in premature deliveries, deliveries by C-section and preeclampsia from those screening negative to GDM by the NDDG criteria, with a similar trend for the frequency of LGA infants. The LGA infant screening-negative and positive were 13.5 and 16.1%, but those with a normal glucose tolerance were 27.0 and 33.8% in those screening positive to GDM by the Carpenter-Coustan and NDDG criteria, respectively(P<0.001). CONCLUSION: Our study demonstrated that increasing glucose tolerance was associated with increasing frequencies of adverse pregnancy outcomes in Korean women. The maternally complicated and LGA infants were significantly higher in women with GDM by the Carpenter-Coustan criteria. Thus the Carpenter- Coustan criteria are recommended for the diagnosis of GDM in Korean Women.
- Effect of Self-monitoring of Blood Glucose on Pregnancy Outcome in Women with Mild Gestational Diabetes.
- Hak Chul Jang, Jeong Eun Park, Chang Hoon Yim, Ho Yeun Chung, Ki Ok Han, Hyun Koo Yoon, In Kwon Han, Moon Young Kim, Jae Hyug Yang, Mi Jung Kim, Sun Young Ko, Yeon Kyung Lee
- Korean Diabetes J. 2001;25(1):93-102. Published online February 1, 2001
- 1,342 View
- 28 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Self-monitoring of blood glucose (SMBG) and intensive therapy with insulin demonstrated to have a positive effects in the reduction of the neonatal complications in women with gestational diabetes (GDM). However the utility of SMBG in the mild GDM who does not requiring insulin has not been formally reported. Therefore, to evaluate the effectiveness of SMBG in the management of mild GDM, we compared the pregnancy outcome and the postpartum glucose tolerance of women who monitored their glycemic control by SMBG to those of women who monitored by laboratory glucose test at each office visit during pregnancy. METHODS: We studied 185 women diagnosed as a GDM by NDDG criteria and their fasting glucose concentration < 5.8 mM. All subjects had singleton pregnancy,and no medical diseases that may affect fetal growth, and were certain of gestational age by early ultrasonography. They were treated with an identical GDM management protocol except glucose monitoring. One hundred five women were monitored by laboratory glucose test at each office visit (office group) and 80 women were monitored by SMBG (SMBG group). Pregnancy outcome including rates of cesarian section, obstetric complication, LGA infant and glucose tolerance status at postpartum were compared between two groups. RESULTS: The age, height, prepregnancy weight, weight at delivery and parity were not significantly different between the two groups. Fasting, 1-h, 2-h glucose concentration during the diagnostic test of GDM in SMBG group were similar to those of office group. However, 3-h glucose concentration of office group was 0.3 mM higher than that of SMBG group. The rate of primary cesarian section, preterm labor and pregnancy-induced hypertension of SMBG group were similar to those of office group. The mean postprandial 2-h glucose concentration of office group measured at each office was 0.5 mM higher than that of SMBG group. Although 5% of office group were treated with insulin, 24% of SMBG group were requiring insulin therapy. The birth weight and LGA infant rate of office group were 3403 432 g and 28%, those were heavier and higher than those of SMBG group (3169 447 g, 13.8%). The 90% of office group and 84% of SMBG group were performed 75 g oral glucose tolerance test at postpartum 6-8 weeks. There was no significant difference in rates of diabetes and IGT between office and SMBG group (9.5%, 11.6%; 7.5%, 9.0% respectively). CONCLUSIONS: This study demonstrated that SMBG is very seful in early detection of maternal hyperglycemia and lowing the postprandial glucose, as well as reducing the rate of LGA infants in women with mild GDM.
- Clinical Characteristics and Pregnancy Outcome in Korean Women with Type I & Type II Diabetes Mellitus.
- Yoon Huh, Dong Won Suh, Hak Chul Jang, Chang Hoon Yim, Ki Ok Han, Hyun Ku Yoon, In Kwon Han, Hun Ki Min, Eun Sung Kim, Moon Young Kim, Hyun Mi Ryu, Sung Won Yang, Hae Kyoung Han
- Korean Diabetes J. 1998;22(3):353-362. Published online January 1, 2001
- 1,477 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The prevalence of diabetes is gradually increasing iin Korean. Moreover, the prevalence of pregnancy complicated by established diabetes seems to be increasing. During the past decades, advances in the diabetes care as well as advances in fetal surveillance and neonatal care, have continued to improve pregnancy outcome of women with diabetes. However, the incidence of congenital anomalies and spontaneous abortion as well as the perinatal morbidity in the women with diabetes are still higher compared to those of the general population. In this study, we estimated the prevalence of prepmncy complicated by both type 1 and type 2 diabetes and described the clinical characteristics and outcome of diabetic pregnancies. METHODS: We analyzed data from four sources: 1) the mother(type and duration of diabetes, diabetic complication, preconceptional care), 2) obstetric outcome(method of delivery, obstetric complication), 3) neonatal outcome(birth weight, perinatal complication, congenital anomaly), 4) glycemic control during pregnancy, of women with pregestational diabetes delivered newborns at Samsung Cheil Hospital from 1992 to 1995. RESULTS: During the study period, 34 singleton infants were delivered by the 28 women with diabetes. The diabetic pregnancy was present in 0.14% of total deliveries in Samsung Cheil Hospital. Patients with IDDM comprised 18%(6/34) of total diabetic pregnancies, 82%(28/34) had NIDDM. The duration of diabetes was 6.3 and 2.1 years in patients with IDDM and NIDDM, respectively. Two IDDM patients presented with proliferative retinopathy, and 3 background retinopathy, one in IDDM and 2 in NIDDM. Three patients with IDDM and 2 patients with NIDDM had diabetic nephropathy. Insulin requirement during pregnancy was increased about 2 times at the time of delivery when compared to the initial in women with IDDM and NIDDM. Preeclampsia was the most common obstetric compliications, which were more frequently observed in women with diabetic complications. LGA was present in 43% of women with NIDDM. One infant of mother with NIDDM, delivered at 28 weeks gestation, was died because of respiratory distress and one infant of mother with IDDM had a congenital heart disease(TOF). Only 3 patients scught for the preconceptional care before pregnancy. CONCLUSION: Pregnancies complicated by diabetes was more frequent than was expected, even though it was much less than the rates in North America. Only 9% of women with diabetes had preconceptional care before pregnancy. The importance of planned pregnancy and prepregnancy counseling should be addressed in women with diabetes of child bearing age.

 KDA
KDA
 First
First Prev
Prev





